Summary
The new SARS-CoV-2/COVID-19 emergency has imposed new disinfection and sanitation measures of work environments also to beauty and health professional workers and in this context ozone shows growing interest. Ozone has proven to be highly effective in killing bacteria, fungi, and molds and inactivating viruses both on the surfaces and suspended in the air. Ozone is proven to be effective also for the inactivation of the SARS virus, while for the novel SARS-CoV-2 it is supposed that it be equally effective but specific studies are needed.
Keywords: Ozone, UV-light, Disinfection, Coronavirus, Work environment
Main
Following the health emergency regarding the new SARS-CoV-2/COVID-19 to limit its spread, the sanitization of environments, devices, and objects has become imperative, in addition to individual protection and prevention measures. This applies not only to the clinical, industrial and public sector but also to beauty and health professionals and their work environments, i.e. beauty centers (beauticians, hairdressers, make-up artists), gyms (personal trainers, slimming professionals), professional ambulatories or functional rehabilitation centers (physiotherapists, physio-aesthetic specialists and non-invasive aesthetic medicine operators).
Numerous disinfection and sanitization methods, including heating sterilization [1], ultraviolet germicidal irradiation (UVGI) [2], and chemical disinfectants [1, 3, 4], have been proposed for work environments and surfaces but also for all kinds of fomites [5], including furniture, work devices, non-disposable work tools, and clothing to prevent and eradicate the spread of the new coronavirus responsible of the SARS-CoV-2 related-disease. Among these, in recent months, there has been particular attention to devices that generate ozone for this purpose [6] and so it is useful to ask if ozone can also be effective on the novel SARS-CoV-2.
Ozone is a gas formed by molecules made up of 3 oxygen atoms (O3) and has the characteristic of being a powerful oxidizing agent. Thanks to this property it has proven to be highly effective in killing bacteria, fungi and molds [7, 8] and inactivating viruses [6, 9].
Ozone can, therefore, be used for the treatment of potentially contaminated surfaces, water, and ambient air thanks to its powerful germicidal effect on a wide spectrum of microorganisms, while it has been shown that on porous materials, such as textiles, it is less effective [10], unlike disinfection with UV lamps (UVGI) that are more effective on these materials [9](Fig. 1). Recently, it was reported that ozone treatment can be also a widely accessible and effective method for the disinfection of personal protective equipment (PPE) for both healthcare workers and patients for safe re-use in times of shortage [11].
Fig. 1.
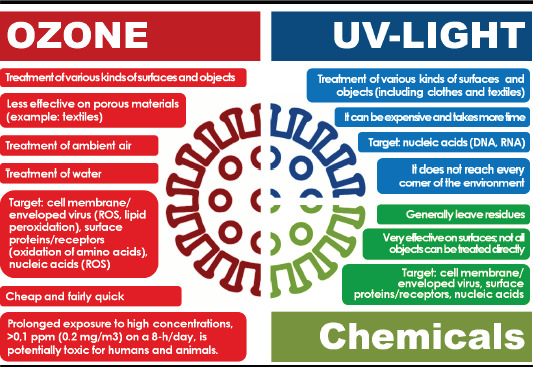
Disinfection and sanitization methods: differences between ozone, UV light and chemical disinfectants. The figure shows the main differences between ozone and UV light sanitization [1, 3, 4, 6, 10, 14-16].
Ozone created by various kinds of devices, such as ozone generators or electrostatic air purifiers, can reach every corner of the environment of a single room or a larger space, depending on the device, without leaving any poisonous residue. The effectiveness of ozone in treating microorganisms, especially bacteria and viruses is related to various factors, i.e. ozone concentration, the temperature of the environment, humidity of the environment and exposure time [14] (Fig. 2).
Fig. 2.
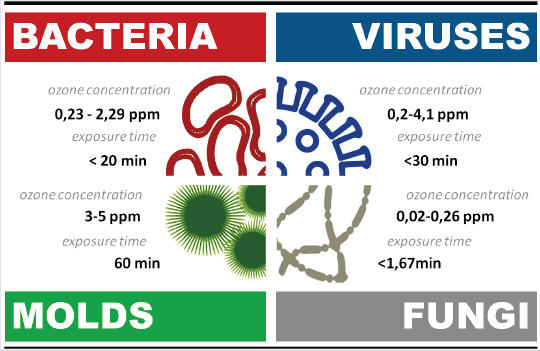
Effective ozone parameters on the microorganisms. The figure shows the ozone concentration (ppm) and time exposure (minutes) necessary to reduce the microbial load by 99% [7, 14, 17].
