Abstract
The control of infectious disease is more dependent on prevention than on treatment.
The first task is to isolate the source of infection. Suspected patients, mildly affected patients, and close contacts of confirmed cases should be placed under medical observation. No matter whether there is an etiological diagnosis or not, suspected patients should be kept in strict isolation. It is difficult to identify the source of infection completely unless compulsory measures are taken, such as door-to-door screening. Therefore, the focus of prevention is how to cut off the transmission routes. Given that droplet transmission and contact transmission appear to be the main routes of transmission of COVID-19, the general public need to refrain from going outdoors as much as possible, wear masks in public, and keep good hygiene including frequent handwashing, and wiping and disinfecting door handles and elevator buttons. It is recommended to stop using central air-conditioning because COVID-19 may also spread through aerosol transmission.
Keywords: COVID-19, Novel coronavirus infected pneumonia, Masks, Gloves, Goggles, Hand hygiene
1. Principles
The control of infectious disease is more dependent on prevention than on treatment.
The first task is to isolate the source of infection. Suspected patients, mildly affected patients, and close contacts of confirmed cases should be placed under medical observation. No matter whether there is an etiological diagnosis or not, suspected patients should be kept in strict isolation. It is difficult to identify the source of infection completely unless compulsory measures are taken, such as door-to-door screening. Therefore, the focus of prevention is how to cut off the transmission routes. Given that droplet transmission and contact transmission appear to be the main routes of transmission of COVID-19, the general public need to refrain from going outdoors as much as possible, wear masks in public, and keep good hygiene including frequent handwashing, and wiping and disinfecting door handles and elevator buttons. It is recommended to stop using central air-conditioning because COVID-19 may also spread through aerosol transmission.
2. Use of personal protective equipment
2.1. Selection of PPE
Medical personnel should take adequate measures to prevent nosocomial infection, which not only protects them, but also better protects patients. On January 26, the National Health Commission of the People's Republic of China issued the Guide of Common Medical Protective Equipment in Novel Coronavirus Infected Pneumonia (Trial).
While coping with infectious diseases transmitted by droplets, use masks at the medical protection level. First of all, the waterproof coating of the mask is key: the common antismog and antidust face masks perform relatively poorly for waterproof functions. In addition, pay attention to the filtering capacity and sealing performance of the mask. Based on the abovementioned factors, patients should use medical surgical masks; medical staff must use medical protective masks when they enter quarantine areas.
The impermeability of protective clothing should also be emphasized and double-layer protection used when necessary. The latest research suggests that, besides droplet and contact transmission, it is possible for COVID-19 to spread through the fecal-oral route, and therefore the protection requirement is considered to be higher. Because there may be aerosol transmission, it is necessary to have a full three-dimensional and omnidirectional protection in high-risk areas, including goggles and face masks.
Medical staff should evaluate the risk level according to their positions, and then use a corresponding level of protection. Higher risk operations require higher levels of protective equipment. High-risk operations contain operations that involve contact with patients’ blood, body fluids, secretions, etc., or operations that may generate aerosols, such as performing tracheal intubation and bronchoscopy, collecting pharyngeal swabs, suctioning sputum, and giving oral nursing. Medium-risk operations refer to direct contact with the patient without performing the abovementioned high-risk operations, and include physical examination, injection, puncture, etc. While conducting medium-risk operations, the protection of medical personnel must include work clothes, gowns, caps, goggles, and medical surgery masks or medical protective masks. Low-risk operations consist of operations that only involve indirect contact with patients and enable personnel to keep a certain distance from the patient, such as prescription of drugs to patients and interviewing patients (where no physical examination is required).
