Abstract
We used the Balloon Analog Risk Task (BART) to examine risk taking and sensitivity to punishment, two relevant aspects of behavioral inhibition, in 203 school-age children with attention-deficit/hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), ADHD+ODD, and controls. Participants earned points on the BART by pumping 30 separate balloons that exploded at variable intervals. No points were earned on a trial when a balloon exploded. The number of pumps across all balloons estimated risk taking and the reduction in pumps following balloon explosions was interpreted as an indicator of sensitivity to negative punishment. We found that all groups significantly differed from one another on risk taking. The ADHD+ODD group pumped the most, followed by the ODD, ADHD, and the control group, respectively. For sensitivity to negative punishment, all groups performed differently, with the ODD group showing the least sensitivity to an exploded balloon, followed by the ADHD, control, and ADHD+ODD groups, respectively. Children with ADHD+ODD demonstrated significantly different patterns of risk taking and sensitivity to negative punishment than children with either ADHD-only or ODD-only. ADHD youth with comorbid ODD had the greatest levels of risk taking, but they were also the most sensitive to negative punishment. The relationship between ADHD and ODD, as well as the nature of comorbidity in constructs related to risk taking and related behaviors, are discussed.
Keywords: ADHD, Oppositional defiant disorder, Risk taking, Punishment, Comorbidity
Attention-deficit/hyperactivity disorder (ADHD) is characterized by an early onset of developmentally aberrant and impairing levels of inattention and/or hyperactivity-impulsivity (American Psychiatric Association [APA] 2000). The worldwide prevalence of ADHD has been estimated at 5.3% (Polanczyk et al. 2007). ADHD is one of the most common referrals for mental health, educational, and pediatric services (Barkley 1998), and the financial burden of managing a child with ADHD has been estimated to be $12,005 to $17,458 per individual annually in the United States (Pelham et al. 2007). Therefore, childhood ADHD is highly prevalent with significant public health implications.
Independent of demographic and clinical confounds, ADHD prospectively predicts negative outcomes and impairment. In two separate samples of preschool children and school-aged girls followed prospectively into adolescence, ADHD probands were less positively adjusted across multiple domains (i.e., comorbidity, social skills, peer relationships) than comparisons, even when academic achievement and ADHD symptoms were excluded from the definition of positive adjustment (Owens et al. 2009; Lee et al. 2008). A recent meta-analysis reported that children with ADHD were significantly more likely to have ever used nicotine and drugs and to develop nicotine, alcohol, and drug abuse or dependence in adolescence and early adulthood (Lee et al. 2011). Thus, ADHD is characterized by multifinality where negative outcomes are widely dispersed across behavioral, academic, and social domains (Cicchetti and Rogosch 1996).
Although behavioral inhibition (BI) deficits have been proposed as a central feature of ADHD (Aron and Poldrack 2005; Barkley 1997), its multifactorial nature, including impulsivity, executive control, working memory, and vigilance, has complicated efforts to identify its precise architecture (Congdon and Canli 2005). Risk taking is a BI-related construct, and consists broadly of the tendency to engage in negative behavior that compromises health, well-being, and the life-course (Jessor 1998). Although engagement in risky behavior increases across childhood and peaks during adolescence (Steinberg 2007), there are important individual differences in risk taking propensity (Tom et al. 2007). Boyer (2006) outlined important processes that influence risk taking behavior, including the psychobiological development of cognitive and affective processes (e.g., knowledge structures, emotion regulation), which may impact perceptions of risk and vulnerability. In fact, the ability to accurately gauge and avoid risky or dangerous situations is necessary to function safely and adaptively (Garon and Moore 2004; Mann et al. 1989; Steinberg and Scott 2003).
Risk taking may be relevant to ADHD for several reasons. For example, risk taking is associated with later substance use (Burt et al. 2000), a common outcome among individuals diagnosed with childhood ADHD (Charach et al. 2011; Lee et al. 2011). ADHD also prospectively predicted risky driving, sexual behavior, gambling, and unintentional injury (Breyer et al. 2009; Flory et al. 2006; Garzon et al. 2008; Thompson et al. 2007). However, it is unclear whether the association between risk taking and ADHD is explained by its frequent comorbidity with disruptive behavior disorders (DBDs) (i.e., oppositional defiant disorder [ODD] and conduct disorder [CD]). Lilienfeld and Waldman (1990) reviewed prospective studies of early ADHD and subsequent antisocial behavior (ASB) and concluded that most were contaminated by comorbid DBD, thereby preventing inferences about the specificity of ADHD and ASB. This limitation may also pertain to previous studies of ADHD and risk taking given that previous studies often ignored the possible effects of comorbid DBD.
A recent study of categorically- and dimensionally-defined ADHD and BI (i.e., impulsivity, delay aversion) did not account for comorbid externalizing problems (Paloyelis et al. 2009). There is also evidence that ADHD was positively associated with BI deficits, controlling for ODD and CD (Nigg et al. 1998) and that ADHD predicted BI even after accounting for concurrent ODD among 6–13 year-old children (de Zeeuw et al. 2008). However, Kuntsi et al. (2001) reported that differences between hyperactive and non-hyperactive children on delay aversion were fully explained by co-occurring DBD. Furthermore, although children with ADHD versus ADHD+ODD performed equivalently on a delay aversion task (Antrop et al. 2006), it is also possible that ADHD and ODD may interact to predict more BI problems or risk taking behavior. Although theoretical formulations suggest that ADHD is uniquely associated with impulsivity whereas ADHD and comorbid ODD are related to socio-affective dysregulation, including altered responses to reward and punishment (Hinshaw 2003; Nigg 2003), these models necessitate formal empirical evaluation. Overall, in light of inconclusive evidence from previous studies (Reynolds et al. 2006) and the fact that risk taking may be related to DBDs (Schwebel et al. 2002), it is important to determine the specificity of risk taking in children with ADHD, DBD, and their combination.
