Abstract
Purpose
Infectious diseases are more frequent and can be associated with worse outcomes in patients with diabetes. The aim of this study was to systematically review and conduct a meta-analysis of the available observational studies reporting the effect of diabetes on mortality among hospitalized patients with COVID-19.
Methods
The Medline, Embase, Google Scholar, and medRxiv databases were reviewed for identification of eligible studies. A random effects model meta-analysis was used, and I2 was utilized to assess the heterogeneity. In-hospital mortality was defined as the endpoint. Sensitivity, subgroup, and meta-regression analyses were performed.
Results
A total of 18,506 patients were included in this meta-analysis (3713 diabetics and 14,793 non-diabetics). Patients with diabetes were associated with a higher risk of death compared with patients without diabetes (OR 1.65; 95% CI 1.35–1.96; I2 77.4%). The heterogeneity was high. A study-level meta-regression analysis was performed for all the important covariates, and no significant interactions were found between the covariates and the outcome of mortality.
Conclusion
This meta-analysis shows that that the likelihood of death seems to be higher in diabetic patients hospitalized with COVID-19 compared with non-diabetic patients. Further studies are needed to assess whether this association is independent or not, as well as to investigate the role of adequate glycemic control prior to infection with COVID-19.
Electronic supplementary material
The online version of this article (10.1007/s42000-020-00246-2) contains supplementary material, which is available to authorized users.
Keywords: COVID-19, SARS-CoV-2, Diabetes, Mortality, Risk factor, Meta-analysis
Introduction
Diabetes mellitus is one of the leading causes of morbidity and mortality worldwide and is associated with significant cardiovascular and renal complications. The estimated global prevalence was 9.3% in 2019 with an upward trend [1, 2]. In the USA alone, more than 34 million adults had known or undiagnosed diabetes in 2018 [3]. In 2017, diabetes was listed as the underlying or contributing cause of death on 270,702 death certificates, which corresponds to a crude rate of 83.1 per 100,000 persons [3].
Infectious diseases are more frequent and can be associated with worse outcomes in patients with diabetes [4]. Therefore, it is not surprising that diabetes has been considered as a possible risk factor or a predictor for worse outcomes in patients with coronavirus disease 2019 (COVID-19) [5–7]. COVID-19 rapidly reached the level of a pandemic and has caused more than 850,000 deaths worldwide within a few months despite unprecedented mitigation measures [8]. The strength of the association between diabetes and COVID-19 has been investigated in observational cohorts around the world.
We aimed to systematically review and conduct a meta-analysis of the available observational studies reporting the effect of diabetes on mortality among hospitalized patients with COVID-19.
Materials and methods
This study was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [9], although only observational studies were included.
Literature search
We conducted a systematic literature search of the Medline, Embase, Google Scholar, and medRxiv (the preprint server for health sciences) databases up to May 10, 2020 for observational studies providing data concerning any kind of association between diabetes and mortality in hospitalized patients with COVID-19. The reference lists of the possibly eligible articles and the relevant secondary research studies were reviewed manually. Two investigators (LP and DGK) independently searched for eligible studies. In cases where there was a disagreement regarding the eligibility of a study, a third investigator (FZ) was involved in order for consensus to be reached. The reference list of pertinent reviews and observational studies were also manually searched for further potentially eligible studies. A combination of the following keywords was used to perform our search: “COVID-19,” “SARS-CoV-2,” “novel coronavirus,” “risk factor,” “mortality,” and “death.” The search algorithms that were used for each database are provided in Supplementary Methods. The pre-specified inclusion criteria were as follows: (i) studies which included adult patients hospitalized for COVID-19 and (ii) studies that provided data on any kind of association between diabetes and mortality in the aforementioned population. The pre-specified exclusion criteria were as follows: (i) certainly or possibly duplicated or overlapping patient populations and (ii) studies that included pre-specified patient populations based on a specific diagnosis (e.g., only hypertensives or only patients with cancer). In the case of duplicated or overlapping populations, the studies with a larger sample size were included.
Data extraction and outcomes
Data extraction was performed based on a pre-defined data extraction form by two independent investigators (NCP and WL) blinded to each other. The pre-specified outcome was in-hospital mortality.
