Abstract
Context
Football is the most popular sport among US high school students and among the highest for sport-related concussion (SRC) incidence. Limited data detail how SRCs affect high school football players' psychosocial and health status beyond short-term injury recovery.
Objective
To longitudinally assess how SRCs affected symptoms, depression, and health-related quality of life (HRQoL) in high school football players up to 12 months after SRC.
Design
Prospective cohort study.
Setting
Thirty-one Wisconsin high schools.
Patients or Other Participants
A total of 1176 interscholastic football players (age = 16.0 ± 1.2 years).
Main Outcome Measure(s)
Participants completed the Post-concussion Symptom Scale (PCSS) from the Sport Concussion Assessment Tool 3 (SCAT3), Patient Health Questionnaire-9 (PHQ-9) for depression, and Pediatric Quality of Life Inventory 4.0 (PedsQL) for HRQoL at enrollment. Participants who sustained an SRC repeated each measure within 72 hours of their injury (onset) and at 7 days (D7), return to play (RTP), and 3 months (M3), 6 months (M6), and 12 months (M12) after SRC. Scores at each time point were compared with each participant's baseline using linear mixed models for repeated measures while controlling for age and previous SRC with participant as a random effect.
Results
Sixty-two participants sustained an SRC. Participants reported a higher number of PCSS symptoms, greater symptom severity, and lower PedsQL physical summary scores at onset and D7. From RTP through M12, PCSS symptoms, PCSS severity scores, PedsQL total scores, physical summary, and psychosocial summary were unchanged or improved relative to baseline. The PHQ-9 scores were not higher than baseline at any post-SRC interval.
Conclusions
High school football players in this study who sustained an SRC described no sustained adverse health outcomes (increased PCSS symptoms or symptom severity, increased depression symptoms, or lower HRQoL) after their RTP through M12 after injury.
Keywords: traumatic brain injuries, longitudinal studies, psychosocial outcomes
Key Points
High school football players who sustained a sport-related concussion displayed increased disablement (increased symptoms and symptom severity, increased depression scores, and lower health-related quality of life) immediately after injury.
This disablement resolved by the date the players were allowed to return to play by their athletic trainer.
No increased disablement was found in these players for the 12 months after concussion.
High school football is the most popular sport in US high schools, with 1.1 million participants.1 Compared with other sports, football ranks among the highest in the incidence of sport-related concussions (SRCs) and accounts for more than 40% of all SRCs sustained by US high school sport participants.2 The incidence of SRC injuries is a significant area of interest and study in the United States and around the world. Further, a great deal of concern has been raised regarding the onset, treatment, and short-term and long-term outcomes of SRCs in youth and adolescent athletes.3,4
Over the past decade, the scientific literature has brought increased attention to the risks football players face for sustaining an SRC and the possible development of depression and neurocognitive changes later in life.5–7 This increased focus has been amplified by reports in the lay press that cited examples of significant disablement among football players who sustained SRCs.8
Beyond the initial restriction from sport, many stakeholders have ongoing concerns regarding short-term and long-term disablement associated with SRCs. Concussion symptoms typically resolve within 7 to 10 days after injury,9 but a significant percentage of adults who presented to a specialty concussion clinic had symptoms beyond 30 days.10 In addition, SRCs have also been associated with an increase in subsequent symptoms of depression11–13 and deficits in health-related quality of life (HRQoL).14,15
Many of the studies that demonstrated disablement associated with SRCs enrolled participants from specialized medical settings or those who experienced severe or prolonged symptoms.16–20 As such, it can be challenging to apply these findings to the general high school football population. Moreover, disablement data associated with SRCs in athlete populations have been collected prospectively from injury onset through a short recovery period or in large cross-sectional or retrospective research designs.21–24 As a result, the trajectory of the possible manifestation and resolution of any disablement associated with SRCs in high school football players has not been well described.
To offset the limitations of previous investigations, we prospectively assessed the effects of SRCs on self-reported SRC symptoms, symptom severity, depression, and HRQoL in a sample of Wisconsin high school football players. To accomplish this, we recruited participants and collected data from a diverse sample of high schools, relying on practicing athletic trainers (ATs) to report the onset, resolution, and long-term effects of these injuries. This study is unique in that understanding how SRCs affected a typical sample of high school football players beyond their initial recovery will provide timely information. These data can ultimately help inform conversations among sports medicine providers, athletes, and athletes' parents regarding what to expect after an SRC sustained while participating in high school football.
