Summary
The concept of Vaccine Hesitancy has begun to appear in the scientific landscape, referring to the reluctance of a growing proportion of people to accept the vaccination offer. A variety of factors were identified as being associated with vaccine hesitancy but there was no universal algorithm and currently there aren’t any established metrics to assess either the presence or impact of vaccine hesitancy. The aim of this study was to systematically review the published questionnaires evaluating parental vaccine hesitancy, to highlight the differences among these surveys and offer a general overview on this matter. This study offers a deeper perspective on the available questionnaires, helping future researches to identify the most suitable one according to their own aim and study setting.
Keywords: Vaccine, Hesitancy, Parents, Questionnaire, Review
Introduction
Vaccines have long been considered as one of the most important public health achievements of the past century and they have largely contributed to the decline in morbidity and mortality related to various infectious diseases [1]. Due to the effectiveness of vaccination programs, many people nowadays have limited or no experience with vaccine-preventable diseases (VPDs), thus parents increasingly assume that the risks associated with VPDs are minimal compared to potential health and safety risks of vaccinations themselves [2, 3]. The concept of Vaccine Hesitancy has subsequently begun to appear in the scientific landscape, referring to the reluctance of a growing proportion of people to accept the vaccination offer [4]. In fact, urban centres with large clusters of vaccine-hesitant individuals are particularly vulnerable to VPD outbreaks among exposed, unimmunized children, as observed with the measles outbreaks in the USA, Canada, and Europe [5-7]. 2014-2015 the Disneyland measles outbreak was a stark reminder of the direct influence of vaccine hesitancy and refusal [8].
The World Health Organization (WHO) defines vaccine hesitancy as the ‘‘delay in acceptance or refusal of vaccines despite availability of vaccination services. Vaccine hesitancy is complex and context specific, varying across time, place and for different vaccines. This phenomenon is influenced by factors such as complacency, convenience and confidence” [9]. The “3Cs” Model, that highlights these three categories, was first proposed in 2011 by the WHO EURO Vaccine Communications Working Group. In the “3 Cs” model, confidence is defined as trust in the effectiveness and safety of vaccines, and in the system that delivers them. This includes the reliability and competence of health services and health professionals and the motivations of policy-makers who decide on the needed vaccines. Vaccination complacency exists where the perceived risks of vaccine-preventable diseases are low and vaccination is not deemed a necessary preventive action. Vaccination convenience is a significant factor when physical availability, affordability, willingness-to-pay, geographical accessibility, ability to understand (language and health literacy) and appeal of immunization services affect the vaccination uptake [10]. There is a wide variety of determinants of vaccine hesitancy. In 2015, the WHO EURO Vaccine Communications Working Group developed the Vaccine Hesitancy Determinants Matrix which categorized determinants into the following groups: contextual, individual and group influences, and vaccine and vaccination-specific issues [11]. Contextual influences include historic, social, cultural, environmental, economic, political and institutional factors which might influence vaccine hesitant populations. The most common is conspiracy theories, which include a fear that vaccines are introduced to serve the economic and/or political interests of pharmaceutical companies [12, 13].
Individual and group influences include personal perceptions or beliefs about vaccines and influences from the social environment such as the belief that vaccines are unsafe. Parents are more afraid of the adverse events related to vaccines, which are thought to be more frequent and more serious than they really are, than of the complications that could arise from infectious diseases [14]. Moreover, some individuals do not perceive a medical need for certain vaccines. Vaccine Hesitancy is a global, complex and constantly changing phenomenon, currently representing one of the most significant problems of public health: in 2019 the World Health Organization (WHO) listed vaccine hesitancy in its top ten threats to global health [15]. To understand the impact that the various determinants have on vaccine hesitancy and what factors can influence vaccination decisions, numerous studies have been conducted over the years [16, 17].
Despite the growing number of articles on vaccine hesitancy published in recent years, there are some discrepancies among publications in terms of what exactly falls under the umbrella of “vaccine hesitancy”, a term that was only introduced by the SAGE Working Group in 2015. Therefore, in order to obtain as much information as possible on this issue, all studies investigating the determinants of vaccine hesitancy, without specifically using the term “vaccine hesitancy”, were also included in this review. A variety of factors were identified as being associated with vaccine hesitancy but there was no universal algorithm and currently there aren’t any established metrics to assess either the presence or impact of vaccine hesitancy. Study methods used to measure “vaccine hesitancy” are too heterogeneous and this makes it difficult to make inferences about the influence of specific factors on vaccine-hesitant behaviour. The aim of this study was to systematically review the published questionnaires evaluating parental vaccine hesitancy, to highlight the differences among these surveys and offer a general overview on this matter. Administration channel, sample size, type of vaccine being investigated, and the type of questions used in the questionnaire are some of the variables that can be considered, when designing a study to investigate vaccine hesitancy. The characteristics of each study, as well as the variables investigated, have been analyzed in order to enable future researchers to choose the most suitable tool for evaluating and measuring vaccine hesitancy over time and in different settings, according to their own needs and goals.
Methods
SEARCH STRATEGY
This is a systematic review conducted in accordance with the PRISMA Guidelines [18]. Several databases were consulted, including PubMed/Medline, Web of Science and The Cochrane Library. The latter was used to identify existing systematic reviews with a similar objective, in order to further screen the lists of references of potentially related articles that might have not been retrieved in the other databases. The systematic search was performed with no time filter, from inception to December 14th, 2017; however, a language limit was adopted, indeed only English and Italian articles were included in our review. The predefined search strategy that was used to identify potential relevant articles included four main aspects: parents or caregivers, vaccine hesitancy/acceptance, immunization and survey. Mesh and text words were combined with Boolean operators AND and OR. The full search strategy is: ((((((questionnair*[Title/Abstract] OR survey[Title/Abstract] OR “Surveys and Questionnaires”[Mesh])) AND (vaccin*[Title/Abstract] OR immuniz*[Title/Abstract] OR immunis*[Title/Abstract] OR shot*[Title/Abstract] OR jab*[Title/Abstract] OR “Vaccines”[Mesh] OR “Immunization”[Mesh] OR “Vaccination”[Mesh])) AND (hesitanc*[Title/Abstract] OR doubt*[Title/Abstract] OR concern*[Title/Abstract] OR criticis*[Title/Abstract] OR rumo*r[Title/Abstract] OR sceptic*[Title/Abstract] OR fear*[Title/Abstract] OR refus*[Title/Abstract] OR reject*[Title/Abstract] OR delay[Title/Abstract] OR accept*[Title/Abstract] OR consen*[Title/Abstract] OR intent*[Title/Abstract] OR confidence[Title/Abstract] OR adherence[Title/Abstract] OR complian*[Title/Abstract] OR uptake[Title/Abstract] OR engagement[Title/Abstract] OR *trust[Title/Abstract] OR a*titude[Title/Abstract] OR perception*[Title/Abstract] OR opinion*[Title/Abstract] OR belief*[Title/Abstract] OR behavi*r[Title/Abstract] OR choice*[Title/Abstract] OR practic*[Title/Abstract] OR barrier*[Title/Abstract] OR facilitator*[Title/Abstract] OR “Health Knowledge, Attitudes, Practice”[Mesh] OR “Vaccination Refusal”[Mesh] OR “Trust”[Mesh] OR “Behavior”[Mesh] OR “Patient Acceptance of Health Care”[Mesh]))) AND (parent*[Title/Abstract] OR caregiver*[Title/Abstract] OR guardian*[Title/Abstract] OR tutor*[Title/Abstract] OR mother*[Title/Abstract] OR father*[Title/Abstract] OR “legally acceptable representative”[Title/Abstract] OR “Parents”[Mesh])). In order to include all publications related to the topic, the list of references was manually screened for all relevant papers. Endnote was used as a software to manage all the retrieved references.
INCLUSION CRITERIA
Studies that fulfilled the inclusion criteria were considered in this review. Papers aimed at investigating parents/caregivers vaccine hesitancy through a survey/questionnaire were considered eligible, regardless of the attitudes and behaviours of the interviewed subjects. As a matter of fact, vaccine hesitancy is complex and driven by a wide variety of factors, as explained by the 3C model developed by the SAGE Working Group. Therefore, knowing the determinants of Vaccine Hesitancy in specific subgroups of parents (such as those who do not trust or have lost confidence in vaccinations) is extremely important in order to develop the right strategies to address it. In addition, including studies selecting the study population according to a negative/positive attitude/behaviour towards vaccination might be helpful for future researchers interested in studying Vaccine Hesitancy in a specific subgroup of parents. Because vaccine hesitancy is a complex phenomenon, strictly depending on several aspects that are country-specific, and because the introduction of vaccine hesitancy as a term in the scientific community is relatively new, we also included studies evaluating public trust/distrust, perceptions, concerns, confidence, attitudes, beliefs about vaccines and vaccination programs. Moreover, we included all types of available vaccines. Furthermore, we only assessed original articles, while other types of publications were not included in the analysis. Lastly, due to the aim of the research, only observational studies were considered: along with cross-sectional studies, we included cohort studies and case-control studies. The last two types of studies are particularly helpful in order to obtain as much information as possible and to have a broader overview of this phenomenon: as a matter of fact, they allowed us to include studies where questionnaires or surveys were used to investigate vaccine hesitancy among parents.
EXCLUSION CRITERIA
Studies were excluded from this review when they investigated vaccine hesitancy in target populations different from parents/caregivers/guardians, for instance physicians, educators, or directly the adolescents. Papers written in languages other than English and Italian were excluded, as well as not original articles (reviews, letters to editor, conference papers, editorials). Additionally, surveys aimed at assessing aspects different than vaccine hesitancy were not included. Lastly, articles were excluded if the vaccines examined were not for humans or were not commercially available yet (such as the HIV vaccine), or if the publications were on vaccine development.
DATA EXTRACTION
Eight couples of reviewers (VG and CA, MN and GV, SP and FD, OG and IB, EA and SDN, OES and LK, OG and AC, FDG and LG), independently performed the screening of titles and abstracts, followed by data extraction of the included articles. Disagreement was solved through a discussion between the authors, if disagreement persisted a third author was consulted (PC). Full-texts were downloaded and consulted only for the included articles. The extracted data were reported in a predefined, ad hoc spreadsheet elaborated in Excel. For each included article, the following items were evaluated: first author’s name and year of publication, when and where the study was conducted, study design and study aim, population characteristics and sample size, types of survey and administration, if the questionnaire was previously validated and if it was attached to the manuscript, number and type of questions, type of vaccine analysed, immunization behaviour and beliefs about vaccines.
DATA CODING
The included articles were coded by study period, country, language, study type and study aim, population characteristics, way of administration, number of items and items categories in the questionnaire, types of vaccine, immunization behaviour, beliefs about vaccine safety/efficacy. Regarding the latter, beliefs were coded as follows: i) no assessment of perceived safety/efficacy vaccines; ii) the assessment was performed and most of the respondents believe vaccinations to be safe/effective; iii) the assessment was performed and most of the respondents do not believe vaccinations to be safe/effective; iv) the assessment was performed but data were not available); v) the assessment was performed, but only qualitative and descriptive data were available (numerical data not available). As for the immunization behaviour, it was classified as follows: i) “acceptance”, if the whole population consisted of people receiving the vaccination; ii) “refusal”, if the whole population consisted of parents refusing the vaccination; iii) “hesitancy/scepticism/doubt”, if the population consisted of both parents accepting the vaccine and parents refusing it; iv) if no information was available, it was considered as missing data.
Results
We identified 5,139 records by running the pre-defined search strategies on the three selected databases (Medline, Web of Science, The Cochrane Library), and 8 additional records were retrieved from the manual searching of reference lists and citation chains of included papers. After removing duplicates, 3,500 papers were assessed for eligibility by title and abstract, and 2,481 papers were removed. After full text screening selection, 334 studies were included in the descriptive analysis and synthesis [3, 16, 19-350]. Figure 1 shows the selection flow. The main results of our systematic review are shown in Table I.
Fig. 1.
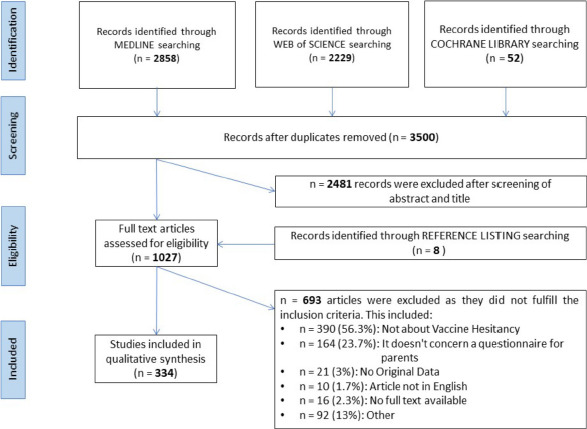
Flow chart of selection process.
Tab. I.
Main characteristics of the included studies.
| Author, year | Study period | Country | Study design | Administration channel | Sample size | Type of vaccine | Type of questions | Validation | Immunization behaviour |
|---|---|---|---|---|---|---|---|---|---|
| Adler A, 2007 | 2007 | Israel | Cross-sectional | Paper-based | 1,474 | Varicella | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Adorador A, 2011 | 2011 | USA | Cross-sectional | Paper-based | 108 | Dtp | Closed | Not | Hesitancy/scepticism/doubt |
| Aharony N, 2017 | 2017 | Israel | Cross-sectional | On-line | 200 | Child vaccines | Likert scale | With statistical methods | Refusal |
| Akis S, 2011 | 2011 | Turkey | Cross-sectional | Paper-based | 611 | Flu | Closed | Not | Acceptance |
| Akmatov MK, 2009 | 2009 | Kyrgyzstan | Cross-sectional | Paper-based | 934 | Child vaccines | Closed | Not | Acceptance |
| Alberts CJ, 2017 | 2017 | Netherlands | Cross-sectional | 1,309 | Hpv | Closed | Statistical methods not reported | Acceptance | |
| Alfredsson R, 2004 | 2004 | Sweden | Cross-sectional | Paper-based | 300 | Mmr | Closed | With statistical methods | Acceptance |
| Allen JD, 2010 | 2010 | USA | Cross-sectional | On-line | 476 | Hpv | Closed | Not | Acceptance |
| Allison MA, 2010 | 2010 | USA | Cross-sectional | Paper-based | 259 | Flu | Likert scale | With statistical methods | Hesitancy/scepticism/doubt |
| Allred NJ, 2005 | 2005 | USA | Cross-sectional | 7,810 | Dt | Closed | With statistical methods | Acceptance | |
| Alshammari TM, 2018 | 2018 | Saudi Arabia | Cross-sectional | Paper-based | 467 | Child vaccines | Closed | Statistical methods not reported | Acceptance |
| Ambe JP, 2001 | 2001 | Nigeria | Cross-sectional | Paper-based | 500 | Measles | Closed | Statistical methods not reported | Refusal |
| Aharon AA, 2017 | 2017 | Israel | Cross-sectional | Paper-based | 731 | Hbv/dtp/mmr | Likert scale | Not | Refusal |
| Arrossi S, 2012 | 2012 | Argentina | Cross-sectional | Paper-based | 1,200 | Hpv | Closed | With statistical methods | Acceptance |
| Azizi FSM, 2017 | 2017 | Malesya | Cross-sectional | Paper-based | 545 | Child vaccines | Closed | With statistical methods | Hesitancy/scepticism/doubt |
| Baglioni A, 2014 | 2014 | Italy | Cross-sectional | Paper-based | 648 | Hpv | Closed | With statistical methods | Acceptance |
| Bakhache P, 2013 | 2013 | Multinational | Cross-sectional | On-line | 2,460 | Menb | Closed | Statistical methods not reported | Acceptance |
| Baldwin AS, 2013 | 2008-2010 | USA | Cross-sectional | Paper-based | 256 | Hpv | Likert scale | With statistical methods | Acceptance |
| Bardenheier B, 2003 | 2000 | USA | Cross-sectional | Paper-based | 648 | Hav | Closed | Not | Acceptance |
| Bardenheier B, 2004 | 2001 | USA | Case-control | Paper-based | 3,586 | Mmr/dtp/hbv | Likert scale | Not | Acceptance |
| Bardenheier BH, 2004 | 1997-1998 | USA | Cross-sectional | Paper-based | 3,552 | Dtp/hib/hbv/polio | Closed | Not | Hesitancy/scepticism/doubt |
| Barnack JL, 2010 | 2006 | USA | Cross-sectional | 200 | Hpv | Likert scale | Not | Acceptance | |
| Barnack-Tavlaris JL, 2016 | 2009 | USA | Cross-sectional | Telephone | 4,666 | Hpv | Closed | Not | Acceptance |
| Bazzano A, 2012 | 2007 | USA | Cross-sectional | Telephone | 197 | Child vaccines | Closed | With statistical methods | Hesitancy/scepticism/doubt |
| Bedford H, 2007 | 2004 | UK | Cross-sectional | Paper-based | 859 | New vaccines | Likert scale | Not | Acceptance |
| Beel ER, 2013 | 2010-2012 | USA | Cross-sectional | Paper-based | 511 | Child vaccines | Closed | With statistical methods | Acceptance |
| Ben Natan M, 2011 | 2008 | Israel | Cross-sectional | Paper-based | 103 | Hpv | Likert scale | With statistical methods | Hesitancy/scepticism/doubt |
| Ben Natan M, 2016 | 2015 | Israel | Cross-sectional | Paper-based | 200 | Flu | Likert scale | With statistical methods | Acceptance |
| Ben Natan M, 2017 | 2016 | Israel | Cross-sectional | Paper-based | 200 | Hpv | Likert scale | With statistical methods | Acceptance |
| Berenson AB, 2014 | 2011-2013 | USA | Cross-sectional | Paper-based | 1,256 | Hpv | Closed | With statistical methods | Acceptance |
| Bettinger JA, 2016 | 2011 | Canada | Cross-sectional | 34 | Flu | Closed | Not | Acceptance | |
| Bham SQ, 2016 | 2015 | Pakistan | Cross-sectional | Paper-based | 210 | Polio | Closed | Not | Acceptance |
| Bianco A, 2014 | 2014 | Italy | Cross-sectional | Paper-based | 566 | Hpv | Likert scale | Not | Acceptance |
| Bigham M, 2006 | 2002-2003 | Canada | Cross-sectional | Telephone | 487 | Hbv | Likert scale | With statistical methods | Hesitancy/scepticism/doubt |
| Alder S, 2015 | 2012 | Argentina | Cross-sectional | Paper-based | 180 | Hpv | Closed | With statistical methods | Acceptance |
| Basu P, 2011 | 2008 | India | Cross-sectional | Paper-based | 522 | Hpv | Closed | Statistical methods not reported | Acceptance |
| Blair A, 1997 | 1997 | Australia | Cross-sectional | Paper-based | 245 | Child vaccines | Open field | Not | Acceptance |
| Blyth CC, 2014 | 2008–2012 | Australia | Cross-sectional | Paper-based | 2,576 | Dtp/hib/hbv | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Bodson J, 2016 | 2013 | USA | Cross-sectional | Paper-based | 119 | Hpv | Closed | With statistical methods | Hesitancy/scepticism/doubt |
| Bonanni P, 2001 | 2001 | Italy | Cross-sectional | Paper-based | 300 | Child vaccines | Closed | Not | Acceptance |
| Borena W, 2016 | 2015 | Austria | Cross-sectional | 439 | Hpv | Closed | Not | Hesitancy/scepticism/doubt | |
| Borras E, 2009 | 2003-2004 | Spain | Cross-sectional | Telephone | 630 | Child vaccines | Closed | Not | Hesitancy/scepticism/doubt |
| Brabin L, 2006 | 2005 | UK | Cross-sectional | 317 | Hpv | Mixed | With statistical methods | Hesitancy/scepticism/doubt | |
| Brambleby P, 1989 | 1988 | UK | Cross-sectional | 977 | Mmr | Mixed | Statistical methods not reported | Refusal | |
| Breitkopf CR, 2009 | 2007 | Vietnam | Cross-sectional | Paper-based | 139 | Hpv | Closed | Not | Hesitancy/scepticism/doubt |
| Brieger D, 2017 | N.A. | Australia | Cross-sectional | Paper-based | 201 | Mmr | Mixed | Not | Hesitancy/scepticism/doubt |
| Brown B, 2017 | 2015-2016 | USA | Cross-sectional | Paper-based | 200 | Hpv | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Brown KF, 2011 | 2009 | UK | Cross-sectional | 535 | Mmr | Mixed | Statistical methods not reported | Hesitancy/scepticism/doubt | |
| Brunson EK, 2013 | 2010 | USA | Cross-sectional | On-line | 196 | Child vaccines | Mixed | With statistical methods | Hesitancy/scepticism/doubt |
| Bults M, 2011 | 2009-2010 | Netherlands | Cross-sectional | Face to face/mail | 1900 | Flu | Open field | With statistical methods | Refusal |
| Burdette AM, 2014 | 2014 | USA | Cross-sectional | Telephone | 20,000 | Hpv | Closed | With statistical methods | Refusal |
| Busse JW, 2011 | 2010 | Canada | Cross-sectional | Paper-based | 95 | Child vaccines | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Buyuktiryaki B, 2014 | 2010 | Turkey | Cross-sectional | Paper-based | 625 | Flu | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Cacciatore MA, 2016 | 2014-2015 | USA | Cross-sectional | On-line | 2,000 | Measles | Mixed | Not | Hesitancy/scepticism/doubt |
| Campbell H, 2017 | 2015 | UK | Cross-sectional | Face to face | 1,792 | Child vaccines | Mixed | Not | Hesitancy/scepticism/doubt |
| Carlos RC, 2011 | N.A. | USA | Cross-sectional | 937 | Hpv | Mixed | Not | Hesitancy/scepticism/doubt | |
| Casiday R, 2006 | 2004 | UK | Cross-sectional | 996 | Mmr | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt | |
| Cassell JA, 2006 | 2004 | Uk | Cross-sectional | 452 | Mmr | Mixed | Statistical methods not reported | Hesitancy/scepticism/doubt | |
| Cataldi JR, 2016 | 2015 | USA | Cross-sectional | On-line | 343 | Mmr | Mixed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Chan JY, 2014 | 2012 | Hong Kong | Cross-sectional | Paper-based | 1,285 | Varicella | Mixed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Chaparro RM, 2016 | 2012 | Argentina | Cross-sectional | Paper-based | 77 | Hpv | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Chau JPC, 2017 | 2013 | Hong Kong | Cross-sectional | Paper-based | 623 | Flu | Likert scale | With statistical methods | Hesitancy/scepticism/doubt |
| Chen CH, 2015 | 2011 | Taiwan | Cross-sectional | 1,300 | Flu | Likert scale | With statistical methods | Hesitancy/scepticism/doubt | |
| Chen MF, 2011 | 2009 | Taiwan | Cross-sectional | Paper-based | 2,778 | Flu | Mixed | With statistical methods | Hesitancy/scepticism/doubt |
| Cheruvu VK, 2017 | 2017 | USA | Cross-sectional | Telephone | 21,467 | Hpv | Closed | Not | Refusal |
| Chung YM, 2017 | 2012-2014 | USA | Cross-sectional | On-line | 5,121 | Child vaccines | Mixed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Cipriano JJ, 2018 | 2016 | USA | Cross-sectional | On-line | 75 | Hpv | Mixed | Not | Acceptance |
| Clark SJ, 2016 | 2012 | USA | Cross-sectional | On-line | 1,799 | Hpv | Mixed | With statistical methods | Acceptance |
| Clark SJ, 2016 | 2012 | USA | Cross-sectional | On-line | 1,799 | Hpv | Mixed | Not | Hesitancy/scepticism/doubt |
| Clark SJ, 2016 | 2013 | USA | Cross-sectional | On-line | 1,799 | Hpv | Mixed | Not | Hesitancy/scepticism/doubt |
| Cockcroft A, 2014 | 2011 | Nigeria | Cross-sectional | Paper-based | 5,257 | Measles | Closed | Not | Acceptance |
| Colon-Lopez V, 2016 | 2013 | Puerto Rico | Cross-sectional | Paper-based | 200 | Hpv | Mixed | Not | Acceptance |
| Colon-Lopez V, 2015 | 2013 | Puerto Rico | Cross-sectional | Paper-based | 200 | Hpv | Mixed | Not | Acceptance |
| Coniglio MA,2011 | 2008 | Italy | Cross-sectional | Paper-based | 1,500 | Child vaccines | Closed | Not | Hesitancy/scepticism/doubt |
| Constantine NA, 2007 | 2006 | USA | Cross-sectional | Telephone | 802 | Hpv | Mixed | Not | Acceptance |