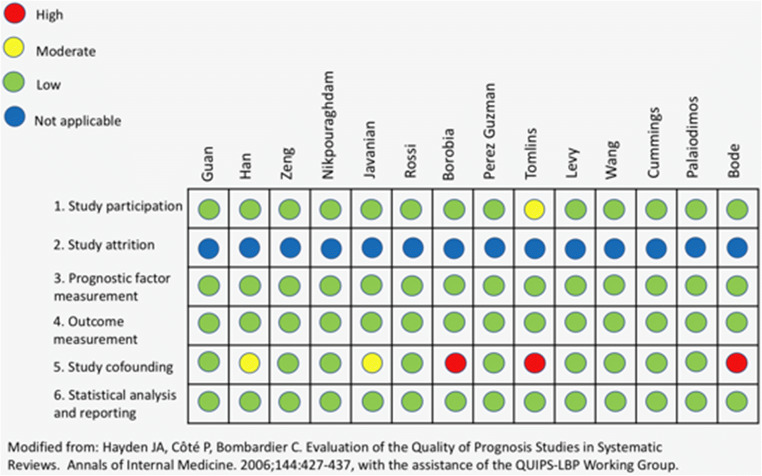
Risk of bias assessment
Two independent reviewers (NCP and PM) assessed the risk of bias of the included studies with the Quality in Prognosis Studies (QUIPS) tool [10]. Studies were assessed as having low, moderate, serious, or critical risk of bias for the following domains: study participation, study attrition, prognostic factor measurement, confounding measurement and account, outcome measurement, analysis, and reporting.
Statistical analysis
We estimated the odds ratios (ORs) and their respective 95% confidence intervals (CI) for all the individual studies. When neither OR nor event rates were provided, we used the unadjusted hazard ratios and converted them to ORs given the short follow-up period. For studies that provided both adjusted and unadjusted ORs, we used the unadjusted effect estimate. We performed a meta-analysis using the random effects model according to the method of Der Simonian and Laird. Heterogeneity among trials for each outcome was assessed with the I2 test. Values < 25% indicated low, 25 to 70% moderate, and > 70% high heterogeneity [11]. Egger’s test and funnel plots were used to assess for publication bias. Subgroup and sensitivity analyses were performed based on the location where the studies were conducted and the mean/median age. A meta-regression analysis was performed for important covariates in order to address high heterogeneity among the included studies. Statistical significance level was set at 0.05 with CI calculated at the 95% level. Stata 14.1 (Stata Corp., College Station, TX, USA) was used for statistical analysis.
Results
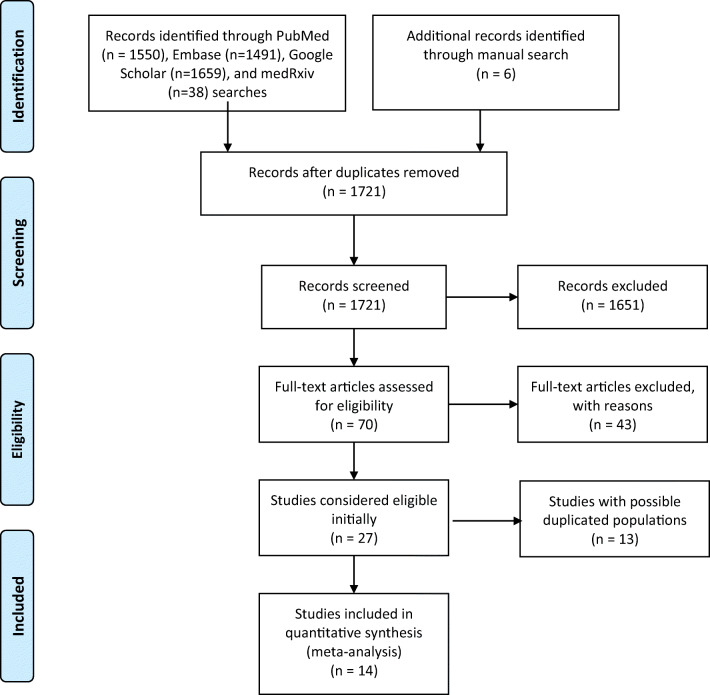
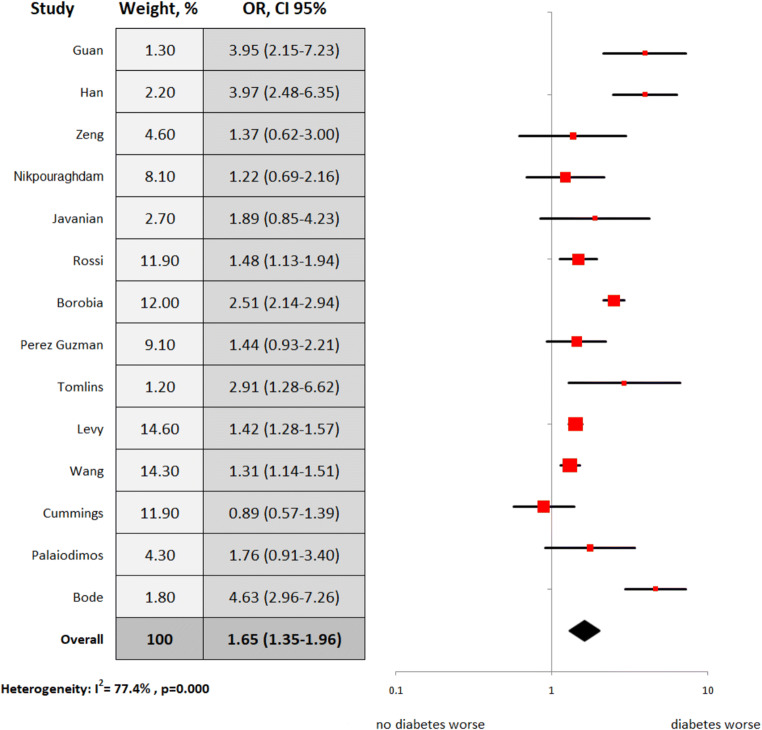
Out of 1721 studies screened from the literature and online sources, 14 observational studies (12 retrospective and two prospective) met the pre-specified criteria for inclusion in the analysis (Fig. 1) [12–25]. The characteristics of these studies are summarized in Table 1. Overall, all the studies were found to have a low risk of bias (Fig. 2). Five studies were conducted in Asia, five in the USA, and four in Europe. The total number of patients included in the final dataset was 18,506 patients, 3713 being diabetics and 14,793 non-diabetics. The mean or median age was above 60 years in 12 studies; 43% (7967) of the population were women (Table 2). Among studies which reported their results in event