METHODS
We prospectively collected data on participants from 31 Wisconsin high schools during the 2016–2017 and 2017–2018 school years. To be included as a data-collection site, each school had to employ an AT at the school on a full-time or part-time basis who would assist with data collection. Potential participants were identified and made aware of the study before the start of each football season at preseason team meetings. To be eligible to participate, players needed to be members of an interscholastic (grades 9–12) football team and have no disabling injuries (concussion or musculoskeletal) precluding them from full activity during the upcoming season. Participants and their parents (if the athlete was under age 18) were required to sign the informed consent (and assent form if appropriate) before enrollment. The study was approved by the University of Wisconsin Health Sciences Institutional Review Board.
Measures
During preseason team meetings, participants completed a baseline form to collect demographic information and their history of SRC. Self-reported concussion symptoms were recorded using the Post-concussion Symptom Scale (PCSS) from the Sport Concussion Assessment Tool 3 (SCAT3). On the PCSS, the respondent reports his or her number of symptoms (yes or no to 22 symptoms commonly associated with SRC, score range = 0–22) and symptom severity on a 6-point Likert scale (score range = 0–132). The PCSS is valid and reliable in high school athletes.25
Depression was measured using the Patient Health Questionnaire-9 (PHQ-9). On this 9-item screening questionnaire, the participant rates the frequency of depression symptoms experienced in the previous 2 weeks. Scores range from 0 to 27, with a higher score indicating a greater level of depression. A change in PHQ-9 scores ≥5 points is considered clinically significant. The PHQ-9 has demonstrated high sensitivity and specificity for depression screening in patients aged 13 to 17 years.26
The HRQoL was measured using the Pediatric Quality of Life 4.0 Acute (PedsQL). The 23-item PedsQL questionnaire is used to assess HRQoL for the previous 7 days. Individual domain scores can be tabulated in addition to physical and subscale summaries. A high HRQoL score indicates greater HRQoL. The PedsQL has been validated for use in children aged 2 to 17 years27 and is used by researchers to measure the impact of SRCs on HRQoL in adolescents.23,24
The ATs working at each school recorded the onset and characteristics of each SRC, which was defined as a “trauma-induced alteration in mental status that may or may not involve loss of consciousness.”28 The ATs also recorded the post-SRC management required for each concussed participant, including the total days with SRC symptoms, participation in a return-to-play (RTP) protocol, and total days out of sport. Per Wisconsin law, each high school athlete suspected of having sustained an SRC was evaluated and cleared by a licensed medical provider (physician or AT) before returning to interscholastic sport competition.29 Injured participants completed the same baseline instruments (PCSS, PHQ-9, and PedsQL) within 24 to 72 hours (onset) and at 7 days (D7), RTP, and 3 months (M3), 6 months (M6), and 12 months (M12) after SRC. Participants were asked to complete the surveys electronically at home if they were unable to do so at their school.
Statistics
Participant demographics by concussion status were summarized by n (%), mean ± SD, or median (interquartile ratio [IQR]), and statistical comparisons between groups for participant demographics were performed using χ2, Student t, or Wilcoxon rank sum tests based on the variable's statistical distribution. Using linear mixed models for repeated measures with participant as a random effect and controlling for age and previous SRC, we estimated the average (95% confidence interval [CI]) paired difference in total score at each time point compared with the participant's own baseline score and tested it against the null hypothesis of no change from baseline. The P values in each linear mixed model were Holm adjusted for 6 tests. Significance level was set to P = .05. All analyses were conducted using R (version 3.3.1; R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Wisconsin high school football players (n = 998, boys = 99.7%, age = 16.0 ± 1.2 years) participated in 1176 player-seasons over the 2-year study period. Of the participants, 243 (20.7%) reported sustaining a previous SRC. The median number of previous SRCs = 0 (IQR 25th–75th = 0–0). During the study, 62 (5.3%) unique participants sustained an SRC. The baseline characteristics of the injured (n = 62) and uninjured (n = 1114) participants are found in Table 1.
Table 1.
