Abstract
Introduction
The COVID-19 pandemic has had a significant impact on nursing practice in intensive care unit and consequently, on workload.
Objective
To assess the nurse-patient ratio required by COVID-19 patients and to identify the factors that influence nursing in this context.
Design
This study was a retrospective observational study that evaluated the ratio using the Nursing Activities Score (NAS).
Setting
Three Belgian French-speaking hospitals, including five ICUs. Patients included COVID-19 and non-COVID-19 patients.
Measurements and main results
The study included 95 COVID-19 patients and 1604 non-COVID-19 patients (control group) resulting in 905 and 5453 NAS measures, respectively. The NAS was significantly higher among the COVID-19 patients than in the control group (p = <0.0001). In the COVID-19 group, these higher scores were also observed per shift and uniformly across the three hospitals. COVID-19 patients required more time in the activities of monitoring and titration (χ2 = 457.60, p = <0.0001), mobilisation (χ2 = 161.21, p = <0.0001), and hygiene (χ2 = 557.77, p = <0.0001). Factors influencing nursing time measured by NAS in the COVID-19 patients were age <65 years old (p = 0.23), the use of continuous venovenous hemofiltration (p = 0.002), a high APACHE II score (p = 0.006) and patient death (p = 0.002). A COVID-19 diagnosis was independently associated with an increase in nursing time (OR = 4.8, 95% CI:3.6–6.4).
Conclusions
Patients hospitalised in the ICU due to COVID-19 require significantly more nursing time and need an average ratio of almost 1:1.
Keywords: Coronavirus, Nursing activities score, Workload, Intensive care unit
Implications for clinical practice.
-
•
The nurse per patient ratio should be adapted in ICU COVID-19 patients.
-
•
Factors significantly increase the nursing time, such a continuous venovenous hemofiltration, high APACHE II score and patient death; this must be taken into account when determining the nurse per patient ratio.
-
•
Further research in other countries is needed to confirm the impact of COVID-19 on intensive care nursing time.
Introduction
Since March 2020, following in the footsteps of China, Europe has been facing the COVID-19 pandemic, caused by the SARS-COV-2 virus (Cucinotta and Vanelli, 2020). In Belgium, the Hospital Emergency Plan (cessation of elective surgery and consultations, and reassignment of nurses to intensive care as well as COVID-19 units) was launched on March 13, 2020. The peak of the epidemic occurred around April 10, 2020, with the country having more than 1500 patients hospitalised in intensive care units (ICU), an increased capacity to 2000 ICU beds (Sciensano, n.d) and an excess mortality of 4.8% in patients over 65 years (Ioannidis et al., 2020).
COVID-19 ICU patients regularly require mechanical ventilation in the prone position or even extracorporeal membrane oxygenation (ECMO) (Elharrar et al., 2020, Grasselli et al., 2020). This significant increase in critically ill patients influences the nursing workload in the ICU (Lucchini et al., 2020) and optimal management of the nurse-patient (N:P) ratio is essential in order to ensure the quality and safety of care. Indeed, studies have demonstrated an association between inadequate N:P ratio and hospital mortality (Aiken et al., 2014, Margadant et al., 2020, Needleman et al., 2020, Neuraz et al., 2015). More specifically, in the ICU there is an association between an increase in N:P ratio and an increase in incidents and adverse events (Stone et al., 2007, Venier et al., 2014, West et al., 2009) and, an increase in nosocomial infections (Cimiotti et al., 2012, Daud-Gallotti et al., 2012, Jansson et al., 2019, Needleman et al., 2020). This association is explained by an increase in missing care when the N:P ratio is inadequate (Ball et al., 2018). Complications are more pronounced in the ICU than in conventional care units because of the critical and urgent nature of the organ support required (Ball et al., 2018).
In Belgium, a recent study in 16 Belgian hospitals, before the COVID-19 pandemic, demonstrated a significant gap between the N:P ratio suggested by the Nursing Activities Score (NAS) scale (1:1.5) and the ratio recommended by Belgian legislation (1:3) (Bruyneel et al., 2019). The impact of COVID-19 on the NAS was analysed in a preliminary Italian study of the first 15 patients admitted to the ICU. Significantly higher NAS was observed in the COVID-19 group (M = 84 ± 10), compared to the non-COVID-19 group (M = 63 ± 15) (Lucchini et al., 2020). However, this first study was carried out with a small cohort of patients, in a single ICU and for a limited time.
In this study, we used the NAS scale to compare the calculated N:P ratio, between COVID-19 patients and those without the virus in five ICUs in Belgium and analysed the factors that increased nursing time.
Materials and methods
Setting and patients
This was a retrospective observational study conducted in three hospitals in French-speaking Belgium and included five ICUs with a total of 42 mixed ICU beds (surgical and medical). These ICUs do not have ECMO, thus, patients in need of this therapy were transferred to a specialised centre. The five ICUs are located in the same Belgian province that was heavily impacted by the pandemic. The occupancy rate in these units was 100% and there was a need to refer patients to other hospitals for lack of beds. However, the five ICUs had no more COVID-19 patients after the end of May 2020. Patients admitted between September 2, 2019 and 16 March 2020 comprised of the non-COVID-19 group, and those admitted from 16 March 2020 through May 17, 2020 comprised of the COVID-19 group.
