ABSTRACT
Background and Aim:
Flexible denture base has been gaining attention as a denture base material because of its toxicological safety, comfort, and enhanced aesthetics. Debonding of acrylic teeth from the flexible denture base material has posed a great problem to the clinician and patient. This study aimed at comparing the bond strength between flexible denture base with acrylic teeth having different mechanical modifications.
Materials and Methods:
Forty mandibular molar teeth (Combination Acry Rock, Badia Polesine (Ro), Italy) were used in four groups for mechanical modifications on the ridge lap area. The groups were group 1 (no mechanical modifications), group 2 (round groove 2 mm in diameter and 2 mm deep on the ridge lap surface), group 3 (horizontal slot 2 mm deep, 2 mm wide, and 4 mm long prepared on the ridge lap surface of the teeth), and group 4 (T-shaped groove 2 mm deep, 2 mm wide, and length of 4 mm mesiodistally and 2 mm buccolingually prepared with a straight fissure bur). The acrylic teeth were attached to a wax block of dimension 1.2 cm × 1.2 cm × 2.5 cm. These were flasked and dewaxed, followed by injection molding with Valplast flexible denture base material. The bond strength was assessed by attaching the specimens to universal testing machine tested under a tensile load at a cross-head speed of 1 mm/min till it fractured. Data obtained were statistically evaluated by one-way analysis of variance and post hoc test.
Results:
There was significant increase in mean bond strength after various mechanical modifications. Group with T-shaped diatoric hole showed greatest bond strength value compared to other groups.
Conclusion:
Incorporating mechanical retentive features with increased surface area and undercut can improve the bonding of acrylic teeth to flexible denture base.
KEYWORDS: Acryrock teeth, bond strength, flexible denture base, Valplast
INTRODUCTION
Prosthodontics is the dental speciality pertaining to the diagnosis, treatment planning, rehabilitation, and maintenance of the oral function, comfort, appearance, and health of patients with clinical conditions associated with missing or deficient teeth and/or maxillofacial tissues using biocompatible substitutes.[1] Emerging concepts, newer materials, and technologies greatly impact the research and clinical practice of prosthodontics.
Loss of teeth due to trauma, dental diseases, pathology, or otherwise not only significantly alters the physiological well-being of the patients, but also disturbs the aesthetics, phonetics, and functional occlusion.[2] Various materials such as wood, bone, ivory, gold, vulcanite, and porcelain were used for the fabrication of teeth in the past.[3] Greater awareness to aesthetics and advancements in material science had led to the development of acrylic teeth, which mimic natural teeth both in function and aesthetics.[4]
Initially, porcelain was the commonly used tooth material because of the rapid wear of acrylic resin. However, acrylic teeth gained popularity over porcelain teeth because of their inherent problems such as brittleness, susceptibility to crazing (denture base) clicking sound, difficulty in grinding, need for mechanical retention, and abrasion of opposing natural teeth.[5] Polymethyl methacrylate (PMMA) introduced by Dr. Walter Wright in 1937 has been used to fabricate denture bases.[6] Some of the problems encountered with acrylic denture bases are allergy to methacrylate monomer, difficulty to insert in undercut areas, and brittleness of the material leading to fracture in spite of various advancements in the denture base materials and research in the field of dental materials and techniques.[7] Allergy, fracture, and difficulty to insert in areas of higher undercut areas in case of PMMA could not be avoided. The excessive trimming of acrylic denture base in areas of higher undercut in turn resulted in loss of retention of dentures. The advent of flexible dentures in the field of prosthodontics remedies the problems pertaining to conventional PMMA to some extent.
Valplast and flexiplast were the first flexible denture base material introduced into dentistry in 1956.[8] They are superpolyamides of nylon family.
Currently, flexible denture base has been popularized as a denture base material due to its toxicological safety to patients allergic to metals and resin monomers, ability to engage the undercut areas, and elimination of the use of metal clasps, which enhances the aesthetics. It also provides minimal polymerization errors and non-polymerized materials because of use of injection molding technique. The most important advantage of these resins is its high impact resistance, low porosity, and high light transparency to reflect the color of the underlying gingival tissues.[9]
Furthermore, its advantageous characteristics such as high elasticity and enhanced molding precision than self-cure acrylic resins facilitate denture retention by engaging the undercuts in the denture base design. This meant that metal clasps can be eliminated from denture base, thus enhancing the aesthetics and minimizing the problems from metallic clasps, such as increased stress on the abutment teeth, and allergy.
