Abstract
Objectives
The aim of this study was to assess the effects of coexposure to job strain and shift work on mental health in railway workers.
Design
Cross-sectional study.
Setting
One Railway Bureau Group in China.
Participants
A total of 1270 front-line railway workers.
Outcome measures
The Symptom Checklist-90-Revised questionnaire was used to measure general mental health. Job strain variables were derived from the Job Content Questionnaire. Based on the records of the work schedule 3 months prior to the survey, the following three shift types were identified: fixed day, fixed night and rotating night shifts. Risks associated with mental health were assessed by carrying out logistic regression analysis which was adjusted for age, job tenure, smoking and exercise. Additionally, a crossover analysis was employed for the combined effects.
Results
High levels of job strain were linked to a higher risk of poor mental health (OR=1.53, 95% CI: 1.10 to 2.11). After adjusting for confounding factors, night shifts and rotating night shifts were significant risk factors for mental health (OR=2.21, 95% CI: 1.60 to 3.07; OR=2.36, 95% CI: 1.73 to 3.22). Compared with participants who experienced a low level of job strain and day shifts, those with a high level of job strain and who worked rotating shifts were at the highest risk of poor mental health (OR=4.68, 95% CI: 2.91 to 8.04), whereas the influence of a low level of job strain and rotating night shifts was not statistically significant.
Conclusion
Job strain and night shifts among workers were associated, both independently and in combination, with an increased risk of poor mental health. Our data suggest that job strain contributes to the risk of poor mental health by means of a combined effect with shift work.
Keywords: mental health, occupational & industrial medicine, public health
Strengths and limitations of this study.
Our study shows the relationship of job strain and shift work on mental health in front-line railway workers.
Our study included three shift types: fixed day, fixed night and rotating night shifts.
A randomly selected sample and analyses controlled by job tenure, smoking and exercise.
Given the cross-sectional research design used, only statistical associations can be observed, and hence, strong causal claims are not strictly proven.
Subjective assessment of job strain (questionnaire) did not allow a more objective evidence.
Introduction
Mental health disorders are a major public health concern, both globally and within China.1 In fact, mental health (including substance abuse) affected more than one billion people globally in 2016, and caused 7% of all global burdens of disease as measured in Disability-Adjusted Life Years, and the trend is still rising.2 3 Mental disorders associated with chronic physical disease are more prevalent among specific occupational groups, and are a leading cause of absenteeism and long-term work incapacity.4 5
Many factors can influence mental health, including work-related stress.6 Epidemiological studies have shown that job strain is linked to mental health and an increased risk of psychological disorders.7 8 A large British cohort study assessed the prospective association between job strain and the onset of common mental disorders, and found that high job demands, low job control and high job strain remained significant independent predictors of the future onset of common mental disorders.9 One study of healthy Swedish working men and women found that job strain was as strongly related to depressive symptoms among men as among women, and women reported higher levels of job strain than men.10 Another study found that repeated job strain and low social support at work were associated with an increased risk of major depressive disorder, and after adjusting for earlier psychological distress, the results held.11 These findings suggest that modifiable work-related risk factors might be an important factor for efforts to reduce the prevalence of mental disorders.
In addition to occupational stressors, shift work can increase the risk of mental health problems.12 Since the industrial revolution, night shift work has become more and more common, and it is widespread within the services and fabricating industries as well as the transportation, hospitality, manufacturing and healthcare sectors.13 Night shift work can be defined as a working schedule which involved working partly or entirely during night.14 Studies have shown that long-term shifts can disrupt the 24-hour circadian rhythms and increase the risk of sleep disorders.15 In addition, a close relationship has been found between shift work and many chronic diseases, such as cancer, metabolic disorders, cardiovascular diseases and mental health disorders.12 16–19 Night shifts are known to disturb circadian rhythms by affecting melatonin secretion, stress hormones and autoimmune functions, which leads to impaired psychological well-being. Moreover, night shifts may also impair an individual’s work–life balance and social interactions, which contributes to greater mental distress.20 21
China’s total railway mileage reached 97 625 km by 2012, and is predicted to top 1 20 000 km by 2020, ranking second in the world after the USA. As the world’s largest populated country and the fourth largest country by area, China has the highest rail transportation density in the world (39.95 million equated ton-km/km in 2012).22 The increasing traffic volume results in a heavy workload for about 2 million railway workers in China. Except for the heavy workload, the front-line workers often have irregular working schedules.23 Workers in transportation industries have higher rates of mental disorders, depression and physical health effects than workers in other occupations, including professional and managerial occupations.24 There is increasing concern about the health and well-being of railway workers, which is related to the safety of the country’s transportation infrastructure.
