Abstract
Background
The I-PASS framework is increasingly being adopted for patient handoffs after a recent study reported a decrease in medical errors and preventable adverse events. A key component of the I-PASS handoff included assignment of illness severity.
Objective
We evaluated whether illness severity categories can identify patients at higher risk of overnight clinical deterioration as defined by activation of the rapid response team (RRT).
Methods
The I-PASS handoff documentation created by internal medicine residents and patient charts with overnight RRT activations from April 2016 through March 2017 were reviewed retrospectively. The RRT activations, illness severity categories, vital signs prior to resident handoff, and patient outcomes were evaluated.
Results
Of the 28 235 written patient handoffs reviewed, 1.3% were categorized as star (sickest patients at risk for higher level of care), 18.8% as watcher (unsure of illness trajectory), and 79.9% as stable (improving clinical status). Of the 98 RRT activations meeting the inclusion criteria, 5.1% were labeled as star, 35.7% as watcher, and 59.2% as stable. Patients listed as watcher had an odds ratio of 2.6 (95% confidence interval 1.7–3.9), and patients listed as star had an odds ratio of 5.2 (95% confidence interval 2.1–13.1) of an overnight RRT activation compared with patients listed as stable. The overall in-hospital mortality of patients with an overnight RRT was 29.6%.
Conclusions
The illness severity component of the I-PASS handoff can identify patients at higher risk of overnight clinical deterioration and has the potential to help the overnight residents prioritize patient care.
What was known and gap
Despite increasing adoption of structured handoff systems like I-PASS by training programs, there are no studies using the components of the handoff to assess risk of clinical decompensation.
What is new
A review of resident-created I-PASS handoff documentation and patient charts with overnight rapid response team activations.
Limitations
The study was conducted at an institution within a single specialty, limiting generalizability. The patient population consisted only of those hospitalized on a teaching internal medicine service, and the handoff process was primarily between 2 postgraduate year 1 residents.
Bottom line
The illness severity component of the I-PASS handoff can identify patients at higher risk for overnight clinical deterioration.
Introduction
Communication failure has been increasingly recognized as a major cause of preventable adverse events in hospitalized patients.1 This is particularly important during patient handoffs, which have increased in frequency after restrictions on resident work hours.2 A recent multicenter study demonstrated that implementing a standardized handoff bundle, referred to as I-PASS, decreased medical errors and preventable adverse events.3,4
I-PASS is a mnemonic for the key elements of the handoff process: I, illness severity; P, patient summary; A, action items; S, situation awareness and contingency planning; and S, synthesis by receiver.5 The illness severity component requires residents to assign patients to 1 of 3 categories based on their clinical assessment of the likelihood of deterioration. The I-PASS study designated the illness severity categories as stable, watcher, and unstable, with watcher defined as “any clinician's ‘gut feeling' that a patient is at risk of deterioration or ‘close to the edge.'”3,4
Effective communication during patient handoffs should prioritize patients who are at a higher risk for deterioration and enable the cross-covering resident to anticipate and efficiently address potential causes of clinical deterioration. Despite increasing adoption of structured handoff systems by training programs, to our knowledge there are no studies using the components of the handoff to assess risk of clinical decompensation. To evaluate the effectiveness of the I-PASS handoff bundle implementation, we evaluated the illness severity assigned to patients who had overnight clinical deterioration defined by rapid response team (RRT) activation.
Methods
All Baylor College of Medicine internal medicine residents receive training on I-PASS, including a competency-based simulation during orientation. In the I-PASS training, Baylor College of Medicine further defines the illness severity categories as stable: improving clinical status and a low likelihood of needing significant interventions overnight; watcher: may need an intervention overnight or unsure of illness trajectory; and star: at risk for needing a higher level of care.
Postgraduate year 1 (PGY-1) residents transition patient care to a night float PGY-1 resident at 6 pm using the I-PASS method with both verbal and written communication. All residents are expected to update the written handoff sheet, including illness severity, on a daily basis.