2.2. Use of masks
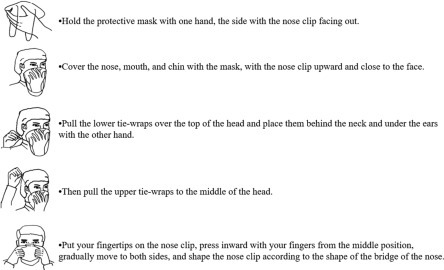
Whether it is a medical surgical mask or a medical protective mask, it is particularly important to wear it correctly. Fig. 6.1 shows how to wear a medical surgical mask. Medical surgical masks can block particles larger than 5 μm, so can curb the spread of droplets. The medical surgical mask is disposable, and its effective protection time is 4 h, which can be extended slightly. The mask must be replaced immediately once contaminated.
Fig. 6.1.

Wearing methods of medical surgical masks.
Fig. 6.2 shows the method of wearing a medical protective mask. In addition to the five steps listed above, there is an essential sixth step: perform a marginal tightness check after wearing the mask as shown in the figure. Although medical protective masks can block particles as small as 0.3 μm, if we just put on the mask but do not wear it well, particles of 3, 10, or even 30 μm will go in; then it is equivalent of wearing no mask.
Fig. 6.2.
Wearing method of medical protective mask.
Some medical personnel wear a surgical mask inside a medical protective mask. This is not permitted, as it will reduce the effectiveness of the protective mask by diminishing the tightness of the protective mask. If you intend to keep using the medical protective mask for a period of time while leaving the contaminated area, you could wear a surgical mask outside the medical protective mask. When you leave the contaminated area, remove the surgical mask and continue to use the inner protective mask. If this is not the case, there is no need to wear a surgical mask outside the medical protective mask. Hand hygiene is required after removing the mask.
2.3. Use of gloves
Common examination gloves are relatively easy to damage and difficult to fix. When we enter high-risk areas, it is better to wear two or even three layers of surgical gloves. However, wearing gloves cannot replace hand hygiene. When taking off protective equipment, hand hygiene should be performed at each step and between each layer. Do not touch unnecessary positions and items after putting on latex gloves, otherwise it will cause the spread of pollution.
2.4. Use of goggles and protective face shields/face screens
The use of goggles and protective face shields/face screens is necessary when performing operations involving splashing of body fluids, blood, etc., as these can protect the eye mucosa. These kinds of protective equipment are generally reusable as long as we ensure that the disinfection procedure meets the requirements. It is forbidden to leave the diagnosis and treatment area while wearing goggles and protective face shields. The three objects do not need to be used at the same time.
2.5. Use of gowns and protective clothing
In terms of gowns and protective clothing, appropriate protective equipment should be used according to the exposure risk of different working environments. Correct wearing technique, and especially correct undressing, is extremely important. It is critical to take PPE off in a standardized way and prevent pollution during this process. What is more, you should not leave the isolation ward while wearing medical protective clothing. In addition, shoe covers should be used in specified areas only. Shoe covers are required when entering a contaminated area from a semicontaminated area, as well as when entering a negative pressure ward from a buffer area. Conversely, shoe covers should be removed when entering a partially contaminated area from the contaminated area or entering into the buffer area from the negative pressure ward. It is absolutely forbidden to walk around casually with shoe covers.
2.6. The procedure for wearing protective articles when entering and leaving the isolation ward is as follows
Hand hygiene is required before putting on a mask when entering a contaminated area from the access area for medical personnel. Medical staff must only enter the isolation ward wearing PPE. About four times of hand hygiene are compulsory to be done when you leave the contaminated area to enter a clean zone. Currently, the requirement of so many times of hand hygiene might bother medical staff because the repetition is fussy. However, hand hygiene is of great importance to ensure the safety and an easy way to lessen the risk of infection. Therefore, certain times of hand hygiene are necessary, and it must perform qualified hand hygiene each time.
3. Nosocomial infection control
The phenomenon of nosocomial infection breaking out and a large number of medical care personnel becoming infected is related to the outbreak of community-acquired infection along with the failure in prevention and control of nosocomial infection. The confidence of governments and society in the control of the epidemic will be greatly undermined if patients get cross-infected or medical staff get infected in medical institutions.
