Summary
Background
Hemodialysis patients are at a high risk for morbidity and mortality. This study aimed to find the predictors of mortality and survival in hemodialysis patients in Hamadan province of Iran.
Methods
A number of 785 patients during the entire 10 years were enrolled into this historical cohort study. Data were gathered by a checklist of hospital records. The survival time was the time between the start of hemodialysis treatment to patient’s death as the end point. Random survival forests (RSF) method was used to identify the main predictors of survival among the patients.
Results
The median survival time was 613 days. The number of 376 deaths was occurred. The three most important predictors of survival were hemoglobin, CRP and albumin. RSF method predicted survival better than the conventional Cox-proportional hazards model (out-of-bag C-index of 0.808 for RSF vs. 0.727 for Cox model).
Conclusions
We found that positivity of CRP, low serum albumin and low serum hemoglobin were the top three most important predictors of low survival for HD patients
Keywords: Hemodialysis, Kidney Failure, Survival, Random Survival Forest
Introduction
Globally, chronic kidney disease (CKD) is an important health challenge with an alarming increase in incidence as well as prevalence [1]. CKD patients have a lower survival rate, and no significant improvement has been achieved on their survival over the past two decades [2]. In Iran, unlike some other countries, hemodialysis (HD) is the main way of renal replacement therapy in end stage renal disease (ESRD) patients [3]. Limited studies have been conducted in Iran regarding the survival of HD patients, suggesting a low survival rate for these patients [4, 5].
Common independent predictors of survival in HD patients are: age, race, albumin and hemoglobin levels, etiology of kidney failure and presence of certain comorbidities [3, 6-9]. Apart from these accepted prognostic factors, the role of some factors such as dialysis frequency is controversial on morbidity and mortality among hemodialysis patients [10].
In general, the interaction occurs when the effect of one risk factor is dependent on the presence of another risk factor [11]. When resources are limited, assessing interactions provides insight into the mechanisms for the outcome and identifying subgroups would benefit most from interventions [11, 12]. Interactions between some variables like three-way interaction between protein-energy wasting (PEW), inflammation and cardiovascular diseases (CVD) [13], interaction between albumin and phosphor [14] and three-way interaction between BMI, physical activity and smoking [15] on HD patients survival were shown previously. However, the lack of knowledge in this regard is still high.
Identification of survival modifiable factors and interactions between them could help in prioritizing the clinical care of HD patients. Evidences regarding the survival rate of hemodialysis patients in developing countries are rare and most of these studies were conducted in developed countries where patients have more access to health cares, and their results cannot be generalized to developing countries. Therefore, in the present study, we aimed to investigate the survival rate and it`s correlates in HD patients in Hamadan province using random survival forests.
Material and methods
STUDY DESIGN
We performed a retrospective cohort study to investigate predictors of mortality among hemodialysis patients.
STUDY SETTINGS
We examined data on 758 patients who underwent hemodialysis treatment in Hamadan province in western Iran from March 2007 to March 2017. Hamadan province, with an area of 19,493 square kilometers in extent, is located in western Iran. According to the national census held by the Statistical Center of Iran, Hamadan province had a population of 1,758,268 people in 2011. We used information of patients from eight hospitals in the province with a dialysis wards, including: Alimoradian, Besat, Vali-asr, Ghaem, Imam Hossein, Valiasr, Imam Reza, and Shahid-Beheshti in Nahavand, Hamadan, Tuyserkan, Asadabad, Malayer, Razan, Kabudarahang and Hamadan city, respectively.
ELIGIBILITY CRITERIA
All ESRD patients who initiated chronic hemodialysis programs at the dialysis units of the above mentioned hospitals during 2007 to 2017 were considered as inclusion criteria. Patients with acute renal failure or under treatment with peritoneal dialysis, patients on transient hemodialysis and patients with incomplete medical records were excluded from study.
