Abstract
Aim
To evaluate the cumulative estimates of reliability and conduct reliability generalization meta-analysis of Cronbach's alpha for the Child Oral Impacts on Daily Performances (C-OIDP) questionnaire.
Methodology
Systematic search of four databases from inception to November 30th, 2019 was performed. Studies that reported Cronbach alpha for the C–OIDP were included. Cronbach's alpha for each publication was used for the meta-analysis. I2 and Q statistics were calculated to assess heterogeneity. Meta-analysis was performed using a random-effects model to derive a pooled estimate of Cronbach's alpha.
Results
Out of 944 publications, data extraction was done from 33 publications after exclusion. The age range among the included publication was from 6 to 19 years. Cronbach's alpha ranged from 0.53 to 0.9. Majority of the publications (n = 21) reported alpha above the benchmark (0.7 and above). Only two publications used condition-specific C-OIDP questionnaires. Twelve publications used self-administered child-OIDP questionnaires. Most of the studies were at a low risk of bias (n = 29). The cumulative alpha was higher in publications with a low ROB (α = 0.74) than a moderate ROB (α = 0.65) The cumulative alpha was 0.73 (SE = 0.02) with a high heterogeneity among the included publications (I2 = 99.28% and Q = 2048.68; P < 0.001).
Conclusion
Overall, the RG estimate of Cronbach's alpha for C-OIDP was above the widely accepted benchmark.
Keywords: Alpha, Cronbach's, Children, Reliability, Oral impacts
1. Introduction
Oral health is defined as a “standard of the oral tissues which contributes to overall physical, psychological and social well-being by enabling individuals to eat, communicate and socialize without discomfort, embarrassment or distress and which enables them to fully participate in their chosen social roles”.1
Locker defined Oral health and subsequently introduced the concept of oral health-related quality of life (OHRQoL), which lead to the voluminous amount of research over the past few decades.1,2 Oral health-related quality of life is defined as a “multidimensional concept that includes a subjective evaluation of the individual's oral health, functional well-being, expectations and satisfaction with care, and sense of self”.3 Over the last few decades, many questionnaires were developed to evaluate OHRQoL, which mainly focussed on adults and subsequently adapted to children and adolescents.
Oral conditions like caries, malocclusion, traumatic dental injuries, fluorosis can have a potential impact on OHRQoL among children and adolescents. There is a vast array of OHRQoL instruments made for use in children and adolescents. Such questionnaires are designed to be self-reported or interviewer-administered, condition-specific or generic, specific to age groups, etc. Many studies evaluated the validity and reliability across populations, disease conditions, cultures, and linguistic variations. One such measure which is commonly used in the literature to assess OHRQoL among children and adolescents is “Child Oral Impacts on Daily Performances” (C-OIDP).4 It was based on the model of oral health consequence, which in turn was based on models of WHO and Locker.1,5 It quantifies the impacts using frequency and severity and differs from the adult version in the recall period.
The C-OIDP is a self-administered questionnaire that measures the extent and impact of an individual's ability to perform regular physical, psychological and social activities that could be compromised due to poor oral health. Children were asked to assess any oral impacts in relation to the eight daily performances (“eating and enjoying food; speaking and pronouncing clearly; cleaning teeth; sleeping and relaxing; smiling; laughing and showing teeth without embarrassment; maintaining usual emotional state without being irritable; study, including going to school and doing homework; and, enjoying contact with people”) in the last three months on a Likert scale. Both the frequency and severity score can be calculated separately and multiplied for getting the total OIDP score.4,6 C-OIDP was translated and adapted to many languages like Thai,7 French,8 Spanish,9 Kiswahili,10 Arabic,11 Italian,12 Brazilian,13 Malay,14 Hebrew,15 Nepali,16 Indonesian,17 and Indian18, 19, 20, 21 (Hindi and Kannada) languages. Internal consistency (Cronbach's alpha) of the C-OIDP in the published studies ranged from 0.53 to 0.9.18,22 Many studies used C-OIDP questionnaire and reported to be a valid and reliable tool to assess the OHRQoL.4,8,10,15, 16, 17, 18,21,23,24
Systematic reviews, methodological quality assessment, and standardized comparisons of C-OIDP and other OHRQoL instruments specific for children and adolescents have been reported in the literature.2,25, 26, 27 However, there was no systematic evaluation of the pooled estimates of the internal consistency reliability of C-OIDP.
Reliability generalization (RG) proposed by Vacha-Haase is the application of meta-analytical methods to explore the variability in the scores of reliability estimates of questionnaires.28 It helps in characterizing the reliability coefficients and identifies the various characteristics of the studies that influenced the scales. It mainly helps in estimating the average and variability of reliability coefficients and identify different associated study characteristics.