rates, the overall frequency of death events in diabetics was 41.1% (991 out of 2413) compared with 17.6% (2113 out of 12,012) in the non-diabetic group. (The numbers of death events in the groups of interest were not provided in three studies; instead, odds or hazard ratios were provided) In our meta-analysis of 14 studies, we found that patients with diabetes were associated with a higher risk of death compared with patients without diabetes, but with significant heterogeneity (OR 1.65; 95% CI 1.35–1.96; I2 77.4%; Fig. 3).
Fig. 1.
PRISMA 2009 flow diagram
Table 1.
Characteristics of the included studies
| Study | Country | Region | Institution | Study design | First patient | Last patient | Number of included patients |
|---|---|---|---|---|---|---|---|
| Guan | China | 31 regions (including Wuhan) | Multicenter | Retrospective | December 25 | January 31 | 1590 |
| Han | China | Wuhan | Tongji Hospital | Retrospective | February 2 | February 15 | 306 |
| Zeng | China | Xi’an and Wuhan | Multicenter (not Tongji Hospital) | Retrospective | February 5 | March 20 | 97 |
| Nikpouraghdam | Iran | Tehran | Baqiyatallah Hospital | Retrospective | February 19 | April 15 | 2964 |
| Javanian | Iran | Babol | Babol University of Medical Sciences | Retrospective | February 25 | March 12 | 100 |
| Rossi | Italy | Reggio Emilia | Multicenter | Prospective | February 27 | April 2 | 1075a |
| Borobia | Spain | Madrid | La Paz University Hospital | Retrospective | February 25 | April 19 | 2226 |
| Perez Guzman | UK | London | Imperial College Healthcare NHS Trust | Retrospective | February 25 | April 5 | 520 |
| Tomlins | UK | Bristol | North Bristol NHS Trust | Retrospective | March 1 | March 30 | 95 |
| Levy | USA | New York | Northwell Health | Retrospective | March 1 | April 12 | 5233 |
| Wang | USA | New York | Mount Sinai Health System | Retrospective | March 7 | April 15 | 3273 |
| Cummings | USA | New York | New York-Presbyterian | Prospective | March 2 | April 1 | 257 |
| Palaiodimos | USA | New York | Montefiore Medical Center | Retrospective | March 9 | March 22 | 200 |
| Bode | USA | 10 states (not New York) | Multicenter | Retrospective | March 1 | April 6 | 570b |
aOnly the subset of patients who were hospitalized were included
bOnly the subset of patients who had been discharged or died were included
Fig. 2.
Risk of bias assessment based on the Quality in Prognosis Studies (QUIPS) tool
Table 2.
