EXECUTIVE SUMMARY
The 2019-2020 Academic Affairs Committee was charged with identifying promising practices in academic-practice partnerships and professional pharmacy organization initiatives that are accelerating the transformation of a workforce prepared to assume responsibility for society’s medication use needs in 2030 and determining the role AACP can plan in supporting these partnerships and initiatives. The committee identified a set of ideal principles, characteristics, and design elements of a high-quality, large-scale workforce development program. The committee also categorized current mechanisms for professional workforce development, in addition to identifying their strengths and weaknesses, with the realization that novel approaches are needed to accomplish the goal of large-scale workforce transformation. This report also highlights two existing initiatives aligned with accelerating the transformation of the workforce (ie, the Community Pharmacy Enhanced Services Network (CPESN) ACT (Academia-CPESN Transformation) Pharmacy Collaborative and the American Pharmacists Association ADVANCE platform) and is proposing a policy statement affirming AACP’s support. Furthermore, the committee is proposing another policy statement supporting colleges and schools of pharmacy taking an active role in implementing innovative and novel approaches for the development of the current workforce. In order to truly understand the many factors influencing large-scale workforce transformation, the committee is also proposing a stakeholder conference with a wide range of participants and a targeted set of questions focused on current and future needs.
Keywords: workforce, development, post-graduate training, continuing professional development, pharmacy services, practice change, practice advancement
INTRODUCTION AND COMMITTEE CHARGES
President Todd Sorensen charged the 2019-20 Academic Affairs Committee (AAC) to critically examine issues related to workforce development and identify strategies to meet medication use needs in the future.1 The specific charges are as follows:
1. Extend the work of the 2018-19 Argus Commission by identifying promising practices in academic-practice partnerships that are accelerating the transformation of a workforce prepared to assume responsibility for society’s medication use needs in 2030.
2. Identify the mechanisms through which professional pharmacy organizations are supporting workforce development and consider opportunities for individual schools and/or AACP to influence these efforts to collaborate with these entities.
3. Determine the role AACP should play in supporting schools in efforts to grow their influence in workforce development.
4. Define strategies and draft an action plan for AACP's role in supporting school engagement in driving workforce development with respect to the knowledge and skills required to accelerate practice transformation.
The AAC conducted their work primarily using conference calls via GoToMeeting and convened for an in-person meeting in January 2020 in Rosslyn, VA. This year’s AAC reaffirms several existing policies regarding postgraduate education and the role of residencies and fellowships, in addition to proposing two new policies related to AACP’s role in supporting schools/colleges and profession-wide initiatives that result in further development of the current workforce.
BACKGROUND
Evolving PharmD curricula to prepare collaboration-ready graduates to succeed in a value-based health care system has been a long-held priority of AACP and its member schools and colleges of pharmacy. However, there is an entire workforce that must gain new knowledge and skills in order to be mobile in the current [and future] health care marketplace.1 While more traditional forms of postgraduate education have played a critical role in this space (eg, residencies, fellowships), they cannot meet all of the needs for pharmacists who are currently out in the workforce. In 2020, the ASHP applicant match rate was 63% for PGY1 programs and 73% for PGY2 programs, with new graduates having the overwhelming advantage in the process (95.5% of matched PGY1 applicants).2 Furthermore, although the number of PGY1 positions has increased 17.8% in the last five years from 3332 in 2016 to 3924 in 2020, the number of available positions is still only about one fourth that of the number of PharmD graduates entering the workforce each year, with almost 15,000 degrees conferred in 2018.3-5 Although residency training is a valuable method for developing one’s skills and abilities to care for patients, there must be other options available to more efficiently develop the current workforce in a rapidly evolving health care system.
In reviewing the committee charges, some additional context and clarifications were helpful for helping the group focus on the task at hand. First, the term “academic-practice partnerships” must be interpreted much more broadly than practice sites affiliated with a school or college of pharmacy. In these partnerships, the term “academic” still means academic pharmacy, but the term “practice” should be interpreted very broadly, ranging from individual pharmacists interested in pursuing a different career path than their current role, to employers needing assistance with up-training their staff to expand their pharmacist-provided services. In addition to the more traditional scenarios encountered during these discussions (ie, ambulatory care practice), there are many other applications for such partnerships, including information technology, pharmacogenomics, personalized medicine, and other advances in medicine that have not yet been discovered. When the profession transitioned to the PharmD degree as the requirement for entry-level practice, schools and colleges set up programs to offer the PharmD to those in the current workforce who wanted it. Most importantly, these programs were developed with the needs of practicing pharmacists in mind, and therefore delivered in a way that was most easily accessible to them. How can the same principles be applied to recent and future advancements to the health care system?