Patient Population
This was a retrospective cohort study of patients at Ben Taub Hospital, a 444-bed county hospital in Houston, Texas. Patients were included if the primary service was an internal medicine teaching service between April 2016 and March 2017. All intensive care unit (ICU) patients were excluded. The RRTs were excluded for patients where RRT activation occurred during the daytime (7 am–6 pm), where handoff information was not available, and if there was a repeat RRTs for the same patient during the same night.
The RRT consists of an ICU nurse, senior overnight resident, respiratory therapist, and the patient's primary nurse. The RRT is primarily activated by nursing due to a change in the patient's clinical status requiring prompt medical attention. A member of the team is responsible for documenting the reason for activation, outcome of the RRT, and other patient details for internal quality review.
Data Collection and Validation
Data were collected by accessing a database of RRT activations between April 2016 and March 2017. Most rapid responses were activated by nurses or other concerned hospital staff who did not have access to physician I-PASS handoff information.
Resident night float handoff sheets located on a protected server were reviewed for the illness severity categorization. For patients with overnight RRT activation, the illness severity in the most recent handoff sheet prior to the event was used. The chart was reviewed for the most recent vital signs prior to the handoff, immediate outcome of the RRT, and patient outcome at hospital discharge.
Statistical Analysis
Basic descriptive statistics (eg, counts, proportions) were calculated using standard methods. Comparisons between proportions were performed using the χ2 or Fisher exact test, as appropriate.6 Logistic regression was used to compare the odds of experiencing an RRT for subjects who were categorized as watcher or star compared with those who were categorized as stable; clustered standard errors were used to adjust for the fact that each subject could contribute multiple observations. Poisson regression was used to analyze whether the number of RRTs depended on the time of night. Stata 12 (StataCorp LLP, College Station, TX) was used for all analyses.
This study was reviewed by the Baylor College of Medicine and Harris Health System institutional review boards, and informed consent was waived.
Results
Patient Illness Severity
A total of 28 235 patient handoffs were available for review, representing 5176 patients. Of all written patient handoffs, 1.3% (337 handoffs) were categorized as star, 18.8% (5309 handoffs) as watcher, and 79.9% (22 549 handoffs) as stable (Table 1).
Table 1.
Patient Handoffs and Rapid Response Teams (RRTs) Categorized by Illness Severity
| Illness Severitya | Patient Handoffs, n (%) | RRTs, n (%) | Incidence of RRT by Illness Severity, % (n/total) |
| Star | 377 (1.3) | 5 (5.1) | 1.33 (5/377) |
| Watcher | 5309 (18.8) | 35 (35.7) | 0.66 (35/5309) |
| Stable | 22 549 (79.9) | 58 (59.2) | 0.26 (58/22 549) |
| Total | 28 235 | 98 | 0.35 (98/28 235) |
Illness severity categories are defined at Baylor College of Medicine as stable, watcher, or star. Stable indicates improving clinical status; do not expect significant interventions overnight. Watcher indicates unsure of illness trajectory; could possibly need intervention overnight. Star indicates the sickest patients at risk of needing higher level of care overnight.
Of the 525 total RRT activations during the study period, 98 were included for further analysis (Figure 1). For patients with an overnight RRT activation, the illness severity listed on the handoff was star in 5.1% (5 patients), watcher in 35.7% (35 patients), and stable in 59.2% (58 patients; Table 1).
Figure 1.
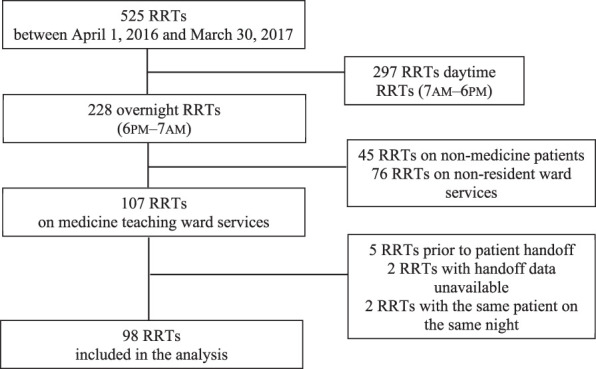
Chart Review Process to Find Patients Meeting the Inclusion Criteria
Abbreviation: RRT, rapid response team.
