ABSTRACT
Aim:
The aim of the study was to compare the shear bond strength of composite resin bonded to polyether ether ketone (PEEK) and zirconia, and also to evaluate the effect of thermocycling on the shear bond strength.
Materials and Methods:
A total of 22 zirconia (Group 1) and 22 PEEK (Group 2) specimens (disks of 10 mm in diameter and 10 mm in thickness) were machine milled using computer-aided design (CAD)/computer-aided manufacturing (CAM) from commercially available zirconia and PEEK. These specimens were air abraded with 110-μm aluminum oxide. Following which these two groups were subdivided into four groups, that is, Group 1A: 11 zirconia specimens before thermocycling, Group 1B: 11 zirconia specimens after thermocycling, Group 2A: 11 PEEK specimens before thermocycling, and Group 2B: 11 PEEK specimens after thermocycling. These four groups of specimens were embedded in an acrylic block, and bonding agent was applied over the upper surfaces of the disks of each of these specimens. Composite resin was then cured, and then Group 1B and group 2B were thermocycled under a standard temperature. The bond strength of the specimen was tested using universal testing machine.
Result:
The result showed that there was no significant difference in shear bond strength between the groups, although higher shear bond strength was observed in the PEEK group.
Conclusion:
Shear bond strength of PEEK is similar to zirconia. The results suggest that the pretreatment method and primers used were effective in improving the bonding of resin cements to zirconia ceramic and the bonding properties of the veneering resin to the PEEK surface.
KEYWORDS: BioHPP, composite, polyether ether ketone, shear bond strength, thermocycling, zirconia
INTRODUCTION
Remarkable progress in the field of implant dentistry in recent years has made implant-supported prosthetic therapy a very predictable treatment modality. The criteria for success of implant-supported prosthesis are shifting from mere survival to a more functional and aesthetic outcome of these restorations.[1] Owing to their excellent properties and the ability to customize using computer-aided design (CAD)/computer-aided manufacturing (CAM), the use of tooth-colored alternatives such as zirconia and polyether ether ketone (PEEK) has seen increased application in the manufacture and restoration of implant abutments. The novel high-performance PEEK is a polymer from the main group of PAEK (polyaryl ether ketone) with its notable mechanical properties.[2]
Zirconia technology has enabled a rapid development of metal-free dentistry over the last decade that can provide high biocompatibility, enhanced aesthetics and enhanced strength. Zirconia, though aesthetic, it remains very white and opaque. So colored zirconia frame was introduced to mimic the color of natural teeth. A traditional approach to ceramic engineering uses two methods to achieve a homogeneous distribution of colors. First solution is by applying coloring oxides to zirconia powders before homogeneous color distribution and another method is by coprecipitation color doping of powder granules, leading to homogeneous color distribution. The need for multiple colors represents a financial hurdle to both approaches. Thus, the core of zirconia is covered with veneering porcelain to realize the aesthetic restoration,[3] as one of the most common complications of zirconia restoration is chipping or lamination of the veneer material. Von Steyern et al.[4] stated that chip-off fractures in porcelain cause the success rate of the DC zircon all-ceramic fixed partial denture to drop from 100% to 85% after 2 years.
PEEK (-C6 H4-OC6 H4-O-C6 H4-CO-)n is a semicrystalline linear polycyclic aromatic polymer developed in 1978 by a group of English researchers. In dentistry, PEEK is more natural, stable, biocompatible, lighter, and has reduced degree of discoloration. This makes it more attractive for patients with high demands on aesthetics.[5,6]
There are, however, certain aesthetic drawbacks that limit the use of PEEK as full-cover monolithic restorations. PEEK’s optical properties included low translucency and a grayish color. Therefore, a veneering layer is required to obtain a satisfactory aesthetic using additional resin composites.[7] However, the material’s bond strength is low when combined with composite resin due to the inert chemical performance, low surface energy, and PEEK’s resistance to surface modification.
With the advances in adhesive technologies and newer composite resins, excellent optical and mechanical properties have been possible to achieve. The composite resins can supplement and complement ceramic restorations. Thermocycling is considered a reasonable method for simulating in vitro aging of specimens to test the bonding properties because the stress is uniform for all specimens.[2]
Thus, the aim of this study was to compare the bond strength of composite resin to PEEK and composite resin to zirconia and also to compare the bond strength before and after thermocycling.