They also possess several disadvantages, particularly due to their fibrous structure, such as decreased color stability, difficulty in polishing, and necessity of diatorics for mechanical retention of teeth to the denture base.[10] They are retained mechanically by creating diatorics into which denture base resin flows to retain the teeth. This technique is known as Retento-Grip tissue-bearing technique.[11] Their drawback was that mechanical retention of denture teeth to flexible denture base increased the chance of acrylic teeth detachment from the flexible denture base.
Previous studies suggest that modifying the retentive grooves increased the bond strength 58% by increasing the amount of undercut in retentive grooves. The bond strength in such cases depended completely on the tensile strength of the Valplast denture base material at the cervical projection of the material into the retentive grooves.[12]
Materials undergoing plastic deformation during tensile loading are generally classified as ductile.[13] Tensile strength of acrylic is lower than nylon.[14] Acrylic dentures will shatter under high stress, possibly cutting and causing trauma to soft tissues. High stress will cause nylon dentures to undergo elastic and then plastic deformation but never sudden breakage, making it the ideal denture base material for use. Even after strictly adhering to the manufacturer guidelines, the retention gained from these diatoric grooves will not be sufficient enough to stop the teeth from popping out or might even weaken the tooth structure, causing it to shear. Minimal research has been conducted on mechanical properties of Valplast flexible denture bases; there is also paucity of research on the diatoric design within the acrylic denture teeth that provides mechanical retention, which is vital for flexible denture longevity.
Thus, the objective of this study was to compare the bond strength of flexible denture base material with acrylic teeth having different mechanical modifications.
MATERIALS AND METHODS
Methodology
Fabrication of test samples
The specimens consisted of cross-linked acrylic mandibular molar tooth and attached to it a block of Valplast flexible denture base 1.2 cm × 1.2 cm × 2.5 cm dimension [Tables 1–3]. The total sample size was 40 and divided into 4 groups, where each group contained 10 samples.
Table 1.
Materials used in the study
| Sl No. | Material | Manufacturer |
|---|---|---|
| 1 | Mandibular first molar acrylic tooth; Shade/ Mould—A2/93 (S8/7L) | Combination Acry Rock, Badia Polesine (Ro), Italy |
| 2 | Poly vinyl siloxane impression material Putty Consistency | Aquasil, Dentsply, Germany |
| 3 | Modeling Wax | Hindustan Modelling Wax No.2, The Hindustan Dental Products, Hyderabad, India |
| 4 | Dental Stone Type III | Elite model, Italy |
| 5 | Separating medium (DPI Cold Mould Seal) | Dental Products of India, Mumbai, India |
| 6 | Valplast flexible denture base cartridge | Valplast International Corporation, Jericho, NY |
Table 3.
Methodology
| Stages | |
|---|---|
| I | Fabrication of test samples |
| • Selection and preparation of acrylic teeth for the test sample | |
| • Preparation of wax model with acrylic denture teeth | |
| II | Flasking and dewaxing of the samples |
| III | Fabrication of the flexible denture base resin to acrylic tooth test samples |
| IV | Finishing and polishing of the test specimens |
| V | Testing the samples for bond strength evaluation |
| VI | Statistical evaluation |
Table 2.
Armamentarium and equipments
| Sl. No. | Materials | Manufacturer |
|---|---|---|
| 1 | Straight fissure tungsten carbide bur | RA 701L, SS White, Lakewood, NJ |
| 2 | Round tungsten carbide bur | RA 701L, SS White, Lakewood, NJ |
| 3 | Injection molding unit | Changsha Aulen Dental Equipment Co. Ltd, China |
| 4 | Straight micromotor handpiece | NSK Nakanishi Inc., Tokyo, Japan |
| 5 | Universal testing machine | Tec-Sol, Chennai, India |
Group 1 (n = 10): control group—denture teeth without any mechanical modifications as supplied by the manufacturer
Group 2 (n = 10): a round groove 2 mm in diameter and 2 mm deep prepared on the ridge lap surface of the cross-linked teeth with round bur
Group 3 (n = 10): a horizontal slot 2 mm deep, 2 mm wide, and 4 mm long prepared on the ridge lap area of the teeth with straight fissure bur
Group 4 (n = 10): a T-shaped groove 2 mm deep, 2 mm wide, and length of 4 mm mesiodistally and 2 mm buccolingually prepared with a straight fissure bur
The Valplast flexible block was first made out of wax; then a heavy body silicone impression mold was made to fabricate the remaining wax patterns of the acrylic rods by pouring molten wax into mold. Mechanical modifications of specific dimensions were made on the ridge lap surface of the teeth by round bur and straight fissure bur. The end of the wax patterns was then carefully placed on the ridge lap area of the acrylic tooth [Figure 1]. The denture base area around the tooth was waxed up to include the neck of the tooth, as well as mesial and distal areas facilitate the design needed for mechanical retention.