The National Health Commission, on January 22, 2020, issued the Technical Guide for Prevention and Control of Novel Coronavirus Infected Pneumonia in Medical Institutions (First Edition) (hereafter this text will be abbreviated as Guide). This is divided into four parts, and the first part is the basic requirements.
There are 10 basic requirements for prevention and control of the novel coronavirus infected pneumonia in medical institutions.
(1) Formulate an emergency plan and workflow. Medical institutions at all levels are required to formulate an emergency plan and workflow for novel coronavirus infected pneumonia.
(2) Train all staff. In addition to medical staff, management, logistical, property, and cleaning personnel should also receive training to be aware of the emergency plan and workflow, and know how to prevent and control the epidemic. The personnel in nonhigh-risk departments should particularly take this training seriously and use standard precautions.
(3) Enhance occupational protection of medical staff. Some medical staff have become infected while this plan was being made, which is related to treatment operations or inadequate protection in hospitals. Therefore, medical institutions should standardize the work of disinfection, quarantine, and protection, and stock up on protective equipment. The Guide particularly emphasizes strengthening the control of contact, droplet, and air transmission based on the strict implementation of standard prevention. The correct selection and wearing of masks and hand hygiene are key measures to contain the epidemic. As a respiratory infectious disease, SARS-Cov-2 cannot cause infection until it enters the respiratory tract through droplets or aerosols. Nothing is more important than the mask—a firewall in front of the mouth and nose. As COVID-19 can spread through close contact, hand hygiene is particularly necessary. Hand hygiene is required when you want to touch any part of your body with your hands. The basic method of hand hygiene is to wash your hands with running water and hand sanitizer or to wipe your hands with instant hand sanitizer. Washing hands effectively cannot be finished in a few seconds and should continue for about 40 s; otherwise the hands will not be washed thoroughly. Quick hand disinfecting needs to last for 15–20 s, and can be achieved only with adequate instant sanitizer.
(4) Pay attention to the health of medical personnel. ① Deploy human resources and arrange shifts reasonably to avoid overwork of medical staff. Alternate work with rest and recreation, and ensure sufficient sleep. ② Provide a nutritious diet to enhance the immune systems of medical staff. ③ Carry out active health monitoring based on staff's characteristics of post and corresponding risk assessment results, including body temperature and respiratory symptoms. Pay attention to the prevention of colds and infection, and improve fitness. Medical staff displaying symptoms such as fever and cough must receive immediate medical treatment, and not work while they are experiencing illness. ④ Take appropriate measures to ensure that medical staff provide medical services to patients safely. More than 3000 medical staff have been infected with COVID-19 in China, which mainly occurred in the early stages of the outbreak, for a number of reasons: lack of understanding of this emerging infectious disease; failure to identify infection early, inadequate knowledge of self-protection; improper use of protective equipment, busy work; and so on. Among these infections, some were caused by household clustering, some were from other community environments, and some were nosocomial.
The following matters need attention: ① Behavioral quarantine is tantamount to or even more important than PPE. Every detail counts. ② Put on and take off PPE in appropriate areas. Do not walk around in contaminated PPE. ③ Post the protocol of putting on and taking off PPE on the wall, and equip a full-length mirror. ④ Ensure hand hygiene by supplying sufficient instant hand sanitizer. Wash hands before leaving wards or eating meals. Do not touch your face with your hands. ⑤ Check the tightness of masks. Wear the appropriate mask in different areas. ⑥ Open windows to provide ventilation.
(5) Strengthen the supervision of infection. Monitor the infection of medical staff and confirmed suffers.
(6) Carry out the management of cleaning and disinfection. ① Strengthen the ventilation of diagnosing and treating environment according to the Management Standards of Air Purification in Hospital. Medical institutions should disinfect air or be equipped with air purifiers if possible. ② Implement the technical standards of disinfection in medical institutions strictly. Clean and disinfect the environment of diagnosis and treatment (including air, object surfaces, ground, etc.), medical devices, patients' items, patients' secretions and vomit, etc. Take scientific disinfection measures, and devise a precise strategy according to the relevant laws and regulations to cut off transmission routes and eventually contain the epidemic. Meanwhile, excessive disinfection should be prohibited, because it not only fails to increase the effect of disinfection, but also threatens public health.
