In 1999, psychologists David Dunning, PhD, and Justin Kruger, PhD, wrote a seminal article titled “Unskilled and Unaware of It: How Difficulties in Recognizing One's Own Incompetence Lead to Inflated Self-Assessments.”1 They described 4 experiments in which they asked college students to estimate their performance on tests involving humor, grammar, and logic. They were struck by the finding that students who performed poorly often grossly overestimated their performance. They also noticed that students who objectively performed well often subjectively underestimated their performance. This phenomenon is commonly known as the Dunning–Kruger Curve or the Dunning–Kruger Effect. It attempts to explain why people experience a blind spot when gauging their competence. Dunning and Kruger suggested that
People hold overly favorable views of their abilities in many social and intellectual domains . . . this overestimation occurs, in part, because people who are unskilled in these domains suffer a dual burden: Not only do these people reach erroneous conclusions and make unfortunate choices, but their incompetence robs them of the metacognitive ability to realize it.1
Further studies found that inaccurate self-assessments are explained both by lack of insight into their own performance in low-performing individuals and by lack of accurate perception of their peers' performances in high-performing individuals.1–3
A graphic depiction of the Dunning–Kruger Effect is shown in the Figure. At point A, inexperienced people often have a falsely elevated sense of confidence about their performance. With time and experience, they realize that they had been unaware of some intricate aspects of the job. This realization plunges their confidence (point B). As they continue to spend more time on the job, they acquire more experience and wisdom, ultimately gaining their earned confidence (point C). However, the confidence is never as high as it was at in the beginning. Paradoxically, by the time low-performing individuals achieve accuracy in their self-assessments, their performance has improved. In a nutshell, competence is required to identify areas of incompetency.
Figure.
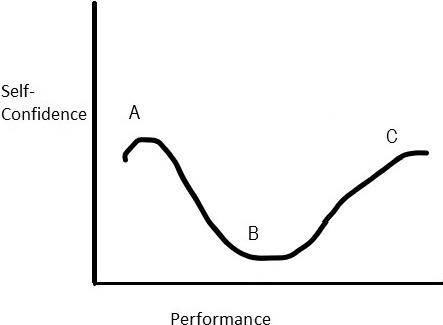
Graphic Depiction of the Dunning–Kruger Effect
Applicability to Residency Training
Understanding the Dunning–Kruger Effect is important for leaders and trainees in graduate medical education because voluntary self-improvement requires recognizing the gaps in one's knowledge and skills as well as knowing how one is perceived by others. Although the Accreditation Council for Graduate Medical Education recommends that residents complete self-assessments periodically,4 studies have demonstrated that self-assessments by medical students, interns, and residents in general surgery, family medicine, and psychiatry are invalid measures of their objective performance.5–9
Several medical studies support different portions of the Dunning–Kruger Curve. For example, 1 study found that junior physicians who were less competent tended to self-rate their efficacy higher than it was demonstrated (point A).10 Comparison of self-assessments and peer assessments of physicians in internal medicine, pediatrics, and psychiatry showed that those assessed in the lowest quartile by their colleagues tended to rate themselves 30 to 40 percentile ranks higher than their peers.11 A study showed that the lowest-performing physicians are the least likely to accept objective feedback on their performance.12 In another study, physicians did not perceive negative feedback as accurate or helpful and did not plan to use it to change their practice.13 Some physicians, after a period of reflection, were able to accept the negative feedback and use it for change. Others not only refused to accept the feedback but also questioned its validity and procedures.13
Researchers have also found that more competent junior physicians tended to self-rate their efficacy lower than less competent ones (point B).10 This was especially true of women.14 It has also been shown that the more the time spent in learning and practicing a skill, the higher one's self-confidence about those skills (point C), regardless of objective improvement. For example, residents' competence across milestones increases with years of training.15 Improvement in competence and self-confidence with time has also been demonstrated in medical students and academic physician faculty.9,16–18
The utility of recognizing the Dunning–Kruger Effect is helping junior physicians navigate their professional development, clinical expertise, and sense of self-confidence. It encourages physicians to be introspective, recognize their weaknesses, and beware of the limitations of self-confidence as a measure of clinical competency.
Practical Suggestions
The author suggests the following practical applications regarding the Dunning–Kruger Effect.
Program directors should be aware that trainees' projected self-confidence and perception of their own performance may not reflect their actual performance, both in trainees who under- and overvalue their performance.19–21
Rather than self-assessments, program directors should consider giving more credence to assessments completed by a variety of faculty, peers, patients, and staff. These assessments taken together may be more accurate than resident self-assessments alone.
When mentoring underperforming residents who appear overconfident, delivering facts and feedback from multiple sources is necessary, but often not sufficient to lead to improvement in performance. Setting clear expectations for measures of competence and potential consequences if those standards are not met may be required.
When mentoring adequately performing residents who remain insecure about their competence, program directors should remember that allowing for self-doubt is a critical step in the phase marked by improved performance. Superficial reassurance will not drive a resident to improve—a resident must tolerate periods of doubt and low self-confidence in order to improve performance and rebuild a positive self-image. Program directors can remind residents of the learning process and encourage hope for improvement with time and perseverance, which should be the ultimate goal of any residency training program.
Footnotes
The author would like to thank Dr. Jaison Nainaparampil for introducing her to the Dunning–Kruger Effect.