Although several studies have highlighted the role of job strain or shift work in mental health, the combined effect of job strain and shift work on mental health in railway workers has received considerably less attention. We addressed this issue among railway workers in the Fuzhou region of Fujian Province in China. The study aimed to examine the main effect of shift work and job strain on mental health, and the effect of the combined exposure to shift work and job strain on mental health.
Methods
Study design and participants
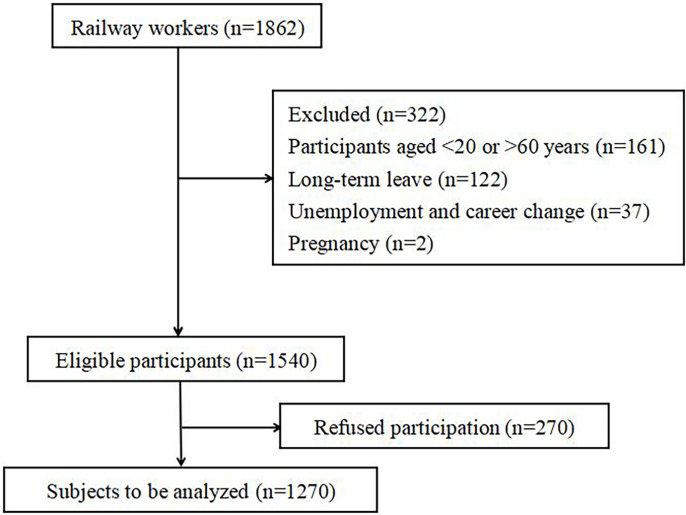
This research was carried out as part of the Occupational Health Study of Railway Workers in China and was conducted between March and September 2019. The target population included front-line employees of the Fuzhou branch of the China Railway Nanchang Bureau Group Co. in Fuzhou City, Fujian province, China. The administration bureau has eight subordinate units and about 20 000 employees, and covers all work related to the railway industry. In summary, we used a stratified sampling method (stratified in shifts) to randomly select participants who had worked for a minimum of 1 year so that they could take part in an interview. Information about the study, with an invitation to participate, was orally passed on to the randomly selected workers by administration bureau’ s managers in face-to-face meetings. Meanwhile, with the assistance of the managers, an announcement was forwarded to workers to explain that the survey was designed ‘to better understand how job strain and shift work affect mental health’. A total of 1862 workers were invited to participate. The exclusion criteria focused on participants’ work experience, as well as their medical and medication history. Participants aged <20 or >60 years, who had been absent from work due to sick and occupational injuries, or who were stationed abroad, were excluded. Based on this criteria, 1540 participants remained eligible. Participants were voluntary; responses were confidential and participation did not affect healthcare benefits. Ultimately, 1270 workers consented to participate in the study (figure 1). Once an individual was identified and their formal consent was obtained, a face-to-face interview was conducted during the annual professional health examination. This interview was carried out by trained interviewers using a questionnaire that included sociodemographic, job strain, shift work and mental health components.
Figure 1.
Flow of excluded individuals in the cross-sectional study.
Exposure assessment
The Job Content Questionnaire (JCQ) is one of the most widely used instruments to estimate job strain, and it is based on the Job Demand-Control model.25 It is believed that job strain stems from an imbalance between work-related demands and an individual’s control. The JCQ is widely used in the field of job strain research. The Chinese version of the JCQ was developed by domestic scholars, and has high reliability and validity.26 In our study, 22 items from the original 49-item JCQ were applied, and they consisted of three dimensions: job demand, job control and workplace social support. Each item was scored using a four-point Likert-type scale which ranged from ‘strongly disagree’ to ‘strongly agree’, with higher scores indicating a higher level of psychological job demands, job control and workplace social support. In line with previously published studies, the scores for these subscales were divided into tertiles (low, medium and high scores).9 27 A job strain measure was computed using a combination of the job demands and control subscales, producing nine exposure categories which were further classified into three levels of job strain including low, intermediate and high.9 In the present study, Cronbach’s alpha coefficients for demand latitude, job control and social support of the JCQ-22 were 0.81, 0.79 and 0.86, respectively.