With this background, we aimed to evaluate the cumulative estimates of reliability and conduct reliability generalization meta-analysis of Cronbach's alpha for the Child Oral Impacts on Daily Performances (C – OIDP) questionnaire. We also aimed to investigate the various characteristics of the studies that might affect the reliability estimates.
2. Materials and methods
2.1. Selection criteria
Studies that reported Cronbach alpha for the C – OIDP questionnaire were included. Conference proceedings/abstracts, editorials, or letters and studies that reported Cronbach's alpha only for the pilot study were excluded.
2.2. Search strategy
A systematic search of four databases (Pubmed, Scopus, Embase, and CINAHL) from inception to November 30th, 2019 was performed using keywords and free text words (“Oral impacts on daily performance” OR “OIDP” AND child OR children OR adolescents) along with limits like English publications. Title and abstract screening was performed in Rayyan website (https://rayyan.qcri.org/) by two review authors independently (PKC and HS) (Kappa = 0.95). Included publications were considered for full-text screening by two review authors (PKC and YSK) independently (Kappa = 0.93). The third review author clarified the discrepancies if any.
2.3. Evaluation of the risk of bias
All publications were subjected to risk of bias evaluation using a nine-item questionnaire.29 The risk of bias questionnaire was assessed based on 9-itemed questionnaire which included questions on “representation of sample to the national population, true or close representation of sampling frame, random selection, non-response bias, data collection from subjects or proxy, use of acceptable case definition, reliability and validity of the study instrument, same method of data collection for all the subjects, appropriate use of numerator and denominator used for the parameter of interest.” Each question was rated as low risk “0” and high risk as “1” and total score is calculated based on which the study was rated as low risk (0–3), moderate risk (4–6) and high risk of bias (7–9). Two reviewer authors (YSK and HS) have independently performed the assessment (ICC = 0.96), and discrepancies were clarified by a third review author.
2.4. Data extraction
Two review authors independently (YSK and PKC) extracted the data from all the publications, and discrepancies were clarified by a third review author. Reliability between the review authors was assessed using ICC for Cronbach alpha (0.99) and for age (1) and sex (1) and sample size (1). Variables included were age, gender, and geographic distribution, study setting (school/others), Cronbach's alpha, study design, type of administration (language, parent or child/self or interview administered/specific or generic), lowest and highest alpha for items in each study.
2.5. Statistical analysis
Cronbach's alpha for each publication was used for the meta-analysis. I2 and Q statistics were calculated to assess heterogeneity. We used untransformed estimates of alpha, and inverse variance weighting. Meta-analysis was performed using a random-effects restricted maximum likelihood model to derive a pooled estimate of Cronbach's alpha and 95% confidence intervals. Mixed effect model was done to evaluate the role of moderator on the overall estimate of Cronbach's alpha. All the analysis was done using Jamovi software (Version 1.2 https://www.jamovi.org).30 Sub-group analysis was performed as appropriate. Fail-Safe N analysis using the Rosenthal approach was used to assess the publication bias. The funnel plot was plotted using the coefficient of alpha on the x-axis and inverse standard error on the y-axis.
3. Results
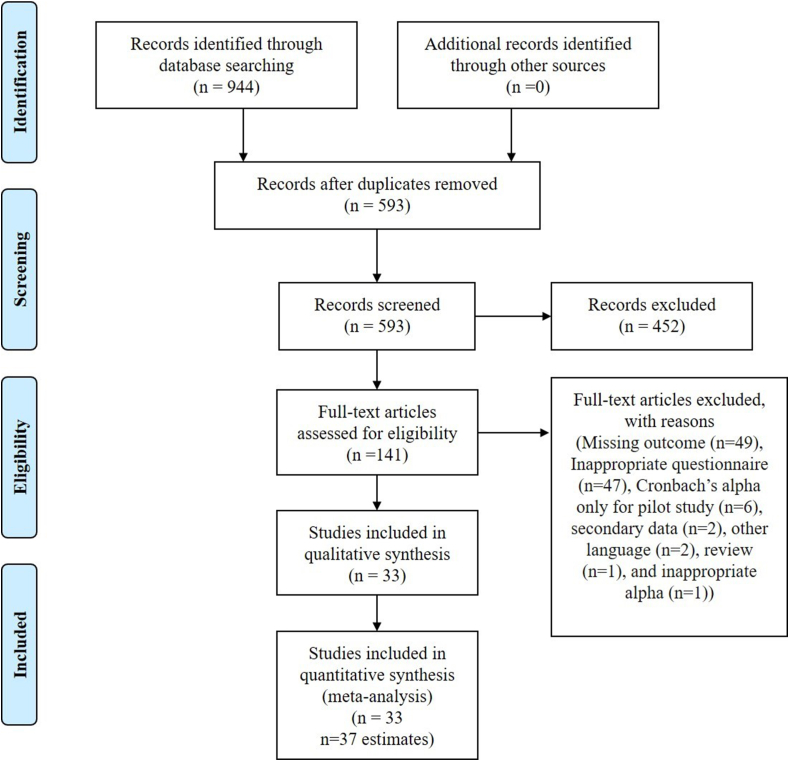
We identified 944 publications from Pubmed (n = 288), Embase (n = 118), Scopus (n = 435) and CINAHL (n = 103) of which 593 publications were eligible for the title and abstract screening. A total of 141 publications were included for full-text screening and 108 publications were excluded due to missing outcome (n = 49), adult OIDP questionnaire (n = 47), Cronbach's alpha only for the pilot study (n = 6), secondary data (n = 2), other languages (n = 2), review (n = 1), and inappropriate alpha (n = 1). Data extraction was done from 33 publications (Fig. 1).
