ABSTRACT
Introduction:
Miswak is a tooth brushing stick that contains many ingredients that are beneficial for maintenance of oral hygiene. The aim of this study is to formulating a film containing miswak extract for treatment of chronic periodontitis.
Materials and Methods:
Here we tested the miswak raw extract invitro against Porphyromonas gingivalis and Herpes simplex virus-1 (HSV-1). The film was prepared using solvent casting method. Disintegration test was conducted to find the stability of the film.
Results:
Cytotoxicity of miswak was also tested. Minimum inhibitory concentration against P. gingivalis was 62.5 µg/mL. Therapuetic index against HSV-1 was 11.3 µg/mL. Cytotoxicity against 50% Vero cells was present at 210 µg/mL. Based on this invitro study 100 µg/mL dose was calculated to be incorporated in a film of size 0.5 mm × 0.4 mm. This film is made of polymers HPMC K 100 and Eudragit L 100. Disintegration test of the film showed that they remained stable for around 5 days.
Conclusion:
In the present study we formulated the miswak raw extract containing film that can act against P. gingivalis and HSV-1. So it can be used to treat chronic periodontitis by placing it in periodontal pockets.
KEYWORDS: Gingivitis, miswak, oral health, periodontitis, Porphyromonas gingivalis
INTRODUCTION
Periodontitis is a pathologic condition that affects the supporting structures of the teeth. It causes destruction of periodontal ligament, loss of alveolar bone, and apical migration of periodontal ligament. It is an inflammatory response to the plaque accumulation in periodontal pocket.[1] Bacteria in plaque are the primary cause but they cannot explain rapid periodontal breakdown in patients with minimal plaque accumulation. The role of herpesviruses are suspected in such cases. Herpesviruses are isolated from gingival crevicular fluid and periodontal tissues.[2]
Periodontitis is treated by mechanical debridement and systemic antibiotics. Mechanical debridement cannot be done effectively in teeth with complex anatomic root structure.[3] They also fail to totally eliminate bacteria such as Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans due to their invasive nature into gingiva and the surrounding tissues. This leads to the use of antimicrobials to overcome the shortcomings of mechanical debridement.[4] Systemic antibiotics, such as penicillins, tetracycline, and metronidazole, have the drawback of developing gastrointestinal disturbances and drug resistance, and they also fail to achieve adequate concentration at the site of action.[3] To overcome these shortcomings, local drug delivery (LDD) system has been developed.[4]
People are turning back to nature for solutions to various ailments. Various herbal products are used nowadays. The use of chewing sticks to brush our teeth is a well-known practice in rural India. Miswak is a lesser known chewing stick [Figure 1] in India, but it is commonly used in Arabic countries. Its botanical name is Salvadora persica. It is basically a small tree, approximately 3 m in height. The leaves, flowers, berries, and sticks have medicinal properties. They are traditionally used to treat cough, asthma, scurvy, piles, and rheumatism. They have mustard smell and pungent taste.[5]
Figure 1.

Miswak chewing sticks
Miswak sticks have various constituents with beneficial effects, listed as the following:
Silica: Abrasive material to remove plaque
Tanins: Reduces gingivitis and the level of Candida albicans
Resins: Forms a layer over enamel and prevents dental caries
Alkaloids: Antifungal and antibacterial activity
Sulfur: Antibacterial activity
Vitamin C: Tissue repair
Sodium bicarbonate: Dentifrice
Calcium: Enamel remineralization
Fluoride: Anticariogenic activity
Chloride: Inhibit calculus formation
Benzyl isothiocyanate: Anticarcinogenic and antibacterial activity
Trimethylamine: Antibacterial activity[6]
LDD can provide sustained release of drug at the site of periodontal pocket. They can provide effective treatment at a much smaller dose. Various forms of LDD that can be used at the site of periodontal pocket are films, gels, fibers, strips, nanoparticles, and microparticles.[1] Hydroxypropyl methylcellulose (HPMC) is a creamy white granular or fibrous powder used in pharmaceutical preparations. It is most widely used because of its various advantages such as chemical inertness, safety, stability, regulation of viscosity, metabolically inert, and solubility in water.[7] Eudragit is a polymer that usually has the capacity to combine with active agents or drugs to release drugs at a specific rate.[8] Miswak possesses many properties, which can used to treat periodontitis. So miswak can be added with HPMC and Eudragit to prepare an LDD agent in the form of film to be placed in periodontal pockets.
