Abstract
OBJECTIVES
This study sought to: 1) Assess the prevalence of diabetes complications and comorbidities screening as recommended by the American Diabetes Association (ADA) for youth and young adults (YYAs) with type 1 diabetes (T1D), 2) Examine the association of previously measured metabolic status related to diabetes complications with receipt of recommended clinical screening, and 3) Examine the association of satisfaction with diabetes care with receipt of recommended clinical screening.
METHODS
The study included 2,172 SEARCH for Diabetes in Youth participants with T1D (>10 years old, diabetes duration >5 years). Mean participant age was 17.7 ± 4.3 years with a diabetes duration of 8.1 ± 1.9 years. Linear and multinomial regression models were used to evaluate associations.
RESULTS
Sixty percent of participants reported having 3 or more HbA1c measurements in the past year. In terms of diabetes complications screening, 93% reported having blood pressure measured, 81% having an eye examination, 71% having lipid levels checked, 64% having a foot exam, and 63% completing albuminuria screening in accordance with ADA recommendations. Youth known to have worse glycemic control in the past had higher odds of not meeting HbA1c screening criteria (OR 1.11, 95% CI = 1.05, 1.17); however, after adjusting for race/ethnicity, this was no longer statistically significant. Greater satisfaction with diabetes care was associated with increased odds of meeting screening criteria for most of the ADA-recommended measures.
CONCLUSIONS
Efforts should be made to improve diabetes complications screening efforts for YYAs with T1D, particularly for those at higher risk for diabetes complications.
Keywords: Type 1 diabetes mellitus, Quality of care, Patient satisfaction, Diabetes complications, Youth, Young Adult
INTRODUCTION
Management of diabetes has been a prominent focus of measurement and quality improvement initiatives since the start of the 21st century, including for youth and young adults with diabetes.1,2 The American Diabetes Association (ADA), for example, has been publishing a single resource on current standards of care pertaining specifically to children and adolescents with type 1 diabetes since 2005.3 With the introduction of the Triple Aim, the Institute for Healthcare Improvement’s framework for optimizing health system performance, efforts to improve the patient experience and quality of care have expanded to include patient satisfaction.4 Evidence, however, suggests that the quality and satisfaction with ambulatory care for youth with diabetes is suboptimal.5,6 Further, less than a quarter of youth and young adults meet recommended targets for glycemic control,7,8 placing them at risk for diabetes complications and comorbidities.
Youth with pediatric-onset diabetes compared to adult-onset face a greater risk for complications secondary to having a longer duration of disease. Complications associated with diabetes are a major contributor to the burden of the disease and it is estimated that up to 45% of the diabetes-attributed medical expenditures in the United States (U.S.) are spent treating complications of diabetes.9 Appropriate diabetes-related complications screening has been shown to decrease the risk for progression of microvascular complications and reduce hospitalizations for diabetes-related complications.10
The recent finding from the SEARCH for Diabetes in Youth study (SEARCH) that approximately one-third of teenagers and young adults diagnosed with type 1 diabetes prior to age 20 years have at least one diabetes-related complication11 underscores the importance of screening for complications and comorbidities in the ambulatory care setting, particularly for those already identified to be at higher risk for complications based on previous metabolic status evaluations. The goal of this study was to assess the prevalence of self-reported receipt of complications and comorbidities screening as recommended by the ADA including frequency of HbA1c, lipid, blood pressure and urinary albumin measurements and frequency of retinal and foot examinations. Second, the association of previously measured metabolic status related to diabetes complications, obtained on a prior SEARCH research study visit, with receipt of clinical screening was determined. Finally, we aimed to examine the association of satisfaction with diabetes care with receipt of clinical screening per ADA guidelines.
METHODS
SEARCH for Diabetes in Youth Study Procedures
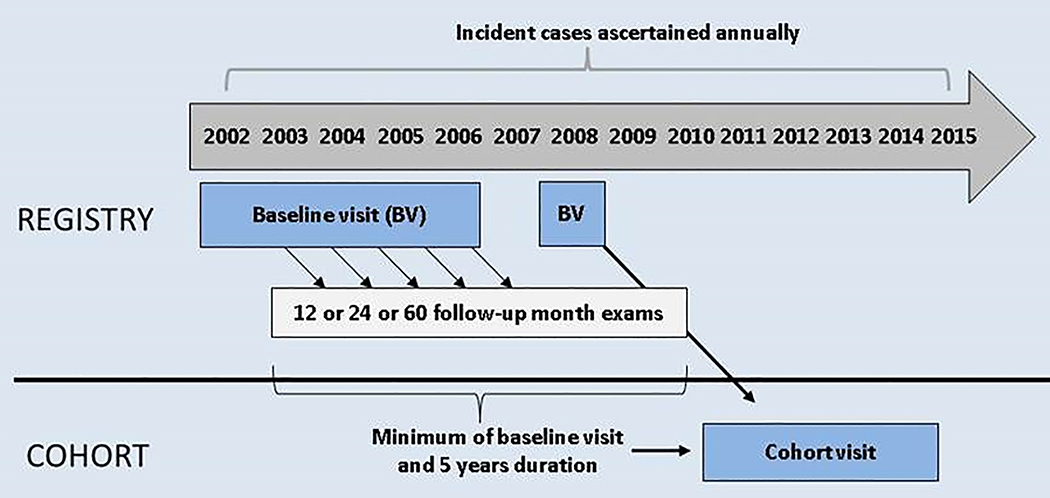
SEARCH is a population-based incidence registry network that includes 5 centers located in California, Colorado, Ohio, South Carolina, and Washington.12 Children and adolescents with diabetes diagnosed before 20 years of age were identified from ongoing surveillance of networks.12 In the first two phases of SEARCH (SEARCH 1 and 2), individuals newly diagnosed with diabetes in 2002–2006 and 2008 were contacted and recruited for a baseline research visit. Incident cases from 2002–2005 were also asked to return for visits at 12, 24, and 60 months after their baseline visit to measure risk factors for diabetes complications (Figure 1).