CLINICAL AND DEMOGRAPHIC MEASURES
Data were gathered by a checklist on hospital records of all HD patients in the province. The checklist used in this study included characteristics related to demographic profiles (age (year), gender (male, female), marital status (married, single, divorce, widow), BMI (kg/m2), residence area (urban, rural), educational level (illiterate, primary, guidance, high school, academic), the history of tobacco use (yes, no) and substance abuse (yes, no)), and clinical information (including Hemoglobin (g/dl), BUN (mg/dL), Creatinine (mg/dL), CRP status (positive, negative), Sodium (mEq/L), Calcium (mg/dL), Phosphor (mg/dL), iPTH (pg/ml), Albumin (g/dl) and ESRD cause (Hypertension, Diabetes, Urologic& obstructive diseases, Polycystic Kidney, Glomerulonephritis, Un-Known)). The clinical and laboratory information of patients at the beginning of their treatment and before receiving the first dialysis treatment was gathered. In order to minimize measurement variability, all two baseline measures (two last measurements before the first dialysis treatment) for each patient were averaged. These records were collected by reviewing patients’ medical records.
OUTCOME
We considered the end point of the patients’ follow up as their death. The survival time was the time between the start of HD treatment to patients death. Patients with renal transplantation, or withdrawal of dialysis, or unable to follow them due to transferred another dialysis facility out of province as well as, patients who died because of injury or accident, or other causes unrelated to renal failure were considered as censored cases.
STATISTICAL ANALYSIS
We utilized the random survival forest (RF) method that ensembles binary decision trees and extends the RF regression model to right-censored survival data. In this technique, a random bootstrap sample (containing two thirds of the original data on average) is drawn for every decision tree. Thus, the remaining one third of the data known as out-of-bag (OOB) data is excluded. Decision trees are grown based on the bootstrap samples by applying a random node splitting process which works as follows: At each node random candidate variables (mtry determined by the square root of the total number of variables) are selected for random node splitting. Then the variable that maximizes the survival differences between two daughter nodes (determined by a splitting rule like the log-rank statistic) for a special split point is selected for node splitting. The growth of a decision tree is stopped when all the terminal nodes contain only a predefined minimal number of unique events.
To comparison, the stepwise Cox proportional hazards model was used. So, the Harrell’s concordance index (C-index) criterion was utilized [16] using out-of-bag (OOB) data. The minimal depths of the covariates were obtained to select predictive variables. Minimal depth is a dimensionless order statistic that measures the predictiveness of a variable in a tree. It can be used to select variables in high-dimensional problems. It assesses the predictiveness of a variable by a depth calculation relative to the root node of a tree. The smaller the minimal depth, the more predictive the variable.
Analyses were performed by using “randomForestSRC”, a freely available package from the Comprehensive R Archive Network (CRAN).
Results
Descriptive statistics of the characteristics of the patients were presented in Tab. I. According to the table, the majority of the patients were male (54.9%), married (79.1%), non-smoker (76.7%), non-substance abused, illiterate (54.9%) and lived in rural area (65.6%). About 47.8% of the patients experienced death. The median survival time was 613 days. The mean and standard deviation of other variables were reported in Table I.
Tab. I.
Descriptive statistics of characteristics related to participants.
