Abstract
Background:
Minimally invasive thymectomy is fast becoming the preferred approach for myasthenia gravis and non-invasive thymoma. The most commonly employed approach for minimally invasive thymectomy is the lateral thoracic approach. Safe achievement of radical resection requires adequate visualisation of both the phrenic nerves along their entire course. In our experience, such visualisation is rather difficult with unilateral transthoracic approaches. We herein describe our technique and initial experience of 25 cases with subxiphoid robotic thymectomy (SRT) for myasthenia gravis with or without thymoma. To the best of our knowledge, this is the first such report from India.
Subjects and Methods:
We retrospectively analysed data of patients who underwent SRT at our centre from June 2017 to September 2018. Twenty-five consecutive patients were analysed, and demographic data, total duration of the procedure, console time, blood transfusion requirement, duration of chest drainage, length of hospital stay, pain score on post-operative day (POD) 1 and day of discharge and post-operative morbidity and mortality within 90 days were recorded.
Results:
A total of 25 patients underwent SRT. All our patients had myasthenia gravis with 4 of them having thymoma. There were 11 males and 14 females with mean age of 29.30 years (range 23–48). The mean console time was 102.85 min (range 88–120) while the mean total operative time was 199.14 (range 180–220). On first POD 1, visual analogue scale score average was 5, and at discharge, it was 2. There was no 30-day or 90-day mortality. All cases of thymoma had a complete R0 resection.
Conclusion:
Our experience suggests that subxiphoid approach offers a good operative view of the thymus in cervical region along with easy identification of bilateral phrenic nerves. Thus, SRT can be performed safely with comparable results.
Keywords: Minimally invasive thymectomy, robotic thymectomy, subxiphoid thymectomy, thoracoscopic thymectomy, thymectomy, thymoma
INTRODUCTION
Minimally invasive thymectomy is fast becoming the preferred approach for myasthenia gravis and non-invasive thymoma. Several methods have been described including transcervical, lateral transthoracic and lately subxiphoid approach. The most commonly employed approach for minimally invasive thymectomy is the lateral thoracic approach.[1,2,3,4]
The choice of approach is guided by the inclination of the surgical team towards the necessity of removal of the entire thymus gland along with all anterior and superior mediastinal fat between the two phrenic nerves from the thyrothymic ligaments in the root of neck to bilateral pericardiophrenic recess in all cases where myasthenia gravis is the indication. Studies show that ectopic thymus has a negative effect on outcomes thereby suggesting towards the need for extended thymectomy.[5]
Safe achievement of such radical resection requires adequate visualisation of both the phrenic nerves along their entire course. In our experience, such visualisation is rather difficult with unilateral transthoracic approaches.
We have been performing robotic radical thymectomy for non-thymomatous myasthenia gravis and thymoma through the left transthoracic approach for over a decade now. Although the visualisation of the right phrenic along its entire intrathoracic course along with inferior pericardial fat in the pericardiophrenic recess was possible in many, it was mostly difficult necessitating the need for a 5-mm thoracoscope on the right side through which the bedside surgeon could guide the console surgeon towards the right phrenic ensuring complete resection. To circumvent these limitations, we tried the trans-subxiphoid robotic approach popularised by Suda et al.[6,7,8,9] We herein describe our technique and initial experience of 25 cases with subxiphoid robotic thymectomy (SRT) for myasthenia gravis with or without thymoma and review the available literature. To the best of our knowledge, this is the first such report from India.
SUBJECTS AND METHODS
From June 2017 to September 2018, we prospectively collected data of 25 consecutive patients who underwent SRT at our centre. Patients with myasthenia gravis without thymoma or those with small (<4 cm in maximum dimension) non-invasive thymoma were taken up for the subxiphoid approach. Patients were carefully selected after adequate myasthenia control. The following parameters were recorded: demographic data, total duration of the procedure, console time, blood loss in procedure, duration of chest drainage, length of hospital stay, pain score on post-operative day (POD) 1 and at the day of discharge and post-operative morbidity and mortality within 90 days.
Surgical procedure: Subxiphoid robotic thymectomy
Patients were induced with general anaesthesia using a standard double-lumen endotracheal tube for lung isolation and subsequently placed in a supine sternotomy position. The left upper limb was placed off the edge of the table with the elbow and forearm supported on a bean bag. The right upper limb was placed on the table with slight abduction at shoulder and flexion at elbow supported on the table.
The left lung was selectively deflated, and two ports were placed in the left chest, one in the 4th intercostal place just behind anterior axillary line and another 8-mm robotic port for robotic arm 1 in the 6th intercostal space (ICS) anterior axillary line. CO2 insufflation was used at a pressure of 8 mmHg. Using these two ports, the mediastinal pleura in the region of xiphisternum was opened, and fat in the retrosternal area beneath the xiphoid process was mobilised away from the sternum. This was continued across the mediastinum up to the right mediastinal pleura, which was opened widely.