Overnight RRT activations occurred in 1.33% of patient handoffs labeled star, 0.66% of patient handoffs labeled watcher, and 0.26% of patient handoffs labeled stable. Compared with patients listed as stable during handoff, patients listed as watcher have an OR of 2.6 (95% CI 1.7–3.9) and patients listed as star have an odds ratio of 5.2 (95% confidence interval 2.1–13.1) for an overnight RRT activation (Figure 2). The RRT led to escalation in the level of care in 38.8% (38 of 98) and death in 4.1% (4 of 98) in patients during the RRT. Overall, the hospital mortality of patients with an overnight RRT was 28.6% (28 patients).
Figure 2.
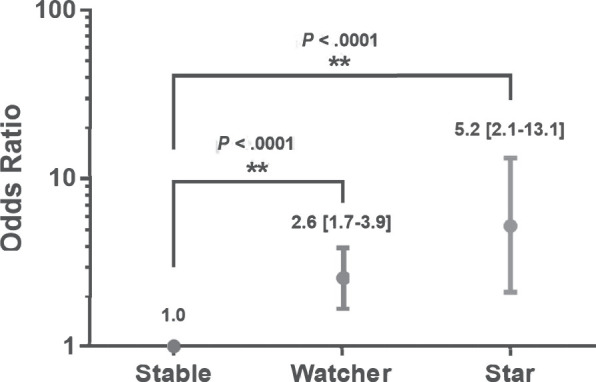
Overnight Rapid Response Team Activation Based on Illness Severity Category on Patient Handoff
RRT Activations
A majority of RRTs were called within 5 days of admission (52.0%, 51 of 98), with 29.6% of RRTs occurring in the first 48 hours. Indications for RRTs included cardiovascular (42.9%), followed by respiratory (36.7%) and neurological (28.6%). A single RRT activation could have multiple indications.
Over the study period, there were no significant month-to-month or day-to-day variations in the rate of RRTs. The incidence of RRTs did not significantly differ between weekend nights and weekday nights or between pre-midnight and post-midnight hours.
All patients with an overnight RRT were reviewed for vital-sign abnormalities documented prior to handoff. At least 1 vital sign abnormality was present in 55.2% (32 patients) labeled stable and 62.5% (25 patients) labeled watcher or star (Table 2). Overall, 58.1% (57 patients) had at least 1 vital-sign abnormality at the time of handoff prior to overnight clinical deterioration.
Table 2.
Vital Sign Abnormalities in Stable Compared With Watcher/Star Patients
| No. of Abnormal Vital Signsa | Stable Patients with Overnight RRT, n (%)b | Star and Watcher Patients with Overnight RRT, n (%)c |
| 0 | 26 (44.8) | 15 (37.5) |
| 1 | 20 (34.5) | 11 (27.5) |
| 2 | 9 (15.5) | 12 (30.0) |
| ≥3 | 3 (5.2) | 2 (5.0) |
Abnormal vital signs were defined as systolic blood pressure <100, heart rate >100 or <60, respiratory rate <12 or >20, and O2 saturation <90%.
N = 58.
N = 40.
Within the subset of patients with overnight RRTs, 38 patients had an escalation of care defined as transfer to the ICU. At handoff, 55.3% (21 patients) were assigned as stable, 39.5% (15 patients) as watcher, and 5.3% (2 patients) as star. Additionally, 36.8% (14 patients) had a preceding medical ICU/cardiac care unit stay during the same hospitalization. At least 1 abnormal vital sign was noted prior to handoff in 68.4% (26 patients) of this group compared with 51.0% (28 patients) of the 55 patients with overnight RRTs without escalation of care. An abnormal heart rate at the time of handoff was recorded for 52.6% (20 of 38) of patients with RRT leading to an escalation of care compared with 27.3% (15 of 55) of patients with RRT without escalation of care.