References
- 1.Kruger J, Dunning D. Unskilled and unaware of it: how difficulties in recognizing one's own incompetence lead to inflated self-assessments. J Pers Soc Psychol. 1999;77(6):1121–1134. doi: 10.1037/0022-3514.77.6.1121. [DOI] [PubMed] [Google Scholar]
- 2.Ehrlinger J, Johnson K, Banner M, Dunning D, Kruger J. Why the unskilled are unaware: further explorations of (absent) self-insight among the incompetent. Organ Behav Hum Decis Process. 2008;105(1):98–121. doi: 10.1016/j.obhdp.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Raat AN, Kuks JBM, van Hell EA, Cohen-Schotanus J. Peer influence on students' estimates of performance: social comparison in clinical rotations. Med Educ. 2013;47(2):190–197. doi: 10.1111/medu.12066. [DOI] [PubMed] [Google Scholar]
- 4.Accreditation Council for Graduate Medical Education. ACGME Milestones Guidebook for Residents and Fellows. 2020 https://acgme.org/LinkClick.aspx?link=PDFs%2fMilestones%2fMilestonesGuidebookforResidentsFellows.pdf&articleId=6039 Accessed August 24.
- 5.Spada M, Lundblad W, Glance J, Rosenstock J, Gopalan P, Azzam PN, et al. Self-assessment of teaching skills among psychiatric residents. Acad Psychiatry. 2018;42(4):477–481. doi: 10.1007/s40596-017-0877-z. [DOI] [PubMed] [Google Scholar]
- 6.Eva KW, Cunnington JP, Reiter HI, Keane DR, Norman GR. How can I know what I don't know? Poor self assessment in a well-defined domain. Adv Health Sci Educ Theory Pract. 2004;9(3):211–224. doi: 10.1023/B:AHSE.0000038209.65714.d4. [DOI] [PubMed] [Google Scholar]
- 7.Barnsley L, Lyon PM, Ralston SJ, Hibbert EJ, Cunningham I, Gordon FC, et al. Clinical skills in junior medical officers: a comparison of self-reported confidence and observed competence. Med Educ. 2004;38(4):358–367. doi: 10.1046/j.1365-2923.2004.01773.x. [DOI] [PubMed] [Google Scholar]
- 8.Lerner BS, Kalish V, Ledford CJ. Exploring residents' skills in diagnosing dementia: the unexpected dissonance between ability and confidence. Fam Med. 2017;49(6):460–463. [PubMed] [Google Scholar]
- 9.Shah D, Haisch CE, Noland SL. Case reporting, competence, and confidence: a discrepancy in the numbers. J Surg Educ. 2018;75(2):304–312. doi: 10.1016/j.jsurg.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 10.Gude T, Finset A, Anvik T, Bærheim A, Fasmer OB, Grimstad H, et al. Do medical students and young physicians assess reliably their self-efficacy regarding communication skills? A prospective study from end of medical school until end of internship. BMC Med Educ. 2017;17(1):107. doi: 10.1186/s12909-017-0943-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Violato C, Lockyer J. Self and peer assessment of pediatricians, psychiatrists and medicine specialists: implications for self-directed learning. Adv Health Sci Educ Theory Pract. 2006;11(3):235–244. doi: 10.1007/s10459-005-5639-0. [DOI] [PubMed] [Google Scholar]
- 12.Hodges B, Regehr G, Martin D. Difficulties in recognizing one's own incompetence: novice physicians who are unskilled and unaware of it. Acad Med. 2001;76(10 suppl):87–89. doi: 10.1097/00001888-200110001-00029. [DOI] [PubMed] [Google Scholar]
- 13.Sargeant J, Mann K, Sinclair D, Van der Vleuten C, Metsemakers J. Understanding the influence of emotions and reflection upon multi-source feedback acceptance and use. Adv Health Sci Educ. 2008;13(3):275–288. doi: 10.1007/s10459-006-9039-x. [DOI] [PubMed] [Google Scholar]
- 14.Madrazo L, Lee CB, McConnell M, Khamisa K. Self-assessment differences between genders in a low-stakes objective structured clinical examination (OSCE) BMC Res Notes. 2018;11(1):393. doi: 10.1186/s13104-018-3494-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Accreditation Council for Graduate Medical Education. ACGME Milestones Annual Report 2017. 2020 https://acgme.org/Portals/0/PDFs/Milestones/MilestonesAnnualReport2017.pdf?ver=2018-02-09-074057-013 Accessed August 24.
- 16.Zawadka M, Graczyńska A, Janiszewska A, Ostrowski A, Michałowski M, Rykowski M, et al. Lessons learned from a study of the integration of a point-of-care ultrasound course into the undergraduate medical school curriculum. Med Sci Monit. 2019;25:4104–4109. doi: 10.12659/MSM.914781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rakofsky JJ, Garlow SJ, Haroon E, Hermida AP, Young JQ, Dunlop BW. Assessing residents' confidence in the context of pharmacotherapy competence. Acad Psychiatry. 2017;41(3):350–353. doi: 10.1007/s40596-016-0613-0. [DOI] [PubMed] [Google Scholar]
- 18.Harris MB, von Keudell A, McMahon G, Bierer B. Physician self-assessment of leadership skills. Physician Exec. 2014;40(2):30–40. 36. [PubMed] [Google Scholar]
- 19.Nasher J. To seem more competent, be more confident. Harvard Business Review. 2020 https://hbr.org/2019/03/to-seem-more-competent-be-more-confident Accessed August 24.
- 20.Blouin D, Dagnone JD. Performance criteria for emergency medicine residents: a job analysis. CJEM. 2008;10(6):539–544. [PubMed] [Google Scholar]
- 21.Chamorro-Premuzic T. Less-confident people are more successful. Harvard Business Review. 2020 https://hbr.org/2012/07/less-confident-people-are-more-su Accessed August 24.