Baseline characteristics of patients per included study
| Study | Age | Female (n, %) | DM (n, %) | HTN (n, %) | HLD (n, %) | CAD (n, %) | HF (n, %) | CKD (n, %) | CVA (n, %) | Smoking (n, %) | COPD (n, %) | Malignancy (n, %) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Guan | 48.9 ± 16.3a | 674 (42.7) | 130 (8.2) | 269 (16.9) | NA | 59 (3.7) | NA | NA | 30 (1.9) | 111 (7.0) | 24 (1.5) | NA |
| Han | 60 (49–70)b | 132 (43.1) | 129 (42.2) | 119 (38.9) | NA | 25 (8.2) | NA | 4 (1.3) | 11 (3.6) | 5 (1.6) | 18 (5.9) | 18 (5.9) |
| Zeng | 67 (57–75)b | 38 (39.2) | 26 (26.8) | 47 (48.5) | NA | NA | NA | 8 (8.2) | NA | NA | 8 (8.2) | NA |
| Nikpouraghdam | 55.5 ± 15.2a | 1009 (34.0) | 113 (3.8) | 59 (1.9) | NA | 37(1.3) | NA | 18 (0.6) | NA | NA | 60 (2.0) | 17 (0.6) |
| Javanian | 60.1 ± 13.9a | 49 (49.0) | 37 (37.0) | 32 (32.0) | NA | NA | NA | 12 (12.0) | 3 (3.0) | NA | 12 (12.0) | 4 (4.0) |
| Rossi | 63.2c | 418 (38.9) | 175 (16.3) | 280 (26.0) | 85 (7.9) | 115 (10.6) | 96 (8.9) | 45 (4.2) | NA | NA | 91 (8.5) | 167 (15.5) |
| Borobia | 61 (46–78)b | 1152 (51.8) | 381 (17.1) | 920 (41.3) | NA | NA | NA | 174 (7.8) | NA | 157 (7.1) | 153 (6.9) | 385 (17.3) |
| Perez Guzman | 67 (41–93)b | 198 (38.0) | 138 (26.5) | 187 (36.0) | 82 (16.0) | 43 (8.2) | 21 (4.0) | 70 (13.4) | 34 (6.5) | NA | 20 (3.8) | 46 (8.8) |
| Tomlins | 75 (59–82)b | 35 (37.0) | 37/95 (38.9) | 35 (37.0) | NA | 21 (22.0) | 15 (16.0) | 22 (23.0) | 8 (8.4) | NA | 10 (11.0) | 20 (21.0) |
| Levy | 21–106d | 2176 (41.6) | 1414 (27.0) | 2474 (50.2) | NA | 454 (9.2) | 219 (4.4) | 326 (6.6) | NA | NA | NA | NA |
| Wang | 60 (46–71) vs. 75 (65–84)e | 1399 (42.7) | 768 (23.5) | 1082 (33.0) | NA | NA | NA | NA | NA | 116 (3.5) | NA | 233 (7.1) |
| Cummings | 62 (51–72)b | 87 (34.0) | 92 (35.8) | 162 (63.0) | NA | NA | NA | 37 (14.0) | NA | NA | 24 (9.0) | 18 (7.0) |
| Palaiodimos | 64 (50–73.5)b | 102 (51.0) | 79/200 (39.5) | 152 (76.0) | 92 (46.2) | 33 (16.5) | 34 (17.0) | 58 (29.0) | 22 (11.0) | 65 (32.5) | 28 (14.0) | 11 (5.5) |
| Bode | 65 (24–95) vs. 61 (18–101)f | 498 (44.4) | 184 (32.3) | NA | NA | NA | NA | NA | NA | NA | NA | NA |
Abbreviations: DM diabetes mellitus, HTN hypertension, HLD hyperlipidemia, CAD coronary artery disease, HF heart failure, CKD chronic kidney disease, CVA cerebrovascular accident, COPD chronic obstructive pulmonary, NA non-available
aMean ± SD
bMedian (IQR)
cMean
dRange
eMedian (IQR) in discharged vs. deceased
fMedian (range) in diabetics vs. non-diabetics
Fig. 3.
Overall analysis: diabetes vs. no diabetes for in-hospital mortality
Sensitivity and subgroup analyses
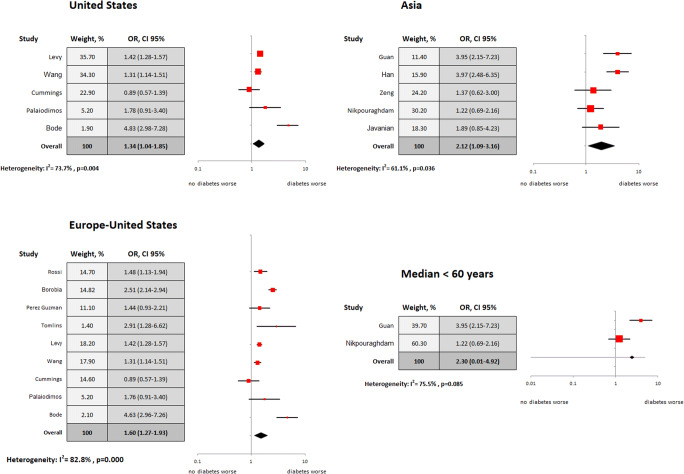
Sensitivity analyses were conducted for studies that were performed in the USA (N = 5), Asia (5), and Western countries (Europe-USA) (N = 9). Similarly, in the overall analysis, our sensitivity analysis for studies conducted in the USA revealed a greater risk of death among diabetic patients compared with the non-diabetes group (OR 1.34; 95% CI 1.04–1.85; I2 73.7%). We found a similar association for studies conducted in Asia (OR 2.12; 95% CI 1.09–3.16; I2 61.1%) and among studies conducted in the Western countries (USA or Europe) (OR 1.60; 95% CI 1.27–1.93; I2 82.8%; Fig. 4). Subgroup analysis of the studies that had a mean or median age less than 60 years (N = 2, both from Asia) did not show a significant difference in mortality between diabetics and non-diabetics (OR 2.3; 95% CI 0.01–4.92; I2 75.5%; Fig. 4) but were likely limited by the small sample given the wide range in confidence intervals.