Figure 1:
Design of the SEARCH for Diabetes in Youth cohort study.
The SEARCH 3 cohort study visit was designed to recruit a subset of SEARCH participants with a duration of diabetes greater than 5 years for an outcome visit between 2011 and 2015, for whom a single assessment of diabetes-related complications was completed. Research visits included questionnaire administration, along with collection of physical measurements and a blood sample. For blood pressure measurement, the mean of 3 systolic and diastolic blood pressure levels was obtained with an aneroid manometer after at least 5 minutes of rest. Blood draws and urine samples occurred after an 8-hour overnight fast and levels of HbA1c, lipids, and urine albumin and creatinine were measured. Diabetic retinopathy was determined by grading 45° color digital fundus images centered on the disc and macula of both eyes, taken with a nonmydriatic camera (Visucam Pro N; Carl Zeiss Meditech).13 The Wisconsin Ocular Epidemiology Reading Center graded photos masked to all clinical characteristics. Finally, peripheral neuropathy was assessed with the Michigan Neuropathy Screening Instrument (MNSI) examination.14,15
Based on the results of the clinical and laboratory measures, participants were classified as having dyslipidemia if they were on a lipid medication and/or had a fasting non-HDL >130 mg/dL, HDL <35 mg/dL, or triglycerides >150 mg/dL. For participants <18 years of age, hypertension was defined as being on an antihypertensive medication and/or a blood pressure measurement ≥95th percentile for age, gender, and height, while those older than 18 were classified as hypertensive if they were on an antihypertensive and/or had a systolic blood pressure of >140 mmHg. Diabetic kidney disease was defined as the presence of albuminuria (≥30 μg/mg of creatinine) on spot urine samples as first morning void samples were only available for SEARCH 3 visits. Diabetic retinopathy was defined as the presence of mild, moderate, or proliferative retinal changes in either eye. Finally, peripheral neuropathy was defined as a score greater than 2 on the MNSI. Of note, data on retinopathy and peripheral neuropathy were not collected in the first two phases of SEARCH.
Quality-of-Care Measures
SEARCH 3 participants completed the SEARCH quality-of-care survey at the cohort study visit. Given that electronic health record data was not available to the study team to capture information related to screening for complications and comorbidities, the SEARCH quality-of-care survey was designed by the study team to solicit information about conformity with ADA-recommended standards of diabetes care, access to care, self-care practices, and satisfaction with care.
The SEARCH quality-of-care survey was completed by the participants themselves if s/he was 18 years or older at the time of survey administration. If the participant was younger than 18 years of age, then the survey was completed by the participant’s parent or guardian. All survey responses were in pre-designated categories and were available in English and Spanish.
For the SEARCH quality-of-care survey responses, receipt of clinical screening responses designated as “meets criteria” were as follows: 1) HbA1c level measurement – “3 or more times” in the past year; 2) Lipid levels measurement – For age 10–17 any response better than “Never”; for age 18+ “In the past year”; 3) Blood pressure measurement – “Every visit” or “most visits” in the past year; 4) Albuminuria measurement – “In the past year;” 5) Eye examination – “In the past year” or “More than a year but less than 2 years;” 6) Foot examination – “In the past year.” Participants were also given the option to select “Do not know/not sure” with each of the quality-of-care questions. Satisfaction with diabetes care was assessed using participant’s response on how s/he would rate overall diabetes care received (response choices: excellent, good, fair, poor).
Study Population
SEARCH participants with type 1 diabetes who were at least 10 years of age at the time of the SEARCH 3 cohort study visit when they completed the SEARCH quality-of-care survey and had physical or laboratory measurements related to diabetes control and complications at the SEARCH 3 cohort study visit and a prior SEARCH study visit, were selected for inclusion in this study (Table 1). If participants had more than one visit prior to the SEARCH 3 cohort study visit, the visit most recent in time to the cohort study visit was included in the analysis. The institutional review boards for all sites approved the study protocol. For all participants, the parent, adolescent or young adult, or both provided consent or assent.