Diagnosis of COVID-19 was performed via Polymerase Chain Reaction (PCR) testing from a nasopharyngeal swab and/or a chest CT scan.
In Belgian ICU units, as determined by Belgian regulations, the N:P ratio is fixed (1:3) but external nurses from outside the ICU (e.g. from the operating room or consultation nurses) were required to increase staffing during the COVID-19 pandemic.
Instruments
The NAS scale represents 81% of nursing activities and is independent of the severity of the pathology. This retrospective scale, specific to intensive care, can be encoded by shift or by 24-hour period (Miranda et al., 2003). Each item representing a nursing activity is subject to a dichotomous variable (for 18 items) and multiple choice (5 items). The score is expressed as a percentage and ranges from 0% to 177%. This represents the proportion of nursing time required to provide patient care.
The NAS scale used in this study has previously been translated for use in Belgium (Bruyneel et al., 2018) and the NAS calculation follow the guidelines published in 2015 (Padilha et al., 2015). The score was encoded in Epimed Monitor® at the end of each shift by nurses at the bedside. Nurses in the study units worked 12 hour shifts (night and day). All scores were encoded on admission and up until the time of discharge. The NAS is encoded as part of routine practice in the three hospitals. The NAS score per 24 hours was obtained by taking the maximum of each item recorded each (Miranda et al., 2003).
Statistical analyses
For comparisons of asymmetric variables, the Mann-Whitney (U) and Kruskal-Wallis (H) tests were used. For symmetric variables, Student’s T (t) test and the Chi-square test (χ2) were used for proportion comparisons. Statistical analyses were performed with Software for Statistics and Data Science (14.0, Texas). A p value < 0.05 was considered statistically significant. Mean and standard deviation (±) were used to describe symmetric variables and median (Mdn) and InterQuartile Range (IQR) were used to describe asymmetric variables.
Spearman’s rank-order (rho) correlation (r) was used to identify relationships between NAS score and age, length of stay, body mass index (BMI), Simplified Acute Physiology (SAPS) 3 scores and Acute Physiology and Chronic Health Evaluation (APACHE) II scores.
Multiple logistic linear regression analyses were performed in order to determine which of the independent variables would work as predictors of higher ICU nursing time. The factors chosen to perform the multivariate analysis were the data items encoded in the files routinely and already analysed in previous studies (Bruyneel et al., 2019, Padilha et al., 2008). We dichotomised (high or low values) the continuous variables by referring to either the median (e.g. NAS > 74.6%) or one of the international cut-offs for Body Mass Index (BMI). Odds ratio (OR) and 95% Confidence Intervals (IC) were used to describe the results.
Ethical considerations
A unique, anonymous number was randomly assigned for each patient and hospital institution included in the study. In addition, the company, Epimed Monitor®, signed confidentiality agreements with all the hospital departments. Finally, all of the hospital ethics committees were consulted and we obtained the authorisation of the local committees for the three hospitals (n°1348:096, 65,417,518 and 11-05-20-01). Due to the observational nature of the study and the anonymisation of the data, the written consent of patients or relatives was not required.
Results
Sociodemographic characteristics
The study included 95 patients with COVID-19 and 1604 patients without COVID-19 admitted to the ICU. The length of stay (U = 26.54, p = 0.0001), proportion of men (χ2 = 8.34, p = 0.004), e BMI (t = 15.7, p = 0.002), and duration of mechanical ventilation (U = −7.36, p = 0.0001) were significantly higher in the COVID-19 patients (Table 1 ). With regard to medical severity scores, no difference was observed between the two groups for the SAPS 3 (U = 1.08, p = 0.28) score and the APACHE II score (U = −2.16, p = 0.03). The death rate was higher (29 vs 11%) in the COVID-19 group. Finally, the most common reason for admission in the non-COVID-19 group were postoperative monitoring (25%), cardiogenic shock (15%), and sepsis (10%) (Table 1).
Table 1.
Sociodemographic characteristics of the patients.
