Abstract
Context
Emergency action plans (EAPs) are a critical component in the management of catastrophic sport-related injury. Some state high school athletics associations and state legislation have required that schools develop EAPs, but little research exists on the influence of a statewide policy requirement on local adoption of these policies.
Objective
To examine the efficacy of a statewide policy requirement on local adoption of an EAP.
Design
Cross-sectional study.
Setting
Online questionnaire.
Patients or Other Participants
Secondary school athletic trainers were invited to complete a survey (n = 9642); 1136 completed the survey, yielding an 11.7% response rate.
Main Outcome Measure(s)
Survey responses on the adoption of EAPs along with cardiopulmonary resuscitation and automated external defibrillator (CPR/AED) requirements were cross-referenced with published statewide policies to determine the prevalence of EAP adoption. We evaluated the adoption of emergency action plan components based on the National Athletic Trainers' Association's emergency planning position statement along with CPR/AED requirements to determine component-specific prevalence. We compared the prevalence of EAP and component adoption between states that required EAPs and specific components of EAPs and states without such requirements.
Results
Athletic trainers in states that required adoption of an EAP reported including more components of the emergency planning position statement (mean = 8 ± 4, median = 9) than in states without a requirement (mean = 7 ± 4, median = 8). The adoption of EAP components did not differ between states that required specific components of the EAP versus development of the EAP only. However, schools in states with both EAP and CPR/AED training requirements reported higher rates of CPR/AED training implementation (95.5%) than states that only required CPR/AED training (81.6%, prevalence ratio = 1.10, 95% confidence interval = 1.01, 1.20).
Conclusions
Based on these data, statewide policy requirements for the development of an EAP may be associated with increasing adoption of EAPs.
Keywords: sports, athletics, catastrophic injury, emergency action plan
Key Points
Identifying the factors that may influence the adoption of emergency action plans (EAPs) in the secondary school setting is imperative.
Athletic trainers working in secondary schools in states that require EAP development tended to adopt a greater proportion of the components of an EAP than those who worked in states without such a requirement.
The prevalence of schools reporting compliance with cardiopulmonary resuscitation and automated defibrillator training for all coaches was highest in states that required both such training and the development of an EAP.
With roughly 8 million student-athletes participating in secondary school sports,1 the risk of a potential catastrophic injury must not be minimized. Between 1982 and 2017, an estimated 777 fatal catastrophic and 1169 nonfatal catastrophic injuries were reported at the secondary school level in the United States.2 Although the cause and outcome of a catastrophic sport-related injury are often multifactorial, a number of strategies, including the development of comprehensive emergency planning, can optimize outcomes.
A method of addressing the emergency preparedness of a secondary school athletics program is the adoption of an emergency action plan (EAP).3 The EAP is an essential component for managing patients with catastrophic injuries, as it provides a succinct, step-by-step plan of action to guide individuals providing care. Survival after sudden cardiac arrest, the leading cause of death in sport and physical activity, was 79% in high schools with an established EAP versus 44% in those without.4 Additionally, exertional heat stroke is 100% survivable with prompt recognition and care via activation of an EAP.5 However, despite the need for EAPs, the results of a recent study6 suggested that athletic trainers (ATs) are not adopting comprehensive policies to prevent catastrophic injuries. In this sports medicine research, adoption was defined as survey responses delineating the school had an EAP.6 A total of 90% of ATs stated they had some form of a written EAP, yet only 9% reported adopting a comprehensive EAP with all 12 components that were outlined in the “National Athletic Trainers' Association Position Statement: Emergency Planning in Athletics” (NATA-PS).3,6 It is vital to begin to understand the factors influencing policy adoption, including facilitators, barriers, and social determinants.
Using the socioecological framework,7–9 we can conceptualize strategies to improve compliance with policy components into various levels of influence: intrapersonal, interpersonal, organizational, environmental, and policy. Policies can be set at the national (eg, federal legislation or national governing body requirements), state (state-enacted legislation or state high school athletics association requirements), county, district, or school level. For readership ease, statewide level in this paper is defined as the policies that apply to secondary schools in a given jurisdiction emanating from either state legislation or a high school athletics association. One approach, requiring a policy by statewide authorities, has been successful in influencing interpersonal and organizational adoption of the policy.10 Previous investigators11,12 found that statewide policy requirements (both state high school athletics association policy requirements and state-enacted legislation) affected local implementation of policies in areas such as heat acclimatization and sport-related concussion. If a policy is required by the state high school athletics association, all member schools in that state are required to abide by the policy in order to participate in the state's athletics association. Although recommendations are likely beneficial, statewide policy requirements have been associated with improved adoption at the local secondary school level.12–14 Regarding EAPs, ATs reported that a statewide policy requirement for an EAP can be a facilitator for development.15 Among states, 51% required the development of an EAP for secondary school athletics programs.16,17 Similarly, 70.5% of states required all coaches to be trained in cardiopulmonary resuscitation (CPR), automated external defibrillator (AED) use, and first aid.17
Emergency planning and essential training, such as in CPR and AED use, can be the difference between life and death. Of the sudden cardiac arrest events that occurred during organized sport participation, more than half (59%) affected secondary school athletes.18 Timely CPR initiation and AED application have been demonstrated to dramatically improve survival rates for patients suffering from an out-of-hospital sudden cardiac arrest.4,18,19 Recently, Drezner et al18 identified a 63% survival rate in athletes (middle school, high school, collegiate, semiprofessional, and professional level) when bystander CPR was provided. Further, research20 suggested that survival rates declined 7% to 10% for every minute that defibrillation with an AED was delayed in patients with out-of-hospital cardiac arrests. Statewide policy requirements for all coaches to be CPR/AED and first aid trained may enhance the number of coaches who are trained and thereby positively affect patient outcomes.