| Variable | Frequency (%) | Variable | Frequency (%)/Mean (SD) |
|---|---|---|---|
| Gender | ESRD cause | ||
| Male | 431 (54.9) | Hypertension | 222 (28.3) |
| Female | 354 (45.1) | Diabetes | 193 (24.6) |
| Marital status | Urologic& obstructive diseases | 75 (9.6) | |
| Married | 621 (79.1) | Polycystic Kidney | 35 (4.5) |
| Single | 81 (10.3) | Glomerulonephritis | 56 (7.1) |
| Divorce | 11 (1.4) | Diabetes and Hypertension | 79 (10.1) |
| Widow | 72 (9.2) | Unknown | - |
| The history of tobacco use | |||
| Yes | 183 (23.3) | BMI (kg/m2) | 23.10 (3.97) |
| No | 602 (76.7) | Hemoglobin (g/dl) | 10.49 (1.92) |
| Substance abuse | Creatinine (mg/dL) | 7.85 (3.18) | |
| Yes | 121 (15.4) | Sodium (mEq/L) | 138.88 (7.24) |
| No | 664 (84.6) | Calcium (mg/dL) | 8.71 (0.86) |
| Residence area | Phosphor (mg/dL) | 5.11 (1.58) | |
| Urban | 487 (62) | Iron | 99.89 (97.58) |
| Rural | 298 (38) | Albumin (g/dl) | 3.69 (0.72) |
| CRP status | |||
| Positive | 270 (34.4) | ||
| Negative | 515 (65.6) | ||
| Education | |||
| Illiterate | 415 (52.9) | ||
| Primary school | 229 (29.2) | ||
| High school | 114 (14.5) | ||
| Academic | 27 (3.4) | ||
Figure 1 shows the minimal depth of the variables obtained from RSF. According to the figure, hemoglobin, CRP, albumin, age at diagnosis and iron were highly predictive and URR, uric acid, dialysis weekly time, PLT, Na, P, Ca, K, HCT, ALK and vascular access were moderately predictive. Moreover, other used variables were unlikely to be predictive. According to the stepwise Cox PH model, the variables of age at diagnosis, marriage status, BMI, addiction, hemoglobin, iron, albumin and CRP were selected as the most important variables (Tab. II). The performance of the RSF was assessed using Harrel’s C-index and compared with the stepwise Cox PH. According to the results, the RSF had a higher c-index (0.808) compared with the Cox model (0.727).
Fig. 1.
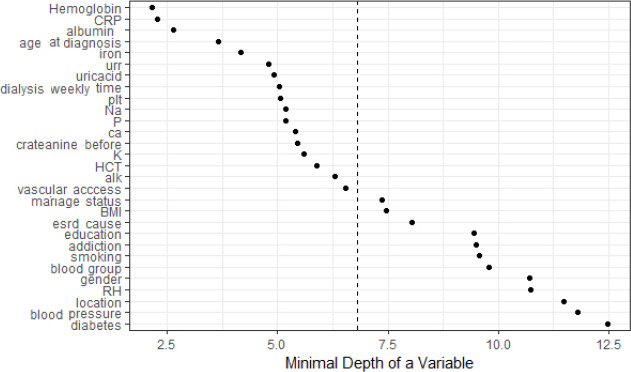
Minimal depth of variables affecting survival of HD patients obtained using random survival forest.
Tab. II.
The results of stepwise Cox proportional Hazards in selecting predictors affecting survival time of HD patients in Hamadan Province from 2007 to 2017.