(7) Strengthen the management of patients to avoid cross infection.
(8) Enhance the health education of patients, including the use of masks, hand hygiene, and the practice of social distancing.
(9) Strengthen the management of infection outbreak.
(10) Strengthen the management of medical waste. Contaminated masks, gloves, shoe covers, caps, gowns, and protective clothing should be put in the right places. Do not discard or scatter medical waste during its transportation.
In terms of key hospital departments, there are four main departments. The first department is the fever clinic where standard prevention, hand hygiene, timely detection (diagnosis) of cases, layout, division, and ventilation should be given attention. The second is the emergency department in which, besides layout, division, and ventilation, there are two points of importance: ① preliminary checking and differentiating diagnosis (direct fever patients to the fever clinic for medical consultations) and ② standard prevention. The third is the general ward, in which standard prevention is the most important. The medical staff must wear masks and practice hand hygiene correctly, otherwise they might become close contacts or infected. Moreover, infected patients must be identified in a timely fashion. The fourth department is the isolation section, in which suspected or confirmed patients with COVID-19 are received and treated. Here, layout, division, ventilation, and work schedule are of great importance. There should be three areas and two passages: a clean area, a partially contaminated area, and a contaminated area; and a corridor for patients and a passage for medical staff. Substantial barriers are required between the three areas. The air current direction should be from the clean area to the contaminated area. The negative pressure room should comply with relevant regulations, if any. Two further points must be noted: ① suspected cases must be isolated in a single room and ② confirmed cases can share a room.
The protocol and pier glass are required while wearing and taking off PPE. Medical staff should supervise and guide each other in order to improve together and protect themselves better.
3.1. Collecting and processing laboratory samples of patients with suspected COVID-19
Generally, there are two aspects. ① All laboratory samples should be considered to be potentially infectious, including blood, lavage fluid, nasopharyngeal swabs, and other body fluids. ② The medical personnel who collect, process, and transport any clinical samples should strictly abide by the following standard control measures and biosafety operations to minimize the possibility of exposure to the pathogens.
Standard control measures and biosafety operations:
-
(1)
Ensure the medical personnel who collect samples use appropriate PPE (such as protective glasses, medical masks, protective clothing with long sleeves, gloves, etc.). If aerosol might be generated in the process of collection, such as the collection of alveolar lavage fluid and sputum aspiration, the collector should wear a special mask (NIOSH-certified N95 respirator or mask achieving EU-certified FFP2 standards, or mask at equivalent protective level).
-
(2)
Ensure all personnel responsible for transporting samples are trained on the safety operation procedures and leakage disposal, which are hard to achieve in most medical institutions due to their wide coverage.
-
(3)
The delivered sample should be placed in a leak-proof sample bag (i.e., a secondary container), which is a separate sealed sample bag (i.e., a plastic biohazard sample bag). During transportation, the secondary container should be placed in a sample container (i.e., a primary container) marked with the patient's information and attached with a clearly written laboratory examination application form.
-
(4)
The laboratory in medical institutions must comply with the corresponding biosafety operation specifications and transportation requirements for different types of biological samples. For example, if the standard operation is not performed for samples possibly containing the virus, it is very likely to cause cross infection in the laboratory.
-
(5)
All samples should be delivered manually whenever possible. A pneumatically driven pipeline system should not be used to deliver samples, because if the sample is overturned in the delivery pipeline, cross infection might happen in the hospital.
-
(6)
The full name and date of birth of each patient and the warning “suspected novel coronavirus infection” must be clearly recorded on the laboratory examination application form.
Finally, once the sample is delivered, notify the laboratory as soon as possible to avoid sending samples to the wrong places and prevent problems during the process of delivery.
To strengthen the management of patients, the following aspects should be dealt with carefully:
-
(1)
Suspected or confirmed patients should be isolated in good time and guided to the isolation area through the specified standard route by related staff.