Fig. 4.
Sensitivity and subgroup analyses based on the region of the study origin and the mean/median age of the study population: diabetes vs. no diabetes for in-hospital mortality
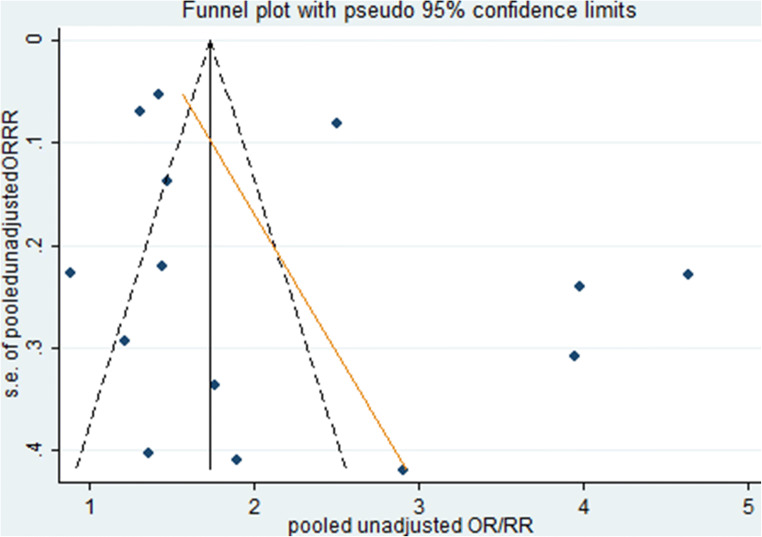
Publication bias assessment findings
Assessment for publication bias was performed in two different ways. Visual assessment of the funnel plot suggested possible publication bias given the asymmetry noted among smaller studies. However, Egger’s test was non-significant; thus, it was not suggestive of publication bias (p = 0.255) (Fig. 5).
Fig. 5.
Funnel plot for assessment of publication bias. Funnel plot is asymmetric among smaller studies suggesting possible publication bias. However, Egger’s test was non-significant, thus, it was not suggestive of publication bias (p = 0.255)
Meta-regression analysis
A study-level meta-regression analysis was performed for all the important covariates (age: p = 0.474, female sex: p = 0.766, hypertension: p = 0.524, coronary artery disease: p = 0.808, heart failure: p = 0.263, chronic kidney disease: p = 0.875, history of stroke: p = 0.252, smoking history: p = 0.639, COPD history: p = 0.620, and malignancy history: p = 0.329). No significant interactions were found between the covariates mentioned above and the outcome of mortality. The detailed meta-regression results can be found in Table 3.
Table 3.
Results of the meta-regression analysis
| Variables | Coefficient | Standard error | p value |
|---|---|---|---|
| Age | − 0.019 | 0.026 | 0.474 |
| Female | − 0.003 | 0.010 | 0.766 |
| HTN | − 0.005 | 0.007 | 0.524 |
| CAD | 0.594 | 0.361 | 0.808 |
| HF | 0.026 | 0.019 | 0.263 |
| CKD | − 0.003 | 0.018 | 0.875 |
| CVA | − 0.078 | 0.058 | 0.252 |
| Smoking | − 0.012 | 0.024 | 0.639 |
| COPD | − 0.022 | 0.043 | 0.620 |
| Malignancy | 0.025 | 0.024 | 0.329 |
Abbreviations: HTN hypertension, CAD coronary artery disease, HF heart failure, CKD chronic kidney disease, CVA cerebrovascular accident, COPD chronic obstructive pulmonary disease
Discussion
Our study was a systematic review and meta-analysis of observational studies looking at the association between diabetes and mortality in adult hospitalized patients with COVID-19. The findings of our study can be summarized as follows: (i) overall, death was 65% more likely to occur in diabetic inpatients compared with non-diabetic patients but was limited by significant heterogeneity; (ii) this association remained significant when the analysis focused on geographical regions of study origin with, once again, significant heterogeneity; and (iii) our meta-regression analysis did not show an association between how frequent the other significant comorbidities were across different studies and our results.