Fig. 1.
Detailing of the publications as per the PRISMA guidelines.
The age range among the included publications was from 6 to 19 years. Only five publications did not report the distribution of gender. The sample size among the included publications ranged from 59 to 7208. Cronbach's alpha ranged from 0.53 to 0.9. The majority of the publications (n = 21) reported alpha above the benchmark (0.7 and above), and 12 publications reported 0.8 and above, and only one publication reported 0.9. Only two publications used condition-specific C-OIDP questionnaires.9,31 Twelve publications used self-administered child-OIDP14,17,18,21, 22, 23,32, 33, 34, 36, 37, 38 questionnaires (see Table 1).
Table 1.
Characteristics of the included studies.
| Author and year | Alpha | N | Setting | Location | Mode of administration | ROB | |
|---|---|---|---|---|---|---|---|
| Gherunpong et al., 20044 | 0.65 | 1100 | S | As | I | L | |
| Tubert-Jeannin et al., 20058 | 0.57 | 414 | S | Eu | I | L | |
| Yusuf et al., 200624 | 0.58 | 228 | S | Eu | I | L | |
| Mtaya et al., 200710 | 0.77 | 1601 | S | Af | I | L | |
| Bernabé et al., 20079 | 0.62 | 805 | S | SA | I | L | |
| Castro et al., 200813 | 0.63 | 342 | S | SA | I | M | |
| Tsakos et al., 200832 | 0.54 | 72 | O | Eu | I | M | |
| 0.55 | 72 | S | |||||
| Krisdapong et al., 20097 | 0.67 | 1066 | S | As | I | L | |
| Mashoto et al., 200949 | 0.85 | 837 | S | Af | I | L | |
| 0.84 | 908 | Af | |||||
| Nurelhuda et al., 201011 | 0.73 | 1109 | S | Eu | I | L | |
| Mashoto et al., 201050 | 0.87 | 1768 | S | Af | I | L | |
| Mbawalla et al., 201033 | 0.85 | 2412 | S | Af | S | L | |
| Bianco et al., 201012 | 0.57 | 530 | S | Eu | I | L | |
| Rosel et al., 201022 | 0.53 | 90 | S | Eu | I | L | |
| 0.53 | 87 | S | |||||
| Cortés-Martinicorena et al., 201034 | 0.68 | 425 | S | Eu | S | L | |
| Castro et al., 201144 | 0.6 | 571 | S | SA | I | L | |
| Raymundo de Andrade et al., 201145 | 0.65 | 59 | O | SA | I | M | |
| Yusof and Jaafar 201214 | 0.8 | 132 | S | As | S | M | |
| Herkrath et al., 201331 | 0.82 | 201 | S | SA | I | L | |
| Agrawal et al., 201320 | 0.6 | 505 | S | As | I | L | |
| Pentapati et al., 201321 | 0.88 | 359 | O | As | S | L | |
| Kushnir et al., 201315 | 0.81 | 179 | O | As | I | L | |
| Carvalho et al., 201352 | 0.7 | 300 | S | SA | I | L | |
| Basavaraj et al., 201419 | 0.87 | 900 | S | As | I | L | |
| Vettore et al., 201642 | 0.76 | 7208 | S | SA | I | L | |
| Åstrøm et al., 201636 | 0.88 | 2412 | S | Af | S | L | |
| 0.88 | 1714 | L | |||||
| Duarte-Rodrigues et al., 201737 | 0.79 | 300 | S | SA | S | L | |
| Singh et al., 201738 | 0.86 | 423 | S | As | S | L | |
| Lazrak et al., 201723 | 0.58 | 1064 | S | Af | S | L | |
| Saujanya et al., 201816 | 0.75 | 1052 | S | As | I | L | |
| Arumrahayu et al., 201817 | 0.72 | 502 | S | As | S | L | |
| Dhawan et al., 201918 | 0.9 | 250 | S | As | S | L | |
| Kassim et al., 201951 | 0.7 | 186 | O | As | I | L | |
S: School/national survey; O: others; ROB: Risk of bias; L: Low risk; M: Moderate risk; I: Interviewer administered; S: self-administered; As: Asia; Af: Africa; SA: South America; Eu: Europe.