Requiring best practices at the policy level of the socioecological model appears to result in the most effective change.10 Although previous investigators have noted a relatively high adoption level of EAP best practices, it is important to better understand the factors that influence the adoption of these policies. The presence of best-practice health and safety policy requirements has been examined at the state level16,17; however, whether statewide policy requirements affect local emergency planning policy development for the adoption of EAPs and CPR/AED training is unknown. Therefore, the purpose of our study was to examine the effect of statewide policy requirements for the development of EAPs on local policy adoption in secondary school athletics.
Hypothesis 1
Athletic trainers in states that require schools to develop an EAP would adopt more components from the NATA-PS than states that did not require schools to develop an EAP.
Hypothesis 2
The prevalence of school compliance with the NATA-PS components would be highest in states that require adoption of the individual components outlined in the NATA-PS for developing an EAP.
Hypothesis 3
The prevalence of schools requiring CPR/AED and first aid training for coaches would be highest in states that require all coaches to complete this training.
METHODS
We used a cross-sectional survey research design. The survey was designed in a manner similar to that of previous researchers and focused on compliance with the NATA-PS.3,12 This study was classified as exempt by the University of Connecticut Institutional Review Board. The data presented in this manuscript are part of a larger study outlined by Scarneo et al.6
Study Recruitment
Participants invited to complete the survey were ATs employed in US secondary schools in the fall of 2017. Only ATs who were either NATA members or had participated in the Athletic Training Locations and Services (ATLAS) Project21 and had also consented to e-mail contact for research purposes via both entities were invited to enroll (n = 9642).
Survey Instrument
The aim of the survey (which has been described previously6) was to evaluate the school's adoption of the 12 components listed in the NATA-PS. Participants were asked to self-report if they had policies and procedures related to EAPs. The survey had been pilot tested with a random sample of 30 ATs who provided care to high school athletes. After the pilot study, we conducted phone interviews to identify gaps in the survey content. Revisions were based on the pilot survey and phone interview data and mainly involved clarifying wording of the questions. Data from the larger study were presented in Scarneo et al.6
Participants
Participants on both the NATA and ATLAS distribution lists who allowed email communication for research purposes were contacted (n = 9642). Nonrespondents received 1 email follow-up reminder 2 weeks after the initial request was sent. Of the 9642 ATs who were invited to take the survey, 1445 started and 1136 completed the survey, yielding an 11.7% response rate. Complete surveys were classified as those with at least 80% of the questions answered, but to have their data included, respondents had to answer the question: “Does your athletics department have a written EAP for managing serious and/or potentially life-threatening sport-related injuries?” Two individuals did not provide a state and, thus, their data were excluded from analysis.
Data Related to Requirements of EAP Development
Adams et al17 evaluated statewide requirements for health and safety policies related to the leading causes of sport-related death and catastrophic injury.22 Each state's high school athletics association, state-enacted legislation, and Department of Education policies were assessed. Health and safety policies were included if they were mandated for state member high schools; those that were only recommended were not included. For a more detailed discussion of the methods used to assess statewide health and safety policies, refer to the aforementioned study.17 For the purpose of this investigation, we used the data on EAP policies required to be developed at the state level from that study.17 For consistency with Adams et al,17 only EAP policies that were mandated for each state's member schools (ie, state high school athletics association-required policies and state-enacted legislation) were included in this investigation. Additionally, we aimed to evaluate the effect of a statewide policy requirement for CPR/AED and first aid training for all coaches on the local adoption of this policy. The emergency preparedness policies that were extracted and used for the current study as well as the states that require these policies are outlined in Table 1. Though we recognize that the United States consists of 50 states and the District of Columbia, we refer to all 51 jurisdictions as states for readership ease.
Table 1.
