Abstract
Objective:
To remedy the notable gap in evidence-based treatments for sexual minority women, this study tested the efficacy of a minority-stress-focused cognitive–behavioral treatment intended to improve this population’s mental and behavioral health.
Method:
The intervention, EQuIP (Empowering Queer Identities in Psychotherapy), was adapted from a transdiagnostic cognitive–behavioral treatment as also recently adapted for sexual minority men. Sexual minority women at risk of mental and behavioral health problems (n = 19) and expert providers with this population (n = 12) shaped the treatment’s development, including by supporting its primary focus on universal and minority-stress-focused processes underlying this population’s disproportionately poor mental and behavioral health. The resulting treatment was then delivered to young adult sexual minority women (n = 60; M age = 25.58; 41.67% racial/ethnic minority; 43.33% transgender/nonbinary) experiencing depression/anxiety and past 90-day heavy alcohol use.
Results:
Compared to waitlist (n = 30), participants randomized to immediately receive EQuIP (n = 30) experienced significantly reduced depression and anxiety (d = 0.85, 0.86, respectively); effects for alcohol use problems were smaller (d = 0.29) and marginally significant. In preto post-intervention pooled analyses, effect sizes for minority stress processes (mean d = .25) and universal risk factors (mean d = .48), through which the treatment was expected to work, were small and moderate, respectively, and in the expected direction.
Conclusions:
This study provides initial support for a minority-stress-focused transdiagnostic cognitive–behavioral treatment for sexual minority women. These first results can launch exploration of other mechanisms and modalities through which to equip this population with evidence-based support.
Keywords: sexual minority, lesbian, gay, bisexual, transgender, evidence-based treatment, LGBT-affirmative treatment, empirically supported treatment
Sexual minority women (i.e., who identify as lesbian, bisexual, pansexual, or queer; engage in same-sex sexual behavior; or report a persistent pattern of same-sex sexual attraction) are significantly more likely to experience a number of mental health and substance use problems, including depression, anxiety, and alcohol use disorders, compared with heterosexual women (Cochran & Mays, 2009; Gilman et al., 2001; King et al., 2008). Accumulating research suggests that these mental and behavioral health disparities are rooted in sexual minority women’s disproportionate exposure to minority stress, which can manifest in stigmatizing social structures, such as discriminatory laws, policies, and community attitudes (Hatzenbuehler, 2014) as well as interpersonal rejection and discrimination (Meyer, 2003). Across multiple studies using diverse methodologies, experiences of sexual-orientation-based discrimination and victimization have been consistently linked to depression, anxiety, and alcohol use problems among sexual minority women (Coulter, Kinsky, Herrick, Stall, & Bauermeister, 2015; Lehavot & Simoni, 2011; Wilson, Gilmore, Rhew, Hodge, & Kaysen, 2016).
Research further points to several psychosocial stress processes as mechanisms through which minority stress operates to compromise mental and behavioral health. Some of these processes are specific to the experience of having a sexual minority identity, such as internalized stigma (Szymanski & Chung, 2003), sexual-orientation-based rejection sensitivity (Dyar, Feinstein, Eaton, & London, 2016), and sexual orientation concealment (Pachankis & Bränström, 2018). Other processes represent universal risk factors for psychopathology. For example, sexual minorities report higher levels of rumination, emotion dysregulation, and social isolation relative to heterosexual individuals (Hatzenbuehler, 2009), which in part accounts for the elevated rates of mental health problems observed among sexual minorities (e.g., Hatzenbuehler, McLaughlin, & Nolen-Hoeksema, 2008; Timmins, Rimes, & Rahman, 2020).
Despite consistent evidence highlighting the role of minority stress as a determinant of depression, anxiety, and alcohol use problems among sexual minority women, no existing intervention, to our knowledge, has sought to address these interrelated mental and behavioral health concerns by targeting the psychosocial mechanisms through which minority stress operates in this population (Chaudoir, Wang, & Pachankis, 2017). This limitation is noteworthy for two reasons. First, sexual minority women remain significantly underrepresented in the study of sexual-orientationbased health disparities (Coulter, Kenst, Bowen, & Scout, 2014), even though they face significant health concerns, minority stressors, and potentially additional stressors related to their minority gender as compared to sexual minority men. Indeed, the sexual orientation disparity in alcohol use problems is greater among women than men (Hughes, Wilsnack, & Kantor, 2016). Second, according to a syndemics framework, rather than addressing one health problem at a time, health promotion interventions are most efficient and cost-effective when they target shared mechanisms underlying the co-occurrence of multiple health concerns within a population (Coulter et al., 2015; Pachankis, 2015). In light of these considerations, the present study tested the efficacy of the first psychosocial intervention designed to improve the mental and behavioral health of sexual minority women by addressing the cognitive, affective, and behavioral mechanisms underlying the adverse impact of minority stress on the health of this population.
Existing research on health promotion interventions for sexual minority men suggests that cognitive–behavioral therapy (CBT) may be particularly well-suited to addressing the co-occurring mental and behavioral health difficulties arising from minority stress. As noted by Pachankis and colleagues (Pachankis, 2014; Pachankis, Hatzenbuehler, Rendina, Safren, & Parsons, 2015; see also Balsam, Martell, & Safren, 2006), CBT empowers clients to cope with adverse environmental circumstances, such as minority stress, by encouraging the development of adaptive cognitive, affective, and behavioral responses, with the goal of promoting coping self-efficacy, personal agency, and resilience. One recently developed CBT-based intervention known as ESTEEM (Effective Skills to Empower Effective Men) has demonstrated preliminary efficacy in reducing depressive symptoms, alcohol use problems, and co-occurring HIV-risk behaviors (e.g., condomless sex with casual partners) among young gay and bisexual men (Pachankis et al., 2015). Adapted from the Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders (Barlow et al., 2011), ESTEEM is transdiagnostic in that it targets psychosocial mechanisms, including those specific to minority stress (i.e., internalized stigma, rejection sensitivity, concealment) and those that represent general risk factors for psychopathology (i.e., rumination, emotion regulation difficulties, social isolation), shared across gay and bisexual men’s syndemic health conditions. As such, ESTEEM serves as an ideal platform upon which to base a transdiagnostic intervention adapted for sexual minority women to address the co-occurring mental and behavioral health challenges facing this population.
In the present study, we adapted ESTEEM to address the minority stress mechanisms and co-occurring mental/behavioral health concerns affecting sexual minority women. To address sexual minority women’s unique needs and experiences, we created this adapted intervention, called EQuIP (Empowering Queer Identities in Psychotherapy), in consultation with mental health providers possessing expertise in sexual minority women’s mental health and with at-risk sexual minority women themselves. We then tested the efficacy of EQuIP for reducing co-occurring depression, anxiety, and alcohol use problems among sexual minority women. To better understand how the intervention operates, we also examined the intervention’s ability to reduce the cognitive, affective, and behavioral mechanisms underlying the adverse impact of minority stress on health, including both minority-stress-specific processes (i.e., internalized stigma, rejection sensitivity, and concealment) and universal risk factors for psychopathology (i.e., rumination, emotion regulation difficulties, social isolation).
Considering the early stages of mental health intervention adaptations for sexual minorities, and consistent with the approach taken by Pachankis and colleagues (2015), we employed a randomized waitlist-controlled trial to assess the adapted intervention’s initial promise for future testing against other forms of mental health treatment. Also consistent with Pachankis and colleagues (2015), we focused our treatment on young adult sexual minority women, given that young adulthood represents a developmental period in which behavioral patterns are formed and identity-related stress is particularly likely to impair health (Arnett, 2000; Rice, Vasilenko, Fish, & Lanza, 2019). Thus, a mental health intervention targeting young adult sexual minority women may be particularly effective in shaping lifelong healthy trajectories and preventing the onset and persistence of psychiatric and substance use disorders.
Method
Participants
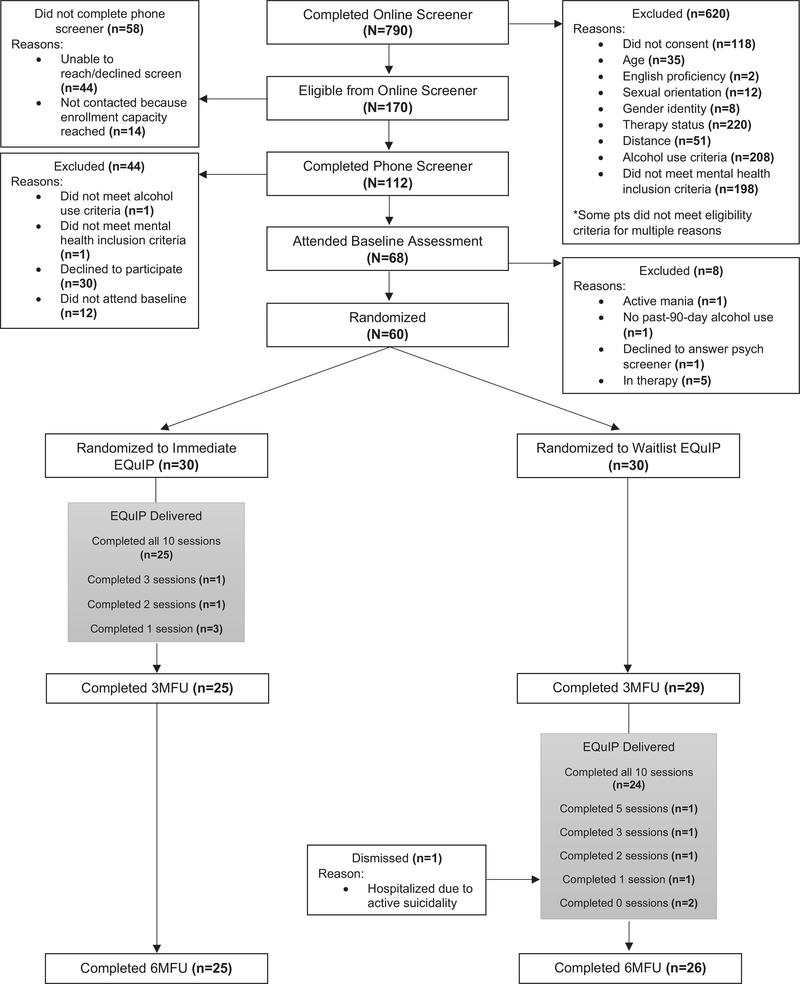
Figure 1 provides an overview of the study structure and describes the number of participants who completed each part of the study, as well as those who were ineligible, withdrew, or declined to participate. From July 2018 through January 2019, we recruited participants through advertisements on social media (e.g., Facebook), college counseling centers, community organizations, businesses, and listservs serving lesbian, gay, bisexual, transsexual, and queer (LGBTQ) communities. We also recruited in-person at LGBTQ events and venues (e.g., Pride events, bars). Participants met the following eligibility criteria: (a) aged 18–35; (b) self-identification as a woman with the option of selecting multiple gender identities; (c) sexual minority status operationalized as identity (e.g., lesbian, bisexual, pansexual, queer), given the minority-stress focus of the intervention and the fact that minority identity, rather than behavior or attraction, is the psychological lens through which minority stress is appraised (Meyer, 2003); (d) symptoms of depression or anxiety within the past 3 months, operationalized as ≥2.5 on either the depression or anxiety scale of the four-item version of the Brief Symptom Inventory given that this cutoff maximizes sensitivity relative to specificity (BSI; Lang, Norman, Means-Christensen, & Stein, 2009); (e) at least one instance of past-3-month heavy episodic drinking (i.e., ≥4 drinks in one sitting; US Department of Health & Human Services, 2015); (f) self-reported 6-month NYC residential stability and availability required to complete the study intervention and assessments; and (g) English fluency.
Figure 1.
Study structure and participant flow through study procedures.