| Cooper Robbins SC, 2011 | 2007 | Australia | Cross-sectional | Paper-based | 169 | Flu | Mixed | Not | Acceptance |
| Costa-Pinto JC, 2017 | 2014-2015 | Australia | Cross-sectional | On-line | 612 | Child vaccines | Mixed | Not | Acceptance |
| Coyne-Beasley T, 2013 | 2008 | USA | Cross-sectional | Telephone | 1281 | Mcv | Mixed | Not | Acceptance |
| Cuninghame CJ, 1994 | 1991-1992 | UK | Cross-sectional | Face to face/telephone/mail | 93 | Child vaccines | Mixed | Not | Acceptance |
| Cunningham-Erves J, 2016 | 2012-2013 | USA | Cross-sectional | Paper-based | 242 | Hpv | Likert scale | Not | Acceptance |
| Dahlstrom LA, 2010 | 2007 | Sweden | Cross-sectional | Web /paper based | 13,946 | Hpv | N.A. | With statistical methods | Acceptance |
| Daley MF, 2007 | 2003 | USA | Cross-sectional | Telephone | 472 | Flu | Mixed | Not | Acceptance |
| Danchin MH, 2017 | 2015-2016 | Australia | Cross-sectional | Questionnaire (ipad), follow-up phone surveys | 975 | Child vaccines | Mixed | Not | Acceptance |
| Danis K, 2010 | 2004–2005 | Greece | Cross-sectional | Paper-based | 3,434 | Child vaccines | Mixed | Not | Acceptance |
| Dannetun E, 2007 | 2005 | Sweden | Cross-sectional | Paper-based and online | 1,229 | Hbv | Mixed | Statistical methods not reported | Acceptance |
| Dannetun E, 2005 | 2003 | Sweden | Cross-sectional | Paper-based | 173 | Mmr | Mixed | Not | Refusal |
| Danova J, 2015 | 2013-2014 | Repubblica Ceca | Cross-sectional | Paper-based | 480 | Child vaccines | Closed | Not | Refusal |
| Darden PM, 2013 | 2008–2010 | USA | Cross-sectional | Telephone | Dtp/mcv/hpv | N.A. | Not | Refusal | |
| Davis K, 2004 | 2003 | USA | Cross-sectional | Paper-based | 575 | Hpv | Mixed | Not | Acceptance |
| Dawar M, 2002 | 1999 | Canada | Cross-sectional | Telephone | 191 | Hbv/dtp/hib | Mixed | Not | Acceptance |
| de Courval FP, 2003 | 2000 | Canada | Cross-sectional | Telephone | 663 | Varicella | Mixed | Not | Refusal |
| de Visser R, 2008 | 2008 | UK | Cross-sectional | Paper-based | 353 | Hpv | Likert scale | Not | Acceptance |
| Dempsey AF, 2011 | N.A. | USA | Cross-sectional | 830 | Hpv | Mixed | Not | Acceptance | |
| Dempsey AF, 2015 | 2012-2013 | USA | Cross-sectional | On-line | 54 | Hpv | Mixed | Not | Acceptance |
| Dempsey AF, 2006 | 2009 | USA | Cross-sectional | On-line | 1,178 | Hpv | Likert scale | Not | Acceptance |
| DiAnna Kinder F, 2017 | N.A. | USA | Cross-sectional | Paper-based | 72 | Hpv | Mixed | Not | Refusal |
| Dinh TA, 2007 | 2005 | Vietnam | Cross-sectional | Paper-based | 181 | Hpv | Likert scale | Statistical methods not reported | Acceptance |
| Dorell C, 2014 | 2010 | USA | Cross-sectional | Telephone | 4103 | Hpv | Closed | Not | Hesitancy/scepticism/doubt |
| Dorell C, 2013 | 2010-2011 | USA | Cross-sectional | Telephone | 8,652 | Hpv/dtp/mcv | Closed | Not | Hesitancy/scepticism/doubt |
| Dorell C, 2011 | 2009-2010 | USA | Cross-sectional | Telephone | 20,066 | Hpv/mcv/dtp | Closed | Not | Hesitancy/scepticism/doubt |
| Dube E, 2012 | 2008-2009 | Canada | Cohort | Paper-based | 413 | Rotavirus | Mixed | Not | Acceptance |
| Dube E, 2015 | 2014 | Canada | Cross-sectional | Telephone | 703 | Menb | Likert scale | Statistical methods not reported | Acceptance |
| Dube E, 2017 | 2015 | Canada | Cross-sectional | On-line | 20,13 | Child vaccines | Mixed | Not | Acceptance |
| Dube E, 2016 | 2014 | Canada | Cross-sectional | Telephone | 589 | Child vaccines | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Ezat SW, 2013 | 2012 | Malesya | Cross-sectional | Not reported | 155 | Hpv | N.A. | Not | Acceptance |
| Ezeanochie MC, 2014 | 2009 | Nigeria | Cross-sectional | Paper-based | 201 | Hpv | Closed | Statistical methods not reported | Acceptance |
| Ezenwa BN, 2013 | 2012 | Nigeria | Cross-sectional | Paper-based | 290 | Hpv | N.A. | Not | Acceptance |
| Farias CC, 2016 | 2015 | Brazil | Cross-sectional | Paper-based | 797 | Hpv | Mixed | Not | Acceptance |
| Flood EM, 2010 | 2009 | USA | Cross-sectional | On-line | 500 | Flu | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Flynn M, 2004 | 1999-2000 | UK | Cohort | Paper-based | 511 | Mmr | Likert scale | Not | Hesitancy/scepticism/doubt |
| Freed GL, 2010 | 2009 | USA | Cross-sectional | On-line | 1,552 | Mmr/varicella/mcv/hpv | N.A. | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Freeman VA, 1999 | 1995 | USA | Cross-sectional | 247 | Varicella | Closed | Not | Hesitancy/scepticism/doubt | |
| Frew PM, 2016 | 2012-2014 | USA | Cross-sectional | On-line | 5,121 | Child vaccines | Closed | Not | Acceptance |
| Frew PM, 2011 | 2009 | USA | Cross-sectional | Not reported | 223 | Flu | Likert scale | Not | Refusal |
| Fry AM, 2001 | 1999-2000 | USA | Case-control | Paper-based | 66 | Hib | Open field | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Fuchs EL, 2016 | 2011-2013 | USA | Cross-sectional | Not reported | 350 | Hpv | Likert scale | Not | Hesitancy/scepticism/doubt |
| Garcia DA, 2014 | 2000 | Colombia | Cross-sectional | Paper-based | 4,802 | Child vaccines | Mixed | Not | Hesitancy/scepticism/doubt |
| Gargano LM, 2013 | 2011 | USA | Cross-sectional | Telephone | 114 | Flu/dtp/mcv/hpv | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Gaudino JA, 2012 | 2004-2005 | USA | Cross-sectional | On-line | 1,588 | Child vaccines | Likert scale | Not | Hesitancy/scepticism/doubt |
| Gefenaite G, 2012 | 2009 | Netherlands | Case-control | 469 | Hpv | Closed | Not | Hesitancy/scepticism/doubt | |
| Gellatly J, 2005 | 2003-2004 | UK | Cross-sectional | Paper-based | 110 | Mmr | Likert scale | Not | Hesitancy/scepticism/doubt |
| Gellin BG, 2000 | 1999 | USA | Cross-sectional | Telephone | 1,600 | Child vaccines | Likert scale | Not | Acceptance |
| Gentile A, 2015 | 2013 | Argentina | Cross-sectional | Not reported | 1,350 | Flu | Likert scale | Not | Hesitancy/scepticism/doubt |
| Gerend MA, 2009 | 2008 | USA | Cross-sectional | Paper-based | 82 | Hpv | Closed | Not | Acceptance |
| Gesser-Edelsburg A, 2016 | 2013 | Israel | Cross-sectional | On-line | 197 | Polio | Open field | Not | Refusal |
| Giambi C, 2014 | 2012 | Italy | Cross-sectional | 1,738 | Hpv | Mixed | Not | Refusal | |
| Gilbert NL, 2016 | 2013 | Canada | Cross-sectional | Telephone | 5,720 | Hpv | Likert scale | Not | Hesitancy/scepticism/doubt |
| Gilkey MB, 2017 | 2014-2015 | USA | Cross-sectional | On-line | 1,484 | Hpv | Closed | Not | Hesitancy/scepticism/doubt |
| Glanz JM, 2013 | 2009-2011 | USA | Cross-sectional | 854 | Child vaccines | Closed | Not | Hesitancy/scepticism/doubt | |
| Glenn BA, 2015 | 2009 | USA | Cross-sectional | Telephone | 444 | Hpv | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Gomez Y, 2012 | 2010 | USA | Cross-sectional | Paper-based | 773 | Flu | N.A. | Not | Hesitancy/scepticism/doubt |
| Gottlieb SL, 2009 | 2007 | USA | Cross-sectional | Telephone | 889 | Hpv | Mixed | Not | Hesitancy/scepticism/doubt |
| Gowda C, 2013 | 2011 | USA | Cross-sectional | On-line | 79 | Mmr | Likert scale | Not | Hesitancy/scepticism/doubt |
| Grabiel M, 2013 | 2012 | USA | Cross-sectional | Paper-based | 129 | Hpv | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Grandahl M, 2014 | 2012 | Sweden | Cross-sectional | Face to face | 25 | Hpv | Open field | Statistical methods not reported | Refusal |
| Grandahl M, 2017 | 2012 | Sweden | Cross-sectional | Paper-based | 200 | Hpv | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Greenberg J, 2017 | 2015 | Canada | Cross-sectional | On-line | 1,121 | Mmr | Likert scale | Statistical methods not reported | Acceptance |
| Greenfield LS, 2015 | 2012 | USA | Cross-sectional | Face to face | 157 | Dtp/mcv/hpv | Mixed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Griebeler M, 2012 | 2010 | USA | Cross-sectional | Paper-based | 102 | Hpv | Likert scale | Statistical methods not reported | Acceptance |
| Guerry SL, 2011 | 2007-2008 | USA | Cross-sectional | Telephone | 509 | Hpv | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Gundogdu Z, 2011 | 2009-2010 | Turkey | Cross-sectional | Paper-based | 300 | Varicella | Likert scale | With statistical methods | Acceptance |
| Gunduz S, 2014 | 2011-2012 | Turkey | Cross-sectional | Paper-based | 285 | Flu | Mixed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Gupta R, 2013 | 2009-2010 | USA | Cross-sectional | Paper-based and online | 381 | Flu | Closed | Not | Hesitancy/scepticism/doubt |
| Gust D, 2005 | 2002 | USA | Cross-sectional | 697 | Child vaccines | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt | |
| Gust DA, 2006 | 2004-2005 | USA | Cross-sectional | Telephone | 2,286 | Mmr/dtp/hbv | Closed | Not | Hesitancy/scepticism/doubt |
| Gust DA, 2008 | 2003-2004 | USA | Cross-sectional | Telephone | 3,924 | Child vaccines | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Gust DA, 2005 | 2003 | USA | Cross-sectional | 642 | Child vaccines | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt | |
| Gust DA, 2004 | 2001 | USA | Case-control | 1,477 | Mmr/dtp/hbv | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt | |
| Gust DA, 2003 | 2002 | USA | Cross-sectional | 1,768 | Child vaccines | Likert scale | Statistical methods not reported | Acceptance | |
| Gustafson R, 2005 | 2003 | Canada | Cross-sectional | Telephone | 1,246 | Varicella | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Haesebaert J, 2012 | 2008 | France | Cross-sectional | Face to face | 32 | Hpv | Open field | Statistical methods not reported | Acceptance |
| Hagan D, 2016 | 2013 | Ghana | Cross-sectional | Paper-based | 303 | Child vaccines | Closed | Statistical methods not reported | Acceptance |
| Hagemann C, 2017 | 2009-2011 | Germany | Cross-sectional | Paper-based | 1,998 | Varicella/measles | N.A. | With statistical methods | Hesitancy/scepticism/doubt |
| Hak E, 2005 | N.A. | Netherland | Cross-sectional | Not reported | 283 | Influenza/hbv/bcg | Likert scale | Not | Refusal |
| Hamama-Raz Y, 2016 | 2014 | Israel | Cross-sectional | On-line | 314 | Child vaccines | Likert scale | Not | Acceptance |
| Han K, Zheng H, 2014 | 2010 | China | Cross-sectional | Face to face | 1,530 | Bcg/dtp/polio/mcv/hbv | Closed | With statistical methods | Hesitancy/scepticism/doubt |
| Hanley SJ, 2012 | 2010 | Japan | Cross-sectional | Paper-based | 862 | Hpv | Likert scale | Not | Acceptance |
| Hanley SJ, 2014 | 2010 | Japan | Cross-sectional | Paper-based | 54 | Hpv | Likert scale | Not | Acceptance |
| Harmsen IA, 2012 | 2011 | Netherlands | Cross-sectional | Paper-based | 906 | Hbv | Likert scale | Not | Acceptance |
| He L, 2015 | 2013 | China | Cross-sectional | Face to face | 298 | Flu | Open field | Not | Hesitancy/scepticism/doubt |
| Healy CM, 2014 | N.A. | USA | Cross-sectional | Not reported | 401 | Hib/pcv/mcv/flu/hbv/hav/hpv/rotavirus | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Henrikson NB, 2017 | 2013-2015 | USA | Cohort | Telephone | 237 | Child vaccines | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Hertweck SP, 2013 | N.A. | USA | Cross-sectional | On-line | 68 | Hpv | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Hilyard KM, 2014 | 2010 | USA | Cross-sectional | Not reported | 684 | Flu | Closed | Not | Hesitancy/scepticism/doubt |
| Hofman R, 2014 | 2009-2011 | Netherlands | Cohort | 793 | Hpv | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt | |
| Hofstetter AM, 2015 | 2011 | USA | Cross-sectional | Face to face | 128 | Flu | Closed | With statistical methods | Hesitancy/scepticism/doubt |
| Hon KL, 2016 | N.A. | Hong Kong | Cross-sectional | Paper-based | 3,479 | Flu | N.A. | Not | Hesitancy/scepticism/doubt |
| Hontelez JA, 2010 | N.A. | Netherland | Cross-sectional | Paper-based | 198 | Hbv | Likert scale | Not | Hesitancy/scepticism/doubt |
| Horn L, 2010 | 2008 | USA | Cross-sectional | Paper-based | 325 | Hpv | Likert scale | With statistical methods | Acceptance |
| How CH, 2016 | 2014 | Singapore | Cross-sectional | Face to face | 200 | Pcv | Likert scale | Not | Hesitancy/scepticism/doubt |
| Hu Y, 2017 | 2014 | China | Cross-sectional | Face to face | 2,772 | Child vaccines | N.A. | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Hwang JH, 2017 | 2014 | South Korea | Cross-sectional | Face to face | 638 | Flu | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Ilter E, 2010 | 2009 | Turkey | Cross-sectional | Face to face | 525 | Hpv | Likert scale | Not | Hesitancy/scepticism/doubt |
| Imburgia TM, 2017 | 2014 | USA | Cross-sectional | On-line | 2,363 | Flu | Likert scale | Not | Hesitancy/scepticism/doubt |
| Impicciatore P, 2000 | 1997 | Italy | Cross-sectional | Face to face | 1,035 | Mmr | Closed | With statistical methods | Acceptance |
| Jani JV, 2008 | 2001 | Mozambique | Cross-sectional | Face to face | 668 | Child vaccines | N.A. | Statistical methods not reported | Acceptance |
| Jaspers L, 2011 | 2009 | Indonesia | Cross-sectional | Face to face | 746 | Hpv | Closed | Not | Acceptance |
| Jessop LJ, 2010 | 2001-2004 | UK | Cohort | Paper-based | 749 | Mmr | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Jolley D, 2014 | 2012 | UK | Cross-sectional | On-line | 89 | Child vaccines | Likert scale | Statistical methods not reported | N.A. |
| Joseph NP, 2012 | 2008-2009 | USA | Cross-sectional | Face to face | 70 | Hpv | Open field | With statistical methods | Hesitancy/scepticism/doubt |
| Joseph NP, 2015 | N.A. | Cross-sectional | Paper-based | 55 | Hpv | Closed | With statistical methods | N.A. | |
| Jung M, 2013 | N.A. | Cross-sectional | On-line | 639 | Flu | N.A. | Not | Hesitancy/scepticism/doubt | |
| Kadis JA, 2011 | 2009 | USA | Cross-sectional | On-line | 496 | Hpv | Closed | Statistical methods not reported | Acceptance |
| Kahn JA, 2009 | 2006-2007 | USA | Cross-sectional | Paper-based | 7,207 | Hpv | Likert scale | With statistical methods | Hesitancy/scepticism/doubt |
| Kalucka SK, 2016 | N.A. | Poland | Cross-sectional | Paper-based | 140 | Child vaccines | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Katz ML, 2012 | 2009 | USA | Cross-sectional | Paper-based | 111 | Hpv | Likert scale | Not | Hesitancy/scepticism/doubt |
| Haesebaert J, 2014 | 2008 | France | Cross-sectional | Paper-based | 99 | Hpv | Open field | With statistical methods | Hesitancy/scepticism/doubt |
| Kaya A, 2017 | 2016 | Turkey | Cross-sectional | Paper-based | 102 | Flu | Mixed | Not | Acceptance |
| Kelley CA, 2015 | N.A. | Case-control | Paper-based | 229 | Child vaccines | Mixed | Statistical methods not reported | Refusal | |
| Kempe A, 2007 | 2003 | USA | Cross-sectional | Telephone | 472 | Flu | Mixed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Kennedy A, 2011 | 2009 | USA | Cross-sectional | 475 | Child vaccines | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt | |
| Kennedy A, 2011 | 2010 | USA | Cross-sectional | 376 | Child vaccines | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt | |
| Kennedy AM, 2005 | 2002 | USA | Cross-sectional | 1527 | Child vaccines | Likert scale | Statistical methods not reported | Hesitancy/scepticism/doubt | |
| Kepka D, 2015 | 2013 | USA | Cross-sectional | Paper-based | 118 | Hpv | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Kepka D, 2015 | 2013 | USA | Cross-sectional | Paper-based | 67 | Hpv | Mixed | With statistical methods | Hesitancy/scepticism/doubt |
| Kepka DL, 2012 | 2009 | USA | Cross-sectional | Paper-based | 578 | Hpv | Closed | With statistical methods | Hesitancy/scepticism/doubt |
| Kester LM, 2013 | 2010 | USA | Cross-sectional | On-line | 501 | Hpv | Mixed | Not | Hesitancy/scepticism/doubt |
| Kettunen C, 2017 | N.A. | USA | Cross-sectional | 84 | Child vaccines | Mixed | Statistical methods not reported | Acceptance | |
| Kim KM, 2017 | 2014-2015 | South Korea | Cross-sectional | Paper-based | 200 | Hpv | Mixed | Not | Acceptance |
| Kinder FD. 2016 | N.A. | USA | Cross-sectional | Paper-based | 72 | Hpv | Mixed | Not | Refusal |
| Ko HS, 2015 | N.A. | South Korea | Cross-sectional | Paper-based | 308 | Dtp | Closed | Not | Acceptance |
| Kong KA, 2014 | 2013 | South Korea | Cross-sectional | Telephone | 800 | Hav | Mixed | Statistical methods not reported | Acceptance |
| Krawczyk A, 2015 | 2010 | Canada | Cross-sectional | 774 | Hpv | Likert scale | Not | Hesitancy/scepticism/doubt | |
| Krawczyk A, 2015 | 2010 | Canada | Cross-sectional | 708 | Hpv | Open field | Not | Refusal | |
| Krieger JL, 2011 | N.A. | USA | Cross-sectional | Paper-based | 182 | Hpv | Closed | Not | Acceptance |
| Lavail KH, 2013 | 2010 | USA | Case-control | 376 | Child vaccines | Likert scale | Not | Acceptance | |
| Le Ngoc Tho S, 2015 | 2013 | France | Cross-sectional | Paper-based | 1,270 | Menb | Mixed | With statistical methods | Acceptance |
| Lechuga J, 2012 | N.A. | USA | Cross-sectional | Paper-based | 150 | Hpv | Open field | Not | Acceptance |
| Lee KN, 2017 | 2015-2016 | South Korea | Cross-sectional | Paper-based | 140 | Hpv | Mixed | Not | Acceptance |
| Lee Mortensen G, 2015 | 2013 | Multinational | Cross-sectional | Paper-based | 1,837 | Hpv | Closed | Not | Acceptance |
| Lehmann BA, 2017 | 2015 | Netherlands | Cross-sectional | Paper-based | 1,615 | Child vaccines | Mixed | Not | Acceptance |
| Lewis T, 1988 | 1988 | USA | Cohort | 2,029 | Dtp | N.A. | Not | N.A. | |
| Liao Q, 2016 | 2012-2013 | Hong Kong | Cross-sectional | Telephone | 1,226 | Flu | Mixed | Not | Acceptance |
| Lin CJ, 2006 | 2003-2004 | USA | Cross-sectional | Paper-based | 951 | Flu | Mixed | Not | Acceptance |
| Linam WM, 2014 | 2010-2011 | USA | Cross-sectional | Paper-based | 372 | Flu | Mixed | Not | Acceptance |
| Lindley MC, 2016 | 2013 | USA | Cross-sectional | 6,676 | Hpv | Mixed | Not | Acceptance | |
| Livni G, 2017 | 2012 | Israel | Cross-sectional | Paper-based | 186 | Flu | Mixed | Statistical methods not reported | Acceptance |
| Loke AY, 2017 | 2010 | Hong Kong | Cross-sectional | Paper-based | 170 | Hpv | Mixed | Not | Hesitancy/scepticism/doubt |
| Low MSF, 2017 | 2015-2016 | Singapore | Cross-sectional | On-line | 332 | Flu | Mixed | Statistical methods not reported | Acceptance |
| Luthy KE, 2010 | N.A. | USA | Cross-sectional | Paper-based | 86 | Child vaccines | Mixed | Not | Hesitancy/scepticism/doubt |
| Luthy KE, 2013 | N.A. | USA | Cross-sectional | Paper-based | 801 | Child vaccines | Mixed | Not | Hesitancy/scepticism/doubt |
| Luthy KE, 2009 | N.A. | USA | Cross-sectional | Paper-based | 86 | Child vaccines | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Maayan-Metzger A, 2005 | 2003 | Israel | Case-control | Paper-based | 204 | Hbv | Closed | Not | Hesitancy/scepticism/doubt |
| MacDonald SE, 2014 | N.A. | Canada | Case-control | 444 | Child vaccines | Closed | Not | Hesitancy/scepticism/doubt | |
| MacDougall DM, 2016 | 2010-2012 | Canada | Case-control | Paper-based | 722 | Rotavirus | Mixed | Statistical methods not reported | Acceptance |
| Madhivanan P, 2014 | 2010 | India | Cross-sectional | 797 | Hpv | Likert scale | Not | Acceptance | |
| Mameli C, 2014 | 2013 | Italy | Cross-sectional | Paper-based | 1,842 | Menb | Closed | Not | Hesitancy/scepticism/doubt |
| Marlow LA, 2007 | 2006 | UK | Cross-sectional | Paper-based | 684 | Hpv | Mixed | Not | Acceptance |
| Marlow LA, 2007 | 2006 | UK | Cross-sectional | Paper-based | 684 | Hpv | Likert scale | With statistical methods | Acceptance |
| Marshall H, 2014 | 2012 | Australia | Cross-sectional | Paper-based | 966 | Menb | N.A. | With statistical methods | Acceptance |
| Marshall H, 2007 | 2006 | Australia | Cross-sectional | Telephone | 2,002 | Hpv | Closed | With statistical methods | Acceptance |
| Mayet AY, 2017 | 2013 | Saudi Arabia | Cross-sectional | Paper-based | 998 | Flu | Mixed | Not | Hesitancy/scepticism/doubt |
| McCauley MM, 2012 | 2010 | USA | Cross-sectional | Telephone | 690 | Child vaccines | Likert scale | Statistical methods not reported | N.A. |
| McHale P, 2016 | 2012-2013 | UK | Cross-sectional | Telephone | 47 | Mmr | Open field | Statistical methods not reported | N.A. |
| Melman ST, 1999 | 1995-1997 | USA | Cross-sectional | Paper-based | 1,059 | Child vaccines | Open field | Not | N.A. |
| Meszaros JR, 1996 | N.A. | USA | Cross-sectional | Paper-based | 294 | Pertussis | Mixed | Not | N.A. |
| Michael CA, 2014 | 2012 | Nigeria | Cross-sectional | Paper-based | 48 | Polio | Open field | Not | N.A. |
| Michael CE, 2014 | 2009 | Nigeria | Cross-sectional | Paper-based | 201 | Hpv | Closed | Not | Acceptance |
| Middleman AB, 2002 | 2000 | USA | Cross-sectional | Paper-based | 563 | Hbv | Closed | Not | Hesitancy/scepticism/doubt |
| Milteer RM, 1996 | 1991-1994 | USA | Cross-sectional | Paper-based | 175 | Child vaccines | Open field | Not | N.A. |
| Morales-Campos DY, 2017 | 2011-2013 | Cameron | Cross-sectional | Paper-based | 317 | Hpv | Mixed | Not | Hesitancy/scepticism/doubt |
| Morhason-Bello IO, 2015 | 2012 | Nigeria | Cross-sectional | Paper-based | 1,002 | Hpv | Likert scale | With statistical methods | Acceptance |
| Morrone T, 2017 | 2015 | Italy | Cross-sectional | Paper-based | 543 | Menb | N.A. | With statistical methods | N.A. |
| Moulsdale P, 2017 | 2014 | UK | Cross-sectional | Paper-based | 86 | Flu | Likert scale | Not | Acceptance |
| Muhwezi WW, 2014 | 2012 | Uganda | Cross-sectional | Paper-based | 870 | Hpv | Closed | With statistical methods | Acceptance |
| Murakami H, 2014 | 2007 | Pakistan | Cross-sectional | Paper-based | 630 | Polio | Open field | Not | Refusal |
| My C, 2017 | 2012 | Australia | Cross-sectional | On-line | 452 | Flu | Closed | Not | Hesitancy/scepticism/doubt |
| Naeem M, 2011 | 2010 | Pakistan | Cross-sectional | Paper-based | 548 | Polio | Closed | Not | Hesitancy/scepticism/doubt |
| Naeem M, 2011 | 2010 | Pakistan | Cross-sectional | Paper-based | 506 | Hbv | Closed | Not | Hesitancy/scepticism/doubt |
| Namuigi P, 2005 | 2003 | Papua New Guinea | Cross-sectional | Paper-based | 120 | Measles | Closed | Not | Hesitancy/scepticism/doubt |
| Niederhauser VP, 2007 | 2003-2004 | USA | Cross-sectional | Paper-based | 64 | Child vaccines | Open field | Not | Hesitancy/scepticism/doubt |
| Oladokun RE, 2010 | 2009 | Nigeria | Cross-sectional | Paper-based | 248 | Bcg/polio/dtp/masles/hbv | Closed | Statistical methods not reported | Acceptance |
| Onnela JP, 2016 | 2012 | India | Cohort | Paper-based | 2,462 | Polio | Closed | Statistical methods not reported | Acceptance |
| Oria PA, 2013 | 2010 | Kenya | Cross-sectional | Paper-based | 7,177 | Flu | Mixed | Not | N.A. |
| Ozawa S, 2017 | 2013 | Nigeria | Cross-sectional | Paper-based | 198 | Dtp/measles/polio | Closed | Statistical methods not reported | N.A. |
| Paek HJ, 2015 | 2014 | South Korea | Cross-sectional | Paper-based | 1,017 | Child vaccines | Mixed | Not | N.A. |
| Painter JE, 2011 | 2009 | USA | Cross-sectional | Paper-based | 102 | Flu | Mixed | Not | N.A. |
| Parrella A, 2013 | 2011 | Australia | Cross-sectional | Telephone | 469 | Child vaccines | Likert scale | Not | N.A. |
| Parrella A, 2012 | 2010 | New Zeland | Cross-sectional | Telephone | 179 | Dtp/polio/hbv/hib/rotavirus/mmrv/mcv/pcv/flu | Closed | Statistical methods not reported | N.A. |
| Paulussen TG, 2006 | 1999 | Netherland | Cross-sectional | On-line | 491 | Dtp/polio/hib/mmr | Closed | Not | N.A. |
| Peleg N, 2015 | 2011 | Israel | Cross-sectional | Paper-based | 273 | Flu | Closed | Statistical methods not reported | N.A. |
| Pelucchi C, 2010 | 2008 | Italy | Cross-sectional | Paper-based | 3,026 | Hpv | N.A. | Not | N.A. |
| Perez S, 2016 | N.A. | Canada | Cross-sectional | On-line | 2,272 | Hpv | Closed | Statistical methods not reported | N.A. |
| Perez S, 2017 | 2014 | Canada | Cross-sectional | On-line | 2,272 | Hpv | Closed | With statistical methods | N.A. |
| Perez S, 2016 | 2014 | Canada | Cross-sectional | On-line | 2,272 | Hpv | Closed | Statistical methods not reported | N.A. |
| Perez S, 2016 | 2014 | Canada | Cross-sectional | On-line | 2,272 | Hpv | Closed | Statistical methods not reported | N.A. |
| Podolsky R, 2009 | N.A. | Usa | Cross-sectional | Paper-based | 308 | Hpv | Mixed | Statistical methods not reported | N.A. |
| Pot M, 2017 | 2015-2016 | Netherlands | Cross-sectional | On-line | 8,062 | Hpv | Closed | Not | N.A. |
| Reiter PL, 2013 | 2008-2010 | Usa | Cross-sectional | 1,951 | Hpv | Mixed | Statistical methods not reported | N.A. | |
| Restivo V, 2015 | 2012-2013 | Italy | Cross-sectional | Telephone | 443 | Mmr | Closed | Not | N.A. |
