ABSTRACT
Aim:
The aim of this study was to evaluate effectiveness of bethanechol and pilocarpine among xerostomic denture wearers.
Materials and Methods:
This in vitro study was conducted in 60 complete denture wearers of both genders. For assessment of salivary flow, resting saliva and stimulated saliva were collected. Patients were split into two groups consisting of 30 patients each. Pilocarpine was given to patients in group I and patients in group II received bethanechol. Salivary flow was measured at baseline, after 2 weeks, and after 4 weeks.
Results:
The mean whole resting saliva in patients of group I was 0.61 mg/mL and in that of group II was 0.65 mg/mL. The mean whole stimulated saliva in patients of group I was 1.35 mg/mL and in group II it was 1.51 mg/mL. The mean whole resting saliva after 2 weeks in patients of group I was 0.83 mg/mL and in group II was 0.92 mg/mL. Whole stimulated saliva in patients of group I was 1.67 mg/mL, and in patients of group II it was 1.86 mg/mL. The difference noted was significant (P < 0.05). The mean whole resting saliva after 4 weeks in patients of group I was 1.23 mg/mL and in that of group II was 1.43 mg/mL. Whole stimulated saliva in patients of group I was 1.98 mg/mL and in patients of group II it was 2.04 mg/mL.
Conclusion:
Authors found that both agents were effective in increasing salivary secretions. However, pilocarpine is a more effective sialagogue as compared to bethanechol in completely edentulous patients with xerostomia.
KEYWORDS: Bethanechol, pilocarpine, sialagogue
INTRODUCTION
Salivary hypofunction is frequently encountered among denture wearers. Saliva is necessary and important for the maintenance of oral health. It helps in swallowing, speech, and oral function, and serves as an adhesive between undersurface of denture and mucosal surface. It also provides protection against chemical, mechanical, and microbial pathogens.[1]
Xerostomia may be due to various reasons that need to be assessed. Complete and thorough evaluation is necessary to assess the case of xerostomia. It is more frequently seen among old age people. Saliva plays an important role in denture retention. Without saliva, patient faces loss of denture retention and irritation. Management of patients with xerostomia includes frequent sipping of water in order to make oral cavity moist. Sugar-free gum or candies/lozenges may be useful up to a certain extent.[2]
Parasympathomimetic agents such as pilocarpine hydrochloride or neostigmine bromide can provide sympathetic relief.[3] Artificial saliva and salivary substitutes provide immediate relief in patients with xerostomia. Aqueous solutions made up of the mineral salts constitute artificial saliva, which are similar to that of salts in human saliva. The hollowed lingual flange of a mandibular denture serves an intraoral saliva reservoir to provide artificial saliva and sometimes even palatal reservoir does the same.[4]
Pilocarpine is a cholinergic agonist. It acts on muscarinic cholinergic receptor by stimulating the function of gland including salivary glands. There have been reports of >90% improvement in completely edentulous patients with xerostomia. Bethanechol, which is an acetylcholine analogue, is usually resistant to rapid destruction by cholinesterase and thus has prolonged activity.[5] This study was conducted to assess efficacy of pilocarpine and bethanechol in xerostomic denture wearers.
MATERIALS AND METHODS
The Department of Prosthodontics, Crown Bridge, and Implantology, Patna Dental College and Hospital, Patna, Bihar carried out this in vitro study in 60 complete denture wearers of both genders. Approval was obtained from the institutional ethics committee. All participants in the study were informed about outcome of the study and consent was obtained in written form.
Data pertaining to each patient were recorded, such as name and age. A thorough oral examination was performed in all patients. History of symptoms, severity, and duration of xerostomia were recorded.
For assessment of salivary flow, pre-weighed wide-mouth centrifuge tubes were used to collect resting saliva and stimulated saliva. Patients were split into two groups consisting of 30 patients each. Pilocarpine was given to patients in group I and patients in group II received bethanechol. Salivary flow was measured at baseline, after 2 weeks, and after 4 weeks.
Statistical analysis
The result thus obtained was entered in MS Excel sheet. The data were evaluated using SPSS, version 21.0 (IBM, Chicago, IL). Salivary flow was measured by paired t test, and results were considered statistically significant when P value was less than 0.05.
RESULTS
In group I, 20 male and 10 female patients were included [Table 1]. In group II, there were 16 male and 14 female patients. Patients in group I were given pilocarpine and patients in group II received bethanechol. Table 2 shows that mean whole resting saliva (WRS) in patients of group I was 0.61 mg/mL and in group II it was 0.65 mg/mL. The mean whole stimulated saliva (WSS) in patients of group I was 1.35 mg/mL, and in group II it was 1.51 mg/mL. Paired t test showed nonsignificant difference in both groups (P > 0.05). Graph 1 shows that mean WRS after 2 weeks in patients of group I was 0.83 mg/mL, and in group II it was 0.92 mg/mL. WSS in patients of group I was 1.67 mg/mL, and in patients of group II it was 1.86 mg/mL. The obtained difference was statistically significant (P < 0.05). Graph 2 shows that mean WRS after 4 weeks in patients of group I was 1.23 mg/mL, and in group II it was 1.43 mg/mL. WSS in patients of group I was 1.98 mg/mL, and in patients of group II it was 2.04 mg/mL. The difference was statistically significant as P value was less than 0.05.
