Abstract
The COVID-19 health crisis has greatly impacted the organization of outpatient consultations, especially in hand surgery. Five reorganization stages were described during the crisis (from week 11 to week 21 in 2020): preparatory stage, 1st organizational stage, wait-and-see stage, 2nd organizational stage, and progressive return stage. The number of patients seen on-site decreased 64% in 2020 compared to 2019, while 78% of consultations were canceled. The logistics (teleconsultation, dedicated COVID-19 patient pathways) and human resources (sick leave, telework, reassignment to other departments) were adapted to ensure that patients who are usually seen in our hand surgery department received adequate care.
Keywords: Outpatient consultations, Coronavirus, COVID-19, Teleconsultation, Telework, COVID-19 patient
Résumé
La crise sanitaire COVID-19 a fortement impacté l’organisation des services de consultations externes, notamment en chirurgie de la main. Cinq phases de réorganisation des consultations externes ont été décrites durant la crise (de la semaine 11 à la semaine 21 en 2020) : une phase préparatoire, une 1ère phase organisationnelle, une phase attentiste, une 2nde phase organisationnelle et une phase de reprise progressive. Le nombre de patients venus en présentiel a baissé en 2020 par rapport à 2019 de 64.5% tandis que 78.2% des créneaux de consultations ont été annulés. Une adaptation des moyens logistiques (téléconsultations, circuits COVID-19) et des moyens humains (arrêts de travail, télétravail, réaffectation dans d’autres services) a été parallèlement instaurée au décours des semaines, ce qui a permis une poursuite adaptée à la crise sanitaire, de la prise en charge des patients habituellement suivis en consultation de chirurgie de la main.
Mots-clefs: Consultations externes, Coronavirus, Covid-19, Téléconsultations, Télétravail, Covid-19 patients
1. Introduction
The health crisis due to coronavirus (COVID-19) hit France during the 1st quarter of 2020. A lockdown was initiated on March 17th, 2020 after stage 3 of the epidemic was reached on the March 14th [1]. A public health emergency was declared on March 23rd, 2020, forcing hospitals to enforce the White Plan (“Plan Blanc”) [2], [3], [4]. The White Plan had four goals: mobilization of all healthcare facilities, mobilization of health professionals, mobilization of health supplies and logistics from private and public facilities, adaptation of the medical activity at these facilities [5].
In the week leading to the lockdown, the crisis unit at our hospital decided to cancel all non-urgent surgical procedures in March to preserve human resources and medical supplies for the care of COVID-19 patients as recommended by the Regional Health Agency. The 1st stage of easing of the lockdown started May 11th, 2020.
Like other surgical departments in other countries [6], outpatient consultations for hand surgery had to abide by the White Plan’s rules and four goals, even more so in one of the French regions most severely hit by the pandemic. Our team had to adapt to follow the guidelines issued by the government, especially the physical distancing measures [7], while providing optimal medical care for patients [8].
The goal of this study was to describe the progressive adaptation of our hand surgery practice for outpatient consultations during the health crisis related to the COVID-19 pandemic.
2. Material and methods
We studied the organizational modifications implemented at our outpatient consultations after the first cases of COVID-19 appeared in France. Our hand surgery department has seven surgeons in a teaching hospital context. We compared the activity between 2019 (considered as the reference year without pandemic) and 2020 (year studied during the COVID-19 pandemic) during the same time frame. Three criteria were studied between weeks 11 and 21 (W11–W21): patient, consultation, and logistics (manpower and supplies).
