Abstract
We present a case of a 44-year-old man with biopsy-proven primary vitreoretinal lymphoma (PVRL), who developed multiple ocular recurrences over the course of six years. Recurrences were imaged with color fundus photography, fundus autofluorescence, and optical coherence tomography. This case demonstrates a single patient with a myriad of imaging findings of PVRL as well as response to a variety of therapeutic interventions.
Keywords: Primary vitreoretinal lymphoma, Imaging, Optical coherence tomography, Fundus photograph, Fundus autofluorescence
1. Case report
A 44-year-old man presented with bilateral floaters for 2 years. He had previously undergone bilateral vitrectomy for floaters; no specimens were sent to pathology. Visual acuity was 20/50 in the right eye and 20/15 in the left. Both eyes had 1-2+ large anterior chamber cells, 2+ large chalky white vitreous cells and haze, without obvious fundus lesions. Repeat vitrectomy with cytological/molecular analysis confirmed primary vitreoretinal lymphoma (PVRL). There was no extraocular malignancy. He was initially treated with systemic methotrexate, and over the next 5 years, underwent intravitreal methotrexate ± rituximab, and ocular irradiation for recurrent retinal disease. Six years later, he developed CNS lesions and received intravenous methotrexate, vincristine, and rituximab. Fundus photography, optical coherence tomography (OCT), and autofluorescence (AF) images were used to monitor recurrences and responses to each treatment (Fig. 1, Fig. 2, Fig. 3, Fig. 4). OCT findings include loss of distinct outer retinal laminations (Fig. 1), retinal pigment epithelial (RPE) detachment (Fig. 2B), sub-RPE infiltrates (Fig. 2B), vertical hyperreflective lesions (Fig. 2D), outer retinal deposits (Fig. 2D), inner retinal spike-like lesions (Fig. 3), and preretinal lesions (Fig. 4). AF findings include hyperautofluorescence (Fig. 1). Color photographs demonstrate deep retinal/subRPE lesions (Fig. 1, Fig. 2), and preretinal lesions (Fig. 3, Fig. 4).
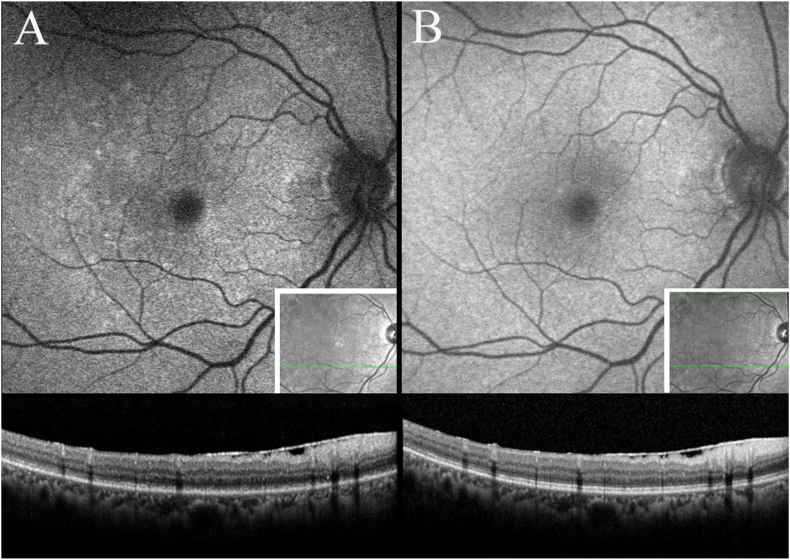
Fig. 1.
Fundus autofluorescence demonstrating hyperautofluorescence, corresponding to disruption of outer retinal laminations (A). Normalization after intravitreal methotrexate (B).
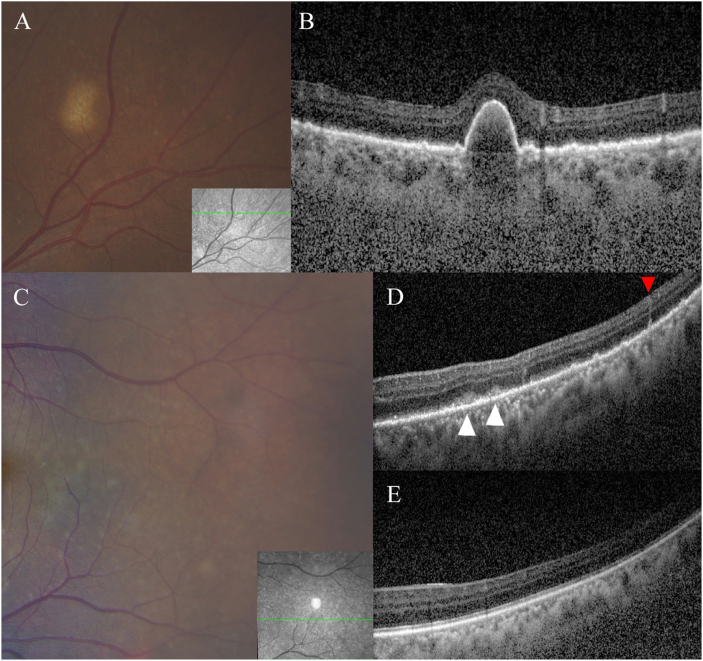
Fig. 2.