The findings of our meta-analysis are consistent with the results of several large observational cohorts. In one of the largest retrospective studies of hospitalized patients with COVID-19 conducted in New York, diabetic patients comprised 33.8% (1808/5700) of the total inpatient population [26], whereas the prevalence of diabetes in the general population in New York is approximately 10.5% [27]. An early cohort of 1099 patients with COVID-19 from China revealed that 17.8% of the entire cohort developed severe disease, while the respective rate in the diabetic subgroup was 34.6% [28]. In contrast, a large study also from New York, which included 4103 patients, showed that diabetes was not an independent risk factor for the development of critical illness from COVID-19, although a trend was noted (OR 1.14, 95% CI 0.83–1.58) [29]. Smaller cohorts included in this meta-analysis did not show an association of diabetes with in-hospital mortality, but these studies had relatively small sample sizes and were likely underpowered (19, 23, 24). Given the heterogeneity of the results across the literature, our meta-analysis sought to answer this significant question by utilizing a total sample of 18,506 patients.
Diabetes is associated with higher susceptibility to infectious diseases and higher infection-related mortality [30]. A retrospective matched control study from Canada of more than one million participants demonstrated that diabetics had a significantly higher risk of being hospitalized due to an infection, develop sepsis, and die regardless of the affected system or organ or whether the infection was viral or bacterial [31]. Similarly, a UK cohort of more than 100,000 diabetics and 200,000 control subjects revealed that diabetic patients had significantly higher rates of all types of infections with an almost double risk for hospitalization and death compared with non-diabetics [32]. Among others, diabetics had 40% higher rates of lower respiratory infections (101.1 vs. 73.3; per 1000 patients/year) [32]. In the 2009 H1N1 pandemic, it was noted that diabetes tripled the risk of hospitalization and quadrupled the risk of admission to intensive care units [33].
Reduced T lymphocyte response, decreased neutrophil function, impaired humoral immunity, increased adherence of microorganisms to diabetic cells, and increased virulence of some microorganisms in patients with hyperglycemia are some of the pathogenetic mechanisms that likely make diabetics more susceptible to infectious diseases [4, 34]. In addition, diabetes is a major cause of endothelial dysfunction [35]. The increasing evidence of endothelial involvement in severe COVID-19 [36, 37], which potentially contributes to COVID-19-associated coagulopathy [38], could raise the hypothesis that dysfunctional endothelium is more susceptible to further damage related to COVID-19.
The main strengths of our study are the strict methodology, robust analysis, and relatively large number of included studies and overall patient sample. Notably, three continents and most of the countries that had high COVID-19 incidence were represented. Sensitivity, subgroup, and meta-regression analyses were performed as needed.
The main limitation of our study is the lack of data on glycemic control prior to infection with COVID-19 or during hospitalization. Therefore, we could not estimate the associations of controlled and uncontrolled diabetes with in-hospital mortality and we recognize that the association could likely be stronger in patients with uncontrolled diabetes and weaker in patients with controlled diabetes. A patient-level meta-analysis would be needed to assess this very important parameter. Second, the estimated association is not adjusted for other important covariates. Unfortunately, only three of the included studies provided adjusted effect estimates with a total of only 977 patients. Pooling the adjusted estimates from these three studies did not show an independent association between diabetes and higher in-hospital mortality, likely because of low statistical power. However, a trend towards significance was observed (OR 1.29; 95% CI 0.87–1.71; I2 0.00%; Supplementary Figure 1). We tried to solve this methodological issue by performing a meta-regression analysis, which demonstrated that the different rates of the other major comorbidities across different studies did not have an impact on the results. Similarly, a patient-level meta-analysis would be the ideal way to adjust for other significant covariates. Third, our meta-analysis was limited by significant heterogeneity, which we tried to assess by using a random effects model, performing subgroups and sensitivity, and meta-regression analysis. Fourth, we followed the PRISMA guidelines instead of the MOOSE guidelines [39]. The latter would be more appropriate given the fact that only observational studies were included in this systematic review and meta-analysis.
In conclusion, the present systematic review and meta-analysis revealed that the likelihood of death seems to be higher in diabetic hospitalized patients with COVID-19 compared with non-diabetics. Although the heterogeneity was substantial, meta-regression analysis did not reveal any significant confounders. Further studies are needed to assess whether this association is independent or not as well as to investigate the role of optimal glycemic control prior to or during the disease. The findings of our study also highlight the importance of preventing and controlling diabetes and its complications to protect this vulnerable population from COVID-19 given the increased risk for adverse outcomes. In addition, attention should be paid to the importance of controlling hyperglycemia in diabetic patients diagnosed with COVID-19 given the possible higher risk for adverse outcomes. While we recognize the limitations, we hope that our study will compliment further research of the effect of diabetes in COVID-19.
Electronic supplementary material
Supplementary Figure. Analysis of the studies that provided adjusted effect estimates. In this meta-analysis the adjusted estimates were pooled: diabetes vs. no diabetes for in-hospital mortality (PNG 15 kb)
Supplementary Methods. The search algorithms that were used for each database. (DOCX 12 kb)
(DOCX 16 kb)
Data availability
Yes, upon request to the first author.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
All authors approved this manuscript.