TABLE 1.
Sociodemographic, Clinical Characteristics, and Satisfaction With Care of SEARCH participants with T1D who completed the Quality-of-Care Survey.
| N | 2172 |
| Age, mean ± SD, y | 17.7 ± 4.3 |
| 10–17, n (%) | 1157 (53) |
| 18+, n (%) | 1015 (47) |
| Diabetes duration, mean ± SD, y | 8.1 ± 1.9 |
| Female gender, n (%) | 1098 (51) |
| Race/ethnicity1, n (%) | |
| Non-Hispanic White | 1633 (75) |
| Non-Hispanic Black | 229 (11) |
| Hispanic | 258 (12) |
| Other race/ethnicity | 51 (2) |
| Health Insurance2, n (%) | |
| Private | 1524 (71) |
| Medicaid/Medicare | 458 (21) |
| Other/None | 179 (8) |
| Highest Parental Education3, n % | |
| High school or less | 339 (16) |
| Some college/Associate degree | 693 (32) |
| College graduate or higher | 1105 (52) |
| Household Income4, n (%) | |
| >$75,000 | 791 (37) |
| $50,000–$74,999 | 334 (15) |
| $25,000–$49,999 | 351 (16) |
| <$25,000 | 332 (15) |
| Do not know/refuse to answer | 357 (16) |
| Diabetes care provider5, n (%) | |
| Pediatric endocrinologist | 1228 (57) |
| Adult endocrinologist | 414 (19) |
| Other provider | 462 (21) |
| None/Not sure | 46 (2) |
| Satisfaction with diabetes care6 | |
| Excellent | 525 (25) |
| Good | 1002 (48) |
| Fair | 485 (23) |
| Poor | 94 (4) |
N=2171
N=2161
N=2137
N=2171
N=2165
N=2150
N=2106
Statistical Analyses
Descriptive information is presented as mean ± SD for continuous, or count (%) for categorical variables. After summarizing the distribution of patient characteristics, we examined the percent meeting ADA screening criteria for HbA1c, lipids, blood pressure, albuminuria, eye exams and foot exams overall and stratified by race/ethnicity. Meeting screening criteria was defined as a 3-level outcome variable: “Meets criteria”, “Does not meet criteria”, “Do not know/Not sure.”
In order to examine the relationship between measurements related to diabetes control and complications at the visit prior to the cohort study visit and meeting ADA-recommended screening criteria at the cohort study visit, we fit a series of multinomial logistic regression models. First, we examined diabetes control and complications as predictors of meeting ADA-recommended screening criteria without adjustment for any covariates (Model 0). Next, we adjusted for age, gender, and duration of diabetes (Model 1) with the additional adjustment of HbA1c at the prior visit in Model 2. After adjusting for potential confounding by demographic and clinical measures, we adjusted for race/ethnicity to examine whether racial and ethnic disparities might explain some of the variation in receipt of screening (Model 3). Finally, we included potential sociodemographic and diabetes care related confounders that are correlated with race/ethnicity, specifically insurance, income, parent education, diabetes care provider, and clinical site (Model 4). Model 5 adjusted for covariates in Model 4 plus past HbA1c. Of note, for the outcome of meeting HbA1c screening criteria, Models 2 and 5 were omitted because past HbA1c is the covariate of interest and is already in the model. Models were also not fit for meeting screening criteria for foot and eye exams because corresponding measures of diabetes complications related to peripheral neuropathy and retinopathy were not available at a prior visit.
This same sequential series of models was fit to examine cross-sectional associations between measurements related to diabetes control and complications (from the SEARCH 3 cohort study visit) and meeting screening criteria at the same visit. In this series of models, meeting screening criteria was the predictor variable and the corresponding measurements related to diabetes control and complications are the outcome. Logistic regression models were fit for binary measurements related to diabetes complications and linear regression for the continuous HbA1c measurement. All models in this series additionally adjusted for the corresponding past physical or laboratory measurements (e.g. models predicting hypertension at the SEARCH 3 cohort study visit additionally adjusted for hypertension at the most recent SEARCH visit preceding the SEARCH 3 cohort study visit). Peripheral neuropathy and retinopathy were not available at past visits and so were not included in their associated models.
Associations between satisfaction with care and the 3-level screening criteria at the SEARCH 3 cohort study visit were examined using multinomial logistic regression models adjusted for age, gender, duration of diabetes, race/ethnicity, health insurance, parent education and household income, diabetes care provider, and study site. For all analyses, models were fit separately for each screening criteria. All statistical analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
Of the 2,172 participants included in the analysis (mean participant age 17.7 years with a mean type 1 diabetes duration of 8.1 years; Table 1), 60% reported having 3 or more HbA1c measurements in the past year (Table 2). In terms of diabetes complications screening, 93% reported having blood pressure measured, 71% having lipid levels checked, and 81% having an eye examination in accordance with ADA recommendations. Fewer participants reported meeting screening criteria for foot examinations (64%) and having their urine tested for protein (63%).