Baseline Demographics for Injured and Uninjured Study Participantsa
| Variable |
Group |
Test Statistic |
P Value |
|
| Injured (n = 62) |
Uninjured (n = 1114) |
|||
| Age, yb | 16.2 ± 1.3 | 16.0 ± 1.2 | t67 = 1.44 | .155 |
| Gradec | χ23 = 2.39 | .465 | ||
| 9 | 19 (30.6) | 311 (27.9) | ||
| 10 | 11 (17.7) | 296 (26.6) | ||
| 11 | 17 (27.4) | 270 (24.2) | ||
| 12 | 15 (24.2) | 237 (21.3) | ||
| Previous sport-related concussion?c | χ21 = 3.43 | .064 | ||
| No | 43 (69.4) | 891 (80) | ||
| Yes | 19 (30.6) | 223 (20.0) | ||
| Previous sport-related concussions, No.c | ||||
| 0 | 43 (69.3) | 891 (79.9) | ||
| 1 | 16 (25.8) | 184 (16.5) | ||
| 2 | 2 (3.2) | 36 (3.2) | ||
| 3 | 1 (1.6) | 2 (0.8) | ||
| Sport Concussion Assessment Tool 3 (SCAT3) scored | ||||
| Total | 0.0 (0.0–1.8) | 0.0 (0.0–1.0) | W = 29 732 | .028 |
| Symptom severity | 0.0 (0.0–2.0) | 0.0 (0.0–1.0) | W = 29 686 | .026 |
| Patient Health Questionnaire-9 total scored | 1.0 (0.0–2.0) | 0.0 (0.0–2.0) | W = 30 652 | .099 |
| Pediatric Quality of Life Inventory 4.0 scored | ||||
| Physical subscale summary | 96.9 (90.6–100.0) | 100 (93.8–100) | W = 39 322 | .041 |
| Psychosocial subscale summary | 93.3 (85.0–100.0) | 96.7 (88.3–100) | W = 39 674 | .044 |
| Total | 95.1 (84.8–99.7) | 96.7 (90.2–100) | W = 39 845 | .038 |
Abbreviation: W, Wilcoxon rank sum test value.
Statistical comparisons between groups in the participant demographics used Student t, χ2, or Wilcoxon rank sums test based on the variable distribution.
Data reported as mean ± SD.
Data reported as n (%).
Data reported as median (interquartile ratio, 25th–75th).
Onset of and Recovery From SRC
The SRC onset, management, and resolution characteristics are found in Table 2. The majority (n = 38, 61%) of the SRCs were sustained during competition, and the same proportion were caused by collision with an opponent. The most common types of contact were head to head (n = 25, 40.3%) and head to another body part (n = 26, 41.9%). An AT was onsite for 55 (89%) injury events, and 46 (74%) of the players were immediately removed from play. The first post-SRC assessment by the AT took place at a median time of 0.1 (IQR 25th–75th = 0.0–24.0) hours after the injury, and participants scores indicated a mean increase of 6.3 from baseline in their PCSS symptoms (95% CI = 5.2, 7.5) and a mean increase of 15.5 in their PCSS severity score (95% CI = 12.0, 19.0).
Table 2.
Sport-Related Concussion (SRC) Onset, Management, and Resolution Characteristics
| Variable |
Total (n = 62) |
| Level of playa | |
| Freshman | 17 (27.4) |
| Junior varsity | 13 (20.9) |
| Varsity | 32 (51.6) |
| Type of exposurea | |
| Practice | 24 (39.8) |
| Competition | 38 (61.2) |
| Injury mechanisma | |
| Collision with opponent | 38 (61.2) |
| Collision with teammate | 16 (25.8) |
| Contact with playing surface | 6 (9.6) |
| Other | 2 (3.2) |
| Type of contacta | |
| Head to other body part | 26 (41.9) |
| Head to head | 25 (40.3) |
| Contact with playing surface | 9 (14.5) |
| Other | 2 (3.2) |
| Player immediately removed from play?a | |
| No | 16 (25.9) |
| Yes | 46 (74.1) |
| Hours until evaluated by the school athletic trainerc | 0.1 (0.0–24.0) |
| Change in Post-concussion Symptom Scale from baselineb | |
| Total symptom score | 6.3 (5.2, 7.5) |
| Total severity score | 15.5 (12.0, 19.0) |
| Total post-SRC assessments by the athletic trainerc | 5.0 (3.0–6.0) |
| Referred to physician?a | |
| No | 22 (35.5) |
| Yes | 40 (64.5) |
| Days with SRC symptomsc | 5.0 (4.0–8.5) |
| Days in return-to-play protocolc | 5.0 (4.0–7.0) |
| Days out from sportc | 14.0 (11.0–18.8) |
Data reported as n (%).
Data reported as mean (95% confidence interval).
Data reported as median (interquartile ratio 25th–75th).
A total of 22 (35.5%) SRCs were managed solely by the AT, while the remaining athletes (40 [64.5%]) were referred to their physician for additional evaluation. Participants underwent a median of 5.0 (IQR 25th–75th = 3.0–6.0) post-SRC assessments. Their symptoms lasted a median of 5.0 (IQR 25th–75th = 4.0–8.5) days; 42 participants (69.3%) reported symptom resolution within 1 week and only 3 participants (4.8%) reported symptom resolution after 28 days. A total of 55 (90%) athletes pursued an RTP protocol under the supervision of their AT. The median number of sport days missed was 14.0 (IQR 25th–75th = 11.0–18.8).