Components of an Emergency Action Plan (EAP) as Outlined in the National Athletic Trainers' Association Position Statement: Emergency Planning in Athletics
| Policy |
No. of States (All 50 states and Washington DC) that Mandated (from Adams et al17) |
| 1. The athletics department has a written EAP for managing serious and/or potentially life-threatening sport-related injuries. | 26 states: AK, AL, AR, DC, DE, GA, IL, KY, MA, ME, MI, MN, MO, NC, NJ, NM, OH, OR, RI, SC, SD, TN, TX, VA, WA, WV |
| Specific component of EAP | |
| 2. Is developed and coordinated with local EMS, school public safety officials, onsite medical personnel or school medical staff, and school administrators. | 10 states: DE, GA, IL, KY, MA, MO, NC, NJ, WA, WV |
| 3. Is distributed and reviewed by all relevant athletics staff members annually. | 10 states: AL, IL, KY, MO, NC, NJ, SD, TX, VA, WV |
| 4. Each venue (practice field, competition field, gym, weight room, etc) athletes play at has its own EAP. | 15 states: AK, AL, AR, DE, IL, KY, MA, MN, MO, NC, NJ, NM, SD, VA, WV |
| 5. Identifies location of onsite emergency equipment. | 10 states: DE, IL, KY, MA, MO, NC, NJ, NM, VA, WV |
| 6. Identifies personnel and their responsibilities to carry out the plan of action with designated chain of command. | 10 states: DE, IL, KY, MA, MO, NC, NJ, TX, VA, WV |
| 7. Lists contact information for EMS and other key personnel, as well as facility address, location. | 12 states: DE, IL, KY, MA, MO, NC, NJ, NM, TX, VA, WA, WV |
| 8. Provides recommendations for documentation that should be taken after a catastrophic incident. | 4 states: IL, KY, MO, NC |
| 9. Is rehearsed annually by AT, AD, coaches, other pertinent medical personnel. | 17 states: AK, AL, AR, IL, KY, MA ME, MI, MO, NC, RI, SD, TN, TX, VA, WA, WV |
| 10. Includes information for health care professionals providing medical coverage which is included in the review and rehearsal. | 11 states: DE, IL, KY, MA, MO, NC, NJ, TX, VA, WA, WV |
| 11. Is updated annually by all relevant athletics staff members. | Not evaluated for state comparisons |
| 12. The EAP is posted at every venue. | Not evaluated for state comparisons |
| Additional component of interest | |
| CPR/AED and first aid training are required for all coaches. | 30 states: AK, AL, AR, AZ, CA, CT, DC, DE, HI, ID, KY, ME, MS, MO, NC, ND, NH, NJ, NM, NV, NY, OH, PA, RI, TX, UT, VT, WA, WI, WY |
Statistical Analysis
Analyses were performed in SPSS (version 24; IBM Corp, Armonk, NY) with an a priori significance level of .05 and conducted in the summer and fall of 2018. We were interested in how compliance by ATs differed between states whose state high school athletics association or state legislation for EAPs met (with-requirement group) or did not meet (without-requirement group) the criteria set forth by the NATA-PS. The main outcome measure (dependent variable) was compliance with the EAP guidelines, as provided by our survey data. The main exposure (independent variable) was states with or without a statewide policy requirement, as demonstrated by previous research.17
For hypothesis 1, we first calculated, for each respondent, the number of EAP-related guidelines that were reported to be compliant with the NATA-PS. Because the resulting sums are discrete count data and thus followed a Poisson distribution, we used a Wilcoxon rank-sum test to compare distributions between respondents from states with and those without a requirement for EAPs.
For hypothesis 2, we examined each EAP policy component individually. Adams et al17 evaluated 10 of the 12 components for EAP implementation at the state level—the overall development of an EAP along with 9 components of the NATA-PS. Therefore, we evaluated 10 of the 12 components for comparison with the previous Adams et al paper.17 To aid in interpretation of the differences that might exist between groups, we calculated prevalence ratios (PRs). All PRs with 95% confidence intervals (CIs) excluding 1.00 were considered statistically significant.
Because a state may require the development of an EAP but not a specific component, we conducted additional analyses to further stratify the with-requirement category into (1) respondents from states with both the general EAP component and the specific component requirement and (2) respondents from states with only the general EAP requirement. For example, as noted in Table 1, 26 states had the general EAP requirement; however, only 10 states had the specific component of identifying the location of onsite emergency equipment. Thus, respondents in these 10 states would be included in the EAP and component-requirement group, whereas those in the remaining 16 states would be included in the EAP-requirement group; the additional 25 states remained in the without-requirement group. Prevalence ratios were calculated to compare between groups; a 95% CI that excluded 1.00 signified statistical significance.
For hypothesis 3, we examined the prevalence of respondents who reported that their school complied with a CPR/AED and first aid training requirement for coaches. Prevalence ratios compared respondents from states with versus without the CPR training requirement. All PRs with 95% CIs excluding 1.00 were considered statistically significant.
In an additional exploratory analysis, we then further stratified states into 4 categories: (1) states with both the general EAP and CPR training requirements (n = 15 states), (2) states with only the general EAP requirement (n = 11 states), (3) states with only the CPR requirement (n = 15 states), and (4) states with neither requirement (n = 10). Prevalence ratios were calculated to compare groups, with the exclusion of 1.00 in the 95% CI signifying statistical significance.