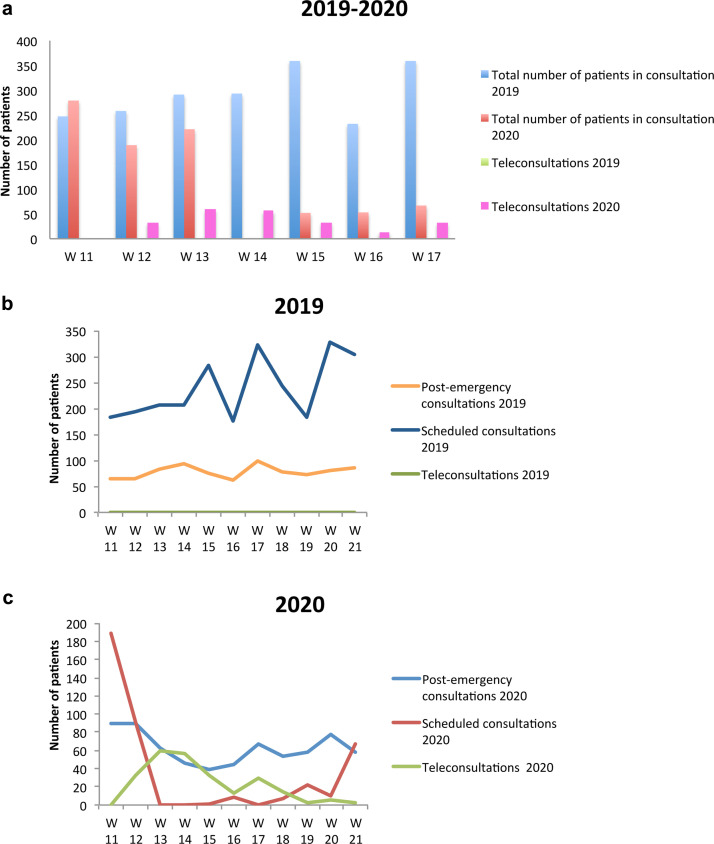
For the “patient” criteria, we counted the number of patients at the consultation (differentiating those seen after an emergency from those seen for a scheduled consultation), the number of patients who did not show up for their consultation and the number of patients treated using teleconsultation (telephone or videoconference) for each week in 2019 and 2020. Headcounts, variation in attendance (in percentage) between 2020 and 2019 and variation in no-shows at the consultations are shown in Fig. 1 a,b,c. The pathologies and mechanisms of injury of patients presenting at the emergency room, number of surgical interventions and results of COVID-19 screening by PCR for operated patients during the lockdown were also recorded. All pathologies and mechanisms of injury seen during post-emergency consultations in 2020 were studied and compared with 2019 over the same period.
Fig. 1.
(a) Total number of patients seen for in-person consultation (post-emergency and scheduled) and teleconsultation from W11 to W21 in 2019 and 2020. (b) Change in the number of patients seen in post-emergency or scheduled consultations and teleconsultations from W11 to W21 in 2019. (c) Change in the number of patients seen in post-emergency or scheduled consultations and teleconsultations from W11 to W21 in 2020.
For the “consultation” criteria, we documented all modifications (delays, cancellations, creations, rescheduled) in the various outpatient consultations.
For the “logistics” criteria, we counted the number of available staff members in this time frame (secretaries, doctors, nurses, physiotherapists, occupational therapists), as well as all the modifications made to the premises and organization of the consultation.