| Roberts JR, 2015 | 2011-2012 | USA | Cross-sectional | Paper-based | 363 | Dtp/mcv/hpv | Closed | Statistical methods not reported | N.A. |
| Robitz R, 2011 | 2007-2008 | USA | Cross-sectional | Telephone | 484 | Hpv | Closed | Statistical methods not reported | N.A. |
| Rogers C, 2014 | N.A. | USA | Cross-sectional | On-line | 51 | Child vaccines | Closed | Not | N.A. |
| Ruffin MT, 2012 | 2006-2008 | USA | Case-control | Telephone | 1,131 | Hpv | Closed | Not | N.A. |
| Salmon DA, 2005 | 2002-2003 | USA | Case-control | 1,367 | Polio/mmrv/dtp/hib/hbv | Closed | Not | N.A. | |
| Salmon DA, 2009 | N.A. | USA | Case-control | 963 | Child vaccines | Closed | Not | N.A. | |
| Sam IC, 2009 | 2007 | Malaysia | Cross-sectional | Paper-based | 362 | Hpv | Mixed | Not | N.A. |
| Sampson R, 2011 | 2008 | UK | Cross-sectional | I part mail, ii part interview | 7 | Flu | Closed | Not | N.A. |
| Rickert VI, 2015 | 2012-2013 | USA | Cross-sectional | On-line | 501 | Child vaccines/flu/pcv/mmr/varicella/dtp/hav/hbv/hpv/mcv | Closed | Not | N.A. |
| Rose SB, 2012 | 2008-2009 | New Zeland | Cross-sectional | Paper-based | 769 | Hpv | Closed | Not | N.A. |
| Santibanez TA, 2016 | 2011-2012 | USA | Cross-sectional | Telephone | 19,178 | Flu | Closed | Not | Hesitancy/scepticism/doubt |
| Saqer A, 2017 | 2017 | Emirati Arabi | Cross-sectional | Paper-based | 400 | Hpv | Closed | With statistical methods | Hesitancy/scepticism/doubt |
| Schollin Ask L, 2017 | 2014 | Sweden | Cross-sectional | On-line | 1,063 | Rotavirus | Closed | With statistical methods | Hesitancy/scepticism/doubt |
| Schwarz NG, 2009 | 2009 | Gabon | Cross-sectional | Paper-based | 40 | Child vaccines | Closed | Statistical methods not reported | Acceptance |
| Selmouni F, 2015 | 2015 | Marocco | Cross-sectional | Paper-based | 1,312 | Hpv | Open field | Not | Acceptance |
| Sengupta B, 1998 | 1998 | India | Cross-sectional | Paper-based | 656 | Polio | Mixed | Not | Hesitancy/scepticism/doubt |
| Seven M, 2015 | 2015 | Turkey | Cross-sectional | Paper-based | 368 | Hpv | Closed | Not | N.A. |
| Shao SJ, 2015 | 2014 | Caraibi | Cross-sectional | Paper-based | 35 | Hpv | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Shapiro GK, 2016 | 2014 | Canada | Cross-sectional | On-line | 1,427 | Hpv | Mixed | Not | Hesitancy/scepticism/doubt |
| Shapiro GK, 2017 | 2016-2017 | Canada | Cross-sectional | On-line | 4,606 | Hpv | Open field | Statistical methods not reported | Acceptance |
| Shawn DH, 1987 | 1986 | Canada | Cross-sectional | Paper-based | 133 | Hib | Closed | Statistical methods not reported | Hesitancy/scepticism/doubt |
| Sheikh A, 2013 | 2012-2013 | Pakistan | Cross-sectional | Paper-based | 1,044 | Polio/tetanus/measles | Closed | Not | Hesitancy/scepticism/doubt |
| Shuaib FM, 2010 | 2008 | Jamaica | Case-control | Paper-based | 285 | Child vaccines | Closed | Not | Hesitancy/scepticism/doubt |
| Skinner J, 1995 | 1992 | Australia | Cohort | 1,004 | Child vaccines | Mixed | Statistical methods not reported | Acceptance | |
| Smailbegovic MS, 2003 | 1999 | UK | Case-control | On-line | 129 | Child vaccines | Closed | Not | Hesitancy/scepticism/doubt |
| Smith MJ, 2009 | 2009 | USA | Cross-sectional | On-line | 121 | Child vaccines | Mixed | Not | Hesitancy/scepticism/doubt |
| Smith PJ, 2011 | 2009 | USA | Cross-sectional | Telephone | 11,206 | Child vaccines | Closed | Not | Hesitancy/scepticism/doubt |
| Smith PJ, 2010 | 2003 | USA | Cross-sectional | Telephone | 2,921 | Child vaccines | Closed | Not | Hesitancy/scepticism/doubt |
| Smith PJ, 2006 | 2001-2002 | USA | Cross-sectional | Telephone | 7,695 | Child vaccines | Closed | Not | Hesitancy/scepticism/doubt |
| Smith PJ, 2015 | 2010-2013 | USA | Cross-sectional | Telephone | 19,144 | Measles | Closed | Not | Hesitancy/scepticism/doubt |
| Smith PJ, 2016 | 2010-2014 | USA | Cross-sectional | Telephone | 8,490 | Hpv | Closed | Not | Hesitancy/scepticism/doubt |
| Sohail MM, 2015 | N.A. | Pakistan | Cross-sectional | Paper-based | 200 | Child vaccines | Mixed | Not | Acceptance |
| Songthap A, 2012 | 2012 | Thailandia | Cross-sectional | Paper-based | 664 | Hpv | Closed | Not | Hesitancy/scepticism/doubt |
| Soyer OU, 2011 | 2003 | USA | Cross-sectional | Telephone | 500 | Flu | Mixed | Not | Acceptance |
| Staras SA, 2014 | 2009 | Usa | Cross-sectional | Telephone | 2,422 | Hpv | Closed | Not | Acceptance |
| SteelFisher GK, 2015 | 2013-2014 | Multinational | Cross-sectional | Paper-based | 6,025 | Polio | Closed | Not | Acceptance |
| Stefanoff P, 2010 | 2008-2009 | Multinational | Cross-sectional | Telephone, paper-based, mail | 6,611 | Child vaccines | Mixed | Not | Acceptance |
| Stein Zamir C, 2017 | 2015 | Israel | Cross-sectional | Paper-based | 45 | Child vaccines | Closed | Not | Acceptance |
| Stephenson JD, 1987 | 1986 | Canada | Cross-sectional | Paper-based | 133 | Hib | Closed | Not | Hesitancy/scepticism/doubt |
| Stockwell MS, 2014 | 2007-2008 | USA | Cross-sectional | Paper-based | 705 | Child vaccines | Mixed | Not | Acceptance |
| Strelitz B, 2015 | 2013-2014 | USA | Cross-sectional | Paper-based | 152 | Flu | Likert scale | Not | Hesitancy/scepticism/doubt |
| Stretch R, 2008 | 2007-2008 | UK | Cross-sectional | Paper-based | 651 | Hpv | Likert scale | Statistical methods not reported | Acceptance |
| Suarez-Castaneda E, 2014 | 2011 | El Salvador | Cross-sectional | Paper-based | 2,550 | Child vaccines | Mixed | Not | Acceptance |
| Sundaram SS, 2010 | N.A. | UK | Cross-sectional | Paper-based | 50 | Hpv | Likert scale | Not | Acceptance |
| Tadesse H, 2009 | 2008 | Ethiopia | Case-control | Paper-based | 266 | Child vaccines | Mixed | Statistical methods not reported | Acceptance |
| Tagbo BN, 2014 | 2014 | Nigeria | Cross-sectional | Paper-based | 426 | Polio | Likert scale | With statistical methods | Hesitancy/scepticism/doubt |
| Taiwo L, 2017 | 2015 | Nigeria | Cross-sectional | Paper-based | 379 | Child vaccines | Mixed | Not | Hesitancy/scepticism/doubt |
| Takahashi K, 2014 | 1999-2003 | Japan | Cross-sectional | Paper-based | 120 | Measles | Mixed | Not | Refusal |
| Tam WW, 2015 | 2003 | HongKong | Cross-sectional | Paper-based | 5,617 | Varicella | Likert scale | Not | Acceptance |
| Tan TNQ, 2017 | 2011-2013 | USA | Cross-sectional | Paper-based | 516 | Hpv | Mixed | Not | Acceptance |
| Tang CW, 2011 | 2006-2008 | Taiwan | Cross-sectional | Paper-based | 539 | Child vaccines | Mixed | Statistical methods not reported | Acceptance |
| Taylor JA, 1996 | 1993 | USA | Case-control | Paper-based | 194 | Child vaccines | Likert scale | Statistical methods not reported | Acceptance |
| Taylor JA, 2002 | 1998-2000 | USA | Cross-sectional | Paper-based | 13,520 | Child vaccines | Mixed | Not | Acceptance |
| Thomas T, 2015 | N.A. | Georgia | Cross-sectional | Paper-based | 37 | Hpv | Mixed | Not | Hesitancy/scepticism/doubt |
| Thomas TL, 2012 | 2010-2011 | USA | Cross-sectional | Paper-based | 400 | Hpv | Mixed | Not | Hesitancy/scepticism/doubt |
| Thomas TL, 2013 | 2009 | USA | Cross-sectional | Paper-based | 200 | Hpv | Likert scale | Statistical methods not reported | N.A. |
| Thomas TL, 2017 | 2010-2011 | USA | Cross-sectional | Paper-based | 341 | Hpv | Likert scale | Not | Acceptance |
| Thompson EL, 2017 | 2012-2015 | USA | Cross-sectional | Telephone | 59,897 | Hpv | Closed | With statistical methods | Hesitancy/scepticism/doubt |
| Tisi G, 2013 | 2011 | Italy | Cross-sectional | Paper-based | 161 | Hpv | Mixed | Not | Acceptance |
| Taylor, JA, 2000 | 1997-1998 | USA | Cross-sectional | Paper-based | 598 | Varicella | Likert scale | Not | Hesitancy/scepticism/doubt |
| Schwartz B, 2000 | 2000-2001 | USA | Cross-sectional | Telephone | 12,060 | Hbv/dtp/measles/varicella | Mixed | Not | N.A. |
| Streng A, 2010 | 2006-2008 | Germany | Cross-sectional | Paper-based | 1,088 | Varicella | Mixed | Statistical methods not reported | Acceptance |
| Opel DJ, 2011 | 2010 | USA | Cross-sectional | 228 | Dtp/polio/mmr | Likert scale | Not | Hesitancy/scepticism/doubt | |
| World Health Organization, 1997 | 1994 | Italy | Cross-sectional | Face to face | 1,800 | Dtp/polio | Closed | With statistical methods | Hesitancy/scepticism/doubt |
N.A.: not available.
STUDY DESIGNS AND STUDY AIMS
Most of the included studies (60.4%, n = 202/334) were conducted between 2010 and 2019, while 30.5% (n = 102/334) articles reported a study period prior to 2008. In a total of 8.9% (n = 30/334) works the study period was not specified. Among the most recent studies, 48.8% (n = 100/334) were conducted in North or South America (Argentina, Brazil, Canada, Caribbean, El Salvator, Puerto Rico and USA). 14.4% of the studies (n = 48/334)) investigated the Asian population (Hong Kong, China, India, Indonesia, Israel, Japan, South Korea, Kyrgyzstan, Malaysia, Pakistan, Saudi Arabia, United Arab Emirates, Singapore, Taiwan, Thailand and Turkey), 12.8% (n = 26/334) the studies were about European people (Italy, Sweden, United Kingdom, Spain, Greece, France, Germany and the Netherlands), and 11.7% (n = 24/334) of the studies the population was from African and Oceanic countries (Cameroon, Ghana, Kenya, Gabon, Nigeria, Uganda, Morocco, Australia and New Zealand). Only 1.9% of the studies (n = 5/334) were carried out in multiple countries and were therefore classified as multinational surveys.
Almost all of the examined studies, 92.8% (n = 310/334), are cross-sectional; 4.8% (n = 16/334) are case-control studies and finally 2.4% (n = 8/334) are cohort studies.
Even though all the studies included in our review aimed at investigating the phenomenon of vaccine hesitancy, each of them focused on specific aspects of this behaviour. In this respect, the main purpose in 30.8% (n = 103/334) of the studies was to investigate parental knowledge, attitudes, practices, beliefs, awareness, concerns and sources of information about childhood vaccinations. In 21.6% (n = 72/334) of the studies the main objective was focused on investigating parents’ attitudes towards childhood vaccinations and exploring possible influential or determining factors. 18.6% (n = 62/334) and 15.0% (n = 50/334) of the studies were aimed respectively at identifying the factors associated with the parental decision to vaccinate and at examining the potential reasons for refusing immunization of their children. In 4.5% (n = 15/334) of the cases, a broad assessment of the vaccine hesitancy phenomenon was specifically investigated.
According to the 3C model, vaccine convenience is determined by physical availability, affordability and willingness-to-pay, geographical accessibility, ability to understand (consisting of both language and health literacy) and appeal of immunization services [9]. Therefore, potential barriers to immunization were also considered in our research and were investigated in 3.6% (n = 12/334) of the studies. Particular attention to the aspect of non-compliance with the vaccination schedule, such as following the correct timing and the complete administration of all the required vaccine doses, was only investigated in 3.3% (n = 11/334) of the analysed studies. Finally, 9 studies (n = 2.7%) explored the various determinants that can condition parental decisions or attitudes towards the immunization of children with pre-existing pathologies or health problems.
POPULATION CHARACTERISTICS
The population interviewed mainly consisted of parents – without any further details (73.1%, n = 244/334) – in approximately 20% of the studies (n = 66/334) the mother was the only parent surveyed, and only 1 study recruited selectively fathers. The sample size ranged from 7 to 59,897, the mean population included was about 1,647 people.
In primary studies, parents were recruited regardless of their attitudes and beliefs in 68.9% of the studies (n = 230/334), while in the remaining 103 articles, the primary studies selected the population based on their attitude: about 13.5% of the studies (45/334) were conducted in people with a positive attitude of acceptance, 38 studies (11.4%) were conducted among a hesitant population and 20 (6%) selected a population with an attitude of refusal towards vaccines. The definition of “acceptant/hesitant/refusing” behaviour was described in every article considered, and even though the specific characteristics might be slightly different among different studies, we relied on the classification provided by each article to analyse our results. Recruiting parents on the basis of their attitude towards vaccinations was very important in order to analyse the determinants of Vaccine Hesitancy in each different subgroup.
QUESTIONNAIRES CHARACTERISTICS
The Authors reported both the number and the type of items only in 38.0% (n = 127/334) of the included studies. Regarding the type, more than half (37.7%, n = 126/334) consisted of closed questions. Likert scales were the second most common type used in the questionnaires (23.6%, n = 79/334), while open-ended questions were used in 14.9% of the studies (n = 50/334).
Frequently the studies were conducted using a self-reported questionnaire (69.2%, n = 231/334), or interview (28.1%, n = 94/334), while in 2.7% (n = 9/334) of the studies data were collected in a multi-phase study. Considering the questionnaires, they were mainly administered either on paper (41.6%, n = 139/334) or as an online version (13.5%, n = 45/334). Other administration channels were mail, face to face interviews (9.9%, n = 33/334) or telephone interviews (13.5% 45/334).
However, in 80.2% of the studies, the questionnaire was not attached to the paper and for this reason it was not possible to obtain any further information. Lastly, in 42.8% of the studies (n = 143/334) the questionnaire had been previously validated; however, statistical methods were reported only in 14.8% of the sample (n = 51/334); while in 57.2% (n = 191/334) of the papers the questionnaire had not been validated.
VACCINES AND IMMUNIZATION BEHAVIOURS
22.4% (n = 75/334) of the included articles regarded childhood vaccinations in general, without addressing a specific vaccine. The HPV vaccine was the most frequently investigated (39.2%, n = 133/334), followed by influenza (13.5%, n = 47/334), measles (10.8%, n = 36/334) and varicella or varicella containing vaccine (MMRV) (4.5%, n = 15/334). 67.4% (n = 225/334) of the papers assessed the attitude towards one specific vaccine (monovalent or combined): 5,7% (n = 19/334) of the articles assessed attitudes towards polio vaccine, while 6,3% (n = 22/334) assessed HBV vaccine; a lower percentage reported the behaviour towards meningococcal vaccinations (1.7% - n = 6/334 MenB and 3.6% - n = 12/334 quadrivalent vaccine), Hib vaccine, HAV vaccine, rotavirus and BCG vaccination. 7.5% (n = 25/334) of the studies focused on more than one vaccine, such as diphtheria, tetanus and pertussis vaccination.
Data about the immunization behaviours were reported in 88% of the studies (n = 294/334). In particular, the subjects involved in the studies showed a behaviour defined as “acceptance” in 38.6% studies (38.6%, n = 129/334), as “hesitancy/scepticism/doubt” in 43.4% (n = 145/334) of the studies (and as “refusal” in 6.6% (n = 22/334) of the studies. In 10.5% (n = 35/334) of the studies assessed this information was not detected.
PARENTS’ BELIEFS ABOUT VACCINE SAFETY/EFFICACY
Parents’ beliefs about vaccine safety/efficacy were evaluated in most (58.7%; n = 196/334) of the papers included in the review. In particular, 52.4% (n = 175/334) gave a quantitative evaluation, among which 53.7% (n = 94/175) showed that the majority of the sample believed vaccines to be safe and effective, 4.6% of the studies (n = 8/175) showed that the minority of the subjects interviewed believed in vaccine safety/efficacy, while 41.7% (73/175) outlined how the beliefs about vaccines’ safety/efficacy are one of the most important barriers in vaccination. Other studies (10.7%, n = 21/196) gave a qualitative and descriptive approach to the issue of “vaccine safety/efficacy”. No information was given in 41.3% of the studies (n = 138/334).
Discussion
This manuscript shows the results of an extensive systematic review conducted using three scientific databases (PubMed/Medline, Web of Science and The Cochrane Library). Out of 3,508 retrieved studies, 334 papers were included in the qualitative evaluation. The inclusion of a great number of relevant studies, of which two thirds have been conducted in the last 10 years, reflects the relevance of this issue nowadays: investigating and therefore understanding the phenomenon of vaccine hesitancy is a necessary step in the process of overcoming it. As a matter of fact, it is extremely important to counteract this attitude, as it might lead to a decrease in vaccination coverage and therefore increase the risk of future epidemics of VPDs. The original papers included in the analysis were mainly studies conducted in western countries, while 1/4 were performed in Asia and 1/7 in Africa and Oceania.
Even if all the studies included in the review aimed at exploring VH among parents or guardians, they differ in their study design, overall number of items, context and response formats. Most of the times, three different types of questions were used in the articles examined: closed questions, likert scales questions and open-ended questions (however, a combination of these types of questions was often used as well). Most of studies had a cross-sectional design and were conducted in the last ten years, aimed to investigate parental knowledge, attitudes, practices and beliefs about childhood vaccinations, while only a small percentage (4.5%) investigated the specific reasons for vaccine hesitancy. Closed questions were the most frequent, mainly through the administration of a self-reported questionnaire, but in most cases it was impossible to get more information about the tool used, because only in 20% of studies the questionnaire was attached to the article.
Closed questions, allowing a quantitative analysis, are a very useful tool although they don’t permit to explain with more details the reasons behind VH for vaccine preventable diseases. In fact, it can be defined as “the means for testing objective theories by examining the relationship among variables which in turn can be measured so that numbered data can be analyzed using statistical procedures”. On the other hand, a qualitative approach is more likely to use open questions as research tool. Open ended questions don’t enable comparisons between different studies but they do provide more detailed information of the issues examined. In fact, a qualitative approach is useful when statistical procedures and numeric data may be insufficient to capture how patients and health care professionals feel about patients’ care, enabling researchers to understand the world as another experiences it [351]. Qualitative tools are connected to the way human behavior can be explained, within the framework of the social structures in which that behavior takes place. However, closed questions represent the easiest way to explore a topic and simplify the analysis for the Authors. It should be considered that the way of administration varied among the studies and might have had an impact on the quality of the data generated [352]. Moreover, since questionnaires are a sort of “diagnostic” epidemiological tool, they should be previously validated in order to effectively measure their outcomes [353]. However, only a small percentage of questionnaire had been previously validated in the studies analysed. This aspect should be taken into account, since effectively monitoring VH and identifying beliefs about vaccines is extremely important in order to fully understand the nature of such hesitancy, to compare the phenomenon among countries and over the time, and lastly, to implement the appropriate types of intervention. In addition, only 14.8% of the included studies reported the statistical methods used to validate the questionnaire in detail.
This review shows that the most frequently analysed vaccines are HPV and flu, followed by measles and varicella containing vaccines. They were mainly investigated for the perception about risks and safety, as well for the low vaccine coverages (compared to the WHO target), which is partly due to the reduction in the perceived risk of these diseases [354]. In this perspective, the reinforcement of mandatory vaccination laws in some European countries (e.g. Italy and France) led to an increase in vaccination coverage, mainly because this intervention tackled the complacency component of VH [355, 356]. In Italy, the reinforcement of the mandatory vaccination law dramatically reduced the number of parents who missed the measles vaccination due to definitive informed dissent or unwillingness to attend the appointment [357].
Fathers were specifically investigated only in 1 study included [175] in this review: further studies should investigate this population, in order to determinate possible gender differences in VH definition. It can be speculated that fathers are little involved, by healthcare professionals, in the vaccination decisions of their children. On the contrary, the involvement of both parents could be important in order to recover the confidence of families, which has diminished over time. In this perspective, healthcare professionals should be adequately trained and properly equipped with communication skills to clearly, transparently and comprehensively deal with this problem [358, 359]. Healthcare professionals are the main source of information on the issue of vaccinations, but they are not the only one: parents frequently rely on the information they obtain on the internet, especially regarding vaccinations and the related diseases [360-362].
Before generalizing the results of this review, some limitation should be acknowledged. First, a small percentage of included studies was validated, and the questions identified didn’t address all the determinants in the Vaccine Hesitancy Matrix.
Secondly, the findings from studies investigating specific vaccines should not be generalized to all vaccines. Moreover, VH evolves rapidly in time and some determinants could change quickly, not only according to the perception of danger of the diseases reported by media in different countries but also due to other socio-cultural influences. Monitoring the trend is important in order to measure parental VH in time and to better understand parents’ concerns and behaviors. Generally speaking, the availability of a good and accurate tool, tested and validated in all settings, and subsequently refined, is necessary to compare the results, to assess the dynamic nature of VH and to develop tailored communication strategies [363-366]. Furthermore, most of the information, especially related to the vaccination status were self-reported and no vaccination cards or Immunization Information System (IIS) were used to verify the information. Healthcare professionals and scientists should be encouraged to use the new technologies, as for instance the IIS, to monitoring both the vaccination coverage and the VH trends [367, 368]. Moreover, according to a recent review, the IIS might greatly improve and counter VH [369].
Nevertheless, a point of strength of this review is the variety of vaccine preventable diseases included. Moreover, to the best of our knowledge, this is the first systematic review that extensively assessed the developed questionnaires aimed to evaluate the parents’ VH.
Conclusions
To conclude, VH is a public health challenge as confirmed by the high number of studies and questionnaires retrieved. No questionnaire can be considered the absolute best a priori, but this study offers a deeper perspective on the available questionnaires, therefore helping future researches to identify the most suitable one according to their own aim and study setting.
Further studies monitoring VH should take into account the questionnaires already available in literature, therefore allowing to improve intra- and inter-country comparability among countries and over time, reducing the time waste in developing a new questionnaire, and improving the financial sustainability of research. Moreover, using a validate questionnaire will improve the methodological quality of future studies.
Figures and tables
Acknowledgements
The Authors would like to thank the components of the “Vaccine and vaccine hesitancy” working group of the Committee of Medical Residents of the Italian Society of Hygiene and Preventive Medicine.