Both approach and avoidance behaviors are necessary for adaptive functioning, as individuals must simultaneously seek opportunities for survival and avoid danger (Everitt and Robbins 2005). Therefore, individuals must effectively negotiate approach and avoidance tendencies. Functional magnetic resonance imaging (fMRI) research suggests overlapping, but dissociable systems are active during tasks sensitive to approach and avoidance behavior (Wrase et al. 2007). While activation in the ventral striatum was associated with both reward and punishment cues and the dorsal striatum was associated with delivered rewards, the anterior cingulate was related to delivered negative punishments. Differences in these neural systems may be related to behavioral dysfunction whereas adaptive decision-making requires both risk-taking and punishment sensitivity, as evidenced by neuropsychological tests such as the Iowa Gambling Task (Bechara et al. 1994). Adaptive behavior, therefore, requires that approach tendencies be modified by the prospect of punishment. Arnett (1992) observed that even during adolescence, a developmental period associated with greatly increased risk taking behavior, the potential for punishment influenced risk taking (Newman 1987). Individuals vary in sensitivity to threat or punishment, and extant research provides evidence that children with ADHD are motivated by the prospect of punishment. For example, children with ADHD performed more accurately on tasks when failure resulted in negative punishment (i.e., the removal of something desired) than on tasks with no contingency for performance (Carlson et al. 2000; Carlson and Tamm 2000). Previous work on reward and negative punishment also suggests that the loss of even small amounts of money increases response time on behavioral tasks in children with ADHD (Arnett et al. 1996).
However, it is unclear whether the degree of punishment sensitivity is consistent across children with versus and without ADHD. Previous studies that examined risk taking and sensitivity to negative punishment found that children with ADHD had greater risk taking in conditions of punishment (DeVito et al. 2008), and fewer behavioral responses to punishment (Masunami et al. 2009). Both studies linked these behaviors to poorer decision-making on gambling tasks. In addition to ADHD, ODD may also relate to decreased sensitivity to negative punishment. Compared to controls, boys with ODD were less likely to modify behavior that was initially rewarded but subsequently punished (Matthys et al. 2004). Thus, children with ODD may be less sensitive to punishment relative to typically developing children. Notably, because studies to date have largely utilized two-group comparisons (e.g., ADHD versus non-ADHD), they have been unable to clarify the specificity of patterns of association in multiple clinical groups (e.g., ADHD and comorbid ODD), an important consideration in studies of externalizing problems (Hinshaw and Lee 2003).
Measurement strategies for BI domains vary considerably, although most studies relied on rating scales. This is a significant limitation because rating scales of child behavior often rely on exclusively on parental report, which can be biased by parental psychopathology (Kroes et al. 2003; Youngstrom et al. 1999). The Balloon Analog Risk Task (BART; Lejuez et al. 2002) is a computer analog that presents 30 separate balloons to participants who pump up balloons for points (more pumps = greater points earned). However, balloons explode at a variable number of pumps and no points are earned on that trial. Previous studies found that balloon pumping on the BART was positively associated with risky sexual behavior (Lejuez et al. 2005), smoking (Lejuez et al. 2003), and a composite of substance use, sexual behavior, delinquency, and health domains (Lejuez et al. 2007). BART also simultaneously presents rewards (points) and negative punishment (points revoked for an exploded balloon), which is necessary to optimally evoke impulsive responding (Gomez 2003). To our knowledge, this is the first study of the BART in children with ADHD.
Our goal was to examine risk taking and sensitivity to punishment via the BART in four groups of children: ADHD-only, ODD-only, ADHD+ODD, and controls (i.e., no ADHD and no ODD). We hypothesized that, relative to controls, children with ODD-only would exhibit the most risk taking and be the least sensitive to punishment relative to children with ADHD only and controls. Given that previous theory and research does not provide clear evidence about the nature of risk taking and sensitivity to punishment in children with ADHD+ODD, we did not formulate specific hypotheses about differences between ODD-only versus ADHD+ODD youth.
Method
Participants
Participants were 203 (71% male) ethnically diverse (49% Caucasian) children with (n=103) and without ADHD (n=100) (Table 1). The full age range consisted of 5–10 year olds (M= 7.39, SD= 1.12), though the majority of participants (98%) were between the ages of 6 and 9 at the time of testing. Participants were recruited using presentations to ADHD self-help groups, flyers mailed to local schools, pediatric offices, and clinical service providers, and referrals from mental health clinics. Children were required to live with at least one biological parent at least half time and both parent and child were required to be fluent in English. Exclusion criteria for all participants consisted of a Full Scale IQ<70, pervasive developmental, seizure, or any neurological disorder that prevented full participation in the study (see Castel et al. 2011 and Humphreys et al. 2011 for additional details).
Table 1.
Age, gender, and ODD status based on ADHD status
| ADHD N=103 | No ADHD N =100 | t-value or χ2 | |
|---|---|---|---|
| Age Mean (SD) | 7.30 (1.11) | 7.49 (1.12) | 1.21 |
| Gender (% Male) | 77% | 66% | 2.85 |
| ODD diagnosis (% Yes) | 47% | 13% | 27.26*** |
ADHD attention-deficit/hyperactivity disorder. ODD oppositional defiant disorder.
p<.001
ADHD and ODD status were ascertained using a structured diagnostic interview with the parent. To avoid recruiting an improbably ‘high-functioning’ control group, which could exaggerate group differences, control children who met criteria for any disorder other than ADHD were included. In order to characterize the precise contribution of ADHD, ODD, and their comorbidity on risk taking and punishment sensitivity, we created four clinical groups: (1) neither ADHD or ODD (Controls; n=87); (2) ADHD without ODD (ADHD-only; n=55), (3) ODD without ADHD (ODD-only; n=13); and (4) ADHD and ODD (ADHD+ODD; n= 48).