Sixty sexual minority women who also frequently identified as other diverse genders (i.e., gender-diverse sexual minority women) enrolled in the study. Table 1 describes sample characteristics. The mean age was 25.58 (SD = 3.26). More than half (58.3%) were white; 41.7% of participants identified as racial or ethnic minorities. Slightly more than half were cisgender (56.7%), with strong representation of gender diverse participants who selected gender identities including gender queer, nonbinary, and gender fluid. Notably, the majority of participants (55.0%) identified as queer and all participants reported having completed at least some college. Slightly more than half of participants earned less than $30,000 per year (53.3%) and were in a relationship (51.7%).
Table 1.
Sample Demographic Characteristics
| Immediate intervention | Waitlist control | ||||
|---|---|---|---|---|---|
| (n = 30) | (n = 30) | ||||
| Variable | n | % | n | % | Condition comparison |
| Age, years | t = —0.75, ns | ||||
| M | 25.27 | 25.90 | |||
| SD | 3.35 | 3.20 | |||
| Gender identity | X2 = 4.34, p = 0.04 | ||||
| Cisgender woman | 13 | 43.3 | 21 | 70.0 | |
| Gender diverse (transgender, gender queer, nonbinary, gender fluid) | 17 | 56.7 | 9 | 30.0 | |
| Race | X2 = .07, ns | ||||
| White | 18 | 60.0 | 17 | 56.7 | |
| Black/African American | 4 | 13.33 | 3 | 10.00 | |
| Asian | 2 | 6.67 | 2 | 6.67 | |
| Multiracial | 0 | 0.00 | 4 | 13.33 | |
| Hispanic/Latinx | 3 | 10.00 | 2 | 6.67 | |
| Other | 3 | 10.00 | 2 | 6.67 | |
| Sexual orientation | X2 = 1.58, ns | ||||
| Lesbian | 6 | 20.0 | 3 | 10.0 | |
| Queer | 15 | 50.0 | 18 | 60.0 | |
| Other (asexual, bisexual, pansexual, uncertain) | 9 | 30.0 | 9 | 30.0 | |
| Education levela | X2 = 3.23, ns | ||||
| Some college/currently in college | 5 | 18.5 | 8 | 27.6 | |
| 4-year college degree | 17 | 63.0 | 17 | 58.6 | |
| Some graduate school or higher | 5 | 18.5 | 4 | 13.8 | |
| Employment status | X2 = 1.42, ns | ||||
| Full-time (40+ hours per week) | 18 | 60.0 | 15 | 50.0 | |
| Part-time employment (<40 hours per week) | 8 | 26.7 | 8 | 26.7 | |
| Student | 3 | 10.0 | 4 | 13.3 | |
| Unemployed | 1 | 3.3 | 3 | 10.0 | |
| Personal income, annually | X2 = 7.71, p = .02 | ||||
| Less than $29,999 | 15 | 50.0 | 17 | 53.1 | |
| $30,000–49,999 | 10 | 33.3 | 2 | 6.8 | |
| More than $50,000 | 5 | 16.7 | 11 | 36.7 | |
| Relationship status | X2 = .60, ns | ||||
| Single or casually dating | 16 | 53.3 | 13 | 43.3 | |
| Partnered | 14 | 46.7 | 17 | 56.7 | |
Immediate intervention (n = 27); waitlist control (n = 29).
Procedure
Screening.
Potential participants were asked to complete a brief online eligibility screener. Individuals who were preliminarily eligible were then contacted via a phone call during which a research assistant obtained consent for phone screening, confirmed preliminary eligibility, and provided an overview of the study. The online and phone screeners assessed the above-listed inclusion criteria. The screeners also assessed the following exclusion criteria: (a) currently in mental health treatment exceeding one day per month and (b) having received any cognitive–behavioral therapy treatment in the past 12 months. During the phone screener, a trained research assistant also screened participants for the following exclusion criteria: (a) active psychosis, mania, suicidality or homicidality using selected questions adapted from the Structured Clinical Interview for DSM–IV—Psychiatric Screen (First, Spitzer, Williams, & Gibbon, 1997); and (b) evidence of gross cognitive impairment using the Mini-Mental Status Examination (Folstein, Folstein, & McHugh, 1975).
If individuals were deemed preliminarily eligible and reported interest in participating in the study, they were scheduled for an in-office assessment appointment and e-mailed a link containing the full study consent form.
Experimental design.
Participants who completed the in-office assessment appointment and were confirmed to be eligible were then randomized via the randomizer feature of Qualtrics, which was programmed to evenly assign participants to receive treatment either immediately or after three months. Randomization was stratified so that equal numbers of white and racial/ethnic minority participants were assigned to each condition, and equal numbers of participants who met criteria for depression only, anxiety only, or both depression and anxiety were assigned to each condition. The Qualtrics randomizer was programmed to present each treatment condition evenly across levels of the two stratifying factors.
Participants randomized to receive immediate treatment were assigned a therapist and scheduled for their first session as soon as possible based on availability. Participants randomized to receive waitlist treatment received one e-mail per month to remind them of their 3-month follow-up assessment and were then assigned a therapist and scheduled for their first session at the end of the in-office 3-month follow-up assessment. The treatment and waitlist windows each lasted three months. Participants randomized to the immediate condition received treatment between their baseline and 3-month assessments. Participants randomized to the waitlist condition received treatment between their 3-month and 6-month assessments.
To assess intervention efficacy, participants were assessed at three time-points: baseline, 3-months postbaseline, and 6-months postbaseline. For each assessment, to guard against fatigue and ensure that sensitive measures were completed on site, participants completed approximately half of the survey measures at home and the other half of the survey measures, as well as a series of behavioral tasks, in-office.
This study was approved by the Human Subjects Committee of Yale University (Protocol 2000020997: “Project EQuIP: Empowering Queer Identities in Psychotherapy”). The primary outcomes of this study were preregistered on clinicaltrials.gov (NCT03721276). This article reports the results of those outcomes as well as several secondary outcomes, including minority stress processes and universal risk processes, that were not preregistered.
Intervention.
EQuIP (Empowering Queer Identities in Psychotherapy) is a 10-session intervention adapted for sexual minority women from the ESTEEM protocol, described in detail elsewhere (Pachankis, 2014). In 2017, sexual minority women (n = 19) who reported recent depression (i.e., ≥2.5 on the two-item BSI screen; Lang et al., 2009), suicidality (i.e., ≥1 on the Suicidal Ideation Attributes Scale; van Spijker et al., 2014), and unhealthy alcohol use (≥4 drinks in one sitting in the past 3 months; U.S. Department of Health & Human Services, 2019) completed a semistructured interview regarding their experiences of minority stress, mental and behavioral health, and mental health treatment experiences. Clinical experts (n = 12) also completed a semistructured interview assessing their experiences addressing minority stress when treating sexual minority women. These experts were identified through a systematic search of publication databases, professional membership rosters, and professional leadership rosters. Those experts with the highest number of relevant publications and who were identified to have direct clinical experience with sexual minority women were contacted for an interview.
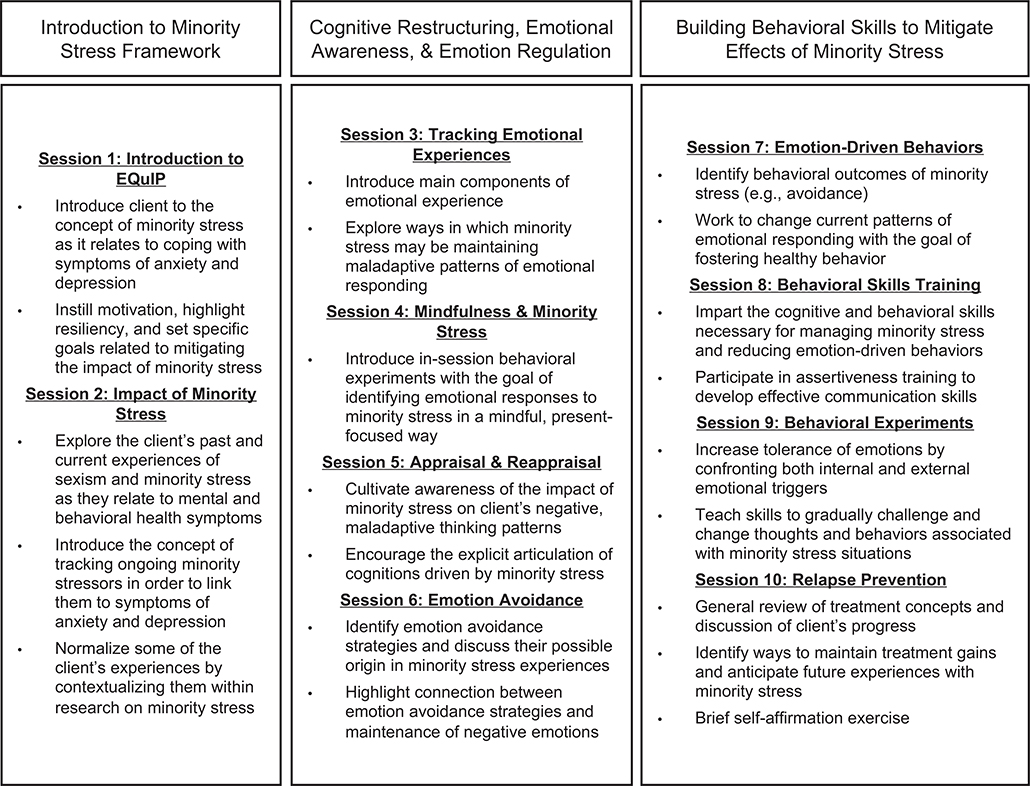
To gather feedback and suggested adaptations to the existing intervention, as part of the interview we asked interviewees—both sexual minority women and expert clinicians—to review a summary of the existing minority stress-focused intervention and its existing modules (originally created for sexual minority men) to generate suggested adaptations for sexual minority women. All interviews were transcribed and data were analyzed using a modified grounded theory approach (Beech, 2000; Corbin & Strauss, 2015) using Dedoose (Version 8.0.31). Specifically, all interviews were open-coded by a trained qualitative researcher. Then, through collaborative and iterative discussions among three psychologists and four graduate student research assistants, a codebook was compiled of relevant themes that emerged from these interviews. These themes confirmed the general relevance of minority stress pathways to sexual minority women’s mental and behavioral health and thus the validity of a transdiagnostic treatment approach for this population. Therefore, the general focus of each module remained the same as the ESTEEM intervention, meaning that it followed the Unified Protocol (Barlow et al., 2011) as adapted to address the transdiagnostic cognitive, behavioral, and emotional pathways through which sexual minority stress have been shown to undermine sexual minorities’ mental and behavioral health (see Figure 2).
Figure 2.
Overview of EQuIP (Empowering Queer Identities in Psychotherapy) treatment modules.
The qualitative results from clinical experts and sexual minority women were then used to inform revisions to the vignettes, worksheets, and behavioral experiments so that they reflected sexual minority women’s unique minority stress antecedents and situational and interpersonal contexts. Notable themes that were used to inform the adaptation of the manual included the intersection of sexism with other forms of oppression (e.g., racism, heterosexism, cis-normativity), the pervasiveness of exposure to sexual assault and harassment, and the impact of gender and social norms on relationships, communities, and identities. In addition, whereas the ESTEEM protocol was developed to address HIV-risk behaviors, we removed this focus from the EQuIP manual given the relatively lower prevalence of HIV among sexual minority women. Instead, the modules addressed sexual health more generally (e.g., how to negotiate sexual safety and healthy boundaries in relationships), consistent with themes that emerged from the qualitative interviews. Also, given the emergent themes of sexual minority women’s unhealthy alcohol use, we added clinical vignettes that specifically addressed strategies to reduce unhealthy alcohol use, such as asserting oneself against positive alcohol use norms commonly perceived in sexual minority women’s communities and establishing relationships with other sexual minority women outside of the context of alcohol. Finally, given pervasive exposure to gender-based assault, harassment, and violence among sexual minority women interviewees, ultimate therapy participants were given the option to identify therapist gender identities that would not impede therapeutic progress so that participants could, in effect, choose the gender identity of their therapist.
Study therapists, supervision, and intervention fidelity.