Shift work categories: according to the work schedules record held by the branch which related to the 3 months prior to the interviews, we classified workers into day shifts, night shifts and rotating night shifts. Day shift workers worked only during the day, according to the schedules, and their working hours were from 8:00 a.m. or 9:00 a.m. to 8:00 p.m. or 9:00 p.m. Night shift workers worked only during the night, according to the nature of the work and the schedules, and their working hours were strictly controlled and operated from 10 p.m. or 11 p.m. to 6 a.m. (need avoid driving hours). Rotating night shift workers was defined as at least five night shifts (not necessarily five consecutive nights) per month in addition to day shifts in that month. Note that if workers has three consecutive night shifts and above, the schedule includes the following 2 days off. Descriptive statistics of the exposures are shown in table 1.
Table 1.
Descriptive statistics of the exposures
| Exposures variable | All | |
| n | % | |
| Job strain | ||
| Low | 349 | 27.5 |
| Medium | 628 | 49.4 |
| High | 293 | 23.1 |
| Shift types | ||
| Day shift | 300 | 23.6 |
| Night shift | 442 | 34.8 |
| Rotating night shift | 528 | 41.6 |
Outcome
We measured the general mental health of participants using the Symptom Checklist-90-Revised (SCL-90-R) which is a self-administrated questionnaire used to measure psychological distress and psychological symptoms, and this questionnaire has been used in several community-based epidemiology studies.28 It consists of 90 items across nine primary symptom domains: (a) somatisation, (b) obsessive–compulsive, (c) interpersonal sensitivity, (d) depression, (e) anxiety, (f) hostility, (g) phobic anxiety, (h) paranoid ideation and (i) psychoticism. Participant’s responses were measured using a five-point Likert-type scale ranging from 0 (‘asymptomatic’) to 4 (‘very severe’). A total score of >160 is a possible indication of mental health problems.29 The Chinese version of the SCL-90-R has high reliability and validity, and can be used to measure psychological distress and psychological symptoms among the Chinese population.30 In the current study, Cronbach’s alpha was 0.854. The internal reliabilities of all nine subscales were greater than 0.8.
Covariates
Several demographic, socioeconomic, occupational and lifestyle factors have been shown to be associated with mental health. Therefore, such factors may represent potential confounding variables for the results of any combined exposure to mental health and job strain or shift work. We considered the following variables in the study: sex, age (<30, 30–40, 40–50, >50 years) and marital status (married/unmarried). Occupational factors included job tenure (<10, 10–20, >20 years). The following lifestyle factors were considered: alcohol consumption, no (never or rarely)/yes (daily or often); smoking, ‘no’ (never or rarely) or ‘yes’ (daily or occasionally); and exercise, which was assessed with the question: ‘During the past month, how many times have you exercised?’ The choice of response included ‘no’ (never or rarely) or ‘regularly’ (three times or more per week, and exercise was at least 1 hour in duration in each occasion).
Statistical analysis
Analyses were carried out using SPSS for Windows V.20.0. Data were summarised using frequencies for categorical data. χ2 tests were used to compare demographic characteristics. ORs and 95% CIs were determined for the risk associated with mental health using logistic regression. The combined effect of job strain and shift work on mental health was evaluated by carrying out a crossover analysis. All of the models were adjusted for age, job tenure, smoking and exercise. The tests were two-tailed and the significance level was set at p<0.05.
Patient and public involvement
Patients and the public were not involved in the design or planning of the study.
Results
The characteristics of 1270 participants who took part in this study are shown in table 2. Approximately, 532 participants were identified as having mental health problems according to the cut-off score. Therefore, the prevalence of mental health problems among participants was 41.9% (532/1270). We found group differences with respect to the prevalence of mental health problems in the case of job tenure, smoking and exercise (p<0.05). Participants whose job tenure was <10 years were more likely to report poor mental health than those whose tenure was 10–20 years or >20 years (45.0% vs 39.5% vs 38.6%). Participants who smoked reported more mental health problems than than those who did not smoke (50.9% vs 36.3%). Participants who did not exercise reported more mental health problems than those who engaged in regular exercise (44.90% vs 35.0%). No statistically significant associations were observed between mental health problems and other variables such as age, sex, marital status and alcohol consumption (p>0.05).