Figure 1.
Wax block attached to the acryrock teeth
Flasking and dewaxing of the samples
Separating medium was applied on the waxed patterns. Dental Stone Type III (Elite model, Italy) slurry was poured into the lower half of the flask, and then the waxed patterns were placed into the stone and sprue was attached to it. Dewaxing was performed and the flasks were allowed to cool.
Fabrication of flexible (nylon) denture base material
The flexible denture base cartridge (flexible nylon granules; Valplast International Corporation, Jericho, NY) [Figure 2] was placed into the heating cylinder and left inside the preheated furnace for 11min to allow the granules to melt. Preheated flask was placed inside the injection unit in horizontal correct position with the aid of the projection at the base of the injection unit. The material was injected into the flask by manual injection unit under a pressure of 5 bars for 5min, cooled, and opened.
Figure 2.
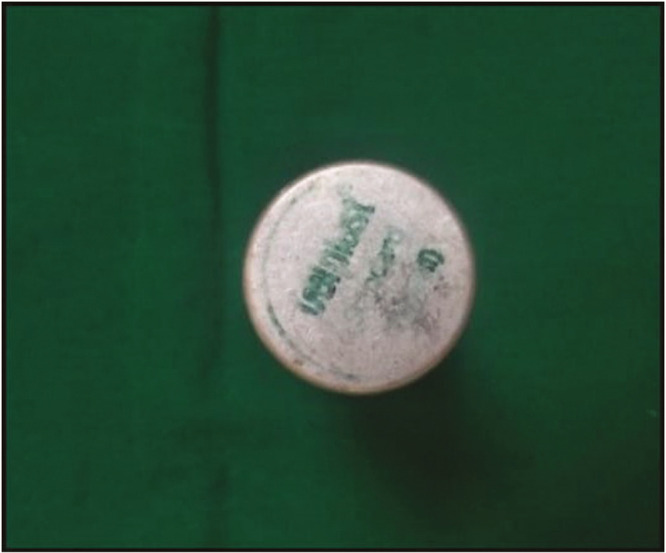
Valplast flexible denture base cartridge
Finishing and polishing of the specimens
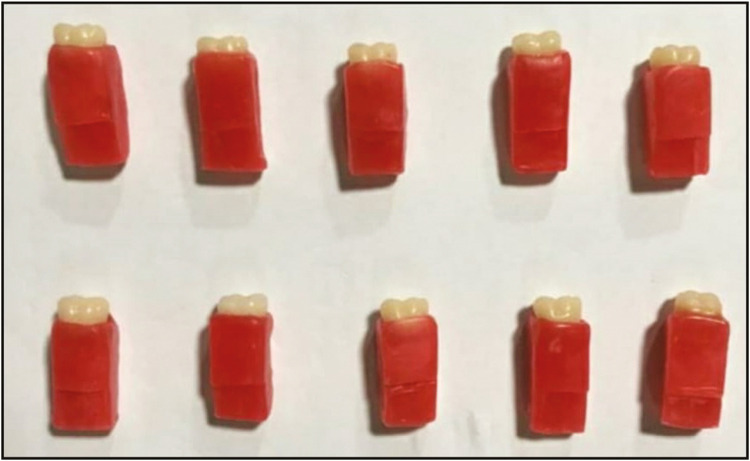
All the samples were finished using silicon carbide paper. Tripoli compound with a rag wheel was used to produce smoothness [Figure 3].
Figure 3.
