Summary
Background
Sociodemographic inequalities in depression are well established. However, less is known about variation in inequalities across countries. In this study, we describe cross-national variation in sociodemographic inequalities in depression among older adults. Comparing inequalities across countries is an important step towards understanding how the social environment shapes depression risk.
Methods
In this cross-sectional study, we harmonised data from eight large ageing cohort studies from 18 countries. We restricted our study to adults aged 55 years and older, and measured depression using established cut points in shortened Center for Epidemiologic Studies Depression or EURO-D scales. Next, we estimated prevalence ratios for each country by age, marital status, educational attainment, and gender with logistic regression. To compare estimates across countries, we standardised estimates to the mean sociodemographic distribution across our sample.
Findings
Between Jan 1, 2007, and May 31, 2015, 93 590 older adults completed questions related to depressive symptoms. Sociodemographic inequalities in depression varied substantially across countries. Variation was most apparent for age: prevalence ratios (adults aged 75 years or older vs adults aged 55–65 years) ranged from 2·66 (95% CI 2·13–3·20) in Israel to 0·78 (95% CI 0·72–0·84) in the USA. Heterogeneity by other factors was also apparent. Gender prevalence ratios (women vs men) ranged from 1·07 (95% CI 1·01–1·14) in Korea to 1·96 (95% CI 1·55–2·36) in Greece. Educational prevalence ratios (less than secondary education vs some post-secondary education) ranged from 1·01 (95% CI 0·88–1·14) in Japan to 2·34 (95% CI 2·14–2·55) in the USA. Marital status prevalence ratios (divorced or separated vs married) ranged from 1·11 (95% CI 1·01–1·21) in Chile to 2·01 (95% CI 1·73–2·29) in England.
Interpretation
Inequalities in depression among older adults vary substantially across countries, which might be due to country-specific aspects of the social environment. Future research should investigate social inequality determinants of mental health that might inform the design and evaluation of social, economic, and mental health-related policies and interventions to reduce depression.
Funding
US National Institute of Mental Health and Chilean National Commission for Scientific and Technological Research.
Introduction
Inequalities in depression are well established. A meta-analysis of 51 population-based studies found that low socioeconomic status (measured broadly as low educational attainment, income, occupational level, social class, or assets) was associated with approximately 1·8 greater odds of depression compared to those in the highest socioeconomic status group,1 and estimates from the Global Burden of Disease Study indicate that worldwide, women have an approximately 1·7 times greater risk of having current major depressive disorder than men (ie, 5·5% of women vs 3·2% of men).2 Additional socioeconomic and demographic indicators, including low educational attainment,3 being separated or divorced,4 and low income,5 are consistently associated with an increased risk of depression. Older adults, who have experienced adverse or beneficial conditions as a consequence of sociodemographic indicators over the life course, might experience especially large inequalities in depression.6 The consequences of depression could also be especially severe in this demographic group. Depression is one of the most common mental health conditions in older adults and is linked with the development of many chronic health conditions and a poorer prognosis upon developing chronic conditions.7 Depression is also a major risk factor for suicide, and older adults have an especially high burden of suicide. In the USA, 38% of all suicide deaths occur among individuals aged 45–64 years and 17% among those aged 65 years or older.9
Although inequalities in depression are well established, much less is known about the heterogeneity in the direction and magnitude of inequalities across countries. The social environment—which encompasses physical surroundings, social relationships, and culture10—shapes the life opportunities of people among various demographic groups and could be a major generator of inequalities. Comparing inequalities across countries is a key way to assess if social environmental factors play a role in depression risk. Although cross-national research into inequalities in depression among older adults is rare, studies that have been done across high-income countries found substantial differences in the magnitude of inequalities by educational attain ment11,12 and gender,11,13,14 and a study3 done in six low-income and middle-income countries (China, Ghana, India, Mexico, Russia, South Africa) found substantial differences in the magnitude of inequalities by wealth. These studies indicate that the magnitude of inequalities differ across countries. However, because studies investigated single demo graphic factors in isolation and were restricted to specific geographical regions (ie, Europe) or a small number of countries, the relative magnitude of inequalities across multiple sociodemographic indicators and a wide variety of countries is unknown.
In this Article, to our knowledge, we provide the most comprehensive assessment to date regarding socio demographic inequalities in depression among older adults. Using harmonised datasets encompassing 93 590 individuals from 18 countries, we estimated inequalities by four primary demographic indicators (gender, marital status, age, educational attainment) and assessed if these inequalities are consistent across countries.