Comparison With Baseline Scores
The post-SRC completion rates for participants were 98% at onset, 98% at D7, 98% at RTP, 84% at M3, 83% at M6, and 71% at M12. Compared with baseline scores, the PCSS symptom scores increased at injury onset (mean = 6.3; 95% CI = 5.2, 7.5; P < .001) and D7 (mean = 1.8; 95% CI = 0.6, 2.9; P = .002). The PCSS symptom score decreased at RTP (mean = –1.2; 95% CI = –2.3, –0.1; P = .030), whereas no differences were noted at M3, M6, and M12. Similarly, the PCSS symptom severity score increased at injury onset (mean = 15.5; 95% CI = 12.0, 19.0; P < .001) and D7 (mean = 4.3; 95% CI = 0.9, 7.8; P = .015), but no change was detected at RTP, M3, M6, and M12. Figure 1 illustrates the changes after SRC from baseline for PCSS symptom and symptom severity scores through M12.
Figure 1.
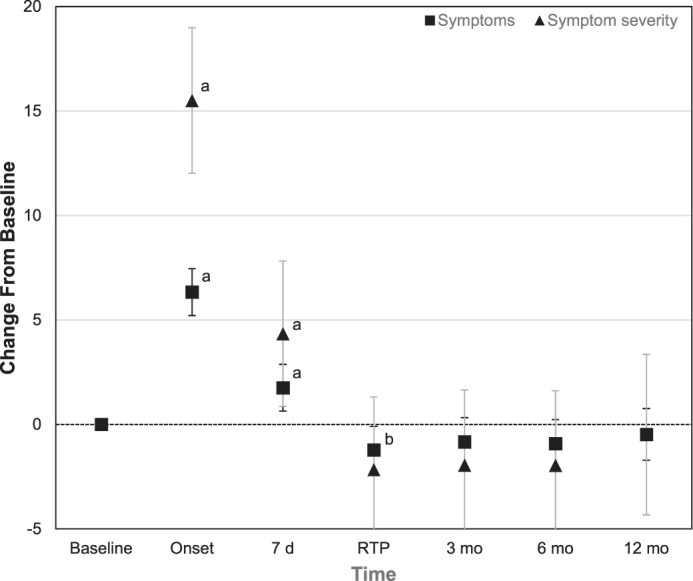
Change in symptoms and symptom severity from baseline through 12 months after sport-related concussion. a Indicates scores significantly worse than baseline. b Indicates scores significantly better than baseline.
Compared with baseline, no differences were evident in the PHQ-9 scores at injury onset, D7, and M12. The mean PHQ-9 scores were decreased at RTP (mean = –1.6; 95% CI = −2.5, –0.7; P = .001), M3 (mean = –1.2; 95% CI = –2.1, –0.2; P = .013), and M6 (mean = –1.4; 95% CI = –2.3, –0.5; P = .003). Figure 2 illustrates the changes after SRC from baseline for PHQ-9 scores through M12.
Figure 2.
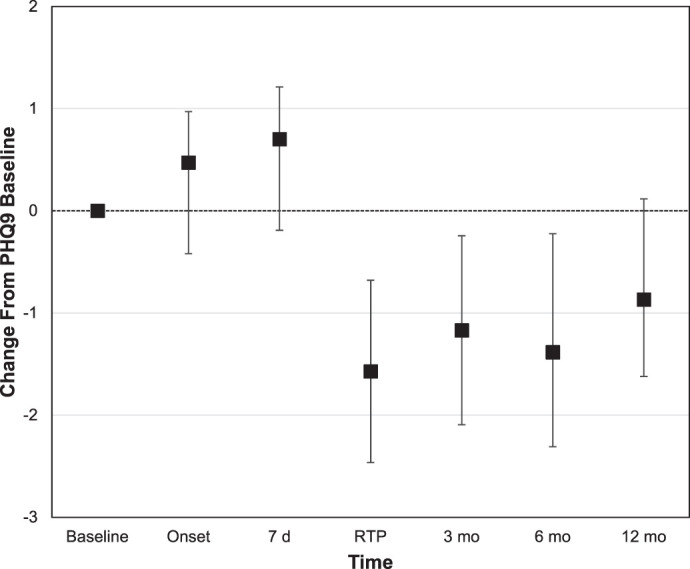
Change in Patient Health Questionnaire-9 (depression) scores from baseline through 12 months after sport-related concussion.