-
(2)
The patient should put on a hospital gown before entering the wards. Their items and clothes should be stored in a designated place and kept by the medical institution after being disinfected.
-
(3)
Educate patients to choose and wear masks, and to follow coughing etiquette and ensure hand hygiene correctly.
-
(4)
Strengthen the management of persons who visit or accompany patients. (For example, each hospitalized patient is allowed to be accompanied by up to one family member; no other person is allowed to visit suspected or confirmed patients.)
-
(5)
For isolated patients, in principle, their activities should be limited to the isolation ward. If they need to leave the isolation ward or isolation area, they should wear medical surgical masks to prevent contaminating other patients or the environment.
-
(6)
When suspected or confirmed patients are discharged or transferred to another hospital, patients should change into clean clothes before leaving and their wards should be disinfected.
-
(7)
The bodies of deceased patients should be disposed of promptly. The method is: fill all open channels of the patients' body (mouth, nose, ears, anus, etc.) with 3000 mg/L chlorine disinfectant or 0.5% peracetic acid cotton ball or gauze, wrap the body with a double layer of cloth, and then put the body into a double-layer corpse bag and send the body directly to the designated place for cremation by specific vehicle. Personal belongings of patients during hospitalization could be cremated with the patient or taken home by their families after being disinfected.
4. Fangcang shelter hospitals/temporary treatment centers
Fangcang shelter hospitals are regarded as a key step at a critical moment. The establishment of Fangcang shelter hospitals is one of the important reasons why this epidemic has been controlled in China. Fangcang shelter hospitals contribute to the rapid examination and isolation of suspected cases and mildly affected patients, reducing the chance of human-to-human transmission in the community, and thus play a pivotal role in slowing down the increase of cases.
In the future, the construction of massive exhibition centers, gymnasiums, warehouses, and factories should leave interface and corresponding auxiliary space outside the interface, which are not used at ordinary times, but can be quickly transformed into a temporary treatment hospital in a short period of time when needed. The significance of Fangcang shelter hospitals is that in the national and even world emergency system, they can be constructed quickly to provide large numbers of medical beds and be operated at low cost. In terms of isolation, treatment, and supervision of patients with mild cases, measures such as Fangcang shelter hospitals also provide practical and significant experiences for other countries.
5. Disease control on a community level
Because there are neither corresponding vaccines nor specific drugs for COVID-19, currently the only effective measures to curb the epidemic are strict social prevention and control, such as the practice of social distancing, wearing masks, and washing hands frequently. If we had not taken strict measures, like the blockade of Wuhan, the situation in foreign countries would be worse right now, and there might be more than one “Wuhan” in China. The Chinese and English reports released by the Chinese expert group and the WHO expert group after the joint investigation clearly described China ’s experience of prevention and control, with particular emphasis on not placing obstacles to nucleic acid testing—carrying out testing for any possible cases.
Faced with the severe COVID-19 epidemic, only by getting ahead of prevention and control at the grassroots level can we finally reduce the number of confirmed cases, critically ill patients, and deaths. In this outbreak, the general hospital receives and treats critically ill patients, while screening suspected cases, managing discharged patients and close contacts at home or centralized isolation, and health education of patients is mainly implemented at the grassroots level. The division of labor between the grassroots and general hospitals played a critical role in curbing this outbreak.
Grassroots medical personnel mainly undertake the following tasks: preexamination and triage; timely detection, isolation, and referral of patients with fever and suspected cases; network management and carpet screening of the community; management of at-home or centralized quarantined patients; follow-up of discharged patients; strengthening education and guidance on the prevention and control of COVID-19; precise management of patients with chronic diseases (follow-up services, implementation of long prescriptions, substitute medicine-taken, home delivery services); and assisting other grassroots institutions in their work and giving professional guidance.
