Abstract
Objective
We have reviewed the data of the patients in order to evaluate the effectiveness of our ureterocystoplasty technique in augmentation cystoplasty operation.
Material and methods
Data of a total of 16 patients with bilateral functional kidneys who had undergone augmentation ureterocystoplasty between January 1995 and June 2018 which were retrieved during the retrospective archive scanning were included in the study. Ultrasonography (USG), serum blood urea nitrogen and creatinine values and Technetium-99 DTPA (Tc-99 DTPA) scan were used to evaluate the renal function of the patients. Intravenous pyelography (IVP) and USG were used to evaluate the ureters before surgery. Magnetic resonance (MR) urographies were performed in our center.
Results
Of the total 16 patients, 10 were male and 6 were female, while ages ranged from 1 to 24 years. Among 16 patients, the most common cause of neurogenic bladder etiology was meningomyelocele. In the urodynamic studies performed before the operation, it was determined that the bladder capacities of the patients were between 40–180 mL and the bladder compliances were 1.0–4.0 cc/cmH2O. At postoperative 3rd months, it was determined that the bladder capacities of the patients were between 180–330 mL and the bladder compliances were between 6.0–24.0 cc/cmH2O.
Conclusion
Augmentation ureterocystoplasty seems to be an appropriate technique in which successful results are obtained with appropriate patient selection. Besides, complications that may occur due to use of ileal segment are avoided.
Keywords: Augmentation ureterocystoplasty, meningomyelocele, neurogenic bladder
Introduction
Augmentation cystoplasty is an enlargement surgery designed to preserve the upper urinary tract in patients with low compliance or inadequate bladder storage capacity. In the normal bladder function, the pressure in the bladder is low during the storage phase. Compliance is the ability of the bladder to expand during filling. With this characteristic feature, the bladder volume increases while the bladder pressure is low. The main indication for bladder augmentation is a low-compliant, low-capacity bladder that causes urinary incontinence and impaired renal function.[1,2]
Inflammatory diseases such as tuberculosis and chronic interstitial cystitis, posterior urethral valve and meningomyelocele, as well as the restored bladder in the extrofied epispadias complex and diseases with neurogenic bladder, such as Hinman’s syndrome, which have no neurological etiology, constitute an augmentation cystoplasty indications.[3]
In the augmentation cystoplasty various organs can be used to enlarge the bladder. Large, or small bowels, stomach and ureter can be used for this purpose. Techniques that use bowels can lead to many metabolic and infective complications in the long run. For this reason, ureterocystoplasty made by using ureter tissue that mimics normal bladder tissue seems to be the most appropriate technique. Ureterocystoplasty is widely accepted with low complication rates compared to techniques that use intestines.[4]
In our study, using retrospective screening technique we analyzed the indications, complications and outcomes of our patients who had undergone ureterocystoplasty.
Material and methods
A total of 16 patients with bilateral functional kidneys who had undergone augmentation ureterocystoplasty between January 1995 and June 2018 were included in the study. All patients were evaluated preoperatively with whole blood, routine biochemical analyzes, complete urinalysis, urine culture, whole abdominal ultrasonography (USG), technetium-99 m diethylenetriaminepentaacetic acid (DTPA) renal scintigraphy, voiding cystourethrography (VCUG) and urodynamic study. Magnetic resonance (MR) urography was used after initial were started to to evaluate ureters before surgery, previously intravenous pyelography (IVP) and USG were used. With the introduction of MR urography in clinical practice, MR urography was started to be used in our center. All surgeries were performed after sterile urine cultures were obtained. Routine intestinal cleansing was performed in all patients in case of possible use of the intestinal segment.
This retrospective study was conducted according to the Helsinki Declaration. Written informed consent was obtained from the parents of the patients and patient who participated in this study.
Surgical technique
In ureterocystoplasty technique used in patients; up to 1999, end-to-side transureteroureterostomy and anastomosis of a single ureter to the bladder was used (ureteroneocystostomy technique). After 1999, ureteroureterostomy was abandoned and both ureters were anastomosed separately to the posterior wall of the bladder through extravesical approach. In both techniques, distal portions of the ureters were used for augmentation.