Table 1.
Distribution of patients
| Parameters | Group I (30) | Group II (30) |
|---|---|---|
| Drug | Pilocarpine | Bethanechol |
| Male | 20 | 16 |
| Female | 10 | 14 |
Table 2.
Assessment of salivary flow at baseline in both groups
| Duration | Group I | Group II | P value |
|---|---|---|---|
| WRS (mg/mL) | 0.61 | 0.65 | 0.816 |
| WSS (mg/mL) | 1.35 | 1.51 | 0.721 |
Paired t test. Significant P < 0.05
Graph 1.
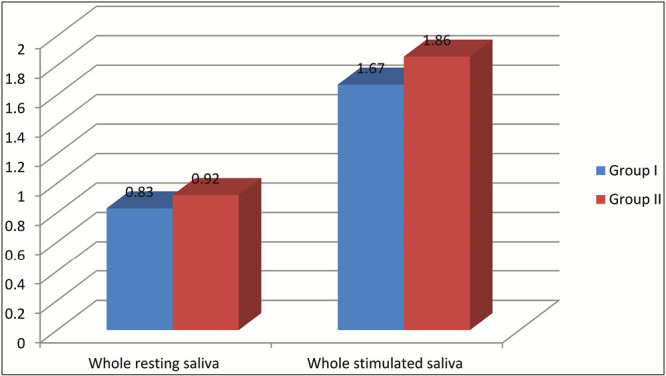
Assessment of salivary flow after 2 weeks in both groups
Graph 2.
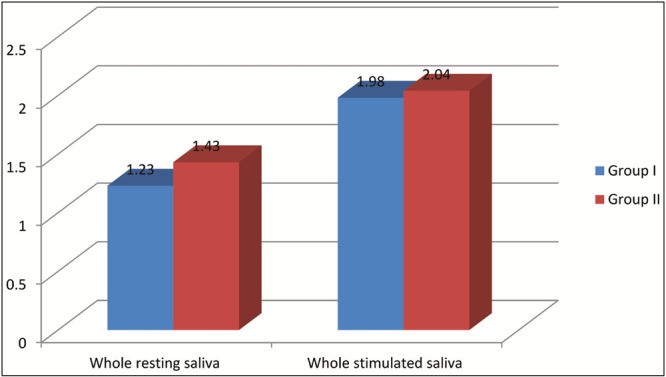
Assessment of salivary flow after 4 weeks in both groups
DISCUSSION
Xerostomia presents as a local symptom and is characterized by decreased salivary flow from salivary glands. Systemic diseases such as diabetes, Sjogren’s syndrome, and alcoholism may cause this condition. It may result from various medications.[6] Radiation therapy for malignancies of head and neck can also affect salivary glands, resulting in decreased salivary outflow in these patients. Most often dry mouth is a regular complaint in edentulous patients with xerostomia associated with other issues such as difficulty in normal functions such as speaking, eating, and swallowing. Denture wearers commonly complain of discomfort for which they seek frequent intervention.[7]
The management of xerostomia depends on the etiological factors. If it is induced by some medication, alteration of dose and drug is mandatory. Some cases need symptomatic treatment such as changes in dietary pattern, sipping water frequently, and administering of artificial salivary substitutes.[8] This study was conducted to assess the efficacy of pilocarpine and bethanechol in xerostomic denture wearers.
In this study, there were 60 denture wearers of both genders. All were diagnosed of xerostomia. Patients were split into two groups comprising 30 patients in each group. Patients in group I were given pilocarpine and patients in group II received bethanechol. In group I, there were 20 male and 10 female patients and in group II, there were 16 male and 14 female patients.
Muralidharan et al.[9] conducted a study on xerostomic edentulous denture wearers to assess the role of pilocarpine and bethanechol as useful saliva substitutes. Thirty xerostomic complete denture patients were reported to the clinic. Collection of WRS and WSS was performed in a test tube for 2 min following which the sialagogue drug is administered for 2–3 weeks’ course. There was significant increase in mean salivary production of both the drugs, which are pilocarpine and bethanechol, respectively, during the first week. On crossover, pilocarpine was found to be more efficient than bethanechol with respect to both WRS and WSS, respectively.
We found that mean WRS in patients of group I was 0.61 mg/mL, and in that of group II was 0.65 mg/mL. The mean WSS in patients of group I was 1.35 mg/mL and in group II was 1.51 mg/mL. There was significant increase in mean WRS after 2 weeks in both groups. It was 0.83 mg/mL in patients of group I and 0.92 mg/mL in patients of group II. WSS in patients of group I was 1.67 mg/mL and in patients of group II it was 1.86 mg/mL.