Funding sources: this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Conflict of interest statement
The authors declare no conflict of interest.
Authors’ contributions
VG and PC conceived the study, PC, GV, IB, GD, MN, OG, FD, PS, SDN, SP, AC, LG, FDA, FDG, EA, OES, LK, CA, VG performed a search of the literature, drafted and revised the manuscript. GD revised the language. VG and IB revised critically the manuscript. All authors read and approved the last version of the manuscript.
References
- [1].Centers for Disease Control and Prevention (CDC), Ten great public health achievements-United States, 1900-1999. MMWR Morb Mortal Wkly Rep 1999;48:241-3. [PubMed] [Google Scholar]
- [2].Orenstein WA, Douglas RG, Rodewald LE, Hinman AR. Immunizations in the United States: success, structure, and stress. Health Aff (Millwood) 2005;24(3):599-6. https://doi.org/10.1377/hlthaff.24.3.599 10.1377/hlthaff.24.3.599 [DOI] [PubMed] [Google Scholar]
- [3].Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Parental vaccine safety concerns in 2009. Pediatrics 2010;125(4): 654-9. https://doi.org/10.1542/peds.2009-1962 10.1542/peds.2009-1962 [DOI] [PubMed] [Google Scholar]
- [4].McClure CC, Cataldi JR, O’Leary ST. Vaccine Hesitancy: Where We Are and Where We Are Going. Clin Ther 2017;39(8): 1550-62. https://doi.org/10.1016/j.clinthera.2017.07.003 10.1016/j.clinthera.2017.07.003 [DOI] [PubMed] [Google Scholar]
- [5].Patel M, Lee AD, Redd SB, Clemmons NS, McNall RJ, Cohn AC, Gastanaduy PA. Increase in Measles Cases - United States, January 1-April 26, 2019. MMWR Morb Mortal Wkly Rep 2019;68(17): 402-4. https://doi.org/10.15585/mmwr.mm6817e1 10.15585/mmwr.mm6817e1 [DOI] [PubMed] [Google Scholar]
- [6].Public Health Agency of Canada. Measles & Rubella Weekly Monitoring Report – Week 20: May 12 to May 18, 2019. 2019 November 2019]; Available from: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/measles-rubella-surveillance/2019/week-20.html
- [7].European Center for Diseases Control and prevention, Monthly measles and rubella monitoring report, May 2019. 2019. [Google Scholar]
- [8].Zipprich J, Winter K, Hacker J, Xia D, Watt J, Harriman K. Center for Disease Control and Prevention, Measles outbreak--California, December 2014-February 2015. MMWR Morb Mortal Wkly Rep 2015;64(6):153-4. [PMC free article] [PubMed] [Google Scholar]
- [9].MacDonald NESage Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015;33(34):4161-4. https://doi.org/10.1016/j.vaccine.2015.04.036 10.1016/j.vaccine.2015.04.036 [DOI] [PubMed] [Google Scholar]
- [10].World Health Organization, Report of the SAGE working group on vaccine hesitancy, 2014. [Google Scholar]
- [11].Larson HJ, Jarrett C, Eckersberger E, Smith DM. Paterson Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine 2014;32(19):2150-9. https://doi.org/10.1016/j.vaccine.2014.01.081 10.1016/j.vaccine.2014.01.081 [DOI] [PubMed] [Google Scholar]
- [12].Gesser-Edelsburg A, Shir-Raz Y, Green M. Why do parents who usually vaccinate their children hesitate or refuse? General good vs. individual risk. Journal of Risk Research 2016;19(4):405-24. https://doi.org/10.1080/13669877.2014.983947 10.1080/13669877.2014.983947 [DOI] [Google Scholar]
- [13].Harmsen IA, Mollema L, Ruiter RA, Paulussen TG, de Melker HE, Kok G. Why parents refuse childhood vaccination: a qualitative study using online focus groups. BMC Public Health 2013;13:1183 https://doi.org/10.1186/1471-2458-13-1183 10.1186/1471-2458-13-1183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].European Centre for Disease Prevention and Control, Rapid literature review on motivating hesitant population groups in Europe to vaccinate. 2015: Stockholm. [Google Scholar]
- [15].World Health Organization. Ten threats to global health in 2019, WHO/Rada Akbar. 2019 November 2019]; Available from: https://www.who.int/emergencies/ten-threats-to-global-health-in-2019.
- [16].Dorell C, Yankey D., Kennedy A, Stokley S. Factors that influence parental vaccination decisions for adolescents, 13 to 17 years old: National Immunization Survey-Teen, 2010. Clin Pediatr (Phila) 2013;52(2):162-70. https://doi.org/10.1177/0009922812468208 10.1177/0009922812468208 [DOI] [PubMed] [Google Scholar]
- [17].Smith LE, Amlot R, Weinman J, Yiend J, Rubin GJ. A systematic review of factors affecting vaccine uptake in young children. Vaccine 2017;35(45):6059-69. https://doi.org/10.1016/j.vaccine.2017.09.046 10.1016/j.vaccine.2017.09.046 [DOI] [PubMed] [Google Scholar]
- [18].Moher D, Liberati A, Tetzlaff J, Altman DG. Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151(4):264-9, W64. https://doi.org/10.7326/0003-4819-151-4-200908180-00135 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- [19].Childhood vaccination coverage in Italy: results of a seven-region survey. The Italian Vaccine Coverage Survey Working Group. Bull World Health Organ 1994;72(6):885-95. [PMC free article] [PubMed] [Google Scholar]
- [20].Adler A, Herring E, Babilsky H, Gazala E, Cohen A, Levy I. Parent-dependent barriers to varicella immunization in Israel: the importance of adequate information. Acta Paediatr 2007;96(3):428-31. https://doi.org/10.1111/j.1651-2227.2007.00118.x 10.1111/j.1651-2227.2007.00118.x [DOI] [PubMed] [Google Scholar]
- [21].Adorador A, McNulty R, Hart D, Fitzpatrick JP. Perceived barriers to immunizations as identified by Latino mothers. Journal of the American Academy of Nurse Practitioners 2011;23(9):501-8. [DOI] [PubMed] [Google Scholar]
- [22].Aharony N, Goldman R. E-health literacy and the vaccination dilemma: an Israeli perspective. Information Research-an International Electronic Journal 2017;22(2). [Google Scholar]
- [23].Akis S, Velipasaoglu S, Camurda AD, Beyazova U, Sahn F. Factors associated with parental acceptance and refusal of pandemic influenza A/H1N1 vaccine in Turkey. Eur J Pediatr 2011; 170(9):1165-72. https://doi.org/10.1007/s00431-011-1425-6 10.1007/s00431-011-1425-6 [DOI] [PubMed] [Google Scholar]
- [24].Akmatov M, Mikolajczyk R, Kretzschmar M, Kramer A. Attitudes and beliefs of parents about childhood vaccinations in post-soviet countries: the example of Kyrgyzstan. The Pediatric infectious disease journal 2009;28(7):637-40. [DOI] [PubMed] [Google Scholar]
- [25].Alberts CJ, van der Loeff MF, Hazeveld Y, de Melker HE, van der Wal MF, Nielen A, El Fakiri, F, Prins M, Paulusse TG. A longitudinal study on determinants of HPV vaccination uptake in parents/guardians from different ethnic backgrounds in Amsterdam, the Netherlands. BMC Public Health 2017;17(1): 220 https://doi.org/10.1186/s12889-017-4091-4 10.1186/s12889-017-4091-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Alfredsson R, Svensson E, Trollfors B, Borres M. Why do parents hesitate to vaccinate their children against measles, mumps and rubella? Acta paediatrica 2004;93(9):1232-7. [PubMed] [Google Scholar]
- [27].Allison M, Reyes M, Young P, Calame L, Sheng X, Weng H. Parental attitudes about influenza immunization and school-based immunization for school-aged children. The Pediatric infectious disease journal 2010;29(8):751-5. [DOI] [PubMed] [Google Scholar]
- [28].Allen J, Othus M, Shelton R, Li Y, Norman N, Tom L. Parental decision making about the HPV vaccine. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology 2010;19(9):2187-98. [DOI] [PubMed] [Google Scholar]
- [29].Allred NJ, Shaw KM, Santibanez TA, Rickert DL, Santoli JM. Parental vaccine safety concerns: results from the National Immunization Survey, 2001-2002. Am J Prev Med 2005;28(2): 221-4. https://doi.org/10.1016/j.amepre.2004.10.014 10.1016/j.amepre.2004.10.014 [DOI] [PubMed] [Google Scholar]
- [30].Alshammari TM, Subaiea GM, Hussain T, Moin A, Yusuff KB. Parental perceptions, attitudes and acceptance of childhood immunization in Saudi Arabia: A cross sectional study. Vaccine 2018;36(1):23-28. https://doi.org/10.1016/j.vaccine.2017.11.050 10.1016/j.vaccine.2017.11.050 [DOI] [PubMed] [Google Scholar]
- [31].Ambe JP, Omotara BA, Mandu Baba M. Perceptions, beliefs and practices of mothers in sub-urban and rural areas towards measles and measles vaccination in Northern Nigeria. Trop Doct 2001; 31(2):89-90. https://doi.org/10.1177/004947550103100211 10.1177/004947550103100211 [DOI] [PubMed] [Google Scholar]
- [32].Aharon A, Nehama H, Rishpon S, Baron-Epel O. Parents with high levels of communicative and critical health literacy are less likely to vaccinate their children. Patient Education and Counseling 2017;100(4):768-75. [DOI] [PubMed] [Google Scholar]
- [33].Arrossi S, Maceira V, Paolino M, Sankaranarayanan R. Acceptability and uptake of HPV vaccine in Argentina before its inclusion in the immunization program: a population-based survey. Vaccine 2012;30(14):2467-74. https://doi.org/10.1016/j.vaccine.2012.01.032 10.1016/j.vaccine.2012.01.032 [DOI] [PubMed] [Google Scholar]
- [34].Mohd Azizi FS, Kew Y, Moy FM. Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine 2017;35(22): 2955-61. https://doi.org/10.1016/j.vaccine.2017.04.010 10.1016/j.vaccine.2017.04.010 [DOI] [PubMed] [Google Scholar]
- [35].Baglioni A, Ceriale E, Bagnoli A, Mercone A, Nante N, Messina G. Parents’ awareness and acceptance of HPV vaccination in Italy. Ig Sanita Pubbl 2014;70(5):489-98. [PubMed] [Google Scholar]
- [36].Bakhache P, Rodrigo C, Davie S, Ahuja A, Sudovar B, Crudup T, Rose M. Health care providers’ and parents’ attitudes toward administration of new infant vaccines - a multinational survey. Eur J Pediatr 2013;172(4):485-92. https://doi.org/10.1007/s00431-012-1904-4 10.1007/s00431-012-1904-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Baldwin AS, Bruce CM, Tiro JA. Understanding how mothers of adolescent girls obtain information about the human papillomavirus vaccine: associations between mothers’ health beliefs, information seeking, and vaccination intentions in an ethnically diverse sample. J Health Psychol 2013;18(7):926-38. https://doi.org/10.1177/1359105312445078 10.1177/1359105312445078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Bardenheier B, Gonzalez IM, Washington ML, Bell BP, Averhoff F, Massoudi MS, Hyams I, Simard EP, Yusuf H. Parental knowledge, attitudes, and practices associated with not receiving hepatitis A vaccine in a demonstration project in Butte County, California. Pediatrics 2003;112(4):e269 https://doi.org/10.1542/peds.112.4.e269 10.1542/peds.112.4.e269 [DOI] [PubMed] [Google Scholar]
- [39].Bardenheier B, Yusuf H, Schwartz B, Gust D, Barker L, Rodewald L. Are parental vaccine safety concerns associated with receipt of measles-mumps-rubella, diphtheria and tetanus toxoids with acellular pertussis, or hepatitis B vaccines by children? Arch Pediatr Adolesc Med 2004;158(6):569-75. https://doi.org/10.1001/archpedi.158.6.569 10.1001/archpedi.158.6.569 [DOI] [PubMed] [Google Scholar]
- [40].Bardenheier BH, Yusuf HR, Rosenthal J, Santoli JM, Shefer AM, Rickert DL, Chu SY. Factors associated with underimmunization at 3 months of age in four medically underserved areas. Public Health Rep 2004;119(5):479-85. https://doi.org/10.1016/j.phr.2004.07.005 10.1016/j.phr.2004.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Barnack JL, Reddy DM, Swain C. Predictors of parents’ willingness to vaccinate for human papillomavirus and physicians’ intentions to recommend the vaccine. Womens Health Issues 20 https://doi.org/10 20(1): 28-34. https://doi.org/10.1016/j.whi.2009.08.007 10.1016/j.whi.2009.08.007 [DOI] [PubMed] [Google Scholar]
- [42].Barnack-Tavlaris JL, Garcini LM, Macera CA, Brodine S, Klonoff EA. Human Papillomavirus Vaccination Awareness and Acceptability Among U.S.-Born and U.S. Foreign-Born Women Living in California. Health Care Women Int 2016;37(4): 444-62. https://doi.org/10.1080/07399332.2014.954702 10.1080/07399332.2014.954702 [DOI] [PubMed] [Google Scholar]
- [43].Bazzano A, Zeldin A, Schuster E, Barrett C, Lehrer D. Vaccine-related beliefs and practices of parents of children with autism spectrum disorders. Am J Intellect Dev Disabil 2012;117(3): 233-42. https://doi.org/10.1352/1944-7558-117.3.233 10.1352/1944-7558-117.3.233 [DOI] [PubMed] [Google Scholar]
- [44].Bedford H, Lansley M. More vaccines for children? Parents’ views. Vaccine 2007;25(45):7818-23. https://doi.org/10.1016/j.vaccine.2007.08.057 10.1016/j.vaccine.2007.08.057 [DOI] [PubMed] [Google Scholar]
- [45].Beel ER, Rench MA, Montesinos DP, Mayes B, Healy CM. Knowledge and attitudes of postpartum women toward immunization during pregnancy and the peripartum period. Hum Vaccin Immunother 2013;9(9):1926-31. https://doi.org/10.4161/hv.25096 10.4161/hv.25096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Ben Natan M, Aharon O, Palickshvili S, Gurman V. Attitude of Israeli mothers with vaccination of their daughters against human papilloma virus. J Pediatr Nurs 2011;26(1):70-7. https://doi.org/10.1016/j.pedn.2009.07.006 10.1016/j.pedn.2009.07.006 [DOI] [PubMed] [Google Scholar]
- [47].Ben Natan M, Kabha S, Yehia M, Hamza O. Factors That Influence Israeli Muslim Arab Parents’ Intention to Vaccinate Their Children Against Influenza. J Pediatr Nurs 2016;31(3):293-8. https://doi.org/10.1016/j.pedn.2015.12.014 10.1016/j.pedn.2015.12.014 [DOI] [PubMed] [Google Scholar]
- [48].Ben Natan M, Midlej K, Mitelman O, Vafiliev K. Intention of Mothers in Israel to Vaccinate their Sons against the Human Papilloma Virus. J Pediatr Nurs 2017;33:41-5. https://doi.org/10.1016/j.pedn.2017.01.001 10.1016/j.pedn.2017.01.001 [DOI] [PubMed] [Google Scholar]
- [49].Berenson AB, Laz TH, Hirth JM, McGrath CJ, Rahman M. Effect of the decision-making process in the family on HPV vaccination rates among adolescents 9-17 years of age. Hum Vaccin Immunother 2014;10(7):1807-11. https://doi.org/10.4161/hv.28779 10.4161/hv.28779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Bettinger JA, Greyson D, Money D. Attitudes and Beliefs of Pregnant Women and New Mothers Regarding Influenza Vaccination in British Columbia. J Obstet Gynaecol Can 2016;38(11): 1045-52. https://doi.org/10.1016/j.jogc.2016.08.004 10.1016/j.jogc.2016.08.004 [DOI] [PubMed] [Google Scholar]
- [51].Bham S, Saeed F, Shah M. Routine Immunization in Children and Unsatisfactory Polio Campaigns; A Cross Sectional Survey Conducted at Darul Sehat Hospital, Karachi. Annals Abbasi Shaheed Hospital & Karachi Medical & Dental College 2016; 21(1):29-36. [Google Scholar]
- [52].Bianco A, Pileggi C, Iozzo F, Nobile CG, Pavia M. Vaccination against human papilloma virus infection in male adolescents: knowledge, attitudes, and acceptability among parents in Italy. Hum Vaccin Immunother 2014;10(9):2536-42. https://doi.org/10.4161/21645515.2014.969614 10.4161/21645515.2014.969614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Bigham M, Remple VP, Pielak K, McIntyre C, White R, Wu W. Uptake and behavioural and attitudinal determinants of immunization in an expanded routine infant hepatitis B vaccination program in British Columbia. Can J Public Health 2006; 97(2): 90-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Alder S, Gustafsson S, Perinetti C, Mints M, Sundstrom K, Andersson S. Mothers’ acceptance of human papillomavirus (HPV) vaccination for daughters in a country with a high prevalence of HPV. Oncol Rep 2015; 33(5):2521-8. https://doi.org/10.3892/or.2015.3817 10.3892/or.2015.3817 [DOI] [PubMed] [Google Scholar]
- [55].Basu P, Mittal S. Acceptability of human papillomavirus vaccine among the urban, affluent and educated parents of young girls residing in Kolkata, Eastern India. J Obstet Gynaecol Res 2011;37(5):393-401. https://doi.org/10.1111/j.1447-0756.2010.01371.x 10.1111/j.1447-0756.2010.01371.x [DOI] [PubMed] [Google Scholar]
- [56].Blair A, Davies E, Nebauer M, Pirozzo S, Saba S, Turner C. Why immunise. Care giver understanding of childhood immunisation. Collegian 1997;4(3):10-7. https://doi.org/10.1016/s1322-7696(08)60235-8 10.1016/s1322-7696(08)60235-8 [DOI] [PubMed] [Google Scholar]
- [57].Blyth CC, Richmond PC, Jacoby P, Thornton P, Regan A, Robins C, Kelly H, Smith DW, Effler PV. The impact of pandemic A(H1N1)pdm09 influenza and vaccine-associated adverse events on parental attitudes and influenza vaccine uptake in young children. Vaccine 2014;32(32):4075-81. https://doi.org/10.1016/j.vaccine.2014.05.055 10.1016/j.vaccine.2014.05.055 [DOI] [PubMed] [Google Scholar]
- [58].Bodson J, Warner EL, Kepka D. Moderate Awareness and Limited Knowledge Relating to Cervical Cancer, HPV, and the HPV Vaccine Among Hispanics/Latinos in Utah. Health Promot Pract 2016;17(4):548-56. https://doi.org/10.1177/1524839916640271 10.1177/1524839916640271 [DOI] [PubMed] [Google Scholar]
- [59].Bonanni P, Bergamini M. Factors influencing vaccine uptake in Italy. Vaccine. 2001;20 Suppl 1:S8-12; discussion S1. https://doi.org/10.1016/s0264-410x(01)00284-5 10.1016/s0264-410x(01)00284-5 [DOI] [PubMed] [Google Scholar]
- [60].Borena W, Luckner-Hornischer A, Katzgraber F, Holm-von Laer D. Factors affecting HPV vaccine acceptance in west Austria: Do we need to revise the current immunization scheme? Papillomavirus Res 2016;2:173-7. https://doi.org/10.1016/j.pvr.2016.10.001 10.1016/j.pvr.2016.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Borras E, Dominguez A, Fuentes M, Batalla J, Cardenosa N, Plasencia A. Parental knowledge of paediatric vaccination. BMC Public Health 2009; 9:154 https://doi.org/10.1186/1471-2458-9-154 10.1186/1471-2458-9-154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Brabin L, Roberts SA, Farzaneh F, Kitchener HC. Future acceptance of adolescent human papillomavirus vaccination: a survey of parental attitudes. Vaccine 2006;24(16):3087-94. https://doi.org/10.1016/j.vaccine.2006.01.048 10.1016/j.vaccine.2006.01.048 [DOI] [PubMed] [Google Scholar]
- [63].Brambleby P, Hanrahan J. Measles immunisation non-acceptance: validation of computer-held records and raising the vaccine uptake at early school age; the Maidstone experience. Public Health 1989;103(4):289-94. https://doi.org/10.1016/s0033-3506(89)80042-3 10.1016/s0033-3506(89)80042-3 [DOI] [PubMed] [Google Scholar]
- [64].Breitkopf CR, Pearson HC, Dinh TA, Tran BC, Vu T, Phan GA, Ngo QV, Tran VD, Rosenthal SL. Human papillomavirus vaccine decision-making in Da Nang, Vietnam: perceived spousal and adolescent-parent concordance. Vaccine 2009;27(17): 2367-71. https://doi.org/10.1016/j.vaccine.2009.02.021 10.1016/j.vaccine.2009.02.021 [DOI] [PubMed] [Google Scholar]
- [65].Brieger D, Edwards M, Mudgil P, Whitehall J. Knowledge, attitudes and opinions towards measles and the MMR vaccine across two NSW cohorts. Aust N Z J Public Health 2017;41(6): 641-646. https://doi.org/10.1111/1753-6405.12720 10.1111/1753-6405.12720 [DOI] [PubMed] [Google Scholar]
- [66].Brown B, Gabra MI, Pellman H. Reasons for acceptance or refusal of Human Papillomavirus Vaccine in a California pediatric practice. Papillomavirus Res 2017;3:42-5. https://doi.org/10.1016/j.pvr.2017.01.002 10.1016/j.pvr.2017.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Brown KF, Shanley R, Cowley NA, van Wijgerden J, Toff P, Falconer M, Ramsay M, Hudson MJ, Green J, Vincent CA, Kroll JS, Fraser G, Sevdalis N. Attitudinal and demographic predictors of measles, mumps and rubella (MMR) vaccine acceptance: development and validation of an evidence-based measurement instrument. Vaccine 2011;29(8):1700-9. https://doi.org/10.1016/j.vaccine.2010.12.030 10.1016/j.vaccine.2010.12.030 [DOI] [PubMed] [Google Scholar]
- [68].Brunson EK. The impact of social networks on parents’ vaccination decisions. Pediatrics 2013;131(5):e1397-404. https://doi.org/10.1542/peds.2012-2452 10.1542/peds.2012-2452 [DOI] [PubMed] [Google Scholar]
- [69].Bults M, Beaujean DJ, Richardus JH, van Steenbergen JE, Voeten HA. Pandemic influenza A (H1N1) vaccination in The Netherlands: parental reasoning underlying child vaccination choices. Vaccine 2011;29(37):6226-35. https://doi.org/10.1016/j.vaccine.2011.06.075 10.1016/j.vaccine.2011.06.075 [DOI] [PubMed] [Google Scholar]
- [70].Burdette AM, Gordon-Jokinen H, Hill TD. Social determinants of HPV vaccination delay rationales: Evidence from the 2011 National Immunization Survey-Teen. Prev Med Rep 2014;1: 21-6. https://doi.org/10.1016/j.pmedr.2014.09.003 10.1016/j.pmedr.2014.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Busse JW, Walji R, Wilson K. Parents’ experiences discussing pediatric vaccination with healthcare providers: a survey of Canadian naturopathic patients. PLoS One 2011;6(8):e22737 https://doi.org/10.1371/journal.pone.0022737 10.1371/journal.pone.0022737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Buyuktiryaki B, Soyer OU, Erkocoglu M, Dogan A, Azkur D, Kocabas CN, Dallar Y, Tuncer A, Sekerel BE. What a pandemic teaches us about vaccination attitudes of parents of children with asthma. Vaccine 2014;32(20):2275-80. https://doi.org/10.1016/j.vaccine.2014.02.076 10.1016/j.vaccine.2014.02.076 [DOI] [PubMed] [Google Scholar]
- [73].Cacciatore MA, Nowak G, Evans NJ. Exploring The Impact Of The US Measles Outbreak On Parental Awareness Of And Support For Vaccination. Health Aff (Millwood) 2016;35(2):334-40. https://doi.org/10.1377/hlthaff.2015.1093 10.1377/hlthaff.2015.1093 [DOI] [PubMed] [Google Scholar]
- [74].Campbell H, Edwards A, Letley L, Bedford H, Ramsay M, Yarwood J. Changing attitudes to childhood immunisation in English parents. Vaccine 2017;35(22):2979-85. https://doi.org/10.1016/j.vaccine.2017.03.089 10.1016/j.vaccine.2017.03.089 [DOI] [PubMed] [Google Scholar]
- [75].Carlos RC, Dempsey AF, Resnicow K, Ruffin M, Patel DA, Straus CM, Vanessa KD. Maternal characteristics that predict a preference for mandatory adolescent HPV vaccination. Hum Vaccin 2011;7(2):225-9. https://doi.org/10.4161/hv.7.2.13691 10.4161/hv.7.2.13691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Casiday R, Cresswell T, Wilson D, Panter-Brick C. A survey of UK parental attitudes to the MMR vaccine and trust in medical authority. Vaccine 2006;24(2):177-84. https://doi.org/10.1016/j.vaccine.2005.07.063 10.1016/j.vaccine.2005.07.063 [DOI] [PubMed] [Google Scholar]
- [77].Cassell JA, Leach M, Poltorak MS, Mercer CH, Iversen A, Fairhead JR. Is the cultural context of MMR rejection a key to an effective public health discourse? Public Health 2006;120(9):783-94. https://doi.org/10.1016/j.puhe.2006.03.011 10.1016/j.puhe.2006.03.011 [DOI] [PubMed] [Google Scholar]
- [78].Cataldi JR, Dempsey AF, O’Leary ST. Measles, the media, and MMR: Impact of the 2014-15 measles outbreak. Vaccine 2016;34(50):6375-80. https://doi.org/10.1016/j.vaccine.2016.10.048 10.1016/j.vaccine.2016.10.048 [DOI] [PubMed] [Google Scholar]