3.1. Study setting
A substantial number of studies were conducted in school settings or as part of the national surveys (n = 28) with a cumulative alpha of 0.73 (Table 2).
Table 2.
Subgroup analysis.
| Number of estimates | Number of studies | Estimate (95% CI) | |
|---|---|---|---|
| Continent | |||
| South America | 8 | 8 | 0.7 (0.64–0.76) |
| Europe | 9 | 7 | 0.60 (0.55–0.66) |
| Africa | 8 | 6 | 0.82 (0.75–0.89) |
| Asia |
12 |
12 |
0.77 (0.71–0.83) |
| Study setting | |||
| School or national level survey | 31 | 28 | 0.73 (0.69–0.77) |
| Others |
6 |
5 |
0.71 (0.6–0.82) |
| Risk of Bias | |||
| Low | 32 | 29 | 0.74 (0.7–0.78) |
| Moderate | 5 | 4 | 0.65 (0.55–0.75) |
3.2. Geographic location
Majority of studies were reported from Asia (n = 12), followed by South America (n = 8), Europe (n = 7), with least being Africa (n = 6). The cumulative alpha was found to be highest among studies reported from Africa (α = 0.82) and least among studies from European countries (α = 0.6) (Table 2).
3.3. Risk of bias (RoB) assessment
Most of the studies were at a low RoB (n = 29). The cumulative alpha was higher in publications with a low RoB (α = 0.74) than a moderate RoB (α = 0.65) (Table 2).
Reliability generalization (meta-analysis of Cronbach's alpha coefficient and meta-regression):
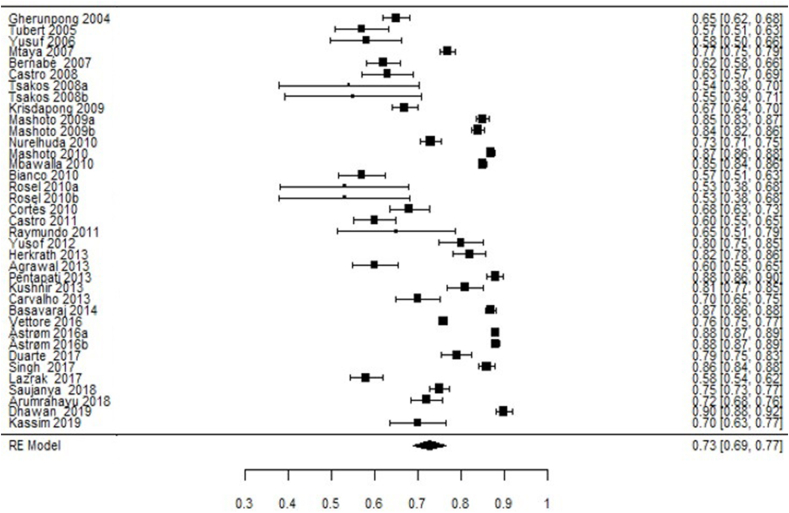
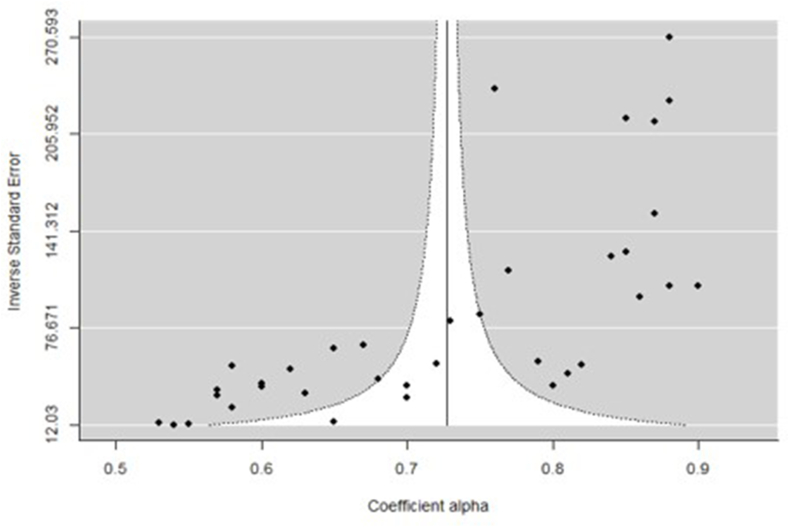
The random-effects model was performed using a restricted Maximum-Likelihood method to calculate the cumulative estimates of Cronbach's alpha and confidence intervals. The number of participants in the included publications ranged from 59 to 7208 with 33 publications (37 estimates) of internal consistency with a combined sample size of 32, 183. The cumulative alpha was 0.73 (SE = 0.02) with a high heterogeneity among the included publications (I2 = 99.28% and Q = 2048.68; P < 0.001) (Fig. 2). The funnel plot for the assessment of bias in publication showed asymmetry (P < 0.001) (Fig. 3).