3. Results
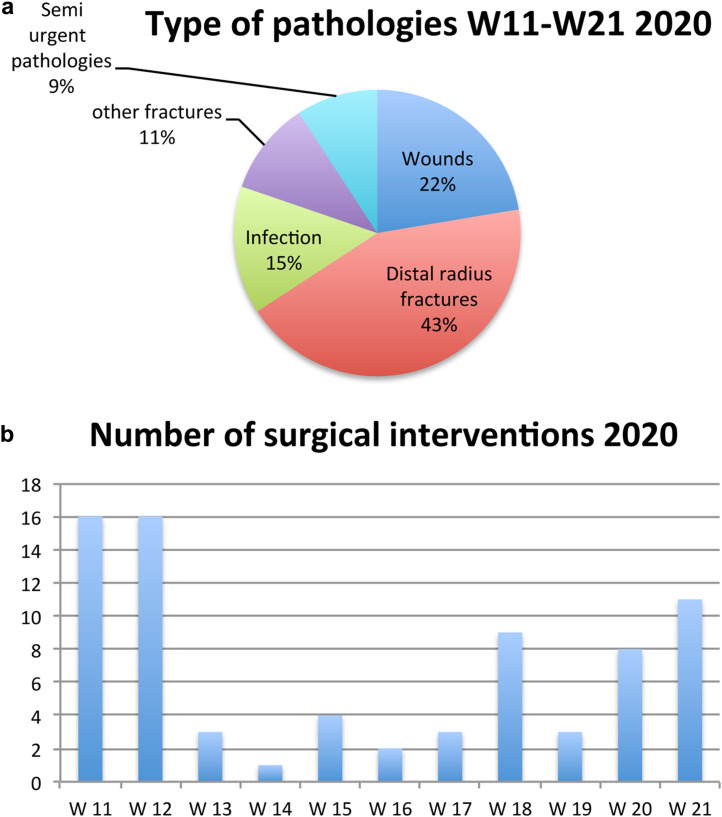
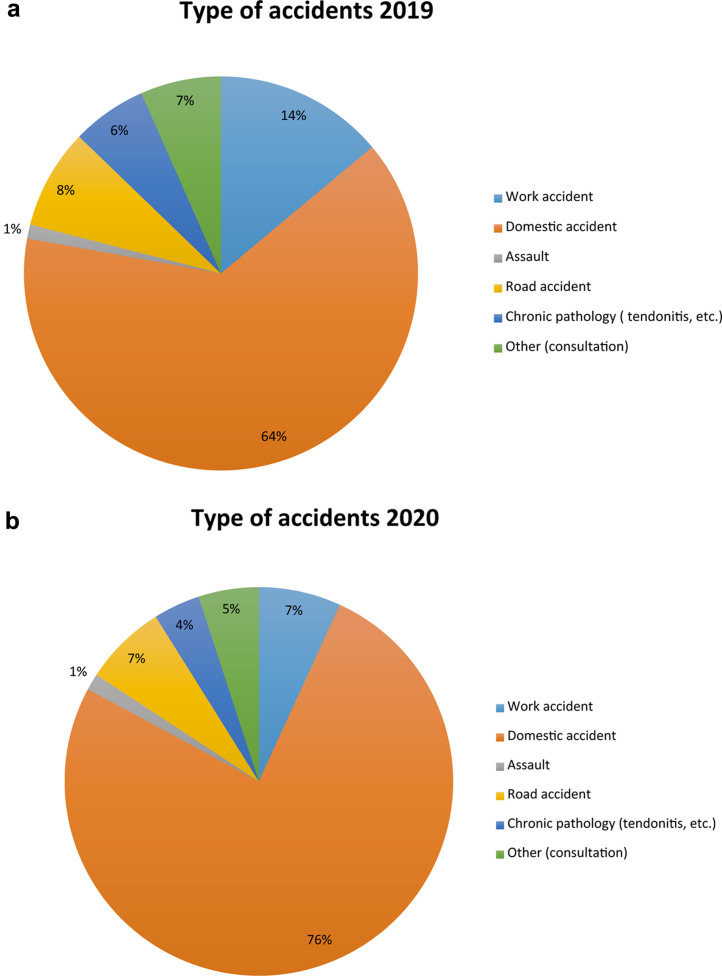
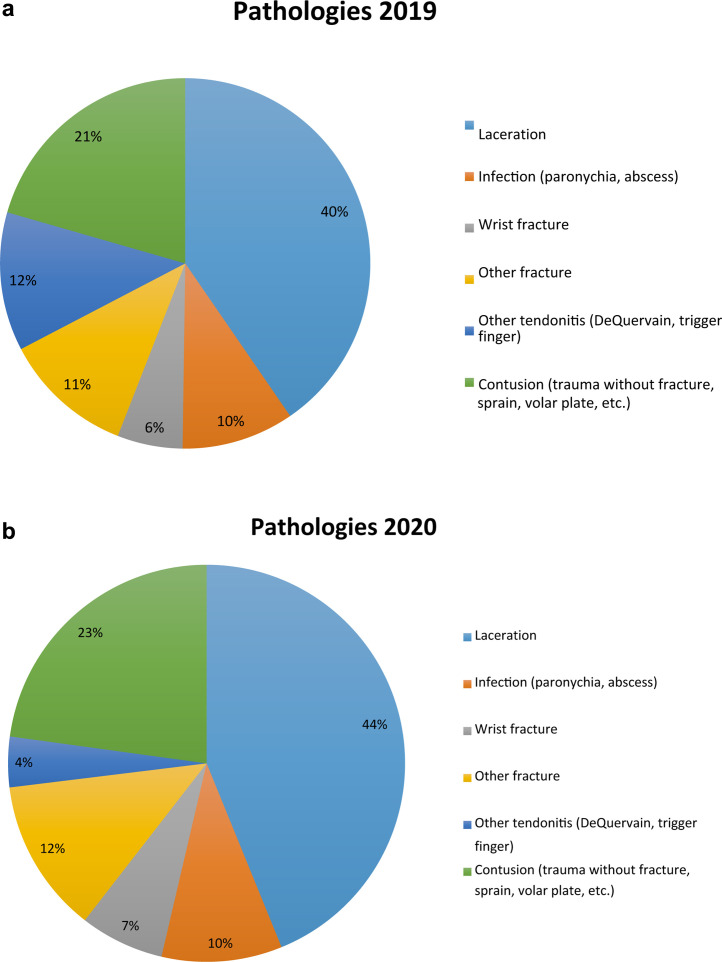
For the “patient” criteria, the results for each week are summarized in Fig. 1a,b,c. During this period, the number of patients seen for consultations decreased 64% between 2019 and 2020 (3426 patients vs 1216), with 58% sustained consultations. Among those patients, the proportion of patients seen for a scheduled consultation decreased 81% (2095 patients vs 395), and the patients seen for a post-emergency consultation decreased 20% (860 patients vs 687). While no patients were seen using teleconsultation in 2019 (Fig. 1b), 248 patients were treated this way in 2020, with a stabilization of this number after week 14 (W14). The study also showed that the rate of no-shows in outpatient consultation increased moderately from 258/2922 in 2019 (9%) to 127/1216 in 2020 (10%). The five main pathologies that were treated surgically during W11–W21 were lacerations, infections, distal radius fractures, hand fractures (e.g. metacarpal bones), other semi-urgent diseases (Fig. 2 a). For patients seen in the emergency room, the mechanism of injury was mainly wounds, sometimes after a fight during confinement at home; there was a decrease in the number of accidents at work while the number of road accidents was the same. Approximately 2 patients were operated per day during W13–W17 (Fig. 2b). All our COVID-19 screenings for operated patients during the lockdown were negative. The percentage of COVID-19 positive patients in the consultation between weeks 11 and 20 was 0.5% (tests started on W14). All pathologies and mechanisms of injury such as the circumstances of the accidents seen during post-emergency consultations were compared between 2019 and 2020 over the same period (Figs. 3a,b and 4 a,b).
Fig. 2.
(a) Type of hand pathologies seen during the lockdown (W11–W21) in 2020. (b) Number of surgical interventions performed during the lockdown (W11–W21) in 2020.
Fig. 3.
(a) Type of accidents encountered in post-emergency consultations in 2019. (b) Type of accidents encountered in post-emergency consultations in 2020.
Fig. 4.
(a) Pathologies encountered in post-emergency consultations in 2019. (b) Pathologies encountered in post-emergency consultations in 2020.