The intervention was delivered by a counseling psychologist and four advanced clinical psychology doctoral students, diverse in race/ethnicity, gender identity, and sexual orientation. Two additional clinical psychologists supervised intervention delivery through weekly group and individual supervisory meetings. All therapy sessions were video recorded for supervision; clinical supervisors reviewed 63 (12.35%) sessions for fidelity to the EQuIP protocol using fidelity checklists created for this study. Checklists were session-specific and contained four to seven questions asking the supervisor to rate fidelity on a 3-point scale from 0 (not covered at all) to 2 (covered thoroughly). For example, Session 2 items included “Explore the ways early and ongoing minority stress may contribute to client’s anxiety/depression/health-risk behaviors” and “Provide feedback on self-reported experiences of past and current minority stress.” Therapists were highly adherent to the protocol, with 89.2% of fidelity items rated as “covered thoroughly.” Nonadherence was discussed during clinical supervision, including during review of recorded sessions, with the goal of improving future adherence.
Retention.
Figure 1 shows participant retention across the study. Fifty-eight of 60 randomized participants completed at least one EQuIP session. Of these 58 participants, 49 (84.48%) completed all 10 sessions of EQuIP, 50 (86.21%) completed five or more, and four (6.90%) completed only one session. Fifty-four (90.00%) of 60 participants completed the 3-month postbaseline assessment and 52 (86.67%) completed the 6-month postbaseline assessment; however, two of these participants only completed the at-home portion of the 3-month postbaseline assessment and one only completed the at-home portion of the 6-month postbaseline assessment.
Outcome Measures
All scales were administered at baseline and 3- and 6-months postbaseline.
Center for Epidemiological Studies—Depression Scale.
The Center for Epidemiological Studies - Depression Scale (CES-D; Radloff, 1977) contains 20 items that ask individuals to rate how often they have experienced past-week depression symptoms (e.g., “I was bothered by things that usually don’t bother me”). Responses are on a 4-point scale ranging from 0 (rarely or none of the time [less than 1 day]) to 3 (most or all of the time [5–7 days]). A summed clinical cutoff score of 16 or higher identifies individuals who are at risk for major depression (Lewinsohn, Seeley, Roberts, & Allen, 1997). Cronbach’s alphas were 0.89, 0.89, and 0.92 at baseline, 3-month, and 6-month follow-up, respectively.
Brief Symptom Inventory.
We used mean scores on the depression and anxiety subscales of the Brief Symptom Inventory (BSI; Derogatis & Melisaratos, 1983; Meijer, de Vries, & van Bruggen, 2011), which assess how much individuals have been distressed by symptoms of depression and anxiety (e.g., “feeling lonely,” “nervousness or shakiness inside”) on a 5-point scale ranging from 0 (not at all) to 4 (extremely). Cronbach’s alphas were 0.90, 0.93, and 0.93 at baseline, 3-month, and 6-month follow-up, respectively.
Overall Depression Severity and Impairment Scale.
The Overall Depression Severity and Impairment Scale (ODSIS; Bentley, Gallagher, Carl, & Barlow, 2014) is a five-item scale that asks individuals to rate the severity and impairment associated with past-week symptoms of depression on a 5-point scale (e.g., “In the past week, when you have felt depressed, how intense or severe was your depression?” responses: 0 [little or none: Depression was absent or barely noticeable.] to 4 [extreme: Depression was overwhelming.]). A validation study of the ODSIS found that a summed cutoff score of 8 correctly classified 82% of outpatients (Bentley et al., 2014). Cronbach’s alphas were 0.91, 0.92, and 0.93 at baseline, 3-month, and 6-month follow-up, respectively.
Overall Anxiety Severity and Impairment Scale.
The Overall Anxiety Severity and Impairment Scale (OASIS; Norman, Cissell, Means-Christensen, & Stein, 2006) is a five-item scale that asks individuals to rate the severity and impairment associated with past-week symptoms of anxiety on a 5-point scale (e.g., “In the past week, when you have felt anxious, how intense or severe was your anxiety?” responses: 0 [little or none: Anxiety was absent or barely noticeable.] to 4 [extreme: Anxiety was overwhelming. It was impossible to relax at all. Physical symptoms were unbearable.]). A validation study of the OASIS found that a summed cutoff score of eight correctly classified 87% of outpatients (Campbell-Sills et al., 2009). Cronbach’s alphas were 0.76, 0.80, and 0.87 at baseline, 3-month, and 6-month follow-up, respectively.
Suicidal Ideation Attributes Scale.
The Suicidal Ideation Attributes Scale (SIDAS; van Spijker et al., 2014) is a five-item scale that assesses past-month frequency and controllability of suicidal thoughts, how close one has come to making an attempt, and distress and impairment associated with thoughts of suicide (e.g., “In the past month, how often have you had thoughts about suicide?”). Responses range from 0 (never or not at all) to 10 (always or extremely). A summed score of 21 or higher serves a cutoff indicating a high risk of suicide behavior. Cronbach’s alphas were 0.85, 0.88, and 0.82 at baseline, 3-month, and 6-month follow-up, respectively.
Short Inventory of Problems—Alcohol.
The Short Inventory of Problems—Alcohol (SIP-A; Alterman, Cacciola, Ivey, Habing, & Lynch, 2009; Blanchard, Morgenstern, Morgan, Lobouvie, & Bux, 2003) is a 15-item scale in which the sum of “yes” responses indicates participants’ past-3-month consequences of alcohol use (e.g., “I have failed to do what is expected of me because of my drinking,”). Internal consistency as measured by the Kuder-Richardson Formula 20 (KR-20) was 0.78, 0.81, and 0.77 at baseline, 3-month, and 6-month follow-up, respectively.
Measures of Minority Stress Processes
Sexual Minority Women’s Rejection Sensitivity Scale.
The Sexual Minority Women Rejection Sensitivity Scale (Dyar et al., 2016) asks participants to rate 16 vignettes in terms of how concerned or anxious each would make them about being rejected because of their sexual orientation, and their likelihood of attributing the rejection to their sexual orientation. For example, one item states, “You are on a date with a woman at a restaurant. Your waiter provides you and your date with poor service.” Responses to the anxiety and likelihood stems range from 1 (very unconcerned/very unlikely) to 7 (very concerned/very likely). Total score is the sum of the products of anxiety and likelihood scores for all items. We adapted the scale to indicate “woman, gender nonconforming, or non-binary partner” and “heterosexual, cisgender” as relevant. Cronbach’s alphas were 0.88, 0.87, and 0.91 at baseline, 3-month, and 6-month follow-up, respectively.
Sexual Orientation Concealment.
In the Sexual Orientation Concealment Scale (Meyer, Rossano, Ellis, & Bradford, 2002), participants rate the degree to which they have disclosed their sexual orientation on a scale from 1 (out to none) to 4 (out to all). The total score is the mean of responses in the following domains: “family,” “LGBTQ friends,” “straight, cisgender friends,” “coworkers”, and “health care providers.” Cronbach’s alphas were 0.75, 0.77, and 0.79 at baseline, 3-month, and 6-month follow-up, respectively.
Lesbian, Gay, and Bisexual Identity Scale—Internalized Homonegativity Subscale.
Internalized stigma was assessed using the mean score on a three-item scale, the Lesbian, Gay, and Bisexual Identity Scale—Internalized Homonegativity Subscale (Mohr & Kendra, 2011), that asks individuals to rate thoughts and feelings related to their LGBTQ identity (e.g., “If it were possible, I would choose to be straight”). Responses range from 1 (disagree strongly) to 6 (agree strongly). Cronbach’s alphas were 0.81, 0.78, and 0.78 at baseline, 3-month, and 6-month follow-up, respectively.
Sexual Orientation Implicit Association Test.
As an additional way of assessing internalized stigma, the Sexual Orientation Implicit Association Test (IAT; Hatzenbuehler, Dovidio, Nolen-Hoeksema, & Phills, 2009), a computer-based task, uses standard IAT procedures (Lane, Banaji, Nosek, & Greenwald, 2007) in which individuals categorize, as either sexual minority or heterosexual and pleasant or unpleasant, four images representing same-sex couples, four representing heterosexual couples, eight positive words, and eight negative words by pressing one of two keys. Two critical response blocks are used to assess implicit associations toward heterosexual people versus sexual minority people. The first of these blocks requires individuals to use the same key to categorize positive words and sexual minority people, and another key to categorize negative words and heterosexual people. The second of these blocks requires an inverse pattern of responding, whereby individuals must use one key to categorize positive words and heterosexual people and another key to categorize bad words and sexual minorities. Individuals who correctly categorize words faster during the first block compared to the second block are considered to have implicit positive associations for sexual minority people compared to heterosexual people, and individuals who correctly categorize words faster during the second block compared to the first block are considered to have implicit positive associations for heterosexual people compared to sexual minority people. The order of these blocks was counterbalanced across participants to account for order effects. The IAT for the current study was scored using the IATgen utility in Qualtrics (Carpenter et al., 2018), which uses Greenwald, Nosek, and Banaji’s (2003) scoring procedures. Higher values indicate more implicit positive associations for heterosexuals relative to sexual minorities (i.e., higher internalized stigma). The sexual orientation IAT has demonstrated strong validity, including prediction of relevant behavioral and attitudinal outcomes (Banse, Seise, & Zerbes, 2001; Jellison, McConnell, & Gabriel, 2004), moderation of treatment outcomes (Millar, Wang, & Pachankis, 2016), and relatively weaker susceptibility to social desirability compared to self-report measures of internalized stigma (Banse et al., 2001). Split-half reliability coefficients (Spearman-Brown correction) were 0.83, 0.68, and 0.87 at baseline, 3-month, and 6-month follow-up, respectively.
Measures of Universal Risk Processes
Difficulties in Emotion Regulation Scale—Short Form.
In the Difficulties in Emotion Regulation Scale—Short Form (DERSSF; Gratz & Roemer, 2004; Kaufman et al., 2016), an 18-item scale, individuals are asked how much each statement regarding emotion regulation (e.g., “When I’m upset, I acknowledge my emotions”) applies to them from 1 (almost never) to 5 (almost always); the items are summed. Cronbach’s alphas were 0.85, 0.87, and 0.85 at baseline, 3-month, and 6-month follow-up, respectively.
Multidimensional Scale of Perceived Social Support.
The mean score on the Multidimensional Scale of Perceived Social Support (MSPSS; Zimet, Powell, Farley, Werkman, & Berkoff, 1990), a 12-item scale, indicates the perceived support that individuals report receiving from family (e.g., “My family really tries to help me”), friends (e.g., “I have friends with whom I can share my joys and sorrows”), and significant others (e.g., “I have a special person who is a real source of comfort to me”) on a scale ranging from 0 (very strongly disagree) to 7 (very strongly agree). Cronbach’s alpha was 0.87 at all three assessment points.
Ruminative Responses Scale—Brooding Subscale.
The sum of the five items on the Ruminative Responses Scale—Brooding Subscale (RRS; Treynor, Gonzalez, & Nolen-Hoeksema, 2003) indicates the frequency with which participants experience brooding thoughts in response to depressed mood (e.g., “Think ‘what am I doing to deserve this?’”) along a scale ranging from 1 (almost never) to 4 (almost always). Cronbach’s alphas were 0.57, 0.65, and 0.66 at baseline, 3-month, and 6-month follow-up, respectively, which were notably low, especially when considered against the more acceptable reliability for this scale in other studies of sexual minority women (i.e., α = .85; Lewis, Mason, Winstead, Gaskins, & Irons, 2016).
Simple Rathus Assertiveness Schedule—Short Form.
The Simple Rathus Assertiveness Schedule—Short Form (SRAS-SF; Rathus, 1973; Jenerette & Dixon, 2010), a 19-item scale, asks individuals to rate the personal typicality of assertive and unassertive behavior (e.g., “I find it embarrassing to return merchandise,” “I have avoided asking questions for fear of sounding stupid”) along a scale from 1 (very uncharacteristic of me) to 6 (very characteristic of me), for a summed total score. Cronbach’s alphas were 0.85, 0.81, and 0.82 at baseline, 3-month, and 6-month follow-up, respectively.