MATERIALS AND METHODS
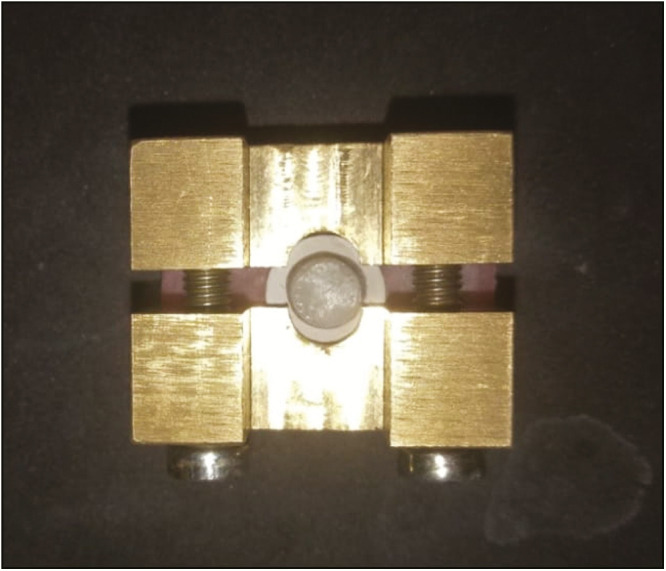
A total of 22 zirconia and 22 PEEK specimens were machine milled using CAD/CAM from commercially available zirconia blank (Ceramill® CAD/CAM milling system, AmannGirrbach, Austria) and PEEK blank (breCAM.BioHPP Milling disk—20 mm/dentin shade; Bredent, Derbyshire, UK). All the specimens were prepared according to the standard procedure. A custom-made rectangular metallic mold of dimension 30 mm × 15 mm × 12 mm was fabricated to make acrylic resin blocks. This rectangular metallic mold was filled with self-cure acrylic resin, and the samples fabricated were then embedded in the center of the acrylic resin [Figure 1]. All the samples were sandblasted with 110-µm aluminum oxide particles at 0.25MPa pressure and placed in an ultrasonic bath with deionized water for 5min.
Figure 1.

Sample embedded in acrylic resin using mold
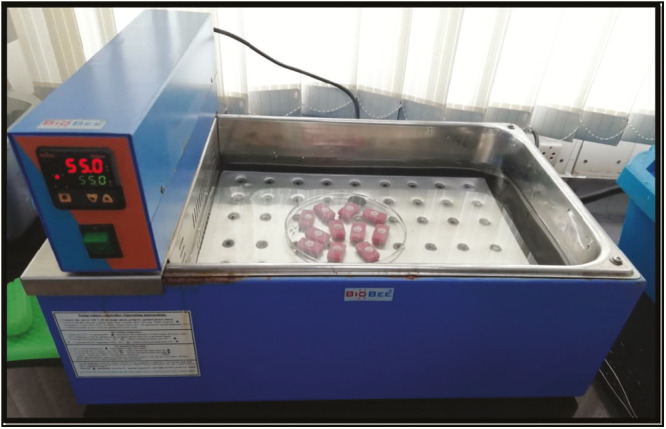
The zirconia group (n = 22) was treated with AZ Primer (Shofu, Kyoto, Japan) for 10s. Following which, the specimens were layered with Ceramage Indirect resin composite (Shofu, Dentin A2 shade). For reproducibility and uniformity, a cylindrically shaped metallic mold (6 mm in diameter and 2 mm in thickness) was used to apply the composite resin, Ceramage Indirect resin composite (Shofu, Dentin A2 shade), by the layering technique [Figure 2]. Finally, veneered specimens were polymerized using the same polymerization unit for 180s, and placed in distilled water for 24h at 37°C.
Figure 2.
Removal of metallic mold after layering of composite
The PEEK group (n = 22) was treated with CRB—Ceraresin Bond (Shofu). One layer of Bond I CRB—Ceraresin Bond (Shofu) was applied and air dried for 10s. Then, Bond II CRB—Ceraresin Bond (Shofu) was applied in one layer and light polymerized. Following which, the specimens were layered with Ceramage Indirect resin composite (Shofu, Dentin A2 shade). For reproducibility and uniformity, a cylindrically shaped metallic mold (6 mm in diameter and 2 mm in thickness) was used to apply the composite resin Ceramage Indirect resin composite (Shofu, Dentin A2 shade) by the layering technique. Finally, veneered specimens were polymerized using the same polymerization unit for 180s and placed in distilled water for 24h at 37°C.