RESULTS
Descriptive Data
The largest percent ages of respondents were from Texas (8.5%, n = 97), followed by Pennsylvania (6.6%) and New Jersey (5.9%; Table 2). Responses were received from all states except Alaska and West Virginia. A majority of the ATs were female (56.9%), were white (89.6%), had obtained a master's degree (64.6%), and had been an AT for ≥15 years (39.6%). Most had been at their school for 1–5 years (39.5%) and were working in public schools (79.7%) with an average (mean ± SD) of 1239 ± 848 students and 476 ± 301 athletes.
Table 2.
Respondents by State
| State |
No. (%) |
| AL | 17 (1.5) |
| AR | 17 (1.5) |
| AZ | 21 (1.8) |
| CA | 66 (5.8) |
| CO | 22 (1.9) |
| CT | 24 (2.1) |
| DC | 1 (0.1) |
| DE | 8 (0.7) |
| FL | 26 (2.3) |
| GA | 23 (2.0) |
| HI | 11 (1.0) |
| IA | 15 (1.3) |
| ID | 6 (0.5) |
| IL | 39 (3.4) |
| IN | 27 (2.4) |
| KS | 17 (1.5) |
| KY | 11 (1.0) |
| LA | 15 (1.3) |
| MA | 35 (3.1) |
| MD | 23 (2.0) |
| ME | 14 (1.2) |
| MI | 31 (2.7) |
| MN | 21 (1.8) |
| MO | 20 (1.8) |
| MS | 6 (0.5) |
| MT | 4 (0.4) |
| NC | 46 (4.0) |
| ND | 5 (0.4) |
| NE | 7 (0.6) |
| NH | 19 (1.7) |
| NJ | 67 (5.9) |
| NM | 3 (0.3) |
| NV | 7 (0.6) |
| NY | 34 (3.0) |
| OH | 47 (4.1) |
| OK | 3 (0.3) |
| OR | 10 (0.9) |
| PA | 75 (6.6) |
| RI | 4 (0.4) |
| SC | 40 (3.5) |
| SD | 4 (0.4) |
| TN | 17 (1.5) |
| TX | 97 (8.5) |
| UT | 16 (1.4) |
| VA | 56 (4.9) |
| VT | 4 (0.4) |
| WA | 28 (2.5) |
| WI | 23 (2.0) |
| WY | 4 (0.4) |
| Total | 1136 (100.0) |
Hypothesis 1: Comparison of Number of Components Adopted Across Groups
Athletic trainers working in states that required schools to develop an EAP, specifically for the management of either serious or both serious and life-threatening sport-related injuries, complied with more NATA-PS components (mean = 8 ± 4, median = 9) than those in states without required development of an EAP (mean = 7 ± 4, median = 8). The Wilcoxon rank sum test showed that the groups differed (P = .02; Figure 1).
Figure 1.
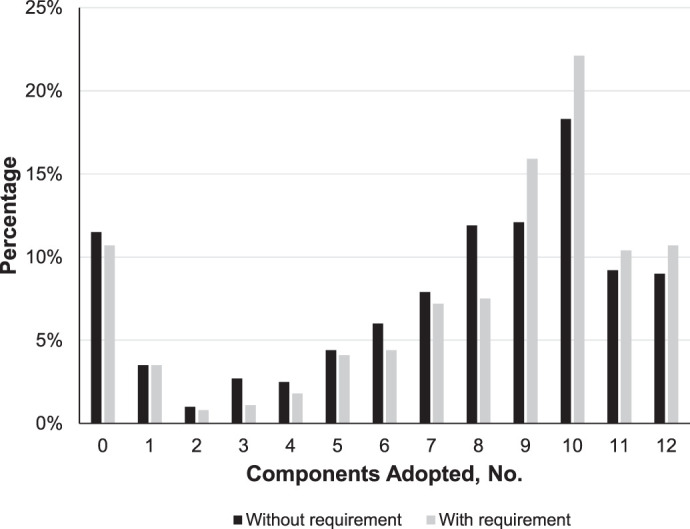
The distribution of the number of components of an emergency action plan (EAP) adopted at local secondary schools as reported by athletic trainers. In states that required schools to develop an EAP, 8 ± 4 components were adopted (median = 9). In states that did not require schools to develop an EAP, 7 ± 4 components were adopted (median = 8; Wilcoxon rank sum test P = .02).
Hypothesis 2: Comparison of Components Adopted Across Groups
Generally, the proportion of ATs who reported that their schools complied with NATA-PS components was higher in states that required versus did not require development of an EAP (Table 3). However, these differences were only statistically significant for 4 of the 10 NATA-PS recommendations. Furthermore, the proportion of ATs who indicated that their school complied with NATA-PS components was higher in states that required both a general EAP and specific EAP components versus those that did not require the development of an EAP; yet only 2 of the recommendations revealed differences (Table 3). In addition, requiring the development of an EAP led to the adoption of more components as recommended in the NATA-PS. Compliance with the general EAP development requirement did not differ between states that did versus did not require development of an EAP (component 1: 89.5% versus 88.5%, PR = 1.01; 95% CI = 0.97, 1.06).