Methods
Study design and participants
Our cross-sectional study used secondary publicly available data from eight longitudinal surveys for 93 590 older adults encompassing 18 countries (in North America, South America, Europe, Asia, and the Middle East), including the Survey of Health, the Ageing and Retirement in Europe (SHARE), the Health and Retirement Survey (HRS), the English Longitudinal Study of Ageing (ELSA), the Japanese Study of Aging and Retirement (JSTAR), the Social Protection Survey (or Encuesta de Previsión Social [EPS]), the China Health and Retirement Survey (CHARLS), and the Korean Longitudinal Study of Aging (KLoSA). We selected these surveys for inclusion in our study because they focused on issues related to health and ageing and included comparable information for a large sample of individuals age 50 and older, including comparable tools to assess depressive symptoms. All surveys were designed to be nationally representative, except for JSTAR, which was only done in ten municipalities. Additional details about the surveys are reported in the appendix (pp 2–4). Most surveys recruited, enrolled, and added newly eligible adults (ie, refreshment samples) to the parent study every few years. Because of timing differences in the enrolment of refreshment samples, and various inclusion criteria across surveys (eg, HRS includes the spouses of participants regardless of age), the age range of participants varied considerably across surveys. We restricted our sample to adults aged 55 years or older because 55 years is the youngest age that primary respondents could have in each of our included surveys for our selected survey year. We used data from the most recent survey year available, which varied by country.
Procedures
Our main outcome was probable depression, which is defined as having a depression symptom score above established cut points. Depressive symptoms were assessed with shortened versions of the Center for Epidemiological Depression scale (CES-D)15 in six surveys and with the EURO-D in 12 surveys.16 The CES-D and EURO-D ask respondents if they experienced negative affect (eg, sadness) and somatic symptoms (eg, trouble sleeping) recently. The CES-D also asks about recent positive affect (eg, happiness). The time frame for the CES-D is the past week, whereas for the EURO-D the time frame is the preceding month. Response options include presence or absence of each symptom. For each item, respondents receive a score of 1 if a negative affect or somatic symptom was present and 0 if the score was absent; positive affect indicators, such as feeling happy, are reversed coded. We constructed a summary score using the 8-item CES-D scale for surveys done in the USA, England, Japan, and Chile; the 10-item CES-D scale for surveys done in China and Korea; and the 12-item EURO-D scale for studies done in Austria, Belgium, France, Germany, Greece, Hungary, Ireland, Israel, and Italy.
These reduced versions of the CES-D and EURO-D have undergone extensive validation among older adults.16–22 Although the CES-D and EURO-D use different time frames (ie, 1 week vs 1 month) and have several different items, validation work indicates that these screening tools have similar classification properties. A study using SHARE data from 13 European countries compared depression classification among 15487 older adults who completed both the 8-item CES-D and the EURO-D in the same survey, and the study found that the CES-D and EURO-D scores highly correlated.23 Given the high degree of validation and adequate psychometric properties for both instruments in classifying probable depression, we used the recommended thresholds derived from validation work among older adults, which includes classifying probable depression among adults who experience 3 or more symptoms for the 8-item CES-D,24 and 4 or more symptoms for the 10-item CES-D19,22 and the EURO-D scale.16 For simplicity, we will refer to people with depressive symptoms above these cut points as having depression, although we acknowledge that these measures are not designed to estimate clinically ascertained depression or depression that meets conventional diagnostic criteria such as DSM-IV or ICD-10.
Sociodemographic indicators were gender, age, educational attainment, and marital status. We examined the distribution of sociodemographic factors in each country, and we constructed sociodemographic categories with a sufficient number of people in each category. The distribution of people within each country, as well as the number of people classified as depressed, is reported in the appendix (p 5). Gender was measured as a dichotomous variable indicating men or women, and age was classified into three groups (55–64, 65–74, and ≥75 years). Educational attainment measured the highest educational degree obtained by the respondent (less than secondary education, completed secondary education, and some post-secondary education). Marital status was measured as a categorical variable including four groups (married or partnered, divorced or separated, widowed, and single adults who were never married).
Statistical analysis
We estimated inequalities in depression prevalence by sociodemographic factors in each country using Stata 16 (StataCorp) in two steps. First, we used a logistic regression model to estimate the odds of depression in each country, and we used the post-estimation command margins in Stata to calculate predicted prevalence. Our model included demographic factors (ie, age, gender, educational attainment, marital status), a fixed effect for country, and interaction terms between the country and each demographic factor (ie, country × age, country × education, country × gender, country × marital status). We included these interaction terms because Wald tests indicated that country-specific effects varied by age (p<0·0001), education (p<0·0001), gender (p<0·0001), and marital status (p<0·0001). We estimated fixed effects in each country because this approach estimates inequalities in depression by sociodemographic factors within each country, thus controlling for potential differences in depression detection due to screening tool or cultural differences in endorsement of depressive symptom items, which can vary considerably among cultures.25 Controlling for country is especially important in studies such as this study, which assessed depression with different tools (ie, 8-item or 10-item CES-D; EURO-D) and was done in diverse settings. This analytic approach has been used in previous research investigating cross-cultural socioeconomic differences in depression.5 Because of the noncomparable way that each survey constructed survey weights, we did not use survey weights.