Measure of Intervention Acceptability
At 6-month follow-up, we administered a 13-item measure created for this study that asked participants to indicate the degree to which the study helped them overall and in various domains (e.g., coping with minority stress, achieving their goals), the extent to which the study was a positive experience, and whether they would recommend the study to a friend (e.g., “Participating in this study helped me”). Participants responded to the items using a scale from 1 (not at all) to 4 (very much so). Cronbach’s alpha was 0.94.
Analytic Plan
Feasibility was assessed in terms of treatment attendance. Acceptability was assessed in terms of responses to the quantitative exit survey that all participants completed at 6-month follow-up and the qualitative exit interview conducted with 20 randomly selected participants after 6-month follow-up. Qualitative exit interviews were transcribed verbatim, and the third and eighth authors served as coders and double-coded all transcripts. Thematic analysis was used to identify patterns of responses, and emergent codes were categorized into larger themes (Braun & Clarke, 2006). We present findings related to the overarching theme of feasibility and acceptability, with salient quotes provided to further contextualize qualitative feedback.
We assessed intervention efficacy using an intent-to-treat analysis including all eligible cases (n = 60). First, to determine randomization effectiveness, differences in baseline demographic characteristics were assessed between the immediate intervention (n = 30) and waitlist control (n = 30) conditions using t tests for continuous measures and chi-square tests for categorical measures (see Table 1). Income and gender identity differed between conditions (p < .05), with the waitlist control group reporting higher income and having a larger proportion of cisgender women; thus, we included income and gender identity as covariates in subsequent analyses. Dependent variables were assessed for normality using skewness and kurtosis thresholds of ±2 (Field, 2013; George & Mallery, 2010). Suicidality and internalized stigma were found to be non-normal; we therefore log-transformed these variables for further statistical tests (reassessment of skewness and kurtosis after transformation showed normal distribution).
In a first set of analyses, we used linear mixed models with maximum likelihood estimation and a compound symmetry covariance structure (selected based on fit criteria, i.e., lowest Akaike information criterion [AIC]) to test the Condition × Time interaction for all intervention outcomes including mental and behavioral health (e.g., depression), minority stress processes (e.g., rejection sensitivity), and universal risk processes (e.g., emotion regulation). To do so, we limited the data to baseline (time = 0) and 3 months postbaseline assessment (time = 1) and examined the Condition × Time interaction effect of receiving immediate EQuIP (condition = 1) versus receiving the 3-month waitlist (condition = 0). Thus, the estimate of interest compared preintervention to immediate postintervention outcomes in the immediate intervention group to prewaitlist and immediate postwaitlist outcomes in the waitlist control group. Effect sizes (d) for linear mixed models were calculated as mean pre–post change in the immediate intervention group minus the mean pre–post change in the waitlist control group, divided by the pooled baseline standard deviation (Morris, 2008).
In a second set of analyses, we examined the clinical significance of observed changes in those mental health outcome measures that possess established clinical cutoffs (i.e., CES-D, ODSIS, OASIS). To do so, we used generalized linear mixed models with a logit link and binomial distribution to examine the Condition × Time interaction effect predicting the odds of meeting or exceeding the clinical cutoff among participants receiving immediate EQuIP (condition = 1) versus those receiving the 3-month waitlist (condition = 0). For interpretability, we report proportions of participants meeting or exceeding clinical cutoff by condition and time.
In a third set of analyses, we conducted a pooled analysis whereby data from all participants were pooled to examine change in outcome from immediate preintervention to postintervention using paired t tests (i.e., baseline to 3 months postbaseline for the immediate intervention group and 3-months postbaseline to 6-months postbaseline for the waitlist control group). Pooled analyses are useful in waitlist-controlled studies (where all participants ultimately receive treatment) to assess the pre–post effect of the intervention in a larger sample than the condition x time analyses allow. One participant assigned to the waitlist control group did not complete 3-month or 6-month assessments and was dropped from the pooled analysis (n = 59). Effect sizes (d) for pooled analyses were calculated as .
Finally, we assessed the longer-term persistence of observed intervention effects by limiting analyses to immediate 3-months postbaseline (time = 1) and 6-months postbaseline (time = 2) among participants in the immediate intervention condition (condition = 1), the only participants to have completed assessments 3-months after receiving the intervention. Specifically, we examined the significance of changes between time points for all outcomes, including mental and behavioral health (e.g., depression), minority stress processes (e.g., rejection sensitivity), and universal processes (e.g., emotion regulation). Results were evaluated at p < .05. We report means, standard errors, and 95% confidence intervals.
Results
Feasibility and Acceptability
Supporting the intervention’s feasibility, we found that 49 out of 60 participants completed all 10 sessions. Supporting the intervention’s acceptability, in an exit survey administered to all participants at the 6-month follow-up, we found that the vast majority of participants indicated that the study at least somewhat helped them (98.1%), was a positive experience (100%), helped them achieve their goals (96.2%), and helped them cope with minority stress (90.4%); 98.1% indicated that they would recommend the study to a friend. Results from exit interview data further support the study’s feasibility and acceptability, as summarized in Table 2. In general, participants considered treatment session length (i.e., one hour), frequency (i.e., once per week), and duration (i.e., 10 weeks) to be optimal. Many participants reported that the sessions fit within their schedules and weekly spacing allowed for sufficient time to learn and apply skills that aligned with their treatment goals. Some participants expressed the desire for longer-duration therapy to explore core issues, especially those related to trauma. Participants expressed that the treatment content was generally considered acceptable. For instance, most participants reported that they were able to consider developmental and contextual influences on their current mood, thought patterns, and behavioral coping strategies, which many “appreciated,” “[found] helpful,” and were “grateful for.” Some participants, particularly those with multiply marginalized identities (e.g., racial/ethnic minority sexual minority women) or histories of violence and abuse, expressed desire for more content related to their intersectional experiences (e.g., related to racism and sexism), trauma, and unhealthy drinking. Most participants reported feeling grateful for the positive and trustworthy relationship they built with their therapist. Some participants expressed a desire for therapist-participant demographic matching (e.g., across race and gender identity), but most reported that they were able to build a strong connection regardless of therapist demographic status. Finally, although most participants expressed that weekly homework helped to consolidate information learned in treatment sessions, some noted that homework felt burdensome.
Table 2.
Condition and Time Comparisons for Mental and Behavioral Health Outcomes
| Immediate intervention (n = 30) | Waitlist control (n = 30) | Pooled data | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Condition × Timeb | (n = 59) | Pre versus post | ||||||||||
| Variable | M | SE | M | SE | Est. | 95% CI | d | M | SE | Est. | 95% CI | d |
| Depression (CESD) | −8.01* | [−14.18, −1.85] | 0.85 | −5.07** | [−8.68, −1.46] | 0.80 | ||||||
| 3-month pre-intervention | — | — | 27.57 | 1.80 | ||||||||
| Immediate pre-intervention | 29.70 | 1.84 | 26.86 | 1.91 | 28.31 | 1.33 | ||||||
| Post-intervention | 20.44 | 1.80 | 24.83 | 2.44 | 22.68 | 1.54 | ||||||
| 3-month follow-up Distress (BSI) | 19.00 | 2.18 | — | — | ||||||||
| Distress (BSI) | −0.37* | [−0.71, −0.03] | 0.60 | −0.27** | [−0.46, −0.09] | 0.86 | ||||||
| 3-month pre-intervention | — | — | 1.80 | 0.10 | ||||||||
| Immediate pre-intervention | 1.74 | 0.14 | 1.85 | 0.09 | 1.80 | 0.09 | ||||||
| Post-intervention | 1.38 | 0.11 | 1.64 | 0.11 | 1.52 | 0.08 | ||||||
| 3-month follow-up | 1.16 | 0.14 | — | — | ||||||||
| Depression (ODSIS) | −3.41** | [−5.81, −0.99] | 0.84 | — 1.74** | [−2.94, −0.53] | 0.83 | ||||||
| 3-month pre-intervention | — | — | 6.17 | 0.78 | ||||||||
| Immediate pre-intervention | 6.30 | 0.83 | 7.69 | 0.73 | 6.98 | 0.56 | ||||||
| Post-intervention | 4.09 | 0.71 | 5.85 | 0.82 | 5.02 | 0.56 | ||||||
| 3-month follow-up | 3.88 | 0.69 | — | — | ||||||||
| Anxiety (OASIS) | −2.54* | [−4.72, −0.36] | 0.86 | −2.18*** | [−3.38, −0.98] | 1.06 | ||||||
| 3-month pre-intervention | — | 8.20 | 0.46 | |||||||||
| Immediate pre-intervention | 8.80 | 0.64 | 8.03 | 0.46 | 8.42 | 0.40 | ||||||
| Post-intervention | 6.00 | 0.70 | 6.08 | 0.60 | 6.04 | 0.45 | ||||||
| 3-month follow-up | 6.17 | 0.68 | — | — | ||||||||
| Suicidality (SIDAS)a | −0.29 | [−.94, .36] | 0.27 | −0.32* | [−0.63, −0.00] | 0.59 | ||||||
| 3-month pre-intervention | — | 5.03 | 1.42 | |||||||||
| Immediate pre-intervention | 4.13 | 1.51 | 5.59 | 1.58 | 4.85 | 1.09 | ||||||
| Post-intervention | 2.09 | 1.04 | 2.73 | 1.05 | 2.43 | 0.74 | ||||||
| 3-month follow-up | 1.46 | 0.75 | — | — | ||||||||
| Unhealthy alcohol use (SIP-A) | −1.14† | [−2.50, 0.21] | 0.29 | −1.04** | [−1.80, −0.28] | 0.81 | ||||||
| 3-month pre-intervention | — | — | 3.93 | 0.54 | ||||||||
| Immediate pre-intervention | 3.63 | 0.57 | 3.34 | 0.60 | 3.49 | 0.41 | ||||||
| Post-intervention | 2.16 | 0.37 | 2.80 | 0.64 | 2.48 | 0.37 | ||||||
| 3-month follow-up | 1.92 | 0.44 | — | — | ||||||||
Note. SE = standard error; Cl = confidence interval; CESD = Center for Epidemiologie Studies Depression Scale; BSI = Brief Symptom Inventory; ODSIS = Overall Depression Severity and Impairment Scale; OASIS = Overall Anxiety Severity and Impairment Scale; SIDAS = Suicidai Ideation Attributes Scale; RSES = Rosenberg Self-Esteem Scale; SIP-A = Short Inventory of Problems—Alcohol.
Estimates, 95% CIs, and d use log-transformed variable. Means and SEs use raw variable.
Models adjust for gender identity and income.
≤ .10.
p < .05.
p ≤ .01.
p ≤ .001.
Mental and Behavioral Health Outcomes
Condition comparisons.
When examining changes in outcomes from baseline and 3-months postbaseline between immediate intervention and waitlist conditions, we found significant Condition × Time interactions, suggesting relative improvements in depression, as measured with both the CES-D (d = 0.85) and the ODSIS (d = 0.84), as well as anxiety (d = 0.86), and psychological distress (d = 0.60; see Table 3). We found a marginally significant Condition × Time interaction effect for alcohol use (d = 0.29). No significant Condition × Time interaction effect was found for suicidality.
Table 3.