- [79].Chan JY, Leung KM, Tam WW, Lee A. Varicella vaccine uptake and associated factors in children in Hong Kong. Epidemiol Infect, 2014; 142(5): 994-1001. https://doi.org/10.1017/S0950268813001994 10.1017/S0950268813001994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Chaparro RM, Em Vargas V, Zorzo LR, Genero S, Cayre A. Acceptance of human papillomavirus vaccination and associated factors in the city of Resistencia, Argentina. Arch Argent Pediatr 2016;114(1):36-43. https://doi.org/10.5546/aap.2016.eng.36 10.5546/aap.2016.eng.36 [DOI] [PubMed] [Google Scholar]
- [81].Chau JPC, Lo SHS, Choi KC, Chau MHK, Tong DWK, Kwong TKY, Thompson DR. Factors Determining the Uptake of Influenza Vaccination Among Children With Chronic Conditions. Pediatr Infect Dis J 2017;36(7):e197-e202. https://doi.org/10.1097/INF.0000000000001550 10.1097/INF.0000000000001550 [DOI] [PubMed] [Google Scholar]
- [82].Chen CH, Chiu PJ, Chih YC, Yeh GL. Determinants of influenza vaccination among young Taiwanese children. Vaccine 2015; 3(16):1993-8. https://doi.org/10.1016/j.vaccine.2015.01.032 10.1016/j.vaccine.2015.01.032 [DOI] [PubMed] [Google Scholar]
- [83].Chen MF, Wang RH, Schneider JK, Tsai CT, Jiang DD, Hung MN, Lin LJ. Using the Health Belief Model to understand caregiver factors influencing childhood influenza vaccinations. J Community Health Nurs 2011;28(1):29-40. https://doi.org/10.1080/07370016.2011.539087 10.1080/07370016.2011.539087 [DOI] [PubMed] [Google Scholar]
- [84].Cheruvu VK, Bhatta MP, Drinkard LN. Factors associated with parental reasons for “no-intent” to vaccinate female adolescents with human papillomavirus vaccine: National Immunization Survey - Teen 2008-2012. BMC Pediatr 2017;17(1):52 https://doi.org/10.1186/s12887-017-0804-1 10.1186/s12887-017-0804-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Chung Y, Schamel J, Fisher A, Frew PM. Influences on Immunization Decision-Making among US Parents of Young Children. Matern Child Health J 2017;21(12):2178-87. https://doi.org/10.1007/s10995-017-2336-6 10.1007/s10995-017-2336-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Cipriano JJ, Scoloveno R, Kelly A. Increasing Parental Knowledge Related to the Human Papillomavirus (HPV) Vaccine. J Pediatr Health Care 2018;32(1):29-35. https://doi.org/10.1016/j.pedhc.2017.06.006 10.1016/j.pedhc.2017.06.006 [DOI] [PubMed] [Google Scholar]
- [87].Clark SJ, Cowan AE, Filipp SL, Fisher AM, Stokley S. Understanding Non-Completion of the Human Papillomavirus Vaccine Series: Parent-Reported Reasons for Why Adolescents Might Not Receive Additional Doses, United States, 2012. Public Health Rep 2016;131(3):390-5. https://doi.org/10.1177/003335491613100304 10.1177/003335491613100304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Clark SJ, Cowan AE, Filipp SL, Fisher AM, Stokley S. Parent Perception of Provider Interactions Influences HPV Vaccination Status of Adolescent Females. Clin Pediatr (Phila) 2016;55(8): 701-6. https://doi.org/10.1177/0009922815610629 10.1177/0009922815610629 [DOI] [PubMed] [Google Scholar]
- [89].Clark SJ, Cowan AE, Filipp SL, Fisher AM, Stokley S. Parent HPV vaccine perspectives and the likelihood of HPV vaccination of adolescent males. Hum Vaccin Immunother 2016;12(1): 47-51. https://doi.org/10.1080/21645515.2015.1073426 10.1080/21645515.2015.1073426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Cockcroft A, Usman MU, Nyamucherera OF, Emori H, Duke B, Umar NA, Andersson N. Why children are not vaccinated against measles: a cross-sectional study in two Nigerian States. Arch Public Health 2014;72(1):48 https://doi.org/10.1186/2049-3258-72-48 10.1186/2049-3258-72-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Colon-Lopez V, Toro-Mejias LM, Conde-Toro A, Serra-Rivera MJ, Martinez TM, Rodriguez V, Rios AM, Berdiel L, Villanueva H. Views on HPV and HPV Vaccination: The Experience at a Federal Qualified Clinic in Puerto Rico. J Health Care Poor Underserved 2016;27(3):1411-26. https://doi.org/10.1353/hpu.2016.0126 10.1353/hpu.2016.0126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Colon-Lopez V, Quinones V, Del Toro-Mejias LM, Conde-Toro A, Serra-Rivera MJ, Martinez TM, Rodriguez V, Berdiel L, Villanueva H. HPV Awareness and Vaccine Willingness Among Dominican Immigrant Parents Attending a Federal Qualified Health Clinic in Puerto Rico. J Immigr Minor Health 2015; 17(4):1086-90. https://doi.org/10.1007/s10903-014-0067-y 10.1007/s10903-014-0067-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Coniglio MA, Platania M, Privitera D, Giammanco G, Pignato S. Parents’ attitudes and behaviours towards recommended vaccinations in Sicily, Italy. BMC Public Health 2011;11:305 https://doi.org/10.1186/1471-2458-11-305 10.1186/1471-2458-11-305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94].Constantine NA, Jerman P. Acceptance of human papillomavirus vaccination among Californian parents of daughters: a representative statewide analysis. J Adolesc Health 2007;40(2): 108-15. https://doi.org/10.1016/j.jadohealth.2006.10.007 10.1016/j.jadohealth.2006.10.007 [DOI] [PubMed] [Google Scholar]
- [95].Cooper Robbins SC, Leask J, Booy R. Parents’ attitudes towards the influenza vaccine and influencing factors. J Paediatr Child Health 2011;47(7):419-22. https://doi.org/10.1111/j.1440-1754.2010.01993.x 10.1111/j.1440-1754.2010.01993.x [DOI] [PubMed] [Google Scholar]
- [96].Costa-Pinto JC, Willaby HW, Leask J, Hoq M, Schuster T, Ghazarian A, O’Keefe J, Danchin MH. Parental Immunisation Needs and Attitudes Survey in paediatric hospital clinics and community maternal and child health centres in Melbourne, Australia. J Paediatr Child Health 2018;54(5):522-529. https://doi.org/10.1111/jpc.13790 10.1111/jpc.13790 [DOI] [PubMed] [Google Scholar]
- [97].Coyne-Beasley T, Reiter PL, Liberty AC, Ford CA, Miles DR, Brewer NT. Awareness is not enough: the need to increase meningococcal vaccine uptake. Clin Pediatr (Phila) 2013;52(5): 441-50. https://doi.org/10.1177/0009922813481847 10.1177/0009922813481847 [DOI] [PubMed] [Google Scholar]
- [98].Cuninghame CJ, Charlton CP, Jenkins SM. Immunization uptake and parental perceptions in a strictly orthodox Jewish community in north-east London. J Public Health Med 1994;16(3): 314-7. [PubMed] [Google Scholar]
- [99].Cunningham-Erves J, Talbott LL, O’Neal MR, Ivankova NV, Wallston KA. Development of a Theory-based, Sociocultural Instrument to Assess Black Maternal Intentions to Vaccinate Their Daughters Aged 9 to 12 Against HPV. J Cancer Educ 2016;31(3): 514-21. https://doi.org/10.1007/s13187-015-0867-3 10.1007/s13187-015-0867-3 [DOI] [PubMed] [Google Scholar]
- [100].Dahlstrom LA, Tran TN, Lundholm C, Young C, Sundstrom K, Sparen P. Attitudes to HPV vaccination among parents of children aged 12-15 years-a population-based survey in Sweden. Int J Cancer, 20 https://doi.org/10 126(2): 500-7. https://doi.org/10.1002/ijc.24712 10.1002/ijc.24712 [DOI] [PubMed] [Google Scholar]
- [101].Daley MF, Crane LA, Chandramouli V, Beaty BL, Barrow J, Allred N, Berman S, Kempe A. Misperceptions about influenza vaccination among parents of healthy young children. Clin Pediatr (Phila) 2007;46(5):408-17. https://doi.org/10.1177/0009922806298647 10.1177/0009922806298647 [DOI] [PubMed] [Google Scholar]
- [102].Danchin MH, Costa-Pinto J, Attwell K, Willaby H, Wiley K, Hoq M, Leask J, Perrett KP, O’Keefe J, Giles ML, Marshall H. Vaccine decision-making begins in pregnancy: Correlation between vaccine concerns, intentions and maternal vaccination with subsequent childhood vaccine uptake. Vaccine 2018;36(44):6473-9. https://doi.org/10.1016/j.vaccine.2017.08.003 10.1016/j.vaccine.2017.08.003 [DOI] [PubMed] [Google Scholar]
- [103].Danis K, Georgakopoulou T, Stavrou T, Laggas D, Panagiotopoulos T. Socioeconomic factors play a more important role in childhood vaccination coverage than parental perceptions: a cross-sectional study in Greece. Vaccine 2010;28(7):1861-9. https://doi.org/10.1016/j.vaccine.2009.11.078 10.1016/j.vaccine.2009.11.078 [DOI] [PubMed] [Google Scholar]
- [104].Dannetun E, Tegnell A, Giesecke J. Parents’ attitudes towards hepatitis B vaccination for their children. A survey comparing paper and web questionnaires, Sweden 2005; BMC Public Health 2007;7:86 https://doi.org/10.1186/1471-2458-7-86 10.1186/1471-2458-7-86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [105].Dannetun E, Tegnell A, Hermansson G, Giesecke J. Parents’ reported reasons for avoiding MMR vaccination. A telephone survey. Scand J Prim Health Care 2005;23(3):149-53. https://doi.org/10.1080/02813430510031306 10.1080/02813430510031306 [DOI] [PubMed] [Google Scholar]
- [106].Danova J, Salek J, Kocourkova A, Celko AM. Factors Associated with Parental Refusal of Routine Vaccination in the Czech Republic. Cent Eur J Public Health 2015;23(4):321-3. https://doi.org/10.21101/cejph.a4395 10.21101/cejph.a4395 [DOI] [PubMed] [Google Scholar]
- [107].Darden PM, Thompson DM, Roberts JR, Hale JJ, Pope C, Naifeh M, Jacobson RM. Reasons for not vaccinating adolescents: National Immunization Survey of Teens, 2008-20 https://doi.org/10 Pediatrics 2013;131(4):645-51. https://doi.org/10.1542/peds.2012-2384 10.1542/peds.2012-2384 [DOI] [PubMed] [Google Scholar]
- [108].Davis K, Dickman ED, Ferris D, Dias JK. Human papillomavirus vaccine acceptability among parents of 10- to 15-year-old adolescents. J Low Genit Tract Dis 2004;8(3):188-94. https://doi.org/10.1097/00128360-200407000-00005 10.1097/00128360-200407000-00005 [DOI] [PubMed] [Google Scholar]
- [109].Dawar M, Dobson S, Kallos A, LaJeunesse C, Weatherill S, Daly P. Measuring hepatitis B uptake in a new universal infant program. Can J Public Health 2002;93(4):281-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110].de Courval FP, De Serres G, Duval B. Varicella vaccine: factors influencing uptake. Can J Public Health 2003;94(4):268-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [111].de Visser R, McDonnell E. Correlates of parents’ reports of acceptability of human papilloma virus vaccination for their school-aged children. Sex Health 2008;5(4):331-8. https://doi.org/10.1071/sh08042 10.1071/sh08042 [DOI] [PubMed] [Google Scholar]
- [112].Dempsey AF, Butchart A, Singer D, Clark S, Davis M. Factors associated with parental intentions for male human papillomavirus vaccination: results of a national survey. Sex Transm Dis 2011;38(8):769-76. https://doi.org/10.1097/OLQ.0b013e318211c248 10.1097/OLQ.0b013e318211c248 [DOI] [PubMed] [Google Scholar]
- [113].Dempsey AF, Maertens J, Beaty B, O’Leary ST. Characteristics of users of a tailored, interactive website for parents and its impact on adolescent vaccination attitudes and uptake. BMC Res Notes 2015;8:739 https://doi.org/10.1186/s13104-015-1721-8 10.1186/s13104-015-1721-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [114].Dempsey AF, Zimet GD, Davis RL, Koutsky L. Factors that are associated with parental acceptance of human papillomavirus vaccines: a randomized intervention study of written information about HPV. Pediatrics 2006;117(5): 1486-93. https://doi.org/10.1542/peds.2005-1381 10.1542/peds.2005-1381 [DOI] [PubMed] [Google Scholar]
- [115].DiAnna Kinder F. Parental Refusal of Human Papillomavirus Vaccine: Multisite Study. J Pediatr Health Care 2018;32(2): 150-6. https://doi.org/10.1016/j.pedhc.2017.09.003 10.1016/j.pedhc.2017.09.003 [DOI] [PubMed] [Google Scholar]
- [116].Dinh TA, Rosenthal SL, Doan ED, Trang T, Pham VH, Tran BD, Tran VD, Phan GA, Chu HK, Breitkopf CR. Attitudes of mothers in Da Nang, Vietnam toward a human papillomavirus vaccine. J Adolesc Health 2007;40(6):559-63. https://doi.org/10.1016/j.jadohealth.2007.02.003 10.1016/j.jadohealth.2007.02.003 [DOI] [PubMed] [Google Scholar]
- [117].Dorell C, Yankey D, Jeyarajah J, Stokley S, Fisher A, Markowitz L, Smith PJ. Delay and refusal of human papillomavirus vaccine for girls, national immunization survey-teen, 2010. Clin Pediatr (Phila) 2014;53(3):261-9. https://doi.org/10.1177/0009922813520070 10.1177/0009922813520070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [118].Dorell C, Yankey D, Strasser S. Parent-reported reasons for nonreceipt of recommended adolescent vaccinations, national immunization survey: teen, 2009. Clin Pediatr (Phila) 2011;50(12): 1116-24. https://doi.org/10.1177/0009922811415104 10.1177/0009922811415104 [DOI] [PubMed] [Google Scholar]
- [119].Dube E, Bettinger JA, Halperin B, Bradet R, Lavoie F, Sauvageau C, Gilca V, Boulianne N. Determinants of parents’ decision to vaccinate their children against rotavirus: results of a longitudinal study. Health Educ Res 2012;27(6):1069-80. https://doi.org/10.1093/her/cys088 10.1093/her/cys088 [DOI] [PubMed] [Google Scholar]
- [120].Dube E, Gagnon D, Hamel D, Belley S, Gagne H, Boulianne N, Landry M, Bettinger JA. Parents’ and adolescents’ willingness to be vaccinated against serogroup B meningococcal disease during a mass vaccination in Saguenay-Lac-St-Jean (Quebec). Can J Infect Dis Med Microbiol 2015;26(3):163-7. https://doi.org/10.1155/2015/732464 10.1155/2015/732464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [121].Dube E, Gagnon D, Ouakki M, Bettinger JA, Witteman HO, MacDonald S, Fisher W, Saini V, Greyson DCanadian Immunization Research N. Measuring vaccine acceptance among Canadian parents: A survey of the Canadian Immunization Research Network. Vaccine 2018;36(4):545-52. https://doi.org/10.1016/j.vaccine.2017.12.005 10.1016/j.vaccine.2017.12.005 [DOI] [PubMed] [Google Scholar]
- [122].Dube E, Gagnon D, Zhou Z, Deceuninck G. Parental Vaccine Hesitancy in Quebec (Canada). PLoS Curr, 2016. 8 https://doi.org/10.1371/currents.outbreaks.9e239605f4d320c6ad27ce2aea5aaad2 10.1371/currents.outbreaks.9e239605f4d320c6ad27ce2aea5aaad2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [123].Ezat SW, Hod R, Mustafa J, Mohd Dali AZ, Sulaiman AS, Azman A. National HPV immunisation programme: knowledge and acceptance of mothers attending an obstetrics clinic at a teaching hospital, Kuala Lumpur. Asian Pac J Cancer Prev 2013;14(5): 2991-9. https://doi.org/10.7314/apjcp.2013.14.5.2991 10.7314/apjcp.2013.14.5.2991 [DOI] [PubMed] [Google Scholar]
- [124].Ezeanochie MC, Olagbuji BN. Human papilloma virus vaccine: determinants of acceptability by mothers for adolescents in Nigeria. Afr J Reprod Health 2014;18(3):154-8. [PubMed] [Google Scholar]
- [125].Ezenwa BN, Balogun MR, Okafor IP. Mothers’ human papilloma virus knowledge and willingness to vaccinate their adolescent daughters in Lagos, Nigeria. Int J Womens Health 2013;5: 371-7. https://doi.org/10.2147/IJWH.S44483 10.2147/IJWH.S44483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [126].Farias CC, Jesus DV, Moraes HS, Buttenbender IF, Martins IS, Souto MG., Goncalves Filho P.H., Costa R.M., Silva Sde O., Ferreira T.S., Coutinho V.V., Minotto H.R., Fonseca A.J. Factors related to non-compliance to HPV vaccination in Roraima-Brazil: a region with a high incidence of cervical cancer. BMC Health Serv Res 2016;16(1):417 https://doi.org/10.1186/s12913-016-1677-y 10.1186/s12913-016-1677-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- [127].Flood EM, Rousculp MD, Ryan KJ, Beusterien KM, Divino VM, Toback SL, Sasane M, Block SL, Hall MC, Mahadevia PJ. Parents’ decision-making regarding vaccinating their children against influenza: A web-based survey. Clin Ther 2010;32(8):1448-67. https://doi.org/10.1016/j.clinthera.2010.06.020 10.1016/j.clinthera.2010.06.020 [DOI] [PubMed] [Google Scholar]
- [128].Flynn M, Ogden J. Predicting uptake of MMR vaccination: a prospective questionnaire study. Br J Gen Pract 2004;54(504): 526-30. [PMC free article] [PubMed] [Google Scholar]
- [129].Freeman VA, Freed GL. Parental knowledge, attitudes, and demand regarding a vaccine to prevent varicella. Am J Prev Med 1999;17(2):153-5. https://doi.org/10.1016/s0749-3797(99)00063-x 10.1016/s0749-3797(99)00063-x [DOI] [PubMed] [Google Scholar]
- [130].Frew PM, Fisher AK, Basket MM, Chung Y, Schamel J, Weiner JL, Mullen J, Omer SB, Orenstein WA. Changes in childhood immunization decisions in the United States: Results from 2012 & 2014 National Parental Surveys. Vaccine 2016;34(46):5689-96. https://doi.org/10.1016/j.vaccine.2016.08.001 10.1016/j.vaccine.2016.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [131].Frew PM, Hixson B, del Rio C, Esteves-Jaramillo A, Omer SB. Acceptance of pandemic 2009 influenza A (H1N1) vaccine in a minority population: determinants and potential points of intervention. Pediatrics. 2011;127 Suppl 1:S113-9. https://doi.org/10.1542/peds.2010-1722Q 10.1542/peds.2010-1722Q [DOI] [PubMed] [Google Scholar]
- [132].Fry AM, Lurie P, Gidley M, Schmink S, Lingappa J, Fischer M, Rosenstein NE. Haemophilus influenzae Type b disease among Amish children in Pennsylvania: reasons for persistent disease. Pediatrics 2001;108(4): E60 https://doi.org/10.1542/peds.108.4.e60 10.1542/peds.108.4.e60 [DOI] [PubMed] [Google Scholar]
- [133].Fuchs EL, Rahman M, Berenson AB. Examining maternal beliefs and human papillomavirus vaccine uptake among male and female children in low-income families. Papillomavirus Res 2016;2: 8-40. https://doi.org/10.1016/j.pvr.2016.02.002 10.1016/j.pvr.2016.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [134].Garcia LD, Velandia-Gonzalez M, Trumbo SP, Pedreira MC, Bravo-Alcantara P, Danovaro-Holliday MC. Understanding the main barriers to immunization in Colombia to better tailor communication strategies. BMC Public Health 2014;14:669 https://doi.org/10.1186/1471-2458-14-669 10.1186/1471-2458-14-669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [135].Gargano LM, Herbert NL, Painter JE, Sales JM, Morfaw C, Rask K, Murray D., Di Clemente RJ, Hughes JM. Impact of a physician recommendation and parental immunization attitudes on receipt or intention to receive adolescent vaccines. Hum Vaccin Immunother 2013;9(12):2627-33. https://doi.org/10.4161/hv.25823 10.4161/hv.25823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [136].Gaudino JA, Robison S. Risk factors associated with parents claiming personal-belief exemptions to school immunization requirements: community and other influences on more skeptical parents in Oregon, 2006. Vaccine 2012;30(6):1132-42. https://doi.org/10.1016/j.vaccine.2011.12.006 10.1016/j.vaccine.2011.12.006 [DOI] [PubMed] [Google Scholar]
- [137].Gefenaite G, Smit M, Nijman HW, Tami A, Drijfhout IH, Pascal A, Postma MJ, Wolters BA, van Delden JJ, Wilschut JC, Hak E. Comparatively low attendance during Human Papillomavirus catch-up vaccination among teenage girls in the Netherlands: Insights from a behavioral survey among parents. BMC Public Health 2012;12:498 https://doi.org/10.1186/1471-2458-12-498 10.1186/1471-2458-12-498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [138].Gellatly J, McVittie C, Tiliopoulos N. Predicting parents’ decisions on MMR immunisation: a mixed method investigation. Fam Pract 2005;22(6):658-62. https://doi.org/10.1093/fampra/cmi066 10.1093/fampra/cmi066 [DOI] [PubMed] [Google Scholar]
- [139].Gellin BG, Maibach EW, Marcuse EK. Do parents understand immunizations? A national telephone survey. Pediatrics 2000; 106(5):1097-102. https://doi.org/10.1542/peds.106.5.1097 10.1542/peds.106.5.1097 [DOI] [PubMed] [Google Scholar]
- [140].Gentile A, Juarez M, Hernandez S, Moya A, Bakir J, Lucion M. Influenza vaccine: Delayed vaccination schedules and missed opportunities in children under 2 years old. Vaccine 2015; 33(32):3913-7. https://doi.org/10.1016/j.vaccine.2015.06.065 10.1016/j.vaccine.2015.06.065 [DOI] [PubMed] [Google Scholar]
- [141].Gerend MA, Weibley E, Bland H. Parental response to human papillomavirus vaccine availability: uptake and intentions. J Adolesc Health 2009;45(5):528-31. https://doi.org/10.1016/j.jadohealth.2009.02.006 10.1016/j.jadohealth.2009.02.006 [DOI] [PubMed] [Google Scholar]
- [142].Gesser-Edelsburg A, Shir-Raz Y, Green M. Why do parents who usually vaccinate their children hesitate or refuse? General good vs. individual risk. Journal of Risk Research 2016;19(4):405-24. [Google Scholar]
- [143].Giambi C, D’Ancona F, Del Manso M, De Mei B, Giovannelli I, Cattaneo C, Possenti V, Declich S. Local Representatives for V. Exploring reasons for non-vaccination against human papillomavirus in Italy. BMC Infect Dis 2014;14:545 https://doi.org/10.1186/s12879-014-0545-9 10.1186/s12879-014-0545-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [144].Gilbert NL, Gilmour H, Dube E, Wilson SE, Laroche J. Estimates and determinants of HPV non-vaccination and vaccine refusal in girls 12 to 14 y of age in Canada: Results from the Childhood National Immunization Coverage Survey, 2013. Hum Vaccin Immunother 2016;12(6):1484-90. https://doi.org/10.1080/21645515.2016.1153207 10.1080/21645515.2016.1153207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [145].Gilkey MB, Calo WA, Marciniak MW, Brewer NT. Parents who refuse or delay HPV vaccine: Differences in vaccination behavior, beliefs, and clinical communication preferences. Hum Vaccin Immunother 2017;13(3):680-6. https://doi.org/10.1080/21645515.2016.1247134 10.1080/21645515.2016.1247134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [146].Glanz JM, Wagner NM, Narwaney KJ, Shoup JA, McClure DL, McCormick EV, Daley MF. A mixed methods study of parental vaccine decision making and parent-provider trust. Acad Pediatr 2013;13(5) 481-8. https://doi.org/10.1016/j.acap.2013.05.030 10.1016/j.acap.2013.05.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [147].Glenn BA, Tsui J, Coronado GD, Fernandez ME, Savas LS, Taylor VM, Bastani R. Understanding HPV vaccination among Latino adolescent girls in three U.S. regions. J Immigr Minor Health 2015;17(1):96-103. https://doi.org/10.1007/s10903-014-9996-8 10.1007/s10903-014-9996-8 [DOI] [PubMed] [Google Scholar]
- [148].Gomez Y, Leguen F, Zhang G, O’Connell E. Correlates of 2009 H1N1 influenza vaccination among day care-aged children, Miami-Dade County. Vaccine 2012;30(27): 4002-6. https://doi.org/10.1016/j.vaccine.2012.04.037 10.1016/j.vaccine.2012.04.037 [DOI] [PubMed] [Google Scholar]
- [149].Gottlieb SL, Brewer NT, Sternberg MR, Smith JS, Ziarnowski K, Liddon N, Markowitz LE. Human papillomavirus vaccine initiation in an area with elevated rates of cervical cancer. J Adolesc Health 2009;45(5):430-7. https://doi.org/10.1016/j.jadohealth.2009.03.029 10.1016/j.jadohealth.2009.03.029 [DOI] [PubMed] [Google Scholar]
- [150].Gowda C, Schaffer SE, Kopec K, Markel A, Dempsey AF. Does the relative importance of MMR vaccine concerns differ by degree of parental vaccine hesitancy?: An exploratory study. Hum Vaccin Immunother 2013;9(2):430-6. https://doi.org/10.4161/hv.22065 10.4161/hv.22065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [151].Grabiel M, Reutzel TJ, Wang S, Rubin R, Leung V, Ordonez A, Wong M, Jordan E. HPV and HPV vaccines: the knowledge levels, opinions, and behavior of parents. J Community Health 2013;38(6):1015-21. https://doi.org/10.1007/s10900-013-9725-6 10.1007/s10900-013-9725-6 [DOI] [PubMed] [Google Scholar]