The aim of this study was to formulate and characterize an LDD agent in the form of film to deliver miswak at the site of action for the treatment of chronic periodontitis.
MATERIALS AND METHODS
The study was conducted in the department of pharmaceutical biotechnology, JSS College of Pharmacy, Ooty, Tamil Nadu, India. Certified miswak powder [Figure 2] was procured commercially from Vilumin Herbals through IndiaMART traders. Miswak extract was obtained from this powder.
Figure 2.

Miswak powder
The minimum inhibitory concentration (MIC)[9] against P. gingivalis and MTT (3-[4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) antiviral assay[10] against herpes simplex virus-1 (HSV-1) of this miswak extract was calculated. The specified bacteria and virus are important pathogens involved in chronic periodontitis. They were collected from the stock preserved in college. The MIC against P. gingivalis was calculated to be 62.5 µg/mL. The therapeutic index against HSV-1 was calculated to be 11.03 µg/mL. The half minimal inhibitory concentration (IC50) was calculated to be 18.6 µg/mL. The cytotoxicity concentration against 50% cells (CC50) was 210 µg/mL. The cell line Vero (African green monkey, kidney) was used. This cell line is comparable to human cells.
The raw materials used for preparing miswak film are as follows:
Miswak raw extract (Vilumin Herbals, Indore, India)
HPMC K 100: HPMC (Colorcon Asia, Goa, India)
Eudragit L 100 (Evonik Roehm Pharma, Mumbai, India)
HPMC K 100[7] is a pharmacologically inert, extended-release matrix-forming agent. Eudragit L 100 is also a pharmacologically inert material. It adds stability[8] to HPMC K 100. Both HPMC K 100 and Eudragit L 100 are used to prepare film coat tablets and oral capsule.
Calculation of dose
From the microbial and viral studies, 100 µg of miswak was calculated to be the ideal dose. This 100 µg is dispersed in a film of size 2 cm2. This film size is suitable for placement in periodontal pocket.
> 2 cm2
Equivalent to 100 µg/mL
0.5 × 0.4 cm
The dose was selected because of the following reasons:
The film remained stable.
It can exhibit therapeutic activity against P. gingivalis and HSV-1.
It does not show cytotoxic effect.
It helps to obtain extended-release activity.
The dental film is prepared by using solvent casting method. Area of the casting plate is 100 cm2 (10 ×10 cm). The amount of miswak raw extract for 100 cm2 is calculated to be 5 mg (100 cm2/2 cm2).
> 100 cm2
Equivalent to 5 mg (100/2 cm2 = 50 fold)
10 × 10 cm
Solvent casting method
Here the water-soluble materials are dissolved to form a viscous solution [Figure 3]. The steps involved in the miswak film preparation are:
Figure 3.
Solvent casting machine
Step 1: 3% of HPMC K 100 and 1.5% of Eudragit L 100 are taken in a empty beaker.
Step 2: 100 mL of 1:1 ratio of ethanol and water are added to the aforementioned mixture. Calculated quantity of miswak raw extract is added to the solution.
Step 3: Thorough mixing with mechanical stirrer at 750rpm for 30 min is carried out.
Step 4: The solution is kept undisturbed for 12h to remove air bubbles. Later, it is casted in casting plate of 100 cm2.
This results in the formation of a film of uniform property and thickness [Figure 4]. Later, it is cut into pieces of desired size.[11]
Figure 4.