TABLE 2.
Percent of SEARCH Participants with T1D Who Reported Receiving ADA-Recommended Standards of Diabetes Care in the Past Year.
| ADA-Recommended Standards of Diabetes Care | Percent Reporting Receipt of Screening (%) | ||
|---|---|---|---|
| Overall | |||
| Meet criteria | Do not meet criteria | Do not know/not sure | |
| HbA1c a | 60.4 | 37.4 | 2.2 |
| Lipid levels b | 71.1 | 9.8 | 19.1 |
| Blood pressure c | 93.4 | 4.4 | 2.2 |
| Albuminuria d | 63.3 | 18.8 | 17.9 |
| Eye exam e | 81.2 | 15.7 | 3.1 |
| Foot exam f | 64.3 | 25.6 | 10.1 |
Quality of care survey responses designated as “meets criteria”:
HbA1c level measurement – “3 or more times” in the past year
Lipid levels measurement – For age 10–17 any response better than “Never”; for age 18+ “In the past year”
Blood pressure measurement – “Every visit” or “most visits” in the past year
Albuminuria measurement – “In the past year”
Eye examination – “In the past year” or “More than a year but less than 2 years”
Foot examination – “In the past year”
When examining the impact of a participant’s prior metabolic status on meeting ADA-recommended screening criteria for HbA1c measurements, YYAs with worse glycemic control at their previous SEARCH study visit had higher odds of not meeting screening criteria (OR 1.11, 95% CI = 1.05, 1.17; Table 3) and not knowing or being unsure (OR 1.24, 95% CI= 1.08, 1.43; Table 3). However, after adjusting for race/ethnicity, these associations were attenuated and no longer statistically significant (OR 1.05, 95% CI = 0.99, 1.11 and OR=1.10, 95% CI=0.95, 1.28, respectively) and they were further attenuated with the addition of socioeconomic factors (OR 1.04, 95% CI 0.98, 1.10 and OR 1.03, 95% CI 0.87, 1.22). In the unadjusted analysis, YYAs with elevated blood pressure at their prior SEARCH visit had increased odds of not meeting screening criteria relative to those without hypertension (OR 2.24, 95% CI = 1.13, 4.45). After adjusting for age, gender and duration of diabetes, however, this association was no longer statistically significant. There was no significant association with prior albuminuria or dyslipidemia with meeting screening criteria. Past measures were not available for peripheral neuropathy and retinopathy.
TABLE 3.
Odds ratios from separate multinomial logistic regression models with past measurements related to diabetes control and complications* as covariate of interest and current screening criteria categories as 3-level outcome (“Meets Criteria” as reference for each measure).
| Covariate of interest (model adjustments) | Does not Meet Criteria vs. Meets Criteria | DK/Not Sure vs. Meets Criteria | |
|---|---|---|---|
| OR (95% CI) p-value |
OR (95% CI) p-value |
||
| Past HbA1c (1-unit increase) | |||
| Model 0: no additional covariates [N=1973] | 1.11 (1.05, 1.17) | 1.24 (1.08, 1.43) | |
| Model 1: adjusted for age, gender, & duration [N=1973] | 1.06 (1.01, 1.13) | 1.17 (1.01, 1.36) | |
| Model 3: Model 1 + race/ethnicity [N=1972] | 1.05 (0.99, 1.11) | 1.10 (0.95, 1.28) | |
| Model 4: Model 3 + insurance, income, parent education, DM care provider, & clinical site [N=1910] | 1.04 (0.98, 1.10) | 1.03 (0.87, 1.22) | |
|
Note - Models 2 and 5 (which add past HbA1c) not included because HbA1c is already in the model | |||
| Past HTN (Yes vs. No) | |||
| Model 0: no additional covariates [N=2032] | 2.24 (1.13, 4.45) | ---‡ | ---‡ |
| Model 1: adjusted for age, gender, & duration [N=2032]^ | 1.93 (0.96, 3.87) | ---‡ | ---‡ |
| Model 2: Model 1 + Past HbA1c [N=1872] ^ | 1.33 (0.59, 3.00) | ---‡ | ---‡ |
| Model 3: Model 1 + race/ethnicity [N= 2031] | 1.84 (0.91, 3.71) | ---‡ | ---‡ |
| Model 4: Model 3 + insurance, income, parent education, DM care provider, & clinical site [N=1972] | 1.67 (0.81, 3.47) | ---‡ | ---‡ |
| Model 5: Model 4 + Past HbA1c [N= 1818] | 1.13 (0.48, 2.63) | ---‡ | ---‡ |
| Past Albumin-to-Creatinine Ratio (ACR) (≥30 vs. <30) | |||