- [152].Grandahl M, Oscarsson M, Stenhammar C, Neveus T, Westerling R, Tyden T. Not the right time: why parents refuse to let their daughters have the human papillomavirus vaccination. Acta Paediatr 2014;103(4):436-41. https://doi.org/10.1111/apa.12545 10.1111/apa.12545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [153].Grandahl M, Tyden T, Westerling R, Neveus T, Rosenblad A, Hedin E, Oscarsson M. To Consent or Decline HPV Vaccination: A Pilot Study at the Start of the National School-Based Vaccination Program in Sweden. J Sch Health 2017;87(1):62-70. https://doi.org/10.1111/josh.12470 10.1111/josh.12470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [154].Greenberg J, Dube E, Driedger M. Vaccine Hesitancy: In Search of the Risk Communication Comfort Zone. PLoS Curr, 2017;9 https://doi.org/10.1371/currents.outbreaks.0561a011117a1d1f9596e24949e8690b 10.1371/currents.outbreaks.0561a011117a1d1f9596e24949e8690b [DOI] [PMC free article] [PubMed] [Google Scholar]
- [155].Greenfield LS, Page LC, Kay M, Li-Vollmer M, Breuner CC, Duchin JS. Strategies for increasing adolescent immunizations in diverse ethnic communities. J Adolesc Health 2015;56(5 Suppl):S47-53. https://doi.org/10.1016/j.jadohealth.2014.10.274 10.1016/j.jadohealth.2014.10.274 [DOI] [PubMed] [Google Scholar]
- [156].Griebeler M, Feferman H, Gupta V, Patel D. Parental beliefs and knowledge about male human papillomavirus vaccination in the US: a survey of a pediatric clinic population. Int J Adolesc Med Health 2012;24(4):315-20. https://doi.org/10.1515/ijamh.2012.045 10.1515/ijamh.2012.045 [DOI] [PubMed] [Google Scholar]
- [157].Guerry SL, De Rosa CJ, Markowitz LE, Walker S, Liddon N, Kerndt PR, Gottlieb SL. Human papillomavirus vaccine initiation among adolescent girls in high-risk communities. Vaccine 2011;29(12):2235-41. https://doi.org/10.1016/j.vaccine.2011.01.052 10.1016/j.vaccine.2011.01.052 [DOI] [PubMed] [Google Scholar]
- [158].Gundogdu Z, Gundogdu O. Parental attitudes and varicella vaccine in Kocaeli, Turkey. Prev Med 2011;52(3-4):278-80. https://doi.org/10.1016/j.ypmed.2011.01.011 10.1016/j.ypmed.2011.01.011 [DOI] [PubMed] [Google Scholar]
- [159].Gunduz S, Yuksel NC, Aktoprak HB, Canbal M, Kaya M. Attitudes towards influenza vaccination in high socioeconomic status Turkish parents. Turk J Med Sci 2014;44(4):649-55. https://doi.org/10.3906/sag-1305-43 10.3906/sag-1305-43 [DOI] [PubMed] [Google Scholar]
- [160].Gupta R, Alkhateeb FM, Latif DA, Farley KN. Parental attitudes affecting compliance with the recommendation for two doses of 2009 pandemic influenza A (H1N1) vaccine in children less than 10 years of age in West Virginia. W V Med J 2013; 109(2):10-4. [PubMed] [Google Scholar]
- [161].Gust D, Brown C, Sheedy K, Hibbs B, Weaver D, Nowak G. Immunization attitudes and beliefs among parents: beyond a dichotomous perspective. Am J Health Behav 2005;29(1):81-92. https://doi.org/10.5993/ajhb.29.1.7 10.5993/ajhb.29.1.7 [DOI] [PubMed] [Google Scholar]
- [162].Gust DA, Campbell S, Kennedy A, Shui I, Barker L, Schwartz B. Parental concerns and medical-seeking behavior after immunization. Am J Prev Med 2006;31(1):32-5. https://doi.org/10.1016/j.amepre.2006.03.017 10.1016/j.amepre.2006.03.017 [DOI] [PubMed] [Google Scholar]
- [163].Gust DA, Darling N, Kennedy A, Schwartz B. Parents with doubts about vaccines: which vaccines and reasons why. Pediatrics 2008;122(4):718-25. https://doi.org/10.1542/peds.2007-0538 10.1542/peds.2007-0538 [DOI] [PubMed] [Google Scholar]
- [164].Gust DA, Kennedy A, Shui I, Smith PJ, Nowak G, Pickering LK. Parent attitudes toward immunizations and healthcare providers the role of information. Am J Prev Med 2005;29(2):105-12. https://doi.org/10.1016/j.amepre.2005.04.010 10.1016/j.amepre.2005.04.010 [DOI] [PubMed] [Google Scholar]
- [165].Gust DA, Strine TW, Maurice E, Smith P, Yusuf H, Wilkinson M, Battaglia M, Wright R, Schwartz B. Underimmunization among children: effects of vaccine safety concerns on immunization status. Pediatrics 2004;114(1):e16-22. https://doi.org/10.1542/peds.114.1.e16 10.1542/peds.114.1.e16 [DOI] [PubMed] [Google Scholar]
- [166].Gust D.A., Woodruff R., Kennedy A., Brown C., Sheedy K., Hibbs B. Parental perceptions surrounding risks and benefits of immunization. Semin Pediatr Infect Dis, 2003; 14(3): 207-12. https://doi.org/10.1016/s1045-1870(03)00035-9 10.1016/s1045-1870(03)00035-9 [DOI] [PubMed] [Google Scholar]
- [167].Gustafson R, Skowronski DM. Disparities in varicella vaccine coverage in the absence of public funding. Vaccine 2005; 23(27):3519-25. https://doi.org/10.1016/j.vaccine.2005.02.001 10.1016/j.vaccine.2005.02.001 [DOI] [PubMed] [Google Scholar]
- [168].Haesebaert J, Lutringer-Magnin D, Kalecinski J, Barone G, Jacquard AC, Regnier V, Leocmach Y, Vanhems P, Chauvin F, Lasset C. French women’s knowledge of and attitudes towards cervical cancer prevention and the acceptability of HPV vaccination among those with 14-18 year old daughters: a quantitative-qualitative study. BMC Public Health 2012;12:1034 https://doi.org/10.1186/1471-2458-12-1034 10.1186/1471-2458-12-1034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [169].Hagan D, Phethlu DR. Determinants of parents’ decisions on childhood immunisations at Kumasi Metropolis in Ghana. Curationis 2016;39(1): e1-e https://doi.org/10. https://doi.org/10.4102/curationis.v39i1.1554 10.4102/curationis.v39i1.1554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [170].Hagemann C, Streng A, Kraemer A, Liese JG. Heterogeneity in coverage for measles and varicella vaccination in toddlers - analysis of factors influencing parental acceptance. BMC Public Health 2017;17(1):724 https://doi.org/10.1186/s12889-017-4725-6 10.1186/s12889-017-4725-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [171].Hak E, Schonbeck Y, De Melker H, Van Essen GA, Sanders EA. Negative attitude of highly educated parents and health care workers towards future vaccinations in the Dutch childhood vaccination program. Vaccine 2005;23(24):3103-7. https://doi.org/10.1016/j.vaccine.2005.01.074 10.1016/j.vaccine.2005.01.074 [DOI] [PubMed] [Google Scholar]
- [172].Hamama-Raz Y, Ginossar-David E, Ben-Ezra M. Parental regret regarding children’s vaccines-The correlation between anticipated regret, altruism, coping strategies and attitudes toward vaccines. Isr J Health Policy Res 2016;5:55 https://doi.org/10.1186/s13584-016-0116-1 10.1186/s13584-016-0116-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [173].Han K, Zheng H, Huang Z, Qiu Q, Zeng H, Chen B, Xu J. Vaccination coverage and its determinants among migrant children in Guangdong, China. BMC Public Health 2014;14:203 https://doi.org/10.1186/1471-2458-14-203 10.1186/1471-2458-14-203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [174].Hanley SJ, Yoshioka E, Ito Y, Konno R, Hayashi Y, Kishi R, Sakuragi N. Acceptance of and attitudes towards human papillomavirus vaccination in Japanese mothers of adolescent girls. Vaccine 2012;30(39):5740-7. https://doi.org/10.1016/j.vaccine.2012.07.003 10.1016/j.vaccine.2012.07.003 [DOI] [PubMed] [Google Scholar]
- [175].Hanley SJ, Yoshioka E, Ito Y, Konno R, Sasaki Y, Kishi R, Sakuragi N. An exploratory study of Japanese fathers’ knowledge of and attitudes towards HPV and HPV vaccination: does marital status matter? Asian Pac J Cancer Prev 2014;15(4): 1837-43. https://doi.org/10.7314/apjcp.2014.15.4.1837 10.7314/apjcp.2014.15.4.1837 [DOI] [PubMed] [Google Scholar]
- [176].Harmsen IA, Lambooij MS, Ruiter RA, Mollema L, Veldwijk J, van Weert YJ, Kok G, Paulussen TG, de Wit GA, de Melker HE. Psychosocial determinants of parents’ intention to vaccinate their newborn child against hepatitis B. Vaccine 2012;30(32): 4771-7. https://doi.org/10.1016/j.vaccine.2012.05.034 10.1016/j.vaccine.2012.05.034 [DOI] [PubMed] [Google Scholar]
- [177].He L, Liao QY, Huang YQ, Feng S, Zhuang XM. Parents’ perception and their decision on their children’s vaccination against seasonal influenza in Guangzhou. Chin Med J (Engl) 2015; 128(3):327-41. https://doi.org/10.4103/0366-6999.150099 10.4103/0366-6999.150099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [178].Healy CM, Montesinos DP, Middleman AB. Parent and provider perspectives on immunization: are providers overestimating parental concerns? Vaccine 2014;32(5): 579-84. https://doi.org/10.1016/j.vaccine.2013.11.076 10.1016/j.vaccine.2013.11.076 [DOI] [PubMed] [Google Scholar]
- [179].Henrikson NB, Anderson ML, Opel DJ, Dunn J, Marcuse EK, Grossman DC. Longitudinal Trends in Vaccine Hesitancy in a Cohort of Mothers Surveyed in Washington State, 2013-2015. Public Health Rep 2017;132(4):451-4. https://doi.org/10.1177/0033354917711175 10.1177/0033354917711175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [180].Hertweck SP, LaJoie AS, Pinto MD, Flamini L, Lynch T, Logsdon MC. Health care decision making by mothers for their adolescent daughters regarding the quadrivalent HPV vaccine. J Pediatr Adolesc Gynecol 2013;26(2):96-101. https://doi.org/10.1016/j.jpag.2012.10.009 10.1016/j.jpag.2012.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [181].Hilyard KM, Quinn SC, Kim KH, Musa D, Freimuth VS. Determinants of Parental Acceptance of the H1N1 Vaccine. Health Educ Behav 2014;41(3):307-14. https://doi.org/10.1177/1090198113515244 10.1177/1090198113515244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [182].Hofman R, van Empelen P, Richardus JH, de Kok IM, de Koning HJ, van Ballegooijen M, Korfage IJ. Predictors of HPV vaccination uptake: a longitudinal study among parents. Health Educ Res 2014;29(1):83-96. https://doi.org/10.1093/her/cyt092 10.1093/her/cyt092 [DOI] [PubMed] [Google Scholar]
- [183].Hofstetter AM, Barrett A, Stockwell MS. Factors impacting influenza vaccination of urban low-income Latino children under nine years requiring two doses in the 2010-2011 season. J Community Health 2015;40(2):227-34. https://doi.org/10.1007/s10900-014-9921-z 10.1007/s10900-014-9921-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- [184].Hon KL, Tsang YC, Chan LC, Ng DK, Miu TY, Chan JY, Lee A, Leung TF. Hong Kong Society of Paediatric Research and Allergy. A community-based cross-sectional immunisation survey in parents of primary school students. NPJ Prim Care Respir Med 2016;26:16011 https://doi.org/10.1038/npjpcrm.2016.11 10.1038/npjpcrm.2016.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [185].Hontelez JA, Hahne SJ, Oomen P, de Melker H. Parental attitude towards childhood HBV vaccination in The Netherlands. Vaccine, 20 https://doi.org/10 28(4): 1015-20. https://doi.org/10.1016/j.vaccine.2009.10.128 10.1016/j.vaccine.2009.10.128 [DOI] [PubMed] [Google Scholar]
- [186].Horn L, Howard C, Waller J, Ferris DG. Opinions of parents about school-entry mandates for the human papillomavirus vaccine. J Low Genit Tract Dis 20 https://doi.org/10 14(1): 43-8. https://doi.org/10.1097/LGT.0b013e3181b0fad4 10.1097/LGT.0b013e3181b0fad4 [DOI] [PubMed] [Google Scholar]
- [187].How CH, Phua See, Chun P, Shafi F, Jakes RW. Parental knowledge, attitudes and perception of pneumococcal disease and pneumococcal conjugate vaccines in Singapore: a questionnaire-based assessment. BMC Public Health 2016;16:923 https://doi.org/10.1186/s12889-016-3597-5 10.1186/s12889-016-3597-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [188].Hu Y, Li Q, Chen Y. Timeliness of Childhood Primary Immunization and Risk Factors Related with Delays: Evidence from the 2014 Zhejiang Provincial Vaccination Coverage Survey. Int J Environ Res Public Health 2017;14(9). https://doi.org/10.3390/ijerph14091086 10.3390/ijerph14091086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [189].Hwang JH, Lim CH, Kim DH, Eun BW, Jo DS, Song YH, Kim YK. A Survey of Parental Perception and Pattern of Action in Response to Influenza-like Illness in Their Children: Including Healthcare Use and Vaccination in Korea. J Korean Med Sci 2017;32(2):204-11. https://doi.org/10.3346/jkms.2017.32.2.204 10.3346/jkms.2017.32.2.204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [190].Ilter E, Celik A, Haliloglu B, Unlugedik E, Midi A, Gunduz T, Ozekici U. Women’s knowledge of Pap smear test and human papillomavirus: acceptance of HPV vaccination to themselves and their daughters in an Islamic society. Int J Gynecol Cancer 20 https://doi.org/10 20(6): 1058-62. https://doi.org/10.1111/IGC.0b013e3181dda2b9 10.1111/IGC.0b013e3181dda2b9 [DOI] [PubMed] [Google Scholar]
- [191].Imburgia TM, Hendrix KS, Donahue KL, Sturm LA, Zimet GD. Predictors of influenza vaccination in the U.S. among children 9-13years of age. Vaccine 2017;35(18):2338-42. https://doi.org/10.1016/j.vaccine.2017.03.060 10.1016/j.vaccine.2017.03.060 [DOI] [PubMed] [Google Scholar]
- [192].Impicciatore P, Bosetti C, Schiavio S, Pandolfini C, Bonati M. Mothers as active partners in the prevention of childhood diseases: maternal factors related to immunization status of preschool children in Italy. Prev Med 2000;31(1):49-55. https://doi.org/10.1006/pmed.2000.0677 10.1006/pmed.2000.0677 [DOI] [PubMed] [Google Scholar]
- [193].Jani JV, De Schacht C, Jani IV, Bjune G. Risk factors for incomplete vaccination and missed opportunity for immunization in rural Mozambique. BMC Public Health 2008;8:161 https://doi.org/10.1186/1471-2458-8-161 10.1186/1471-2458-8-161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [194].Jaspers L, Budiningsih S, Wolterbeek R, Henderson FC, Peters AA. Parental acceptance of human papillomavirus (HPV) vaccination in Indonesia: a cross-sectional study. Vaccine 2011;29(44):7785-93. https://doi.org/10.1016/j.vaccine.2011.07.107 10.1016/j.vaccine.2011.07.107 [DOI] [PubMed] [Google Scholar]
- [195].Jessop LJ, Murrin C, Lotya J, Clarke AT, O’Mahony D, Fallon UB, Johnson H, Bury G, Kelleher CC, Murphy AW. Lifeways Cohort Study Steering G. Socio-demographic and health-related predictors of uptake of first MMR immunisation in the Lifeways Cohort Study. Vaccine 20 https://doi.org/10 28(38): 6338-43. https://doi.org/10.1016/j.vaccine.2010.06.092 10.1016/j.vaccine.2010.06.092 [DOI] [PubMed] [Google Scholar]
- [196].Jolley D, Douglas KM. The effects of anti-vaccine conspiracy theories on vaccination intentions. PLoS One 2014;9(2): e89177 https://doi.org/10.1371/journal.pone.0089177 10.1371/journal.pone.0089177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [197].Joseph NP, Clark JA, Bauchner H, Walsh JP, Mercilus G, Figaro J, Bibbo C, Perkins RB. Knowledge, attitudes, and beliefs regarding HPV vaccination: ethnic and cultural differences between African-American and Haitian immigrant women. Womens Health Issues 2012;22(6): e571-9. https://doi.org/10.1016/j.whi.2012.09.003 10.1016/j.whi.2012.09.003 [DOI] [PubMed] [Google Scholar]
- [198].Joseph NP, Shea K, Porter CL, Walsh JP, Belizaire M, Estervine G, Perkins R. Factors Associated with Human Papillomavirus Vaccine Acceptance Among Haitian and African-American parents of Adolescent Sons. J Natl Med Assoc 2015;107(2):80-8. https://doi.org/10.1016/S0027-9684(15)30028-6 10.1016/S0027-9684(15)30028-6 [DOI] [PubMed] [Google Scholar]
- [199].Jung M, Lin L, Viswanath K. Associations between health communication behaviors, neighborhood social capital, vaccine knowledge, and parents’ H1N1 vaccination of their children. Vaccine 2013;31(42):4860-6. https://doi.org/10.1016/j.vaccine.2013.07.068 10.1016/j.vaccine.2013.07.068 [DOI] [PubMed] [Google Scholar]
- [200].Kadis JA, McRee AL, Gottlieb SL, Lee MR, Reiter PL, Dittus PJ, Brewer NT. Mothers’ support for voluntary provision of HPV vaccine in schools. Vaccine 2011;29(14):2542-7. https://doi.org/10.1016/j.vaccine.2011.01.067 10.1016/j.vaccine.2011.01.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [201].Kahn JA, Ding L, Huang B, Zimet GD, Rosenthal SL, Frazier AL. Mothers’ intention for their daughters and themselves to receive the human papillomavirus vaccine: a national study of nurses. Pediatrics 2009;123(6):1439-45. https://doi.org/10.1542/peds.2008-1536 10.1542/peds.2008-1536 [DOI] [PubMed] [Google Scholar]
- [202].Kalucka S, Lopata E. Age-conditioned differences in parents’ attitudes towards compulsory vaccination. Family Medicine and Primary Care Review 2016;18(4):425-8. [Google Scholar]
- [203].Katz ML, Kam JA, Krieger JL, Roberto AJ. Predicting human papillomavirus vaccine intentions of college-aged males: an examination of parents’ and son’s perceptions. J Am Coll Health 2012;60(6):449-59. https://doi.org/10.1080/07448481.2012.673523 10.1080/07448481.2012.673523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [204].Haesebaert J, Lutringer-Magnin D, Kalecinski J, Barone G, Jacquard AC, Leocmach Y, Regnier V, Vanhems P, Chauvin F, Lasset C. Disparities of perceptions and practices related to cervical cancer prevention and the acceptability of HPV vaccination according to educational level in a French cross-sectional survey of 18-65 years old women. PLoS One 2014;9(10):e109320 https://doi.org/10.1371/journal.pone.0109320 10.1371/journal.pone.0109320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [205].Kaya A, Altinel N, Karakaya G, Cetinkaya F. Knowledge and attitudes among patients with asthma and parents and physicians towards influenza vaccination. Allergol Immunopathol (Madr) 2017;45(3):240-3. https://doi.org/10.1016/j.aller.2016.08.003 10.1016/j.aller.2016.08.003 [DOI] [PubMed] [Google Scholar]
- [206].Kelley CA, Velazco CS, Delaney TV, Bensimhon A, Huang KN, Jarvis PR, Jolin JS, Schaberg KB, Burke M, Finley C, Carney JK. Factors contributing to suboptimal rates of childhood vaccinations in Vermont. J Child Health Care 2015;19(4):558-68. https://doi.org/10.1177/1367493514530955 10.1177/1367493514530955 [DOI] [PubMed] [Google Scholar]
- [207].Kempe A, Daley MF, Crane LA, Barrow J, Chandramouli V, Beaty BL, Allred NJ, Berman S. Misperceptions regarding influenza vaccine safety for individuals with chronic medical illness. Prev Med 2007;45(1):80-2. https://doi.org/10.1016/j.ypmed.2006.12.001 10.1016/j.ypmed.2006.12.001 [DOI] [PubMed] [Google Scholar]
- [208].Kennedy A, Basket M, Sheedy K. Vaccine attitudes, concerns, and information sources reported by parents of young children: results from the 2009 HealthStyles survey. Pediatrics. 2011;127 Suppl 1: S92-9. https://doi.org/10.1542/peds.2010-1722N 10.1542/peds.2010-1722N [DOI] [PubMed] [Google Scholar]
- [209].Kennedy A, Lavail K, Nowak G, Basket M, Landry S. Confidence about vaccines in the United States: understanding parents’ perceptions. Health Aff (Millwood) 2011;30(6):1151-9. https://doi.org/10.1377/hlthaff.2011.0396 10.1377/hlthaff.2011.0396 [DOI] [PubMed] [Google Scholar]
- [210].Kennedy AM, Brown CJ, Gust DA. Vaccine beliefs of parents who oppose compulsory vaccination. Public Health Rep 2005; 120(3):252-8. https://doi.org/10.1177/003335490512000306 10.1177/003335490512000306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [211].Kepka D, Ding Q, Bodson J, Warner EL, Mooney K. Latino Parents’ Awareness and Receipt of the HPV Vaccine for Sons and Daughters in a State with Low Three-Dose Completion. J Cancer Educ 2015;30(4):808-12. https://doi.org/10.1007/s13187-014-0781-0 10.1007/s13187-014-0781-0 [DOI] [PubMed] [Google Scholar]
- [212].Kepka D, Warner EL, Kinney AY, Spigarelli MG, Mooney K. Low human papillomavirus (HPV) vaccine knowledge among Latino parents in Utah. J Immigr Minor Health 2015;17(1): 125-31. https://doi.org/10.1007/s10903-014-0003-1 10.1007/s10903-014-0003-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [213].Kepka DL, Ulrich AK, Coronado GD. Low knowledge of the three-dose HPV vaccine series among mothers of rural Hispanic adolescents. J Health Care Poor Underserved 2012;23(2):626-35. https://doi.org/10.1353/hpu.2012.0040 10.1353/hpu.2012.0040 [DOI] [PubMed] [Google Scholar]
- [214].Kester LM, Zimet GD, Fortenberry JD, Kahn JA, Shew ML. A national study of HPV vaccination of adolescent girls: rates, predictors, and reasons for non-vaccination. Matern Child Health J 2013;17(5):879-85. https://doi.org/10.1007/s10995-012-1066-z 10.1007/s10995-012-1066-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- [215].Kettunen C, Nemecek J, Wenger O. Evaluation of low immunization coverage among the Amish population in rural Ohio. Am J Infect Control 2017;45(6):630-4. https://doi.org/10.1016/j.ajic.2017.01.032 10.1016/j.ajic.2017.01.032 [DOI] [PubMed] [Google Scholar]
- [216].Kim KM, Choi JS. Mothers’ intentions to vaccinate their teenaged children against human papillomavirus, as predicted by sex in South Korea: An application of the theory of planned behavior. Jpn J Nurs Sci 2017;14(4):288-96. https://doi.org/10.1111/jjns.12155 10.1111/jjns.12155 [DOI] [PubMed] [Google Scholar]
- [217].Kinder F. Parental Refusal of the Human Papillomavirus Vaccine. Journal of Pediatric Health Care 2016;30(6):551-7. [DOI] [PubMed] [Google Scholar]
- [218].Ko HS, Jo YS, Kim YH, Park YG, Wie JH, Cheon J, Moon HB, Lee Y, Shin JC. Knowledge and Acceptability about Adult Pertussis Immunization in Korean Women of Childbearing Age. Yonsei Med J 2015;56(4):1071-8. https://doi.org/10.3349/ymj.2015.56.4.1071 10.3349/ymj.2015.56.4.1071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [219].Kong KA, Yoon SH, Cho SJ, Kim HW, Kim KH. Public acceptance and willingness to hepatitis a vaccination in children aged 7-18 years in Republic of Korea. J Korean Med Sci 2014; 29(11):1528-35. https://doi.org/10.3346/jkms.2014.29.11.1528 10.3346/jkms.2014.29.11.1528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [220].Krawczyk A, Knauper B, Gilca V, Dube E, Perez S, Joyal-Desmarais K, Rosberger Z. Parents’ decision-making about the human papillomavirus vaccine for their daughters: I. Quantitative results. Hum Vaccin Immunother 2015;11(2):322-9. https://doi.org/10.1080/21645515.2014.1004030 10.1080/21645515.2014.1004030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [221].Krawczyk A, Perez S, King L, Vivion M, Dube E, Rosberger Z. Parents’ decision-making about the human papillomavirus vaccine for their daughters: II. Qualitative results. Hum Vaccin Immunother 2015;11(2):330-6. https://doi.org/10.4161/21645515.2014.980708 10.4161/21645515.2014.980708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [222].Krieger J, Kam J, Katz M, Roberto A. Does mother know best? An actor-partner model of college-age women’s human papillomavirus vaccination behavior. Human Communication Research, 2011;31(1):107-24. [Google Scholar]
- [223].Lavail KH, Kennedy AM. The role of attitudes about vaccine safety, efficacy, and value in explaining parents’ reported vaccination behavior. Health Educ Behav 2013;40(5):544-51. https://doi.org/10.1177/1090198112463022 10.1177/1090198112463022 [DOI] [PubMed] [Google Scholar]
- [224].Le Ngoc, Tho S, Ader F, Ferry T, Floret D, Arnal M, Fargeas S, Chidiac C, Valour F. Vaccination against serogroup B Neisseria meningitidis: Perceptions and attitudes of parents. Vaccine 2015; 33(30):3463-70. https://doi.org/10.1016/j.vaccine.2015.05.073 10.1016/j.vaccine.2015.05.073 [DOI] [PubMed] [Google Scholar]