Based on the charges set forth for the committee and the direction provided by President Sorensen, the AAC generated four actionable goals related to the role of AACP and academic pharmacy in developing the pharmacist workforce.
GOAL 1: Create a repository of training programs related to workforce development
The committee’s first two charges were directly related to identifying the current landscape of existing work in this area, including within academic pharmacy and by other professional pharmacy organizations. Looking internally within academic pharmacy, the AAC was interested in better understanding what each AACP member institution was doing related to development of the current pharmacist workforce.
Committee members felt there is likely an abundance of activity at the local level, including continuing education (CE) programming and partnerships with state, regional, and national pharmacy associations. However, committee members expressed concern about reaching out directly to each individual school and college of pharmacy for two reasons. First, there were significant concerns related to survey fatigue and the inability to obtain an adequate sampling of the Academy, especially since other departments and committees within AACP were having difficulties with survey response rates. Second, AAC members had to do quite a bit of baseline work in the beginning of the year to get all members on the same page regarding the terminology and expectations of the charges, resulting in concerns that the specific request(s) within the survey to member schools would come across unclear and result in more confusion. Therefore, rather than attempting to build a comprehensive survey, the AAC decided to use a backwards design approach to the first charge; the committee was asked to identify the ideal principles, characteristics, and design elements of a high-quality program for developing the current pharmacist workforce, specifically targeting “mid-career” pharmacists approximately 10-20 years out from completing their PharmD program. Committee members were invited to openly contribute thoughts and ideas to a Google Doc for a period of two weeks, as well as comment on and/or elaborate upon each other’s contributions. After everyone had an opportunity to contribute their perspectives, the comments were organized into themes, including who should be involved in developing and delivering a program, what the program might entail, when and where the program would be offered, why a program would be developed, how the program would be developed, and other important factors and considerations (Table 1).
Table 1.
Ideal Principles, Characteristics, and Design Elements of a High-Quality Workforce Development Program
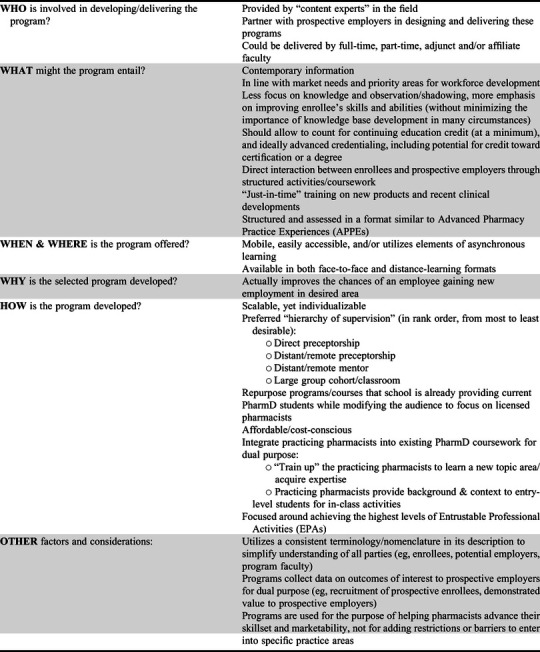
Overall, the committee felt that the profession is in need of training opportunities beyond the traditional knowledge-based CE offerings, and a transition to the Continuing Professional Development approach has never been more critical.6,7 It is imperative that pharmacists reflect on any existing deficits in their knowledge, skills, and abilities in order to determine the most appropriate training opportunity to pursue. However, these workforce development programs must be designed from the perspective of what employers are actually looking for in order to increase the overall value and utility of this training. The cost of these programs to individual pharmacists will be critical, as enrollees would likely be pharmacists in between jobs or looking to transition into a different area of practice, because in both cases, there is no employer sponsoring, providing, or otherwise supporting this additional training. If an employer group is involved, there may be an opportunity or need to develop the knowledge, skills, and abilities of their staff in a structured manner over a relatively short period of time. In all these scenarios, the schools/colleges of pharmacy can serve the profession, either as a go-to source for quickly up-training groups of pharmacists or serving as a neutral third party to help train practicing pharmacists to do something outside of their current job.