Further, zirconia and PEEK groups were subdivided into the following groups:
Group 1A: 11 samples of composite bonded to zirconia block before thermocycling
Group 1B: 11 samples of composite bonded to zirconia block after thermocycling
Group 2A: 11 samples of composite bonded to PEEK block before thermocycling
Group 2B: 11 samples of composite bonded to PEEK block after thermocycling
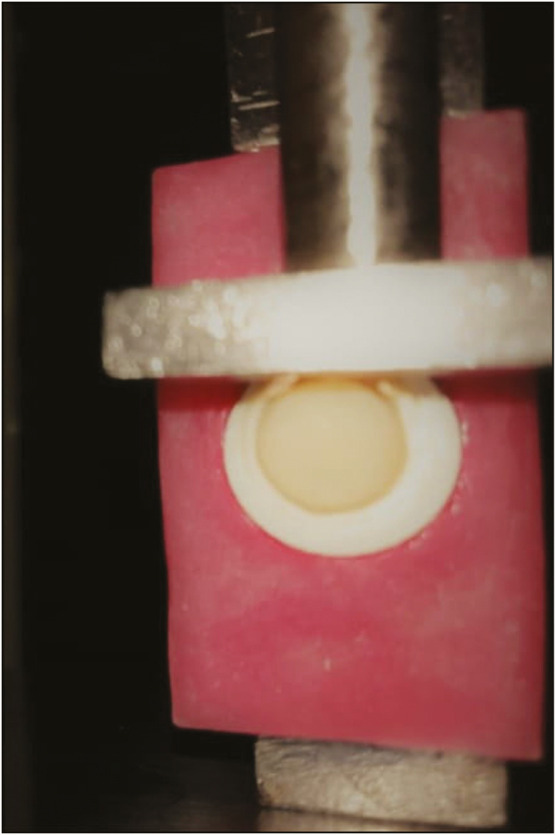
Group 1B and Group 2B were placed in a thermocycling unit with 5000 thermal cycles in water temperatures between 5°C and 55°C with a dwell time of 30s [Figure 3].
Figure 3.
Samples kept in thermocycling unit
The samples were mounted on the universal testing machine (TSI-Tecsol, Chennai, India). The shear bond strength was measured by using a loading head at a speed of 0.5 mm/min [Figure 4]. The Shear Bond Strength values were calculated as follows:
Figure 4.
A loading head with 0.5 mm/min loaded on the specimen
Statisticalanalysis: Statistical Package for the Social Sciences (SPSS, IBM, Chicago) software (version 23.0) was used for analyzing the data. One-way analysis of variance (ANOVA) was conducted to check for significant difference of shear bond strength between the test groups. Independent t test was performed to check for intergroup significance of shear bond strength.
RESULTS
The materials used in the study were zirconia, PEEK (a high-performance polymer), and composite resin.
Group 1A: 11 samples of composite bonded to zirconia block before thermocycling
Group 1B: 11 samples of composite bonded to zirconia block after thermocycling
Group 2A: 11 samples of composite bonded to PEEK block before thermocycling
Group 2B: 11 samples of composite bonded to PEEK block after thermocycling
All the 44 samples were secured to the holding device of universal testing machine (TSI-Tecsol) to perform shear bond tests under static condition. Samples were subjected to shear load at a crosshead speed of 0.5 mm/min. The load required to debond each specimen was recorded in kilogram force. One-way ANOVA, multiple comparisons, and t test were used for statistical analysis.
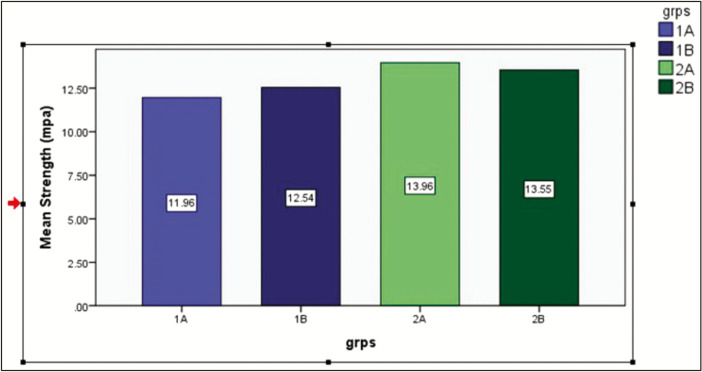
The mean values of the shear bond strength recorded for each group are listed in Table 1. The bond strength of composite to the PEEK was higher both before and after thermocycling 13.964 and 13.546MPa, respectively. Descriptive statistics (mean and standard deviation) was used, and these values were compared using the independent sample t test, and they were not found to be statistically insignificant (P = 0.745; confidence interval [CI] = -2.230–3.066). Composite bonded to zirconia recorded a slightly lower shear bond strength, and the comparison using the t test did not show any significance (P = 0.643; CI = -3.181 - 2.0 I). It was interesting to note that the shear bond strength of composite to zirconia improved after thermocycling [Table 1, Graph 1]. No statistically significant difference was observed between the mean strength of four groups.