Procedures
Eligibility for the study was determined through an initial telephone screening. Parents completed behavior rating scales and families were invited to our research laboratory for in-person assessments of child behavior and family functioning. Whenever possible, children were assessed in our laboratory without psychotropic medication. Approximately 15% of parents reported that their children were taking psychotropic medication on the day of the assessment. If a child normally received medication, we asked that parents and teachers provide ratings based on the child’s unmedicated behavior. Similar procedures have been used in other ADHD studies, including the Multimodal Treatment Study of ADHD (Lee et al. 2008; Hinshaw et al. 1997). All interviewers were blind to the child’s diagnostic status. Parents consented and children assented to all procedures. The Institutional Review Board approved all study procedures.
Background Measures
ADHD and ODD
Diagnostic Interview Schedule for Children—Fourth Edition (DISC-IV; Schaffer et al. 2000) Diagnostic criteria for ADHD and ODD were determined by administering the computerized DISC-IV to each participant’s parent. This fully structured interview probes required symptoms, duration, age of onset, and impairment. Test-retest reliability for ADHD diagnosed by the DISC was between .51 and .64 and for ODD was .54 in the DSM-IV Field Trials (Lahey et al. 1994a, b). Diagnostic designations from the DISC have shown predictive validity in other studies of ADHD (Owens et al. 2009; Lee et al. 2008).
Risk Taking and Sensitivity to Punishment
Balloon Analogue Risk Task (BART; Lejuez et al. 2002; Lejuez et al. 2007) Two different computerized versions of the BART were used. For both versions, each child was asked to pump 30 separate balloons and earned points based on the number of pumps for each balloon (i.e., more pumps earned more points). Balloons exploded at an unknown, variable number of pumps, resulting in the loss of all points for that trial. In the first BART version, participants pressed the mouse for each pump. In the second version, participants typed in the number of pumps for each balloon. Both versions had an average explosion point of 65 pumps. Children exchanged their points for stickers at the end of the task. We examined two variables: (1) total number of pumps across the task (TotalPumps). The mean TotalPumps score was 923.44 (SD= 489.16), and ranged from 167 to 2288; (2) To assess sensitivity to negative punishment, for each balloon that exploded, we subtracted the number of pumps made on the balloon trial immediately following the exploded balloon from the number of pumps made on the trial preceding the exploded balloon. Positive values indicate fewer pumps on the subsequent balloon whereas negative values indicate more pumps following a balloon explosion. We summed each difference score following explosions to approximate post explosion behavior (PostExp). The mean PostExp score was 66.67 (SD =144.21), suggesting that, on average, children pumped less following an exploded balloon. Scores ranged from −345 to 519. We added 346 to each case to accommodate data analyses, which required positive integers. Given that individuals differed in the number of explosions across the task and each explosion allowed estimating post explosion behavior, the number of explosions was covaried in the models of post explosion behavior.
Data Analysis
Our goal was to examine risk taking and sensitivity to punishment in four groups of children: 1) Controls, 2) ADHD-only, 3) ODD-only, and 4) ADHD+ODD. Total-Pumps and PostExp, our two key dependent variables, reflect counts of behaviors (e.g., number of pumps). We used a generalized linear model specifying Poisson regression in Predictive Analytics SoftWare Statistics (PASW) 18.0 to accommodate the non-normal distribution, which is highly characteristic of count data. Next, because the BART is sensitive to age effects (MacPherson et al. 2010), we controlled for the child’s age, as well as the BART version. We conducted two separate Poisson regression models where the number of pumps from TotalPumps and PostExp (i.e., count data) constituted our dependent variables and a dummy-coded variable coded for the four groups represented our independent variable. When an omnibus test for the dummy-coded group variable significantly predicted the dependent variable, estimated means for each diagnostic group was computed, adjusting for covariates. We then conducted pairwise comparisons using Fisher’s least significant difference (LSD) post hoc test to probe group differences, thereby providing a conservative test to protect against Type I error.
Results
Table 2 presents the correlation matrix for ADHD and ODD status with age, sex, and the two outcome variables of interest (TotalPumps and PostExp). As expected, ADHD and ODD status were moderately correlated (r=.38). Age was significantly associated with TotalPumps, but child sex was not significantly associated with either outcome variable. A modest significant association was found for risk taking and sensitivity to negative punishment (r=.18), suggesting that these constructs are related but meaningfully different and justify separate examination.
Table 2.
Correlation matrix demographic, predictor, and outcome variables
| Age | Male | ADHD | ODD | TotalPumps | PostExp | |
|---|---|---|---|---|---|---|
| Age | 1 | |||||
| Male=1 | −.06 | 1 | ||||
| ADHD Y/N | −.11 | .09 | 1 | |||
| ODD Y/N | .04 | .04 | .38*** | 1 | ||
| TotalPumps | .16* | −.00 | −.01 | .13† | 1 | |
| PostExpa | −.08 | −.08 | −.02 | .06 | .18** | 1 |
FSIQ Full Scale IQ. ADHD attention-deficit/hyperactivity disorder. ODD oppositional defiant disorder. TotalPumps Number of Pumps on the BART. PostExp Post Explosion behavior on the BART.