As a second step, to provide estimates that are comparable across countries and demographic factors, we estimated depression prevalence ratios (PR) among people in each sociodemographic stratum (eg, widowed adults) using the post-estimation command margins in Stata. This estimation command allowed us to standardise depression prevalence to the mean level of the other considered sociodemographic factors across surveys, including age (55–65 years age group=41·9%, 65–74 years age group=33·8%, ≥75 years age group=24·3%), gender (men=45·8%, women=54·2%), educational attainment (less than secondary education=23·8%, secondary education=28·7%, some post-secondary education=47·5%) and marital status (married or partnered=72·5%, divorced or separated=7·6%, widowed=15·6%, single adults who were never married=4·2%). We then used these weighted estimates to calculate depression PR between demographic groups (eg, widowed adults vs married or partnered adults). Methodological papers about the reporting of inequalities recommend reporting results on both the absolute (eg, difference) and relative (eg, ratio) scales;26,27 therefore, in additional analyses, we used the standardised prevalence estimates to calculate prevalence differences (eg, the prevalence of depression among widowed adults minus the prevalence among married or partnered adults).
The described estimation procedure allows a valid comparison of inequalities in depression across countries and sociodemographic factors. Standardisation across countries accounts for country-specific differences in demographic composition, which can be a result of many factors, including varying inclusion criteria of surveys and differences in the demographic composition of individuals within countries. Standardisation across sociodemographic indicators accounts for differential distribution of other factors related to these indicators. For example, widowed individuals tend to be older than married people and age is a risk factor for depression.