A 2-cm transverse incision was made about 2 cm below the xiphoid process. A 12-mm port was then placed under vision in the subxiphoid location. The 5-mm port in the 4th ICS was then used for camera, and the subxiphoid and the 5-mm port in 6th ICS were used to mobilise all the fat in the left inferior pericardiophrenic recess.
After complete mobilisation of left inferior pericardial fat, an 8-mm port was placed in the 6th ICS in anterior axillary line on the right side for robotic arm 2 [Figure 1a].
Figure 1.
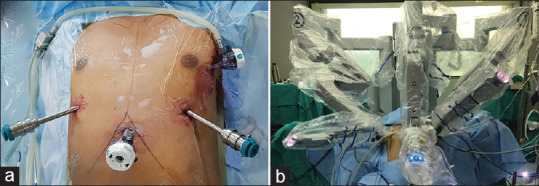
Port placement and docking for subxiphoid robotic thymectomy. (a) Port placement. (b) The patient cart being docked from over the patient's head
At this stage, the robotic arms were docked (robot being brought in from the head end) with camera in the subxiphoid port and arm 1 and 2, respectively, onto the left and right 8-mm ports [Figure 1b]. A bipolar Maryland forceps was attached to the right arm and Cadiere forceps was attached to the left arm. The mediastinal pleura on the either side was opened completely. The mobilisation of the right pericardial fat was initiated using robotic assistance, and an extended thymectomy was then performed removing all the fat and thymic tissue between the two phrenic nerves right up to the bilateral thyrothymic ligaments. Figure 2 shows the intraoperative view through the subxiphoid port through various stages of surgery.
Figure 2.
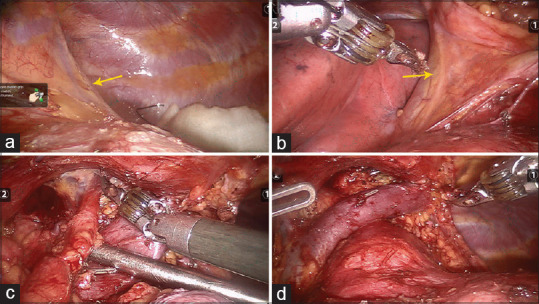
Intraoperative view of various stages of subxiphoid robotic thymectomy. (a) View of the left phrenic nerve (arrow). (b) View of the right phrenic nerve (arrow). (c) Dissection of the thymic horns. (d) View after completion of dissection displaying the left innominate vein
After procedure completion, the specimen placed in a specimen bag was retrieved through the subxiphoid port. A single drain was placed through the subxiphoid ports followed by closure of rest of the ports. All patients were extubated on table and shifted to post-operative recovery room.
RESULTS
A total of 25 patients underwent SRT. The demographic characteristics and surgical outcomes have been described in Table 1. All our patients had myasthenia gravis with 4 of them having thymoma. There were 11 males and 14 females with mean age of 29.30 (range 23–48). The mean console time was 102.85 min (range 88–120) while the mean total operative time was 199.14 (range 180–220). No patient required any blood transfusion. In all patients, the chest drain was removed on the first POD. The average hospital stay was 3 days (range 2–3 days). Intravenous analgesics were given for 2 days and oral painkillers were given for 10 days. Assessment of pain was done using the Visual Analogue Scale (VAS). On first POD 1, VAS score average was 5, and at discharge, it was 2. There was no mortality. All cases of thymoma had a complete R0 resection.
Table 1.
Demography and surgical outcomes of 25 patients who underwent subxiphoid robotic thymectomy
| Patient Variables | |
|---|---|
| Total number | 25 |
| Male: female | 11:14 |
| Average age (years) (range) | 29.3 (23-48) |
| Myasthenia gravis | 25 |
| Thymoma | 4 |
| Average size of thymoma (cm) (range) | 2.25 |
| Total duration of surgery (min) (range) | 199.14 (180-220) |
| Console time (min) (range) | 102.85 (88-120) |
| Blood transfusion | None |
| Average chest tube duration (days) | 1 |
| Average length of hospital stay (days) (range) | 2 (2-3) |
| Complication | None |
| Post-operative mortality 90 days | None |
DISCUSSION
Safe achievement of radical resection of entire thymus and all the mediastinal and pericardial fat requires adequate visualisation of both the phrenic nerves along their entire course. Such visualisation is usually rather difficult with unilateral transthoracic approaches. It is very difficult if not impossible to visualise the contralateral phrenic along the entire course. In most cases, the contralateral phrenic nerve can only be visualised with some difficulty in the upper half of its course. In our experience, if a right-sided transthoracic approach is employed for thymectomy, the visualisation of the left phrenic nerve is even more tedious.