| Characteristic | COVID patients (n = 95) | Non-COVID-19 patients (n = 1,604) | Test values | p value* | Total (n = 1,699) |
|---|---|---|---|---|---|
| Age-y, mean ± | 64.1 ± 16.2 | 63.0 ± 12.5 | t = 1,57 | 0.51 | 65.0 ± 16.0 |
| Men, n (%) | 66 (70) | 871 (54) | χ2 = 8.34 | 0.004 | 937 (55) |
| BMI - kg/m2, mdn (IQR) | 29.4 (7.4) | 26.7 (8.7) | t = −15,72 | 0.002 | 27.3 (8.5) |
| Length of stay - d, mdn (IQR) | 9 (16) | 2 (3) | U = −26,54 | <0.0001 | 2 (4) |
| APACHE II, mdn (IQR) | 17 (11) | 14 (16) | U = −2.16 | 0.03 | 14 (15) |
| SAPS 3, mdn (IQR) | 48 (21) | 46 (24) | U = 1.08 | 0.28 | 46 (24) |
| Readmission ICU, n (%) | 8 (8.4) | 87 (5.4) | χ2 = 3.52 | 0.06 | 95 (5.6) |
| Ventilated patients, n (%) | 62 (65) | 439 (27) | χ2 = 49.03 | <0.0001 | 501 (29) |
| Mechanical ventilation time-d, mdn (IQR) | 11 (15) | 2 (4) | U = −7.36 | <0.0001 | 2 (6) |
| Patients with CVVH, n (%) | 32 (34) | 82 (5) | χ2 = 116.97 | <0.0001 | 114 (7) |
| Type of admission n (%) | |||||
| Emergency | 30 (31) | 674 (42) | χ2 = 3.27 | 0.07 | 704 (41) |
| Ward | 65 (69) | 366 (23) | χ2 = 116.84 | <0.0001 | 431 (25) |
| Elective surgery | 0 | 473 (29) | – | 473 (27) | |
| Urgent surgery | 0 | 77 (5) | – | 77 (4) | |
| Destination, n (%) | |||||
| Deceased | 28 (29) | 188 (11) | χ2 = 19.40 | <0.0001 | 216 (13) |
| Ward | 55 (58) | 1254 (78) | χ2 = 384.54 | <0.0001 | 1309 (77) |
| Other hospital | 12 (12) | 122 (8) | χ2 = 113.49 | <0.0001 | 134 (8) |
| Home | 0 | 40 (2) | – | 40 (2) | |
| Reason for admission, n (%) | |||||
| Sepsis/Sepsis shock | – | 156 (10) | – | – | |
| Cardiogenic shock / cardiac decompensation | – | 241 (15) | – | – | |
| Hemorrhagic shock / severe hemorrhage | – | 108 (6) | – | – | |
| Trauma | – | 72 (5) | – | – | |
| De novo acute respiratory failure | – | 186 (11) | – | – | |
| Decompensation of chronic respiratory failure | – | 74 (5) | – | – | |
| Coma / convulsions | – | 110 (7) | – | – | |
| Acute renal failure | – | 105 (6) | – | – | |
| Acute liver failure | – | 33 (2) | – | – | |
| Cardiac arrest | – | 46 (3) | – | – | |
| Intoxication | – | 48 (4) | – | – | |
| Post-operative monitoring | – | 400 (25) | – | – | |
| Other | – | 25 (1) | – | – | |
Abbreviations: y = years, BMI = Body Mass Index, d = days, APACHE II = Acute Physiology And Chronic Health Evaluation, SAPS 3 = Simplified Acute Physiology Score, CVVH = Continuous VenoVenous Hemofiltration
*pvalue: T test for parametric variable (t), the Wilcoxon ranksum test for non-parametric test (U) and chi-square for categorical variables (χ2)
Nursing activities score
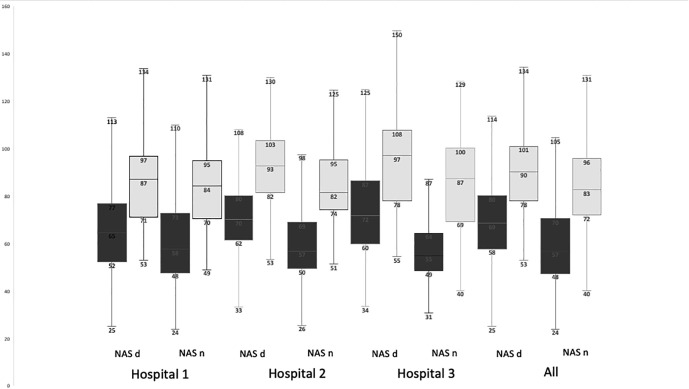
A total of 905 NAS scores recorded for the COVID-19 group and 5453 NAS scores recorded for the non-COVID-19 group were included in the study. The average NAS increased significantly by 20% for the COVID-19 group (M = 92.0 ± 16.1 vs 71.7 ± 18.2, t = −31.48, p < 0.0001), with a higher NAS on admission to the ICU. The distribution of the NAS score was also significantly different. In fact, more than 50% of the NAS scores were between 76% and 100% for COVID-19 patient with 30% of them over 100%, while for the non-COVID-19 group 49% were between 51% and 75%. Nursing activities also differed significantly. Patients with COVID-19 required more time for monitoring, mobilisation, and hygiene care (Table 2 ). COVID-19 significantly increased the NAS in the three hospitals and on the two shifts (day and night). This increase was more marked at night than during the day (27% vs 21%, respectively) (Fig. 1 ).
Table 2.