Using the classical transureteroureterostomy technique, through infraumbilical median incision the abdominal cavity was entered, both ureters were found and held with suspension sutures. Later, the ureters were released towards both proximal and distal directions taking care not to disturb their circulation. The ureter of the kidney with lower fractional function was anastomosed in an end-to-side fashion to the ureter of the kidney with higher functional function with 5/0 polyglactin sutures. The distal end of the ureter that was used for end-to-side anastomosis was cut to be used for augmentation, while its proximal end was cut to be used for reimplantation to the bladder. Distal parts of both ureters were detubularized and anastomosed to the bladder. Proximal ureter was anastomosed to the bladder using extravesical approach.
In the second technique through Pfannenstiel incision abdominal cavity was entered. Ureters were found where they cross over common iliac arteries, and and held with suspension sutures. Then, the ureters were released towards both proximal and distal directions taking care not to disturb their circulation. Both ureters were cut at their distal ends to be used for augmentation, and their ends were cut so as to anastomose them to the bladder. The bladder was divided into two parts at its coronal plane between both ureter orifices. This bladder incision was advanced to the medial side of both ureters so as to include the ureter orifices on both sides. Distal ureters were detubularized. The constructed patch was anastomosed to anterior and posterior bladder halves on both sides with 4/0 polyglactin sutures. Proximal parts of the ureters were excisionally tapered, and reimplanted via extravesical route (Figure 1 and 2).[5] Both ureteral double J (DJ) catheters were inserted into both ureters. The bladder dome was sutured and the procedure was completed. Suprapubic tube was not placed, and the procedure was terminated by inserting urethral Foley catheter.
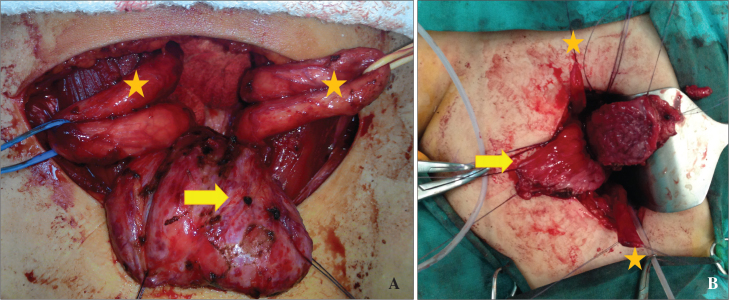
Figure 1. a, b.
Bladder to be augmented (arrow), and both of dilated ureters (star) to be used for augmentation (a). Preparation of the bladder for augmentation (arrow), and distal ureteral segments to be used for cystoplasty (star) (b)
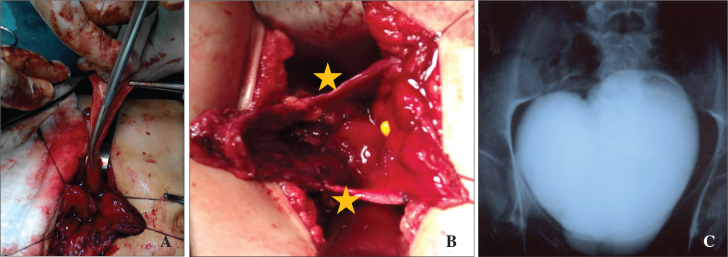
Figure 2. a–c.
Detubularization of ureteral segments to be used for augmentation starting from their orifices (a) Anastomosis of detubularized ureters to the lateral wall of the blsdder (star) (b). Postoperative cystogram (c)
Follow-up
Patients’ urethral catheters were removed on postoperative day 7, and DJ stents on day 21. In the first postoperative month, kidneys and ureters were evaluated with USG At postoperative 3rd month, DTPA renal scintigraphy was used to rule out obstruction, and videourodynamic evaluation was performed to evaluate bladder dynamics, and reflux. Afterwards the patients were checked with annual follow-ups.
Results
Of the 16 patients, 10 were male and 6 were female. The ages of our cases ranged from 1 to 24 years (mean 8.6±5.5 years). All patients had large ureters and bilateral functioning kidneys, and bladders with low-capacity, and compliance When we looked at the etiology of hydroureteronephrosis, the patients had meningomyelocele (n=9), posterior urethral valve (PUV) (n=3), Hinman syndrome (n=2), and 2 patients had their bladders repaired due to bladder extrophy.
Preoperative urodynamic studies were performed to measure the patients’ bladder capacities (median, 115 mL; range, 40–180 mL) and compliance (median, 2.4 cc/cmH2O; range, 1.0 4.0 cc/cmH2O). All patients had bilateral high grade (grade 4–5) VUR before surgery.