| Variables | B | SE | P.Value | Exp(B) | 95% CI for Exp(B) | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Age at diagnosis | -0.023 | 0.006 | < 0.001 | 0.977 | 0.966 | 0.988 | |
| Marriage status | Married | 1.000 | |||||
| Single | -1.423 | 0.615 | 0.021 | 0.241 | 0.072 | 0.804 | |
| Divorce | -0.174 | 0.464 | 0.707 | 0.840 | 0.338 | 2.085 | |
| Widow | 0.308 | 0.486 | 0.526 | 1.361 | 0.525 | 3.525 | |
| Location | Urban | 1.000 | |||||
| Rural | -0.220 | 0.110 | 0.046 | 0.803 | 0.647 | 0.996 | |
| BMI status | < 18.5 kg/m2 | 1.000 | 0.010 | ||||
| 18.5-25 kg/m2 | 1.000 | 0.303 | 0.001 | 2.719 | 1.500 | 4.926 | |
| 25-30 kg/m2 | 0.663 | 0.250 | 0.008 | 1.941 | 1.190 | 3.165 | |
| > 30 kg/m2 | 0.740 | 0.265 | 0.005 | 2.096 | 1.247 | 3.523 | |
| Addiction | Yes | 1.000 | |||||
| No | -0.326 | 0.136 | 0.017 | 0.722 | 0.552 | 0.942 | |
| Hemoglobin | -0.203 | 0.030 | < 0.001 | 0.816 | 0.769 | 0.866 | |
| Iron | -0.003 | 0.001 | < 0.001 | 0.997 | 0.996 | 0.999 | |
| Albumin | -0.421 | 0.070 | < 0.001 | 0.656 | 0.572 | 0.753 | |
| CRP | -1.157 | 0.119 | < 0.001 | 0.314 | 0.249 | 0.397 |
The effects of the most four influential variables found in the RSF with 5-year partial survival plots analysis were demonstrated in Figure 2. The estimated partial survival for a variable shows the estimated survival for different levels of the variable when the effects of all other variables are justified. For example, patients with negative CRP shower a higher 5-year predicted survival compared with those with positive CRP. The non-linear nature of the selected variables is evident from the figure. For example, as hemoglobin increases up to about 10 (g/dl (the five-year predicted survival increases very slightly and it tends to increase dramatically after that point up to.
Fig. 2.
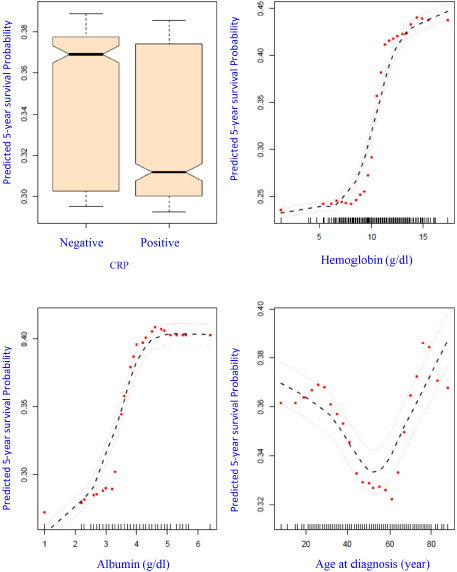
Partial 5-year predicted survival for four most influential variables on survival in HD data. Dashed red lines are ± 2 standard error bars (red dots indicates the estimated survival at the observed levels of each correlate and the black hatches are the smoothed curves based on the loess curves for the estimated survival for each individual.
Figure 3 displays interaction between the three important variables of CRP, hemoglobin, and Albumin on 5 year predicted survival. Patients with positive CRP and hemoglobin values lower than 11 have the worst survival (see the first row, second column) and most had low albumin. Survival was best for patients with negative CRP and hemoglobin ≥ 11 (see second row, first column) and further dependent on changes in albumin.
Fig. 3.
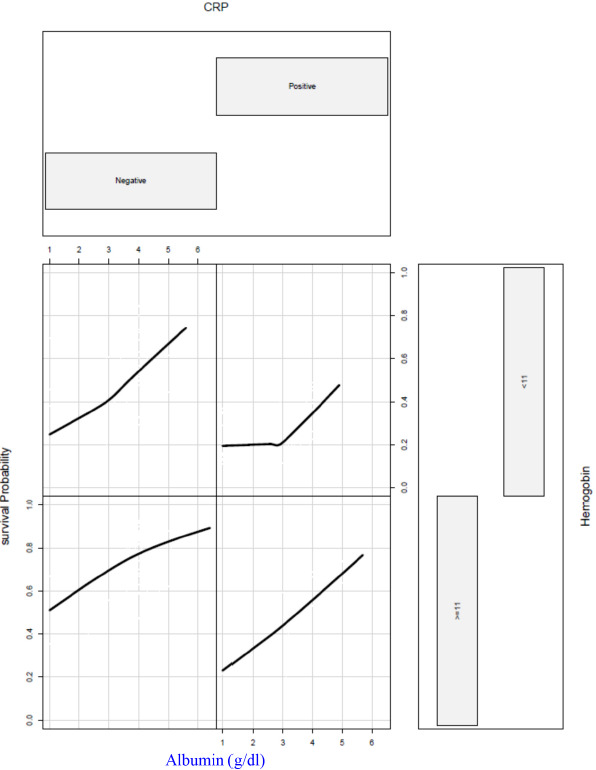
Random survival forest estimated five-year survival as a function of CRP, Hemoglobin, and Albumin. Smoothed curves are loess curves of the estimated survival for each individual.