Table 3.
Respondents Reporting Compliance With a Specific Policy Component by Whether or Not State Mandates Specific Components of an Emergency Action Plan (EAP)a
| Specific Component of EAPb |
Athletic Trainer Responses, % (n) |
Prevalence Ratio (95% CI) |
||||
| States With Both EAP and Component Mandates (Both) |
States With EAP Mandate Only (EAP Only) |
States Without EAP and Component Mandates (Without) |
With Both Versus Without |
With Both Versus EAP Only |
EAP Only Versus Without |
|
| 2. Is developed and coordinated with local EMS, school public safety officials, onsite medical personnel or school medical staff, and school administrators. | 84.3 (193/229) | 82.5 (466/565) | 77.1 (317/411) | 1.09c (1.01, 1.18) | 1.02 (0.96, 1.09) | 1.07c (1.002, 1.14) |
| 3. Is distributed and reviewed by all relevant athletics staff members annually. | 83.1 (255/307) | 83.2 (471/566) | 80.1 (330/412) | 1.04 (0.97, 1.11) | 1.00 (0.94, 1.06) | 1.04 (0.98, 1.10) |
| 4. Each venue (practice field, competition field, gym, weight room, etc) our athletes play at has its own EAP. | 92.7 (127/137) | 91.0 (506/556) | 90.3 (372/412) | 1.03 (0.97, 1.09) | 1.02 (0.97, 1.07) | 1.01 (0.97, 1.05) |
| 5. Identifies location of onsite emergency equipment. | 95.0 (227/239) | 94.3 (533/565) | 93.4 (380/407) | 1.02 (0.98, 1.06) | 1.01 (0.97, 1.04) | 1.01 (0.98, 1.04) |
| 6. Identifies personnel and their responsibilities to carry out the plan of action with designated chain of command. | 93.1 (295/317) | 93.6 (530/566) | 89.8 (370/412) | 1.04 (0.99, 1.08) | 0.99 (0.96, 1.03) | 1.04c (1.003, 1.08) |
| 7. Lists contact information for EMS and other key personnel, as well as facility address, location. | 93.4 (323/346) | 94.2 (533/566) | 89.9 (365/406) | 1.04 (0.99, 1.08) | 0.99 (0.96, 1.03) | 1.05c (1.01, 1.09) |
| 8. Provides recommendations for documentation that should be taken after a catastrophic incident. | 59.4 (57/96) | 63.2 (355/562) | 61.6 (250/406) | 0.96 (0.80, 1.16) | 0.94 (0.79, 1.12) | 1.03 (0.93, 1.13) |
| 9. Is rehearsed annually by AT, AD, coaches, other pertinent medical personnel. | 59.1 (220/372) | 59.2 (336/568) | 51.2 (210/410) | 1.15c (1.02, 1.31) | 1.00 (0.90, 1.11) | 1.15c (1.03, 1.30) |
| 10. Includes information for health care professionals providing medical coverage that is included in the review and rehearsal. | 71.6 (245/342) | 75.1 (425/566) | 72.4 (294/406) | 0.99 (0.90, 1.08) | 0.95 (0.88, 1.04) | 1.04 (0.96, 1.12) |
Hypothesis 3: Comparison of CPR/AED and First Aid Training Across Groups
The prevalence of schools reporting compliance with CPR/AED and first aid training was highest among respondents from schools in states with both CPR and EAP requirements (95.5%; Figure 2). The CPR and EAP requirement group had a higher prevalence of local adoption of this guideline than all other groups (PRs ranged from 1.17 to 1.29). The group with the next highest prevalence was the group that required CPR training only. The prevalence of schools complying with CPR/AED and first aid training was higher among the CPR requirement-only group than the EAP requirement-only group (81.6% versus 76.7%, respectively; PR = 1.10, 95% CI = 1.01, 1.20).
Figure 2.
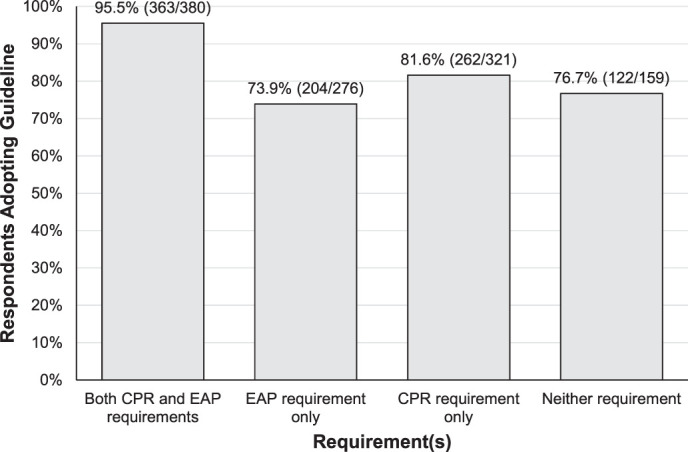
Prevalence of compliance with the component “CPR [cardiopulmonary resuscitation], AED [automated external defibrillator] and first aid training are required for all coaches at my school” compared across 4 groups: (1) state required CPR/AED guideline and development of an EAP, (2) state required development of an EAP only, (3) state required CPR/AED training only, and (4) state did not require either.
