Physician-scientists and trainees who are underrepresented minorities in medicine (URiMs) have navigated a daunting path to achieve the level they have reached, and face additional obstacles as they move forward in their careers. Their professional development is impacted by conscious and unconscious biases that create multiple hurdles to advancement, and even as progress is made, URiM achievements are not necessarily recognized in an equivalent manner to non-URiMs (1–4). Biases based on schemas and embedded stereotypes may prevent an opportunity, for example, to interview for a residency, fellow, or faculty position despite having a sound record of achievement, or may result in unfair evaluations that may affect future opportunities (5). Some preconceptions of ability are derived from the person’s racial or ethnic background, whereas others stem from past experiences of URiMs that were shaped by systemic structures of racism (socioeconomic status, job availability, etc.), which determined where they lived or the schools they attended (6, 7). For many URiMs, these biases, even small ones, accrue disadvantages over time and have a significant impact on future opportunity. URiMs either tolerate the structures and culture to achieve some level of growth in academic medicine or become overwhelmed and simply give up (1–3, 7, 8). Certainly, the numbers of URiMs in the pipeline for medical school, residency and fellowship, and academic faculty are adversely affected by current processes (5, 6, 9).
Challenges to the advancement of URiMs
All trainees at the resident and fellowship level want to learn and excel in their specialty to become independent practitioners, and URiM trainees are no different. Some URiMs and non-URiMs want to care for a diverse set of patients during their training to gain medical expertise across the entire scope of race and ethnicities (9); this aspect may drive match-list choice to avoid programs not perceived as providing care for a diverse patient population. URiM trainees may also experience direct patient biases particularly if a patient is not from the same racial or ethnic background (6, 7, 9). In most programs, there may be only one or a few trainees who are URiMs in the entire program, which can generate feelings of loneliness and isolation if there is no support network. URiMs are more likely to encounter microaggressions as a result of their race or ethnic background, some recognized and some not fully recognized initially by the trainee, that may affect performance (10). URiMs may not have role models with relatable experiences due to the dearth of URiMs among faculty.
URiM faculty members face similar challenges to those of trainees, with some additional barriers. Like URiM trainees, many physician-scientists want to take care of a diverse set of patients in their academic clinical practice and may face patient biases from those whose backgrounds are different. And like trainees, there are often very limited numbers of URiMs on a large faculty. As a young URiM faculty member, they may lack representative role models and mentors to help them mature (1, 6, 9). New challenges occur, such as being asked repeatedly to be representative on committees (the “minority faculty tax”) because there are so few URiMs on faculty — the intention of the institution might be sound for diverse representation, but incessant service undermines their clinical and research development maturation for future success and promotion (5, 6). As one of few URiMs on the faculty, they are expected to be the representative for any URiM student who comes through their unit; while the intention is good, this responsibility would be manageable if there were more URiM mentors to serve in this role (6). If the URiM faculty member is research oriented, they have a higher challenge (about 10% lower chance) in obtaining an NIH research project grant, a key piece of currency for promotion (11). As with trainees, microaggressions from colleagues and staff may occur, potentially undermining confidence and progress.
It is remarkable for URiM trainees and physician-scientists to complete and excel at their levels despite the additional challenges they may face. Seeing a URiM faculty member who has achieved full professor rank is unfortunately relatively rare, due to the systemic challenges and biased academic hurdles. In reality, more attention needs to be paid to URiM trainees and faculty to help them overcome challenges, and to succeed and fully contribute to trainee and faculty academic life. Socioeconomic inequities, student debt, family care and obligations, lack of role models, and lack of mentorship are disproportionately higher among URiMs (1, 5). In academia and elsewhere, diverse teams outperform homogeneous teams (12), and diverse research teams result in higher manuscript citations and impact over homogeneous teams (13). Most academic institutions strive for diversity to grow innovation; however, it has been very challenging to achieve high diversity with current constructs and processes.
Effective strategies for institutions to promote diversity
How can a department and institution promote diversity among its trainees and faculty? First, the institution and department must have the will to address diversity: leadership involvement and persistence is a key component. Without significant leadership backing, efforts often falter due to lack of support. Second, the institution and department need to assess where they are with diversity. This assessment can include demographic data as well as surveys of the faculty and trainees on the diversity culture. Third, task forces, committees, and leadership should craft a vision and mission statement on the importance of actively addressing diversity and subsequently develop a strategic plan informed by their earlier assessment. Fourth, the strategic plan must be implemented with clear communication, integrating the plan within divisions of the department and across departmental structures, to achieve lasting improvements in diversity.