NAS description and score according to admission source.
| Characteristic | COVID-19 patients (NAS = 905) | Non-COVID-19 patients (NAS = 5,453) | Test values | p value* | Total (NAS = 6,358) |
|---|---|---|---|---|---|
| NAS per 24 h, mean ± | 92.0 ± 16.1 | 71.7 ± 18.2 | t = −31.48 | <0.0001 | 74.6 ± 0.19.3 |
| NAS per 24 h admission day, mdn (IQR) | 96.4 (29.2) | 71.1 (21.5) | U = −29.52 | <0.0001 | 81.75 (24.5) |
| NAS per 24 h discharge ICU, mdn (IQR) | 91.8 (16.7) | 68.3 (22.6) | U = −30.52 | <0.0001 | 69.7 (18.3) |
| NAS < 50%, n (%) | 1 (0.1) | 611 (11) | χ2 = 109.82 | <0.0001 | 612 (10) |
| NAS : 51%–75%, n (%) | 148 (16) | 2,680 (49) | χ2 = 338.01 | <0.0001 | 2,828 (44) |
| NAS : 76%–100%, n (%) | 482 (53) | 1,793 (33) | χ2 = 140.28 | <0.0001 | 2,275 (36) |
| NAS > 100%, n (%) | 274 (30) | 369 (7) | χ2 = 471.90 | <0.0001 | 643 (10) |
| Analysis by item | |||||
| Monitoring and titration n (%) | |||||
| Normal (4.5% in NAS) | 220 (24) | 3,524 (65) | χ2 = 521.09 | <0.0001 | – |
| More than normal (12.1% in NAS) | 489 (54) | 1,743 (32) | χ2 = 165.04 | <0.0001 | – |
| Much more than normal (19.6% in NAS) | 196 (22) | 186 (3) | χ2 = 457.60 | <0.0001 | – |
| Hygiene and procedures n (%) | |||||
| Normal (4.1% in NAS) | 41 (4) | 2,817 (52) | χ2 = 665.95 | <0.0001 | – |
| More than normal (16.5% in NAS) | 535 (60) | 2,148 (39) | χ2 = 151.67 | <0.0001 | – |
| Much more than normal (20.0% in NAS) | 329 (36) | 488 (9) | χ2 = 557.77 | <0.0001 | – |
| Mobilisation and positioning n (%) | |||||
| Normal (5.5% in NAS) | 53 (6) | 1,306 (24) | χ2 = 151.20 | <0.0001 | – |
| More than normal (12.4% in NAS) | 637 (70) | 3,640 (67) | χ2 = 4.66 | 0.031 | – |
| Much more than normal (17.0% in NAS) | 215 (24) | 507 (9) | χ2 = 161.21 | <0.0001 | – |
Abbreviations: ICU = Intensive Care Unit, NAS = Nursing Activities Score
*pvalue: T test for parametric variable (t), the Wilcoxon ranksum test for non-parametric test (U) and chi-square for categorical variables (χ2)
Fig. 1.
Box plots representing the median NAS according to shift and hospital. Black: no-COVID-19 patients. Grey: COVID-19 patients; NAS d = NAS day; NAS n = NAS night. All comparisons are significant (H: 4613,77, p value < 0.001).
Factors associated with nursing time
No factor is significantly correlated with NAS in COVID-19 patients. For the non-COVID-19 group, length of stay (r = 0.17, p = <0.0001), SAPS 3 (r = 0.26, p = <0.0001), and APACHE II (r = 0.22, p = <0.0001) demonstrated a weak but significant correlation with the NAS ( Table 3 ).
Table 3.
Factors related to high nursing workload in the ICU (NAS cut-off: 74.6).
| Characteristic | COVID-19 patients | p value | Non-COVID-19 patients | p value | Total | p value |
|---|---|---|---|---|---|---|
| Statistical test | r (95%CI) | r (95%CI) | r (95%CI) | |||
| Age- y | 0.006 (−0.003–0.138) | 0.061 | −0.04 (−0.04–0.00) | 0.157 | −0.03 (-0.05–0.00) | 0.008 |
| Length of stay-d | 0.01 (−0.05–0.08) | 0.602 | 0.17 (0.14–0.20) | <0.0001 | 0.26 (0.23–0.28) | <0.0001 |
| BMI -kg/m2 | 0.06 (−0.03–0.15) | 0.189 | 0.08 (0.04–0.12) | 0.0001 | 0.19 (0.15–0.22) | <0.0001 |
| SAPS 3 | 0.12 (−0.05–0.20) | 0.762 | 0.26 (0.23–0.28) | <0.0001 | 0.22 (0.19–0.25) | <0.0001 |
| APACHE II | 0.11 (−0.09–0.31) | 0.278 | 0.22 (0.16–0.28) | <0.0001 | 0.23 (0.17–0.29) | <0.0001 |
| Statistical test | OR (95%CI) | OR (95%CI) | OR (95%CI) | |||
| COVID (ref: no COVID) | – | – | – | – | 4.84 (3.63–6.42) | <0.0001 |
| Age (ref: <65 years with median) | 0.39 (0.17–0.87) | 0.023 | 0.79 (0.64–0.97) | 0.024 | 0.79 (0.65–0.96) | 0.018 |
| BMI (ref: <30 kg/m2, threshold for obesity) | 0.58 (0.30–1.12) | 0.104 | 1.31 (1.08–1.60) | 0.006 | 1.21 (1.01–1.46) | 0.034 |
| CVVH (ref: no CVVH) | 10.27 (2.42–20.58) | 0.002 | 5.79 (3.76–8.91) | <0.0001 | 5.87 (3.91–8.82) | <0.0001 |
| SAPS 3 (ref: <46 with median) | 2.36 (0.79–2.49) | 0.238 | 1.82 (1.44–2.32) | <0.0001 | 1.82 (1.45–2.28) | <0.0001 |
| APACHE II (ref. < 14 with median) | 6.37 (1.78–31.78) | 0.006 | 2.65 (1.97–3.56) | <0.0001 | 3.07 (2.30–4.10) | <0.0001 |
| Patients ventilated (ref: no ventilation) | 1.41 (0.79–2.49) | 0.238 | 3.89 (3.05–4.97) | <0.0001 | 3.25 (2.61–4.06) | <0.0001 |
| Death (ref: survivor) | 3.34 (1.56–7.31) | 0.002 | 1.21 (0.87–1.6) | 0.250 | 1.41 (1.07–187) | 0.015 |
| Readmission (ref: no readmission) | 1.62 (0.38–6.98) | 0.511 | 1.18 (0.86–1.63) | 0.298 | 1.26 (0.03–1.71) | 0.136 |
| Sex (ref: women) | 0.99 (0.58–1.66) | 0.960 | 1.13 (0.93–1.38) | 0.223 | 1.12 (0.93–1.25) | 0.227 |
Abbreviations: y = years; d = day; BMI = Body Mass Index; APACHE II = Acute Physiology And Chronic Health Evaluation; SAPS 3 = Simplified Acute Physiology Score; NAS = Nursing Activities Score; CVVH = Continuous VenoVenous Hemofiltration.