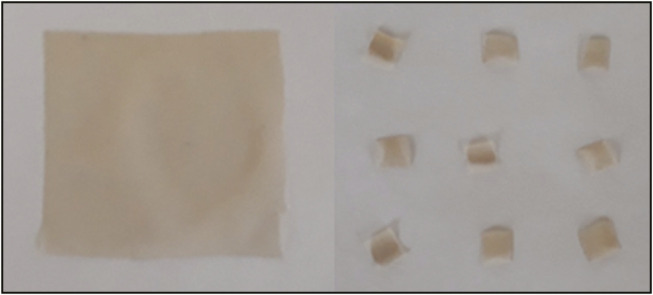
Miswak films
Disintegration test
The film of 0.5 × 0.4 cm was subjected to disintegration in phosphate buffer at pH 6.8 in a plastic vial of 5 mL capacity [Figure 5]. The vial was agitated occasionally (approximately once every 1h) and controlled at 37°C.[12]
Figure 5.

Disintegration test vials
The film was observed to completely disintegrate into solution at the end of 137h (5 days 17h).
DISCUSSION
In our study, we had attempted to create an LDD agent containing miswak in the form of film for the treatment of periodontitis. No such formulation has been attempted so far. This is the first time such an attempt has been made.
Al Sadhan and Almas,[13] in 1999, in his article has discussed about miswak, their composition and their properties. Shetti et al.,[14] in 2016, had shown that miswak in the form of mouthwash reduced plaque score and gingival score effectively. A review by Sukkarwalla et al.,[15] in 2013, showed that miswak shows antibacterial property against various gram-positive and gram-negative bacteria.
In our study, we studied the antibacterial effect against P. gingivalis and antiviral effect against HSV-1. P. gingivalis is a common periodontopathic bacteria.[16] Recent studies show that HSV-1 has been positively related to chronic periodontitis.[16] The therapeutic dose against P. gingivalis was calculated to be 62.5 µg/mL. The therapeutic index against HSV-1 was calculated to be 11.3 µg/mL. Cell cytotoxicity was calculated to be 210 µg/mL, which was done on Vero cells. These cell lines are the most commonly used mammalian cell line for the study of bacteria, virus, and various chemicals.[17] The antibacterial and antiviral activity could be due to benzyl isothiocyanate in miswak raw extract.[13]
Keeping the aforementioned results in mind, a dose of 100 µg/mL was selected. This dose can act against P. gingivalis and HSV-1; also, it is not cytotoxic to cells. This dose was used to create the miswak film. Delivering antimicrobial in the form of LDD provides 100-fold greater concentration than a systemic regimen.[18]
The film is made of polymers HPMC K 100 and Eudragit L 100. They are basically a type of HPMC and Eudragit. HPMC is nontoxic and water soluble. Antimicrobials can be mixed with HPMC without affecting their nature. HPMC is also chemically inert and not absorbed or metabolized in human body.[7] Eudragit provides adhesive property and decreases the drug release rate. So it is mixed with HPMC to enhance its drug-release properties.[8]
The film, thus formed by the mixture of miswak raw extract, HPMC K 100, and Eudragit L 100, was subjected to disintegration test. The test showed that the film remained considerably stable and underwent complete disintegration only after 5 days 17h. This showed that the film can release the miswak extract at the site of periodontal pocket for around 5 days.
CONCLUSION
In this study, we formulated the miswak raw extract–containing film. This film can act against P. gingivalis and HSV-1. It does not affect the mammalian cells and remains stable for around 5 days. So it can be used to treat chronic periodontitis by placing it in periodontal pockets.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We are thankful to Dr. Gowthamrajan of JSS College of Pharmacy, Ooty, Tamil Nadu, India, for helping us conduct this study.