Such a strategic plan, which is often led by someone highly committed to diversity, is typically a marathon rather than a sprint and requires continuous focus for broad execution. Contents of a diverse strategic plan will address culture and climate, inclusiveness (14), and approaches to recruitment (15). Tactics from the strategy can be developed to help execute the plan, and will include metrics in which to set goals for targets and can be part of an ongoing leadership dashboard, such as the percentage of diverse presenters at weekly grand round talks (16), which provides representation and potential role models for URiM trainees and faculty members. Such a strategic plan will likely take multiple “small” steps that accumulate, slowly changing culture and approaches to achieve improved diversity. Some steps will be easy, others may be very complex and hard. The commitment must be there if the department and institution want to succeed at diversity in all of their missions.
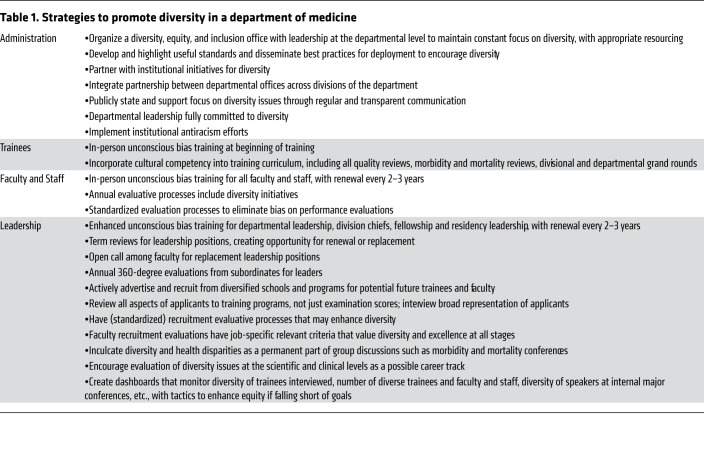
A diversity strategic plan needs to permeate through the department and institution. Administrative leadership, faculty, staff, and trainees affect the culture and thus must be involved in promoting a diverse culture. At my own institution and department, we commenced several years ago, providing in-person unconscious bias training for all trainees, staff, and faculty. Leaders responsible for recruitment at the faculty and trainee level underwent an enhanced and longer version of unconscious bias training. We added diversity components to our residency and fellowship core curricula. We added meaningful and actionable metrics to our leadership dashboard. We modified our evaluation processes of leaders and faculty to include diversity issues. Later, we created a diversity office overseen by a vice chair of the department, resourced with personnel and funds to disseminate best practices regarding diversity and to continuously obtain feedback for improvement. We encouraged and continually made adjustments to the trainee applicant processes. Several of these strategies and other items that we implemented regarding diversity are listed in Table 1.
Table 1. Strategies to promote diversity in a department of medicine.
Overcoming racial biases and microaggressions — changing the culture — takes focus, stamina, and continued will. In the era of coronavirus disease 2019 (COVID-19), which has disproportionately impacted minority racial and ethnic groups (17), subsequent societal consequences may provide new opportunities for recruitment of URiMs. Because of COVID-19–induced travel restrictions and avoidance of large gatherings, trainee recruitment will be conducted through virtual technologies for the near future. Academic departments can take this opportunity to broaden and increase the diversity of their interviews, as applicants are not limited by the financial costs of travel to specific programs.
Conclusions
We in academic medicine have worked hard for over 100 years to fulfill our stated tripartite mission of research, education, and clinical care. For academic medicine departments to continually improve upon those missions, I propose a fourth mission of diversity. The effort we put into the classic tripartite objectives involve mentorship, role models, training researchers and clinicians, encouragement for careers, and the provision of resources for success. The exact same items and hard work are needed for this fourth mission of diversity — as diversity will enhance the other three missions, enhance innovation, and increase scientific impact (13). Tailored mentorship is a critical piece to achieve diversity, and special attention to URiM trainees and faculty in this regard needs to be front and center for a department if they are to be successful (1, 3, 6, 8).
Acknowledgments
Supported by the US Public Health Service (R01 CA206010) and the A. Alfred Taubman Medical Research Institute of the University of Michigan. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of this manuscript.
Version 1. 09/29/2020
In-Press Preview
Version 2. 10/19/2020
Electronic publication
Version 3. 11/02/2020
Print issue publication
Footnotes
Conflict of interest: The author has declared that no conflict of interest exists.
Copyright: © 2020, American Society for Clinical Investigation.