The other aspect of this charge involved determining what professional associations are currently offering in the area of workforce development for practicing pharmacists. Because the number of professional organizations was a relatively small number of groups to investigate and professional association websites tend to be easier to navigate than university websites, the committee decided to review currently available offerings. During this search, it quickly became clear that there was a wide variety of offerings available, but they all fit within a limited set of categories. Therefore, rather than catalog every program available, the committee decided to put forth a framework for categorizing workforce development programs (Table 2), with a focus on the strengths and limitations of each, from the perspective of successfully developing the current pharmacist workforce.
Table 2.
Current Mechanisms for Professional Workforce Development
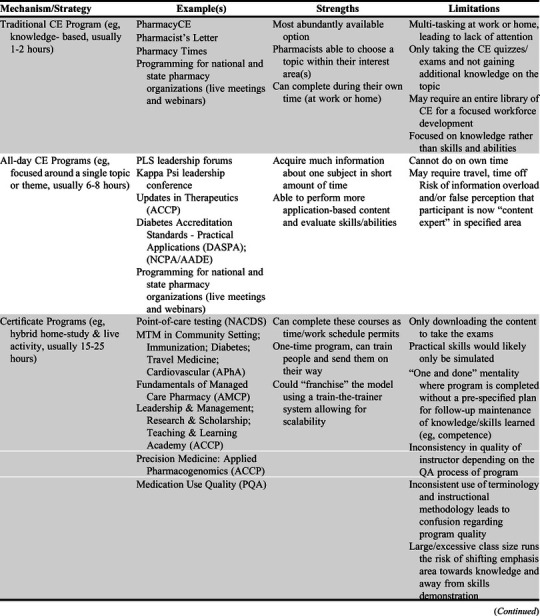
Overall, the committee identified that opportunities abound in multiple areas for pharmacists to engage in professional development, especially in the area of traditional knowledge-based continuing education. Although there is evidence that an increase in knowledge can improve self-confidence in a specific content area, knowledge and self-confidence are only one aspect of the current situation.8-10 Anecdotally, employers are emphasizing skills and abilities more than knowledge of therapeutic content when identifying prospective candidates, so a shift in focus towards more interactive workforce development programs is warranted to give participants more hands-on experience in the area(s) in which they are seeking additional training (eg, interactive workshop, apprenticeship/consultancy). Similarly, although board certification is focused on acquisition and application of knowledge, becoming board certified can demonstrate to potential employers an applicant’s ongoing commitment to maintaining competence in a specific area of practice. Lastly, the committee felt it was important to include networking platforms and niche conferences in the mix of workforce development modalities. Although these are not directly used to train or otherwise educate the workforce, they help to connect people to each other, and allow current employers to identify new talent in their field.
In creating a repository of training programs for workforce development, individual programs should identify how they meet the ideal principles, characteristics, and design elements when submitting for inclusion (Table 1). The specifics of where this repository will be hosted and maintained is still under consideration. The initial idea was to utilize space on the AACP website, similar to how the AACP Consultants and Speakers Bureau is set up.11 However, in order to increase efficiency and intraprofessional collaboration, an alternative solution is to collaborate with the American Pharmacists Association to house these professional development opportunities within a platform they have been developing specifically for this purpose, APhA ADVANCE.12 More information on this initiative will be discussed later on in this report, under Goal 2.
GOAL 2: Align with other organizations/associations providing Continuous Professional Development (CPD) initiatives focused on large-scale pharmacist workforce development
As noted earlier, large-scale pharmacist workforce development will require a collaborative effort between multiple entities, including academic pharmacy. With this thought in mind, the AAC sought out other initiatives that aligned with large-scale pharmacist workforce development, consistent with Charge #2. Over the course of the year, two emerging initiatives caught the attention of the committee members.