Role of funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. RAR, EC, and JTM had full access to all the data in the study. The corresponding author had final responsibility for the decision to submit for publication.
Results
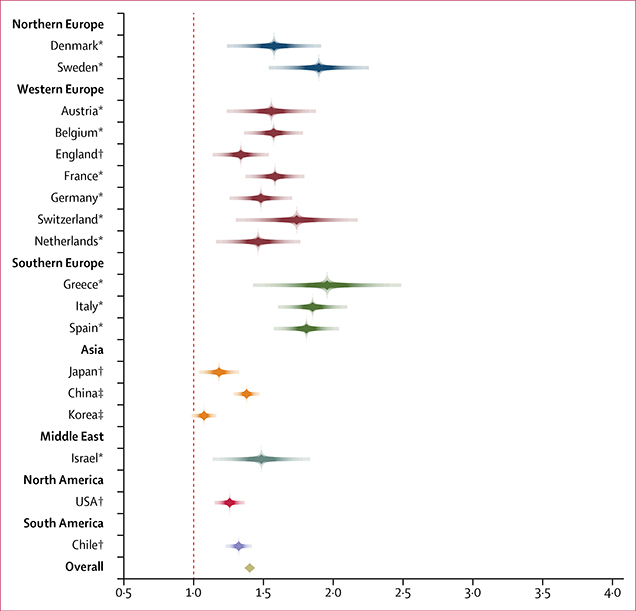
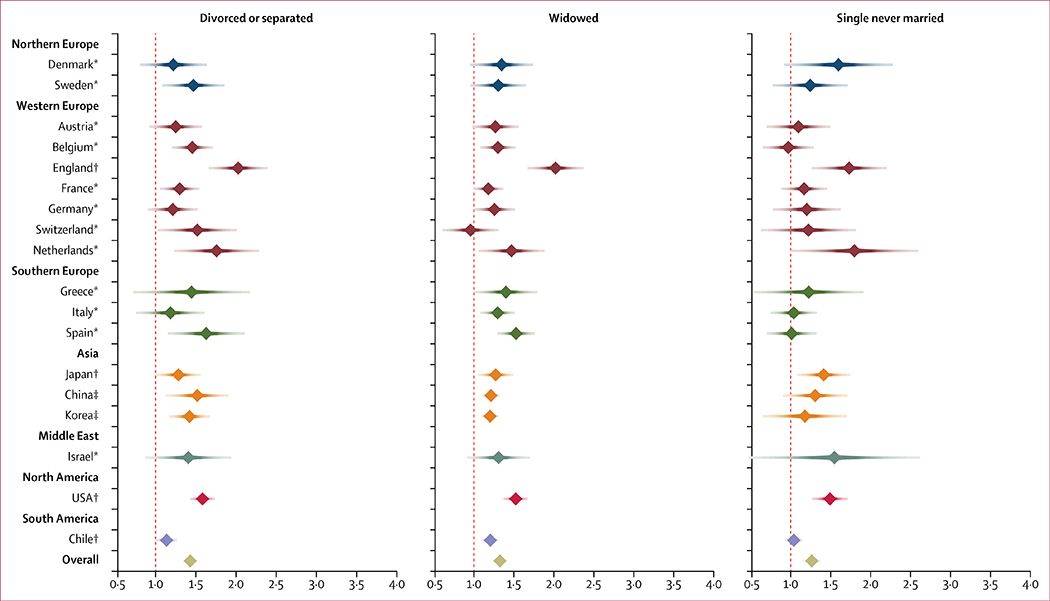
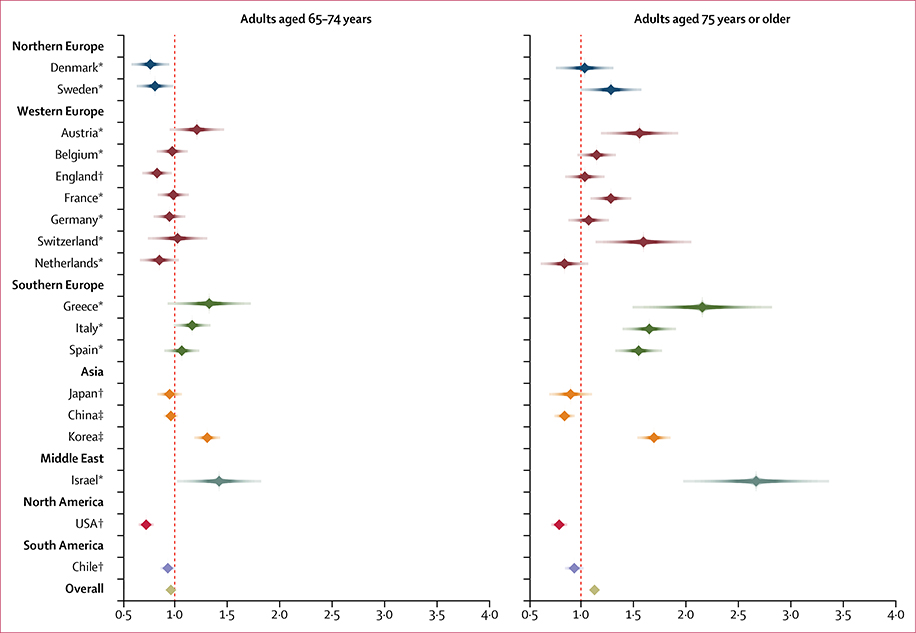
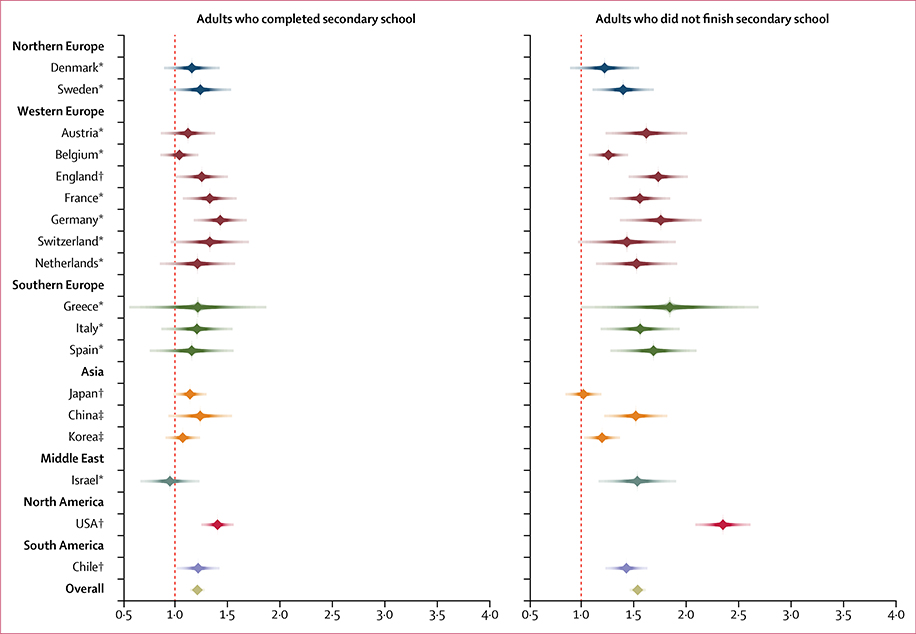
Between Jan 1, 2007, and May 31, 2015, 100 145 total respondents aged 55 years or older from 18 countries completed the surveys, and 93% of respondents (n=93 590) completed questions related to depressive symptoms and were therefore included in our study. The table shows the prevalence of depression within our sample, which ranged from 17·1% (Denmark) to 63·7% (Chile). These prevalence estimates are unweighted, and thus can be interpreted as prevalence estimates of survey participants in each country but not necessarily the prevalence in the general population of older adults. Standardised estimates, which provide comparable estimates across countries, indicate depression prevalence was generally highest among women, individuals aged 75 years or older, those who were divorced, widowed, or single, and those who did not attain a secondary education(figures 1–4). We found the same general pattern of inequalities when estimating prevalence differences (appendix pp 6–7). Unstandardised and partially (ie, age and gender) standardised PR reveal a similar pattern, although the magnitude of the ratios was generally attenuated in the fully standardised estimates (appendix pp 8–11).