Value in bold = Significant
In multivariate analysis, the presence of CVVH (OR = 10.27, 95% CI: 2.42–20.58), APACHE II (OR = 6.37, 95% CI: 1.78–31.78), and patient mortality (OR = 3.34, 95% CI: 1.56–7.31) were significant predictors of a higher NAS in the COVID-19 group. In non-COVID-19 patients, BMI > 30 kg/m2 (OR = 1.31, 95% CI: 1.08–1.60), presence of CVVH (OR = 5.79, 95% CI: 3.76–8.91), SAPS 3 > 46 (OR = 1.82, 95% CI: 1.44–2.32), APACHE II > 14 (OR = 2.65, 95% CI: 1.97–3.56), and mechanical ventilation (OR = 3.89, 95% CI: 3.05–4.97) were significant predictors of a higher NAS. Finally, for the whole sample, COVID-19 was strong predictor of a higher NAS (OR = 4.84, 95% CI: 3.63–6.42) (Table 3).
Discussion
In this study, the proportion of men BMI, length of stay and APACHE II scores were higher in COVID-19 patients. This has previously been observed in other COVID-19 studies (Caussy et al., 2020, Grasselli et al., 2020, Petrilli et al., 2020, Zou et al., 2020). With regard to the duration of mechanical ventilation, duration was significantly higher in COVID-19 patients than in non-COVID-19 patients, supporting previous findings (Bhatraju et al., 2020, Grasselli et al., 2020). Finally, the mortality rate (29%) we observed in intensive care for COVID-19 patients was very close to that reported in a recent literature review (26%) (Quah et al., 2020). COVID-19 has fundamentally changed medical practice in intensive care in terms of the severity of the condition, mortality and the number of ventilated patients.
To assess nursing time, the NAS was chosen because it is highly cited in the literature (Hoogendoorn et al., 2020, Lachance et al., 2015). Furthermore, the tool is used worldwide (Padilha et al., 2015) and takes very little time to encode (Bruyneel et al., 2018).
The mean NAS in COVID-19 patients (M = 92 ± 16) in this study was very high compared to other internationally published NAS scores (Aziz et al., 2020, Lucchini et al., 2014, Padilha et al., 2015, Stafseth et al., 2011). In an Italian study in 15 COVID-19 patients, the authors reported a mean score (M = 84 ± 10) slightly lower than in our study. In our study, nursing activities were significantly higher in monitoring and titration, mobilisation, and hygiene care items. This is explained by the fact that COVID-19 patients were more critical as indicated by their higher APACHE II score, the use of the prone position, and by isolation measures that require increased time direct care.
The NAS score per shift was slightly lower on the night shift when compared to the morning shift as already demonstrated in a previous study (Bruyneel et al., 2019). In fact, in Belgium, a majority of hygiene care is carried out during the day, which explains this difference. The NAS score increased in COVID-19 patients fairly uniformly across the five ICUs.
According to the NAS score, COVID-19 patients demand an ideal N:P ratio close to 1:1 while the legal N:P ratio in Belgium in the ICU is 1:3. Due to the fact that additional pandemic waves of COVID-19 are possible (Kissler et al., 2020), it is necessary to urgently adapt the nursing staff in intensive care in Belgium to maintain quality of care (Margadant et al., 2020, Phua et al., 2020, Sprung et al., 2010, Rosa et al., 2020). Competent nurses trained in critical care and easily mobilised to the hospital could be a solution to manage this need to increase the N:P ratio. The NAS observed in this study for non-COVID-19 patients was very similar to an earlier in Belgium study published recently (Bruyneel et al., 2019).