Correlation with TotalPumps presented after partialling out number of explosions and BART version
p<.10.
p<.05.
p<.01.
p<.001
Risk Taking
Controlling for age and BART version, the omnibus test for the group variable was significantly related to risk taking (i.e., TotalPumps) (Wald χ2=372.81, p<.001). Post hoc analyses revealed that all groups significantly differed from one another with ADHD+ODD children pumping the most. This was followed by the ODD-only group, and then the ADHD-only group. The comparison children pumped the least across the task (Fig. 1).
Fig. 1.
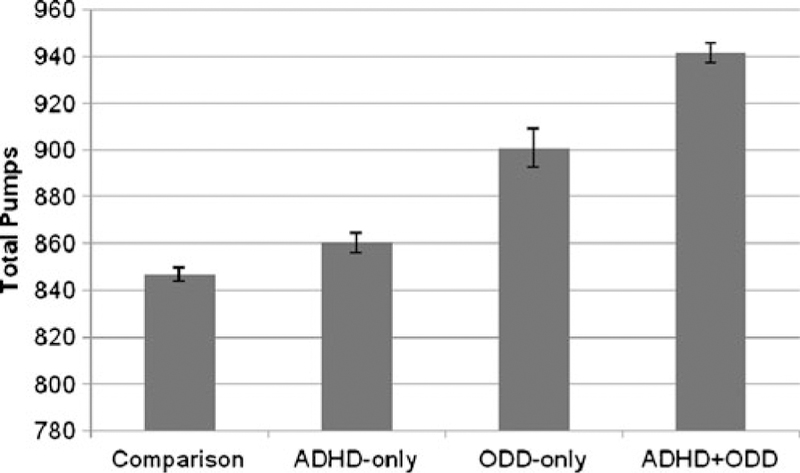
Total pumps by group status. Note. Means and standard errors are modeled after adjusting for BART version and age. ADHD = attention-deficit/hyperactivity disorder. ODD = oppositional defiant disorder
Sensitivity to Punishment
Controlling for age, BART version, and the number of explosions, the omnibus test for group status and post explosion behavior was significant (Wald χ2=200.24, p<.001). Post hoc tests found that that all groups significantly differed from one another. As higher values suggest greater reactivity to explosions (i.e., fewer pumps following a balloon explosion), the ODD group was the least sensitive to punishment, followed by the ADHD-only and the control group (Fig. 2). Interestingly, the ADHD+ODD group was the most sensitive to punishment.
Fig. 2.
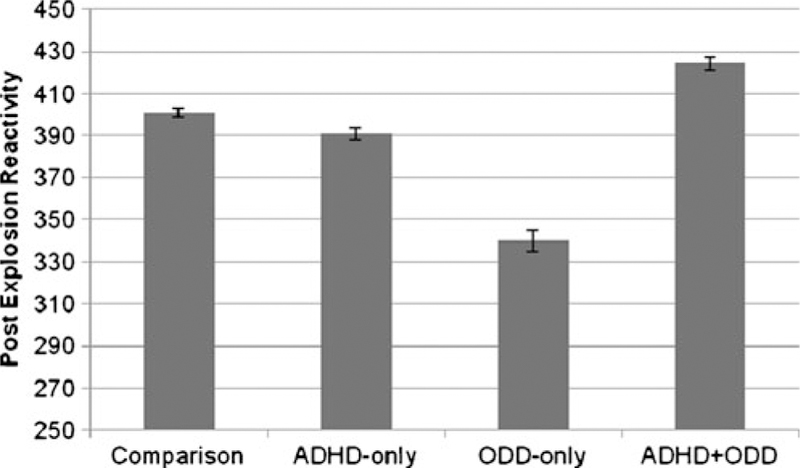
Post explosion reactivity by group status. Note. Means and standard errors are modeled after adjusting for BART version, age, and number of explosions. Higher numbers indicate greater reduction in pumps following explosions. ADHD = attention-deficit/hyperactivity disorder. ODD = oppositional defiant disorder
Discussion
Among 203 5–10 year-old children (controls, ODD-only, ADHD-only, ADHD+ODD), “pure” ADHD (i.e., without ODD) positively predicted increased risk taking relative to controls. ODD predicted the greatest level of risk taking (Schwebel et al. 2002), as children with ODD and ADHD+ODD pumped more than the ADHD-only and control groups. Children with both ADHD and ODD had the greatest level of risk taking, further supporting that this group of children is a clinically significant subgroup of the population by virtue of its elevated risk for negative outcomes (Gadow and Nolan 2002; Kuhne et al. 1997). Results also indicated that the ADHD+ODD group was the most sensitive to punishment.
ADHD is associated with increased impulsivity on tasks of motoric inhibition (e.g., Stop Task) (Alderson et al. 2007), yet the association of ADHD with non-inhibitory BI tasks, such as the BART, appears to vary as a function of comorbid DBDs. Although “pure” ADHD was associated with moderately higher levels of risk taking compared to controls, ODD was associated the highest level of risk taking. These patterns are generally consistent with Nigg’s (2003) assertion that ADHD-Combined Type and early-onset CD were prototypical disorders of cognitive and motivational impulsivity, respectively. Our findings suggest that deficient motivational gradients may also be related to ODD, a frequent precursor to early-onset CD (Loeber et al. 2000). The increased risk taking found in children with ADHD+ODD provides additional evidence that this group is distinct from ADHD-only or ODD-only (Hinshaw et al. 1993; Lahey et al. 1999). Consistent with these findings, previous work indicated that children with ADHD and DBD were more impulsive than children with ADHD-only (Newcorn et al. 2001). In fact, some negative outcomes associated with childhood ADHD may be partially explained by co-occurring DBD, including expulsion and school drop-out (Barkley et al. 1990).