Finished samples of acryrock teeth attached to flexible denture base
Testing the samples
The samples were subjected to a tensile force with a universal testing machine [Figure 4] at a cross-head speed of 1 mm/min. Load was applied till the cross-linked acrylic tooth separated from the flexible denture base resin.
Figure 4.

Load applied on the test specimen
The bond strengths were recorded and statistically analyzed.
where F is the force applied and A is the area.
Statistical evaluation
SPSS software, version 22.0 (IBM, Armonk, NY), was used for analyzing the data. Mean and standard deviation of bond strength values of all groups were obtained. One-way analysis of variance (ANOVA) was conducted to check for significant difference of bond strength between the test groups. Post hoc test was performed to check for intergroup significance of bond strengths.
RESULTS
ANOVA test was performed to compare the mean bond strength among different groups. The group 1 samples of cross-linked acryrock tooth without any mechanical modifications did not show any bonding to flexible nylon denture base material. Group 2 with round grooves showed mean bond strength value of 1.63MPa [Table 4]. Group 3 with horizontal slot had mean bond strength value of 1.91MPa, and group 4 with T-shaped retentive groove had 2.28MPa. Highest mean bond strength was recorded in group 4, followed by group 3 and group 2. Difference in mean bond strength among the groups was found to be statistically significant. One-way ANOVA was used to determine the significant difference in the average bond strength across different groups. Here we noticed that there is significant difference between the groups with P < 0.001.
Table 4.
Data on the mean and standard deviation of bond strength among three groups (2 [round groove], 3 [horizontal slot], 4 [sandblast and monomer], 5 [dichloromethane]) using one-way ANOVA test
| Groups | N | Mean (MPa) | Std. Deviation | Minimum | Maximum | P value |
|---|---|---|---|---|---|---|
| Group 2 | 10 | 1.63 | 0.22 | 1.36 | 2.02 | |
| Group 3 | 10 | 1.91 | 0.34 | 1.28 | 2.38 | <0.001 |
| Group 4 | 10 | 2.28 | 0.16 | 2.09 | 2.52 |
Group 4 is with highest strength (2.28 ± 0.22) followed by group 3 (1.91 ± 0.34) and group 2 (1.63 ± 0.22).
From Graph 1, it can be noted that the highest bond strength was obtained in group 4 with T-shaped retentive grooves, followed by group 3 with horizontal slot and group 2 with round groove.
Graph 1.

Comparison of the mean bond strength values of group 2 (round groove), group 3 (horizontal slot), and group 4 (T-shaped groove)
Further Tukey’s post hoc test was performed for multiple comparisons [Table 5].
Table 5.
Post hoc test values for intragroup significance
| Groups | N | Mean (MPa) | Std. Deviation | Minimum | Maximum | P value |
|---|---|---|---|---|---|---|
| Group 2 | 10 | 1.63 | 0.22 | 1.36 | 2.02 | |
| Group 3 | 10 | 1.91 | 0.34 | 1.28 | 2.38 | <0.001 |
| Group 4 | 10 | 2.28 | 0.16 | 2.09 | 2.52 |
From post hoc test, we observed that strength of group 4 is significantly different from that of group 2 and group 3 (P value <0.001), whereas bond strength does not vary significantly between group 2 and group 3 (P value = 0.54).
DISCUSSION
The results of this study suggest that the bond strength increases with increase in surface area of the retentive grooves created in the cross-linked acryrock tooth. Valplast flexible denture base material was used for this study because of its advantages over PMMA with respect to patient compliance. Despite the popularity of PMMA, it has several drawbacks like compromised aesthetics due of exposure of metal clasps and difficulty to insert the denture in areas of higher undercut. Hence, nylon denture base polymers are gaining acceptance in clinical practice as denture base materials because of a diverse range of advantageous characteristics such as their high elasticity, which produces minimal dimensional changes during polymerization, and the absence of residual monomers.[9] Even though flexible denture base possess many advantages, popping out of tooth from the denture base continues to be a major conflict of interest.