Versus baseline, the PedsQL physical summary scores were decreased at injury onset (mean = –6.7; 95% CI = –10.4, –2.9; P = .001) and D7 (mean = –7.2; 95% CI = –11.0, –3.4; P < .001) and increased at RTP (mean = 4.5; 95% CI = 0.7, 8.2; P = .020), M3 (mean = 4.6; 95% CI = 0.7, 8.5; P = .021), and M6 (mean = 4.6; 95% CI = 0.8, 8.5; P = .019), whereas no change was present at M12. The PedsQL psychosocial summary scores were no different from baseline at onset or D7. Mean PedsQL psychosocial summary scores were increased at RTP (mean = 8.0; IQR 25th–75th = 5.2–10.9; P < .001), M3 (mean = 6.5; 95% CI = 3.5, 9.5; P < .001), M6 (mean = 7.2; 95% CI = 4.3, 10.2; P < .001), and M12 (mean = 5.5; 95% CI = 2.4, 8.7; P = .001). The PedsQL total scores were unchanged from baseline at onset and D7 but increased at RTP (mean = 6.8; IQR 25th–75th = 3.9–9.7; P < .001), M3 (mean = 5.9; 95% CI = 2.8, 8.9; P < .001), M6 (mean = 6.3; 95% CI = 3.3, 9.3; P < .001), and M12 (mean = 4.9; 95% CI = 1.7, 8.1; P = .003). Figure 3 illustrates the changes from baseline through M12 for the PedsQL physical summary, PedsQL psychosocial summary, and PedsQL total scores. The total scores and score changes from baseline for symptom, depression, and PedsQL scores from baseline through M12 post-SRC are shown in the Supplemental Table.
Figure 3.
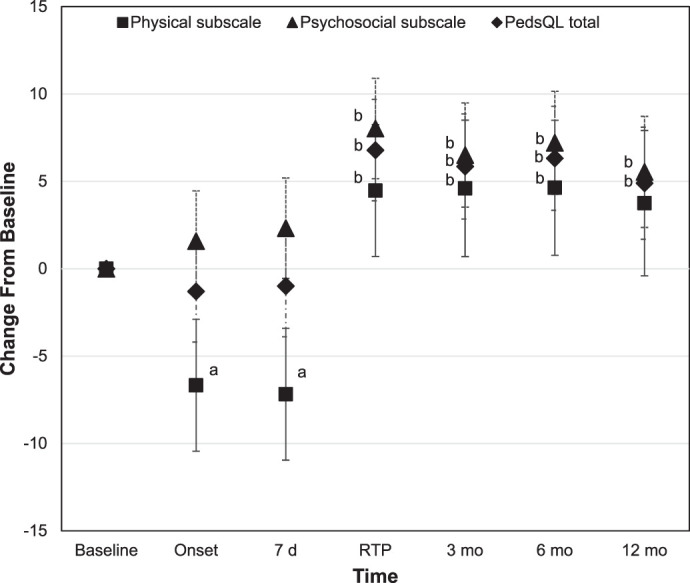
Change in Pediatric Quality of Life Inventory 4.0 (health-related quality-of-life) scores from baseline through 12 months after sport-related concussion. a Indicates scores significantly worse than baseline. b Indicates scores significantly better than baseline.
DISCUSSION
Our main finding suggests that this sample of high school football players who sustained an SRC did not report disablement as quantified by increased concussion symptoms or symptom severity, increased depression symptoms, or decreased HRQoL once they returned to unrestricted sport participation. This result is counter to the literature,3–5 which indicated that SRCs may be associated with disablement for significant periods of time.
Symptom Reporting
Our results demonstrating no increase in self-reported symptoms from RTP and beyond contrast with previous indications that symptoms in high school athletes can persist for an extensive period after SRC. Iverson et al20 noted higher symptom scores in participants with a history of multiple SRCs as well as preexisting psychosocial conditions (depression, attention-deficit/hyperactivity disorder, migraines, or learning disabilities). Using a similar cross-sectional design, Snedden et al21 described a larger number of symptoms and higher symptom severity scores in healthy participants with a previous SRC. It should be noted that we did not try to capture other preexisting conditions associated with increased symptom reporting beyond a history of SRC and baseline PCSS scores. However, the difference in our findings may reflect the fact that retrospective cross-sectional data are more likely to be affected by recall bias than our prospective methods.
Prolonged postconcussion symptoms (>28 days) have also been documented in patients being treated in clinical settings. From a systematic review of patients aged 2 to 18 years, Zemek et al17 observed that a loss of consciousness was associated with persistent concussion symptoms. In contrast, none of our participants experienced loss of consciousness.