Table:
Depression prevalence by country
| Prevalence (SD) | Number of individual with depression/sample size | |
|---|---|---|
| Austria* | 19·7% (39·8) | 726/3681 |
| Belgium* | 28.7% (45·2) | 1299/4527 |
| Chile† | 63·7% (48·1) | 2871/4509 |
| China‡ | 42.0% (49·4) | 4343/10 334 |
| Denmark* | 17·1% (37·6) | 568/3329 |
| England† | 19·4% (39·5) | 1561/8047 |
| France* | 34·6% (47·6) | 1363/3937 |
| Germany* | 23·6% (42·5) | 1046/4435 |
| Greece* | 19·0% (39·2) | 481/2531 |
| Israel* | 25·0% (43·3) | 504/2015 |
| Italy* | 36·2% (48·1) | 1447/4000 |
| Japan† | 34·8% (47·6) | 1361/3912 |
| Korea‡ | 47·5% (49·9) | 3044/6404 |
| Netherlands* | 17·5% (38·0) | 621/3549 |
| Spain* | 30·7% (46·1) | 1688/5501 |
| Sweden* | 18·4% (38·8) | 759/4124 |
| Switzerland* | 17·5% (38·0) | 464/2650 |
| USA† | 22·1% (41·5) | 3553/16 105 |
| Overall | 29·6% (45·6) | 27 699/93 590 |
Probable depression assessed with EURO-D.
Probable depression assessed with the 8-item Center for Epidemiologic Studies Depression scale.
Probable depression assessed with the 10-item Center for Epidemiologic Studies Depression scale.
Figure 1: Predicted depression prevalence ratio by gender.
The reference group is men. The regression model was standardised to mean age, marital status, and education distribution across surveys. The Wald test for heterogeneity across countries was significant, p<0·0001. *Probable depression assessed with EURO−D. †Probable depression assessed with the 8-item Center for Epidemiologic Studies Depression scale. ‡Probable depression assessed with the 10-item Center for Epidemiologic Studies Depression scale.
Figure 4: Predicted depression prevalence ratio by marital status.
The reference group is married or partnered adults. The regression model was standardised to mean gender, age, and education distribution across surveys. The Wald test for heterogeneity across countries was significant, p<0·0001. *Probable depression assessed with EURO−D. †Probable depression assessed with the 8-item Center for Epidemiologic Studies Depression scale. ‡Probable depression assessed with the 10-item Center for Epidemiologic Studies Depression scale.
Inequalities in depression by sociodemographic indicators varied substantially by country. Figure 1 shows inequalities by gender. Although across all countries women had a higher prevalence of depression than men, the magnitude of this inequality varied substantially between countries (p<0·0001). This inequality was generally higher in southern European countries and lowest in Asian countries. For example, Greece had the largest inequality between men and women (PR=1·96, 95% CI 1·55–2·36), and Korea had the smallest (PR=1·07, 95% CI 1·01–1·14; appendix p 8).
Figure 2 shows inequalities in depression by age, which also substantially varied by country (p<0·0001). Among all investigated sociodemographic factors, inequalities due to age varied the most across countries. Whereas in some countries there was almost no inequality in depression between those aged 75 years or older and those aged 55–65 years (eg, Denmark, England, Germany), in other countries this inequality was substantial. The largest inequality in depression between adults aged 75 years or older and those aged 55–65 years was in Israel (PR=2·66, 95% CI 2·13–3·20) and Greece (PR=2·15, 95% CI 1·64–2·66; appendix p 9).
Figure 2: Predicted depression prevalence ratio by age.
The reference group is adults aged 55–65 years. The regression model was standardised to mean gender, marital status, and education distribution across surveys. The Wald test for heterogeneity across countries was significant, p<0·0001. *Probable depression assessed with EURO−D. †Probable depression assessed with the 8-item Center for Epidemiologic Studies Depression scale. ‡Probable depression assessed with the 10-item Center for Epidemiologic Studies Depression scale.
Figure 3 shows inequalities in depression by educational attainment. Although inequalities among all countries showed a general trend indicating that lower levels of educational attainment were associated with a higher prevalence of depression, the magnitude of these inequalities varied substantially by country (p<0·0001). Inequalities between those with less than a secondary education compared with those with some post-secondary education were greatest in the USA (PR=2·34, 95% CI 2·14–2·55) and Greece (PR=1·84, 95% CI 1·19–2·48), and smallest in Japan (PR=1·01, 95% CI 0·88–1·14; appendix p 10).
Figure 3: Predicted depression prevalence ratio by educational attainment.
The reference group is adults with at least some post-secondary education. The regression model was standardised to mean gender, marital status, and age distribution across surveys. The Wald test for heterogeneity across countries was significant, p<0·0001. *Probable depression assessed with EURO−D. †Probable depression assessed with the 8-item Center for Epidemiologic Studies Depression scale. ‡Probable depression assessed with the 10-item Center for Epidemiologic Studies Depression scale.
Figure 4 shows inequalities in depression by marital status. Widowed, divorced or separated, and single adults who were never married had a higher standardised depression prevalence than married people. Although the magnitude of these inequalities varied by country (p<0·0001), inequalities by marital status were generally smaller than for other sociodemographic indicators, and there were no clear outliers (figure 4; appendix p 11).