DISCUSSION
Previous researchers6,12 identified (and our results support) that, overall, a high percentage of ATs reported adoption of the best practices for developing an EAP. Our aim was to evaluate whether the association of statewide policy requirements facilitated even greater local policy adoption in the secondary school setting. By enhancing our understanding of facilitators and barriers that may affect EAP adoption, we can create strategies that are tailored to these findings to improve patient outcomes overall. Our study suggests that ATs working in secondary schools in states that required the development of an EAP tended to adopt a greater proportion of the components of an EAP compared with those who worked in states without a requirement. Furthermore, the proportion of ATs who reported their schools complied with the NATA-PS components appeared to be higher among those in states that required versus did not require development of an EAP. Finally, the prevalence of ATs at schools reporting compliance with CPR/AED training for all coaches was highest in states that required both CPR/AED training and the development of a general EAP. Overall, these results highlight that a statewide EAP requirement (via either the state high school athletics association or state-enacted legislation) may have a positive influence on local policy adoption by secondary school ATs.
Previous researchers11,12 who used the socioecological framework identified that the policy level, specifically at the state level, had a positive effect on local intervention adoption. Specifically, high school football programs in states with requirements regarding the implementation of exertional heat illness guidelines complied with more components of the NATA Inter-Association Task Force heat-acclimatization document than programs in states that did not require the guidelines.12,23 We found that the adoption of EAP components was highest by ATs who were working at secondary schools in states that required development of an EAP, demonstrating that statewide policy requirements may be effective for local adoption. Our data suggest that implementing this 1 component was associated with an overall increase in the number of components adopted at the local secondary school level.
The NATA-PS provided 12 components that are deemed essential for a comprehensive EAP. The first component, developing an EAP, is a necessary first step to implementing the remaining components outlined in the NATA-PS (ie, schools cannot implement components 2–12 without developing an EAP [component 1]). However, it is interesting to note that, when comparing the prevalence of compliance with individual components of an EAP (hypothesis 2), a specific statewide policy requirement for an individual component appeared to not be associated with the individual component analysis. For example, a statewide policy requirement for development of a general EAP (Table 1, component 1) appeared to not be associated with the overall adoption of an EAP at the local level (statewide policy requirement: 89.5% local adoption; no statewide policy requirement: 88.5% adoption). This finding raises the question of why a statewide policy requirement for a general EAP may be associated with more components being adopted (hypothesis 1) but not overall development of an EAP. Although many plausible explanations may exist, 1 explanation may be that the statewide policy requirement prompted the ATs to develop an EAP, and thus, they were using their educational experiences to develop an EAP that was more comprehensive. In contrast, those without an EAP may be unaware of the statewide policy or may be affected by other factors, such as a lack of administrative support to develop the EAP.
Few authors have addressed the effectiveness of each component individually, but the NATA-PS indicated that adoption of the guidelines would “provide prompt and proper emergency care.”3(p101) We noted that ATs in states that required schools to develop the EAP with emergency medical services to identify personnel and their responsibilities and to list contact information for emergency medical services had a greater prevalence of adopting the component compared with states without the requirements. However, it is important to remember that, despite the statistical significance, the clinical significance of these findings remains unknown. This is likely because of the large percentage of respondents who reported adoption, which in turn affected the PR.24 When the prevalence of adoption is lower, the prevalence ratio is greater, implicating stronger clinical relevance. Although these data may suggest an association between a statewide policy requirement and local adoption, future researchers should assess the strength of these findings in a prospective manner. Though we are speculating, we argue that a change of 1 policy may be clinically significant due to the likelihood that any positive change in the implementation of best practices may facilitate improved patient outcomes. We also aimed to stratify responses to evaluate the EAP-only group coupled with the individual component group (with both). The prevalence of school compliance between the groups did not differ. Similar to hypothesis 1, this result helps to support the notion that, if states are looking to implement a single component of the EAP guidelines, requiring schools to develop an EAP may be the most effective component recommended in the NATA-PS.
The presence of an onsite AED in sports facilities has been associated with increased survival in 93% of cases,19 highlighting the need for onsite AEDs and CPR training for potential responders (eg, coaches). Our findings showed that states that mandated schools to develop an EAP and to require CPR/AED and first aid training for all coaches displayed an increased prevalence of local secondary school adoption of these standards. Although we saw an increased proportion of local secondary school adoption in states that solely required CPR/AED and first aid training compared with no requirement, the benefit of a combination of EAP and CPR/AED requirements at the state level is clear. By improving local policy adoption through statewide policies, we can increase the survival rate for patients with sudden cardiac arrest and other catastrophic injuries.