Reference information: J Clin Invest. 2020;130(11):5626–5628. https://doi.org/10.1172/JCI144527.
References
- 1.Carethers JM. Diversification in the medical sciences fuel growth of physician-scientists. J Clin Invest. 2019;129(12):5051–5054. doi: 10.1172/JCI131589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carr PL, Palepu A, Szalacha L, Caswell C, Inui T. ‘Flying below the radar’: a qualitative study of minority experience and management of discrimination in academic medicine. Med Educ. 2007;41(6):601–609. doi: 10.1111/j.1365-2923.2007.02771.x. [DOI] [PubMed] [Google Scholar]
- 3.Oliver KB, Jr, Nadamuni MV, Ahn C, Nivet M, Cryer B, Okorodudu DO. Mentoring black men in medicine. Acad Med. doi: 10.1097/ACM.0000000000003685. doi: 10.1097/ACM.0000000000003685. [published online September 1, 2020]. [DOI] [PubMed] [Google Scholar]
- 4.Storage D, Horne Z, Cimpian A, Leslie SJ. The frequency of “brilliant” and “genius” in teaching evaluations predicts the representation of women and African Americans across fields. PLoS One. 2016;11(3):e0150194. doi: 10.1371/journal.pone.0150194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barber PH, Hayes TB, Johnson TL, Marquez-Magana L, 10,234 signatories Systemic racism in higher education. Science. 2020;369(6510):1440–1441. doi: 10.1126/science.abd7140. [DOI] [PubMed] [Google Scholar]
- 6.Carethers JM. Facilitating minority medical education, research, and faculty. Dig Dis Sci. 2016;61(6):1436–1439. doi: 10.1007/s10620-016-4057-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriquez JE, Campbell KM, Mouratidis RW. Where are the rest of us? Improving representation of minority faculty in academic medicine. South Med J. 2014;107(12):739–744. doi: 10.14423/SMJ.0000000000000204. [DOI] [PubMed] [Google Scholar]
- 8.Flores G, et al. Keys to academic success for under-represented minority young investigators: recommendations from the Research in Academic Pediatrics Initiative on Diversity (RAPID) National Advisory Committee. Int J Equity Health. 2019;18(1):93. doi: 10.1186/s12939-019-0995-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carethers JM, Quezada SM, Carr RM, Day LW. Diversity within US gastroenterology physician practices: the pipeline, cultural competencies, and gastroenterology societies approaches. Gastroenterology. 2019;156(4):829–833. doi: 10.1053/j.gastro.2018.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Torres MB, Salles A, Cochran A. Recognizing and reacting to microaggressions in medicine and surgery. JAMA Surg. 2019;154(9):868–872. doi: 10.1001/jamasurg.2019.1648. [DOI] [PubMed] [Google Scholar]
- 11.Nikaj S, Roychowdhury D, Lund PK, Matthews M, Pearson K. Examining trends in the diversity of the U.S. National Institutes of Health participating and funded workforce. FASEB J. 2018;32(12):6410–6422. doi: 10.1096/fj.201800639. [DOI] [PubMed] [Google Scholar]
- 12. Page SE. The Diversity Bonus: How Great Teams Pay off in the Knowledge Economy. Princeton University Press; 2017. [Google Scholar]
- 13.Al Shebli BK, Rahwan T, Woon WL. The preeminence of ethnic diversity in scientific collaboration. Nature Commun. 2018;9(1):5163. doi: 10.1038/s41467-018-07634-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coe IR, Wiley R, Bekker LG. Organisational best practices towards gender equality in science and medicine. Lancet. 2019;393(10171):587–593. doi: 10.1016/S0140-6736(18)33188-X. [DOI] [PubMed] [Google Scholar]
- 15.Dossett LA, Mulholland MW, Newman EA, Michigan Promise Working Group for Faculty Life Research Building high-performing teams in academic surgery: The opportunities and challenges of inclusive recruitment strategies. Acad Med. 2019;94(8):1142–1145. doi: 10.1097/ACM.0000000000002647. [DOI] [PubMed] [Google Scholar]
- 16.Boiko JR, Anderson AJM, Gordon RA. Representation of women among academic grand round speakers. JAMA Intern Med. 2017;177(5):722–724. doi: 10.1001/jamainternmed.2016.9646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carethers JM, Sengupta R, Blakey R, Ribas A, D’Souza G. Disparities in cancer prevention in the COVID-19 era. Cancer Prev Research. doi: 10.1158/1940-6207.CAPR-20-0447. doi: 10.1158/1940-6207.CAPR-20-0447. [published online September 17, 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]