For the “consultation” criteria, the consultation was normally run by seven hand surgeons during W11–W21 of 2019: 18 slots for scheduled consultations, 2 slots for pediatric consultations, 3 slots for private consultations and 5 slots for post-emergency consultations. During the pandemic, starting at week 13, consultations only took place in the morning; all afternoon consultations were cancelled (Table 1 ). A total of 18 consultations slots were cancelled each week (78%). One week after the lockdown was eased (W21) only 10 slots were cancelled. The patients who had scheduled consultations for “semi-urgent” conditions were seen during the post-emergency consultation slots (infection, hardware removal, cast renewal, corticosteroid injections, etc.). Teleconsultations were not used in 2019 in the department and were all initiated during the COVID-19 pandemic (Fig. 1a,b,c). These consultations took place either in the morning alongside the post-emergency consultations with a different surgeon or in the afternoon for private and physiotherapy consultations (created in 2020).
Table 1.
Comparison of the number of weekly consultation slots between 2019 and 2020.
| Monday |
Tuesday |
Wednesday |
Thursday |
Friday |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | 2019 | 2020 | 2019 | 2020 | 2019 | 2020 | 2019 | 2020 | |
| Morning | 2 | 1 | 3 | 1 | 4 | 1 | 4 | 1 | 2 | 1 |
| Afternoon | 3 | 0 | 3 | 0 | 3 | 0 | 2 | 0 | 1 | 0 |
For the “manpower and supply logistics” criteria, the normal number of medical and paramedical staff was 26. The number of absent or reassigned staff was reduced during the lockdown but started to return to normal after restrictions were eased: 24/26 staff present on week 11 (Table 2a ), 12 staff on week 13 (Table 2b ), 14 staff on week 17 (Table 2c ), 23 staff on week 21 (Table 2d ). Week 13 saw an increase in absences due to vacation, sick leave, child-care or COVID-19 infection and also a large number of medical staff being reassigned to other duties (helping to change of position of patients in intensive care units (ICU), call to the families, regulation of calls to the emergency phone number) [9].
Table 2a.
Medical and paramedical staff assignments during W11 (Stage 1).
| W11 in 2020 | Present | Sick leave | Telework | Reassigned to other departments | Vacation |
|---|---|---|---|---|---|
| Stage 1 | |||||
| 7 secretaries | 6 | 0 | 0 | 0 | 1 |
| 13 doctors | 12 | 0 | 0 | 0 | 1 |
| 4 physical/occupational therapists | 4 | 0 | 0 | 0 | 0 |
| 2 nurses | 2 | 0 | 0 | 0 | 0 |
| Total | 24/26 | 0/26 | 0/26 | 0/26 | 2/26 |
Table 2b.
Medical and paramedical staff assignments during W13 (Stage 2).
| W13 in 2020 | Present | Sick leave | Telework | Reassigned to other departments | Vacation |
|---|---|---|---|---|---|
| Stage 2 | |||||
| 7 secretaries | 3 | 2 | 2 | 0 | 0 |
| 13 doctors | 7 | 1 | 0 | 4 | 1 |
| 4 physical/occupational therapists | 1 | 0 | 0 | 1 | 2 |
| 2 nurses | 1 | 0 | 0 | 1 | 0 |
| Total | 12/26 | 3 /26 | 2/26 | 6/26 | 3/26 |
Table 2c.
Medical and paramedical staff assignments during W17 (Stage 3).
| W17 in 2020 | Present | Sick leave | Telework | Reassigned to other departments | Vacation |
|---|---|---|---|---|---|
| Stage 3 | |||||
| 7 secretaries | 1 | 1 | 1 | 1 | 3 |
| 13 doctors | 11 | 0 | 1 | 1 | 0 |
| 4 physical/occupational therapists | 1 | 0 | 0 | 2 | 1 |
| 2 nurses | 1 | 0 | 0 | 1 | 0 |
| Total | 14/26 | 1/26 | 2/26 | 5/26 | 4/26 |
Table 2d.