Athletic trainers have reported that statewide policy requirements may help to facilitate EAP adoption15; however, we raise concern about the lack of adoption or implementation of these best practices with or without statewide policy requirements by trained health care professionals. Statewide policy is often determined by individuals who have no medical or health care background. State legislators or executive directors of the state high school athletics associations often determine whether a health and safety policy will be implemented—not a health care professional trained in the current best practices and best evidence. Therefore, these nonmedical individuals may (or may not) rely on health care professionals such as ATs to determine the policies that should be required. Athletic trainers currently practicing in the secondary school setting should consider using these data to start or support initiatives in their states that facilitate enhanced health and safety policies. By becoming more involved with the NATA committees (eg, Secondary School) or state legislative or sports medicine advisory committees to the state high school athletics associations, ATs can help to enhance the policies and standardize patient care across their states. This is especially important for those secondary schools without access to athletic training services. Future authors should investigate the effect of a statewide policy requirement on EAP adoption in schools with and those without an AT.
Limitations
The analyses performed for this study were conducted on a cross-sectional basis; therefore, we cannot prove causality. Also, survey research includes inherent limitations regarding recall and social desirability bias. Typical response rates for survey data are between 7% and 15%25; our response rate fell within this range (11.7%) and yielded 1136 responses. Given that more than 1000 ATs responded to each question and the CIs were relatively small, we are confident in our ability to draw meaningful conclusions from these data. Although 49/51 states were included in this sample, future research may benefit from state-specific studies to elucidate the factors that facilitate adoption in each state. Moreover, the purpose of this project was not to evaluate the origin of these policies (state high school athletics association or legislation). Therefore, we cannot determine which method might be more effective than another. Future investigators should identify the clinically meaningful difference in the adoption of policies: in other words, how many EAP policy components are needed to improve patient outcomes. Regarding the components of the EAP, we are not aware of evidence to support the adoption of all 12 versus fewer components of the NATA-PS in optimizing outcomes. In other words, we can only speculate that adopting more components of an EAP is better than adopting fewer components. The data provided in this study may offer preliminary evidence to support the implication of statewide policy requirement on local policy adoption. Therefore, future authors should prospectively investigate the implementation of EAPs at the state level following statewide policy requirements.
CONCLUSIONS
The presence of statewide policy requirements for EAPs appeared to be associated with the local adoption of policies in secondary schools. With a statewide policy requirement for the development of an EAP, a higher proportion of schools reported compliance with the components of an EAP versus states without the requirement. Moreover, the proportion of ATs who indicated their schools complied with the requirement that coaches be CPR/AED and first aid trained was higher in states that required development of an EAP and CPR/AED training. Overall, the results of this investigation highlight that a statewide policy requirement appeared to have a positive influence on local policy adoption by secondary school ATs. Athletic trainers practicing in the secondary school setting should be familiar with their state policy (ie, state legislation and state high school athletics association requirements) and should aim to become involved in influencing statewide policy through the NATA, state legislative efforts, or the sports medicine advisory committee for the state high school athletics association. However, ATs should be mindful that best practices should be adopted regardless of statewide policy requirements.
Footnotes
Abbreviations: AD, athletic director; AED, automated external defibrillator; AT, athletic trainer; CPR, cardiopulmonary resuscitation; EMS, emergency medical services.
Abbreviations: AD, athletic director; AT, athletic trainer; CI, confidence interval; EMS, emergency medical services.
Missing responses were excluded case-wise.
Components originated from the National Athletic Trainers' Association position statement on emergency planning in athletics3; group sizes varied per specific component because of variations in component-specific mandates by state (see Table 1).
Denotes significant prevalence ratio (ie, 95% CI does not include 1.00).
REFERENCES
- 1.2013–14 high school athletics participation survey. National Federation of State High School Associations Web site. 20182020 https://www.nfhs.org/media/1020200/2013-14_hs_participation_survey.pdf. Published. Accessed February 18.
- 2.Yau RK, Kucera KL, Thomas LC, Price HM, Cantu RC. Catastrophic sports injury research. Thirty-fifth annual report: fall 1982—spring 2017. National Center for Catastrophic Sports Injury Research Web site. 20182020 https://nccsir.unc.edu/files/2018/09/NCCSIR-35th-Annual-All-Sport-Report-1982_2017_FINAL.pdf Published September 27. Accessed February 18.