Table 1.
Descriptive statistics for all the 4 groups derived using the students t test. t (20)= 0.471 and t (20) = 0.329 are t values for both groups. The p value for both the groups were statistically insignificant, p > 0.05
| Groups | Mean strength in MPA | SD | P value | |
|---|---|---|---|---|
| Zirconia | 1A | 11.957 | 2.928 | 0.643 |
| 1B | 12.543 | 2.907 | ||
| PEEK | 2A | 13.964 | 2.927 | 0.745 |
| 2B | 13.546 | 3.026 | ||
Graph 1.
Mean values (MPa) of shear bond strength of composite resin to zirconia and PEEK before and after thermocycling
One-way ANOVA was used to compare the shear bond strength of composite resin to PEEK and composite resin to zirconia before and after thermocycling. Difference in mean bond strength among the groups was found to be statistically insignificant (P = 0.375).
DISCUSSION
Owing to its biocompatibility, light weight, wear, and chemical degradation resistance, PEEK has become an attractive material for framework production of dental prostheses in the last few years. Given these common benefits, the use of PEEK is still difficult in the anterior aesthetic zone due to its opaque gray color. This limitation can be overcome by layering PEEK frameworks with composite resins to achieve a better shade and translucency.[8] Also the zirconia–feldspathic veneer interface is one of the major weak points of these restorations, and in some cases, it results in fractures, exposing the underlying zirconia.[9,10]
This study compared the shear bond strength of composite resin bonded to PEEK and zirconia, and also evaluated the effect of thermocycling on the shear bond strength. In this study, it has been observed that although no statistically significant difference was observed between the four groups, groups with PEEK showed the highest bond strength. The shear test was used to evaluate the strength of the bond, which is the most common test used to assess the strength of the repair bond. Repairing composite restorations is much easier than replacing the entire tooth structure in terms of cost, accuracy, and preservation. To ensure an adequate functional outcome and long-term stability, prolonged bonding to veneering materials is required. Depending on the composition of the materials used and their interactions, binding force can be obtained by chemical adhesion, mechanical interlocking, or a combination of both.[11]
Surface roughness has been shown to play an important role in the bonding technique for adhesives. The roughness of the material has greatly contributed to the initial bonding strength in shear bond testing.[12] In this study, before applying the bonding agent, an initial surface preparation was performed with air abrasion using aluminum oxide particles to clean the substrate, remove impurities, increase surface roughness, change surface energy, and increase wettability. Sandblasting increases surface roughness to create micro-mechanical interlocks and to clean the surface by removing organic contaminants from the composite material surface.[13]
Initially, air abrasion without a primer can result in high strength, but the strength of the bond decreases sharply even to zero over time.[9] In a study of different zirconia surface preparation methods, although the surface roughness was higher with the use of Neodymium-doped Yttrium Aluminium Garnet (Nd: YAG) laser compared with other classes, air abrasion surface preparation yielded higher shear bond strength.[5] Before thermocycling, the pressure time and size of the air abrading particles had no significant effect on the bond strength; however, after thermocycling, they clearly resulted in the long-term bond strength. In another study, sandblasting was found to alter the morphology of the PEEK composite layer, helping the luting cement to penetrate the composite material to strengthen micro-mechanical interlocks and improve the bond strength eventually.[14]
In this study, thermocycling was performed in water temperatures between 5°C and 55°C with a dwelling time of 30s at 5000 thermal cycles. A thermal cycling monitoring system to replicate changes in oral temperature under in vitro conditioning was used to determine the longevity of the restorations.[15] Bektas et al. found that 5000 thermal cycles decreased bond strength only in bur-prepared samples and had no significant effect on laser-prepared sample bond strength. However, we noticed no statistical difference between shear bond power of zirconia and PEEK before and after thermocycling.[10]