Discussion
We found substantial variation in the magnitude and direction of inequalities in depression by country and sociodemographic indicators. Previous research investigated inequalities in depression by gender, educational attainment, and wealth in isolation.3,11–14 Our study expands this knowledge by investigating multiple sociodemographic indicators together across a heterogeneous range of countries, and by investigating two factors that have not been previously investigated among older adults: age and marital status. To our knowledge, our study provides the most robust evidence to date that depression inequalities vary across countries.
Our study points to the potential role that the social environment within countries could play in shaping inequalities. For all four investigated sociodemographic factors, we found substantial cross-national differences in inequalities. Our figures, which group countries’ results by region of the world, did not reveal any clear regional patterns. This finding implies that broad characteristics of countries that tend to cluster by region—including collectivist or individualist societies (eg, Asian cultures tend to be more collectivist, whereas European and North Americans cultures tend to be more individualistic),28 gross domestic product, and climate—might not be substantial drivers of depression inequalities. We also did not find that one country consistently had the largest inequalities across all investigated sociodemographic factors, which implies that each inequality is shaped by different aspects of the social environment. For example, aspects related to gender, such as anti-discrimination laws that promote gender equality, might reduce gender-based inequalities, whereas norms about the acceptability of divorce or being single might affect inequalities in marital status. Taken together, our results imply that country-specific characteristics are more important than regional characteristics and that these characteristics shape inequalities through distinct pathways.
Among all investigated factors, we found the most pronounced depression inequalities by age, and age was the only sociodemographic indicator where inequalities could be positive or negative. For example, compared with those aged 55–65 years, those aged 75 years or older had a higher prevalence of depression in Israel (PR=2·66, 95% CI 2·13–3·20), but a lower prevalence of depression in China (PR=0·83, 95% CI 0·76–0·90). Although identifying specific factors that might contribute to inequalities is beyond the scope of this Article, this line of research would be an important addition to the literature.
Our study has limitations. First, we classified people as having probable depression on the basis of depression screening tools (ie, 8-item or 10-item CES-D, EURO-D). Thus, the estimates reported in our Article are not based on clinical appraisal or diagnostic criteria and should be interpreted with caution as depression prevalence estimates. Indeed, the estimates of probable depression in these surveys are generally higher than those reported for older adults in other studies using diagnostic instruments,29 which is probably reflective of the greater heterogeneity and the potentially lower severity of depressed mood captured in depressive symptom scales.
Second, because our study used three separate depression screening tools, differential endorsement of depressive symptoms due to cultural differences or the screening tool is a potential source of measurement bias. We used a fixed effects approach that estimated differences in depression prevalence by sociodemographic indicators within the same country, thus controlling for potential differences due to screening tool (which is consistent within each country) or cultural endorsement of depressive symptoms, or both. Although this approach potentially accounts for substantial measurement bias, biases could persist if depression detection varies by sociodemographic factors within countries. This bias might be especially of concern when comparing age-related inequalities using different screening tools: the EURO-D, which was developed to detect depression in older adults, might be better at detecting depression than the CES-D, which was developed for the general population. A validation study among older adults living in 13 European countries found slight measurement discrepancies: men, older adults, unmarried people, and those with less educational attainment reported slightly more depressive symptoms with the 8-item CES-D than with the EURO-D.23 Although these differences were small, we cannot completely rule out differences in detection due to screening tool as a source of bias. However, we did not find that sociodemographic inequalities were systemically higher when using one screening tool versus another, which suggests that these different screening tools are not differentially detecting depression. For example, the countries with the highest age-related inequalities used the EURO-D (Israel) and the 10-item CES-D (Korea), whereas the greatest gender-related inequalities were detected with the 8-item CES-D (Italy) and the EURO-D (Chile).
Third, our analysis included a restricted set of sociodemographic factors because only a few variables were collected and defined consistently across all surveys. Not including other socioeconomic variables related to depression—such as wealth, income, and race or ethnicity—might have resulted in residual confounding that could bias estimates. These indicators are likely important determinants of depression inequalities in their own right, and investigating cross-national differences in these factors might be a fruitful direction of future research. In addition, future research could investigate comorbidities (especially frailty), which might be important drivers of depression inequalities at both the individual and country level.
Finally, surveys had substantial differences in participation rates, and each survey had slightly different inclusion criteria, sampling frames, recruitment strategies, and interview methods. Although the magnitude of the observed inequalities between countries could be, in part, an artefact of survey methods, we believe these differences did not substantially bias estimates. Our primary estimates are depression PR among sociodemographic groups. Notably, an unbiased effect estimate does not require accurate population prevalence estimates, but instead requires accurate estimation of depression prevalence within sociodemographic groups. Thus, with this estimation strategy, differential or nonrepresentative participation in surveys is only a source of bias if participation is jointly related to depression status and sociodemographic indicators. Previous research shows that adults of lower socioeconomic status who have depression are less likely to participate in research studies,30 and if the same occurred in our study, inequalities in depression might be underestimated and the magnitude of underestimation might differ by country. Although we cannot definitively rule out this potential bias, the validity of our research is bolstered by previous research that has reached similar conclusions. A previous study compared inequalities in depressive symptoms in the USA and Japan using nationally representative datasets composed of both younger and older adults.5 The study found that in both countries, women had more depressive symptoms than men, and unmarried people had more depressive symptoms than married people. However, in Japan there was no evidence of educational inequalities, whereas in the USA people with low educational attainment had more depressive symptoms than people with high educational attainment. This study, which used different surveys and was done in a different population (eg, all adults), mirrors our study: we found substantial inequalities by gender and marital status in Japan and the USA, but educational inequalities only in the USA and not in Japan.