The median length of the ureters used for the augmentation was 8.5 cm (range, 6 to 11 cm (median) and their median width ranged from 1.5 to 3.5 cm (median 2.1 cm).
Any major postoperative complications were not observed in any patient in the early postoperative period, wound site infections and urine leakage were seen in 2 patients. The urine leakage was resolved spontaneously and wound site infection was healed with appropriate antibiotic. In one patient the DJ stent was reimplanted to the patient upon detection of pain after DJ stent extraction and it was withdrawn after one month. Patient’s pain had disappeared during follow-up period.
Urodynamic evaluation of the patients at 3rd postoperative months revealed increase in bladder capacities up to 180–330 mL (median 245 mL) and bladder compliance up to 6.0 to 24.0 cc/cmH2O (mean 13.1 cc/cmH2O) (Table 1). Vesico uretral reflux (VUR) was not detected in any of the patients. DTPA renal scintigraphy showed no evidence of impairment of renal function and finding suggestive of any obstruction in any patient.
Table 1.
Demographic characteristics of the patients
| Patient | Age (year) | Gender | Primary pathology | Preoperative | Postoperative | ||
|---|---|---|---|---|---|---|---|
| Bladder volume (mL) | Bladder compliance (cc/cmH2O) | Bladder volume (mL) | Bladder compliance (cc/cmH2O) | ||||
| 1 | 1 | M | Meningo-myelocele | 50 | 1.0 | 180 | 9.5 |
| 2 | 7 | M | Meningo-myelocele | 40 | 1.0 | 330 | 24.0 |
| 3 | 6 | F | Meningo-myelocele | 65 | 1.6 | 310 | 14.8 |
| 4 | 5 | F | Meningomyelocele | 50 | 1.1 | 295 | 15.6 |
| 5 | 6 | M | Meningomyelocele | 170 | 4.0 | 320 | 14.6 |
| 6 | 4 | F | Meningomyelocele | 80 | 1.7 | 270 | 11.8 |
| 7 | 4 | M | Meningomyelocele | 70 | 2.0 | 250 | 17.9 |
| 8 | 12 | M | PUV | 155 | 3.4 | 215 | 10.8 |
| 9 | 5 | F | Vesical extrophy | 125 | 2.8 | 190 | 7.6 |
| 10 | 11 | M | PUV | 165 | 3.1 | 240 | 16.0 |
| 11 | 8 | M | Vesical extrophy | 125 | 2.2 | 205 | 13.7 |
| 12 | 10 | F | Meningo-myelocele | 150 | 2.3 | 215 | 8.2 |
| 13 | 16 | M | Hinman Syndrome | 130 | 2.8 | 205 | 11.4 |
| 14 | 24 | F | Hinman Syndrome | 160 | 3.2 | 230 | 11.5 |
| 15 | 7 | F | Meningo-myelocele | 125 | 2.4 | 195 | 6.0 |
| 16 | 12 | M | PUV | 180 | 3.6 | 270 | 15.0 |
| Mean | 115 (40–180) | 2.4 (1.0–4.0) | 245 (180–330) | 13.1 (6.0–24.0) | |||
PUV: posterior urethral valve
Among our patients who underwent ureterocystoplasty 5 of them was able to urinate spontaneously and without severe residual urine. The remaining 11 patients were able to void their urine using clean intermittent catheterization procedure.
Our average follow-up period was 30 months (4–72 months). During the follow-up period two patients who had undergone transurethral endarterectomy underwent end-to-side anastomosis due to development of restenosis at the anastomosis site. Any augmentation procedure was not necessary in any patient during follow-up period. All patients were continent.
Discussion
Bladder augmentation has been practiced since 1950’s. Although most frequently ileal segment is used, nowadays there is no consensus about which of the tissues used in the bladder augmentation is more ideal. Intestinal segments such as ileum, stomach, ileocecal valve, ascending colon and sigmoid colon, as well as dilate ureters are also used for augmentation purposes in eligible cases.[3–7]
Intestinal segments increase bladder capacity as much as desired and provide improved bladder compliance. Intestinal segments have disadvantages arising from persistence of mucus production, and absorptive ability of intestinal segments including mucus-associated stone formation, absorption of stored urine, and potential development of malignancy due to chronic contact of intestinal mucosa with urine related to.[6,7]
In pediatric patients, gastrocystoplasty has been started to be applied with the use of a gastric segment to avoid complications that might develop due to mucus release. However, because of development of hematuria, dysuria, ulceration, and metabolic alkalosis during the postoperative period use of gastric segment was discouraged.[8]
In 1973, Eckstein et al.[9] firstly performed nephrectomy in a child with a unilateral hypofunctional kidney and used ipsilateral ureter for augmentation and published their case. However, this technique has gained popularity after Bellinger et al.[10] in 1993, nephrectomized nonfunctional kidney, and applied augmentation ureterocystoplasty using detubularized ipsilateral ureter, and publication of ureterocystoplasty technique in functional kidneys performed by Churchill et al.[11] in the same year.