In this study, 6-methacryloyloxyhexyl phosphonoacetate (6-MHPA) was used as an adhesive agent for zirconia and composite veneer. Previous studies have shown that applying an 10- Methacryloyloxydecyl dihydrogen phosphate (MDP)-containing bonding or silane-bonding agent mixture to ceramic zirconia yields superior shear bond strength.[16] 6-MHPA are water-soluble monomers that can be partially or completely ionized with a small amount of water. The effective zirconia bonding was thought to be due to the good chemical interaction between the 6-MHPA or 6-MHPP (- P(=O)(OH)2) phosphonic acid group and metal oxides on the zirconia surface.[17] Sato[18] found that commercial metal primers (AZ Primer, Shofu), containing the 6-MHPA monomer of phosphonic acid, were successful in maintaining a strong bond between dual-curing luting cement, ResiCem (Shofu), and all-ceramic prostheses based on alumina and zirconia.[19]
To obtain adhesion between PEEK and composite, two bonding agents were used—BOND 1 consists of ethanol, silane-coupling agent, and BOND 2 consists of acetone, 4-AET, UDMA (urethane dimethacrylate), and polymerization initiator.[16]
In this study, it was observed that there was no statistically significance for the shear bond strength between the groups, and it was noticed that SBS value for zirconia is 11.96MPa and for PEEK is 13.96MPa. Reynolds[20] proposed that the minimum bond strength of 6–8MPa would be adequate for most clinical requirements. Such qualities of the bonds are considered capable of withstanding masticatory and orthodontic forces.[20] All bond strength values were above the minimum requirement in this experiment. A possible explanation for this observation could be the rewetting effect of primer or “healing” of minor surface defects on the airborne-particle abraded the surface. In addition, the phosphonate monomers of the primer can develop a bond with the oxides in the substrate and have resin terminal end groups, which can enable cohesive bonding.[17]
Reliable instructions for bonding to the PEEK surface are not available. Manufacturers recommend adhesive systems based on the chemistry of acrylic, cyanoacrylate, epoxy, or polyurethane and used in one or two components. Therefore, it can be indicated that surface cleaning and roughening (Al2O3, tribochemical treatment, H2SO4) is required to achieve good bonding between PEEK and veneering composite.[12]
Jin et al.[21] observed that the bond strength of BioHPP with the composite resin was greater than that of titanium. Therefore, BioHPP could be a suitable alternative to metal as a composite resin veneering framework.[21] Although no statistically significant difference was observed in shear bond strength between zirconia or BioHPP, this study showed a high bond strength comparable to the bond strength of metal or zirconia ceramic layering materials.
CONCLUSION
The shear bond strength of PEEK is similar to that of zirconia. The results suggest that the pretreatment process and primers used have been successful in improving the bonding of resin cements to the PEEK surface of ceramic zirconia and the bonding properties of veneering resin. As an alternative to metal, BioHPP can thus be recommended as a framework to be veneered with composite resin.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Santing HJ, Meijer HJ, Raghoebar GM, Özcan M. Fracture strength and failure mode of maxillary implant-supported provisional single crowns: a comparison of composite resin crowns fabricated directly over PEEK abutments and solid titanium abutments. Clin Implant Dent Relat Res. 2012;14:882–9. doi: 10.1111/j.1708-8208.2010.00322.x. [DOI] [PubMed] [Google Scholar]
- 2.Stawarczyk B, Keul C, Beuer F, Roos M, Schmidlin PR. Tensile bond strength of veneering resins to PEEK: impact of different adhesives. Dent Mater J. 2013;32:441–8. doi: 10.4012/dmj.2013-011. [DOI] [PubMed] [Google Scholar]
- 3.El-Ghany OS, Sherief AH. Zirconia based ceramics, some clinical and biological aspects. Future Dent J. 2016;2:55–64. [Google Scholar]