The clinical efficacy of sialogogues and their adverse effects were evaluated by Chainani et al.,[10] who studied the role of pilocarpine, bethanechol, and cevimeline in patients with xerostomia. Measurement of WSS and unstimulated saliva was conducted in all the patients who showed increased salivary flow and decreased symptoms. Increase in stimulated saliva to a greater extent was seen by the use of bethanechol over pilocarpine. Patients experienced increased sweating, which was frequently seen with pilocarpine and not with bethanechol or cevimeline. Hence, authors concluded that sialogogues treatment in intermittent manner as an alternative to treatment with sialogogues in continuous manner.
We found that mean WRS after 4 weeks in patients of group I was 1.23 mg/mL and in group II was 1.43 mg/mL. WSS in patients of group I was 1.98 mg/mL and in patients of group II was 2.04 mg/mL.
Saliva is essential for retention of the complete denture thereby ensuring patient’s comfort. The chances of cases of denture stomatitis increases if there are symptoms of xerostomia.[11] Other common ailments seen in these patients are oral ulcers, which are due to the excessive force applied by the complete dentures over the denture-bearing mucosa. Therefore, saliva secretion should not be affected in denture wearers.[12] Both pilocarpine and bethanechol are effective pharmacological agents in increasing the salivary production in patients with xerostomia. The limitation of the study is that sample size selected is quite small and needs to be ascertained in larger one.
CONCLUSION
Authors found that both agents were effective in increasing salivary secretions. However, pilocarpine is a more effective sialagogue as compared to bethanechol in completely edentulous patients with xerostomia. Management of xerostomia is important to ensure success of complete denture in edentulous patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Saleh J, Figueiredo MA, Cherubini K, Salum FG. Salivary hypofunction: an update on aetiology, diagnosis and therapeutics. Arch Oral Biol. 2015;60:242–55. doi: 10.1016/j.archoralbio.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 2.Gurkar H, Venkatesh OY, Somashekar JM, Gowda MH, Dwivedi M, Ningthoujam I. Prosthodontic management of xerostomic patient: a technical modification. Case Rep Dent. 2016;2016:8905891. doi: 10.1155/2016/8905891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Silverman S., Jr . Oral cancer. 3rd ed. Atlanta, GA: American Cancer Society; 1990. [Google Scholar]
- 4.Al-Dwairi Z, Lynch E. Xerostomia in complete denture wearers: prevalence, clinical findings and impact on oral functions. Gerodontology. 2014;31:49–55. doi: 10.1111/ger.12002. [DOI] [PubMed] [Google Scholar]
- 5.Ravisankar A, Anand S. Xerostomia in denture patients. Int J Sci Res. 2016;5:906–8. [Google Scholar]
- 6.Iqtidar Z, Aslam A, Naeem S, Zafar N, Adeem U. Xerostomia and its effect on complete denture stability. Pak Oral Dent J. 2017;37:188–91. [Google Scholar]
- 7.Doppalapudi R, Vundavalli S, Rao AK, Vadapalli SB, Rao DC, Thabusum A. Relation between clinical oral dryness score and denture satisfaction among patients’ in a tertiary care centre, India. J Clin Diagn Res. 2017;11:ZC64–7. doi: 10.7860/JCDR/2017/25696.9881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmed Elmorsy AE, Ahmed Ibraheem EM, Ela AA, Fahmy A, Nassani MZ. Do flexible acrylic resin lingual flanges improve retention of mandibular complete dentures? J Int Soc Prev Community Dent. 2015;5:365–71. doi: 10.4103/2231-0762.165928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muralidharan J, Dhanraj M, Jain AR. Comparison of pilocarpine and bethanechol as effective sialogogue agents in xerostomic completely edentulous patients. Drug Invention Today. 2018;10:958–61. [Google Scholar]
- 10.Chainani-Wu N, Gorsky M, Mayer P, Bostrom A, Epstein JB, Jr, Silverman S., Jr Assessment of the use of sialogogues in the clinical management of patients with xerostomia. Sp Care Den. 2006;26:164–70. doi: 10.1111/j.1754-4505.2006.tb01719.x. [DOI] [PubMed] [Google Scholar]
- 11.Miranda-Rius J, Brunet-Llobet L, Lahor-Soler E, Farré M. Salivary secretory disorders, inducing drugs, and clinical management. Int J Med Sci. 2015;12:811–24. doi: 10.7150/ijms.12912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gil-Montoya JA, Silvestre FJ, Barrios R, Silvestre-Rangil J. Treatment of xerostomia and hyposalivation in the elderly: a systematic review. Med Oral Patol Oral Cir Bucal. 2016;21:e355–66. doi: 10.4317/medoral.20969. [DOI] [PMC free article] [PubMed] [Google Scholar]