| Model 0: no additional covariates [N=1750] | 1.03 (0.69, 1.55) | 0.76 (0.48, 1.20) | |
| Model 1: adjusted for age, gender, & duration [N=1750] | 1.05 (0.70, 1.58) | 0.75 (0.47, 1.20) | |
| Model 2: Model 1 + Past HbA1c [N=1704] | 0.98 (0.65, 1.49) | 0.72 (0.45, 1.16) | |
| Model 3: Model 1 + race/ethnicity [N= 1749] | 1.05 (0.70, 1.58) | 0.75 (0.47, 1.20) | |
| Model 4: Model 3 + insurance, income, parent education, DM care provider, & clinical site [N=1692] | 1.07 (0.70, 1.65) | 0.70 (0.43, 1.15) | |
| Model 5: Model 4 + Past HbA1c [N= 1648] | 1.02 (0.65, 1.58) | 0.67 (0.40, 1.11) | |
| Past Dyslipidemia (Yes vs. No) | |||
| Model 0: no additional covariates [N=1793] | 1.16 (0.81, 1.65) | 0.82 (0.61, 1.11) | |
| Model 1: adjusted for age, gender, & duration [N=1793] | 0.89 (0.61, 1.29) | 0.84 (0.62, 1.14) | |
| Model 2: Model 1 + Past HbA1c [N=1787] | 0.84 (0.58, 1.24) | 0.73 (0.54, 1.00) | |
| Model 3: Model 1 + race/ethnicity [N= 1792] | 0.89 (0.61, 1.29) | 0.84 (0.62, 1.13) | |
| Model 4: Model 3 + insurance, income, parent education, DM care provider, & clinical site [N=1740] | 0.88 (0.60, 1.30) | 0.81 (0.59, 1.12) | |
| Model 5: Model 4 + Past HbA1c [N= 1734] | 0.87 (0.59, 1.29) | 0.75 (0.54, 1.03) | |
Past measure not available for Peripheral Neuropathy or Retinopathy
Estimates not available due to empty cell in 3×2 table (HTN=Y, Screening=DK) – DK excluded, logistic model shown for “Does not Meet Criteria” vs. “Meets Criteria” (DK/Not Sure excluded)
Hosmer and Lemeshow Goodness-of-Fit test p<0.05
In the linear regression model examining whether meeting HbA1c screening criteria is associated cross-sectionally with glycemic control after adjusting for covariates, participants who did not meet, or were unsure about meeting ADA screening criteria for HbA1c had higher current HbA1c than those meeting criteria (p < 0.01). Specifically, HbA1c was 0.28% higher among participants not meeting screening criteria and 0.81% higher among those unsure about meeting screening criteria compared to participants meeting screening criteria (Supplemental Table). The logistic regression models did not demonstrate statistically significant associations between the presence of hypertension, albuminuria, and peripheral neuropathy with meeting screening criteria.
Greater satisfaction with diabetes care was associated with increased odds of meeting screening criteria for most of the ADA-recommended measures (Table 4). For HbA1c measurements, a 1-step increase in satisfaction showed, averaged over all levels of satisfaction, an odds ratio of 1.39 (95% CI = 1.23, 1.58) of meeting screening criteria. Similarly, greater satisfaction was associated with SEARCH participants meeting screening criteria for blood pressure measurements (OR 1.32, 95% CI = 1.01, 1.72), dyslipidemia screening (OR 1.27, 95% CI = 1.04, 1.55), retinopathy evaluations (OR 1.22, 95% CI = 1.04, 1.44), and foot examinations (OR 1.26, 95% CI = 1.10, 1.45).
TABLE 4. Odds ratios from separate multinomial regression models with satisfaction with diabetes care as covariate of interest and current screening criteria as 3-level outcome (“Meets Criteria” as reference).*.
Estimates in table are odds ratios (95% CI) for 1-step increase in satisfaction.
| ADA-Recommended Standards of Diabetes Care | Meets Criteria vs. Does Not Meets Criteria | Meets Criteria vs. Do Not Know/Not Sure |
|---|---|---|
| OR* (95% CI) | OR* (95% CI) | |
| HbA1c | 1.39 (1.23, 1.58) | 1.29 (0.86, 1.94) |
| Blood pressure | 1.32 (1.01, 1.72) | 1.44 (0.97, 2.14) |
| Albuminuria | 1.14 (0.98, 1.33) | 1.14 (0.97, 1.33) |
| Lipid levels | 1.27 (1.04, 1.55) | 1.30 (1.11, 1.51) |
| Eye examination | 1.22 (1.04, 1.44) | 1.15 (0.82, 1.63) |
| Foot examination | 1.26 (1.10, 1.45) | 1.34 (1.09, 1.63) |
Models adjust for age, gender, duration of diabetes, race/ethnicity, insurance, parent education and income, diabetes care provider, and clinical site.