Table 2.
Prevalence of poor mental health according to participant characteristics
| Characteristics | n | No. of mental health problems | Prevalence (%) | χ2 | P value |
| Age (years) | |||||
| <30 | 552 | 228 | 41.3 | 3.012 | 0.390 |
| 30–40 | 217 | 102 | 47.0 | ||
| 40–50 | 277 | 110 | 39.7 | ||
| >50 | 224 | 92 | 41.1 | ||
| Sex | |||||
| Male | 1242 | 520 | 41.9 | 0.011 | 0.916 |
| Female | 28 | 12 | 42.9 | ||
| Job tenure (years) | |||||
| <10 | 720 | 324 | 45.0 | 6.959 | 0.031 |
| 10–20 | 167 | 60 | 35.9 | ||
| >20 | 383 | 148 | 38.6 | ||
| Marital status | |||||
| Unmarried | 404 | 180 | 44.6 | 1.728 | 0.189 |
| Married | 866 | 352 | 40.6 | ||
| Alcohol consumption | |||||
| Yes | 961 | 404 | 42.0 | 0.036 | 0.849 |
| No | 309 | 128 | 41.4 | ||
| Smoking | |||||
| Yes | 483 | 246 | 50.9 | 26.178 | <0.001 |
| No | 787 | 286 | 36.3 | ||
| Exercise | |||||
| Regularly | 386 | 135 | 35.0 | 10.895 | 0.001 |
| No | 884 | 397 | 44.9 |
The results of unconditional logistic regression analyses of the relationship between mental health and job strain after adjusting for age, job tenure, smoking and exercise are shown in table 3. The risk of poor mental health was higher among those who experienced a high level of job strain compared with low levels of job strain (OR=1.80, 95% CI: 1.31 to 2.47). The significant association persisted after adjusting for all other confounding factors, and greater odds of exhibiting case-level symptoms of common mental disorders were observed in relation to higher level of job strain (OR=1.53, 95% CI: 1.10 to 2.11), higher job demands (OR=2.28, 95% CI: 1.64 to 3.17), lower job control (OR=1.54, 95% CI: 1.18 to 2.02) and lower social support (OR=2.00, 95% CI: 1.46 to 2.75).
Table 3.
ORs for mental health in relation to the different job strain exposures
| Variables | Model 1 | Model 2 | |||
| n (%) | OR (95% CI) | P value | OR (95% CI) | P value | |
| Job strain | |||||
| Low | 349 (27.5%) | 1.00 | — | 1.00 | — |
| Medium | 628 (49.4%) | 1.04 (0.79 to 1.36) | 0.781 | 0.99 (0.75 to 1.30) | 0.932 |
| High | 293 (23.1%) | 1.80 (1.31 to 2.47) | 0.009 | 1.53 (1.10 to 2.11) | 0.011 |
| Job demand | |||||
| Low | 496 (39.1%) | 1.00 | — | 1.00 | — |
| Medium | 519 (40.9%) | 1.49 (1.08 to 2.06) | 0.016 | 1.45 (1.04 to 2.03) | 0.030 |
| High | 255 (20.0%) | 2.54 (1.85 to 3.50) | <0.001 | 2.28 (1.64 to 3.17) | <0.001 |
| Job control | |||||
| Low | 585 (46.1%) | 1.70 (1.31 to 2.21) | <0.001 | 1.54 (1.18 to 2.02) | 0.002 |
| Medium | 279 (22.0%) | 1.49 (1.09 to 2.04) | 0.013 | 1.49 (1.08 to 2.06) | 0.008 |
| High | 406 (31.9%) | 1.00 | – | 1.00 | – |
| Social support | |||||
| Low | 540 (42.5%) | 2.06 (1.52 to 2.79) | <0.001 | 2.00 (1.46 to 2.75) | <0.001 |
| Medium | 457 (36.0%) | 1.33 (0.97 to 1.82) | 0.078 | 1.30 (0.94 to 1.80) | 0.109 |
| High | 273 (21.5%) | 1.00 | – | 1.00 | – |
Model 1 is crude. Model 2 is adjusted for age, job tenure, smoking and exercise.
CI, confidence interval; OR, odds ratio.