5.1. Use information and communication technology to get ahead of prevention and control
(1) Fully carry out registration, screening and reporting of community residents. Use direct reporting systems to support epidemic data filling and level-by-level statistics, focus on the coverage of suspected and confirmed cases, and continuously improve the efficiency and quality of data reporting. Use mobile apps, WeChat, and other forms to complete the registration of residents’ travel information and health status. Set up a “high-risk reminder” in the information system to focus on and track high-risk and suspected people, and master the regional control situation comprehensively and dynamically. Use the Internet information system to screen, prediagnose, and triage patients with fever, and immediately refer to the nearest higher-level hospital with fever clinic if necessary. The information should be reported promptly after completing registration.
(2) Implement the information registration and reporting of home observers: ① Patient management during medical observation. Use network resources to assist in tracking and supervising home medical watch of personnel from epidemic areas. Within 14 days of medical observation, monitor their health status through network systems. For example, patients or their family members can report personal changes in time in the form of “electronic patient log card” through WeChat, mobile app, network registration, or telephone. Community health workers conduct real-time monitoring and report abnormal situations promptly. ② Management of the elderly and patients with underlying disease. Gradually realize the “remote bed monitoring system.” Grassroots doctors use the internet to strengthen online precise management and services and focus on the “online health management” for the elderly and patients with chronic diseases such as hypertension and diabetes within their jurisdiction.
(3) Improve the efficiency of community health services with an intelligent voice system. Qualified communities can use the intelligent voice follow-up system to assist in various epidemic control work.
(4) Use “Internet +” to expand the scope of medical services: ① Online medical inquiry platform. Establish an online medical inquiry platform to provide consultation services for community residents. ② Online guide for medical attention. Construct an online platform which introduces the regional official registration platform: providing third-party services such as fever clinic inquiry and online registration to help residents conduct online self-assessment before visiting the fever clinic. If a resident has fever symptoms, they could also enquire about the fever clinic nearest to their home and patient-guiding services through the platform in advance.
(5) Construct the correct guidance of public opinion, dispel rumors, and create an online science education platform.
(6) Provide online courses for basic level medical staff.
5.2. Improve the effectiveness of diagnosis and treatment with information technology
(1) Realize remote diagnosis and treatment. Take advantage of major hospitals and build a multilevel interactive service platform for diagnosis and treatment. Major hospitals provide services such as remote consultation and prevention guidance, and utilize expert resources with information technology to improve the capacity to deal with epidemic situations of grassroots medical institutions, ease the pressure of diagnosis and treatment in designated hospitals, and reduce the risk of cross-regional transmission. Construct remote diagnosis and treatment service for digital images and form a daily procedure of “remote consultation of suspected cases.”
(2) Use a “medical consortium“ to promote multilevel linkage interaction. Use the “Internet +” information platform to form a medical consortium of third-level hospitals in the same area with second-level hospitals, community hospitals, and township health centers in order to strengthen the exchange and sharing of information between the primary medical units and each superior medical unit. Make full use of the “novel coronavirus infected pneumonia sharing platform” constructed by the state and the data platforms in various regions to promote the effective linkage of multilevel medical institutions.
5.3. Construction of prevention and control platform
(1) Screen suspected patients, understand transmission for infection, and find “super spreaders.” Collect and disseminate relevant information: the information of those who have been to the epidemic area, including the time of arrival in the epidemic area, the people contacted in the epidemic area, the way out of the epidemic area, and the places they have visited. Collect suspected symptoms: relevant residents upload their health status on the platform (whether they have fever, cough, expectoration, fatigue, diarrhea, and/or other symptoms). The abovementioned data can be conducive to screening suspected patients, understanding the transmission route, and finding super spreaders, which is of great significance for prevention and control of the epidemic.
(2) Cut off transmission routes and circumvent the source of infection. Through an epidemic map, in which the real-time locations of suspected and confirmed patients are shown, the public can avoid the source of infection on their own initiative.
6. Vaccine development
What if COVID-19 becomes a “long-standing disease”? This is a matter of great concern at home and abroad. The development of vaccines is complicated; however, vaccine is an indispensable means of epidemic prevention in the battle against a persistent communicable disease.