In this group the 5 years predicted survival was over 70% for those with albumin values greater than 4, but only about 50% for those with albumin of 1 (g/dl). It is important to note that these interactions and non-linear relationships were identified by the random survival forest, and not prespecified by the analyst. The median survival time in the two categories of low Hemoglobin/positive CRP and high Hemoglobin/negative CRP were 5.38 and 40.53 months, respectively.
Discussion
Hemodialysis is a common treatment modality for ESRD patients in Iran. In this study we investigated the predictors of survival in HD patients. The findings of this study can be used to improve quality of cares provided for the HD patients and better resource allocation. We found that hemoglobin level, albumin level, and CRP status were the top three most important predictors of survival for HD patients in the present study.
Along with the results of this study, the role of low hemoglobin level in increasing the risk of mortality in HD patients has been shown in previous studies [17, 18]. Anemia is one of the main risk factors in the development of left ventricular hypertrophy (LVH), and consequence cardiac mortality and morbidity in ESRD patients [19]. Early management of anemia is associated with reduction in the severity of comorbid conditions and can slow the progression to renal failure [20]. Robert et al. showed that normalization of hemoglobin through preventing the development of LV dilation, leads to improved quality of life of HD patients [21].
In agreement with our finding, other studies results indicated that low serum albumin is one of the main predictors of poor survival in HD patients [22, 23]. Hypo-albuminemia usually considered as the proxy of malnutrition. Mafra et al. in a Brazilian cohort of hemodialysis patients found that both low BMI and hypo-albuminemia are strong predictors of death [24]. Combe et al. showed that a decrease in serum albumin over time correlated with increased CVD death [25].
One of the other main predictors of mortality in HD patients in this study was CRP status. Similar findings have been obtained in other studies [26, 27]. Lseki et al. in their study showed that regardless of serum albumin and other possible confounders, CRP is a significant predictor of death in HD patients [28]. Inflammation usually is in relation with insulin resistance, oxidative stress, wasting, infections and endothelial dysfunction [29].
Interactions between some modifiable variables on survival of HD patients were seen previously [13, 15]. We found that the combined effect of CRP status with serum Hemoglobin and CRP status has the significant effect on the survival of HD patients. This finding is important because HD patients with a high mortality risk can be identified through regular screening. More studies are needed to determine multiple pathophysiological pathways may underlie these combined effects.
This study had some limitations as well. First, because of the retrospective design of the study, verifying quality control of the data was not possible. Second, the addiction and smoking status of patients was based on their self-report and therefore was prone to information bias and finally quality of the services and technology may vary over time, and also the quality of service provision in the dialysis wards of hospitals is not the same, which could not be considered in this study. Despite these limitations there was strength for this study which was the utilization of the RSF to analyze the data set. RSF can handle the issues with the traditional Cox model like proportionality assumption automatically. This will help analysts to deal with the relationships (i.e. linear, nonlinear) between variables over time without any previous knowledge.
Conclusions
We found that higher levels of CRP, low serum albumin and low serum hemoglobin were the top three most important predictors of poor survival for HD patients.
Figures and tables
Acknowledgement
This study was approved by the Ethics Committee of Hamadan University of Medical Sciences. The Authors would like to thank all contributors and participants who make this study project possible as well as the personnel of the hemodialysis wards in hospitals of Hamadan province for their kind collaboration.