Community Pharmacy Enhanced Services Network (CPESN USA) & ACT (Academia-CPESN Transformation) Pharmacy Collaborative
CPESN USA is a clinically integrated network of community pharmacies across America that coordinates patient care with broader care teams to provide medication optimization activities and enhanced services for high-risk patients.13 The primary objective of CPESN USA is to improve patient outcomes through enhanced patient care services in the community pharmacy setting. In order to expand the impact of these clinically integrated networks, the ACT Pharmacy Collaborative was developed as an operational learning and acting collaborative between colleges and schools of pharmacy and clinically integrated networks of community-based pharmacies to support the transformation of community-based pharmacy practice from a product-based care model to a community-based pharmacy care delivery model.14 Specifically, the ACT Pharmacy Collaborative aims to achieve the following:
1. Unite schools and colleges of pharmacy and pharmacist leaders nationwide with a common focus to transform community-based pharmacy practice;
2. Mobilize stakeholders and resources to support and facilitate implementation of community-based pharmacy care; and
3. Amplify the development and implementation of sustainable community-based pharmacy care delivery.
Community pharmacies are easily accessible and the first place where members of the community meet a pharmacist for their health care needs. There is a significant need to transform the traditional, product-focused practice model into a patient-centered care model. Hence, this Collaborative allows schools to leverage their research and clinical expertise to improve care delivery models and evaluate relevant outcomes in community pharmacy settings, while benefiting from the availability of resources to integrate during PharmD coursework with real-world applicability and high-caliber experiential sites in the community pharmacy setting.
To transform community-based pharmacy practice, several initiatives are taking place within the ACT Pharmacy Collaborative such as National Day of Service, Legislative Day, student scholarships, and the Patient Case Challenge. Through these initiatives, community pharmacists, student pharmacists, and faculty from colleges and schools of pharmacy have come together to create, support, implement and establish innovative patient care services in the community pharmacy. Community practice faculty at colleges and schools of pharmacy are actively participating in bi-weekly ACT webinars, sharing new pilot programs and student experiences, and implementing new resources such as the eCare Plan documentation platform. In addition, there is an annual ACT Patient Case Challenge that enables pharmacists and student pharmacists to collect and share impactful patient cases that demonstrate enhanced patient care provided in the community pharmacy setting. Additional opportunities to engage with this initiative include a new AACP Connect Community for members titled “ACT Pharmacy Collaborative” and a Community Pharmacy Practice Transformation Workshop sponsored by AACP, CPESN and the Community Pharmacy Foundation hosted by the University of Pittsburgh in November 2020. This will be a highly interactive team format and cover topics such as eCare Plan documentation, workforce transformation, and scaling innovation through partnerships.
American Pharmacists Association (APhA) ADVANCE
APhA ADVANCE is a platform designed for the advancement of continuing professional development (CPD) for the pharmacy profession.12 It can be utilized by pharmacists and student pharmacists and is designed to offer customized training opportunities based on the individual user’s self-identified desired areas of development. Currently in pilot-testing form, it offers a limited number of assessments and training pathways related to immunizations, opioid safety, community pharmacy management, diabetes, and medication management, but the capacity to incorporate additional training programs and opportunities is unlimited. The platform ensures comprehensive professional development across a wide spectrum of topics related to patient care, management, leadership, community service, and well-being/resilience. It builds off the APhA Career Pathway Evaluation Program for Pharmacy Professionals, allows tracking of strengths and gaps within the workforce, and provides data to demonstrate the need for additional training.15
AACP has a memorandum of understanding with APhA regarding joint commitment to ADVANCE Briefly, this collaboration serves to:
1. Engage to promote the use of ADVANCE within colleges and schools of pharmacy through meetings and other channels of communication;
2. Explore the development of pathways (including activities and experiences) that would add value to colleges and schools of pharmacy (eg, practice transformation; preceptor development; career/workforce development);
3. Explore and pursue the development and implementation of a data sharing strategy that identifies data elements and creates efficient data transfer between PharmCAS, ADVANCE, and Pharmacy Profiles;
4. Identify strategies to inform data analytics and the development of aggregate reports intended to decrease the burden associated with colleges and schools of pharmacy accreditation;
5. Identify the need for and structure of activity mapping within ADVANCE to facilitate reporting and achievement of CAPE Outcomes; and
6. Facilitate the collection of strategic input on the functionality, use, applications, and effectiveness of ADVANCE to meet the needs of colleges and schools of pharmacy.
In addition to the two initiatives introduced above, discussions with other professional associations regarding workforce development have occurred and will continue to occur over the coming months, including conversations with members from the Joint Commission of Pharmacy Practitioners. As one example, an “Exploring Practice Transformation and Workforce Development” workshop occurred in February 2020 with representatives from AACP, ACCP, APhA, and BPS. One idea that resulted from that discussion was micro-credentialing and stackable credentials, which may be particularly suitable for non-traditional students and practicing pharmacists who are trying to balance their professional development needs with other responsibilities, such as full-time jobs. Another initiative engaged in workforce transformation where AACP is involved is the Get the Medications Right (GTMR) Institute, an initiative focused on implementing a personalized, patient-centered, systematic, and coordinated approach to medication use to vastly improve outcomes and reduce overall health care costs.16 The plan is to expand these conversations and reach out to other associations/organizations, with the goal of incentivizing innovation, engaging stakeholders, removing barriers and developing meaningful solutions.