Our findings support previous research that ODD predicts risk taking (Garzon et al. 2008; Schwebel et al. 2002) and reduced reactivity to punishment (Matthys et al. 2004; van Bokhoven et al. 2005). Although the interpersonal and affective features of psychopathy are not part of the diagnostic criteria for ODD (Loeber et al. 2009), the antecedents of psychopathy can be reliably measured in young children and predict future conduct problems (Kochanska and Aksan 2006; Ostrov 2006). Further work should investigate whether punishment sensitivity is differentially associated with early-onset CD or psychopathic traits.
The literature consists of inconsistent evidence on the association of ADHD and sensitivity to punishment, including reports of diminished reactivity (Masunami et al. 2009) and comparable sensitivity to controls (Geurts et al. 2006). Our findings suggest that children with ADHD-only were slightly less sensitive to punishment compared to control children, but more sensitive than children with ODD-only. This association is consistent with previous work that ADHD was positively related to response cost (Carlson et al. 2000; Carlson and Tamm 2000). We note that punishment should be differentiated according to negative punishment (i.e., removal of a desired object) versus positive punishment (i.e., application of an aversive stimulus). We suggest that failing to consider DBD in previous studies may have contributed to findings that ADHD predicted increased reactivity to negative punishment, given that the comorbid ADHD+ODD group was the most sensitive to punishment.
Nigg et al. (2004) proposed that children with ADHD and DBD are centrally characterized by poor affect regulation. Therefore, although children with ADHD and DBD engage in greater risk, we cannot assume that they are immune to the feedback loop of punishment. In fact, these children may be too reactive or unable to adaptively respond to punishment, and therefore may be more inclined to perform inconsistently across the task by taking greater risks but also greatly moderating their behavior when their actions led to an undesirable outcome (i.e., loss of points). The ability to accurately determine the importance of an event (i.e., balloon explosion) may require the ability to efficiently recover from a punishment or negative consequence, and children with ADHD and ODD may be more prone to excessive emotional reactivity to minor negative events. Post-explosion behavior may also reflect a failure to learn the task appropriately. Pleskac (2008) observed that the sequential nature of the BART implies a learning effect, which enables participants to determine the nonstationary probablistic nature of the task. Children with ADHD+ODD may be slower to learn that the balloon trials were equally likely to explode over time and that each trial had the same probability of exploding.
These findings should be considered in light of important limitations. Our cross-sectional design did not address relevant questions such as the sensitivity of the BART to ADHD and ODD across time. It should also be noted that alternative BART outcome measures have been used by other researchers (e.g., Lejuez et al. 2003; Pleskac 2008) and our sample size prevented examination of potential sex or racial-ethnic differences. In addition, some children had taken their usual medication on the day of testing, and it is unclear if medication influenced BART performance. Given that medication use is not randomly distributed in the population, we could not meaningfully examine the effects of medication on these findings. Another consideration was that we did not determine whether ODD per se related to BART performance or whether ODD was a proxy for callous-unemotional traits or temperament (e.g., harm avoidance) or other constitutional features that may underlie ODD.
It is well known that ADHD is clinically heterogeneous (Faraone 2000; Wåhlstedt et al. 2009), particularly with respect to comorbidity. Our findings substantiate the importance of considering DBD in studies of ADHD, BI, risk taking, and punishment sensitivity. Given that the association of ADHD and BART differed by comorbid ODD, studies of ADHD that ignore DBD may misrepresent ADHD and critical BI dimensions. For example, comorbid DBD may mediate the relation between ADHD and substance use outcomes (Flory and Lynam 2003; Lee et al. 2011). Whereas ADHD has been linked to negative outcomes, this study suggests that “pure” ADHD (i.e., independent of ODD) may be nominally related to risk taking whereas ADHD+ODD is related to the greatest levels of risk taking. In addition, ADHD+ODD was associated increased sensitivity to punishment unlike the “pure” ODD group, which was the least sensitive to punishment. The field must precisely characterize how ADHD and DBD, independently and interactively, predict different facets of risky behavior. Importantly, future studies must empirically evaluate the underlying architecture of BI to advance innovations in treatment for the many forms of psychopathology that are associated with BI deficits.
Acknowledgements
We wish to thank Dr. Lara Ray for her comments and revisions on earlier versions of this manuscript. We also thank the families for participation in the study and the research staff for their help with data collection and management. This work was partially supported by the Consortium for Neuropsychiatric Phenomics (CNP) (NIH Roadmap for Medical Research grant UL1-DE019580, RL1DA024853) and NIH grant 1R03AA020186-01 to Steve S. Lee. This work was also supported by a National Science Foundation (NSF) Graduate Research Fellowship to the first author.