The results of multivariate analyses of the relationship between mental health and shift types after adjusting for age, job tenure, smoking and exercise are shown in table 4. The significant association persisted after adjusting for all other confounding factors, and mental disorders were associated with shift types, especially night shifts (OR=2.21, 95% CI: 1.60 to 3.07) and rotating night shifts (OR=2.36, 95% CI: 1.73 to 3.22).
Table 4.
ORs for mental health in relation to the different shift type exposures
| Shift types | Model 1 | Model 2 | |||
| n (%) | OR (95% CI) | P value | OR (95% CI) | P value | |
| Day shift | 300 (23.6%) | 1.00 | – | 1.00 | – |
| Night shift | 442 (34.8%) | 2.64 (1.91 to 3.66) | <0.001 | 2.21 (1.60 to 3.07) | <0.001 |
| Rotating night shift | 528 (41.6%) | 3.18 (2.32 to 4.36) | <0.001 | 2.36 (1.73 to 3.22) | <0.001 |
Model 1 is crude. Model 2 is adjusted for age, job tenure, smoking and exercise.
CI, confidence interval; OR, odds ratio.
To investigate the combined exposure to job strain and shift work with respect to mental health, participants were divided into high-job-strain, low-job-strain or moderate-job-strain groups, and day-shift, night-shift or rotating night shift types (table 5). The crossover analysis showed that compared with participants with low or moderate levels of job strain who worked day shifts, day shift workers with high levels of job strain were more likely to have poor mental health (OR=2.80, 95% CI: 1.95 to 4.02), as were participants with high levels of job strain who worked night shifts (OR=4.57, 95% CI: 2.78 to 7.52). Those with high levels of job strain who work rotating night shifts had the highest likelihood of experiencing mental health problems (OR=5.53, 95% CI: 3.45 to 8.88). Participants with low or moderate levels of job strain who worked night shifts were at risk of poor mental health (OR=2.33, 95% CI: 1.61 to 3.39). The combined effect to job strain and shift work remained significant after adjusting for confounding factors, including age, job tenure, smoking and exercise, which were associated with poor mental health (OR=2.52, 95% CI: 1.64 to 3.57 for high levels of job strain and the day shift; and OR=4.33, 95% CI: 2.63 to 7.14 for high levels of job strain and the night shift and OR=4.68, 95% CI: 2.91 to 8.04 for high levels of job strain and the rotating night shift when compared with lower or moderate levels of job strain and the day shift).
Table 5.
The combined effect to job strain and shift types on mental health
| Job strain | Shift types | Model 1 | Model 2 | ||
| OR (95% CI) | P value | OR (95% CI) | P value | ||
| Low and medium | Day shift | 1.00 | – | 1.00 | – |
| Low and medium | Night shift | 2.33 (1.61 to 3.39) | <0.001 | 2.06 (1.42 to 2.99) | <0.001 |
| Low and medium | Rotating night shift | 1.16 (0.62 to 2.17) | 0.651 | 0.90 (0.43 to 1.72) | 0.935 |
| High | Day shift | 2.80 (1.95 to 4.02) | <0.001 | 2.52 (1.64 to 3.57) | <0.001 |
| High | Night shift | 4.57 (2.78 to 7.52) | <0.001 | 4.33 (2.63 to 7.14) | <0.001 |
| High | Rotating night shift | 5.53 (3.45 to 8.88) | <0.001 | 4.68 (2.91 to 8.04) | <0.001 |
Model 1 is crude. Model 2 is adjusted for age, job tenure, smoking and exercise.
CI, confidence interval; OR, odds ratio.
Discussion
This study investigated the potential relationship between job stress, shift work, psychological and behavioural factors and mental health. This is the first study to examine a combined effect between job strain and shift types with respect to mental health among Chinese railway workers. This study’s main findings show that job strain and shift work are correlated with mental health, and a combined exposure to high levels of job strain and rotating shifts were associated with poor mental health among railway workers.