Regarding factors associated with nursing time (age, length of stay, BMI, severity score), no correlations were significant in COVID-19 patients. On the other hand, there was a weak positive association for length of stay, BMI, SAPS 3, and the APACHE II score in non-COVID-19 patients. This supports findings of other published studies (Altafin et al., 2014, Padilha et al., 2008) and the NAS was written to assess nursing time independently of the patient's pathology (Miranda et al., 2003). In multivariate analysis, three factors are associated with a higher NAS score in the COVID-19 group: presence of a CVVH, APACHE II, and patient mortality. Conversely, older patients were associated with a lower NAS. This can perhaps be explained by therapeutic limitations in the elderly. In the non-COVID-19 group, there were other factors associated with a higher NAS score, BMI, SAPS 3, and patients on mechanical ventilation. We observed different factors in the two groups because COVID-19 patients have a greater disease severity, a very high average NAS, and were more often on mechanical ventilation. The APACHE II score significantly influenced the NAS in COVID-19 patients but not the SAPS 3. For the entire sample, the diagnosis of COVID-19 was a significant predictor of a high NAS. These factors can, therefore, help to manage the distribution of patients in the nursing team.
Limitations
This study has certain limitations. First, we had a limited number of COVID-19 patients (95 patients) and only five ICUs. It would be interesting to repeat this study with more patients and more ICUs in order to improve representation and statistical power. Second, it would also be interesting to carry out an international study on the association between the NAS and COVID-19 to assess the impact of this pathology on nursing work time in several countries. Third, there are factors missing that could explain the association with a high NAS. For example, we do not have patients on ECMO (Lucchini et al., 2019) and we did not extract prone positioning sessions. Finally, we compared patients at different times of the year. However, one study has shown that the NAS score is not significantly different between winter and summer (Bruyneel et al., 2019).
Conclusions
COVID-19 significantly increases the nursing time in the intensive care unit and the ideal nurse-to-patient ratio is close to 1:1. Consequently, there is a need to increased ICU nursing staff numbers to adequately manage new waves of COVID-19 or other possible infectious disease pandemics. Further research is needed in this area.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
The authors would like to acknowledge the contributions of Lionel Di Pierdomenico, Lionel Haentjens and Pierre Smith.
The authors acknowledge the contribution of a medical writer, Sandy Field, PhD, for English language editing and formatting of the manuscript.
References
- Aiken L.H., Sloane D.M., Bruyneel L., Van den Heede K., Griffiths P., Busse R., Diomidous M., Kinnunen J., Kózka M., Lesaffre E., McHugh M.D., Moreno-Casbas M.T., Rafferty A.M., Schwendimann R., Scott P.A., Tishelman C., van Achterberg T., Sermeus W. Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet. 2014;383(9931):1824–1830. doi: 10.1016/S0140-6736(13)62631-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altafin J.A.M., Grion C.M.C., Tanita M.T., Festti J., Cardoso L.T.Q., Veiga C.F.F., Kamiji D., Barbosa Á.R.G., Matsubara C.C.T., Lara A.B., Lopes C.C.B., Blum D., Matsuo T. Nursing activities score and workload in the intensive care unit of a university hospital. Revista Brasileira de Terapia Intensiva. 2014;26 doi: 10.5935/0103-507X.20140041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aziz S., Arabi Y.M., Alhazzani W., Evans L., Citerio G., Fischkoff K., Salluh J., Meyfroidt G., Alshamsi F., Oczkowski S., Azoulay E., Price A., Burry L., Dzierba A., Benintende A., Morgan J., Grasselli G., Rhodes A., Møller M.H., Chu L., Schwedhelm S., Lowe J.J., Bin D.u., Christian M.D. Managing ICU surge during the COVID-19 crisis: rapid guidelines. Intensive Care Med. 2020;46(7):1303–1325. doi: 10.1007/s00134-020-06092-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball J.E., Bruyneel L., Aiken L.H., Sermeus W., Sloane D.M., Rafferty A.M., Lindqvist R., Tishelman C., Griffiths P. Post-operative mortality, missed care and nurse staffing in nine countries: a cross-sectional study. Int. J. Nursing Stud. 2018;78:10–15. doi: 10.1016/j.ijnurstu.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatraju P.K., Ghassemieh B.J., Nichols M., Kim R., Jerome K.R., Nalla A.K., Greninger A.L., Pipavath S., Wurfel M.M., Evans L., Kritek P.A., West T.E., Luks A., Gerbino A., Dale C.R., Goldman J.D., O’Mahony S., Mikacenic C. Covid-19 in critically Ill patients in the seattle region — case series. N. Engl. J. Med. 2020;382(21):2012–2022. doi: 10.1056/NEJMoa2004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruyneel A., Guerra C., Tack J., Droguet M., Maes J., Miranda D.R., Mootien J., Bretonnière C. Traduction sémantique en français et implémentation du Nursing Activities Score en Belgique. Méd. Intensive Réa. 2018;27(3):260–272. doi: 10.3166/rea-2018-0029. [DOI] [Google Scholar]