- [225].Lechuga J, Swain G, Weinhardt LS. Perceived need of a parental decision aid for the HPV vaccine: content and format preferences. Health Promot Pract 2012;13(2):214-21. https://doi.org/10.1177/1524839910388622 10.1177/1524839910388622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [226].Lee KN, Chang KH, Cho SS, Park SH, Park ST. Attitudes Regarding HPV Vaccinations of Children among Mothers with Adolescent Daughters in Korea. J Korean Med Sci 2017;32(1): 130-4. https://doi.org/10.3346/jkms.2017.32.1.130 10.3346/jkms.2017.32.1.130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [227].Lee Mortensen G, Adam M, Idtaleb L. Parental attitudes towards male human papillomavirus vaccination: a pan-European cross-sectional survey. BMC Public Health 2015;15:624 https://doi.org/10.1186/s12889-015-1863-6 10.1186/s12889-015-1863-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [228].Lehmann BA, de Melker HE, Timmermans DRM, Mollema L. Informed decision making in the context of childhood immunization. Patient Educ Couns 2017;100(12):2339-45. https://doi.org/10.1016/j.pec.2017.06.015 10.1016/j.pec.2017.06.015 [DOI] [PubMed] [Google Scholar]
- [229].Lewis T, Osborn LM, Lewis K, Brockert J, Jacobsen J, Cherry JD. Influence of parental knowledge and opinions on 12-month diphtheria, tetanus, and pertussis vaccination rates. Am J Dis Child 1988;142(3):283-6. https://doi.org/10.1001/archpedi.1988.02150030053018 10.1001/archpedi.1988.02150030053018 [DOI] [PubMed] [Google Scholar]
- [230].Liao Q, Lam WW, Cowling BJ, Fielding R. Psychosocial Influences on Parental Decision-Making Regarding Vaccination Against Seasonal Influenza for Young Children in Hong Kong: a Longitudinal Study, 2012-2013. Int J Behav Med 2016;23(5): 621-34. https://doi.org/10.1007/s12529-016-9551-1 10.1007/s12529-016-9551-1 [DOI] [PubMed] [Google Scholar]
- [231].Lin CJ, Nowalk MP, Zimmerman RK, Ko FS, Zoffel L, Hoberman A, Kearney DH. Beliefs and attitudes about influenza immunization among parents of children with chronic medical conditions over a two-year period. J Urban Health 2006;83(5): 874-83. https://doi.org/10.1007/s11524-006-9084-z 10.1007/s11524-006-9084-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- [232].Linam WM, Gilliam CH, Honeycutt M, Wisdom C, Swearingen CJ, Romero JR. Parental perceptions about required influenza immunization of pediatric healthcare personnel. Infect Control Hosp Epidemiol 2014;35(10):1301-3. https://doi.org/10.1086/678061 10.1086/678061 [DOI] [PubMed] [Google Scholar]
- [233].Lindley MC, Jeyarajah J, Yankey D, Curtis CR, Markowitz LE, Stokley S. Comparing human papillomavirus vaccine knowledge and intentions among parents of boys and girls. Hum Vaccin Immunother 2016;12(6):1519-27. https://doi.org/10.1080/21645515.2016.1157673 10.1080/21645515.2016.1157673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [234].Livni G, Wainstein A, Birk E, Chodick G, Levy I. Influenza Vaccination Rate and Reasons for Nonvaccination in Children With Cardiac Disease. Pediatr Infect Dis J 2017;36(11):e268-e271. https://doi.org/10.1097/INF.0000000000001579 10.1097/INF.0000000000001579 [DOI] [PubMed] [Google Scholar]
- [235].Loke AY, Chan ACO, Wong YT. Facilitators and barriers to the acceptance of human papillomavirus (HPV) vaccination among adolescent girls: a comparison between mothers and their adolescent daughters in Hong Kong. BMC Res Notes 2017;10(1): 390 https://doi.org/10.1186/s13104-017-2734-2 10.1186/s13104-017-2734-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [236].Low MSF, Tan H, Hartman M, Tam CC, Hoo C, Lim J, Chiow S, Lee S, Thng R, Cai M, Tan Y, Lock J. Parental perceptions of childhood seasonal influenza vaccination in Singapore: A cross-sectional survey. Vaccine 2017;35(45):6096-102. https://doi.org/10.1016/j.vaccine.2017.09.060 10.1016/j.vaccine.2017.09.060 [DOI] [PubMed] [Google Scholar]
- [237].Luthy KE, Beckstrand RL, Callister LC. Parental hesitation in immunizing children in Utah. Public Health Nurs, 20 https://doi.org/10 27(1):25-31. https://doi.org/10.1111/j.1525-1446.2009.00823.x 10.1111/j.1525-1446.2009.00823.x [DOI] [PubMed] [Google Scholar]
- [238].Luthy KE, Beckstrand RL, Meyers CJ. Common perceptions of parents requesting personal exemption from vaccination. J Sch Nurs 2013;29(2):95-103. https://doi.org/10.1177/1059840512455365 10.1177/1059840512455365 [DOI] [PubMed] [Google Scholar]
- [239].Luthy KE, Beckstrand RL, Peterson NE. Parental hesitation as a factor in delayed childhood immunization. J Pediatr Health Care 2009;23(6):388-93. https://doi.org/10.1016/j.pedhc.2008.09.006 10.1016/j.pedhc.2008.09.006 [DOI] [PubMed] [Google Scholar]
- [240].Maayan-Metzger A, Kedem-Friedrich P, Kuint J. To vaccinate or not to vaccinate--that is the question: why are some mothers opposed to giving their infants hepatitis B vaccine? Vaccine,2005; 23(16):1941-8. https://doi.org/10.1016/j.vaccine.2004.10.015 10.1016/j.vaccine.2004.10.015 [DOI] [PubMed] [Google Scholar]
- [241].MacDonald SE, Schopflocher DP, Vaudry W. Parental concern about vaccine safety in Canadian children partially immunized at age 2: a multivariable model including system level factors. Hum Vaccin Immunother 2014;10(9):2603-11. https://doi.org/10.4161/21645515.2014.970075 10.4161/21645515.2014.970075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [242].MacDougall DM, Halperin BA, Langley JM, MacKinnon-Cameron D, Li L, Halperin SA. Maritime Universal Rotavirus Vaccination Program. Knowledge, attitudes, beliefs, and behaviors of parents and healthcare providers before and after implementation of a universal rotavirus vaccination program. Vaccine 2016; 34(5):687-95. https://doi.org/10.1016/j.vaccine.2015.09.089 10.1016/j.vaccine.2015.09.089 [DOI] [PubMed] [Google Scholar]
- [243].Madhivanan P, Li T, Srinivas V, Marlow L, Mukherjee S, Krupp K. Human papillomavirus vaccine acceptability among parents of adolescent girls: obstacles and challenges in Mysore, India. Prev Med 2014;64:69-74. https://doi.org/10.1016/j.ypmed.2014.04.002 10.1016/j.ypmed.2014.04.002 [DOI] [PubMed] [Google Scholar]
- [244].Mameli C, Faccini M, Mazzali C, Picca M, Colella G, Duca PG, Zuccotti GV. Acceptability of meningococcal serogroup B vaccine among parents and health care workers in Italy: a survey. Hum Vaccin Immunother 2014;10(10):3004-10. https://doi.org/10.4161/21645515.2014.971602 10.4161/21645515.2014.971602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [245].Marlow LA, Waller J, Wardle J. Trust and experience as predictors of HPV vaccine acceptance. Hum Vaccin 2007;3(5):171-5. https://doi.org/10.4161/hv.3.5.4310 10.4161/hv.3.5.4310 [DOI] [PubMed] [Google Scholar]
- [246].Marlow LA, Waller J, Wardle J. Parental attitudes to pre-pubertal HPV vaccination. Vaccine 2007;25(11):1945-52. https://doi.org/10.1016/j.vaccine.2007.01.059 10.1016/j.vaccine.2007.01.059 [DOI] [PubMed] [Google Scholar]
- [247].Marshall H, Clarke M, Sullivan T. Parental and community acceptance of the benefits and risks associated with meningococcal B vaccines. Vaccine 2014;32(3):338-44. https://doi.org/10.1016/j.vaccine.2013.11.042 10.1016/j.vaccine.2013.11.042 [DOI] [PubMed] [Google Scholar]
- [248].Marshall H, Ryan P, Roberton D, Baghurst P. A cross-sectional survey to assess community attitudes to introduction of Human papillomavirus vaccine. Aust N Z J Public Health 2007;31(3): 235-42. https://doi.org/10.1111/j.1467-842x.2007.00054.x 10.1111/j.1467-842x.2007.00054.x [DOI] [PubMed] [Google Scholar]
- [249].Mayet AY, Al-Shaikh GK, Al-Mandeel HM, Alsaleh NA, Hamad AF. Knowledge, attitudes, beliefs, and barriers associated with the uptake of influenza vaccine among pregnant women. Saudi Pharm J 2017;25(1):76-82. https://doi.org/10.1016/j.jsps.2015.12.001 10.1016/j.jsps.2015.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [250].McCauley MM, Kennedy A, Basket M, Sheedy K. Exploring the choice to refuse or delay vaccines: a national survey of parents of 6- through 23-month-olds. Acad Pediatr 2012;12(5): 375-83. https://doi.org/10.1016/j.acap.2012.06.007 10.1016/j.acap.2012.06.007 [DOI] [PubMed] [Google Scholar]
- [251].McHale P, Keenan A, Ghebrehewet S. Reasons for measles cases not being vaccinated with MMR: investigation into parents’ and carers’ views following a large measles outbreak. Epidemiol Infect 2016;144(4):870-5. https://doi.org/10.1017/S0950268815001909 10.1017/S0950268815001909 [DOI] [PubMed] [Google Scholar]
- [252].Melman ST, Nguyen TT, Ehrlich E, Schorr M, Anbar RD. Parental compliance with multiple immunization injections. Arch Pediatr Adolesc Med 1999;153(12):1289-91. https://doi.org/10.1001/archpedi.153.12.1289 10.1001/archpedi.153.12.1289 [DOI] [PubMed] [Google Scholar]
- [253].Meszaros JR, Asch DA, Baron J, Hershey JC, Kunreuther H, Schwartz-Buzaglo J. Cognitive processes and the decisions of some parents to forego pertussis vaccination for their children. J Clin Epidemiol 1996;49(6):697-703. https://doi.org/10.1016/0895-4356(96)00007-8 10.1016/0895-4356(96)00007-8 [DOI] [PubMed] [Google Scholar]
- [254].Michael CA, Ogbuanu IU, Storms AD, Ohuabunwo CJ, Corkum M, Ashenafi S, Achari P, Biya O, Nguku P, Mahoney F, Team NORS. An assessment of the reasons for oral poliovirus vaccine refusals in northern Nigeria. J Infect Dis. 2014;210 Suppl 1:S125-30. https://doi.org/10.1093/infdis/jiu436 10.1093/infdis/jiu436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [255].Michael EC, Olagbuji BN. Human papilloma virus vaccine: determinants of acceptability by mothers for adolescents in Nigeria. Afr J Reprod Health 2014;18(3):154-8. [PubMed] [Google Scholar]
- [256].Middleman AB, Guajardo AD, Sunwoo E, Sansaricq KM. Parent knowledge and attitudes about school-based hepatitis B immunization programs. J Sch Health 2002;72(8):348-51. https://doi.org/10.1111/j.1746-1561.2002.tb07923.x 10.1111/j.1746-1561.2002.tb07923.x [DOI] [PubMed] [Google Scholar]
- [257].Milteer RM, Jonna S. Parental reasons for delayed immunizations in children hospitalized in a Washington, DC, public hospital. J Natl Med Assoc 1996;88(7):433-6. [PMC free article] [PubMed] [Google Scholar]
- [258].Morales-Campos DY, Parra-Medina D. Predictors of Human Papillomavirus Vaccine Initiation and Completion Among Latino Mothers of 11- to 17-Year-Old Daughters Living Along the Texas-Mexico Border. Fam Community Health 2017;40(2): 139-49. https://doi.org/10.1097/FCH.0000000000000144 10.1097/FCH.0000000000000144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [259].Morhason-Bello IO, Wallis S, Adedokun BO, Adewole IF. Willingness of reproductive-aged women in a Nigerian community to accept human papillomavirus vaccination for their children. J Obstet Gynaecol Res 2015;41(10):1621-9. https://doi.org/10.1111/jog.12775 10.1111/jog.12775 [DOI] [PubMed] [Google Scholar]
- [260].Morrone T, Napolitano F, Albano L, Di Giuseppe G. Meningococcal serogroup B vaccine: Knowledge and acceptability among parents in Italy. Hum Vaccin Immunother 2017;13(8): 1921-7. https://doi.org/10.1080/21645515.2017.1313940 10.1080/21645515.2017.1313940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [261].Moulsdale P, Grant A, Fletcher M, Finn A. Parents’ perceptions of influenza and why they accept or decline the nasal vaccine for their child. Nurs Child Young People 2017;29(3):28-33. https://doi.org/10.7748/ncyp.2017.e854 10.7748/ncyp.2017.e854 [DOI] [PubMed] [Google Scholar]
- [262].Muhwezi WW, Banura C, Turiho AK, Mirembe F. Parents’ knowledge, risk perception and willingness to allow young males to receive human papillomavirus (HPV) vaccines in Uganda. PLoS One 2014;9(9):e106686 https://doi.org/10.1371/journal.pone.0106686 10.1371/journal.pone.0106686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [263].Murakami H, Kobayashi M, Hachiya M, Khan ZS, Hassan SQ, Sakurada S. Refusal of oral polio vaccine in northwestern Pakistan: a qualitative and quantitative study. Vaccine 2014;32(12): 1382-7. https://doi.org/10.1016/j.vaccine.2014.01.018 10.1016/j.vaccine.2014.01.018 [DOI] [PubMed] [Google Scholar]
- [264].My C, Danchin M, Willaby HW, Pemberton S, Leask J. Parental attitudes, beliefs, behaviours and concerns towards childhood vaccinations in Australia: A national online survey. Aust Fam Physician 2017;46(3):145-51. [PubMed] [Google Scholar]
- [265].Naeem M, Adil M, Abbas SH, Khan MZ, Naz SM, Khan A, Khan MU. Coverage and causes of missed oral polio vaccine in urban and rural areas of Peshawar. J Ayub Med Coll Abbottabad 2011;23(4):98-102. [PubMed] [Google Scholar]
- [266].Naeem M, Khan MZ, Abbas SH, Adil M, Khan MU, Naz SM. Factors associated with low hepatitis B vaccination; a user and provider perspective study in Peshawar. J Pak Med Assoc 2011;61(11):1125-7. [PubMed] [Google Scholar]
- [267].Namuigi P, Phuanukoonnon S. Barriers to measles immunization: the beliefs and attitudes of caregivers in Goroka, Eastern Highlands Province, Papua New Guinea. P N G Med J,2005; 48(3-4):183-7. [PubMed] [Google Scholar]
- [268].Niederhauser VP, Markowitz M. Barriers to immunizations: Multiethnic parents of under- and unimmunized children speak. J Am Acad Nurse Pract 2007;19(1):15-23. https://doi.org/10.1111/j.1745-7599.2006.00185.x 10.1111/j.1745-7599.2006.00185.x [DOI] [PubMed] [Google Scholar]
- [269].Oladokun RE, Adedokun BO, Lawoyin TO. Children not receiving adequate immunization in Ibadan, Nigeria: what reasons and beliefs do their mothers have? Niger J Clin Pract 20 https://doi.org/10 13(2):173-8. [PubMed] [Google Scholar]
- [270].Onnela JP, Landon BE, Kahn AL, Ahmed D, Verma H, O’Malley AJ, Bahl S, Sutter RW, Christakis NA. Polio vaccine hesitancy in the networks and neighborhoods of Malegaon, India. Soc Sci Med 2016;153:99-106. https://doi.org/10.1016/j.socscimed.2016.01.024 10.1016/j.socscimed.2016.01.024 [DOI] [PubMed] [Google Scholar]
- [271].Oria PA, Arunga G, Lebo E, Wong JM, Emukule G, Muthoka P, Otieno N, Mutonga D, Breiman RF, Katz MA. Assessing parents’ knowledge and attitudes towards seasonal influenza vaccination of children before and after a seasonal influenza vaccination effectiveness study in low-income urban and rural Kenya, 2010-2011. BMC Public Health 2013;13:391 https://doi.org/10.1186/1471-2458-13-391 10.1186/1471-2458-13-391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [272].Ozawa S, Wonodi C, Babalola O, Ismail T, Bridges J. Using best-worst scaling to rank factors affecting vaccination demand in northern Nigeria. Vaccine 2017;35(47):6429-37. https://doi.org/10.1016/j.vaccine.2017.09.079 10.1016/j.vaccine.2017.09.079 [DOI] [PubMed] [Google Scholar]
- [273].Paek HJ, Shin KA, Park K. Determinants of caregivers’ vaccination intention with respect to child age group: a cross-sectional survey in South Korea. BMJ Open 2015;5(9):e008342 https://doi.org/10.1136/bmjopen-2015-008342 10.1136/bmjopen-2015-008342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [274].Painter JE, Gargano LM, Sales JM, Morfaw C, Jones LM, Murray D, Di Clemente RJ, Hughes JM. Correlates of 2009 H1N1 influenza vaccine acceptability among parents and their adolescent children. Health Educ Res 2011;26(5):751-60. https://doi.org/10.1093/her/cyr025 10.1093/her/cyr025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [275].Parrella A, Gold M, Marshall H, Braunack-Mayer A, Baghurst P. Parental perspectives of vaccine safety and experience of adverse events following immunisation. Vaccine 2013. 31(16): 2067-74. https://doi.org/10.1016/j.vaccine.2013.02.011 10.1016/j.vaccine.2013.02.011 [DOI] [PubMed] [Google Scholar]
- [276].Parrella A, Gold M, Marshall H, Braunack-Mayer A, Watson M, Baghurst P. Parental views on vaccine safety and future vaccinations of children who experienced an adverse event following routine or seasonal influenza vaccination in 20 https://doi.org/10 Hum Vaccin Immunother 2012;8(5):662-7. https://doi.org/10.4161/hv.19478 10.4161/hv.19478 [DOI] [PubMed] [Google Scholar]
- [277].Paulussen TG, Hoekstra F, Lanting CI, Buijs GB, Hirasing RA. Determinants of Dutch parents’ decisions to vaccinate their child. Vaccine 2006;24(5):644-51. https://doi.org/10.1016/j.vaccine.2005.08.053 10.1016/j.vaccine.2005.08.053 [DOI] [PubMed] [Google Scholar]
- [278].Peleg N, Zevit N, Shamir R, Chodick G, Levy I. Seasonal influenza vaccination rates and reasons for non-vaccination in children with gastrointestinal disorders. Vaccine 2015;33(1):182-6. https://doi.org/10.1016/j.vaccine.2014.10.086 10.1016/j.vaccine.2014.10.086 [DOI] [PubMed] [Google Scholar]
- [279].Pelucchi C, Esposito S, Galeone C, Semino M, Sabatini C, Picciolli I, Consolo S, Milani G, Principi N. Knowledge of human papillomavirus infection and its prevention among adolescents and parents in the greater Milan area, Northern Italy. BMC Public Health 2010;10:378 https://doi.org/10.1186/1471-2458-10-378 10.1186/1471-2458-10-378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [280].Perez S, Shapiro GK, Tatar O, Joyal-Desmarais K, Rosberger Z. Development and Validation of the Human Papillomavirus Attitudes and Beliefs Scale in a National Canadian Sample. Sex Transm Dis 2016;43(10):626-32. https://doi.org/10.1097/OLQ.0000000000000506 10.1097/OLQ.0000000000000506 [DOI] [PubMed] [Google Scholar]
- [281].Perez S, Tatar O, Gilca V, Shapiro GK, Ogilvie G, Guichon J, Naz A, Rosberger Z. Untangling the psychosocial predictors of HPV vaccination decision-making among parents of boys. Vaccine 2017;35(36):4713-21. https://doi.org/10.1016/j.vaccine.2017.07.043 10.1016/j.vaccine.2017.07.043 [DOI] [PubMed] [Google Scholar]
- [282].Perez S, Tatar O, Ostini R, Shapiro GK, Waller J, Zimet G, Rosberger Z. Extending and validating a human papillomavirus (HPV) knowledge measure in a national sample of Canadian parents of boys. Prev Med 2016;91:43-49. https://doi.org/10.1016/j.ypmed.2016.07.017 10.1016/j.ypmed.2016.07.017 [DOI] [PubMed] [Google Scholar]
- [283].Perez S, Tatar O, Shapiro GK, Dube E, Ogilvie G, Guichon J, Gilca V, Rosberger Z. Psychosocial determinants of parental human papillomavirus (HPV) vaccine decision-making for sons: Methodological challenges and initial results of a pan-Canadian longitudinal study. BMC Public Health 2016;16(1):1223 https://doi.org/10.1186/s12889-016-3828-9 10.1186/s12889-016-3828-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [284].Podolsky R, Cremer M, Atrio J, Hochman T, Arslan AA. HPV vaccine acceptability by Latino parents: a comparison of U.S. and Salvadoran populations. J Pediatr Adolesc Gynecol 2009; 22(4):205-15. https://doi.org/10.1016/j.jpag.2008.05.010 10.1016/j.jpag.2008.05.010 [DOI] [PubMed] [Google Scholar]
- [285].Pot M, van Keulen HM, Ruiter RAC, Eekhout I, Mollema L, Paulussen T. Motivational and contextual determinants of HPV-vaccination uptake: A longitudinal study among mothers of girls invited for the HPV-vaccination. Prev Med 2017;100: 41-49. https://doi.org/10.1016/j.ypmed.2017.04.005 10.1016/j.ypmed.2017.04.005 [DOI] [PubMed] [Google Scholar]
- [286].Reiter PL, Katz ML, Paskett ED. Correlates of HPV vaccination among adolescent females from Appalachia and reasons why their parents do not intend to vaccinate. Vaccine 2013;31(31): 3121-5. https://doi.org/10.1016/j.vaccine.2013.04.068 10.1016/j.vaccine.2013.04.068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [287].Restivo V, Napoli G, Marsala MG, Bonanno V, Sciuto V, Amodio E, Calamusa G, Vitale F, Firenze A. Factors associated with poor adherence to MMR vaccination in parents who follow vaccination schedule. Hum Vaccin Immunother 2015;11(1): 140-5. https://doi.org/10.4161/hv.34416 10.4161/hv.34416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [288].Roberts JR, Thompson D, Rogacki B, Hale JJ, Jacobson RM, Opel DJ, Darden PM. Vaccine hesitancy among parents of adolescents and its association with vaccine uptake. Vaccine 2015; 33(14):1748-55. https://doi.org/10.1016/j.vaccine.2015.01.068 10.1016/j.vaccine.2015.01.068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [289].Robitz R, Gottlieb SL, De Rosa CJ, Guerry SL, Liddon N, Zaidi A, Walker S, Smith JS., Brewer N.T., Markowitz L.E., Parent attitudes about school requirements for human papillomavirus vaccine in high-risk communities of Los Angeles, California. Cancer Epidemiol Biomarkers Prev 2011;20(7):1421-9. https://doi.org/10.1158/1055-9965.EPI-10-1236 10.1158/1055-9965.EPI-10-1236 [DOI] [PubMed] [Google Scholar]
- [290].Rogers C. Parents’ vaccine beliefs: a study of experiences and attitudes among parents of children in private pre-schools. R I Med J (2013), 2014;97(4):27-30. [PubMed] [Google Scholar]
- [291].Ruffin MTT, Hade EM, Gorsline MR, DeGraffinreid CR, Katz ML, Kobrin SC, Paskett ED. Human papillomavirus vaccine knowledge and hypothetical acceptance among women in Appalachia Ohio. Vaccine 2012;30(36):5349-57. https://doi.org/10.1016/j.vaccine.2012.06.034 10.1016/j.vaccine.2012.06.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [292].Salmon DA, Moulton LH, Omer SB, DeHart MP, Stokley S, Halsey NA. Factors associated with refusal of childhood vaccines among parents of school-aged children: a case-control study. Arch Pediatr Adolesc Med 2005;159(5) 470-6. https://doi.org/10.1001/archpedi.159.5.470 10.1001/archpedi.159.5.470 [DOI] [PubMed] [Google Scholar]
- [293].Salmon DA, Sotir MJ, Pan WK, Berg JL, Omer SB, Stokley S, Hopfensperger DJ, Davis JP, Halsey NA. Parental vaccine refusal in Wisconsin: a case-control study. WMJ, 2009;108(1):17-23. [PMC free article] [PubMed] [Google Scholar]
- [294].Sam IC, Wong LP, Rampal S, Leong YH, Pang CF, Tai YT, Tee HC, Kahar-Bador M. Maternal acceptance of human papillomavirus vaccine in Malaysia. J Adolesc Health 2009;44(6) 610-2. https://doi.org/10.1016/j.jadohealth.2008.11.014 10.1016/j.jadohealth.2008.11.014 [DOI] [PubMed] [Google Scholar]
- [295].Sampson R, Wong L. Macvicar R. Parental reasons for non-uptake of influenza vaccination in young at-risk groups: a qualitative study. Br J Gen Pract 2011;61(588):e386-91. https://doi.org/10.3399/bjgp11X583155 10.3399/bjgp11X583155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [296].Rickert VI, Rehm SJ, Aalsma MC, Zimet GD. The role of parental attitudes and provider discussions in uptake of adolescent vaccines. Vaccine 2015;33(5):642-7. https://doi.org/10.1016/j.vaccine.2014.12.016 10.1016/j.vaccine.2014.12.016 [DOI] [PubMed] [Google Scholar]
- [297].Rose SB, Lawton BA, Lanumata TS, Hibma M, Baker MG. Predictors of intent to vaccinate against HPV/cervical cancer: a multi-ethnic survey of 769 parents in New Zealand. N Z Med J 2012;125(1350):51-62. [PubMed] [Google Scholar]