Debonding of acrylic tooth from the denture base is a major issue faced by patients using flexible dentures. Singh et al.[7] reported 22.2% debonding of acrylic teeth after 18 months in flexible dentures. Darbaret al. determined the prevalence of type of denture fracture and concluded that 33% were due to debonded or detached teeth.[10] In cases of acrylic dentures, Yadav et al.[15] reported that debonding occurs in the body of the tooth rather than in the junction, so there is no need of surface treatment of ridge lap surface, whereas Darbar et al. recommended use of a diatoric placed in the ridge lap of denture teeth attached to flexible denture base because majority of failures were adhesive.[10]
This study compared the bond strength of flexible denture base material with acrylic teeth having different mechanical modifications. The bonding between the flexible nylon denture base material and cross-linked acryrock teeth was purely mechanical, in contrast to the chemical bonding present in acrylic denture bases. This was clear by the absence of bonding in group 1 samples where no mechanical modifications were made on the ridge lap surface of tooth. Krishna et al.[16] stated that chemical surface treatment did not alter the bonding of teeth with flexible denture base material. Among the groups tested, the highest bond strength was noted in group 4, in which T-shaped grooves were made on the ridge lap area, followed by group 3 (rectangular-shaped groove) and least for group 2 (round groove). From this it can be clearly concluded that bond strength increases with increase in surface area of the retentive grooves prepared. In some of the debonded samples, it was seen that the flexible material did not flow completely into the retentive grooves. This could be because of the shrinkage that the Valplast nylon flexible denture base underwent, which was about 2.5%, compared to the conventional PMMA, which was 0.9%, according to Parvizi et al.[8] This decreased the amount of nylon engaging the undercuts in the teeth with prefabricated retentive means, thus minimizing the bond between the teeth and flexible denture base material.[12]
When comparing the bond strength, the group with increased surface area—group 4 (T-shaped retentive groove)—had the increased bond strength value, whereas the difference in the strength value was not statistically significant between group 2 (round-shaped retentive groove) and group 3 (rectangular-shaped retentive groove), although group 3 had increased surface area. This could be probably because of the presence of undercut in group 2, where round bur was used for mechanical modification. Abass et al.[12] stated that modifying the prefabricated retentive means increased bond strength by 58%.[12]
Thus, as per the results obtained in this study, the hypothesis that stated that there is difference in the bond strengths of the acrylic denture teeth to denture base was accepted. The results proved that the control group had the least bond strength when compared with that of the mechanically modified groups. Among the mechanically modified groups, the denture teeth with T-shaped retentive group had the highest bond strength. Thus, the major disadvantages of debonding of acrylic teeth from the flexible denture base can be rectified by incorporating diatoric holes with increased surface area and undercuts within the clinical limitations. Thus, the disadvantage of decreased bond strength while using Valplast denture base with acrylic teeth of prefabricated retentive means could be partially resolved by incorporating more undercuts in the teeth.
In this study, the surface area of the ridge lap surface of the teeth for measuring the bond strength value was analyzed using Image J software.[17] All the samples were measured by the same software for the purpose of standardization. Also, it was ensured that all test pieces were identical. Highly accurate test piece duplication was carried out with silicone, and the same tooth mold was used for all test samples fabricated.
Only one type of flexible denture base material (Valplast) and one type of acrylic tooth (Combination Acryrock; Ruthinium, Badia Polesine, Italy) were used in this study. Other materials could possibly be used in a separate study of the same nature to verify or disprove the findings of this study.
The force applied to denture teeth is a combination of tensile and shear forces. However, it is hardly feasible to simulate 1:1 in an in vitro experiment.[18] There is no standardized test for determining the retention of acrylic denture teeth in flexible nylon denture base materials. In this study, standard test for the retention of acrylic denture teeth to flexible denture base materials was modified to suit the needs of the research to be carried out. Therefore, the results of this study should be further considered and it is recommended that further development of a standard test, especially for acrylic denture teeth in pure nylon denture base materials, should be performed.
CONCLUSION
Within the limitations of this study, the following conclusions were made:
No bonding with flexible nylon denture base material was observed in the group without any mechanical modifications on the ridge lap surface of the tooth.
Significant improvement in bond strength was obtained by increasing the surface area of the retentive grooves on the cross-linked acryrock tooth.
Mechanical undercuts in the retentive grooves increased the bond strength between the flexible nylon denture base and cross-linked acryrock teeth.