The mean time from handoff to RRT activation for patients requiring escalation of care and those without escalation was 399 and 391 minutes, respectively (P = .87, unpaired t test).
Discussion
This study demonstrated that the illness severity category of I-PASS handoffs could identify patients at higher risk for overnight clinical deterioration. Compared with patients categorized as stable, the likelihood for overnight clinical deterioration was 2.6 times higher for patients listed as watcher and 5.2 times higher for those listed as star.
Several studies have shown variations in clinical care and RRT activation based on month of the academic year, timing in the night, and weekends.7–9 Our study showed no statistical differences for these analyses, which may be partly due to the inadequate power from the number of RRT activations meeting the inclusion criteria. Escalation of patient care occurred in 38.8% of RRTs, which mirrors findings of a larger nationwide study.10 In-hospital mortality after overnight RRT in this study was 28.6%, near the upper range of 15% to 29% reported in the literature.10,11
Our results showed that illness severity within I-PASS handoffs could be an effective early warning system for clinical deterioration. Several early warning systems have been studied, including the Patient Acuity Rating, Modified Early Warning System, and others.12–16 The advantage to using the I-PASS illness severity is the increasing adoption of this method for handoffs, so additional training and information at the time of handoff is not needed.
Previous studies have shown that abnormal vital signs during hospitalization led to increased risk for clinical deterioration.17 The majority of patients had at least 1 abnormal vital sign at handoff prior to clinical deterioration, which is higher than reported in a previous study.17 This study also found that abnormal heart rate at the time of handoff was more closely linked to a higher need for escalation of care. The concept of combining clinical judgment and vital-sign abnormalities has been shown to be more accurate.18 Incorporating vital sign abnormalities into the illness severity categories could potentially improve the tool.
Churpek et al7 suggested that the goal of an early warning score is to increase the frequency of monitoring in a high-risk patient population. Since this study identified patients at risk of clinical deterioration, several quality improvement initiatives have been implemented. First, the I-PASS training for residents now includes more descriptive definitions of the illness severity categories, which encourages active review of vital-sign abnormalities prior to handoff. Second, the written communication is now documented through the handoff functionality within the electronic medical record, making the information more accessible. Finally, the RRT and overnight residents are encouraged to evaluate all patients labeled as star prior to any clinical deterioration. The impact of these initiatives is still being evaluated.
This study has several limitations. First, it was conducted at a single institution with residents from a single internal medicine residency program. With variability in the implementation of RRT across hospitals, general applicability may be limited. Training in how to categorize patients is very important, and this study demonstrated some variability in how this may be interpreted by different residents. Second, this study focused on overnight RRT activations so extrapolation of risk predictability to daytime activations is limited. Third, the study did not account for overnight escalation of care through ICU transfers or code blue events in the absence of an RRT activation. The patient population was narrowed to only patients hospitalized on a teaching internal medicine service, so results may differ for other clinical services. In addition, this study evaluated vital signs prior to overnight RRT activation without comparisons to the patient population without RRT activation. Finally, the handoff process was primarily between 2 PGY-1 residents, so the results may have been different with senior residents.
Conclusions
This study provides evidence that the illness severity component of the I-PASS handoff can identify patients at higher risk for overnight clinical deterioration. The study further confirms the importance of using I-PASS handoff during transitions in patient care.
Footnotes
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
References
- 1.The Joint Commission. Sentinel Event Data. 2020 https://www.jointcommission.org/se_data_event_type_by_year_/ Accessed August 17.