Code availability
Yes, upon request to the first author
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhou B, Lu Y, Hajifathalian K, Bentham J, Di Cesare M, Danaei G, Bixby H, Cowan MJ, Ali MK, Taddei C, Lo WC. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–1530. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clin Pract. 2019;157:107843. doi: 10.1016/j.diabres.2019.107843. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (2020) National diabetes statistics report. US Department of Health and Human Services. https://www.cdc.gov/diabetes/data/statistics-report/index.html. Accessed 20 June 2020
- 4.Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: a review of pathogenesis. Indian J Endocrinol Metab. 2012;16(Suppl1):S27. doi: 10.4103/2230-8210.94253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hussain A, Bhowmik B, do Vale Moreira NC. COVID-19 and diabetes: knowledge in progress. Diabetes Res Clin Pract. 2020;162:108142. doi: 10.1016/j.diabres.2020.108142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maddaloni E, Buzzetti R (2020) Covid-19 and diabetes mellitus: unveiling the interaction of two pandemics. Diabetes Metab Res Rev:e33213321. 10.1002/dmrr.3321 [DOI] [PMC free article] [PubMed]
- 7.Angelidi AM, Belanger MJ, Mantzoros CS. COVID-19 and diabetes mellitus: what we know, how our patients should be treated now, and what should happen next. Metabolism. 2020;107:154245. doi: 10.1016/j.metabol.2020.154245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO (2020) Coronavirus disease (COVID-19) dashboard. https://covid19.who.int/. Accessed: August 10, 2020
- 9.Moher D, Liberati A, Tetzlaff J, the PRISMA group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 10.Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–286. doi: 10.7326/0003-4819-158-4-201302190-00009. [DOI] [PubMed] [Google Scholar]
- 11.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 12.Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, Liu XQ, Chen RC, Tang CL, Wang T, Ou CQ. Comorbidity and its impact on 1590 patients with Covid-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5):2000547. doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han M, Ma K, Wang X, Yan W, Wang H, You J, Wang Q, Chen H, Wang J, Chen L, Xu D (2020) Higher fasting plasma glucose reduced the survival rate of 306 hospitalized patients with COVID-19 in Wuhan. China SSRN. 10.2139/ssrn.3576809
- 14.Zeng X, Fan H, Lu D, Huang F, Meng X, Li Z, Tang M, Zhang J, Liu N, Liu Z, Zhao J (2020) Association between ABO blood groups and clinical outcome of coronavirus disease 2019: evidence from two cohorts. medRxiv:20063107. 10.1101/2020.04.15.20063107
- 15.Nikpouraghdam M, Farahani AJ, Alishiri G, Heydari S, Ebrahimnia M, Samadinia H, Sepandi M, Jafari NJ, Izadi M, Qazvini A, Dorostkar R. Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in IRAN: a single center study. J Clin Virol. 2020;127:104378. doi: 10.1016/j.jcv.2020.104378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Javanian M, Bayani M, Shokri M, Sadeghi-Haddad-Zavareh M, Babazadeh A, Yeganeh B, Mohseni S, Mehraein R, Sepidarkish M, Bijani A, Rostami A. Clinical and laboratory findings from patients with COVID-19 pneumonia in Babol North of Iran: a retrospective cohort study. Rom J Intern Med. 2020;58(3):161–167. doi: 10.2478/rjim-2020-0013. [DOI] [PubMed] [Google Scholar]
- 17.Rossi PG, Marino M, Formisano D, Venturelli F, Vicentini M, Grilli R, Reggio Emilia COVID-19 Working Group Characteristics and outcomes of a cohort of SARS-CoV-2 patients in the Province of Reggio Emilia, Italy. PLoS One. 2020;15(8):e0238281. doi: 10.1371/journal.pone.0238281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Borobia AM, Carcas AJ, Arnalich F, Alvarez-Sala R, Montserrat J, Quintana M, Figueira JC, Santos-Olmo RM, Garcia-Rodriguez J, Martin-Vega A, Ramirez E. A cohort of patients with COVID-19 in a major teaching hospital in Europe. J Clin Med. 2020;9(6):1733. doi: 10.3390/jcm9061733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perez Guzman PN, Daunt A, Mukherjee S, Crook P, Forlano R, Kont M, Lochen A, Vollmer M, Middleton P, Judge R, Harlow C (2020) Clinical characteristics and predictors of outcomes of hospitalized patients with COVID-19 in a multiethnic London NHS Trust: a retrospective cohort study. Clin Infect Dis ciaa1091. 10.1093/cid/ciaa1091 [DOI] [PMC free article] [PubMed]