Increased symptom reporting was also discussed by Corbin-Berrigan and Gagnon,18 who found that higher symptom scores at 10 days were associated with prolonged symptoms (>28 days). However, only 17 (27%) of our participants had symptom scores that were higher than baseline at 7 days after SRC and 1 day (n = 1 [1.6%]) after returning to unrestricted play.
Fehr et al19 noted that in a clinic population, the median time to symptom resolution was 40 days, with loss of consciousness being associated with prolonged symptoms. The primary difference in our results is most likely attributable to the fact that both of these groups18,19 enrolled patients who sustained moderate or severe brain injuries and subsequently sought treatment in a concussion specialty clinic, which is quite different from our participants, who were enrolled and, in many cases, managed in a high school setting.
Sport-Related Concussion and Depression
We did not detect increased depression scores at any post-SRC interval. This contrasts with previous research from Chrisman et al,11 who demonstrated a 3-fold increased risk for depression among adolescents with a history of concussion.11 However, the authors used a cross-sectional study design, which is inherently subject to recall bias. Yang et al12 and Vargas et al13 demonstrated that nearly 20% of collegiate athletes recovering from an SRC reported increased symptoms of depression. Yet both studies were short term, and data were collected only until RTP.
Health-Related Quality of Life
Short-term and some long-term deficits in HRQoL have consistently been recognized after SRC.14 Participants in our study had decreased HRQoL at injury onset and at D7 before their scores returned to baseline. This result was similar to that in a prospective study by Houston et al,22 who saw that by 10 days after SRC, athletes' PedsQL scores improved from baseline. This finding is also similar to that in a prospective study by Valovich McLeod et al23: participants with a prolonged recovery (>13 days) described lower HRQoL compared with those who had short-duration or moderate-duration recoveries.24 However, all participants in their study displayed improvements by day 30, indicating that SRC had limited lasting effects on HRQoL.
Conversely, Fineblit et al14 stated that a select group of patients who sustained concussions experienced poor HRQoL outcomes for up to 1 year after injury. Predictors of poor HRQoL included older age, lower socioeconomic status, and a history of headaches. Although our participants were similar in age, we did not record their socioeconomic status or history of sleep disturbance or headaches. As a result, we cannot rule out the possibility that these factors were present in our participants.
Long-Term Disablement Associated With High School Football
Evidence is conflicting regarding the association of participation in football and the development of long-term disablement. Kerr et al5 reported lower HRQoL in former collegiate players who sustained multiple SRCs. In addition, neurocognitive deficits have been shown in selective samples of former NFL players.6,7 However, extrapolating the findings from these studies to high school football athletes is problematic because only a small fraction go on to play at the collegiate or professional level.
In contrast, Janssen et al29 found no increased disablement in a cohort of former high school football players compared with other high school athletes. In a large study of 3900 participants, Deshpande et al30 similarly detected no increase in later-life cognitive impairments among former high school football players versus participants who did not play football. We did not follow our participants beyond 12 months post-SRC, though we recognize that SRCs may be associated with impairments that appear in the players' later years. Future authors should prospectively enroll a cohort of high school players and longitudinally assess possible disablement in the decades after their football participation ends.
Limitations
This study had several limitations. First, these data were collected in a single state, with specific regulations regarding the recognition and management of SRCs in high school athletes. These regulations encourage each school to have an AT available at the school, emphasize consistent post-SRC management, and require medical clearance before the athlete is allowed to return to sport. In addition, recent researchers31 determined that the presence of an AT affected the reported incidence and management practices for players with SRCs. As such, the outcomes experienced by our participants may not be similar to those of players in states without AT access or management.
Second, the SRCs in our study could be characterized as milder than injuries in previous studies, particularly those captured in specialized clinics. Although we acknowledge this fact, we also note that our purpose was to document the disablement associated with SRCs in a typical high school football population rather than a clinic population.
Third, we did not completely screen each participant for preexisting conditions that might have affected the recovery from an SRC. We realize that this would have been optimal, but the extensive resources required to collect these data were not available to us. Instead, we relied on symptom reporting, which is a proxy measure for prolonged health effects after SRC.
Finally, the response rates at each post-SRC interval were less than 100%. It is important to note that a number of our participants were in the 12th grade, which made data collection challenging. To counter this, our study team repeatedly used email, phone, and mail solicitations to contact athletes who had finished their sport involvement to encourage them to complete the post-SRC surveys.