Fig. 2.
Forest plot for the reliability generalization of child-OIDP.
Fig. 3.
Funnel plot for the assessment of publication bias.
Mixed model analysis was done using study setting, continent and RoB, age, and gender as the moderators. No significant effect was seen with study setting (Coefficient = 0.02; 95% CI: −0.09 – 0.13; R2 = 0%), continent (Coefficient = 0.05; 95% CI: −0.04 – 0.13; R2 = 37.59%), and RoB (Coefficient = −0.06; 95% CI: −0.19 – 0.07; R2 = 0%). A total of 29 and 32 estimates reported the mean of age and gender distribution respectively which were used as a moderators. It was seen that age (coefficient = 0.03; 95% CI: 0.004–0.06; R2 = 13.44%) and gender (coefficient = 0.496; 95% CI: 0.18–0.82; R2 = 22.19%) have significant effect on the overall estimate.
4. Discussion
The coefficient of alpha is one of the essential and popular aspects of reliability assessment in psychometric research and a commonly reported method for indicating internal consistency. The popularity of the alpha could be attributed to its ability to provide estimates from a single questionnaire administered once,39 a readily available tool in statistical software, and one or only reliability method taught to students.
RG is one of the accepted methods for combining the estimates of alpha from multiple publications.28 Our review used the RG method to calculate the cumulative reliability estimates of the child OIDP questionnaire. In general, the advantages of calculating the cumulative alpha help in understanding the integrity of the questionnaire and helps to quantify and predict the variance.
High heterogeneity was seen among the included publications, and results must be interpreted with caution. Overall, the RG estimate of Cronbach's alpha for C-OIDP was above the widely accepted benchmark (0.7).40 Similar values of alpha were reported from national surveys.7,42 George and Malley had provided multiple cut-off points with values < 0.5 is unacceptable, >0.5 is poor, >0.6 is questionable, >0.7 is acceptable, >0.8 is good and >0.9 is excellent which also suggests that alpha values are acceptable when they were >0.7.43 There were no studies which reported alpha below <0.5 and eight estimates from six publications had reported poor alpha values.8,12,22, 23, 24,32 Eight publications showed values in the questionable category.4,9,13,20,34,44,45,7
A substantial number of publications have been excluded for the lack of reporting and clarity on the internal consistency coefficient (n = 49). STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement has not included the reporting of reliability and validity of the instruments or questionnaires used. Quality of reporting of the publications needs to be strengthened, and standard guidelines need to be developed and mandated concerning the reporting of questionnaire surveys. A systematic review of the reporting guidelines for survey research highlighted the deficiencies of STROBE guidelines. Few authors proposed reporting guidelines for surveys which incorporated the concepts of validity and reliability of the survey instruments.46, 47, 48 Future research using questionnaires or surveys should incorporate these guidelines to improve the quality of reporting.
5. Conclusion
Our study highlights the inadequate reporting of the reliability coefficients in the published literature. Pooling of reliability estimates helps in understanding the psychometric properties of the questionnaire in diverse populations. It also helps in understanding the source of variation across studies. Overall, the pooled Cronbach's alpha for C-OIDP questionnaire yielded good reliability estimates. Age and gender have significant influence on the reliability estimates. Future studies should report reliability estimates when using questionnaires.
Source of funding
Nil.
Conflicts of interest
Nil.
Ethics committee approval
Not applicable.
Acknowledgements
Nil.