We have been performing robotic radical thymectomy through the left transthoracic approach for over a decade now. Although we were able to perform a complete radical thymectomy as described above in all our cases, visualisation of contralateral fat pad and the phrenic nerve in its inferior extent necessitated use of a 5-mm thoracoscope on the contralateral side in a significant majority of our cases to ensure the radicality of the resection as well as preservation of the contralateral nerve. Moreover, the proper visualisation of the root of the neck and region of the thymic horns appeared somewhat compromised in some cases. To improve visualisation of the horns, the camera port needed to be placed more medially and inferiorly, which compromises the position of the other two robotic ports and makes dissection of inferior pericardial fat in the pericardiophrenic recess more tedious.
These difficulties prompted us to try the subxiphoid approach which was first reported by Suda et al.[6] They reported that this approach provides a good operative vision in the in the region of thymic horns along with excellent visualisation of bilateral phrenic nerves, which is expected because of the camera being in the subxiphoid location. We assessed the feasibility of this novel technique with slight modification. In our initial experience, we realised that while excellent visualisation of the region of thymic horns and bilateral phrenic nerve is achieved, the visualisation of inferior pericardiophrenic recess along with the pericardial fat, particularly on the left side, was very limited pushing us to mobilise the left inferior pericardial fat thoracoscopically at the start of the procedure with three ports (two ports in the left pleural cavity and one subxiphoid port) as described above. Thus, we were able to achieve an outstandingly radical resection in all our cases. We believe this approach is more suited for minimally invasive thymectomy compared to lateral thoracic approaches in view of the obvious anatomic advantages as mentioned by Suda.[7]
Our operative and console time were comparable to Suda et al.,[6] and the procedure could be completed without the need for conversion in all our cases. Although larger data are required to make any recommendations, this procedure is feasible and can be safely performed. This study is not a comparative one between conventional robotic and subxiphoid approach, but some early differences that we observed are outlined below. First, the dissection of the superior horns was far simpler than in lateral transthoracic approach due to a direct line of vision. Secondly, for the patient, it appears to be less painful possibly due to the placement of chest tube in the subxiphoid location, which avoids the ICS and the resultant pain. However, the creation of the subxiphoid port is technically more demanding but can be adapted over time.
To the best of our knowledge, this is the first report from India of the use of the da Vinci Surgical System through the subxiphoid route for performing minimally invasive thymectomy.
CONCLUSION
Our experience suggests that subxiphoid approach offers a good operative view of the thymus in the cervical region along with easy identification of bilateral phrenic nerves. This combined with the articulated endowrist movements of the surgical robot makes the surgery easier. Thus, robotic subxiphoid thymectomy can be performed safely with comparable results.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Landreneau RJ, Dowling RD, Castillo WM, Ferson PF. Thoracoscopic resection of an anterior mediastinal tumor. Ann Thorac Surg. 1992;54:142–4. doi: 10.1016/0003-4975(92)91162-3. [DOI] [PubMed] [Google Scholar]
- 2.Sugarbaker DJ. Thoracoscopy in the management of anterior mediastinal masses. Ann Thorac Surg. 1993;56:653–6. doi: 10.1016/0003-4975(93)90942-b. [DOI] [PubMed] [Google Scholar]
- 3.Cooper JD, Al-Jilaihawa AN, Pearson FG, Humphrey JG, Humphrey HE. An improved technique to facilitate transcervical thymectomy for myasthenia gravis. Ann Thorac Surg. 1988;45:242–7. doi: 10.1016/s0003-4975(10)62457-5. [DOI] [PubMed] [Google Scholar]
- 4.Kido T, Hazama K, Inoue Y, Tanaka Y, Takao T. Resection of anterior mediastinal masses through an infrasternal approach. Ann Thorac Surg. 1999;67:263–5. doi: 10.1016/s0003-4975(98)01210-7. [DOI] [PubMed] [Google Scholar]
- 5.Ponseti JM, Gamez J, Vilallonga R, Ruiz C, Azem J, López-Cano M, et al. Influence of ectopic thymic tissue on clinical outcome following extended thymectomy in generalized seropositive nonthymomatous myasthenia gravis. Eur J Cardiothorac Surg. 2008;34:1062–7. doi: 10.1016/j.ejcts.2008.07.049. [DOI] [PubMed] [Google Scholar]
- 6.Suda T, Tochii D, Tochii S, Takagi Y. Trans-subxiphoid robotic thymectomy. Interact Cardiovasc Thorac Surg. 2015;20:669–71. doi: 10.1093/icvts/ivv001. [DOI] [PubMed] [Google Scholar]
- 7.Suda T. Robotic subxiphoid thymectomy. J Vis Surg. 2016 Jul 22;:2–118. doi: 10.21037/jovs.2016.07.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Suda T. Subxiphoid thymectomy: Single-port, dual-port, and robot-assisted. J Vis Surg. 2017;3:75. doi: 10.21037/jovs.2017.05.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suda T, Kaneda S, Hachimaru A, Tochii D, Maeda R, Tochii S, et al. Thymectomy via a subxiphoid approach: Single-port and robot-assisted. J Thorac Dis. 2016;8:S265–71. doi: 10.3978/j.issn.2072-1439.2016.02.34. [DOI] [PMC free article] [PubMed] [Google Scholar]