Funding sources: this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Conflict of interest statement
The authors declare no conflict of interest.
Authors’ contributions
SK and LT are responsible for the design of the study. They analyzed the data and wrote the paper. VSH and EJ dealt with the collection of information. All authors reviewed and approved the final version of the manuscript.
References
- [1].Grassmann A, Gioberge S, Moeller S, Brown G. ESRD patients in 2004: global overview of patient numbers, treatment modalities and associated trends. Nephrol Dial Transplant 2005;20:2587-93. https://doi.org/10.1093/ndt/gfi159 10.1093/ndt/gfi159 [DOI] [PubMed] [Google Scholar]
- [2].Collins AJ, Foley RN, Herzog C, Chavers B, Gilbertson D, Ishani A, Kasiske B, Liu J, Mau LW, McBean M, Murray A, St Peter W, Guo H, Gustafson S, Li Q, Li S, Li S, Peng Y, Qiu Y, Roberts T, Skeans M, Snyder J, Solid C, Wang C, Weinhandl E, Zaun D, Arko C, Chen SC, Dalleska F, Daniels F, Dunning S, Ebben J, Frazier E, Hanzlik C, Johnson R, Sheets D, Wang X, Forrest B, Constantini E, Everson S, Eggers P, Agodoa L. US renal data system 2010 annual data report. Am J Kidney Dis 2011;1(57):A8, e1-526. 10.1053/j.ajkd.2010.10.007 [DOI] [PubMed] [Google Scholar]
- [3].Mafra D, Farage NE, Azevedo DL, Viana GG, Mattos JP, Velarde LGC, Fouque D. Impact of serum albumin and body-mass index on survival in hemodialysis patients. Int Urol Nephrol 2007;39:619-24. https://doi.org/10.1007/s11255-007-9201-2 10.1007/s11255-007-9201-2 [DOI] [PubMed] [Google Scholar]
- [4].Mousavi SSB, Hayati F, Ansari MJA, Valavi E, Cheraghian B, Shahbazian H, et al. Survival at 1, 3, and 5 years in diabetic and nondiabetic patients on hemodialysis. Iran J Kidney Dis 2010;4:74. [PubMed] [Google Scholar]
- [5].Montaseri M, Yazdani Cherat J, Espahbodi F, Mousavi SJ. Five-year survival rate in hemodialysis patients Attending Sari Imam Khomeini Hospital. Journal of Mazandaran University of Medical Sciences 2013;23(101):78-85. [Google Scholar]
- [6].Bleyer AJ, Tell GS, Evans GW, Ettinger WH, Burkart JM. Survival of patients undergoing renal replacement therapy in one center with special emphasis on racial differences. Am J Kidney Dis 1996;28:72-81. https://doi.org/10.1016/s0272-6386(96)90133-x 10.1016/s0272-6386(96)90133-x [DOI] [PubMed] [Google Scholar]
- [7].Brodowska-Kania D, Rymarz A, Gibin K. First year survival of patients on maintenance dialysis treatment in Poland. Nagoya J Med Sci 2015;77:629. [PMC free article] [PubMed] [Google Scholar]
- [8].Akizawa T, Saito A, Gejyo F, Suzuki M, Nishizawa Y, Tomino Y, omino Y, Tsubakihara Y, Akiba T, Hirakata H, Watanabe Y, Kawanishi H, Bessho M, Udagawa Y, Aoki K, Uemura Y, Ohashi Y, JET Study Group Low hemoglobin levels and hypo-responsiveness to erythropoiesis-stimulating agent associated with poor survival in incident japanese hemodialysis patients. Ther Apher Dial 2014;18:404-13. https://doi.org/10.1111/1744-9987.12155 10.1111/1744-9987.12155 [DOI] [PubMed] [Google Scholar]