References
- 1.Locker D. Measuring oral health: a conceptual framework. Community Dent Health. 1988;5(1):3–18. [PubMed] [Google Scholar]
- 2.Thomson W.M., Broder H.L. Oral–health–related quality of life in children and adolescents. Pediatr Clin. 2018;65(5):1073–1084. doi: 10.1016/j.pcl.2018.05.015. [DOI] [PubMed] [Google Scholar]
- 3.Sischo L., Broder H.L. Oral health-related quality of life. J Dent Res. 2011;90(11):1264–1270. doi: 10.1177/0022034511399918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gherunpong S., Tsakos G., Sheiham A. Developing and evaluating an oral health-related quality of life index for children; the CHILD-OIDP. Community Dent Health. 2004;21(2):161–169. [PubMed] [Google Scholar]
- 5.World Health Organization . 1980. International Classification of Impairments, Disabilities, and Handicaps: A Manual of Classification Relating to the Consequences of Disease, Published in Accordance with Resolution WHA29.35 of the Twenty-Ninth World Health Assembly. [Google Scholar]
- 6.Gherunpong S., Tsakos G., Sheiham A. The prevalence and severity of oral impacts on daily performances in Thai primary school children. Health Qual Life Outcome. 2004;2:57. doi: 10.1186/1477-7525-2-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krisdapong S., Sheiham A., Tsakos G. Oral health-related quality of life of 12- and 15-year-old Thai children: findings from a national survey. Community Dent Oral Epidemiol. 2009;37(6):509–517. doi: 10.1111/j.1600-0528.2009.00503.x. [DOI] [PubMed] [Google Scholar]
- 8.Tubert-Jeannin S., Pegon-Machat E., Gremeau-Richard C., Lecuyer M.-M., Tsakos G. Validation of a French version of the Child-OIDP index. Eur J Oral Sci. 2005;113(5):355–362. doi: 10.1111/j.1600-0722.2005.00230.x. [DOI] [PubMed] [Google Scholar]
- 9.Bernabé E., Flores-Mir C., Sheiham A. Prevalence, intensity and extent of Oral Impacts on Daily Performances associated with self-perceived malocclusion in 11-12-year-old children. BMC Oral Health. 2007;7(1):6. doi: 10.1186/1472-6831-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mtaya M., Åstrøm A.N., Tsakos G. Applicability of an abbreviated version of the Child-OIDP inventory among primary schoolchildren in Tanzania. Health Qual Life Outcome. 2007;5(1):40. doi: 10.1186/1477-7525-5-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nurelhuda N.M., Ahmed M.F., Trovik T.A., Åstrøm A.N. Evaluation of oral health-related quality of life among Sudanese schoolchildren using Child-OIDP inventory. Health Qual Life Outcome. 2010;8(1):152. doi: 10.1186/1477-7525-8-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bianco A., Fortunato L., Nobile C.G.A., Pavia M. Prevalence and determinants of oral impacts on daily performance: results from a survey among school children in Italy. Eur J Publ Health. 2010;20(5):595–600. doi: 10.1093/eurpub/ckp179. [DOI] [PubMed] [Google Scholar]
- 13.Castro R.A.L., Cortes M.I.S., Leão A.T. Child-OIDP index in Brazil: cross-cultural adaptation and validation. Health Qual Life Outcome. 2008;6(1):68. doi: 10.1186/1477-7525-6-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yusof Z.Y.M., Jaafar N. A Malay version of the child oral impacts on daily performances (Child-OIDP) index: assessing validity and reliability. Health Qual Life Outcome. 2012;10(1):63. doi: 10.1186/1477-7525-10-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kushnir D., Natapov L., Ram D., Shapira J., Gabai A., Zusman S.P. Validation of a Hebrew version of the child-OIDP index, an oral health-related quality of life measure for children. Oral Health Prev Dent. 2013;11(4):323–330. doi: 10.3290/j.ohpd.a30173. [DOI] [PubMed] [Google Scholar]
- 16.Saujanya K., Marja-Liisa L., Manoj H., Jari P., Vuokko A. Adaptation and validation of a Nepali version of the child-oral impacts on daily performances index (C-OIDP) Community Dent Health. 2018;35(2):119–126. doi: 10.1922/CDH_4164Saujanya08. [DOI] [PubMed] [Google Scholar]
- 17.Arumrahayu W., Maharani D.A., Adiatman M. An Indonesian version of child oral impact on daily performances (C-OIDP): assessing validity and reliability. J Int Dent Med Res. 2018;11(3):1049–1052. [Google Scholar]