GOAL 3: Determine what/how AACP and academic pharmacy can contribute to a stakeholder conference related to addressing current/future needs for large-scale workforce development
Acknowledging that employers and pharmacists need these workforce development programs, and currently available opportunities may not fully meet these needs on a large-scale basis; it is imperative that the profession develop a consensus regarding how to address the current and future needs for large-scale workforce development. The profession has used stakeholder conferences in the past to tackle similarly large issues such as the future of clinical practice in pharmacy, quality in pharmacy education, and most recently, pharmacist well-being and resilience.17-19 As workforce issues impact the entire profession, the committee felt it was important to at least identify what this type of conference should address, with the understanding that such an endeavor would need to be endorsed at a much higher level than AACP as a single organization, such as by the Joint Commission of Pharmacy Practitioners (JCPP).
The role of the pharmacist in the current health care system has been described previously, including provider of medication management, medication reconciliation, preventative care, and patient education services, especially through interprofessional and collaborative care models.20 In order to better comprehend the emerging and future roles pharmacists serve within the health care system, we must first identify what the needs are within the rapidly evolving health care system. Current health care trends are evolving with shifting demographics, alternative payment models, increasing number of integrated health systems, added emphasis on quality over quantity of care, increasing patient engagement and shared-decision making, and advances in technology.21,22 Review of these emerging health care trends and future opportunities for the pharmacy profession would help to identify how and in what areas workforce transformation is needed, including which specific knowledge, skills, and abilities need to be developed to help transform the pharmacist workforce to more readily meet these needs of the health care system.
A stakeholder conference can help the profession more accurately identify barriers and develop meaningful solutions to the issue of large-scale workforce development. In order to have a meaningful impact, this conference needs to be a collaborative effort across a wide cross-section of participants, including representatives from within the profession (eg, practitioners, regulators, educators, accreditors) and perhaps more importantly, outside the profession (eg, payers, other health care professionals, patient advocacy groups, and health care consumers). Practitioners need to be the pharmacists who are closest to patient care. While the perspectives of district or corporate-level pharmacists are valuable, the perspective of pharmacists engaged in patient care are of particular value in determining the true needs of the workforce. In addition, the stakeholder conference should not be exclusive to pharmacists talking to pharmacists about pharmacists, but rather other entities within the health care system need to be present in order to effect actual large-scale change. Academic pharmacy, represented by AACP, can provide insight into how schools can leverage their existing educational infrastructure to facilitate large-scale workforce transformation. The insights of payers will be critical as they are the predominant drivers of the financial viability of pharmacists’ roles within the health care system. Accreditors (ie, ACPE) oversee pharmacists’ continuous professional development, and their input will be essential for operationalizing a final plan. To enhance coordination and integration of health care, other health professions must be present to provide their perspectives. Last, but certainly not least, consumers must be present to identify their health care needs, and how pharmacists can help address any unmet needs and care gaps.
Potential questions to be addressed during such a conference include:
1. What are the current, emerging, and anticipated unmet needs within the health care system?
2. How can pharmacists address these unmet needs, both directly and indirectly?
3. What additional knowledge, skills, and abilities are required for pharmacists to be able to meet these needs?
4. How can the profession maintain equilibrium between pharmacist opportunities and the capacity for large-scale workforce development?
5. What existing infrastructure can be leveraged to support large-scale workforce development?
6. What is the role of individual colleges/schools of pharmacy in these efforts?
7. What are the barriers to leveraging the pharmacist workforce to address the health care system’s unmet needs?
8. How can the identified barriers be overcome?
9. What are the short, intermediate, and long-term goals for these workforce transformation efforts?
GOAL 4: Communicate with CEO Deans Regarding the Role of Colleges/Schools in Workforce Development/Transformation
Academic pharmacy stepped in to assist the pharmacists in the workforce who wished to obtain a PharmD degree twenty years ago when the profession adopted it as the entry-level degree requirement for pharmacist licensure. Similarly, the AAC feels that AACP and its member institutions can play a vital role in workforce development again. The committee acknowledged potential concerns about the limited bandwidth that schools and colleges are facing, constantly being asked “to do more with less.” Therefore, the committee wanted to obtain the opinion of others to see how feasible such a policy recommendation would be and capitalized on the opportunity to meet directly with CEO deans at the 2020 AACP Interim Meeting.