- [9].Iseki K, Tozawa M, Takishita S. Effect of the duration of dialysis on survival in a cohort of chronic haemodialysis patients. Nephrol Dial Transplant 2003;18:782-7. https://doi.org/10.1093/ndt/gfg145 10.1093/ndt/gfg145 [DOI] [PubMed] [Google Scholar]
- [10].Slinin Y, Greer N, Ishani A, MacDonald R, Olson C, Rutks I, Wilt TJ. Timing of dialysis initiation, duration and frequency of hemodialysis sessions, and membrane flux: a systematic review for a KDOQI clinical practice guideline. Am J Kidney Dis 2015;66:823-36. https://doi.org/10.1053/j.ajkd.2014.11.031 10.1053/j.ajkd.2014.11.031 [DOI] [PubMed] [Google Scholar]
- [11].VanderWeele TJ, Knol MJ. A tutorial on interaction. Epidemiologic Methods. 2014;3:33-72. [Google Scholar]
- [12].de González AB, Cox DR. Interpretation of interaction: a review. Ann Appl Stat 2007;1:371-85. [Google Scholar]
- [13].de Mutsert R, Grootendorst DC, Axelsson J, Boeschoten EW, Krediet RT, Dekker FW, NECOSAD Study Group Excess mortality due to interaction between protein-energy wasting, inflammation and cardiovascular disease in chronic dialysis patients. Nephrol Dial Transplant 2008;23:2957-64. https://doi.org/10.1093/ndt/gfn167 10.1093/ndt/gfn167 [DOI] [PubMed] [Google Scholar]
- [14].Zitt E, Lamina C, Sturm G, Knoll F, Lins F, Freistätter O, Kronenberg F, Lhotta K, Neyer U. Interaction of time-varying albumin and phosphorus on mortality in incident dialysis patients. Clin J Am Soc Nephrol 2011;6:2650-6. https://doi.org/10.2215/CJN.03780411 10.2215/CJN.03780411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Hallan S, de Mutsert R, Carlsen S, Dekker FW, Aasarød K, Holmen J. Obesity, smoking, and physical inactivity as risk factors for CKD: are men more vulnerable? Am J Kidney Dis 2006;47:396-405. https://doi.org/10.1053/j.ajkd.2005.11.027 10.1053/j.ajkd.2005.11.027 [DOI] [PubMed] [Google Scholar]
- [16].Harrell FE, Jr., Califf RM, Pryor DB, Lee KL, Rosati RA. Evaluating the yield of medical tests. JAMA 1982;247:2543-6. [PubMed] [Google Scholar]
- [17].Regidor DL, Kopple JD, Kovesdy CP, Kilpatrick RD, McAllister CJ, Aronovitz J, Greenland S, Kalantar-Zadeh K. Associations between changes in hemoglobin and administered erythropoiesis-stimulating agent and survival in hemodialysis patients. J Am Soc Nephrol 2006;17:1181-91. https://doi.org/10.1681/ASN.2005090997 10.1681/ASN.2005090997 [DOI] [PubMed] [Google Scholar]
- [18].Gilbertson DT, Ebben JP, Foley RN, Weinhandl ED, Bradbury BD, Collins AJ. Hemoglobin level variability: associations with mortality. Clin J Am Soc Nephrol 2008;3:133-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Berweck S, Hennig L, Sternberg C, Dingerkus H, Ludat K, Hampl H. Cardiac mortality prevention in uremic patients. Therapeutic strategies with particular attention to complete correction of renal anemia. Clin Nephrol 2000;53(1 Suppl):S80-5. [PubMed] [Google Scholar]
- [20].Kausz AT, Khan SS, Abichandani R, Kazmi WH, Obrador GT, Ruthazer R, Pereira BJ. Management of patients with chronic renal insufficiency in the Northeastern United States. J Am Soc Nephrol 2001;12:1501-7. [DOI] [PubMed] [Google Scholar]