Condition and Time Comparisons for Minority Stress Measures and Universal Risk Processes
| Variable | Immediate intervention (n = 30) |
Waitlist control (n = 30) |
Condition × Timea |
d | Pooled data (n = 59) |
Pre versus post |
d | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SE | M | SE | Est. | 95% Cl | M | SE | Est. | 95% Cl | |||
| Minority stress measures | ||||||||||||
| Rejection sensitivity | −0.38 | [−3.42, 2.67] | 0.15 | −1.49† | [−3.12, 0.13] | 0.53 | ||||||
| 3-month preintervention | — | — | 24.98 | 1.63 | ||||||||
| Immediate preintervention | 25.19 | 1.38 | 23.03 | 1.58 | 24.13 | 1.05 | ||||||
| Postintervention | 22.10 | 1.51 | 22.12 | 1.76 | 22.11 | 1.16 | ||||||
| 3-month follow-up | 22.78 | 1.72 | — | — | ||||||||
| Sexual orientation concealment | 0.10 | [−0.09, 0.29] | −0.14 | −0.05 | [−0.15, 0.06] | 0.24 | ||||||
| 3-month preintervention | — | — | 1.89 | 0.12 | ||||||||
| Immediate preintervention | 1.87 | 0.11 | 1.67 | 0.12 | 1.77 | 0.08 | ||||||
| Postintervention | 1.74 | 0.12 | 1.77 | 0.14 | 1.75 | 0.09 | ||||||
| 3-month follow-up | 1.75 | 0.13 | — | — | ||||||||
| Internalized stigma | 0.02 | [−0.16, 0.20] | −0.16 | −0.04 | [−0.12, 0.05] | 0.24 | ||||||
| 3-month preintervention | — | — | 1.49 | 0.13 | ||||||||
| Immediate preintervention | 1.72 | 0.19 | 1.32 | 0.10 | 1.53 | 0.85 | ||||||
| Postintervention | 1.63 | 0.16 | 1.36 | 0.12 | 1.49 | 0.73 | ||||||
| 3-month follow-up | 1.49 | 0.13 | — | — | ||||||||
| IAT—Internalized stigma | −0.07 | [−0.33, 0.18] | 0.15 | 0.01 | [−0.13, 0.14] | −0.03 | ||||||
| 3-month preintervention | — | — | −0.26 | 0.07 | ||||||||
| Immediate preintervention | −0.22 | 0.09 | −0.20 | 0.07 | −0.21 | 0.06 | ||||||
| Postintervention | −0.23 | 0.08 | −0.17 | 0.07 | −0.20 | 0.05 | ||||||
| 3-month follow-up | −0.23 | 0.09 | — | — | ||||||||
| Universal risk processes | ||||||||||||
| Emotion dysregulation (DERS) | −3.32 | [−8.83, 2.18] | 0.44 | −3.76* | [−7.07, −0.44] | 0.66 | ||||||
| 3-month preintervention | — | — | 49.37 | 1.92 | ||||||||
| Immediate preintervention | 47.50 | 1.82 | 47.07 | 1.74 | 47.29 | 1.25 | ||||||
| Postintervention | 40.74 | 1.89 | — | — | 43.45 | 1.38 | ||||||
| 3-month follow-up | 40.58 | 1.64 | — | — | ||||||||
| Social support (MSPSS) | −1.35** | [−2.34, −0.35] | −1.10 | 0.27 | [−0.13, 0.67 | 0.40 | ||||||
| 3-month preintervention | — | — | 3.39 | 0.25 | ||||||||
| Immediate preintervention | 3.72 | 0.21 | 5.39 | 0.14 | 4.54 | 0.17 | ||||||
| Postintervention | 4.31 | 0.28 | 5.35 | 0.17 | 4.86 | 0.18 | ||||||
| 3-month follow-up | 5.12 | 0.24 | — | — | ||||||||
| Rumination (RRS) | −0.73 | [−2.50, 1.04] | 0.30 | −1.20* | [−2.20, −0.20]] | 0.70 | ||||||
| 3-month preintervention | — | — | 13.57 | 0.55 | ||||||||
| Immediate preintervention | 13.80 | 0.45 | 13.52 | 0.54 | 13.66 | 0.35 | ||||||
| Postintervention | 12.91 | 0.57 | 12.04 | 0.66 | 12.45 | 0.44 | ||||||
| 3-month follow-up | 11.25 | 0.48 | — | — | ||||||||
| Unassertiveness (RAS) | 1.47 | [−7.52, 10.46] | −0.03 | 0.91 | [−2.34, 4.18] | 0.16 | ||||||
| 3-month preintervention | — | — | 62.80 | 2.67 | ||||||||
| Immediate preintervention | 66.87 | 3.10 | 57.86 | 2.11 | 62.44 | 1.96 | ||||||
| Postintervention | 62.43 | 3.05 | 59.42 | 2.29 | 60.84 | 1.87 | ||||||
| 3-month follow-up | 62.46 | 3.13 | — | — | ||||||||
Note. Cl = confidence intervals; IAT = Implicit Association Test; DERS = Difficulties in Emotion Regulation Scale; MSPSS = Multi dimensionai Scale of Perceived Social Support; RRS = Ruminative Responses Scale; RAS = Rathus Assertiveness Schedule.
Estimates, 95% CI, and d use log-transformed variable. Means and SEs use raw variable.
Models adjust for gender identity and income.
≤ .10.
p ≤ .05.
p ≤.01.
p ≤ .001.
Clinical significance.
In clinical significance analyses, which examined the reduction in the proportion of participants meeting or exceeding predetermined clinical cutoffs from baseline to 3-months postbaseline assessment, we found a significant Condition × Time interaction effect on depression as measured with the ODSIS (46.7% to 24.0% for immediate intervention, 30.0% to 55.2% for waitlist, p < .01) and a marginally significant Condition × Time interaction effect on anxiety as measured with the OASIS (70.0% to 32.0% for immediate intervention, 66.7% to 58.6% for waitlist, p < .10). No significant interaction effect was found for depression as measured with the CES-D.
Pooled analyses.
In pooled analyses, which examined pre– post intervention effects across immediate intervention and waitlist conditions, we found significant improvements in all primary outcomes from immediate preintervention to immediate postintervention, including suicidality (d = 0.59) and alcohol use problems (d = 0.81; see Table 3). Effect sizes for all outcomes were large (mean d = 0.88) and in the expected direction.
Minority Stress and Universal Processes
Condition comparisons.
We found a significant Condition × Time interaction effect for perceived social support (d = −1.10), not in the expected direction, as the mean increase in perceived social support from baseline to 3-months postbaseline assessment for the waitlist condition (+2.00) was greater than the mean increase in perceived social support for the immediate intervention condition (+0.59). No other significant Condition × Time interaction effects were found for minority stress processes or for universal processes (see Table 4). Effect sizes for minority stress and universal processes not found to have significant Condition × Time effects were small (mean d = 0.15) and in the expected direction.
Table 4.
Feasibility and Acceptability Data From Exit Interview Participants (n = 20)
| Feasibility/acceptability domain | Summary | Qualitative example |
|---|---|---|
| Length of each session | Length of session was considered feasible/acceptable. Some participants expressed desire for longer sessions. | “It usually felt like enough. Sometimes it felt like not enough. But I think it was mostly depending on whenever the mood struck me. It was just a matter of like how I’m feeling during that particular session—but it never felt like too much.” “Sometimes I felt like it was cut short a little. I guess it was ’cause I—it’s just hard to, when you’re getting in-depth about your personal life, to wrap up perfectly … if that makes sense.” |
| Length of treatment | Length of treatment was considered feasible/acceptable. Some participants expressed desire for longer treatment. | “I thought it was fine. I mean it’s something when you think about therapy, you know, usually people go once a week if it’s not some kind of intensive thing. So, it felt pretty normal and it was good to just have one day out of the week where you can kind of just like express all the stuff from the frustration, and from the previous week. So, having it that frequent, felt good.” “I would obviously have loved for them to be more, just because I wound up liking my therapist so much and really feeling like—it really did feel like I was seeing change, and things were getting a lot better, so I would’ve loved for it to go on longer, but you know, it was a short-term study, so I think it made sense that it was the length that it was.” |
| Scheduling sessions | Scheduling sessions around participant and therapist schedules was considered feasible/ acceptable with some personal exceptions. | “I found [scheduling sessions] to be smooth. I don’t recall anything that stood out as burdensome or being a hassle.” “So, I have a 9-to-5 job. And so, it was kind of difficult to schedule around getting to the office and then doing that for an hour, and then coming back. And it was a bit emotionally draining.” |
| Treatment content | Treatment content was generally considered acceptable. Some participants expressed desire for more content related to intersectionality (e.g., racism, sexism), trauma, and unhealthy drinking. | “The treatment was definitely relevant. The intention was there and the first few sessions dealt a lot with getting to the root of things, just analyzing the shit out of everything, which I appreciated. I liked the deconstructing all the things that make me sad. That was good. I find that helpful and it’s—some of those elements, the uncovered, the analyzed elements are with me and I’m grateful for it.” “[Trauma] definitely came up a lot. I think it was addressed in, like, a way. And the only way it could be addressed in the format of the intervention—because you can’t address a bunch of cumulative, traumatic experiences over a very long period of time into a 10-week CBT-type thing. And so, I think—we went about it by discussing effects and avoidance patterns and stuff, things like that. And talking about the limitations of the different experiments for avoidance patterns and things like that … But the format of the intervention isn’t really a format in which you can really do any type of trauma unpacking, I guess.” |
| Therapist-participant rapport | Therapist-participant rapport was considered positive and acceptable. Several participants expressed desire for therapist-participant demographic matching (e.g., across race, gender identity, etc.). | “So I want to say that I’m really grateful for my—for the person— the professional that was working with me. It was generally a very genuine human being and I’m thankful for that. It was good.” “I think it would have also been nice to have been paired with a therapist that was not white-passing. So, I think I would have felt more comfortable talking to someone that maybe understood that intersection more so than someone that was white-passing.” |
| Homework | Feasibility/acceptability related to homework was mixed. Some participants expressed that homework was burdensome, while others expressed that it helped to consolidate information learned in treatment sessions. | “The first [homework] for me was—I think it got my buy-in immediately … just to have to critically think about how I construct a thought or an action… . Just gives me so much more agency over why—how I ended up where I am at and it—I’m somebody who I think is often accused of being reactive or when I tell stories, it’s however the things are happening to me. And in having to do that… . That definitely was helpful and then thinking just through grew from there.” “Most [homework] where I had to write down long-term goals. For a certain goal, it might feel—for certain things I wanna do for goals could be concrete, but I just felt like in terms of a goal of—maybe introducing my mom to my girlfriend—it was really hard sometimes to come up with the steps to take. There were so many variables even within that goal. I would say generally things where I had to list goals were difficult for me …” |
Pooled analyses.
In pooled analyses, we found significant pre-post reductions in emotion regulation difficulties (d = 0.66) and rumination (d = 0.70) and marginally significant reductions in rejection sensitivity (d = 0.53; see Table 4). Overall, effect sizes for minority stress processes (mean d = 0.25) were small and for universal processes (mean d = 0.48) were small-to-medium.
Follow-up assessment.
To assess the longer-term persistence of effects, we compared 3-months postbaseline to 6-months postbaseline scores for all outcomes for immediate intervention participants. As shown in Tables 3 and 4, intervention effects generally continued to decrease from 3-months to 6-months postbaseline for mental and behavioral health outcomes, minority stress processes, and universal processes. Notably, BSI scores continued to significantly decrease from postintervention to 3-month follow-up (95% CI [−0.49, −0.17]; p < .001). In addition, rumination continued to decrease across time points by an estimated 1.64 points (95% CI [−2.55, −0.72], p < .01) and perceived social support continued to significantly increase across time points by an estimated 0.70 points (95% CI [0.12, 1.28], p < .05).
Correction for Multiple Comparisons
Because our examination of multiple outcomes might have inflated Type I error, we performed a post hoc adjustment of p values using Benjamini-Hochberg procedures (Benjamini & Hochberg, 1995) for main condition comparisons for mental health outcomes and universal psychosocial processes. For mental health outcomes, all effects that were significant at p < .05 before adjustment remained significant at p < .05 postadjustment. The depression impairment (ODSIS) p value (unadjusted: p = .0066) was slightly attenuated to p = .035. For universal psychosocial processes, the social support p value (unadjusted: p = .0089) was slightly attenuated to p = .036.