- 3.Andersen J, Courson RW, Kleiner DM, McLoda TA. National Athletic Trainers' Association position statement: emergency planning in athletics. J Athl Train. 2002;37(1):99–104. [PMC free article] [PubMed] [Google Scholar]
- 4.Drezner JA, Toresdahl BG, Rao AL, Huszti E, Harmon KG. Outcomes from sudden cardiac arrest in US high schools: a 2-year prospective study from the National Registry for AED Use in Sports. Br J Sports Med. 2013;47(18):1179–1183. doi: 10.1136/bjsports-2013-092786. [DOI] [PubMed] [Google Scholar]
- 5.Demartini JK, Casa DJ, Stearns R, et al. Effectiveness of cold water immersion in the treatment of exertional heat stroke at the Falmouth Road Race. Med Sci Sports Exerc. 2015;47(2):240–245. doi: 10.1249/MSS.0000000000000409. [DOI] [PubMed] [Google Scholar]
- 6.Scarneo SE, DiStefano LJ, Stearns RL, Register-Mihalik JK, Denegar CR, Casa DJ. Emergency action planning in secondary-school athletics: a comprehensive evaluation of current adoption of best practice standards. J Athl Train. 2019;54(1):99–105. doi: 10.4085/1062-6050-82-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scarneo SE, Kerr ZY, Kroshus E, et al. The socio-ecological framework: a multi-faceted approach to prevent sport-related death in high school sports. J Athl Train. 2019;54(4):356–360. doi: 10.4085/1062-6050-173-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513–531. [Google Scholar]
- 9.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 10.Emery CA. Risk factors for injury in child and adolescent sport: a systematic review of the literature. Clin J Sport Med. 2003;13(4):256–268. doi: 10.1097/00042752-200307000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Yang J, Comstock RD, Yi H, Harvey HH, Xun P. New and recurrent concussions in high-school athletes before and after traumatic brain injury laws, 2005–2016. Am J Public Health. 2017;107(12):1916–1922. doi: 10.2105/AJPH.2017.304056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kerr ZY, Marshall SW, Comstock RD, Casa DJ. Implementing exertional heat illness prevention strategies in US high school football. Med Sci Sports Exerc. 2014;46(1):124–130. doi: 10.1249/MSS.0b013e3182a11f45. [DOI] [PubMed] [Google Scholar]
- 13.Kerr ZY, Register-Mihalik JK, Pryor RR, et al. The association between mandated preseason heat acclimatization guidelines and exertional heat illness during preseason high school American football practices. Environ Health Perspect. 2019;127(4):47003. doi: 10.1289/EHP4163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kerr ZY, Register-Mihalik JK, Pryor RR, Hosokawa Y, Scarneo-Miller SE, Casa DJ. Compliance with the National Athletic Trainers' Association Inter-Association Task Force preseason heat-acclimatization guidelines in high school football. J Athl Train. 2019;54(7):749–757. doi: 10.4085/1062-6050-373-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson S, Norcross MF, Bovbjerg V, Koester M. Barriers and facilitators of implementing emergency action plans in Oregon high schools [abstract] J Athl Train. 2018;53(6 suppl) S–216. [Google Scholar]
- 16.Adams WM, Scarneo SE, Casa DJ. Assessment of evidence-based health and safety policies on sudden death and concussion management in secondary school athletics: a benchmark study. J Athl Train. 2018;53(8):756–767. doi: 10.4085/1062-6050-220-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adams WM, Scarneo SE, Casa DJ. State-level implementation of health and safety policies to prevent sudden death and catastrophic injuries within secondary school athletics. Orthop J Sports Med. 2017;5(9):2325967117727262. doi: 10.1177/2325967117727262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drezner JA, Peterson DF, Siebert DM, et al. Survival after exercise-related sudden cardiac arrest in young athletes: can we do better? Sports Health. 2019;11(1):91–98. doi: 10.1177/1941738118799084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aschieri D, Penela D, Pelizzoni V, et al. Outcomes after sudden cardiac arrest in sports centres with and without on-site external defibrillators. Heart. 2018;104(16):1344–1349. doi: 10.1136/heartjnl-2017-312441. [DOI] [PubMed] [Google Scholar]
- 20.Valenzuela TD, Roe DJ, Cretin S, Spaite DW, Larsen MP. Estimating effectiveness of cardiac arrest interventions: a logistic regression survival model. Circulation. 1997;96(10):3308–3313. doi: 10.1161/01.cir.96.10.3308. [DOI] [PubMed] [Google Scholar]
- 21.Athletic Training Locations and Services (ATLAS) Project. Korey Stringer Institute Web site. 2018 https://ksi.uconn.edu/nata-atlas/ Accessed February 15.
- 22.Casa DJ, Almquist J, Anderson SA, et al. The Inter-Association Task Force for Preventing Sudden Death in Secondary School Athletics Programs: best-practices recommendations. J Athl Train. 2013;48(4):546–553. doi: 10.4085/1062-6050-48.4.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Casa DJ, Csillan D. Inter-Association Task Force for Preseason Secondary School Athletics Participants, et al. Preseason heat-acclimatization guidelines for secondary school athletics. J Athl Train. 2009;44(3):332–333. doi: 10.4085/1062-6050-44.3.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilkerson GB, Denegar CR. A growing consensus for change in interpretation of clinical research evidence. J Athl Train. 2018;53(3):320–326. doi: 10.4085/1062-6050-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baruch Y, Holtom BC. Survey response rate levels and trends in organizational research. Hum Relat. 2008;61(8):1139–1160. [Google Scholar]