The influence of work conditions on mental health has been extensively studied over the past decades. Specifically, the adverse effect of high levels of job strain on mental health problems has been widely accepted.7 Indeed, in the present study, the multivariate logistic regression analyses revealed that workers with high levels of job strain, encompassing lower job control and higher job demands, were at a greater risk of poor mental health than those who experienced low or moderate levels of strain. Some studies also suggest that exposure to chronic stressors, such as job strain, can cause dysregulation of the hypothalamic–pituitary–adrenal (HPA) axis and subsequent physiological changes that are involved in the pathophysiology of depression, including loss of neuroplasticity, inhibition of neurogenesis and increased inflammation, which implies that stress disrupts normal mental health via HPA axis activation.31
Shift work is now very common in most countries.32 The high prevalence of shift work has led to concerns about its potential adverse impact on health. The current research indicated that shift work has an even clearer impact on mental health than job strain. Night shifts, especially rotating night shifts, were identified as a risk factor for psychological problems among front-line railway workers in China. Our findings are consistent with a previous study which reported higher risks of mental health problems among night shift workers than day shift workers.12 33 Interestingly, the role of rotating night shifts has been noticed. The sample population in this study largely included male front-line railway workers, and rotating night shifts were also found associated with increased mental health symptoms. A study found that rotating night shifts were associated with greater health risks than permanent night shifts, suggesting that the former shift type might be implicated in greater disruptions to physiological rhythms, and workers may have less time to adapt to the circadian clock.34
Our findings offer new insight into the impact of job strain and night shifts on mental health. The results of this study suggest that a combined exposure to high levels of job strain and rotating night shifts may occur in a additive fashion. In other words, the combined effect (OR=5.53) was greatest, and the relationship was also confirmed by adjusting potential confounding factors. These results suggest that employers should consider strategies for reducing the mental health burden of shift workers, such as offering more job control, reducing job strain and providing more social support at work. Workplace policies, programmes and practices could promote awareness of the associated risk factors, and enable access to mental health services.12 Moreover, the magnitude of the OR was not statistically significant for the subgroup who worked rotating night shifts when compared with those who worked day shifts, when there is low and moderate job strain. This may suggest a mediating role for job strain in the shift work and mental health relationship.12 According to the Job Demand-Control model, low job strain means low job demand or high job control, and may include a high level of social support. Multiple studies suggest that these factors may act as a buffer in regulating mental health.35 36
Some limitations of the current study and recommendations for future efforts should be considered. First, both job strain and mental health were self-reported, which may lead to single/common source bias and inflate the ORs.37 Second, lifestyle factors, such as alcohol, smoking and exercise, may vary greatly, for example, ‘never or rarely alcohol’ versus ‘daily or often’. This may lead to reporting bias, such that more participants reported ‘never’ or ‘rarely’ responses. Third, individual differences in terms of vulnerability to mental health could be expected. For instance, evening-type people who have a better ability to cope with shift work may have self-selected night jobs. Moreover, younger workers are more likely to be assigned night shifts or rotating night shifts. On the other hand, poor health conditions might cause workers to quit shift work, which could lead to a healthy worker selection bias. Longitudinal studies, which follow workers’ occupational paths, are needed to confirm the causal relationships between shift work and health outcomes, as well as to avoid selection effects.
Conclusion
Our study suggests that workers who experience job strain or who work night shifts were more likely to suffer from mental health problems than day shift workers. Furthermore, we found that rotating night shift workers were also at a high risk of mental health problems. While further studies are needed to fully understand the biological and social consequences of job strain, night shifts and rotating shift among different genders and different subgroups, we suggest that employers and occupational health practitioners should pay attention to the impacts of the combined exposure to job strain and shift work, and effects on workers’ health and well-being. Furthermore, a suitable working schedule should be designed to minimise adverse health consequences.
Supplementary Material
Acknowledgments
The authors wish to acknowledge all of the participants in this study.
Footnotes
Contributors: YJ participated in the study design, data collation, analysis, interpretation of the data and drafted the manuscript and tables. CW contributed to interpretation of the data. TH, MC and WL assisted field investigation and collected the data. YZ, ZC and XX contributed data curation and formal analysis. All authors critically revised the manuscript.
Funding: This research was funded by the Startup Fund for scientific research, Fujian Medical University (grant number 2018QH1008), Fujian Medical University's Research Foundation for Talented Scholars (grant number XRCZX2018011) and the 2019 Provincial Health Research Talent Training Program-Youth Research Project (grant number 2019-1-59).