In summary, we found substantial differences in the magnitude of sociodemographic inequalities in depression by country, which were especially pronounced by age. Our results indicate that the social environment might play an important role in generating depression inequalities. Identifying inequalities can be the starting point for designing and evaluating social, economic, and mental health-related interventions to reduce these avoidable inequalities in depression.
Supplementary Material
Research in context.
Evidence before this study
Few studies have evaluated cross-national variation in sociodemographic inequalities in depression among older adults. Using the general search terms “depression”, “socio-economic factors”, and “older adults”, we searched PubMed and PsycINFO, without language restrictions, for articles published before Aug 20, 2019. We also searched the reference lists of included studies. We found five studies. Three studies investigated differences across European countries, one study investigated differences in European countries and the USA, and one study investigated differences in low-income and middle-income countries. These studies investigated single, specific sociodemographic factors, including gender (two studies), educational attainment (two studies), and wealth (one study). The studies either provided crude comparisons (one study), estimates standardised by age and gender (one study), or estimates adjusted for multiple health, psychosocial, or socioeconomic variables (three studies). Because each study controlled for different factors, a direct comparison of the magnitude of inequalities across studies is not possible.
Added value of this study
Our study harmonised data across 18 low-income, middle-income, and high-income countries, and investigated four sociodemographic factors simultaneously, including two that have not been investigated in previous research (ie, marital status, age). For each of these four factors, we estimated country-specific inequalities, which were standardised to the mean distribution of our other investigated sociodemographic factors across all countries. This approach accounts for differences in the sociodemographic makeup of different countries, and thus allows comparison of the magnitude of inequalities across multiple sociodemographic factors. Our study provides the most comprehensive assessment to date of sociodemographic inequalities in depression worldwide.
Implications of all the available evidence
We found that inequalities in depression varied substantially by country for all investigated sociodemographic factors. The most pronounced differences in inequalities were due to age, which is one sociodemographic factor that has not been investigated in previous research. Within-country comparisons of prevalence differences by age revealed that adults aged 75 years or older had either lower or a substantially higher prevalence of depression than did those aged 55–65 years. These results suggest that sociodemographic variation in depression risk is not constant and is shaped by country-level characteristics of the social environment. Our results provide a starting point for future research that seeks to identify which aspects of the social environment drive inequalities. Ultimately, this line of research could inform effective interventions to address these avoidable inequalities.
Acknowledgments
This study was supported by funding from the Chilean National Fund for Scientific and Technological Development (FONDECYT Regular #1181009). RAR’s work was supported by the National Institute of Mental Health (T32 MH013043).
Footnotes
Declaration of interests
We declare no competing interests.
Contributor Information
Robin A Richardson, Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, NY, USA.
Katherine M Keyes, Department of Epidemiology, Mailman School of Public Health, Robert N Butler Columbia Aging Center, Columbia University, New York, NY, USA; Society and Health Research Center, School of Public Health, Universidad Mayor, Santiago, Chile.
José T Medina, Society and Health Research Center, School of Public Health, Laboratory on Aging and Social Epidemiology, Facultad de Humanidades, Universidad Mayor, Santiago, Chile.
Esteban Calvo, Department of Epidemiology, Mailman School of Public Health, Robert N Butler Columbia Aging Center, Columbia University, New York, NY, USA.