DISCUSSION
Data from this large multicenter study further confirm that many youth and young adults with type 1 diabetes in the U.S. are not receiving ADA-recommended clinical screening, thereby increasing the likelihood that risk factors for diabetes complications remain unrecognized and reducing the opportunities for early intervention to prevent progression of complications. The findings that only 60% of YYAs report meeting criteria for HbA1c screening and that participants with higher past HbA1c levels had decreased odds of meeting screening criteria or not knowing/being unsure about meeting screening criteria underscore the need for improving the delivery of care to older teens and young adults, particularly given that poor glycemic control is known to be associated with the development of diabetes complications.16,17 Further, improving satisfaction with care may offer an additional modifiable factor to help YYAs meet recommended standards of care.
Our results demonstrate that YYAs with worse glycemic control are at higher risk of not receiving ADA-recommended care in terms of receipt of clinical tests. Previous studies have highlighted that patients with diabetes who have poor glycemic control more frequently miss clinic appointments, which certainly may increase the likelihood of missed screening for complications screening.18–20 However, the fact that the association between higher HbA1c and not receiving ADA-recommended clinical screening was no longer present in the analyses after adjustment for race/ethnicity, and was further attenuated by socioeconomic factors, suggests that these factors are related to the reasons why many youth and young adults are not receiving recommended screening. Our findings highlight the need for providers and health care systems to consider measuring healthcare disparities in their efforts to provide high-quality care.21 Diabetes providers, for example, should be encouraged to use the National Quality Forum’s National Voluntary Consensus Standards for Ambulatory Care to evaluate the quality of care being provided at an institutional level.22
Recognizing that the evaluation of glycemic control is an integral component of a diabetes clinic visit and most SEARCH sites use point-of-care HbA1c measurements,23 our finding that two-fifths of youth and young adults report not meeting HbA1c screening criteria suggests that poor clinic attendance likely remains a barrier to receiving optimal diabetes care. Infrequent clinic attendance is problematic not only as it interferes with the ability to complete necessary screening of diabetes complications but also results in missed opportunities for receiving diabetes management guidance, additional education, and support.24 Strategies that promote creative and flexible options that work to address disparities related to diabetes care such as telemedicine should be considered.
Since the introduction of the Triple Aim by the Institute for Healthcare Improvement as a framework for optimizing health system performance that included an emphasis to improve the experience of care, patient satisfaction has increasingly been recognized as an important aspect of the quality of medical care.4,25 Previous studies have demonstrated that patient perceptions of quality are remarkably accurate even if the technical details are not as well understood.26,27 Our study highlights that participants who reported higher satisfaction with diabetes care were more likely to have met screening criteria for most of the ADA-recommended measures. This, along with the recent finding that anticipatory guidance around health-promoting opportunities in young adults with diabetes is positively associated with both increased satisfaction with health care and ratings of overall personal health in youth with diabetes, suggests that quality improvement efforts around improving treatment satisfaction could be prioritized to provide care consistent with recommendations.28
Data from our study indicate that quality improvement efforts could help ensure that diabetes care team members are carrying out appropriate tests related to diabetes complications in the clinical setting. Of interest was the number of participants that “did not know” or were “not sure” of their status regarding various clinical tests, suggesting that communication around measures being taken to support complications screening may be suboptimal or ineffective. Efforts to improve shared-decision making and incorporate deliberate dialogue around screening of complications may be helpful and should be encouraged.29 In addition, efforts may need to be directed toward pediatric care providers to enable them to be more comfortable addressing, with parents and adolescents with diabetes, the need for screening for risk of complications.
This study has limitations. First, given that we did not have access to clinical care data from medical records, we relied on self-report to assess the frequency of screening which were then compared with ADA-recommended standards of care. Previous work has demonstrated that there is reasonable concordance between patient report and information in medical records in ambulatory care settings and when assessing comorbid conditions.30–32 Second, social desirability bias could have led to participants over-reporting the frequency of screening;33 however, the need for quality improvement efforts would remain, given the substantial percentage of participants that reported suboptimal screening frequency. Third, given that cohort study visits took place over a 5-year period, some of the physical measurements may not have been reflective of current metabolic status, though all youth and young adults should be receiving clinical screening and appropriate screening based on recommended guidelines regardless of the absence or presence of a comorbidity. Fourth, the lack of data on clinic attendance limited the ability to comment in detail on clinical opportunities for screening. Fifth, our findings may not be generalizable to resource challenged settings. Finally, given the lack of access to electronic health records, we were unable to comment on whether clinical screening had been performed, or ordered but then not completed. We are also unable to quantify communication between visits as a modifier of access or satisfaction with care.
The quality of ambulatory diabetes care for individuals with type 1 diabetes is important relative to their overall health.34 With the rising incidence of type 1 diabetes among youth in the U.S.,35 more children and adolescents are at risk for the development of diabetes-related complications. Evidence-based clinical guidelines are useful tools to promote effective and efficient care.36 Our study highlights the challenges in achieving ADA-recommended standards of care in YYAs with diabetes in terms of diabetes complications screening. In addition, continued work to engage adolescents and young adults may help to facilitate regular medical care. Given the large economic burden of diabetes complications on the individual, society and the health care system, efforts to further improve the quality of diabetes care in YYAs are warranted.