- 2.Desai SV, Feldman L, Brown L, Dezube R, Yeh H-C, Punjabi N, et al. Effect of the 2011 vs 2003 duty hour regulation-compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff: a randomized trial. JAMA Intern Med. 2013;173(8):649–655. doi: 10.1001/jamainternmed.2013.2973. [DOI] [PubMed] [Google Scholar]
- 3.Starmer AJ, Spector ND, Srivastava R, West DC, Rosenbluth G, Allen AD, et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803–1812. doi: 10.1056/NEJMsa1405556. [DOI] [PubMed] [Google Scholar]
- 4.Starmer AJ, Sectish TC, Simon DW, Koehane C, McSweeney ME, Chung EY, et al. Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA. 2013;310(21):2262–2270. doi: 10.1001/jama.2013.281961. [DOI] [PubMed] [Google Scholar]
- 5.Starmer AJ, Spector ND, Srivastava R, Allen AD, Landrigan CP, Sectish TC. I-PASS. a mnemonic to standardize verbal handoffs. Pediatrics. 2012;129(2):201–204. doi: 10.1542/peds.2011-2966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agresti A. Categorical Data Analysis 3rd ed. New York, NY: Wiley;; 2013. [Google Scholar]
- 7.Churpek MM, Edelson DP, Lee JY, Carey K, Snyder A. Association between survival and time of day for rapid response team calls in a national registry. Crit Care Med. 2017;45(10):1677–1682. doi: 10.1097/CCM.0000000000002620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sundararajan K, Flabouris A, Thompson C. Diurnal variation in the performance of rapid response systems: the role of critical care services—a review article. J Intensive Care. 2016;4:15. doi: 10.1186/s40560-016-0136-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones D, Bates S, Warrillow S, Opdam H, Goldsmith D, Gutteridge G, et al. Circadian pattern of activation of the medical emergency team in a teaching hospital. Crit Care. 2005;9(4):R303–R306. doi: 10.1186/cc3537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shappell C, Snyder A, Edelson DP, Churpek MM. Predictors of in-hospital mortality after rapid response team calls in a 274 hospital nationwide sample. Crit Care Med. 2018;46(7):1041–1048. doi: 10.1097/CCM.0000000000002926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tirkkonen J, Tamminen T, Skrifvars MB. Outcome of adult patients attended by rapid response teams: a systematic review of the literature. Resuscitation. 2017;112:43–52. doi: 10.1016/j.resuscitation.2016.12.023. [DOI] [PubMed] [Google Scholar]
- 12.Phillips AW, Yuen TC, Retzer E, Woodruff J, Arora V, Edelson DP. Supplementing cross-cover communication with the patient acuity rating. J Gen Intern Med. 2013;28(3):406–411. doi: 10.1007/s11606-012-2257-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Edelson DP, Retzer E, Weidman EK, Woodruff J, Davis AM, Minsky BD, et al. Patient acuity rating: quantifying clinical judgment regarding inpatient stability. J Hosp Med. 2011;6(8):475–479. doi: 10.1002/jhm.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ratelle JT, Kelm DJ, Halvorsen AJ, West CP, Oxentenko AS. Predicting and communicating risk of clinical deterioration: an observational cohort study of internal medicine residents. J Gen Intern Med. 2015;30(4):448–453. doi: 10.1007/s11606-014-3114-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O'Donnell C, Thomas S, Johnson C, Verma L, Bae J, Gallagher D. Incorporating patient acuity rating score into patient handoffs and the correlation with rapid responses and unexpected ICU transfers. Am J Med Qual. 2017;32(2):122–128. doi: 10.1177/1062860616630809. [DOI] [PubMed] [Google Scholar]
- 16.Smith ME, Chiovaro JC, O'Neil M, Kansagara D, Quiñones AR, Freeman M, et al. Early warning system scores for clinical deterioration in hospitalized patients: a systematic review. Ann Am Thorac Soc. 2014;11(9):1454–1465. doi: 10.1513/AnnalsATS.201403-102OC. [DOI] [PubMed] [Google Scholar]
- 17.Lighthall GK, Markar S, Hsiung R. Abnormal vital signs are associated with an increased risk for critical events in US veteran inpatients. Resuscitation. 2009;80(11):1264–1269. doi: 10.1016/j.resuscitation.2009.08.012. [DOI] [PubMed] [Google Scholar]
- 18.Patel AR, Zadravecz FJ, Young RS, Williams MV, Churpek MM, Edelson DP. The value of clinical judgment in the detection of clinical deterioration. JAMA Intern Med. 2015;175(3):456–458. doi: 10.1001/jamainternmed.2014.7119. [DOI] [PubMed] [Google Scholar]