- 20.Tomlins J, Hamilton F, Gunning S, Sheehy C. Clinical features of 95 sequential hospitalized patients with novel coronavirus 2019 disease (COVID-19), the first UK cohort. J Inf Secur. 2020;81(2):e59–e61. doi: 10.1016/j.jinf.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Levy TJ, Richardson S, Coppa K, Barnaby DP, McGinn T, Becker LB, Davidson KW, Hirsch JS, Zanos T (2020) Development and validation of a survival calculator for hospitalized patients with COVID-19. medRxiv. 10.1101/2020.04.22.20075416
- 22.Wang Z, Zheutlin AB, Kao YH, Ayers KL, Gross SJ, Kovatch P, Nirenberg S, Charney AW, Nadkarni GN, O'Reilly PF, Just AC (2020) Analysis of hospitalized COVID-19 patients in the Mount Sinai Health System using electronic medical records (EMR) reveals important prognostic factors for improved clinical outcomes. medRxiv. 10.1101/2020.04.28.20075788
- 23.Cummings MJ, Baldwin MR, Abrams D, Jacobson SD, Meyer BJ, Balough EM, Aaron JG, Claassen J, Rabbani LE, Hastie J, Hochman BR (2020) Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. medRxiv. 10.1101/2020.04.15.20067157 [DOI] [PMC free article] [PubMed]
- 24.Palaiodimos L, Kokkinidis DG, Li W, Karamanis D, Ognibene J, Arora S, Southern WN, Mantzoros CS. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism. 2020;108:154262. doi: 10.1016/j.metabol.2020.154262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bode B, Garrett V, Messler J, McFarland R, Crowe J, Booth R, Klonoff DC. Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States. J Diabetes Sci Technol. 2020;14(4):813–821. doi: 10.1177/1932296820924469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, Barnaby DP, Becker LB, Chelico JD, Cohen SL, Cookingham J, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Department of Health (2020) Diabetes and diabetes prevention. New York State. https://www.health.ny.gov/diseases/conditions/diabetes/. Accessed May 23, 2020
- 28.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DS, Du B. Clinical characteristics of coronavirus disease 2019 in China. NEJM. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Petrilli CM, Jones SA, Yang J, Rajagopalan H, O'Donnell LF, Chernyak Y, Tobin K, Cerfolio RJ, Francois F, Horwitz LI (2020) Factors associated with hospitalization and critical illness among 4,103 patients with COVID-19 disease in New York City. medRxiv. 10.1101/2020.04.08.20057794 [DOI] [PMC free article] [PubMed]
- 30.Knapp S. Diabetes and infection: is there a link? A mini-review. Gerontology. 2003;59(2):99–104. doi: 10.1159/000345107. [DOI] [PubMed] [Google Scholar]
- 31.Shah BR, Hux JE. Quantifying the risk of infectious diseases for people with diabetes. Diabetes Care. 2003;26(2):510–513. doi: 10.2337/diacare.26.2.510. [DOI] [PubMed] [Google Scholar]
- 32.Carey IM, Critchley JA, DeWilde S, Harris T, Hosking FJ, Cook DG. Risk of infection in type 1 and type 2 diabetes compared with the general population: a matched cohort study. Diabetes Care. 2018;41(3):513–521. doi: 10.2337/dc17-2131. [DOI] [PubMed] [Google Scholar]
- 33.Allard R, Leclerc P, Tremblay C, Tannenbaum TN. Diabetes and the severity of pandemic influenza A (H1N1) infection. Diabetes Care. 2010;33(7):1491–1493. doi: 10.2337/dc09-2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Geerlings SE, Hoepelman AI. Immune dysfunction in patients with diabetes mellitus (DM) FEMS Immunol Med Microbiol. 1999;26(3–4):259–265. doi: 10.1111/j.1574-695X.1999.tb01397.x. [DOI] [PubMed] [Google Scholar]
- 35.Avogaro A, Albiero M, Menegazzo L, de Kreutzenberg S, Fadini GP. Endothelial dysfunction in diabetes: the role of reparatory mechanisms. Diabetes Care. 2011;34(Supplement 2):S285–S290. doi: 10.2337/dc11-s239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H (2020) Endothelial cell infection and endotheliitis in COVID-19. Lancet 395(10234):1417–1418 [DOI] [PMC free article] [PubMed]
- 37.Escher R, Breakey N, Lämmle B (2020) Severe COVID-19 infection associated with endothelial activation. Thromb Res 190:62. 10.1016/j.thromres.2020.04.014 [DOI] [PMC free article] [PubMed]
- 38.Connors JM, Levy JH (2020) COVID-19 and its implications for thrombosis and anticoagulation. Blood 135(23):2033–2040 [DOI] [PMC free article] [PubMed]
- 39.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2020;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure. Analysis of the studies that provided adjusted effect estimates. In this meta-analysis the adjusted estimates were pooled: diabetes vs. no diabetes for in-hospital mortality (PNG 15 kb)
Supplementary Methods. The search algorithms that were used for each database. (DOCX 12 kb)
(DOCX 16 kb)
Data Availability Statement
Yes, upon request to the first author.