References
- Alderson RM, Rapport MD, & Kofler MJ (2007). Attention-deficit/hyperactivity disorder and behavioral inhibition: A meta-analytic review of the stop-signal paradigm. Journal of Abnormal Child Psychology, 35, 745–758. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev). Washington, DC: Author. [Google Scholar]
- Antrop I, Stock P, Verté S, Wiersema JR, Baeyens D, & Roeyers H (2006). ADHD and delay aversion: The influence of non-temporal stimulation on choice for delayed rewards. Journal of Child Psychology and Psychiatry, 47, 1152–1158. [DOI] [PubMed] [Google Scholar]
- Arnett JJ (1992). Reckless behavior in adolescence: a developmental perspective. Developmental Review, 12, 339–373. [Google Scholar]
- Arnett PA, Fischer M, & Newby RF (1996). The effect of Ritalin on response to reward and punishment in children with ADHD. Child Study Journal, 26, 51–70. [Google Scholar]
- Aron AR, & Poldrack RA (2005). The cognitive neuroscience of response inhibition: Relevance for genetic research in attention-deficit/hyperactivity disorder. Biological Psychiatry, 57, 1285–1292. [DOI] [PubMed] [Google Scholar]
- Barkley RA (1997). Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychological Bulletin, 121, 65–94. [DOI] [PubMed] [Google Scholar]
- Barkley RA (1998). Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment (2nd ed.). New York: Guilford. [Google Scholar]
- Barkley RA, Fischer M, Edelbrock CS, & Smallish L (1990). The adolescent outcome of hyperactive children diagnosed by research criteria: I. An 8-year prospective follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry, 29, 546–557. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio AR, Damasio H, & Anderson SW (1994). Insensitivity to future consequences following damage to human prefrontal cortex. Cognition, 50, 7–15. [DOI] [PubMed] [Google Scholar]
- Boyer TW (2006). The development of risk-taking: A multi-perspective review. Developmental Review, 26, 291–345. [Google Scholar]
- Breyer JL, Botzet AM, Winters KC, Stinchfield RD, August G, & Realmuto G (2009). Young adult gambling behaviors and their relationship with the persistence of ADHD. Journal of Gambling Studies, 2, 227–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt RD, Dinh KT, Peterson AV, & Sarason IG (2000). Predicting adolescent smoking: A prospective study of personality variables. Preventive Medicine, 30, 115–125. [DOI] [PubMed] [Google Scholar]
- Carlson CL, & Tamm L (2000). Responsiveness of children with attention deficit–hyperactivity disorder to reward and response cost: Differential impact on performance and motivation. Journal of Consulting and Clinical Psychology, 68, 73–83. [DOI] [PubMed] [Google Scholar]
- Carlson CL, Mann M, & Alexander DK (2000). Effects of reward and response cost on the performance and motivation of children with ADHD. Cognitive Therapy and Research, 24, 87–98. [Google Scholar]
- Castel AD, Lee SS, Humphreys KL, & Moore AN (2011). Memory capacity, selective control and value-directed remembering in children with and without attention-deficit/hyperactivity Disorder (ADHD). Neuropsychology, 25, 15–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charach A, Yeung E, Climans T, & Lillie E (2011). Childhood attention-deficit/hyperactivity disorder and future substance use disorders: Comparative meta-analyses. Journal of the American Academy of Child and Adolescent Psychiatry, 50, 9–21. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Rogosch FA (1996). Equifinality and multifinality in developmental psychopathology. Development and Psychopathology, 8, 597–600. [Google Scholar]
- Congdon E, & Canli T (2005). The endophenotype of impulsivity: Reaching consilience through behavioral, genetic, and neuroimaging approaches. Behavioral and Cognitive Neuroscience Reviews, 4, 262–281. [DOI] [PubMed] [Google Scholar]
- de Zeeuw P, Aarnoudse-Moens C, Bijlhout J, König C, Uiterweer AP, Papanikolau A, et al. (2008). Inhibitory performance, response speed, IIV, and response accuracy in ADHD. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 808–816. [DOI] [PubMed] [Google Scholar]
- DeVito EE, Blackwell AD, Kent L, Ersche KD, Clark L, Salmond CH, et al. (2008). The effects of methylphenidate on decision making in attention-deficit/hyperactivity disorder. Biological Psychiatry, 64, 636–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everitt BJ, & Robbins TW (2005). Neural systems of reinforcement for drug addiction: From actions to habits to compulsion. Nature Neuroscience, 8(11), 1481–1489. [DOI] [PubMed] [Google Scholar]
- Faraone SV (2000). Genetics of childhood disorders: XX. ADHD, part 4: Is ADHD genetically heterogeneous? Journal of the American Academy of Child & Adolescent Psychiatry, 39, 1455–1457. [DOI] [PubMed] [Google Scholar]
- Flory K, & Lynam DR (2003). The relation between attention deficit hyperactivity disorder and substance abuse: What role does conduct disorder play? Clinical Child and Family Psychology Review, 6, 1–16. [DOI] [PubMed] [Google Scholar]
- Flory K, Molina BSG, Pelham WE, Gnagy E, & Smith B (2006). Childhood ADHD predicts risky sexual behavior in young adulthood. Journal of Clinical Child and Adolescent Psychology, 35, 571–577. [DOI] [PubMed] [Google Scholar]
- Gadow KD, & Nolan EE (2002). Differences between preschool children with ODD, ADHD, and ODD+ ADHD symptoms. Journal of Child Psychology and Psychiatry, 43, 191–201. [DOI] [PubMed] [Google Scholar]
- Garon N, & Moore C (2004). Complex decision-making in early childhood. Brain and Cognition, 55, 158–170. [DOI] [PubMed] [Google Scholar]