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: This study was approved by the ethics committees of Fujian Medical University (FJMU2019025).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Huang Y, Wang Y, Wang H, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry 2019;6:211–24. 10.1016/S2215-0366(18)30511-X [DOI] [PubMed] [Google Scholar]
- 2.Rehm J, Shield KD. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep 2019;21:10. 10.1007/s11920-019-0997-0 [DOI] [PubMed] [Google Scholar]
- 3.Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the global burden of disease study 2010. Lancet 2013;382:1575–86. 10.1016/S0140-6736(13)61611-6 [DOI] [PubMed] [Google Scholar]
- 4.Rantonen O, Alexanderson K, Pentti J, et al. Trends in work disability with mental diagnoses among social workers in Finland and Sweden in 2005-2012. Epidemiol Psychiatr Sci 2017;26:644–54. 10.1017/S2045796016000597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scott KM, Lim C, Al-Hamzawi A, et al. Association of mental disorders with subsequent chronic physical conditions: world mental health surveys from 17 countries. JAMA Psychiatry 2016;73:150–8. 10.1001/jamapsychiatry.2015.2688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Milner A, Aitken Z, Kavanagh A, et al. Persistent and contemporaneous effects of job stressors on mental health: a study testing multiple analytic approaches across 13 waves of annually collected cohort data. Occup Environ Med 2016;73:787–93. 10.1136/oemed-2016-103762 [DOI] [PubMed] [Google Scholar]
- 7.Madsen IEH, Nyberg ST, Magnusson Hanson LL, et al. Job strain as a risk factor for clinical depression: systematic review and meta-analysis with additional individual participant data. Psychol Med 2017;47:1342–56. 10.1017/S003329171600355X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Theorell T, Hammarström A, Aronsson G, et al. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health 2015;15:738. 10.1186/s12889-015-1954-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harvey SB, Sellahewa DA, Wang M-J, et al. The role of job strain in understanding midlife common mental disorder: a national birth cohort study. Lancet Psychiatry 2018;5:498–506. 10.1016/S2215-0366(18)30137-8 [DOI] [PubMed] [Google Scholar]
- 10.Theorell T, Hammarström A, Gustafsson PE, et al. Job strain and depressive symptoms in men and women: a prospective study of the working population in Sweden. J Epidemiol Community Health 2014;68:78–82. 10.1136/jech-2012-202294 [DOI] [PubMed] [Google Scholar]
- 11.Stansfeld SA, Shipley MJ, Head J, et al. Repeated job strain and the risk of depression: longitudinal analyses from the Whitehall II study. Am J Public Health 2012;102:2360–6. 10.2105/AJPH.2011.300589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Torquati L, Mielke GI, Brown WJ, et al. Shift work and poor mental health: a meta-analysis of longitudinal studies. Am J Public Health 2019;109:e13–20. 10.2105/AJPH.2019.305278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alterman T, Luckhaupt SE, Dahlhamer JM, et al. Prevalence rates of work organization characteristics among workers in the U.S.: data from the 2010 National health interview survey. Am J Ind Med 2013;56:647–59. 10.1002/ajim.22108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kogevinas M, Espinosa A, Papantoniou K, et al. Prostate cancer risk decreases following cessation of night shift work. Int J Cancer 2019;145:2597–9. 10.1002/ijc.32528 [DOI] [PubMed] [Google Scholar]
- 15.Wright KP, Bogan RK, Wyatt JK. Shift work and the assessment and management of shift work disorder (SWD). Sleep Med Rev 2013;17:41–54. 10.1016/j.smrv.2012.02.002 [DOI] [PubMed] [Google Scholar]
- 16.Lim YC, Hoe VCW, Darus A, et al. Association between night-shift work, sleep quality and metabolic syndrome. Occup Environ Med 2018;75:716–23. 10.1136/oemed-2018-105104 [DOI] [PubMed] [Google Scholar]
- 17.Jaradat Y, Birkeland Nielsen M, Kristensen P, et al. Job satisfaction and mental health of palestinian nurses with shift work: a cross-sectional study. Lancet 2018;391 Suppl 2:S50. 10.1016/S0140-6736(18)30416-1 [DOI] [PubMed] [Google Scholar]
- 18.Behrens T, Rabstein S, Wichert K, et al. Shift work and the incidence of prostate cancer: a 10-year follow-up of a German population-based cohort study. Scand J Work Environ Health 2017;43:560–8. 10.5271/sjweh.3666 [DOI] [PubMed] [Google Scholar]