It was shown that after 30 seconds of in vitro direct exposure to ozone, 99 percent of the viruses are inactivated [13]. Although this evidence is of considerable importance, outside of the laboratory models, there are various parameters that influence the time required to obtain the same result. First of all, it was seen that the inactivation of 99% of viruses by ozonation requires its spread at concentrations higher than those necessary for the bacteria [9, 14]. A longer exposure time, about 30 minutes, is necessary for the treatment of the surfaces of the environment (surface viruses), while for any viral particles suspended in the air (airborne viruses) 8-10 minutes are enough to remove 99.9% of them [17]. Viruses in water are more susceptible to ozone inactivation and short contact time, about 1 min or little more, are sufficient to inactivate 99% of them [9, 18].
Virus inactivation is complicated by two factors. The first is the presence or not of an envelope: in fact, it seems that enveloped viruses are more sensitive to ozone than naked viruses [1, 19]. The second factor is that highly related viruses may exhibit different response kinetics to the same biocide due to the variation of structural or genomic components [16]. However, ozone has been shown to cause the inactivation of viruses by affecting various molecular targets.
Capsid surface proteins, as well as membrane receptors present on enveloped viruses, are the first targets of ozone because it reacts directly with amino acids and functional groups of proteins. This leads to various consequences both on the structure of the virus, which is compromised, and on its infectious capacity because the specific viral receptors used by the virus to bind to host cells and invade them are altered. Furthermore, ozone damages the membranes of the enveloped viruses through peroxidation of phospholipids and generating numerous reactive oxygen species (ROS) capable of damaging also other viral macromolecules [9, 14, 20, 21]. In addition, ozone can inactivate viruses by causing damage to their genetic material, both DNA and RNA [14, 22]. The main mechanisms by which ozone acts on viruses, therefore, are due to the direct oxidation of various molecules and, indirectly, with the generation of ROS.
Ozone was shown to be highly effective to inactivate the SARS virus, in fact, it shows an inactivation rate not lesser than 99% [12]. The novel SARS-CoV2 (2019), an enveloped virus like all other coronaviruses, shows 80% of genome sequence similarity to SARS-CoV (2002) and this suggests that ozone could be equally effective also on the novel coronavirus [12, 18].
In conclusion, although the existing scientific literature supports the effectiveness of ozone in the inactivation of viruses, there are very few studies about it on the SARS virus e not still a single study about its efficiency of inactivation on SARS-CoV-2. Therefore, in the absence of scientific literature, it is possible to assume that ozone is equally effective in inactivating SARS-CoV-2, however specific studies must be conducted to know also the ozone dose and effective exposure times.
Figures and tables
Acknowledgements
Funding sources: this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
ABBREVIATIONS
- COVID-19
coronavirus infectious disease 2019.
- SARS
severe acute respiratory syndrome.
- SARS-CoV
severe acute respiratory syndrome coronavirus (2002).
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2 (2019).
Footnotes
Conflict of interest statement
The author is employed in the Prestige company and has received a salary also for the research activities for the preparation of this paper
References
- [1].Castaño N, Cordts SC, Jalil MK, Zhang K, Koppaka S, Bick AD, Paul R, Tang SK. Fomite transmission and disinfection strategies for SARS-CoV-2 and related viruses. 2020. https://arxiv.org/abs/2005.11443 [DOI] [PMC free article] [PubMed]
- [2].Cutler TD, Zimmerman JJ. Ultraviolet irradiation and the mechanisms underlying its inactivation of infectious agents. Anim Health Res Rev 2011;12:15-23. https://doi.org/10.1017/S1466252311000016 10.1017/S1466252311000016 [DOI] [PubMed] [Google Scholar]