- Bruyneel A., Tack J., Droguet M., Maes J., Wittebole X., Miranda D.R., Pierdomenico L.D. Measuring the nursing workload in intensive care with the Nursing Activities Score (NAS): a prospective study in 16 hospitals in Belgium. J. Crit. Care. 2019;54:205–211. doi: 10.1016/j.jcrc.2019.08.032. [DOI] [PubMed] [Google Scholar]
- Caussy C., Pattou F., Wallet F., Simon C., Chalopin S., Telliam C., Mathieu D., Subtil F., Frobert E., Alligier M., Delaunay D., Vanhems P., Laville M., Jourdain M., Disse E. Prevalence of obesity among adult inpatients with COVID-19 in France. Lancet Diabet. Endocrinol. 2020;8(7):562–564. doi: 10.1016/S2213-8587(20)30160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cimiotti J.P., Aiken L.H., Sloane D.M., Wu E.S. Nurse staffing, burnout, and health care–associated infection. Am. J. Infect. Control. 2012;40(6):486–490. doi: 10.1016/j.ajic.2012.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cucinotta D., Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Bio Medica Atenei Parmensis. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daud-Gallotti R.M., Costa S.F., Guimarães T., Padilha K.G., Inoue E.N., Vasconcelos T.N., da Silva Cunha Rodrigues F., Barbosa E.V., Figueiredo W.B., Levin A.S. Nursing workload as a risk factor for healthcare associated infections in ICU: a prospective study. PLoS One. 2012;7 doi: 10.1371/journal.pone.0052342. e52342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elharrar X., Trigui Y., Dols A.-M., Touchon F., Martinez S., Prud’homme E., Papazian L. Use of prone ^ositioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA. 2020 doi: 10.1001/jama.2020.8255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A., Cereda D., Coluccello A., Foti G., Fumagalli R., Iotti G., Latronico N., Lorini L., Merler S., Natalini G., Piatti A., Ranieri M.V., Scandroglio A.M., Storti E., Cecconi M., Pesenti A. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoogendoorn M.E., Margadant C.C., Brinkman S., Haringman J.J., Spijkstra J.J., de Keizer N.F. Workload scoring systems in the Intensive Care and their ability to quantify the need for nursing time: a systematic literature review. Int. J. Nurs. Stud. 2020;101:103408. doi: 10.1016/j.ijnurstu.2019.103408. [DOI] [PubMed] [Google Scholar]
- Ioannidis J.P.A., Axfors C., Contopoulos-Ioannidis D.G. Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters (preprint) medRxiv. 2020 doi: 10.1101/2020.04.05.20054361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansson M.M., Syrjälä H.P., Ala-Kokko T.I. Association of nurse staffing and nursing workload with ventilator-associated pneumonia and mortality: a prospective, single-center cohort study. J. Hosp. Infect. 2019;101(3):257–263. doi: 10.1016/j.jhin.2018.12.001. [DOI] [PubMed] [Google Scholar]
- Kissler S.M., Tedijanto C., Goldstein E., Grad Y.H., Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368(6493):860–868. doi: 10.1126/science:abb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachance J., Douville F., Dallaire C., Padilha K.G., Gallani M.C. The use of the Nursing Activities Score in clinical settings: an integrative review. Rev. esc. enferm. USP. 2015;49(spe):147–156. doi: 10.1590/S0080-623420150000700021. [DOI] [PubMed] [Google Scholar]
- Lucchini A., De Felippis C., Elli S., Schifano L., Rolla F., Pegoraro F., Fumagalli R. Nursing Activities Score (NAS): 5 Years of experience in the intensive care units of an Italian University hospital. Intensive Critical Care Nurs. 2014;30:152–158. doi: 10.1016/j.iccn.2013.10.004. [DOI] [PubMed] [Google Scholar]
- Lucchini A., Elli S., De Felippis C., Greco C., Mulas A., Ricucci P., Fumagalli R., Foti G. The evaluation of nursing workload within an Italian ECMO Centre: a retrospective observational study. Intensive Crit. Care Nurs. 2019;55:102749. doi: 10.1016/j.iccn.2019.07.008. [DOI] [PubMed] [Google Scholar]
- Lucchini A., Giani M., Elli S., Villa S., Rona R., Foti G. Nursing activities score is increased in COVID-19 patients. Intensive Crit. Care Nurs. 2020;59:102876. doi: 10.1016/j.iccn.2020.102876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margadant C., Wortel S., Hoogendoorn M., Bosman R., Spijkstra J.J., Brinkman S., de Keizer N. The nursing activities score per nurse ratio is associated with in-hospital mortality, whereas the patients per nurse ratio is not. Crit. Care Med. 2020;48(1):3–9. doi: 10.1097/CCM.0000000000004005. [DOI] [PubMed] [Google Scholar]