A roundtable discussion was held with CEO deans in attendance to explore whether schools and colleges of pharmacy perceive themselves as serving an important role in the development and transformation of the current pharmacist workforce, in addition to the future workforce. An affirmative and emphatic consensus was quickly reached that academic pharmacy must be a key contributor to workforce transformation, current and future. The importance of partnerships with practitioner organizations, corporate and independent community pharmacy organizations, and health systems, was emphasized so that efforts are not redundant, as discussed in Goal 2 above. Various approaches were shared by individuals present, including mentorship in clinical skills development, advocacy, leadership, certificate training programs, access to advances in pharmacotherapy, and offering programming using various accessible approaches. Further discussion of specific measures and existing college/school exemplars would be helpful, much of which can be communicated via AACP Connect or other means. With consideration of strategic partnerships to advance common goals and interests, the CEO Deans present likewise endorsed a proposed stakeholder consensus conference, with the caveat that the presence of a rich potential consortium is essential to the success of the conference, not merely academia. As such, the committee proposes a policy statement regarding AACP’s support of schools and colleges of pharmacy in taking an active role in implementing innovative and novel approaches for workforce development.
CONCLUSION
As unique opportunities for pharmacists become increasingly available within the health care system, large-scale workforce development options are needed to help pharmacists develop their knowledge, skills and abilities, especially those who have been out in practice and need to learn new skills or enhance an existing skill set. Traditional residency and fellowship training are useful, but not sufficient for achieving large-scale workforce development. Rather, innovative and novel approaches must be implemented, with academic pharmacy leading these efforts in collaboration with others. These initiatives must be well-informed and intentionally designed in order to be worthwhile and impactful, so specific goals and outcomes should be derived from the proposed multi-stakeholder conference. Opportunities to collaborate with other organizations should be pursued, as AACP is not alone in these efforts. To garner support for these initiatives, the committee has set forth policy recommendations for how AACP and its members can actively support workforce development to help transform future pharmacy practice.
PROPOSED POLICY STATEMENTS AND RECOMMENDATIONS
Proposed Policy Statement 1
AACP supports colleges and schools of pharmacy taking an active role in implementing innovative and novel approaches for the development of the current workforce.
Proposed Policy Statement 2
AACP supports the development of novel approaches to enabling workforce development for students and pharmacists, including, but not limited to, APhA ADVANCE and the Academia-CPESN Transformation (ACT) Pharmacy Collaborative
Recommendation 1: Create a repository of workforce development activities
The 2020-2021 Academic Affairs Committee should be charged with facilitating the addition of high-quality training opportunities for practicing pharmacists into such a repository, and should continue collaborating with the American Pharmacists Association to determine how best to house these professional development opportunities within the APhA ADVANCE platform.
Recommendation 2: Collaborate with other organizations/associations providing CPD initiatives focused on large-scale pharmacist workforce development
AACP should specifically align workforce development efforts with other organizations & associations focused on large-scale pharmacist workforce development, including, but not limited to, the Community Pharmacy Enhanced Services Network (CPESN USA) and Academia-CPESN Transformation (ACT) Pharmacy Collaborative as well as APhA ADVANCE.
Recommendation 3: Convene a stakeholder conference, focusing on the needs for large-scale workforce development
AACP should lead the planning and execution of a conference with all relevant stakeholders (practitioners, patient care advocates, health care consumers, other health professionals, regulators, educators, payers, accreditors) to address the current and future needs for large-scale pharmacist workforce development.
Recommendation 4: Determine the role of schools/colleges of pharmacy in workforce development
AACP should work with CEO Deans to determine specific efforts that schools/colleges can undertake to enhance workforce development in their local communities and to identify and promote exemplars.
REFERENCES
- 1.Sorensen TD. Leading in Dickensian times: address of the president-elect at the 2019 AACP annual meeting. Am J Pharm Educ. 2019;83(6):7780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Society of Health System Pharmacists. Summary results of the Match for positions beginning in 2020 combined Phase I and II applicants. National Matching Services Inc. https://natmatch.com/ashprmp/stats/2020applstats.pdf. Accessed April 14, 2020.