- Garzon DL, Huang H, & Todd RD (2008). Do attention deficit/hyperactivity disorder and oppositional defiant disorder influence preschool unintentional injury risk? Archives of Psychiatric Nursing, 22, 288–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geurts HM, van der Oord S, & Crone EA (2006). Hot and cool aspects of cognitive control in children with ADHD: Decision-making and inhibition. Journal of Abnormal Child Psychology, 34, 813–824. [DOI] [PubMed] [Google Scholar]
- Gomez R (2003). Underlying processes in the poor response inhibition of children with attention-deficit/hyperactivity disorder. Journal of Attention Disorders, 6, 111–122. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP (2003). Impulsivity, emotion regulation, and developmental psychopathology: Specificity versus generality of link-ages. In King JA, Ferris CF, & Lederhendler II (Eds.), Roots of mental illness in children (pp. 149–159). New York: New York Academy of Sciences. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, & Lee SS (2003). Conduct and oppositional defiant disorders. In Mash EJ & Barkley RA (Eds.), Child psychopathology (2nd ed., pp. 144–198). New York: Guilford. [Google Scholar]
- Hinshaw SP, Lahey BB, & Hart EL (1993). Issues of taxonomy and comorbidity in the development of conduct disorder. Development and Psychopathology, 5, 31–49. [Google Scholar]
- Hinshaw SP, March JS, Abikoff H, Arnold LE, Cantwell DP, Conners CK, et al. (1997). Comprehensive assessment of childhood Attention-Deficit Hyperactivity Disorder in the context of a multisite, multimodal clinical trial. Journal of Attention Disorders, 1, 217–234. [Google Scholar]
- Humphreys KL, Mehta N, & Lee SS (2011). Association of parental ADHD and depression with externalizing and internalizing dimensions of child psychopathology. Journal of Attention Disorders, (in press). http://jad.sagepub.com/content/early/2010/10/31/1087054710387264.long. [DOI] [PMC free article] [PubMed]
- Jessor R (1998). New perspectives on adolescent risk behavior Cambridge, England: Cambridge University Press. [Google Scholar]
- Kochanska G, & Aksan N (2006). Children’s conscience and self-regulation. Journal of Personality, 74, 1587–1617. [DOI] [PubMed] [Google Scholar]
- Kroes G, Veerman JW, & De Bruyn EEJ (2003). Bias in parental reports? Maternal psychopathology and the reporting of problem behavior in clinic-referred children. European Journal of Psychological Assessment, 19, 195–203. [Google Scholar]
- Kuhne M, Schachar R, & Tannock R (1997). Impact of comorbid oppositional or conduct problems on attention-deficit hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 1715–1725. [DOI] [PubMed] [Google Scholar]
- Kuntsi J, Oosterlaan J, & Stevenson J (2001). Psychological mechanisms in hyperactivity: I response inhibition deficit, working memory impairment, delay aversion, or something else? Journal of Child Psychology and Psychiatry, 42, 199–210. [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Barkley RA, Garfinkel B, McBurnett K, Kerdyk L, et al. (1994a). DSM-IV Field Trials for oppositional defiant disorder and conduct disorder in children and adolescents. The American Journal of Psychiatry, 151, 1163–1171. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, McBurnett K, Biederman J, Greenhill L, Hynd GW, et al. (1994b). DSM-IV Field Trials for attention deficit hyperactivity disorder in children and adolescents. The American Journal of Psychiatry, 151, 1673–1685. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Waldman ID, & McBurnett K (1999). Annotation: The development of antisocial behavior: An integrative causal model. Journal of Child Psychology and Psychiatry, 40, 669–682. [PubMed] [Google Scholar]
- Lee SS, Lahey BB, Owens EB, & Hinshaw SP (2008). Few preschool boys and girls with ADHD are well-adjusted during adolescence. Journal of Abnormal Child Psychology, 36, 373–383. [DOI] [PubMed] [Google Scholar]
- Lee SS, Humphreys KL, Flory K, Liu R, & Glass K (2011). Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: A meta-analytic review 31, 328–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez CW, Read JP, Kahler CW, Richards JB, Ramsey SE, Stuart GL, et al. (2002). Evaluation of a behavioral measure of risk-taking: The Balloon Analogue Risk Task (BART). Journal of Experimental Psychology. Applied, 6, 75–84. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Aklin WM, Jones HA, Richards JB, Strong DR, Kahler CW, et al. (2003). The Balloon Analogue Risk Task (BART) differentiates smokers and nonsmokers. Experimental and Clinical Psychopharmacology, 11, 26–33. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Bornovalova M, Daughters SB, & Curtin JJ (2005). Differences in impulsivity and sexual risk-taking behavior among inner-city crack/cocaine and heroin users. Drug and Alcohol Dependence, 77, 169–175. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Aklin W, Daughters S, Zvolensky M, Kahler C, & Gwadz M (2007). Reliability and validity of the youth version of the balloon analogue risk task (BART-Y) in the assessment of risk taking behavior among inner-city adolescents. Journal of Clinical Child and Adolescent Psychology, 36, 106–111. [DOI] [PubMed] [Google Scholar]
- Lilienfeld SO, & Waldman ID (1990). The relation between childhood attention-deficit hyperactivity disorder and adult antisocial behavior reexamined: The problem of heterogeneity. Clinical Psychology Review, 10, 699–725. [Google Scholar]
- Loeber R, Burke JD, Lahey BB, Winters A, & Zera M (2000). Oppositional defiant and conduct disorder: A review of the past 10 years, part I. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 1468–1484. [DOI] [PubMed] [Google Scholar]
- Loeber R, Burke J, & Pardini DA (2009). Perspectives on oppositional defiant disorder, conduct disorder, and psychopathic features. Journal of Child Psychology and Psychiatry, 50, 133–142. [DOI] [PubMed] [Google Scholar]