The greatest advantages of this technique is the lack of mucus secretion and metabolic complications of the ureters used for augmentation and relatively lower risk of infection and stone formation. In addition, the intestinal mucosa is a foreign mucosa for the urinary system, and the chronic contact of the mucosa with the urine reduces the risk of developing malignancy over many years.[11]
A limited number of studies compared ureterocystoplasty with ileocystoplasty techniques in the literature and publications reporting urodynamic results of augmentation ureterocystoplasty techniques are also available.[12,13]
In studies comparing augmentation cystoplasty operations using ileal and ureteral segments Landau et al.[12] reported that ureterocystoplasty technique can provide adequate bladder capacity and compliance as the ileocystoplasty technique, besides Landau et al.[12] reported that the and that the disadvantages of ileal segment usage are not encountered in ureterocystoplasties. In our cases, mean bladder capacities of the patients were found to be in the range of 180 to 330 mL (median 245 mL) and urinary bladder compiliances increased up to 6.0 to 24.0 cc/cmH2O (mean 13.1±4.29 cc/cmH2O) as estimated in urodynamic examinations performed at 3 months postoperatively.
Complications such as ureteral anastomotic stricture, ureterovesical anastomotic stricture, anastomotic leakage, VUR, insufficient bladder capacity and urinary infection have been reported in the literature.[11,14] The most common complication is the potential development of stenosis at the uretero-ureterostomy line especially in cases of transureteroureterostomy technique. Churchill et al.[11] reported that ureterovesical stenosis developed in 2 of their 16 patients who had undergone transureteroureterostomy. In our series in two patients who underwent transureteroureterostomy, stenosis developed on the site of anastomosis which required re-application of end-to-side anastomosis. In one patient, dilatation in the collecting system of both kidneys was detected due to the presence of a stone in the lower end of the ureter and dilatation of both kidneys regressed after intervention to the stone.
We did not encounter any other complications reported in the literature. However, we modified our operative technique for reasons such as the end-to-side anastomotic stenosis, and adverse effects of distal ureteral stones on both kidneys. We think that one by one anastomosis of ureters using extravasical technique posterior to the bladder is an important factor which helps us to observe the complications mentioned in the literature.
When the postoperative period was evaluated in terms of patient comfort; we see that the ureterocystoplasty technique is superior to ileocystoplasty. We are applying both techniques in our center and we have observed that in patients who underwent ureterocystoplasty, the intestinal integrity is not impaired and it provides a faster return to normal life, besides the patient is protected from possible intestinal anastomotic leakage.
The most important factor limiting the augmentation ureterocystoplasty technique is the risk that the hydronephrotic dilated ureters are not always present, and therefore adequate bladder volume can not be achieved after augmentation. Several publications in the literature have indicated that expanded ureteral tissue was used for the purpose of cystoplasty to reduce this risk.[15] When considering the use of ureter the cases to be selected for cystoplasty should be well evaluated preoperatively.
In all of our cases, using imaging methods we investigate whether the degree of dilatation of the ureters is suitable for operation. When we think that the use of the ureters will not provide enough bladder volume during the operation, we perform bowel cleaning in all of our patients before surgery to considering the possibility of using ileum segment.
As a result, augmentation ureterocystoplasty seems to be a good technique in which successful results can be obtained with appropriate patient selection. During the preoperative period, the anatomical findings of the patient should be evaluated very well.
Footnotes
Ethics Committee Approval: Authors declared that the research was conducted according to the principles of the World Medical Association Declaration of Helsinki “Ethical Principles for Medical Research Involving Human Subjects”, (amended in October 2013).