- [3].Tseng C-C, Li C-S. Inactivation of viruses on surfaces by ultraviolet germicidal irradiation. J Occup Environ Hyg 2007;4:400-5. https://doi.org/10.1080/15459620701329012 10.1080/15459620701329012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Rabenau HF, Kampf G, Cinatl J, Doerr HW. Efficacy of various disinfectants against SARS coronavirus. J Hosp Infect 2005;61:107-11. https://doi.org/10.1016/j.jhin.2004.12.023 10.1016/j.jhin.2004.12.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Vasickova P, Pavlik I, Verani M, Carducci A. Issues concerning survival of viruses on surfaces. Food Environ Virol 2010;2:24-34. https://doi.org/10.1007/s12560-010-9025-6 10.1007/s12560-010-9025-6 [DOI] [Google Scholar]
- [6].Hudson JB, Sharma M, Vimalanathan S. Development of a practical method for using ozone gas as a virus decontaminating agent. Ozone: Sci Eng 2009;31:216-23. https://doi.org/10.1080/01919510902747969 10.1080/01919510902747969 [DOI] [Google Scholar]
- [7].Najafi MBH, Khodaparast MHH. Efficacy of ozone to reduce microbial populations in date fruits. Food Control 2009;20:27-30. https://doi.org/10.1016/j.foodcont.2008.01.010 10.1016/j.foodcont.2008.01.010 [DOI] [Google Scholar]
- [8].Li C-S, Wang Y-C. Surface germicidal effects of ozone for microorganisms. AIHA Journal 2003;64:533-7. https://doi.org/10.1080/15428110308984851 10.1080/15428110308984851 [DOI] [PubMed] [Google Scholar]
- [9].Tseng C, Li C. Inactivation of surface viruses by gaseous ozone. J Environ Health 2008;70:56-63. [PubMed] [Google Scholar]
- [10].Menetrez MY, Foarde KK, Schwartz TD, Dean TR, Betancourt DA. An evaluation of the antimicrobial effects of gas-phase ozone. Ozone: Sci Eng 2009;31:316-25. https://doi.org/10.1080/01919510903043772 10.1080/01919510903043772 [DOI] [Google Scholar]
- [11].Blanchard EL, Lawrence JD, Noble JA, Xu M, Joo T, Ng NL, Schmidt BE, Santangelo PJ, Finn MG. Enveloped virus inactivation on personal protective equipment by exposure to ozone. medRxiv 2020. https://doi.org/10.1101/2020.05.23.20111435 10.1101/2020.05.23.20111435 [DOI] [Google Scholar]
- [12].Zhou M. Ozone: a powerful weapon to combat COVID-19 outbreak. 2020. http://www.china.org.cn/opinion/2020-02/26/content_75747237_4.htm (accessed 09.05.20).
- [13].Roy D, Wong PK, Engelbrecht RS, Chian ES. Mechanism of enteroviral inactivation by ozone. Appl Environ Microbiol 1981;41:718-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kim JG, Yousef AE, Dave S. Application of ozone for enhancing the microbiological safety and quality of foods: a review. J Food Prot 1999;62:1071-87. https://doi.org/10.4315/0362-028x-62.9.1071 10.4315/0362-028x-62.9.1071 [DOI] [PubMed] [Google Scholar]
- [15].Wickramatillake A, Kurukularatne C. SARS-CoV-2 human disinfection chambers: a critical analysis. Occup Med (Lond) 2020;kqaa078 https://doi.org/10.1093/occmed/kqaa078 10.1093/occmed/kqaa078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Wigginton KR, Pecson BM, Sigstam T, Bosshard F, Kohn T. Environ Sci Technol 2012;46:12069-78. https://doi.org/10.1021/es3029473 10.1021/es3029473 [DOI] [PubMed] [Google Scholar]
- [17].Kowalski WJ, Bahnfleth WP, Whittam TS. Bactericidal effects of high airborne ozone concentrations on Escherichia coli and Staphylococcus aureus. Ozone: Sci Eng 1998;20:205-21. https://doi.org/10.1080/01919519808547272 10.1080/01919519808547272 [DOI] [Google Scholar]
- [18].Shin GA, Sobsey MD. Reduction of norwalk virus, poliovirus 1, and bacteriophage ms2 by ozone disinfection of water. Appl Environ Microbiol 2003;69:3975-8. https://doi.org/10.1128/aem.69.7.3975-3978.2003 10.1128/aem.69.7.3975-3978.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Dennis R, Cashion A, Emanuel S, Hubbard D. Ozone gas: scientific justification and practical guidelines for improvised disinfection using consumer-grade ozone generators and plastic storage boxes. J Sci Med 2020;2(1). https://doi.org/10.37714/JOSAM.V2I1.35 10.37714/JOSAM.V2I1.35 [DOI] [Google Scholar]
- [20].Wigginton KR, Kohn T. Virus disinfection mechanisms: the role of virus composition, structure, and function. Curr Opin Virol 2012;2:84-9. https://doi.org/10.1016/j.coviro.2011.11.003 10.1016/j.coviro.2011.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Schentag JJ, Akers C, Campagna P, Chirayath P. Sars: clearing the air. Institute of Medicine (US) Forum on Microbial Threats; Knobler S, Mahmoud A, Lemon S, et al., editors. Learning from SARS: preparing for the next disease outbreak: workshop summary. Washington (DC): National Academies Press; 2004. https://www.ncbi.nlm.nih.gov/books/NBK92445 [PubMed] [Google Scholar]
- [22].Victorin K. Review of the genotoxicity of ozone. Mutat Res 1992;277:221-38. https://doi.org/10.1016/0165-1110(92)90045-B 10.1016/0165-1110(92)90045-B [DOI] [PubMed] [Google Scholar]