Failure type was predominantly adhesive.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ferro KJ, Morgano SM, Driscoll CF, Freilich MA, Guckes AD, Knoernschild KL. The glossary of prosthodontic terms. J Prosthet Dent. 2017;117:e1–05. [Google Scholar]
- 2.Zarb GA, Bolender CL, Carlsson GE. Boucher’s prosthodontic treatment for edentulous patients. St. Louis, MO: Mosby; 1997. [Google Scholar]
- 3.Khindria SK, Mittal S, Sukhija U. Evolution of denture base materials. J Ind Prosthodont Soc. 2009;9:64. [Google Scholar]
- 4.Shankar YR, Krishna P, Sharma S, Srinivas K. Evaluation of bond strength of acrylic teeth to the denture base resins with chemical surface treatment and mechanical modification-An in-vitro comparative study. BFUDJ. 2014;5:169–78. [Google Scholar]
- 5.Anusavice KJ. Phillip’s science of dental materials. 11th ed. St. Louis, MO: Saunders Company; 2004. Autopolymerising denture resins to denture teeth. [Google Scholar]
- 6.Ragher M, Vinayakumar G, Patil S, Chatterjee A, Mallikarjuna DM, Dandekeri S, et al. Variations in flexural strength of heat-polymerized acrylic resin after the usage of denture cleansers. J Contemp Dent Pract. 2016;17:322–6. doi: 10.5005/jp-journals-10024-1848. [DOI] [PubMed] [Google Scholar]
- 7.Singh JP, Dhiman RK, Bedi RP, Girish SH. Flexible denture base material: a viable alternative to conventional acrylic denture base material. Contemp Clin Dent. 2011;2:313–7. doi: 10.4103/0976-237X.91795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parvizi A, Lindquist T, Schneider R, Williamson D, Boyer D, Dawson DV. Comparison of the dimensional accuracy of injection-molded denture base materials to that of conventional pressure-pack acrylic resin. J Prosthodont. 2004;13:83–9. doi: 10.1111/j.1532-849X.2004.04014.x. [DOI] [PubMed] [Google Scholar]
- 9.Katsumata Y, Hojo S, Hamano N, Watanabe T, Yamaguchi H, Okada S, et al. Bonding strength of autopolymerizing resin to nylon denture base polymer. Dent Mater J. 2009;28:409–18. doi: 10.4012/dmj.28.409. [DOI] [PubMed] [Google Scholar]
- 10.Darbar UR, Huggett R, Harrison A. Denture fracture - a survey. Brit Dent J. 1994;176:342. doi: 10.1038/sj.bdj.4808449. [DOI] [PubMed] [Google Scholar]
- 11.Singh K, Aeran H, Kumar N, Gupta N. Flexible thermoplastic denture base materials for aesthetical removable partial denture framework. J Clin Diagn Res. 2013;7:2372–3. doi: 10.7860/JCDR/2013/5020.3527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abass SM, Abdulsahib AJ, Khalaf BS. Bond strength of acrylic teeth to heat cure acrylic resin and thermoplastic denture base materials. Journal of Kerbala University. 2011;9:35–44. [Google Scholar]
- 13.Phillips RW, Anusavice KJ. Phillips’ science of dental materials. St. Louis, MO: Elsevier/Saunders; 2013. [Google Scholar]
- 14.Stern MN. Flexible partials: aesthetic retention for the removable dental prosthesis. Dental Practice. 2007;7:28–9. [Google Scholar]
- 15.Yadav NS, Somkuwar S, Mishra SK, Hazari P, Chitumalla R, Pandey SK. Evaluation of bond strength of acrylic teeth to denture base using different polymerization techniques: a comparative study. J Int Oral Health. 2015;7:54–6. [PMC free article] [PubMed] [Google Scholar]
- 16.Krishna VP, Premalatha A, Babu PJ, Raju DS, Kumar MP, Rao DB. Effect of various chemicals on the bond strength of acrylic tooth and denture base—an in vitro comparative study. J Int Oral Health. 2014;6:100. [PMC free article] [PubMed] [Google Scholar]
- 17.Image J (for Windows) Barcelona, Spain:: Softonic; 2020. [Last accessed on 2019 June 17]. Version: 1.52u. Available from: https://imagej.en.softonic.com . [Google Scholar]
- 18.Palitsch A, Hannig M, Ferger P, Balkenhol M. Bonding of acrylic denture teeth to MMA/PMMA and light-curing denture base materials: the role of conditioning liquids. J Dent. 2012;40:210–21. doi: 10.1016/j.jdent.2011.12.010. [DOI] [PubMed] [Google Scholar]