REFERENCES
- 1.Kaplish V, Walia MK, Kumar HSL. Local drug delivery in the treatment of periodontitis: a review. Pharmacophore. 2013;4:39–49. [Google Scholar]
- 2.Petrovic SM, Zelic K, Milasin J, Poovic B, Pucar A, Zelic O. Detection of herpes simplex virus type 1 in gingival crevicular fluid of gingival sulcus/periodontal pocket using polymerase chain reaction. Srp Arh Celok Lek. 2014;142:296–300. [PubMed] [Google Scholar]
- 3.Rajpoot AS, Parihar AS, Thakur S, Choudhary K, Rajput P, Chaudhary A. Local drug delivery in periodontics. Int J Res Health Allied Sci. 2017;3:63–7. [Google Scholar]
- 4.Sharma NK, Prasad A. Evaluation of efficacy of tetracycline as a local drug delivery system in the treatment of chronic periodontitis as an adjunct to scaling and root planning—a clinical and microbiological study. Int J Contemp Med Res. 2017;4:998–1003. [Google Scholar]
- 5.Kshirsagar JT, Jareen AJ. The miracle twig—miswak. Int J Appl Dent Sci. 2017;3:66–70. [Google Scholar]
- 6.Haque MM, Alsareii S. A review of the therapeutic effects of using Miswak (Salvadora persica) on oral health. Saudi Med J. 2015;36:530–43. doi: 10.15537/smj.2015.5.10785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huichao W, Shouying D, Ying L, Ying L, Wang Di. The application of biomedical polymer material hydroxyl propyl methyl cellulose (HPMC) in pharmaceutical preparations. J Chem Pharm Res. 2014;6:155–60. [Google Scholar]
- 8.Nikam VK, Kotade KB, Gaware VM, Dolas RT, Dhamak KB, Somwanshi SB, et al. Eudragit a versatile polymer: a review. Pharmacologyonline. 2011;1:152–64. [Google Scholar]
- 9.Miles AA, Misra SS. Estimation of bactericidal power of blood. J Hyg. 1938;38:732. doi: 10.1017/s002217240001158x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kurokawa M, Wadhwani A, Kai H, Hidaka M, Yoshida H, Sugita C, et al. Activation of cellular immunity in herpes simplex virus type 1-infected mice by the oral administration of aqueous extract of Moringa olifera Lam. leaves. Phytotherapy Res. 2016;30:797–804. doi: 10.1002/ptr.5580. [DOI] [PubMed] [Google Scholar]
- 11.Kulkarni AS, Deokule HA, Mane MS, Ghadge DM. Exploration of different polymers for use in the formulation of oral fast dissolving strips. J Curr Pharm Res. 2010;2:33–5. [Google Scholar]
- 12.Gupta VK, Assmus MW, Beckert TE, Price JC. A novel pH- and time-based multi-unit potential colonic drug delivery system. II. Optimization of multiple response variables. Int J Pharm. 2001;213:93–102. doi: 10.1016/s0378-5173(00)00650-5. [DOI] [PubMed] [Google Scholar]
- 13.Al Sadhan RI, Almas K. Miswak (chewing stick): a cultural and scientific heritage. Saudi Dent J. 1999;11:80–8. [Google Scholar]
- 14.Shetti NA, Metgud R, Pattar V, Hugar SS. Salvadora persica (miswak) mouthwash: a promising home care agent. Annals Dent Speciality. 2016;4:6–9. [Google Scholar]
- 15.Sukkarwalla A, Ali SM, Lundberg P, Tanwir F. Efficacy of miswak on oral pathogens. Dent Res J (Isfahan) 2013;10:314–20. doi: 10.4103/1735-3327.115138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chatzopoulou E, Trianti M, Fanourakis G, Dereka X. Herpes simplex virus 1 and 2 in chronic periodontitis: prevalence and association with clinical parameters. Dent Health Curr Res. 2018;4:2. [Google Scholar]
- 17.Ammerman NC, Beier-Sexton M, Azad A. Growth and maintenance of Vero cell lines. Curr Protoc Microbiol. 2008;11:A.4E.1–7. doi: 10.1002/9780471729259.mca04es11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pandit N, Dhahiya R, Gupta R, Bali D, Kathuria A. Comparative evaluation of locally delivered minocycline and metronidazole in the treatment of periodontitis. Contemp Clin Dent. 2013;4:48–53. doi: 10.4103/0976-237X.111615. [DOI] [PMC free article] [PubMed] [Google Scholar]