- 18.Dhawan P., Singh A., Agarwal A., Aeran H. Psychometric properties of Hindi version of child oral impact on daily performances (C-OIDP) index amongst school children in North India. J Oral Biol Craniofac Res. 2019;9(1):10–13. doi: 10.1016/j.jobcr.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Basavaraj P., Sunil M.K., Nagarajappa R., Ashish S., Ramesh G. Correlation between oral health and child-OIDP index in 12- and 15-year-old children from modinagar, India. Asia Pac J Publ Health. 2014;26(4):390–400. doi: 10.1177/1010539513510553. [DOI] [PubMed] [Google Scholar]
- 20.Agrawal N., Pushpanjali K., Garg A.K. The cross cultural adaptation and validity of the child-OIDP scale among school children in Karnataka, South India. Community Dent Health. 2013;30(2):124–126. [PubMed] [Google Scholar]
- 21.Pentapati K.C., Acharya S., Bhat M., Krishna Rao S.V., Singh S. Oral health impact, dental caries, and oral health behaviors among the National Cadets Corps in South India. J Invest Clin Dent. 2013;4(1):39–43. doi: 10.1111/j.2041-1626.2012.00134.x. [DOI] [PubMed] [Google Scholar]
- 22.Rosel E., Tsakos G., Bernabé E., Sheiham A., Bravo M. Assessing the level of agreement between the self- and interview-administered Child-OIDP. Community Dent Oral Epidemiol. 2010;38(4):340–347. doi: 10.1111/j.1600-0528.2010.00533.x. [DOI] [PubMed] [Google Scholar]
- 23.Lazrak L., Bourzgui F., Serhier Z., Diouny S., Othmani M. Crosscultural translation and adaptation of the Moroccan version of the child-oral impacts on daily performance 11–14 oral health-related quality of life. J Int Oral Health. 2017;9(5):236. doi: 10.4103/jioh.jioh_84_17. [DOI] [Google Scholar]
- 24.Yusuf H., Gherunpong S., Sheiham A., Tsakos G. Validation of an English version of the Child-OIDP index, an oral health-related quality of life measure for children. Health Qual Life Outcome. 2006;4(1):38. doi: 10.1186/1477-7525-4-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gilchrist F., Rodd H., Deery C., Marshman Z. Assessment of the quality of measures of child oral health-related quality of life. BMC Oral Health. 2014;14(1):40. doi: 10.1186/1472-6831-14-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zaror C., Pardo Y., Espinoza-Espinoza G. Assessing oral health-related quality of life in children and adolescents: a systematic review and standardized comparison of available instruments. Clin Oral Invest. 2019;23(1):65–79. doi: 10.1007/s00784-018-2406-1. [DOI] [PubMed] [Google Scholar]
- 27.Hettiarachchi R.M., Kularatna S., Byrnes J., Scuffham P.A. Pediatric quality of life instruments in oral health research: a systematic review. Value Health. 2019;22(1):129–135. doi: 10.1016/j.jval.2018.06.019. [DOI] [PubMed] [Google Scholar]
- 28.Vacha-Haase T. Reliability generalization: exploring variance in measurement error affecting score reliability across studies. Educ Psychol Meas. 1998;58(1):6–20. doi: 10.1177/0013164498058001002. [DOI] [Google Scholar]
- 29.Hoy D., Brooks P., Woolf A. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–939. doi: 10.1016/j.jclinepi.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 30.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Software. 2010;36(3):1–48. doi: 10.18637/jss.v036.i03. [DOI] [Google Scholar]
- 31.Herkrath F.J., Rebelo M.A., Herkrath A.P., Vettore M.V. Comparison of normative methods and the sociodental approach to assessing orthodontic treatment needs in 12-year-old schoolchildren. Oral Health Prev Dent. 2013;11(3):211–220. doi: 10.3290/j.ohpd.a30168. [DOI] [PubMed] [Google Scholar]
- 32.Tsakos G., Bernabe E., O'Brien K.D., Sheiham A., de Oliveira C.M. Comparison of the self-administered and interviewer-administered modes of the Child-OIDP. Health Qual Life Outcome. 2008;6(1):40. doi: 10.1186/1477-7525-6-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mbawalla H.S., Masalu J.R., Åstrøm A.N. Socio-demographic and behavioural correlates of oral hygiene status and oral health related quality of life, the Limpopo - arusha school health project (LASH): a cross-sectional study. BMC Pediatr. 2010;10(1):87. doi: 10.1186/1471-2431-10-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cortés-Martinicorena F.J., Rosel-Gallardo E., Artázcoz-Osés J., Bravo M., Tsakos G. Adaptation and validation for Spain of the child-oral impact on daily performance (C-OIDP) for use with adolescents. Med Oral Patol Oral Cir Bucal. 2010;15(1) doi: 10.4317/medoral.15.e106. [DOI] [PubMed] [Google Scholar]