Medical and paramedical staff assignments during W21 (Stage 5).
| W21 in 2020 | Present | Sick leave | Telework | Reassigned to other departments | Vacation |
|---|---|---|---|---|---|
| Stage 5 | |||||
| 7 secretaries | 6 | 0 | 1 | 0 | 0 |
| 13 doctors | 12 | 0 | 0 | 0 | 1 |
| 4 physical/occupational therapists | 2 | 0 | 0 | 2 | 0 |
| 2 nurses | 2 | 0 | 0 | 0 | 0 |
| Total | 22/26 | 0/26 | 1/26 | 2/26 | 1/26 |
The modifications made to the premises were (in chronological order): set-up of COVID-19 signs [7] and hand sanitizer stations (W10), set-up of glass panels at the secretaries’ desks (W12) (Fig. 5 a), dedicated room for the care of COVID-19 patients with dedicated equipment at the entrance (W14) (Fig. 5b), access restricted to every other seat in the waiting room using caution tape (S14) (Fig. 5c) according to the recommendations of the hospital's health safety committee [10], [11].
Fig. 5.
(a) Glass panel set-up at the welcome desk of outpatient consultations. (b) Examination room dedicated to COVID-19 positive patients with protection equipment at the entrance. (c) Waiting room where only every other seat can be used to enforce physical distancing.
In chronological order, the modifications made to the organization of the consultation were the set-up of telework for secretaries (W13), set-up of teleconsultations using Odys web (Pulsy) for the surgeons (W12) and physiotherapists (W16), safety regulations for use of nitrogen monoxide and oxygen (MEOPA) in a ventilated room (W14). A dedicated protocol for radiological examinations of COVID-19 positive patients required calling ahead to the radiology department to set up the appropriate protective measures and accompanying the patient to and from the radiology department to prevent contaminations along the way (W14) [12], [13]. We started to increase outpatient consultation slots of one week after the lockdown was eased (W21).
4. Discussion
Our results show that the outpatient consultations for hand surgery during the COVID-19 pandemic in France were organized in five stages.
Stage 1 was the preparatory phase before the lockdown. We found a continuation of the normal pace of consultations (with figures comparable to 2019). It lasted until the end of week 11 while France was in stage 2 of the pandemic [14]. This time was used to prepared for the following stages. Surgeons asked their secretaries to call and cancel non-urgent, pediatric, and private consultations from week 12 on. Surprisingly, the number of no-shows was not greater in 2020 compared to 2019 as the patients took the time to cancel their appointments.
Stage 2 was the 1st organizational phase during the lockdown. It lasted 3 weeks (W12–W14) matching the beginning of the lockdown and the governmental restrictions on circulation [15], [16], [17]. The cancellation of consultations continued. To free time for the medical, paramedical and secretary staff [9], all consultations were grouped in the morning (Table 2b). Despite a dramatic decrease in the number of available consultations, 58% of on-site consultations were maintained. At the same time, teleconsultations were set-up rapidly for follow-up consultations with 59 teleconsultations a week starting in W13 (Fig. 1c). During this stage, the patients continued to call to cancel their appointments. Some emergency cases were transferred to another hand center because of severe lack of anesthesiologists.
Stage 3 was the wait-and-see phase during the lockdown. It started on W15 and had a stable number of post-emergency consultations and teleconsultations (Fig. 1c). The number of post-emergency consultations did not decrease despite a decrease in the number of hand emergencies during this period; this is explained by the fact that “semi-urgent” patients were also seen during post-emergency consultations.
Stage 4 was the 2nd organizational stage, before and during easing of the lockdown restrictions from W18 to W20. New protocols were disseminated according to the recommendations of the hospital’s health safety committee. COVID-19 screening for operated patients was mandatory.
Stage 5 was a progressive return, with outpatient consultations at first (W21). We started to operate on scheduled patients during W23.
The human measures and logistics matched these five phases. During Stage 1, we enforced the physical distancing measures as much as possible; hand sanitizer gel was usually available but sometimes was stolen or out of stock. A glass panel was set-up to enforce the physical distancing between patients and secretaries. The number of staff was normal (except for 2 who were on vacation) (Table 2a).