CONCLUSIONS
High school football players who sustained SRCs reported increased symptoms and symptom severity and lower HRQoL immediately after their injuries. However, by RTP and through the 12 months after their SRC, we did not detect an increase in concussion-related symptoms or symptom severity, increased depression scores, or decreased HRQoL scores. These results can better inform conversations among sports medicine providers, football players, and parents regarding the effects of SRCs in the first year after injury.
Supplementary Material
ACKNOWLEDGMENTS
We thank Allie Wiedman for her assistance in collecting data for this study. We also thank all of the participating high school coaches, athletic trainers, interscholastic athletes, and athletes' parents for their willingness to take part in this study. This study was funded by the National Athletic Trainers' Association Research and Education Foundation (Award No. 15OUT003) and the Department of Orthopedics and Rehabilitation at the University of Wisconsin School of Medicine and Public Health.
REFERENCES
- 1.High School Particiaption Statistics. National Federation of State High School Associations Web site. 2019 http://www.nfhs.org/ParticipationStatistics/PDF/2017-1820High School Athletics Participation Survey.pdf Accessed January 11.
- 2.Summary report: National High School Injury Surveillance Study. Reporting Injuries Online Web site. 2019 http://www.ucdenver.edu/academics/colleges/PublicHealth/research/ResearchProjects/piper/projects/RIO/Documents/2017-18.pdf Accessed January 11.
- 3.Broglio SP, Cantu R, Gioia GA, et al. National Athletic Trainers' Association position statement: management of sport concussion. J Athl Train. 2014;49(2):245–265. doi: 10.4085/1062-6050-49.1.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCrory P, Meeuwisse W, Dvorak J, et al. Consensus statement on concussion in sport: the 5th International Conference on Concussion in Sport held in Berlin, October 2016. Br J Sports Med. 201751(11):838–847. doi: 10.1136/bjsports-2017-097699. [DOI] [PubMed] [Google Scholar]
- 5.Kerr ZY, Thomas LC, Simon JE, McCrea M, Guskiewicz KM. Association between history of multiple concussions and health outcomes among former college football players: 15-year follow-up from the NCAA Concussion Study (1999–2001) Am J Sports Med. 2018;46(7):1733–1741. doi: 10.1177/0363546518765121. [DOI] [PubMed] [Google Scholar]
- 6.Vos BC, Nieuwenhuijsen K, Sluiter JK. Consequences of traumatic brain injury in professional American football players: a systematic review of the literature. Clin J Sport Med. 2018;28(2):91–99. doi: 10.1097/JSM.0000000000000432. [DOI] [PubMed] [Google Scholar]
- 7.Baugh CM, Kroshus E, Kiernan PT, Mendel D, Meehan WP., III Football players' perceptions of future risk of concussion and concussion-related health outcomes. J Neurotrauma. 2017;34(4):790–797. doi: 10.1089/neu.2016.4585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feudtner C, Miles SH. Traumatic brain injury news reports and participation in high school tackle football. JAMA Pediatr. 2018;172(5):492–494. doi: 10.1001/jamapediatrics.2017.5242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCrea M, Guskiewicz KM, Marshall SW, et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290(19):2556–2563. doi: 10.1001/jama.290.19.2556. [DOI] [PubMed] [Google Scholar]
- 10.Meehan WP, III, O'Brien MJ, Geminiani E, Mannix R. Initial symptom burden predicts duration of symptoms after concussion. J Sci Med Sport. 2016;19(9):722–725. doi: 10.1016/j.jsams.2015.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chrisman SPD, Richardson LP. Prevalence of diagnosed depression in adolescents with history of concussion. J Adolesc Health. 2014;54(5):582–586. doi: 10.1016/j.jadohealth.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang J, Peek-Asa C, Covassin T, Torner JC. Post-concussion symptoms of depression and anxiety in Division I collegiate athletes. Dev Neuropsychol. 2015;40(1):18–23. doi: 10.1080/87565641.2014.973499. [DOI] [PubMed] [Google Scholar]
- 13.Vargas G, Rabinowitz A, Meyer J, Arnett PA. Predictors and prevalence of postconcussion depression symptoms in collegiate athletes. J Athl Train. 2015;50(3):250–255. doi: 10.4085/1062-6050-50.3.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fineblit S, Selci E, Loewen H, Ellis M, Russell K. Health-related quality of life after pediatric mild traumatic brain injury/concussion: a systematic review. J Neurotrauma. 2016;33(17):1561–1568. doi: 10.1089/neu.2015.4292. [DOI] [PubMed] [Google Scholar]