Informed Consent: Written informed consent was obtained from the parents of the patients and patient who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - G.E.; Design - G.E., Y.K.; Supervision - Y.K., M.D.; Resources - G.E., B.K., T.E.; Materials - G.E., Y.K., M.D.; Data Collection and/or Processing - G.E., T.E., B.K.; Analysis and/or Interpretation - G.E., T.E.; Literature Search - G.E., B.K., T.E.; Writing Manuscript - G.E., Y.K., T.E.; Critical Review - G.E., Y.K., M.D.; Other - T.E., B.K.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Kurpad R, Kennelly MJ. The evaluation and management of refractory neurogenic overactive bladder. Curr Urol Rep. 2014;15:444. doi: 10.1007/s11934-014-0444-z. [DOI] [PubMed] [Google Scholar]
- 2.Eswara JR, Castellan M, González R, Mendieta N, Cendron M. The urological management of children with spinal cord injury. World J Urol. 2018 doi: 10.1007/s00345-018-2433-1. doi: 10.1007/s00345-018-2433-1. [DOI] [PubMed] [Google Scholar]
- 3.Johal NS, Hamid R, Aslam Z, Carr B, Cuckow PM, Duffy PG. Ureterocystoplasty: long-term functional results. J Urol. 2008;179:2373–6. doi: 10.1016/j.juro.2008.01.170. [DOI] [PubMed] [Google Scholar]
- 4.Malone MJ, Izes JK, Hurley LJ. Carcinogenesis. The fate of intestinal segments used in urinary reconstruction. Urol Clin North Am. 1997;24:723–8. doi: 10.1016/S0094-0143(05)70414-6. [DOI] [PubMed] [Google Scholar]
- 5.Babu R, Ragoori D. Bladder augmentation: Distal ureterocystoplasty with proximal ureteric reimplantation: A novel technique. J Indian Assoc Pediatr Surg. 2012;17:165–7. doi: 10.4103/0971-9261.102337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stampfer DS, McDougal WS, McGovern FJ. The use of in bowel urology. Metabolic and nutritional complications. Urol Clin North Am. 1997;24:715–22. doi: 10.1016/S0094-0143(05)70413-4. [DOI] [PubMed] [Google Scholar]
- 7.Malone MJ, Izes JK, Hurley LJ. Carcinogenesis. The fate of intestinal segments used in urinary reconstruction. Urol Clin North Am. 1997;24:723–8. doi: 10.1016/S0094-0143(05)70414-6. [DOI] [PubMed] [Google Scholar]
- 8.Gosalbez R, Jr, Woodard JR, Broecker BH, Parrott TS, Massad C. The use of stomach in pediatric urinary reconstruction. J Urol. 1993;150:438–40. doi: 10.1016/S0022-5347(17)35594-5. [DOI] [PubMed] [Google Scholar]
- 9.Eckstein HBMM. Uretero-cystoplastic. Act Urol. 1973:255–7. [Google Scholar]
- 10.Bellinger MF. Ureterocystoplasty: a unique method for vesical augmentation in children. J Urol. 1993;149:811–3. doi: 10.1016/S0022-5347(17)36215-8. [DOI] [PubMed] [Google Scholar]
- 11.Churchill BM, Aliabadi H, Landau EH, McLorie GA, Steckler RE, McKenna PH, et al. Ureteral bladder augmentation. J Urol. 1993;150:716–20. doi: 10.1016/S0022-5347(17)35596-9. [DOI] [PubMed] [Google Scholar]
- 12.Landau EH, Jayanthi VR, Khoury AE, Churchill BM, Gilmour RF, Steckler RE, et al. Bladder augmentation: ureterocystoplasty versus ileocystoplasty. J Urol. 1994;152:716–9. doi: 10.1016/S0022-5347(17)32689-7. [DOI] [PubMed] [Google Scholar]
- 13.Gericke D, Kovac W, Flamm H. Experimental studies on mycoplasma-induced leukemogenesis. Zentralbl Bakteriol Orig A. 1971;218:343–55. [PubMed] [Google Scholar]
- 14.Gosalbez R, Jr, Kim CO., Jr Ureterocystoplasty with preservation of ipsilateral renal function. J Pediatr Surg. 1996;31:970–5. doi: 10.1016/S0022-3468(96)90425-X. [DOI] [PubMed] [Google Scholar]
- 15.Ikeguchi EF, Stifelman MD, Hensle TW. Ureteral tissue expansion for bladder augmentation. J Urol. 1998;159:1665–8. doi: 10.1097/00005392-199805000-00086. [DOI] [PubMed] [Google Scholar]