Discussion
Results of this first randomized controlled trial of an intervention for sexual minority women’s co-occurring depression, anxiety, and alcohol use problems suggest initial promise and directions for future research. That the treatment significantly reduced symptoms of depression and anxiety compared to waitlist; marginally reduced alcohol use compared to waitlist; showed clinically meaningful reductions in depression; and yielded comparable effects sizes for depression and anxiety as the standard Unified Protocol (Barlow et al., 2017) suggests that this treatment, grounded in a cognitive–behavioral approach focused on minority stress, is preliminarily efficacious. That the pooled analyses also showed significant reductions in universal psychosocial risks, such as emotion dysregulation and rumination, suggests that future research should perhaps investigate whether the treatment might work through the Unified Protocol’s hypothesized transdiagnostic mechanisms (Wilamowska et al., 2010), which are consistently elevated among sexual minority women compared to heterosexuals (Hatzenbuehler et al., 2008; Timmins et al., 2020). At the same time, because the treatment was associated with only small reductions in minority stress processes and did not affect suicidality, future research is needed to elucidate the potentially unique mechanisms underlying sexual minority women’s mental and behavioral health.
Effect sizes for depression and anxiety were large and in the expected direction, suggesting that this treatment can have a powerful impact on the mental health of young adult sexual minority women. Still, the effect sizes for depression and anxiety found here (e.g., ODSIS = 0.84 and OASIS = 0.86) are somewhat similar to those found in a large waitlist comparison of the standard, non-adapted Unified Protocol (e.g., ODSIS = 0.45 and OASIS = 0.91; Barlow et al., 2017). Also, although our theoretical model (i.e., minority stress theory; Hatzenbuehler, 2009; Meyer, 2003) and adaptation research with sexual minority women supports a treatment focused on minority stress and associated universal processes, the EQuIP intervention yielded only small effects on these processes. Further, although we recruited participants with recent heavy drinking, the EQuIP intervention yielded only small effects on alcohol use.
Together, the present findings suggest the importance of considering additional treatment targets specific to sexual minority women that could enhance standard cognitive–behavioral interventions for this population (Pachankis, 2018). One important treatment consideration not systematically addressed by the current treatment is sexual minority women’s disproportionate exposure to violence and abuse (Roberts, Austin, Corliss, Vandermorris, & Koenen, 2010). Violence and abuse are known correlates of sexual minority women’s mental and behavioral health problems, including alcohol use (e.g., Dworkin et al., 2018; Gilmore et al., 2014; Kaysen, Lehavot, & Dworkin, 2019), and might lend themselves to a different mechanistic conceptualization of current symptomatology. Normative peer influences represent another important determinant of alcohol use problems among sexual minority young women (Drabble, Midanik, & Trocki, 2005; Hatzenbuehler, Corbin, & Fromme, 2008; Litt, Lewis, Rhew, Hodge, & Kaysen, 2015). Sexual minority individuals are also known to experience stress from within sexual minority communities, potentially related to exacerbated gender-related stress in those communities but not necessarily related to stigma-based minority stress (Pachankis, Clark, et al., 2020), yet such stressors were not systematically addressed in this treatment focused specifically on minority stress.
Intersecting forms of identity-based stress, including gender-, sexual-minority-, and other minority-based (e.g., racial/ethnic) stress (Lehavot, Balsam, & Ibrahim-Wells, 2009; Meyer & Ouellette, 2009) represent another important future treatment consideration. Although EQuIP’s framework focused on identity-based stressors as antecedents to current mental and behavioral health challenges and was driven by an individualized case conceptualization, it did not systematically address intersectional stressors. Future research ought to consider that sexual minority women’s mental and behavioral health might be maintained by factors other than or in addition to sexual minority stress and seek to identify mechanisms capable of yielding robust impact on sexual minority women’s alcohol use problems (Drabble & Eliason, 2012). Given that nearly half of the participants were gender diverse (e.g., transgender, genderqueer, nonbinary), future intervention research with sexual minority women ought to consider means for systematically addressing the intersection of sexual and gender identity.
The lack of strong minority stress effects and associated universal processes also raises the question of whether existing cognitive–behavioral interventions need to be tailored for sexual minority women. The evidence is currently mixed regarding whether sexual minorities experience less benefit from existing treatments compared to heterosexuals (e.g., Beard et al., 2017; Rimes, Ion, Wingrove, & Carter, 2019) and sexual minorities in the United States do not seem to experience disproportionate lack of access to mental health treatment (Cochran, Björkenstam, & Mays, 2017; Grella, Greenwell, Mays, & Cochran, 2009). Further, all cognitive–behavioral treatments rely on an individualized case conceptualization, meaning that any sensitively trained clinician would consider the potential relevance of minority stress to their sexual minority clients’ presenting concerns (American Psychological Association, 2011). Although it is essential for mental health providers to deliver LGBTQ-affirmative care, whether that care requires an explicit focus on minority stress as an etiological source of sexual minority women’s mental and behavioral health remains unknown. Also, because the present study was conducted in a highly progressive urban center with numerous LGBTQ-supportive resources, it is impossible to know whether a minority-stress-focused treatment might be more relevant to sexual minority women who seek treatment in higher structural stigma environments. In fact, meta-analytic data show that structural stigma is associated with lower benefit from behavioral interventions for minority populations and might determine whether those interventions need to be tailored to address the impact of structural stigma on well-being (Reid, Dovidio, Ballester, & Johnson, 2014).
Results must be interpreted in light of several methodological features of the present study. We utilized a waitlist-controlled trial to test the efficacy of this first minority-stress-focused mental and behavioral health treatment for sexual minority women. Although use of a waitlist can control for time effects, expectancies, and repeated assessments, this design also introduces several limitations. For instance, waitlists involve the ethical decision of whether to refer waitlisted participants to outside care. We provided all participants with a list of outside mental health referrals and found that 24.13% of the waitlist participants reported utilizing such referrals during the waitlist period. We also unexpectedly found that participants in this control condition reported greater increases in social support than participants in the EQuIP condition. Perhaps participants on the waitlist—impeded in their goal to receive immediate treatment—in addition to seeking outside treatment, were also motivated to seek additional sources of support from friends, family, and significant others during the wait. Use of a waitlist might also explain why EQuIP participants, who had the support of their therapists during treatment, did not experience significant increases in social support until three months after treatment.
A waitlist design also cannot establish efficacy against existing treatments. Future studies ought to compare this treatment against existing evidence-based treatments involving other theoretical frameworks and modalities. For instance, trauma-informed psychotherapy can be fruitfully adapted to meet the presenting concerns of sexual minority women, especially the large proportion of those with violence and abuse histories as an antecedent cause of current distress (Kaysen et al., 2019). Briefer online treatments (e.g., Lelutiu-Weinberger et al., 2018; Pachankis, Williams, et al., 2020) also represent an important future comparison given their cost-effectiveness and ability to transcend geographic and other access barriers. Comparing the EQuIP intervention to the non-adapted Unified Protocol would pose a strong test of the necessity of EQuIP’s minority-stress-focused components. At the same time, not all benefits of minority-adapted treatments are detected in outcome improvements. Some benefit from such treatments likely derives from lowering access barriers that a minority-specific treatment might address (Bernal, Jiménez-Chafey, & Domenech Rodríguez, 2009; Lau, 2006), improving the treatment’s acceptability, and enhancing patient engagement and retention. Future research ought to test these possibilities.
Other methodological features of this study constrain conclusions. Our assessments relied on self-report rather than interviewer-based diagnoses. Reliability of the rumination scale was low, perhaps weakening our ability to detect intervention effects on this construct. Our minority stress measurements might not have yielded sufficient variability to detect an effect, especially given possible range restriction of some variables (e.g., identity concealment, internalized stigma) in our urban sample, despite our use of an implicit measure to partially circumvent this problem (e.g., the implicit association task of internalized stigma). Future treatment research might wish to recruit participants from a larger range of venues across additional geographic locations, including those likely to contain sexual minorities who experience high degrees of minority stress (e.g., Pachankis, Williams, et al., 2020). Larger diverse samples would allow us to test whether participant characteristics, such as baseline minority stress or demographics, moderate treatment efficacy. Testing intervention efficacy moderation by sexual identity (e.g., bisexual, queer, lesbian) also represents an important future goal given the sizable mental health disparities that exist even within sexual minority populations, particularly those affecting bisexual women, who also experience distinct minority stressors (Dyar & London, 2018; Feinstein & Dyar, 2017) and coping strategies (Davila, Jabbour, Dyar, & Feinstein, 2019). Insufficient range in our alcohol use outcome, introduced by our relatively weak alcohol use inclusion criterion (e.g., one instance of past 90-day heavy drinking) may have also dampened effects. Our follow-up timeframe, while allowing us to detect persistence of some intervention effects over 3 months, was insufficient for allowing us to determine longer-term effects or examine temporal mediators of efficacy. Perhaps outcomes showing weak or nonsignificant effects here, such as minority stress processes, require more time to change. Longer follow-up periods would also allow the longitudinal detection of these processes as intervention mechanisms.
Finally, the relatively small sample size of this trial might have limited power necessary to detect significant changes in all outcomes. Although our sample size was similar to, or somewhat larger than, those used in several previous randomized controlled trials of the Unified Protocol across diverse samples (Farchione et al., 2012; Ehrenreich-May et al., 2017; Kennedy, Bilek, & Ehrenreich-May, 2019) and in previous tests of other CBT-related interventions with sexual minorities (Blashill et al., 2017; Pachankis et al., 2015), the effect sizes found for suicidality and alcohol use problems suggest that future intervention trials would perhaps need to enroll more participants than we did in this relatively small trial to detect a significant effect for these outcomes in condition comparisons. At the same time, we caution against using effect sizes found in this relatively small trial to estimate necessary sample sizes for larger trials (Kraemer, Mintz, Noda, Tinklenberg, & Yesavage, 2006; Leon, Davis, & Kraemer, 2011).1 Or perhaps, as noted above, an intervention that addresses other determinants of sexual minority women’s mental and behavioral health besides minority stress might find stronger effects detectable with smaller sample sizes.
This study begins to remedy the notable gap in evidence-based treatments specifically created and evaluated for sexual minority women. We found that a minority-stress-focused cognitive–behavioral intervention yielded strong improvements in sexual minority women’s mental health outcomes (i.e., depression and anxiety) compared to waitlist control and showed small and moderate reductions in minority stress and universal psychosocial processes, respectively, in pooled pre-post intervention analyses. Future research can determine treatment mechanisms necessary to foster more robust change in alcohol use outcomes, particularly relevant for this population, and clarify the relative importance of a minority stress focus in such a treatment. Ultimately, this study can serve as a starting point from which to explore mechanisms and modalities through which to equip this population with evidence-based mental and behavioral health support.
What is the public health significance of this article?
Sexual minority women represent one of the highest-risk populations for depression, anxiety, and alcohol use problems, yet no intervention has been tested for efficacy for this population’s co-occurring health risks. This first randomized trial of such a treatment shows that a transdiagnostic minority-stress-focused approach has potential to exert robust impact on sexual minority women’s mental health. Future research into additional treatment targets, perhaps beyond minority stress, and factors relevant for reducing alcohol use problems, is needed.
Acknowledgments
The authors would like to acknowledge the following individuals for their help with study coordination, data collection, intervention delivery, and/or clinical supervision: Oluwaseyi Adeyinka, Ricardo Albarran, Alex Belser, Charles Burton, Nitzan Cohen, Emily Finch, Skyler Jackson, Rebecca Kaplan, Colin Kimberlin, Meghan Michalski, Faithlynn Morris, Zachary Rawlings, Maxwell Richardson, Craig Rodriguez-Seijas, Ingrid Solano, Timothy Sullivan, Tenille Taggart, Arjan van der Star, and Roxanne Winston. The authors would like to thank Tonda Hughes and Laurie Drabble for helpful feedback on an earlier version of this manuscript. This study was funded by the National Institute of Mental Health (R01MH109413-02S1: John E. Pachankis), the GLMA Lesbian Health Fund, the Fund for Lesbian and Gay Studies at Yale, and the David R. Kessler, MD ‘55 Fund for LGBTQ Mental Health Research at Yale. The content contained herein is the authors’ own and does not necessarily reflect the views of the funders or the Department of Veterans Affairs.