- 3.American Society of Health System Pharmacists. Summary of programs and positions offered and filled: the 2016 Match - combined Phase I and Phase II. National Matching Services Inc; https://natmatch.com/ashprmp/stats/2016summpos.pdf. Accessed April 14, 2020. [Google Scholar]
- 4.American Society of Health System Pharmacists. Summary of programs and positions offered and filled: 2020 Match - combined Phase I and Phase II. National Matching Services Inc; https://natmatch.com/ashprmp/stats/2020summpos.pdf. Accessed April 14, 2020. [Google Scholar]
- 5.AACP 2017-18 Profile of Pharmacy Students. American Association of Colleges of Pharmacy. https://www.aacp.org/sites/default/files/2019-05/fall-2018-profile-of-pharmacy-students-degrees-conferred.pdf. Accessed April 14, 2020.
- 6.Janke KK, Tofade T. Making a curricular commitment to continuing professional development in doctor of pharmacy programs. Am J Pharm Educ. 2015;79(8):112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rouse MJ, Trewet CB, Janke KK. Advancing learning to advance pharmacy practice. J Am Pharm Assoc. 2018;58(2):151-155. [DOI] [PubMed] [Google Scholar]
- 8.Shoji M, Onda M, Okada H. The change in pharmacists’ attitude, confidence and job satisfaction following participation in a novel hypertension support service. Int J Pharm Pract. 2019;27(6):520-527. [DOI] [PubMed] [Google Scholar]
- 9.Papastergiou J, Kheir N, Ladova K, et al. Pharmacists’ confidence when providing pharmaceutical care on anticoagulants, a multinational survey. Int J Clin Pharm. 2017;39(6):1282-1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nielsen S, Menon N, Larney S, et al. Community pharmacist knowledge, attitudes and confidence regarding naloxone for overdose reversal. Addiction. 2016;111(12):2177-2186. [DOI] [PubMed] [Google Scholar]
- 11.AACP Consultants and Speakers Bureau. American Association of Colleges of Pharmacy. https://www.aacp.org/resource/consultants-and-speakers-bureau. Accessed April 14, 2020.
- 12.APhA ADVANCE. American Pharmacists Association. https://www.aphaadvance.com. Accessed April 14, 2020.
- 13.Community Pharmacy Enhanced Services Networks. CPESN. https://www.cpesn.com. Accessed April 14, 2020.
- 14.Academia-CPESN Transformation Pharmacy Collaborative. https://www.actforpharmacy.com. Accessed April 14, 2020.
- 15.APhA Career Pathway Evaluation Program for Pharmacy Professionals. American Pharmacists Association. http://www.pharmacist.com/apha-career-pathway-evaluation-program-pharmacy-professionals. Accessed April 14, 2020.
- 16.Get The Medications Right (GTMR) Institute. https://gtmr.org. Accessed April 14, 2020.
- 17.Directions for clinical pharmacy. Am J Hosp Pharm. 1985;42(6):1287-1292. [PubMed] [Google Scholar]
- 18.Zellmer WA, Vlasses PH, Beardsley RS. Summary of the ACPE consensus conference on advancing quality in pharmacy education. Am J Pharm Educ. 2013;77(3):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Enhancing well-being and resilience among the pharmacist workforce: a national consensus conference. American Pharmacists Association. https://www.pharmacist.com/sites/default/files/audience/APhA_Well_Being_Resilience_Report_%200719.pdf. Accessed April 14, 2020.
- 20.Avalere Health. Exploring pharmacists’ role in a changing healthcare environment. https://avalere.com/insights/exploring-pharmacists-role-in-a-changing-healthcare-environment. Published May 21, 2014. Accessed April 14, 2020.
- 21.ASHP Council on Education and Workforce Development. ASHP long-range vision for the pharmacy workforce in hospitals and health systems. Am J Health-Syst Pharm. 2020;77:386-400 [DOI] [PubMed] [Google Scholar]
- 22.Dolovich L, Austin Z, Waite N, et al. Pharmacy in the 21st century: enhancing the impact of the profession of pharmacy on people’s lives in the context of health care trends, evidence and policies. Can Pharm J. 2019;152(1):45-53. [DOI] [PMC free article] [PubMed] [Google Scholar]