- [21].Ofsthun N, Labrecque J, Lacson E, Keen M, Lazarus JM. The effects of higher hemoglobin levels on mortality and hospitalization in hemodialysis patients. Kidney Int 2003;63:1908-14. https://doi.org/10.1046/j.1523-1755.2003.00937.x 10.1046/j.1523-1755.2003.00937.x [DOI] [PubMed] [Google Scholar]
- [22].Kalantar-Zadeh K, Supasyndh O, Lehn RS, McAllister CJ, Kopple JD. Normalized protein nitrogen appearance is correlated with hospitalization and mortality in hemodialysis patients with Kt/V greater than 1.20. J Ren Nutr 2003;13:15-25. https://doi.org/10.1053/jren.2003.50005 10.1053/jren.2003.50005 [DOI] [PubMed] [Google Scholar]
- [23].Kalantar-Zadeh K, Kilpatrick RD, Kuwae N, McAllister CJ, Alcorn H, Jr, Kopple JD, Greenland S. Revisiting mortality predictability of serum albumin in the dialysis population: time dependency, longitudinal changes and population-attributable fraction. Nephrol Dial Transplant 2005;20:1880-8. https://doi.org/10.1093/ndt/gfh941 10.1093/ndt/gfh941 [DOI] [PubMed] [Google Scholar]
- [24].Mafra D, Farage NE, Azevedo DL, Viana GG, Mattos JP, Velarde LG, Fouque D. Impact of serum albumin and body-mass index on survival in hemodialysis patients. Int Urol Nephrol 2007;39:619-24. https://doi.org/10.1007/s11255-007-9201-2 10.1007/s11255-007-9201-2 [DOI] [PubMed] [Google Scholar]
- [25].Combe C, Chauveau P, Laville M, Fouque D, Azar R, Cano N, Canaud B, Roth H, Leverve X, Aparicio M, French Study Group Nutrition in Dialysis Influence of nutritional factors and hemodialysis adequacy on the survival of 1,610 French patients. Am J Kidney Dis 2001;37:S81-S8. https://doi.org/10.1053/ajkd.2001.20756 10.1053/ajkd.2001.20756 [DOI] [PubMed] [Google Scholar]
- [26].Yeun JY, Levine RA, Mantadilok V, Kaysen GA. C-reactive protein predicts all-cause and cardiovascular mortality in hemodialysis patients. Am J Kidney Dis 2000;35:469-76. https://doi.org/10.1016/s0272-6386(00)70200-9 10.1016/s0272-6386(00)70200-9 [DOI] [PubMed] [Google Scholar]
- [27].de Filippi C, Wasserman S, Rosanio S, Tiblier E, Sperger H, Tocchi M, Christenson R, Uretsky B, Smiley M, Gold J, Muniz H, Badalamenti J, Herzog C, Henrich W. Cardiac troponin T and C-reactive protein for predicting prognosis, coronary atherosclerosis, and cardiomyopathy in patients undergoing long-term hemodialysis. JAMA 2003;290:353-9. https://doi.org/10.1001/jama.290.3.353 10.1001/jama.290.3.353 [DOI] [PubMed] [Google Scholar]
- [28].Iseki K, Tozawa M, Yoshi S, Fukiyama K. Serum C-reactive protein (CRP) and risk of death in chronic dialysis patients. Nephrol Dial Transplant 1999;14:1956-60. https://doi.org/10.1093/ndt/14.8.1956 10.1093/ndt/14.8.1956 [DOI] [PubMed] [Google Scholar]
- [29].Furuland H, Linde T, Ahlmén J, Christensson A, Strömbom U, Danielson BG. A randomized controlled trial of haemoglobin normalization with epoetin alfa in pre-dialysis and dialysis patients. Nephrol Dial Transplant 2003;18:353-61. https://doi.org/10.1093/ndt/18.2.353 10.1093/ndt/18.2.353 [DOI] [PubMed] [Google Scholar]