Footnotes
We would like to thank one of the anonymous reviewers of this manuscript for this helpful suggestion.
Contributor Information
John E. Pachankis, Yale School of Public Health.
Erin M. McConocha, Yale School of Public Health.
Kirsty A. Clark, Yale School of Public Health
Katie Wang, Yale School of Public Health.
Kriti Behari, Yale School of Public Health.
Benjamin K. Fetzner, Yale School of Public Health.
Cal D. Brisbin, Yale School of Public Health.
Jillian R. Scheer, Yale School of Public Health.
Keren Lehavot, VA Puget Sound Health Care System, Seattle, Washington, and University of Washington.
References
- Alterman AI, Cacciola JS, Ivey MA, Habing B, & Lynch KG (2009). Reliability and validity of the alcohol short index of problems and a newly constructed drug short index of problems. Journal of Studies on Alcohol and Drugs, 70, 304–307. 10.15288/jsad.2009.70.304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association. (2011). Practice guidelines for LGB Clients: Guidelines for psychological practice with lesbian, gay, and bisexual clients Retrieved from https://www.apa.org/pi/lgbt/resources/guidelines
- Arnett JJ (2000). Emerging adulthood. A theory of development from the late teens through the twenties. American Psychologist, 55, 469–480. 10.1037/0003-066X.55.5.469 [DOI] [PubMed] [Google Scholar]
- Balsam KF, Martell CR, & Safren SA (2006). Affirmative cognitive-behavioral therapy with lesbian, gay, and bisexual people In Hays PA & Iwamasa GY (Eds.), Culturally responsive cognitive-behavioral therapy: Assessment, practice, and supervision (pp. 223–243). Washington, DC: American Psychological Association; 10.1037/11433-010 [DOI] [Google Scholar]
- Banse R, Seise J, & Zerbes N (2001). Implicit attitudes towards homosexuality: Reliability, validity, and controllability of the IAT. Zeitschrift für Experimentelle Psychologie, 48, 145–160. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, MurrayLatin H, Sauer-Zavala S, … Cassiello-Robbins C. (2017). The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders compared with diagnosis-specific protocols for anxiety disorders: A randomized clinical trial. Journal of the American Medical Association Psychiatry, 74, 875–884. 10.1001/jamapsychiatry.2017.2164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Sauer-Zavala S, Latin HM, Ellard KK, Bullis JR, … Cassiello-Robbins C. (2011). Unified Protocol for Transdiagnostic Treatment of Emotional Disorders. New York, NY: Oxford University Press. [Google Scholar]
- Beard C, Kirakosian N, Silverman AL, Winer JP, Wadsworth LP, & Björgvinsson T (2017). Comparing treatment response between LGBQ and heterosexual individuals attending a CBT- and DBT-skills-based partial hospital. Journal of Consulting and Clinical Psychology, 85, 1171–1181. 10.1037/ccp0000251 [DOI] [PubMed] [Google Scholar]
- Beech AR (2000). Basics of qualitative research: Techniques and procedures for developing grounded theory. Management Learning, 31, 521–542. [Google Scholar]
- Benjamini Y, & Hochberg Y (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society Series B. Methodological, 57, 289–300. 10.1111/j.2517-6161.1995.tb02031.x [DOI] [Google Scholar]
- Bentley KH, Gallagher MW, Carl JR, & Barlow DH (2014). Development and validation of the Overall Depression Severity and Impairment Scale. Psychological Assessment, 26, 815–830. 10.1037/a0036216 [DOI] [PubMed] [Google Scholar]
- Bernal G, Jiménez-Chafey MI, & Domenech Rodríguez MM (2009). Cultural adaptation of treatments: A resource for considering culture in evidence-based practice. Professional Psychology: Research and Practice, 40, 361–368. 10.1037/a0016401 [DOI] [Google Scholar]
- Blanchard KA, Morgenstern J, Morgan TJ, Lobouvie EW, & Bux DA (2003). Assessing consequences of substance use: Psychometric properties of the inventory of drug use consequences. Psychology of Addictive Behaviors, 17, 328–331. 10.1037/0893-164X.17.4.328 [DOI] [PubMed] [Google Scholar]
- Blashill AJ, Safren SA, Wilhelm S, Jampel J, Taylor SW, O’Cleirigh C, & Mayer KH (2017). Cognitive behavioral therapy for body image and self-care (CBT-BISC) in sexual minority men living with HIV: A randomized controlled trial. Health Psychology, 36, 937–946. 10.1037/hea0000505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V, & Clarke V (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Campbell-Sills L, Norman SB, Craske MG, Sullivan G, Lang AJ, Chavira DA, … Stein MB (2009). Validation of a brief measure of anxiety-related severity and impairment: The Overall Anxiety Severity and Impairment Scale (OASIS). Journal of Affective Disorders, 112(1–3), 92–101. 10.1016/j.jad.2008.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter T, Pogacar R, Pullig C, Kouril M, Aguilar S, LaBouff JP, … Chakroff A. (2018). Survey-software Implicit Association Tests: A methodological and empirical analysis. Behavior Research Methods, 51, 2194–2208. [DOI] [PubMed] [Google Scholar]
- Chaudoir SR, Wang K, & Pachankis JE (2017). What reduces sexual minority stress? A review of the intervention “toolkit.” Journal of Social Issues, 73, 586–617. 10.1111/josi.12233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran SD, Björkenstam C, & Mays VM (2017). Sexual orientation differences in functional limitations, disability, and mental health services use: Results from the 2013–2014 National Health Interview Survey. Journal of Consulting and Clinical Psychology, 85, 1111–1121. 10.1037/ccp0000243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran SD, & Mays VM (2009). Burden of psychiatric morbidity among lesbian, gay, and bisexual individuals in the California Quality of Life Survey. Journal of Abnormal Psychology, 118, 647–658. 10.1037/a0016501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbin J, & Strauss A (2015). Basics of qualitative research: Techniques and procedures for developing grounded theory (4th ed.). Thousand Oaks, CA: SAGE Publications, Inc. [Google Scholar]
- Coulter RWS, Kenst KS, Bowen DJ, & Scout. (2014). Research funded by the National Institutes of Health on the health of lesbian, gay, bisexual, and transgender populations. American Journal of Public Health, 104, e105–e112. 10.2105/AJPH.2013.301501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulter RWS, Kinsky SM, Herrick AL, Stall RD, & Bauermeister JA (2015). Evidence of syndemics and sexuality-related discrimination among young sexual-minority women. LGBT Health, 2, 250–257. 10.1089/lgbt.2014.0063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davila J, Jabbour J, Dyar C, & Feinstein BA (2019). Bi visibility: Characteristics of those who attempt to make their bisexual identity visible and the strategies they use. Archives of Sexual Behavior, 48, 199–211. 10.1007/s10508-018-1284-6 [DOI] [PubMed] [Google Scholar]
- Derogatis LR, & Melisaratos N (1983). The Brief Symptom Inventory: An introductory report. Psychological Medicine, 13, 595–605. 10.1017/S0033291700048017 [DOI] [PubMed] [Google Scholar]
- Drabble L, & Eliason MJ (2012). Substance use disorders treatment for sexual minority women. Journal of LGBT Issues in Counseling, 4, 274–292. 10.1080/15538605.2012.726150 [DOI] [Google Scholar]
- Drabble L, Midanik LT, & Trocki K (2005). Reports of alcohol consumption and alcohol-related problems among homosexual, bisexual and heterosexual respondents: Results from the 2000 National Alcohol Survey. Journal of Studies on Alcohol, 66, 111–120. 10.15288/jsa.2005.66.111 [DOI] [PubMed] [Google Scholar]
- Dworkin ER, Gilmore AK, Bedard-Gilligan M, Lehavot K, Guttmannova K, & Kaysen D (2018). Predicting PTSD severity from experiences of trauma and heterosexism in lesbian and bisexual women: A longitudinal study of cognitive mediators. Journal of Counseling Psychology, 65, 324–333. 10.1037/cou0000287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyar C, Feinstein BA, Eaton NR, & London B (2016). Development and initial validation of the Sexual Minority Women Rejection Sensitivity Scale. Psychology of Women Quarterly, 40, 120–137. 10.1177/0361684315608843 [DOI] [Google Scholar]
- Dyar C, & London B (2018). Longitudinal examination of a bisexual-specific minority stress process among bisexual cisgender women. Psychology of Women Quarterly, 42, 342–360. 10.1177/0361684318768233 [DOI] [Google Scholar]
- Ehrenreich-May J, Rosenfield D, Queen AH, Kennedy SM, Remmes CS, & Barlow DH (2017). An initial waitlist-controlled trial of the unified protocol for the treatment of emotional disorders in adolescents. Journal of Anxiety Disorders, 46, 46–55. 10.1016/j.janxdis.2016.10.006 [DOI] [PubMed] [Google Scholar]
- Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, … Barlow DH (2012). Unified protocol for transdiagnostic treatment of emotional disorders: A randomized controlled trial. Behavior Therapy, 43, 666–678. 10.1016/j.beth.2012.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinstein BA, & Dyar C (2017). Bisexuality, minority stress, and health. Current Sexual Health Reports, 9, 42–49. 10.1007/s11930-017-0096-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field A (2013). Discovering statistics using IBM SPSS statistics. Atlanta, GA: Sage. [Google Scholar]
- First MB, Spitzer RL, Williams JBW, & Gibbon M (1997). Structured Clinical Interview for DSM–IV Axis I Disorders (SCID-I): User’s guide and interview. Washington, DC: American Psychiatric Association Press. [Google Scholar]
- Folstein MF, Folstein SE, & McHugh PR (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198. 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- George D, & Mallery P (2010). SPSS for Windows step by step A simple study guide and reference. Boston, MA: Pearson Education, Inc. [Google Scholar]
- Gilman SE, Cochran SD, Mays VM, Hughes M, Ostrow D, & Kessler RC (2001). Risk of psychiatric disorders among individuals reporting same-sex sexual partners in the National Comorbidity Survey. American Journal of Public Health, 91, 933–939. 10.2105/AJPH.91.6.933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore AK, Koo KH, Nguyen HV, Granato HF, Hughes TL, & Kaysen D (2014). Sexual assault, drinking norms, and drinking behavior among a national sample of lesbian and bisexual women. Addictive Behaviors, 39, 630–636. 10.1016/j.addbeh.2013.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 26, 41–54. 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- Greenwald AG, Nosek BA, & Banaji MR (2003). Understanding and using the implicit association test: I. An improved scoring algorithm. Journal of Personality and Social Psychology, 85, 197–216. 10.1037/0022-3514.85.2.197 [DOI] [PubMed] [Google Scholar]
- Grella CE, Greenwell L, Mays VM, & Cochran SD (2009). Influence of gender, sexual orientation, and need on treatment utilization for substance use and mental disorders: Findings from the California Quality of Life Survey. BMC Psychiatry, 9, 52 10.1186/1471-244X-9-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML (2009). How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin, 135, 707–730. 10.1037/a0016441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML (2014). Structural stigma and the health of lesbian, gay, and bisexual populations. Current Directions in Psychological Science, 23, 127–132. 10.1177/0963721414523775 [DOI] [Google Scholar]
- Hatzenbuehler ML, Corbin WR, & Fromme K (2008). Trajectories and determinants of alcohol use among LGB young adults and their heterosexual peers: Results from a prospective study. Developmental Psychology, 44, 81–90. 10.1037/0012-1649.44.1.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Dovidio JF, Nolen-Hoeksema S, & Phills CE (2009). An implicit measure of anti-gay attitudes: Prospective associations with emotion regulation strategies and psychological distress. Journal of Experimental Social Psychology, 45, 1316–1320. 10.1016/j.jesp.2009.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, McLaughlin KA, & Nolen-Hoeksema S (2008). Emotion regulation and internalizing symptoms in a longitudinal study of sexual minority and heterosexual adolescents. Journal of Child Psychology and Psychiatry, 49, 1270–1278. 10.1111/j.1469-7610.2008.01924.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes TL, Wilsnack SC, & Kantor LW (2016). The influence of gender and sexual orientation on alcohol use and alcohol-related problems: Toward a Global perspective. Alcohol Research: Current Reviews, 38, 121–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jellison WA, McConnell AR, & Gabriel S (2004). Implicit and explicit measures of sexual orientation attitudes: In group preferences and related behaviors and beliefs among gay and straight men. Personality and Social Psychology Bulletin, 30, 629–642. 10.1177/0146167203262076 [DOI] [PubMed] [Google Scholar]