Fundus photograph demonstrating a yellow-colored lesion surrounded by smaller cream-colored lesions (A), corresponding to a pigment epithelial detachment with surrounding sub-RPE deposits (B). Fundus photograph of cream-colored lesions (C), corresponding to pre-RPE deposits (white arrowhead) and subclinical vertical hyperreflective lesion (red arrowhead) (D). Resolution after ocular irradiation (E). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
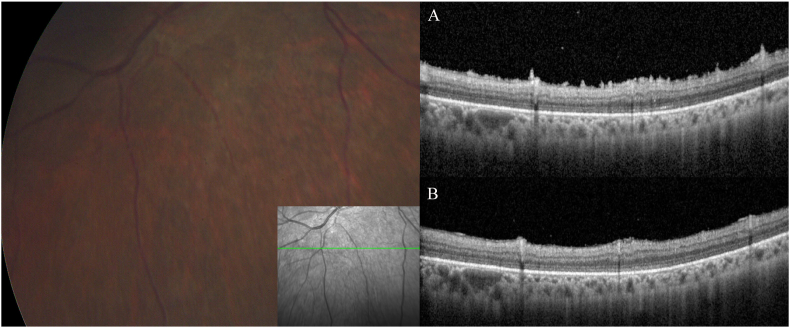
Fig. 3.
Cream-colored lesions on fundus photograph, corresponding to spike-like lesions on the inner retina (A). Resolution after intravitreal methotrexate (B).
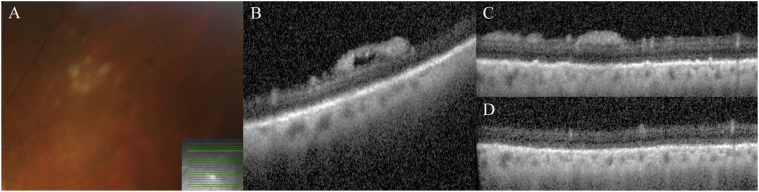
Fig. 4.
Cream-colored lesions on fundus photograph (A), corresponding to pre-retinal deposits (B, C). Resolution after systemic chemotherapy (D).
2. Discussion
PVRL is a high-grade intraocular malignancy. In the largest multicenter study, median age of diagnosis was 60 years, with a wide age range (16–82 years).1 Therefore, PVRL warrants consideration regardless of age. Diagnostic delays of ≥2 years are now less common given greater awareness of disease2 and more well-documented lymphomatous patterns on imaging.3 In this case, evaluation of the first vitrectomy specimen may have led to earlier detection, highlighting the importance of not discarding specimens. This case illustrates the diverse manifestations of PVRL, some commonly recognized but others can be mistaken for other entities. Additionally, we demonstrate patterns of regression with therapy.
3. Conclusion
Vitreoretinal lymphoma has myriad presentations. This case highlights imaging features of commonly and less commonly described findings, all in a single patient.
Financial support
No funding or grant support
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Patient consent
Written consent to publish this case has not been obtained. This report does not contain any personal identifying information.
Declaration of competing interest
D.A.G: consultant and participated in review activities—AbbVie Inc; Consultant—Adverum.
Acknowledgements
Kaitlyn Veto (photographer, technical help).
References
- 1.Grimm S.A., McCannel C.A., Omuro A.M. Primary CNS lymphoma with intraocular involvement: international PCNSL collaborative group report. Neurology. 2008;71:1355–1360. doi: 10.1212/01.wnl.0000327672.04729.8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jang H.S., Sepah Y.J., Sophie R. Longitudinal spectral domain optical coherence tomography changes in eyes with intraocular lymphoma. Journal of Ophthalmic Inflammation and Infection. 2013;3:59. doi: 10.1186/1869-5760-3-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cassoux N., Merle-Beral H., Leblond V. Ocular and central nervous system lymphoma: clinical features and diagnosis. Ocul Immunol Inflamm. 2000;8:243–250. doi: 10.1076/ocii.8.4.243.6463. [DOI] [PubMed] [Google Scholar]