- 15.Manley G, Gardner AJ, Schneider KJ, et al. A systematic review of potential long-term effects of sport-related concussion. Br J Sports Med. 2017;51(12):969–977. doi: 10.1136/bjsports-2017-097791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Howell DR, Zemek R, Brilliant AN, Mannix RC, Master CL, Meehan WP., III Identifying persistent post concussion symptom risk in a pediatric sports medicine clinic. Am J Sports Med. 2018;46(13):3254–3261. doi: 10.1177/0363546518796830. [DOI] [PubMed] [Google Scholar]
- 17.Zemek RL, Farion KJ, Sampson M, McGahern C. Prognosticators of persistent symptoms following pediatric concussion: a systematic review. JAMA Pediatr. 2013;167(3):259–265. doi: 10.1001/2013.jamapediatrics.216. [DOI] [PubMed] [Google Scholar]
- 18.Corbin-Berrigan LA, Gagnon I. Postconcussion symptoms as a marker of delayed recovery in children and youth who recently sustained a concussion: a brief report. Clin J Sport Med. 2017;27(3):325–327. doi: 10.1097/JSM.0000000000000355. [DOI] [PubMed] [Google Scholar]
- 19.Fehr SD, Nelson LD, Scharer KR, et al. Risk factors for prolonged symptoms of mild traumatic brain injury: a pediatric sports concussion clinic cohort. Clin J Sport Med. 2019;29(1):11–17. doi: 10.1097/JSM.0000000000000494. [DOI] [PubMed] [Google Scholar]
- 20.Iverson GL, Silverberg ND, Mannix S, et al. Factors associated with concussion like symptom reporting in high school athletes. JAMA Pediatr. 2015;169(12):1132–1140. doi: 10.1001/jamapediatrics.2015.2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Snedden TR, Brooks MA, Hetzel S, McGuine T. Normative values of the Sport Concussion Assessment Tool 3 (SCAT3) in high school athletes. Clin J Sport Med. 2017;27(5):462–467. doi: 10.1097/JSM.0000000000000389. [DOI] [PubMed] [Google Scholar]
- 22.Houston MN, Bay RC, Valovich McLeod TC. The relationship between post-injury measures of cognition, balance, symptom reports and health-related quality-of-life in adolescent athletes with concussion. Brain Inj. 2016;30(7):891–898. doi: 10.3109/02699052.2016.1146960. [DOI] [PubMed] [Google Scholar]
- 23.Valovich McLeod TA, Bay C, Lam KC, Snyder-Valier AR. The association between length of recovery following sport-related concussion and generic and specific health-related quality of life in adolescent athletes: a prospective, longitudinal study. J Head Trauma Rehabil. 2018;34(1):E1–E9. doi: 10.1097/HTR.0000000000000394. [DOI] [PubMed] [Google Scholar]
- 24.Chin EY, Nelson LD, Barr WB, McCrory P, McCrea MA. Reliability and validity of the Sport Concussion Assessment Tool–3 (SCAT3) in high school and collegiate athletes. Am J Sports Med. 2016;44(9):2276–2285. doi: 10.1177/0363546516648141. [DOI] [PubMed] [Google Scholar]
- 25.Richardson LP, McCauley E, Grossman DC, et al. Evaluation of the Patient Health Questionnaire-9 Item for detecting major depression among adolescents. Pediatrics. 2010;126(6):1117–1123. doi: 10.1542/peds.2010-0852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Varni JW, Seid M, Kurtin PS. PedsQLTM 4.0: reliability and validity of the Pediatric Quality of Life InventoryTM version 4.0. Generic core scales in healthy and patient populations. Med Care. 2001;39(8):800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Practice parameter: the management of concussion in sports (summary statement) Neurology. 1997;48(3):581–585. doi: 10.1212/wnl.48.3.581. Report of the Quality Standards Subcommittee. [DOI] [PubMed] [Google Scholar]
- 28.Wisconsin Act 172. Wisconsin State Concussion Law. Wisconsin State Legislature. 2011.
- 29.Janssen PH, Mandrekar J, Mielke MM, et al. High school football and late-life risk of neurodegenerative syndromes, 1956-1970. Mayo Clin Proc. 2017;92(1):66–71. doi: 10.1016/j.mayocp.2016.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Deshpande SK, Hasegawa RB, Rabinowitz AR, et al. Association of playing high school football with cognition and mental health later in life. JAMA Neurol. 2017;74(8):909–918. doi: 10.1001/jamaneurol.2017.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McGuine TA, Post EG, Pfaller A, Hetzel SJ, Brooks MA, Broglio SP. The influence of athletic trainers on the incidence and management of concussions in high school athletes. J Athl Train. 2018;53(11):1017–1024. doi: 10.4085/1062-6050-209-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