- [298].Santibanez TA, Kennedy ED. Reasons given for not receiving an influenza vaccination, 2011-12 influenza season, United States. Vaccine 2016;34(24):2671-8. https://doi.org/10.1016/j.vaccine.2016.04.039 10.1016/j.vaccine.2016.04.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [299].Saqer A, Ghazal S, Barqawi H, Babi JA, Al Khafaji R, Elmekresh MM. Knowledge and Awareness about Cervical Cancer Vaccine (HPV) Among Parents in Sharjah. Asian Pac J Cancer Prev 2017;18(5):1237-41. https://doi.org/10.22034/APJCP.2017.18.5.1237 10.22034/APJCP.2017.18.5.1237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [300].Schollin Ask L, Hjern A, Lindstrand A, Olen O, Sjogren E, Blennow M, Ortqvist A. Receiving early information and trusting Swedish child health centre nurses increased parents’ willingness to vaccinate against rotavirus infections. Acta Paediatr 2017;106(8):1309-16. https://doi.org/10.1111/apa.13872 10.1111/apa.13872 [DOI] [PubMed] [Google Scholar]
- [301].Schwarz NG, Gysels M, Pell C, Gabor J, Schlie M, Issifou S, Lell B, Kremsner PG, Grobusch MP, Pool R. Reasons for non-adherence to vaccination at mother and child care clinics (MCCs) in Lambarene, Gabon. Vaccine 2009;27(39):5371-5. https://doi.org/10.1016/j.vaccine.2009.06.100 10.1016/j.vaccine.2009.06.100 [DOI] [PubMed] [Google Scholar]
- [302].Selmouni F, Zidouh A, Nejjari C, Bekkali R. Acceptability of the human papilloma virus vaccine among Moroccan parents: a population-based crosssectional study. East Mediterr Health J 2015;21(8):555-63. https://doi.org/10.26719/2015.21.8.555 10.26719/2015.21.8.555 [DOI] [PubMed] [Google Scholar]
- [303].Sengupta B, Sinha RN, Sarkar GN, Biswas AB, Mukherjee KL. Perception and practice regarding pulse polio immunisation in an urban community of Calcutta. J Indian Med Assoc 1998;96(8):247-8. [PubMed] [Google Scholar]
- [304].Seven M, Guvenc G, Sahin E, Akyuz A. Attitudes to HPV Vaccination among Parents of Children Aged 10 to 13 Years. J Pediatr Adolesc Gynecol 2015;28(5):382-6. https://doi.org/10.1016/j.jpag.2014.11.005 10.1016/j.jpag.2014.11.005 [DOI] [PubMed] [Google Scholar]
- [305].Shao SJ, Nurse C, Michel L, Joseph MA, Suss AL. Attitudes and Perceptions of the Human Papillomavirus Vaccine in Caribbean and African American Adolescent boys and Their Parents. J Pediatr Adolesc Gynecol 2015;28(5): 373-7. https://doi.org/10.1016/j.jpag.2014.11.003 10.1016/j.jpag.2014.11.003 [DOI] [PubMed] [Google Scholar]
- [306].Shapiro GK, Holding A, Perez S, Amsel R, Rosberger Z. Validation of the vaccine conspiracy beliefs scale. Papillomavirus Res 2016;2:167-72. https://doi.org/10.1016/j.pvr.2016.09.001 10.1016/j.pvr.2016.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [307].Shapiro GK, Perez S, Naz A, Tatar O, Guichon JR, Amsel R, Zimet GD, Rosberger Z. Investigating Canadian parents’ HPV vaccine knowledge, attitudes and behaviour: a study protocol for a longitudinal national online survey. BMJ Open 2017; 7(10):e017814 https://doi.org/10.1136/bmjopen-2017-017814 10.1136/bmjopen-2017-017814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [308].Shawn DH, Gold R. Survey of parents’ attitudes to the recommended Haemophilus influenzae type b vaccine program. CMAJ 1987;136(10):1038-40. [PMC free article] [PubMed] [Google Scholar]
- [309].Sheikh A, Iqbal B, Ehtamam A, Rahim M, Shaikh HA, Usmani HA, Nasir J, Ali S, Zaki M, Wahab TA, Wasim W, Aftab AA. Reasons for non-vaccination in pediatric patients visiting tertiary care centers in a polio-prone country. Arch Public Health 2013;71(1):19 https://doi.org/10.1186/0778-7367-71-19 10.1186/0778-7367-71-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [310].Shuaib FM, Kimbrough D, Roofe M, McGwin GJr, Jolly P. Factors associated with incomplete childhood immunization among residents in St. Mary, Jamaica. West Indian Med J 2010;59(5):549-54. [PMC free article] [PubMed] [Google Scholar]
- [311].Skinner J, March L, Simpson JM. A retrospective cohort study of childhood immunisation status in northern Sydney. Aust J Public Health 1995;19(1):58-63. https://doi.org/10.1111/j.1753-6405.1995.tb00298.x 10.1111/j.1753-6405.1995.tb00298.x [DOI] [PubMed] [Google Scholar]
- [312].Smailbegovic MS, Laing GJ, Bedford H. Why do parents decide against immunization? The effect of health beliefs and health professionals. Child Care Health Dev 2003;29(4):303-11. https://doi.org/10.1046/j.1365-2214.2003.00347.x 10.1046/j.1365-2214.2003.00347.x [DOI] [PubMed] [Google Scholar]
- [313].Smith MJ, Woods CR, Marshall GS. Parental vaccine concerns in Kentucky. J Ky Med Assoc 2009;107(9):342-9. [PubMed] [Google Scholar]
- [314].Smith PJ, Humiston SG, Marcuse EK, Zhao Z, Dorell CG, Howes C, Hibbs B. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the Health Belief Model. Public Health Rep. 2011;126 Suppl 2:135-46. https://doi.org/10.1177/00333549111260S215 10.1177/00333549111260S215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [315].Smith PJ, Humiston SG, Parnell T, Vannice KS, Salmon DA. The association between intentional delay of vaccine administration and timely childhood vaccination coverage. Public Health Rep 2010;125(4):534-41. https://doi.org/10.1177/003335491012500408 10.1177/003335491012500408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [316].Smith PJ, Kennedy AM, Wooten K, Gust DA, Pickering LK. Association between health care providers’ influence on parents who have concerns about vaccine safety and vaccination coverage. Pediatrics 2006;118(5):e1287-92. https://doi.org/10.1542/peds.2006-0923 10.1542/peds.2006-0923 [DOI] [PubMed] [Google Scholar]
- [317].Smith PJ, Marcuse EK, Seward JF, Zhao Z, Orenstein WA. Children and Adolescents Unvaccinated Against Measles: Geographic Clustering, Parents’ Beliefs, and Missed Opportunities. Public Health Rep 2015;130(5):485-504. https://doi.org/10.1177/003335491513000512 10.1177/003335491513000512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [318].Smith PJ, Stokley S, Bednarczyk RA, Orenstein WA, Omer SB. HPV vaccination coverage of teen girls: the influence of health care providers. Vaccine 2016;34(13):1604-10. https://doi.org/10.1016/j.vaccine.2016.01.061 10.1016/j.vaccine.2016.01.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [319].Sohail M, Mahmood B, Asim M. Mother’s Knowledge, Attitude and Practices about child immunization: A study in district Faisalabad, Pakistan. Rawal Medical Journal 2015;40(4): 441-4. [Google Scholar]
- [320].Songthap A, Pitisuttithum P, Kaewkungwal J, Fungladda W, Bussaratid V. Knowledge, attitudes, and acceptability of a human papilloma virus vaccine among students, parents and teachers in Thailand. Southeast Asian J Trop Med Public Health 2012;43(2):340-53. [PubMed] [Google Scholar]
- [321].Soyer OU, Hudaverdiyev S, Civelek E, Isik E, Karabulut E, Kocabas C, Sekerel BE. Parental perspectives on influenza vaccination in children with asthma. Pediatr Pulmonol 2011;46(2): 139-44. https://doi.org/10.1002/ppul.21332 10.1002/ppul.21332 [DOI] [PubMed] [Google Scholar]
- [322].Staras SA, Vadaparampil ST, Patel RP, Shenkman EA. Parent perceptions important for HPV vaccine initiation among low income adolescent girls. Vaccine 2014;32(46):6163-9. https://doi.org/10.1016/j.vaccine.2014.08.054 10.1016/j.vaccine.2014.08.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [323].Steel Fisher GK, Blendon RJ, Guirguis S, Brule A, Lasala-Blanco N, Coleman M, Petit V, Ahmed M, Mataruse N, Corkum M, Nisar M, Ben-Porath EN, Gigli S, Sahm C. Threats to polio eradication in high-conflict areas in Pakistan and Nigeria: a polling study of caregivers of children younger than 5 years. Lancet Infect Dis 2015;15(10):1183-92. https://doi.org/10.1016/S1473-3099(15)00178-4 10.1016/S1473-3099(15)00178-4 [DOI] [PubMed] [Google Scholar]
- [324].Stefanoff P, Mamelund SE, Robinson M, Netterlid E, Tuells J, Bergsaker MA, Heijbel H, Yarwood J, Europe V. Tracking parental attitudes on vaccination across European countries: The Vaccine Safety, Attitudes, Training and Communication Project (VACSATC). Vaccine 2010;28(35):5731-7. https://doi.org/10.1016/j.vaccine.2010.06.009 10.1016/j.vaccine.2010.06.009 [DOI] [PubMed] [Google Scholar]
- [325].Stein Zamir C, Israeli A. Knowledge, Attitudes and Perceptions About Routine Childhood Vaccinations Among Jewish Ultra-Orthodox Mothers Residing in Communities with Low Vaccination Coverage in the Jerusalem District. Matern Child Health J 2017;21(5):1010-17. https://doi.org/10.1007/s10995-017-2272-5 10.1007/s10995-017-2272-5 [DOI] [PubMed] [Google Scholar]
- [326].Stephenson JD. Survey of parents’ attitudes to the recommended Haemophilus influenzae type b vaccine program. CMAJ, 1987;137(5):371-2. [PMC free article] [PubMed] [Google Scholar]
- [327].Stockwell MS, Irigoyen M, Andres Martinez R, Findley SE. Failure to return: parental, practice, and social factors affecting missed immunization visits for urban children. Clin Pediatr (Phila), 2014; 53(5): 420-7. https://doi.org/10.1177/0009922814527497 10.1177/0009922814527497 [DOI] [PubMed] [Google Scholar]
- [328].Strelitz B. Gritton J, Klein EJ, Bradford MC, Follmer K, Zerr DM, Englund JA, Opel DJ. Parental vaccine hesitancy and acceptance of seasonal influenza vaccine in the pediatric emergency department. Vaccine 2015;33(15):1802-7. https://doi.org/10.1016/j.vaccine.2015.02.034 10.1016/j.vaccine.2015.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [329].Stretch R, Roberts SA, McCann R, Baxter D, Chambers G, Kitchener H, Brabin L. Parental attitudes and information needs in an adolescent HPV vaccination programme. Br J Cancer 2008;99(11):1908-11. https://doi.org/10.1038/sj.bjc.6604766 10.1038/sj.bjc.6604766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [330].Suarez-Castaneda E, Pezzoli L, Elas M, Baltrons R, Crespin-Elias EO, Pleitez OA, de Campos MI, Danovaro-Holliday MC. Routine childhood vaccination programme coverage, El Salvador, 2011-In search of timeliness. Vaccine 2014;32(4):437-44. https://doi.org/10.1016/j.vaccine.2013.11.072 10.1016/j.vaccine.2013.11.072 [DOI] [PubMed] [Google Scholar]
- [331].Sundaram SS, Roberts C, Rowen D, Patel R. Parental attitudes towards the human papillomavirus vaccine in ethnic minorities: a community survey. Int J STD AIDS 2010;21(6):449 https://doi.org/10.1258/ijsa.2010.010105 10.1258/ijsa.2010.010105 [DOI] [PubMed] [Google Scholar]
- [332].Tadesse H, Deribew A, Woldie M. Predictors of defaulting from completion of child immunization in south Ethiopia, May 2008: a case control study. BMC Public Health,2009;9:150 https://doi.org/10.1186/1471-2458-9-150 10.1186/1471-2458-9-150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [333].Tagbo BN, Ughasoro MD, Esangbedo DO. Parental acceptance of inactivated polio vaccine in Southeast Nigeria: a qualitative cross-sectional interventional study. Vaccine 2014;32(46): 6157-62. https://doi.org/10.1016/j.vaccine.2014.08.053 10.1016/j.vaccine.2014.08.053 [DOI] [PubMed] [Google Scholar]
- [334].Taiwo L, Idris S, Abubakar A, Nguku P, Nsubuga P, Gidado S, Okeke L, Emiasegen S, Waziri E. Factors affecting access to information on routine immunization among mothers of under 5 children in Kaduna State Nigeria, 2015. Pan Afr Med J 2017; 27:186 https://doi.org/10.11604/pamj.2017.27.186.11191 10.11604/pamj.2017.27.186.11191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [335].Takahashi K, Kanda H, Kim JY. Reasons for Non-vaccination among Patients Who Acquired Measles: Lessons from the Local Measles Epidemics in Japan. West Indian Med J 2014;63(6): 647-9. https://doi.org/10.7727/wimj.2013.310 10.7727/wimj.2013.310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [336].Tam WW, Chan J, Lo KK, Lee A, Chan PK, Chan D, Nelson EA. Parental Attitudes and Factors Associated With Varicella Vaccination in Preschool and Schoolchildren in Hong Kong: A Cross-Sectional Study. Medicine (Baltimore) 2015;94(36): e1519 https://doi.org/10.1097/MD.0000000000001519 10.1097/MD.0000000000001519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [337].Tan TQ, Gerbie MV. Perception, Awareness, and Acceptance of Human Papillomavirus Disease and Vaccine Among Parents of Boys Aged 9 to 18 Years. Clin Pediatr (Phila) 2017;56(8):737-43. https://doi.org/10.1177/0009922816682788 10.1177/0009922816682788 [DOI] [PubMed] [Google Scholar]
- [338].Tang C, Huang S, Weng K, Ger L, Hsieh K. Parents’ views about the vaccination program in Taiwan. Pediatrics and neonatology 2011;52(2):98-102 [DOI] [PubMed] [Google Scholar]
- [339].Taylor JA, Cufley D. The association between parental health beliefs and immunization status among children followed by private pediatricians. Clin Pediatr (Phila) 1996;35(1):18-22. https://doi.org/10.1177/000992289603500104 10.1177/000992289603500104 [DOI] [PubMed] [Google Scholar]
- [340].Taylor JA, Darden PM, Brooks DA, Hendricks JW, Wasserman RC, Bocian AB. Pediatric Research in Office, S., and National Medical, A., Association between parents’ preferences and perceptions of barriers to vaccination and the immunization status of their children: a study from Pediatric Research in Office Settings and the National Medical Association. Pediatrics, 2002;110(6):1110-6. https://doi.org/10.1542/peds.110.6.1110 10.1542/peds.110.6.1110 [DOI] [PubMed] [Google Scholar]
- [341].Thomas T, Blumling A, Delaney A. The Influence of Religiosity and Spirituality on Rural Parents’ Health Decision Making and Human Papillomavirus Vaccine Choices. ANS Adv Nurs Sci 2015;38(4):E1-E12. https://doi.org/10.1097/ANS.0000000000000094 10.1097/ANS.0000000000000094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [342].Thomas TL, Strickland OL, Di Clemente R, Higgins M, Haber M. Rural African American parents’ knowledge and decisions about human papillomavirus vaccination. J Nurs Scholarsh 2012;44(4):358-67. https://doi.org/10.1111/j.1547-5069.2012.01479.x 10.1111/j.1547-5069.2012.01479.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [343].Thomas TL, Strickland OL, Di Clemente R, Higgins M, Williams B, Hickey K. Parental Human Papillomavirus Vaccine Survey (PHPVS): nurse-led instrument development and psychometric testing for use in research and primary care screening. J Nurs Meas 2013;21(1):96-109. https://doi.org/10.1891/1061-3749.21.1.96 10.1891/1061-3749.21.1.96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [344].Thomas TL, Strickland OL, Higgins M. Mothers, Fathers, Sons, and Human Papillomavirus Immunization Practices. Fam Community Health,2017;40(3):278-87. https://doi.org/10.1097/FCH.0000000000000104 10.1097/FCH.0000000000000104 [DOI] [PubMed] [Google Scholar]
- [345].Thompson EL, Rosen BL, Vamos CA, Kadono M, Daley EM. Human Papillomavirus Vaccination: What Are the Reasons for Nonvaccination Among U.S. Adolescents? J Adolesc Health 2017;61(3):288-93. https://doi.org/10.1016/j.jadohealth.2017.05.015 10.1016/j.jadohealth.2017.05.015 [DOI] [PubMed] [Google Scholar]
- [346].Tisi G, Salinaro F, Apostoli P, Bassani R, Bellicini A, Groppi L, Donarini P, Pecorelli S. HPV vaccination acceptability in young boys. Ann Ist Super Sanita 2013;49(3):286-91. https://doi.org/10.4415/ANN_13_03_09 10.4415/ANN_13_03_09 [DOI] [PubMed] [Google Scholar]
- [347].Taylor JA, Newman RD. Parental attitudes toward varicella vaccination. The Puget Sound Pediatric Research Network. Arch Pediatr Adolesc Med 2000;154(3):302-6. https://doi.org/10.1001/archpedi.154.3.302 10.1001/archpedi.154.3.302 [DOI] [PubMed] [Google Scholar]
- [348].Wright RA, Battaglia M, Wilkinson M, Huggins VJ, Abt Associates. The National Immunization Survey: design of a study on knowledge, attitudes, and practices (NIS-KAP). Proceedings of the section on Survey Research Methods, Indianapolis. American Statistical Association, 2000:697–702. [Google Scholar]
- [349].Streng A, Seeger K, Grote V, Liese JG. Varicella vaccination coverage in Bavaria (Germany) after general vaccine recommendation in 2004. Vaccine 20 https://doi.org/10 28(35): 5738-45. https://doi.org/10.1016/j.vaccine.2010.06.007 10.1016/j.vaccine.2010.06.007 [DOI] [PubMed] [Google Scholar]
- [350].Opel DJ, Taylor JA, Mangione-Smith R, Solomon C, Zhao C, Catz S, Martin D. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine 2011;29(38):6598-605. https://doi.org/10.1016/j.vaccine.2011.06.115 10.1016/j.vaccine.2011.06.115 [DOI] [PubMed] [Google Scholar]
- [351].Austin Z, Sutton J. Qualitative research: getting started. Can J Hosp Pharm 2014;67(6):436-40. https://doi.org/10.4212/cjhp.v67i6.1406 10.4212/cjhp.v67i6.1406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [352].Gianfredi V, Nucci D, Salvatori T, Orlacchio F, Villarini M, Moretti M. PErCEIVE IN UMBRIA STUDY GROUP. “PErCEIVE in Umbria”: evaluation of anti-influenza vaccination’s perception among Umbrian pharmacists. J Prev Med Hyg 2018;59(1):E14-E19. https://doi.org/10.15167/2421-4248/jpmh2018.59.1.806 10.15167/2421-4248/jpmh2018.59.1.806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [353].Meadows KA. So you want to do research? 5: Questionnaire design. Br J Community Nurs 2003;8(12):562-70. https://doi.org/10.12968/bjcn.2003.8.12.11854 10.12968/bjcn.2003.8.12.11854 [DOI] [PubMed] [Google Scholar]
- [354].Keszei A.P., Novak M., Streiner D.L. Introduction to health measurement scales. J Psychosom Res 20 https://doi.org/10 68(4): 319-23. https://doi.org/10.1016/j.jpsychores.2010.01.006 10.1016/j.jpsychores.2010.01.006 [DOI] [PubMed] [Google Scholar]
- [355].Tabacchi G, Costantino C, Napoli G, Marchese V, Cracchiolo M, Casuccio A, Vitale FThe Esculapio Working Group. Determinants of European parents’ decision on the vaccination of their children against measles, mumps and rubella: A systematic review and meta-analysis. Hum Vaccin Immunother 2016;12(7): 1909-23. https://doi.org/10.1080/21645515.2016.1151990 10.1080/21645515.2016.1151990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [356].Gualano MR, Bert F, Voglino G, Buttinelli E, D’Errico MM, De Waure C, Di Giovanni P, Fantini MP, Giuliani AR, Marranzano M, Masanotti G, Massimi A, Nante N, Pennino F, Squeri R, Stefanati A, Signorelli C, Siliquini R. Attitudes towards compulsory vaccination in Italy: Results from the NAVIDAD multicentre study. Vaccine 2018;36(23):3368-3374. https://doi.org/10.1016/j.vaccine.2018.04.029 10.1016/j.vaccine.2018.04.029 [DOI] [PubMed] [Google Scholar]
- [357].Gualano MR, Olivero E, Voglino G, Corezzi M, Rossello P, Vicentini C, Bert F, Siliquini R. Knowledge, attitudes and beliefs towards compulsory vaccination: a systematic review. Hum Vaccin Immunother 2019;15(4):918-31. https://doi.org/10.1080/21645515.2018.1564437 10.1080/21645515.2018.1564437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [358].Gianfredi V, D’Ancona F, Maraglino F, Cenci C, Iannazzo S. Polio and measles: reasons of missed vaccination in Italy, 2015-2017. Ann Ig 2019;31(3):191-201. https://doi.org/10.7416/ai.2019.2282 10.7416/ai.2019.2282 [DOI] [PubMed] [Google Scholar]
- [359].Gianfredi V, Grisci C, Nucci D, Parisi V, Moretti M. [Communication in health.]. Recenti Prog Med 2018;109(7):374-83. https://doi.org/10.1701/2955.29706 10.1701/2955.29706 [DOI] [PubMed] [Google Scholar]
- [360].Gianfredi V, Odone A, Fiacchini D, Rosselli R, Battista T, Signorelli C. Trust and reputation management, branding, social media management nelle organizzazioni sanitarie: sfide e opportunità per la comunità igienistica italiana. J Prev Med Hyg 2019;60(3):E108-E109. [Google Scholar]
- [361].Bragazzi NL, Barberis I, Rosselli R, Gianfredi V, Nucci D, Moretti M, Salvatori T, Martucci G, Martini M. How often people google for vaccination: Qualitative and quantitative insights from a systematic search of the web-based activities using Google Trends. Hum Vaccin Immunother 2017;13(2):464-9. https://doi.org/10.1080/21645515.2017.1264742 10.1080/21645515.2017.1264742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [362].Bragazzi NL, Gianfredi V, Villarini M, Rosselli R, Nasr A, Hussein A, Martini M, Behzadifar M. Vaccines Meet Big Data: State-of-the-Art and Future Prospects. From the Classical 3Is (“Isolate-Inactivate-Inject”) Vaccinology 1.0 to Vaccinology 3.0, Vaccinomics, and Beyond: A Historical Overview. Front Public Health 2018;6:62 https://doi.org/10.3389/fpubh.2018.00062 10.3389/fpubh.2018.00062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [363].Gianfredi V, Bragazzi NL, Mahamid M, Bisharat B, Mahroum N, Amital H, Adawi M. Monitoring public interest toward pertussis outbreaks: an extensive Google Trends-based analysis. Public Health 2018;165:9-15. https://doi.org/10.1016/j.puhe.2018.09.001 10.1016/j.puhe.2018.09.001 [DOI] [PubMed] [Google Scholar]
- [364].Kazi AM, Khalid W. Questionnaire designing and validation. J Pak Med Assoc 2012;62(5):514-6. [PubMed] [Google Scholar]
- [365].Gianfredi V, Nucci D, Ceccarelli F, Villarini M, Moretti M. PILATES (Physical Activity and Diet Survey): An Italian Self-Administered Questionnaire Evaluating Diet Habits of Gym-Goers. Validation Process. J Diet Suppl 2019;16(3):307-17. https://doi.org/10.1080/19390211.2018.1456501 10.1080/19390211.2018.1456501 [DOI] [PubMed] [Google Scholar]
- [366].Nucci D, Licitra L, Sciara S, Moretti M, Gianfredi V. PRuNUS: design and validation of a questionnaire among prisoners - data of pilot study in the Penitentiary Institute of Perugia, Italy. Int J Prison Health 2019;16(2):165-83. https://doi.org/10.1108/IJPH-01-2019-0001 10.1108/IJPH-01-2019-0001 [DOI] [PubMed] [Google Scholar]
- [367].Cuda A, Gentile L, Voglino G, Gianfredi V. Gruppo di lavoro Vaccini e Vaccine Hesitancy Consulta degli Specializzandi, SII, [Design and validation of a questionnaire for assessing Public Health residents’ opinions and knowledge regarding the new mandatory vaccination law in Italy (DL 73/2017)]. Ig Sanita Pubbl,2018;74(2):137-52. [PubMed] [Google Scholar]
- [368].Derrough T, Olsson K, Gianfredi V, Simondon F, Heijbel H, Danielsson N, Kramarz P, Pastore-Celentano L. Immunisation Information Systems - useful tools for monitoring vaccination programmes in EU/EEA countries, 2016. Euro Surveill 2017;22(17). https://doi.org/10.2807/1560-7917.ES.2017.22.17.30519 10.2807/1560-7917.ES.2017.22.17.30519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [369].Gianfredi V, Balzarini F, Gola M, Mangano S, Carpagnano LF, Colucci ME, Gentile L, Piscitelli A, Quattrone F, Scuri S, Mantovani LG, Auxilia F, Castaldi S, Capolongo S, Pelissero G, Odone A, Signorelli C. Leadership in Public Health: Opportunities for Young Generations Within Scientific Associations and the Experience of the “Academy of Young Leaders”. Front Public Health 2019;7:378 https://doi.org/10.3389/fpubh.2019.00378 10.3389/fpubh.2019.00378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [370].Gianfredi V, Moretti M, Lopalco PL. Countering vaccine hesitancy through immunization information systems, a narrative review. Hum Vaccin Immunother 2019;1-19. https://doi.org/10.1080/21645515.2019.1599675 10.1080/21645515.2019.1599675 [DOI] [PMC free article] [PubMed] [Google Scholar]