- 19.Thomas C, Power C. Shift work and risk factors for cardiovascular disease: a study at age 45 years in the 1958 British birth cohort. Eur J Epidemiol 2010;25:305–14. 10.1007/s10654-010-9438-4 [DOI] [PubMed] [Google Scholar]
- 20.Ramin C, Devore EE, Wang W, et al. Night shift work at specific age ranges and chronic disease risk factors. Occup Environ Med 2015;72:100–7. 10.1136/oemed-2014-102292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moreno CRC, Marqueze EC, Sargent C, et al. Working time Society consensus statements: evidence-based effects of shift work on physical and mental health. Ind Health 2019;57:139–57. 10.2486/indhealth.SW-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Qian M. China Railway Yearbook. Beijing, China: China Railway Yearbook Editional Office, 2013. [Google Scholar]
- 23.Zhang X, Chen G, Xu F, et al. Health-Related quality of life and associated factors of frontline Railway workers: a cross-sectional survey in the Ankang area, Shaanxi Province, China. Int J Environ Res Public Health 2016;13:E1192. 10.3390/ijerph13121192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al-Dubai SAR, Ganasegeran K, Elkalmi R, et al. Perceived stress among Malaysian Railway workers. Malays J Med Sci 2016;23:38–43. 10.21315/mjms2016.23.5.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karasek R, Brisson C, Kawakami N, et al. The job content questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol 1998;3:322–55. 10.1037/1076-8998.3.4.322 [DOI] [PubMed] [Google Scholar]
- 26.Li J, Yang W, Liu P, et al. Psychometric evaluation of the Chinese (mainland) version of job content questionnaire: a study in university hospitals. Ind Health 2004;42:260–7. 10.2486/indhealth.42.260 [DOI] [PubMed] [Google Scholar]
- 27.Stansfeld SA, Clark C, Caldwell T, et al. Psychosocial work characteristics and anxiety and depressive disorders in midlife: the effects of prior psychological distress. Occup Environ Med 2008;65:634–42. 10.1136/oem.2007.036640 [DOI] [PubMed] [Google Scholar]
- 28.Derogatis LR. The SCL-90 manual I: scoring, administration and procedures for the SCL-90. Baltimore (MD): Clinical Psychometric Research, 1977. [Google Scholar]
- 29.Liao J, Ma X, Gao B, et al. Psychological status of nursing survivors in China and its associated factors: 6 years after the 2008 Sichuan earthquake. Neuropsychiatr Dis Treat 2019;15:2301–11. 10.2147/NDT.S203909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen S, Li L. Re-Testing reliability, validity, and norm applicatility of SCL-90. Chin J Nerv Ment Dis 2003;29:323–7. [Google Scholar]
- 31.Lamers F, Vogelzangs N, Merikangas KR, et al. Evidence for a differential role of HPA-axis function, inflammation and metabolic syndrome in melancholic versus atypical depression. Mol Psychiatry 2013;18:692–9. 10.1038/mp.2012.144 [DOI] [PubMed] [Google Scholar]
- 32.Wickwire EM, Geiger-Brown J, Scharf SM, et al. Shift work and shift work sleep disorder: clinical and organizational perspectives. Chest 2017;151:1156–72. 10.1016/j.chest.2016.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Angerer P, Schmook R, Elfantel I, et al. Night work and the risk of depression. Dtsch Arztebl Int 2017;114:404–11. 10.3238/arztebl.2017.0404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Muecke S. Effects of rotating night shifts: literature review. J Adv Nurs 2005;50:433–9. 10.1111/j.1365-2648.2005.03409.x [DOI] [PubMed] [Google Scholar]
- 35.Chen J, Li J, Cao B, et al. Mediating effects of self-efficacy, coping, burnout, and social support between job stress and mental health among young Chinese nurses. J Adv Nurs 2020;76:163–73. 10.1111/jan.14208 [DOI] [PubMed] [Google Scholar]
- 36.Fan JK, Mustard C, Smith PM. Psychosocial work conditions and mental health: examining differences across mental illness and well-being outcomes. Ann Work Expo Health 2019;63:546–59. 10.1093/annweh/wxz028 [DOI] [PubMed] [Google Scholar]
- 37.Madsen IEH, Nyberg ST, Magnusson Hanson LL, et al. Job strain as a risk factor for clinical depression: systematic review and meta-analysis with additional individual participant data. Psychol Med 2017;47:1342–56. 10.1017/S003329171600355X [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.