- Jenerette C, & Dixon J (2010). Developing a short form of the simple Rathus assertiveness schedule using a sample of adults with sickle cell disease. Journal of Transcultural Nursing, 21, 314–324. 10.1177/1043659609360712 [DOI] [PubMed] [Google Scholar]
- Kaufman EA, Xia M, Fosco G, Yaptangco M, Skidmore CR, & Crowell SE (2016). The Difficulties in Emotion Regulation Scale Short Form (DERS-SF): Validation and replication in adolescent and adult samples. Journal of Psychopathology and Behavioral Assessment, 38, 443–455. 10.1007/s10862-015-9529-3 [DOI] [Google Scholar]
- Kaysen D, Lehavot K, & Dworkin ER (2019). Application of evidence-based practices for trauma-related disorders among sexual minority women In Pachankis JE & Safren SA (Eds.), Handbook of evidence-based mental health practice with sexual and gender minorities (pp. 244–267). New York, NY: Oxford University Press. [Google Scholar]
- Kennedy SM, Bilek EL, & Ehrenreich-May J (2019). A randomized controlled pilot trial of the unified protocol for transdiagnostic treatment of emotional disorders in children. Behavior Modification, 43, 330–360. 10.1177/0145445517753940 [DOI] [PubMed] [Google Scholar]
- King M, Semlyen J, Tai SS, Killaspy H, Osborn D, Popelyuk D, & Nazareth I (2008). A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry, 8, 70 10.1186/1471-244X-8-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Mintz J, Noda A, Tinklenberg J, & Yesavage JA (2006). Caution regarding the use of pilot studies to guide power calculations for study proposals. Archives of General Psychiatry, 63, 484–489. 10.1001/archpsyc.63.5.484 [DOI] [PubMed] [Google Scholar]
- Lane KA, Banaji MR, Nosek BA, & Greenwald AG (2007). Understanding and using the Implicit Association Test: IV In Wittenbrink B & Schwarz N (Eds.), Implicit measures of attitudes (pp. 59–102). New York, NY: Guilford Press. [Google Scholar]
- Lang AJ, Norman SB, Means-Christensen A, & Stein MB (2009). Abbreviated brief symptom inventory for use as an anxiety and depression screening instrument in primary care. Depression and Anxiety, 26, 537–543. [DOI] [PubMed] [Google Scholar]
- Lau AS (2006). Making the case for selective and directed cultural adaptations of evidence-based treatments: Examples from parent training. Clinical Psychology: Science and Practice, 13, 295–310. 10.1111/j.1468-2850.2006.00042.x [DOI] [Google Scholar]
- Lehavot K, Balsam KF, & Ibrahim-Wells GD (2009). Redefining the American quilt: Definitions and experiences of community among ethnically diverse lesbian and bisexual women. Journal of Community Psychology, 37, 439–458. 10.1002/jcop.20305 [DOI] [Google Scholar]
- Lehavot K, & Simoni JM (2011). The impact of minority stress on mental health and substance use among sexual minority women. Journal of Consulting and Clinical Psychology, 79, 159–170. 10.1037/a0022839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lelutiu-Weinberger C, Manu M, Ionescu F, Dogaru B, Kovacs T, Dorobăntescu C, … Pachankis JE(2018). An mHealth intervention to improve young gay and bisexual men’s sexual, behavioral, and mental health in a structurally stigmatizing national context. JMIR mHealth and uHealth, 6(11), e183 10.2196/mhealth.9283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon AC, Davis LL, & Kraemer HC (2011). The role and interpretation of pilot studies in clinical research. Journal of Psychiatric Research, 45, 626–629. 10.1016/j.jpsychires.2010.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Seeley JR, Roberts RE, & Allen NB (1997). Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and Aging, 12, 277–287. 10.1037/0882-7974.12.2.277 [DOI] [PubMed] [Google Scholar]
- Lewis RJ, Mason TB, Winstead BA, Gaskins M, & Irons LB (2016). Pathways to hazardous drinking among racially and socioeconomically diverse lesbian women: Sexual minority stress, rumination, social isolation, and drinking to cope. Psychology of Women Quarterly, 40, 564–581. 10.1177/0361684316662603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt DM, Lewis MA, Rhew IC, Hodge KA, & Kaysen DL (2015). Reciprocal relationships over time between descriptive norms and alcohol use in young adult sexual minority women. Psychology of Addictive Behaviors, 29, 885–893. 10.1037/adb0000122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meijer RR, de Vries RM, & van Bruggen V (2011). An evaluation of the Brief Symptom Inventory-18 using item response theory: Which items are most strongly related to psychological distress? Psychological Assessment, 23, 193–202. 10.1037/a0021292 [DOI] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129, 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, & Ouellette SC (2009). Unity and purpose at the intersections of racial/ethnic and sexual identities In Hammack PL & Cohler BJ (Eds.), The story of sexual identity: Narrative perspectives on the gay and lesbian life course (pp. 79–106). New York, NY: Oxford University Press; 10.1093/acprof:oso/9780195326789.003.0004 [DOI] [Google Scholar]
- Meyer IH, Rossano L, Ellis JM, & Bradford J (2002). A brief telephone interview to identify lesbian and bisexual women in random digit dialing sampling. Journal of Sex Research, 39, 139–144. 10.1080/00224490209552133 [DOI] [PubMed] [Google Scholar]
- Millar BM, Wang K, & Pachankis JE (2016). The moderating role of internalized homonegativity on the efficacy of LGB-affirmative psychotherapy: Results from a randomized controlled trial with young adult gay and bisexual men. Journal of Consulting and Clinical Psychology, 84, 565–570. 10.1037/ccp0000113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr JJ, & Kendra MS (2011). Revision and extension of a multidimensional measure of sexual minority identity: The Lesbian, Gay, and Bisexual Identity Scale. Journal of Counseling Psychology, 58, 234–245. 10.1037/a0022858 [DOI] [PubMed] [Google Scholar]
- Morris SB (2008). Estimating effect sizes from pretest-posttest-control group designs. Organizational Research Methods, 11, 364–386. 10.1177/1094428106291059 [DOI] [Google Scholar]
- Norman SB, Cissell SH, Means-Christensen AJ, & Stein MB (2006). Development and validation of an Overall Anxiety Severity and Impairment Scale (OASIS). Depression and Anxiety, 23, 245–249. 10.1002/da.20182 [DOI] [PubMed] [Google Scholar]
- Pachankis JE (2014). Uncovering clinical principles and techniques to address minority stress, mental health, and related health risks among gay and bisexual men. Clinical Psychology: Science and Practice, 21, 313–330. 10.1111/cpsp.12078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE (2015). A transdiagnostic minority stress treatment approach for gay and bisexual men’s syndemic health conditions. Archives of Sexual Behavior, 44, 1843–1860. 10.1007/s10508-015-0480-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE (2018). The scientific pursuit of sexual and gender minority mental health treatments: Toward evidence-based affirmative practice. American Psychologist, 73, 1207–1219. 10.1037/amp0000357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, & Bränström R (2018). Hidden from happiness: Structural stigma, sexual orientation concealment, and life satisfaction across 28 countries. Journal of Consulting and Clinical Psychology, 86, 403–415. 10.1037/ccp0000299 [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Clark K, Burton C, White Hughto JM, Bränström R, & Keene DE (2020). Sex, status, competition, and exclusion: Intraminority stress from within the gay community and sexual minority men’s mental health. Journal of Personality and Social Psychology. Advance online publication. 10.1037/pspp0000282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, Hatzenbuehler ML, Rendina HJ, Safren SA, & Parsons JT (2015). LGB-affirmative cognitive-behavioral therapy for young adult gay and bisexual men: A randomized controlled trial of a transdiagnostic minority stress approach. Journal of Consulting and Clinical Psychology, 83, 875–889. 10.1037/ccp0000037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, Williams SL, Behari K, Job S, McConocha EM, & Chaudoir SR (2020). Brief online interventions for LGBTQ young adult mental and behavioral health: A randomized controlled trial in a high-stigma, low-resource context. Journal of Consulting and Clinical Psychology, 88, 429–444. 10.1037/ccp0000497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Rathus SA (1973). A 30-item schedule for assessing assertive behavior. Behavior Therapy, 4, 398–406. 10.1016/S0005-7894(73)80120-0 [DOI] [Google Scholar]
- Reid AE, Dovidio JF, Ballester E, & Johnson BT (2014). HIV prevention interventions to reduce sexual risk for African Americans: The influence of community-level stigma and psychological processes. Social Science & Medicine, 103, 118–125. 10.1016/j.socscimed.2013.06.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice CE, Vasilenko SA, Fish JN, & Lanza ST (2019). Sexual minority health disparities: An examination of age-related trends across adulthood in a national cross-sectional sample. Annals of Epidemiology, 31, 20–25. 10.1016/j.annepidem.2019.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimes KA, Ion D, Wingrove J, & Carter B (2019). Sexual orientation differences in psychological treatment outcomes for depression and anxiety: National cohort study. Journal of Consulting and Clinical Psychology, 87, 577–589. 10.1037/ccp0000416 [DOI] [PubMed] [Google Scholar]
- Roberts AL, Austin SB, Corliss HL, Vandermorris AK, & Koenen KC (2010). Pervasive trauma exposure among U.S. sexual orientation minority adults and risk of posttraumatic stress disorder. American Journal of Public Health, 100, 2433–2441. 10.2105/AJPH.2009.168971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szymanski DM, & Chung YB (2003). Internalized homophobia in lesbians. Journal of Lesbian Studies, 7, 115–125. 10.1300/J155v07n01_08 [DOI] [PubMed] [Google Scholar]
- Timmins L, Rimes KA, & Rahman Q (2020). Minority stressors, rumination, and psychological distress in lesbian, gay, and bisexual individuals. Archives of Sexual Behavior. Archives of Sexual Behavior, 49, 661–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treynor W, Gonzalez R, & Nolen-Hoeksema S (2003). Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research, 27, 247–259. 10.1023/A:1023910315561 [DOI] [Google Scholar]
- U.S. Department of Health and Human Services. (2015). Drinking levels defined Retrieved from https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking [DOI] [PubMed]
- van Spijker BAJ, Batterham PJ, Calear AL, Farrer L, Christensen H, Reynolds J, & Kerkhof AJ (2014). The Suicidal Ideation Attributes Scale (SIDAS): Community-based validation study of a new scale for the measurement of suicidal ideation. Suicide & Life-Threatening Behavior, 44, 408–419. 10.1111/sltb.12084 [DOI] [PubMed] [Google Scholar]
- Wilamowska ZA, Thompson-Hollands J, Fairholme CP, Ellard KK, Farchione TJ, & Barlow DH (2010). Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depression and Anxiety, 27, 882–890. 10.1002/da.20735 [DOI] [PubMed] [Google Scholar]
- Wilson SM, Gilmore AK, Rhew IC, Hodge KA, & Kaysen DL (2016). Minority stress is longitudinally associated with alcohol-related problems among sexual minority women. Addictive Behaviors, 61, 80–83. 10.1016/j.addbeh.2016.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet GD, Powell SS, Farley GK, Werkman S, & Berkoff KA (1990). Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. Journal of Personality Assessment, 55, 610–617. 10.1080/00223891.1990.9674095 [DOI] [PubMed] [Google Scholar]