Supplementary Material
ACKNOLWEDGEMENTS
The SEARCH for Diabetes in Youth Study is indebted to the many youth and their families, and their health care providers, whose participation made this study possible.
SEARCH 3/4: The authors wish to acknowledge the involvement of the Kaiser Permanente Southern California’s Clinical Research Center (funded by Kaiser Foundation Health Plan and supported in part by the Southern California Permanente Medical Group; the South Carolina Clinical & Translational Research Institute, at the Medical University of South Carolina, NIH/National Center for Advancing Translational Sciences (NCATS) grant number UL1 TR000062, UL1 TR001450; Seattle Children’s Hospital and the University of Washington, NIH/NCATS grant number UL1 TR00423; University of Colorado Pediatric Clinical and Translational Research Center, NIH/NCATS grant Number UL1 TR000154; the Barbara Davis Center at the University of Colorado at Denver (DERC NIH grant number P30 DK57516); the University of Cincinnati, NIH/NCATS grant number UL1 TR000077, UL1 TR001425; and the Children with Medical Handicaps program managed by the Ohio Department of Health. This study includes data provided by the Ohio Department of Health, which should not be considered an endorsement of this study or its conclusions.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the National Institute of Diabetes and Digestive and Kidney Diseases.
Funding:
Grant Support (SEARCH 3):
SEARCH for Diabetes in Youth is funded by the Centers for Disease Control and Prevention (PA numbers 00097, DP-05-069, and DP-10-001) and supported by the National Institute of Diabetes and Digestive and Kidney Diseases.
Grant Support (SEARCH 4):
The SEARCH for Diabetes in Youth Cohort Study (1UC4DK108173) is funded by the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases and supported by the Centers for Disease Control and Prevention.
The Population Based Registry of Diabetes in Youth Study (1U18DP006131, U18DP006133, U18DP006134, U18DP006136, U18DP006138, U18DP006139) is funded by the Centers for Disease Control and Prevention and supported by the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.
Sites (SEARCH 3/4):
Kaiser Permanente Southern California (U18DP006133, U48/CCU919219, U01 DP000246, and U18DP002714), University of Colorado Denver (U18DP006139, U48/CCU819241-3, U01 DP000247, and U18DP000247-06A1), Cincinnati’s Children’s Hospital Medical Center (U18DP006134, U48/CCU519239, U01 DP000248, and 1U18DP002709), University of North Carolina at Chapel Hill (U18DP006138, U48/CCU419249, U01 DP000254, and U18DP002708), Seattle Children’s Hospital (U18DP006136, U58/CCU019235-4, U01 DP000244, and U18DP002710-01), Wake Forest University School of Medicine (U18DP006131, U48/CCU919219, U01 DP000250, and 200-2010-35171).
REFERENCES
- 1.American Diabetes Association. Standards of Medical Care in Diabetes - 2018. Diabetes Care. 2018. [Google Scholar]
- 2.O’Connor PJ, Bodkin NL, Fradkin J, et al. Diabetes performance measures: current status and future directions. Diabetes Care. 2011;34(7):1651–1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Silverstein J, Klingensmith G, Copeland K, et al. Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care. 2005;28(1):186–212. [DOI] [PubMed] [Google Scholar]
- 4.Institute for Healthcare Improvement. The IHI Triple Aim. http://www.ihi.org/Engage/Initiatives/TripleAim/pages/default.aspx.
- 5.Waitzfelder B, Pihoker C, Klingensmith G, et al. Adherence to guidelines for youths with diabetes mellitus. Pediatrics. 2011;128(3):531–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wood JR, Miller KM, Maahs DM, et al. Most youth with type 1 diabetes in the T1D Exchange Clinic Registry do not meet American Diabetes Association or International Society for Pediatric and Adolescent Diabetes clinical guidelines. Diabetes Care. 2013;36(7):2035–2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miller KM, Foster NC, Beck RW, et al. Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D Exchange clinic registry. Diabetes Care. 2015;38(6):971–978. [DOI] [PubMed] [Google Scholar]
- 8.Pettitt DJ, Talton J, Dabelea D, et al. Prevalence of diabetes in U.S. youth in 2009: the SEARCH for diabetes in youth study. Diabetes Care. 2014;37(2):402–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Diabetes A. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36(4):1033–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Petrosyan Y, Bai YQ, Kone Pefoyo AJ, et al. The Relationship between Diabetes Care Quality and Diabetes-Related Hospitalizations and the Modifying Role of Comorbidity. Can J Diabetes. 2017;41(1):17–25. [DOI] [PubMed] [Google Scholar]