- 36.Åstrøm A.N., Lie S.A., Mbawalla H. Do self-efficacy and depression predict oral impacts on daily performances across time? A 2-yr follow-up of students in Tanzania. Eur J Oral Sci. 2016;124(4):358–367. doi: 10.1111/eos.12274. [DOI] [PubMed] [Google Scholar]
- 37.Duarte-Rodrigues L., Ramos-Jorge J., Drumond C.L., Diniz P.B., Marques L.S., Ramos-Jorge M.L. Correlation and comparative analysis of the CPQ8-10 and child-OIDP indexes for dental caries and malocclusion. Braz Oral Res. 2017;31:e111. doi: 10.1590/1807-3107bor-2017.vol31.0111. [DOI] [PubMed] [Google Scholar]
- 38.Singh A., Dhawan P., Gaurav V., Rastogi P., Singh S. Assessment of oral health-related quality of life in 9-15 year old children with visual impairment in Uttarakhand, India. Dent Res J. 2017;14(1):43. doi: 10.4103/1735-3327.201132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thompson Bruce. Sage Publications; 2002. Score Reliability: Contemporary Thinking on Reliability Issues. [Google Scholar]
- 40.Jum C. second ed. McGraw-Hill; 1978. Nunnally. Psychometric Theory. [Google Scholar]
- 42.Vettore M.V., Meira G. de F., Rebelo M.A.B., Rebelo Vieira J.M., Machuca C. Multimorbidity patterns of oral clinical conditions, social position, and oral health-related quality of life in a population-based survey of 12-yr-old children. Eur J Oral Sci. 2016;124(6):580–590. doi: 10.1111/eos.12304. [DOI] [PubMed] [Google Scholar]
- 43.George D., Mallery P. ninth ed. 2008. SPSS for Windows Step by Step: A Simple Guide and Reference, 16.0 Update. [Google Scholar]
- 44.Castro R. de AL., Portela M.C., Leão A.T., de Vasconcellos M.T.L. Oral health-related quality of life of 11- and 12-year-old public school children in Rio de Janeiro. Community Dent Oral Epidemiol. 2011;39(4):336–344. doi: 10.1111/j.1600-0528.2010.00601.x. [DOI] [PubMed] [Google Scholar]
- 45.Raymundo de Andrade L.H., de Souza Rocha B., Castro G.F., Ribeiro de Souza I.P. Impact of oral problems on daily activities of HIV-infected children. Eur J Paediatr Dent. 2011;12(2):75–80. [PubMed] [Google Scholar]
- 46.Draugalis J.R., Coons S.J., Plaza C.M. Best practices for survey research reports: a synopsis for authors and reviewers. Am J Pharmaceut Educ. 2008;72(1):11. doi: 10.5688/aj720111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Burns K.E.A., Duffett M., Kho M.E. A guide for the design and conduct of self-administered surveys of clinicians. Can Med Assoc J. 2008;179(3):245–252. doi: 10.1503/cmaj.080372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kelley K. Good practice in the conduct and reporting of survey research. Int J Qual Health Care. 2003;15(3):261–266. doi: 10.1093/intqhc/mzg031. [DOI] [PubMed] [Google Scholar]
- 49.Mashoto KO, Astrøm AN, David J, Masalu JR. Dental pain, oral impacts and perceived need for dental treatment in Tanzanian school students: a cross-sectional study. Health Qual Life Outcomes. 2009;7:73. doi: 10.1186/1477-7525-7-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mashoto KO, Åstrøm AN, Skeie MS, Masalu JR. Changes in the quality of life of Tanzanian school children after treatment interventions using the Child-OIDP. Eur J Oral Sci. 2010;118(6):626–634. doi: 10.1111/j.1600-0722.2010.00776.x. [DOI] [PubMed] [Google Scholar]
- 51.Kassim S, Bakeer H, Alghazy S, Almaghraby Y, Sabbah W, Alsharif A. Socio-Demographic Variation, Perceived Oral Impairment and Oral Impact on Daily Performance among Children in Saudi Arabia. Int J Environ Res Public Health. 2019;16(14):2450. doi: 10.3390/ijerph16142450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carvalho JC, Rebelo MAB, Vettore MV. The relationship between oral health education and quality of life in adolescents. Int J Paediatr Dent. 2013;23(4):286–296. doi: 10.1111/ipd.12006. [DOI] [PubMed] [Google Scholar]