- MacPherson L, Magidson JF, Reynolds EK, Kahler CW, & Lejuez CW (2010). Changes in sensation seeking and risk taking propensity predict increases in alcohol use among early adolescents. Alcoholism, Clinical and Experimental Research, 34, 1400–1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann L, Harmoni R, & Power C (1989). Adolescent decision-making: the development of competence. Journal of Adolescence, 12, 265–278. [DOI] [PubMed] [Google Scholar]
- Masunami T, Okazaki S, & Maekawa H (2009). Decision-making patterns and sensitivity to reward and punishment in children with attention-deficit hyperactivity disorder. International Journal of Psychophysiology, 72, 283–288. [DOI] [PubMed] [Google Scholar]
- Matthys W, Van Goozen SHM, Snoek H, & Van Engeland H (2004). Response perseveration and sensitivity to reward and punishment in boys with oppositional defiant disorder. European Child & Adolescent Psychiatry, 13, 362–364. [DOI] [PubMed] [Google Scholar]
- Newcorn JH, Halperin JM, Jensen PS, Abikoff HB, Arnold LE, Cantwell DP, et al. (2001). Symptom profiles in children with ADHD: Effects of comorbidity and gender. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 137–146. [DOI] [PubMed] [Google Scholar]
- Newman JP (1987). Reaction to punishment in extraverts and psychopaths: Implications for the impulsive behavior of disinhibited individuals. Journal of Research in Personality, 21, 464–480. [Google Scholar]
- Nigg JT (2003). Response inhibition and disruptive behaviors: Toward a multiprocess conception of etiological heterogeneity for ADHD combined type and conduct disorder early-onset type. In King JA, Ferris CF, & Lederhendler II (Eds.), Roots of mental illness in children (pp. 170–182). New York: New York Academy of Sciences. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Hinshaw SP, Carte ET, & Treuting JJ (1998). Neuropsychological correlates of childhood attention-deficit/hyperactivity disorder: Explainable by comorbid disruptive behavior or reading problems? Journal of Abnormal Psychology, 107, 468–480. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Goldsmith HH, & Sachek J (2004). Temperament and attention deficit hyperactivity disorder: The development of a multiple pathway model. Journal of Clinical Child and Adolescent Psychology, 33, 42–53. [DOI] [PubMed] [Google Scholar]
- Ostrov JM (2006). Deception and subtypes of aggression in early childhood. Journal of Experimental Child Psychology, 93, 322–336. [DOI] [PubMed] [Google Scholar]
- Owens EB, Hinshaw SP, Lee SS, & Lahey BB (2009). Few girls with childhood attention-deficit/hyperactivity disorder show positive adjustment during adolescence. Journal of Clinical Child and Adolescent Psychology, 38, 132–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paloyelis Y, Asherson P, & Kuntsi J (2009). Are ADHD symptoms associated with delay aversion or choice impulsivity? A general population study. Journal of the American Academy of Child and Adolescent Psychiatry, 48, 837–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelham WE, Foster EM, & Robb JA (2007). The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. Journal of Pediatric Psychology, 32, 711–727. [DOI] [PubMed] [Google Scholar]
- Pleskac TJ (2008). Decision making and learning while taking sequential risks. Journal of Experimental Psychology. Learning, Memory, and Cognition, 34, 167–185. [DOI] [PubMed] [Google Scholar]
- Polanczyk G, Silva de Lima M, Horta BL, Biederman J, & Rohde LA (2007). The worldwide prevalence of ADHD: A systematic review and metaregression analysis. The American Journal of Psychiatry, 164, 942–948. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Ortengren A, Richards JB, & de Wit W (2006). Dimensions of impulsive behavior: Personality and behavioral measures. Personality and Individual Differences, 40, 305–315. [Google Scholar]
- Schaffer D, Fisher P, Lucas CP, Dulcan MK, & Schwab-Stone ME (2000). NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 28–38. [DOI] [PubMed] [Google Scholar]
- Schwebel DC, Speltz ML, Jones K, & Bardina P (2002). Unintentional injury in preschool boys with and without early onset of disruptive behavior. Journal of Pediatric Psychology, 27, 727–737. [DOI] [PubMed] [Google Scholar]
- Steinberg L (2007). Risk taking in adolescence: New perspectives from brain and behavioral science. Current Directions in Psychological Science, 16, 55–59. [Google Scholar]
- Steinberg L, & Scott ES (2003). Less guilty by reason of adolescence: Developmental immaturity, diminished responsibility, and the juvenile death penalty. American Psychologist, 58, 1009–1018. [DOI] [PubMed] [Google Scholar]
- Thompson AL, Molina BSG, Pelham W, & Gnagy EM (2007). Risky driving in adolescents and young adults with childhood ADHD. Journal of Pediatric Psychology, 32, 745–759. [DOI] [PubMed] [Google Scholar]
- Tom SM, Fox CR, Trepel C, & Poldrack RA (2007). The neural basis of loss aversion in decision-making under risk. Science, 315, 515–518. [DOI] [PubMed] [Google Scholar]
- van Bokhoven I, Matthys W, van Goozen SHM, & van Engeland H (2005). Prediction of adolescent outcome in children with disruptive behaviour disorders: A study of neurobiological, psychological and family factors. European Child & Adolescent Psychiatry, 14, 153–163. [DOI] [PubMed] [Google Scholar]
- Wåhlstedt C, Thorell LB, & Bohlin G (2009). Heterogeneity in ADHD: Neuropsychological pathways, comorbidity and symptom domains. Journal of Abnormal Child Psychology, 37, 551–564. [DOI] [PubMed] [Google Scholar]
- Wrase J, Kahnt T, Schlagenhauf F, Beck A, Cohen MX, et al. (2007). Different neural systems adjust motor behavior in response to reward and punishment. NeuroImage, 36, 1253–1262. [DOI] [PubMed] [Google Scholar]
- Youngstrom E, Izard C, & Ackerman B (1999). Dysphoria-related bias in maternal ratings of children. Journal of Consulting and Clinical Psychology, 67, 905–916. [DOI] [PubMed] [Google Scholar]