- 4.Von Steyern P, Carlson P, Nilner K. All-ceramic fixed partial dentures designed according to the DC-zirkon technique. A 2-year clinical study. J Oral Rehabil. 2005;32:180–7. doi: 10.1111/j.1365-2842.2004.01437.x. [DOI] [PubMed] [Google Scholar]
- 5.Tannous F, Steiner M, Shahin R, Kern M. Retentive forces and fatigue resistance of thermoplastic resin clasps. Dent Mater. 2012;28:273–8. doi: 10.1016/j.dental.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 6.Hallmann L, Mehl A, Sereno N, Hämmerle CH. The improvement of adhesive properties of PEEK through different pre-treatments. Appl Surf Sci. 2012;258:7213–8. [Google Scholar]
- 7.Keul C, Lieberman A, Schmidilin PR, Roos M, Sener B, Stawarczyk B. Influence of peek surface modification on surface properties and bond strength to veneering resin composites. J Adhesive Dent. 2014;16:383–92. doi: 10.3290/j.jad.a32570. [DOI] [PubMed] [Google Scholar]
- 8.Younis M, Unkovskiy A, ElAyouti A, Geis-Gerstorfer J, Spintzyk S. The effect of various plasma gases on the shear bond strength between unfilled polyether ether ketone (PEEK) and veneering composite following artificial aging. Materials. 2019;12:1447. doi: 10.3390/ma12091447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zakavi F, Mombeini M, Dibazar S, Gholizadeh S. Evaluation of shear bond strength of zirconia to composite resin using different adhesive systems. J Clin Exp Dent. 2019;11:e257–63. doi: 10.4317/jced.55428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bektas O, Eren D, Herguner Siso S, Akin G E. Effect of thermocycling on the bond strength of composite resin to bur and laser treated composite resin. Laser Med Sci. 2012;27:723–8. doi: 10.1007/s10103-011-0958-2. [DOI] [PubMed] [Google Scholar]
- 11.Kiomarsi N, Saburian P, Chiniforush N, Karazifard MJ, Hashemikamangar SS. Effect of thermocycling and surface treatment on repair bond strength of composite. J Clin Exp Dent. 2017;9:e945–51. doi: 10.4317/jced.53721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosentritt M, Preis V, Behr M, Sereno N, Kolbeck C. Shear bond strength between veneering composite and PEEK after different surface modifications. Clin Oral Investig. 2015;19:739–44. doi: 10.1007/s00784-014-1294-2. [DOI] [PubMed] [Google Scholar]
- 13.Sari F, Secilmis A, Simsek I, Ozsevik S. Shear bond strength of indirect composite material to monolithic zirconia. J Adv Prosthodont. 2016;8:267–74. doi: 10.4047/jap.2016.8.4.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schmidlin PR, Stawarczyk B, Wieland M, Attin T, Hämmerle CH, Fischer J. Effect of different surface pre-treatments and luting materials on shear bond strength to PEEK. Dent Mater. 2010;26:553–9. doi: 10.1016/j.dental.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 15.Zhou L, Qian Y, Gan K, Liu H, Liu X, Niu D. Effect of different surface treatments and thermocycling on shear bond strength to polyether ether ketone. High Performance Polymers. 2017;29:87–93. [Google Scholar]
- 16.Blatz MB, Sadan A, Martin J, Lang B. In vitro evaluation of shear bond strengths of resin to densely-sintered high-purity zirconium-oxide ceramic after long-term storage and thermal cycling. J Prosthet Dent. 2004;91:356–62. doi: 10.1016/j.prosdent.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Rani S, Shankar MS, Jacob PC, Rai N, Jagadeesh KN. To evaluate the tensile bond strength of zirconia primer on the retention of zirconium oxide ceramic crowns—an in vitro study. Indian J Oral Sci. 2015;6:113. [Google Scholar]
- 18.Sato T. The adhesive priming agent for zirconia- and alumina-based all-ceramic prosthesis. Proceedings of the 2nd International Congress of Adhesive Dentistry; 2005. pp. 22–24. [Google Scholar]
- 19.Ikemura K, Jogetsu Y, Shinno K, Nakatsuka T, Endo T, Kadoma Y. Effects of a newly designed HEMA-free, multi-purpose, single-bottle, self-etching adhesive on bonding to dental hard tissues, zirconia-based ceramics, and gold alloy. Dent Mater J. 2011;30:616–25. doi: 10.4012/dmj.2011-076. [DOI] [PubMed] [Google Scholar]
- 20.Reynolds IR. A review of direct orthodontic bonding. Br J Orthod Craniofac Res. 1975;2:171–8. [Google Scholar]
- 21.Jin HY, Teng MH, Wang ZJ, Li X, Liang JY, Wang WX, et al. Comparative evaluation of BioHPP and titanium as a framework veneered with composite resin for implant-supported fixed dental prostheses. J Prosthet Dent. 2019;122:383–8. doi: 10.1016/j.prosdent.2019.03.003. [DOI] [PubMed] [Google Scholar]