- Miranda D.R., Nap R., de Rijk A., Schaufeli W., Iapichino G. Nursing activities score. Crit. Care Med. 2003;31(2):374–382. doi: 10.1097/01.CCM.0000045567.78801.CC. [DOI] [PubMed] [Google Scholar]
- Needleman J., Liu J., Shang J., Larson E.L., Stone P.W. Association of registered nurse and nursing support staffing with inpatient hospital mortality. BMJ Qual. Saf. 2020;29(1):10–18. doi: 10.1136/bmjqs-2018-009219. [DOI] [PubMed] [Google Scholar]
- Neuraz A., Guérin C., Payet C., Polazzi S., Aubrun F., Dailler F., Lehot J.-J., Piriou V., Neidecker J., Rimmelé T., Schott A.-M., Duclos A. Patient mortality is associated with staff resources and workload in the ICU: a multicenter observational study. Crit. Care Med. 2015;43(8):1587–1594. doi: 10.1097/CCM.0000000000001015. [DOI] [PubMed] [Google Scholar]
- Padilha K.G., de Sousa R.M.C., Queijo A.F., Mendes A.M., Miranda D.R. Nursing activities score in the intensive care unit: analysis of the related factors. Intensive Crit. Care Nurs. 2008;24(3):197–204. doi: 10.1016/j.iccn.2007.09.004. [DOI] [PubMed] [Google Scholar]
- Padilha K.G., Stafseth S., Solms D., Hoogendoom M., Monge F.J.C., Gomaa O.H., Giakoumidakis K., Giannakopoulou M., Gallani M.C., Cudak E., de Nogueira L.S., Santoro C., de Sousa R.C., Barbosa R.L., dos Miranda D.R. Nursing Activities Score: an updated guideline for its application in the Intensive Care Unit. Rev. esc. enferm. USP. 2015;49(spe):131–137. doi: 10.1590/S0080-623420150000700019. [DOI] [PubMed] [Google Scholar]
- Petrilli C.M., Jones S.A., Yang J., Rajagopalan H., O’Donnell L., Chernyak Y., Tobin K.A., Cerfolio R.J., Francois F., Horwitz L.I. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020 doi: 10.1136/bmj.m1966. m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phua J., Weng L., Ling L., Egi M., Lim C.-M., Divatia J.V., Shrestha B.R., Arabi Y.M., Ng J., Gomersall C.D., Nishimura M., Koh Y., Du B. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Resp. Med. 2020;8(5):506–517. doi: 10.1016/S2213-2600(20)30161-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quah P., Li A., Phua J. Mortality rates of patients with COVID-19 in the intensive care unit: a systematic review of the emerging literature. Crit. Care. 2020;24 doi: 10.1186/s13054-020-03006-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa W.E., Binagwaho A., Catton H., Davis S., Farmer P.E., Iro E., Karanja V., Khanyola J., Moreland P.J., Welch J.C., Aiken L.H. Rapid investment in nursing to strengthen the global COVID-19 response. Int. J. Nurs. Stud. 2020;109:103668. doi: 10.1016/j.ijnurstu.2020.103668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- sciensano, n.d. BULLETIN EPIDEMIOLOGIQUE DU 20 JUIN 2020.
- Sprung C.L., Zimmerman J.L., Christian M.D., Joynt G.M., Hick J.L., Taylor B., Richards G.A., Sandrock C., Cohen R., Adini B. Recommendations for intensive care unit and hospital preparations for an influenza epidemic or mass disaster: summary report of the European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mass disaster. Intensive Care Med. 2010;36:428–443. doi: 10.1007/s00134-010-1759-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafseth S.K., Solms D., Bredal I.S. The characterisation of workloads and nursing staff allocation in intensive care units: a descriptive study using the Nursing Activities Score for the first time in Norway. Intensive Crit. Care Nurs. 2011;27(5):290–294. doi: 10.1016/j.iccn.2011.07.003. [DOI] [PubMed] [Google Scholar]
- Stone P.W., Mooney-Kane C., Larson E.L., Horan T., Glance L.G., Zwanziger J., Dick A.W. Nurse working conditions and patient safety outcomes. Med. Care. 2007;45:571–578. doi: 10.1097/MLR.0b013e3180383667. [DOI] [PubMed] [Google Scholar]
- Venier A.-G., Leroyer C., Slekovec C., Talon D., Bertrand X., Parer S., Alfandari S., Guerin J.-M., Megarbane B., Lawrence C., Clair B., Lepape A., Perraud M., Cassier P., Trivier D., Boyer A., Dubois V., Asselineau J., Rogues A.-M., Thiébaut R. Risk factors for Pseudomonas aeruginosa acquisition in intensive care units: a prospective multicentre study. J. Hosp. Infect. 2014;88(2):103–108. doi: 10.1016/j.jhin.2014.06.018. [DOI] [PubMed] [Google Scholar]
- West E., Mays N., Rafferty A.M., Rowan K., Sanderson C. Nursing resources and patient outcomes in intensive care: a systematic review of the literature. Int. J. Nurs. Stud. 2009;46(7):993–1011. doi: 10.1016/j.ijnurstu.2007.07.011. [DOI] [PubMed] [Google Scholar]
- Zou X., Li S., Fang M., Hu M., Bian Y., Ling J., Yu S., Jing L., Li D., Huang J. Acute physiology and chronic health evaluation II score as a predictor of hospital mortality in patients of Coronavirus disease 2019. Crit. Care Med. 2020 doi: 10.1097/CCM.0000000000004411. Publish Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]