References
- 1.Lorant V, Deliège D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol 2003; 157: 98–112. [DOI] [PubMed] [Google Scholar]
- 2.Ferrari AJ, Charlson FJ, Norman RE, et al. The epidemiological modelling of major depressive disorder: application for the Global Burden of Disease Study 2010. PLoS One 2013; 8: e69637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brinda EM, Rajkumar AP, Attermann J, Gerdtham UG, Enemark U, Jacob KS. Health, social, and economic variables associated with depression among older people in low and middle income countries: World Health Organization Study on Global AGEing and Adult Health. Am J Geriatr Psychiatry 2016; 24: 1196–208. [DOI] [PubMed] [Google Scholar]
- 4.Afifi TO, Cox BJ, Enns MW. Mental health profiles among married, never-married, and separated/divorced mothers in a nationally representative sample. Soc Psychiatry Psychiatr Epidemiol 2006; 41: 122–29. [DOI] [PubMed] [Google Scholar]
- 5.Inaba A, Thoits PA, Ueno K, Gove WR, Evenson RJ, Sloan M. Depression in the United States and Japan: gender, marital status, and SES patterns. Soc Sci Med 2005; 61: 2280–92. [DOI] [PubMed] [Google Scholar]
- 6.Liu S, Jones RN, Glymour MM. Implications of lifecourse epidemiology for research on determinants of adult disease. Public Health Rev 2010; 32: 489–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chapman DP, Perry GS, Strine TW. The vital link between chronic disease and depressive disorders. Prev Chronic Dis 2005; 2: A14. [PMC free article] [PubMed] [Google Scholar]
- 8.Turvey CL, Conwell Y, Jones MP, et al. Risk factors for late-life suicide: a prospective, community-based study. Am J Geriatr Psychiatry 2002; 10: 398–406. [PubMed] [Google Scholar]
- 9.Stone DM, Simon TR, Fowler KA, et al. Vital signs: trends in state suicide rates—United States, 1999–2016 and circumstances contributing to suicide—27 States, 2015. MMWR Morb Mortal Wkly Rep 2018; 67: 617–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barnett E, Casper M. A definition of “social environment”. Am J Public Health 2001; 91: 465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hansen T, Slagsvold B, Veenstra M. Educational inequalities in late-life depression across Europe: results from the generations and gender survey. Eur J Ageing 2017; 14: 407–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ladin K Risk of late-life depression across 10 European Union countries: deconstructing the education effect. J Aging Health 2008; 20: 653–70. [DOI] [PubMed] [Google Scholar]
- 13.Schmitz A, Brandt M. Gendered patterns of depression and its determinants in older Europeans. Arch Gerontol Geriatr 2019; 82: 207–16. [DOI] [PubMed] [Google Scholar]
- 14.Crimmins EM, Kim JK, Solé-Auró A. Gender differences in health: results from SHARE, ELSA and HRS. Eur J Public Health 2011; 21: 81–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Radloff LS. The CES-D scale: a self report depression scale for research in the general population. Appl Psychol Meas 1977; 1: 385–401. [Google Scholar]
- 16.Prince MJ, Reischies F, Beekman AT, et al. Development of the EURO-D scale—a European Union initiative to compare symptoms of depression in 14 European centres. Br J Psychiatry 1999; 174: 330–38. [DOI] [PubMed] [Google Scholar]
- 17.Guerra M, Ferri C, Llibre J, Prina AM, Prince M. Psychometric properties of EURO-D, a geriatric depression scale: a cross-cultural validation study. BMC Psychiatry 2015; 15: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Castro-Costa E, Dewey M, Stewart R, et al. Ascertaining late-life depressive symptoms in Europe: an evaluation of the survey version of the EURO-D scale in 10 nations. The SHARE project. Int J Methods Psychiatr Res 2008; 17: 12–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheng ST, Chan AC. The Center for Epidemiologic Studies Depression Scale in older Chinese: thresholds for long and short forms. Int J Geriatr Psychiatry 2005; 20: 465–70. [DOI] [PubMed] [Google Scholar]
- 20.Missinne S, Vandeviver C, Van de Velde S, Bracke P. Measurement equivalence of the CES-D 8 depression-scale among the ageing population in eleven European countries. Soc Sci Res 2014;46: 38–47. [DOI] [PubMed] [Google Scholar]
- 21.Karim J, Weisz R, Bibi Z, ur Rehman S. Validation of the eight-item Center for Epidemiologic Studies Depression Scale (CES-D) among older adults. Curr Psychol 2015; 34: 681–92. [Google Scholar]
- 22.Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D). Arch Intern Med 1999; 159: 1701–04. [DOI] [PubMed] [Google Scholar]
- 23.Courtin E, Knapp M, Grundy E, Avendano-Pabon M. Are different measures of depressive symptoms in old age comparable? An analysis of the CES-D and Euro-D scales in 13 countries. Int J Methods Psychiatr Res 2015; 24: 287–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Health and Retirement Study’s Health Working Group. Documentation of affective functioning measures in the health and retirement study. Michigan: University of Michigan, 2000. [Google Scholar]
- 25.Iwata N, Roberts CR, Kawakami N. Japan–U.S. comparison of responses to depression scale items among adult workers. Psychiatry Res 1995; 58: 237–45. [DOI] [PubMed] [Google Scholar]
- 26.Mackenbach JP, Kunst AE. Measuring the magnitude of socioeconomic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med 1997; 44: 757–71. [DOI] [PubMed] [Google Scholar]
- 27.Kelly MP, Morgan A, Bonnefoy J, Butt J, Bergmann V. The social determinants of health: developing an evidence base for action, 2007.
- 28.Triandis HC. The self and social behavior in differing cultural contexts. Psychol Rev 1989; 96: 506–20. [Google Scholar]
- 29.Hasin DS, Sarvet AL, Meyers JL, et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry 2018; 75: 336–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bergman P, Ahlberg G, Forsell Y, Lundberg I. Non-participation in the second wave of the PART study on mental disorder and its effects on risk estimates. Int J Soc Psychiatry 2010; 56: 119–32. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.