- 11.Dabelea D, Stafford JM, Mayer-Davis EJ, et al. Association of Type 1 Diabetes vs Type 2 Diabetes Diagnosed During Childhood and Adolescence With Complications During Teenage Years and Young Adulthood. JAMA. 2017;317(8):825–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamman RF, Bell RA, Dabelea D, et al. The SEARCH for Diabetes in Youth study: rationale, findings, and future directions. Diabetes Care. 2014;37(12):3336–3344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klein R, Klein BE, Magli YL, et al. An alternative method of grading diabetic retinopathy. Ophthalmology. 1986;93(9):1183–1187. [DOI] [PubMed] [Google Scholar]
- 14.Herman WH, Pop-Busui R, Braffett BH, et al. Use of the Michigan Neuropathy Screening Instrument as a measure of distal symmetrical peripheral neuropathy in Type 1 diabetes: results from the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications. Diabet Med. 2012;29(7):937–944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jaiswal M, Lauer A, Martin CL, et al. Peripheral neuropathy in adolescents and young adults with type 1 and type 2 diabetes from the SEARCH for Diabetes in Youth follow-up cohort: a pilot study. Diabetes Care. 2013;36(12):3903–3908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diabetes Control and Complications Trial Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–986. [DOI] [PubMed] [Google Scholar]
- 17.Diabetes Control and Complications Trial Group. Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial. J Pediatr. 1994;125(2):177–188. [DOI] [PubMed] [Google Scholar]
- 18.Karter AJ, Parker MM, Moffet HH, et al. Missed appointments and poor glycemic control: an opportunity to identify high-risk diabetic patients. Med Care. 2004;42(2):110–115. [DOI] [PubMed] [Google Scholar]
- 19.Fortin K, Pries E, Kwon S. Missed Medical Appointments and Disease Control in Children With Type 1 Diabetes. J Pediatr Health Care. 2016;30(4):381–389. [DOI] [PubMed] [Google Scholar]
- 20.Schectman JM, Schorling JB, Voss JD. Appointment adherence and disparities in outcomes among patients with diabetes. J Gen Intern Med. 2008;23(10):1685–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Diabetes Association. Promoting Health and Reducing Disparities in Populations. Diabetes Care. 2017;40(Suppl 1):S6–S10. [DOI] [PubMed] [Google Scholar]
- 22.National Quality Forum. National voluntary consensus standards for ambulatory care—measuring healthcare disparities. 2008.
- 23.Pihoker C, Forsander G, Fantahun B, et al. ISPAD Clinical Practice Consensus Guidelines 2018: The delivery of ambulatory diabetes care to children and adolescents with diabetes. Pediatr Diabetes. 2018;19 Suppl 27:84–104. [DOI] [PubMed] [Google Scholar]
- 24.International Society for Pediatric and Adolescent Diabetes. Global IDF/ISPAD Guideline for Diabetes in Childhood and Adolescence [Internet]. 2011:pp. 1–132. Available from: http://www.ispad.org/NewsFiles/IDF-ISPAD_Diabetes_in_Childhood_and%120Adolescence_Guidelines_2011.pdf
- 25.Cleary PD, McNeil BJ. Patient satisfaction as an indicator of quality care. Inquiry. 1988;25(1):25–36. [PubMed] [Google Scholar]
- 26.Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41–48. [PubMed] [Google Scholar]
- 28.Corathers SD, Kichler JC, Fino NF, et al. High health satisfaction among emerging adults with diabetes: Factors predicting resilience. Health Psychol. 2017;36(3):206–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tamhane S, Rodriguez-Gutierrez R, Hargraves I, Montori VM. Shared Decision-Making in Diabetes Care. Curr Diab Rep. 2015;15(12):112. [DOI] [PubMed] [Google Scholar]
- 30.Lovaas KF, Cooper JG, Sandberg S, Roraas T, Thue G. Feasibility of using self-reported patient data in a national diabetes register. Bmc Health Serv Res. 2015;15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tisnado DM, Adams JL, Liu H, et al. What is the concordance between the medical record and patient self-report as data sources for ambulatory care? Med Care. 2006;44(2):132–140. [DOI] [PubMed] [Google Scholar]
- 32.Ye F, Moon DH, Carpenter WR, et al. Comparison of Patient Report and Medical Records of Comorbidities: Results From a Population-Based Cohort of Patients With Prostate Cancer. JAMA Oncol. 2017;3(8):1035–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Warnecke RB, Johnson TP, Chavez N, et al. Improving question wording in surveys of culturally diverse populations. Ann Epidemiol. 1997;7(5):334–342. [DOI] [PubMed] [Google Scholar]
- 34.Tricco AC, Ivers NM, Grimshaw JM, et al. Effectiveness of quality improvement strategies on the management of diabetes: a systematic review and meta-analysis. Lancet. 2012;379(9833):2252–2261. [DOI] [PubMed] [Google Scholar]
- 35.Mayer-Davis EJ, Lawrence JM, Dabelea D, et al. Incidence Trends of Type 1 and Type 2 Diabetes among Youths, 2002–2012. N Engl J Med. 2017;376(15):1419–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Woolf SH, Grol R, Hutchinson A, Eccles M, Grimshaw J. Clinical guidelines: potential benefits, limitations, and harms of clinical guidelines. BMJ. 1999;318(7182):527–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.