During Stage 2, teleconsultation software was tested and rolled out. Phone consultations were more frequent than videoconferences. Dedicated paths for COVID-19 patients were set-up after they were approved by the hospital's health safety committee (outpatient consultations, use of MEOPA, and outpatient radiology). The number of staff decreased due to reassignments to other departments, especially to help the medical staff in the ICU [9], due to sick leave [18], and due to telework that became a part of our secretaries’ work schedule. Telework enabled our staff to reduce the risk of being contaminated and to adapt to the reduced availability of public transportation [19].
During Stage 3, teleconsultation was also started for physiotherapists after the surgeon referred the patient to limit functional sequelae. Indeed, most physiotherapists in private practice had stopped all activity based on governmental recommendations [20], [21], [22]. This consultation method allowed us to give advice and self-directed rehabilitation exercises, supplemented as needed by written protocols (FESUM, GEMMSOR websites). Meanwhile physiotherapists were reassigned to provide chest physiotherapy in COVID-19 units.
During Stage 4, more staff members (except physiotherapists working in COVID-19 units) were invited to return to the hand surgery department.
During Stage 5, we progressively returned to a subnormal activity level with increasing human measures and logistics.
Teleconsultations by videoconference had several technological limitations. Before a teleconsultation, a secretary had to call the patient beforehand to set-up an appointment but also make sure he had a camera, a microphone, and an Internet connection. Up to 50% of patients preferred to wait for an on-site consultation or did not have the required equipment for the videoconference. Videoconferences were sometimes interrupted by temporary network failures that extended the time necessary to complete the teleconsultation. For private consultations and first consultations, other software packages were used (Doctolib, Deuxiemeavis). Pediatric consultations, especially those regarding birth defects, were conducted by teleconsultation starting at W15. The two main upsides of teleconsultations (phone call and videoconference) were the protection of the patients [19], [23], [24] and staff against contamination. Indeed, some patients were afraid to be in a waiting room with other patients who might carry the SARS-CoV-2 virus and preferred this type of consultation. Teleconsultations also enabled the surgeons to stay home and work despite not having secretaries and nurses to welcome the patients. The downsides of teleconsultations were the difficulty in doing a radiological follow-up, difficulty in doing an objective physical examination, temporary internet failures [25], and difficulty in collecting payment from the patients. These limitations should be addressed by continued use of this type of consultation beyond the pandemic. The average teleconsultation time was 25 min but after a 5–6 week learning curve, the consultation time was the same as a conventional in-office consultation (15 min).
5. Conclusion
The COVID-19 epidemic was an exceptional situation with major repercussions on the French healthcare system, especially in the Eastern part of France [3], [4]. Measures had to be progressively taken in our outpatient hand surgery department following governmental recommendations, lockdown restrictions as well as protective measures for our staff and our patients and then easing of the lockdown [23], [24]. Thanks to these five specific phases, it was possible for us to continue outpatient consultations. We were able to maintain 35% of our activity (compared to 2019) and started using two new technological tools in our practice: teleconsultation and telework.
The 2nd preparatory phase before the end of the lockdown was crucial to prepare for a gradual return to normal. Permanent reorganization of outpatient consultations was necessary to follow the public health situation. Our experience could help hand departments prepare for a new viral pandemic in the future.
Funding
This work did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
All authors attest that they meet the current International Committee of Medical Journal Editors (ICMJE) criteria for Authorship.
Conflicts of interest
P. Liverneaux has conflicts of interest with Newclip™, Technics™ and Argomedical™.
The other authors declare that they have no conflicts of interest related to this article.
References
- 1.Coronavirus: 1, 2 et 3… que veulent dire les différents stades de l’épidémie? Available through: https://www.lemonde.fr/les-decodeurs/article/2020/03/05/coronavirus-a-quoi-correspondent-les-trois-stades-du-plan-d-action-contre-l-epidemie_6031948_4355770.html.
- 2.Loi n° 2004-806 du 9 août 2004 relative à la politique de santé publique (1). Titre III: Modernisation du système de veille, d’alerte et de gestion des situations d’urgence sanitaire. Chapitre II: Prévention et gestion des menaces sanitaires graves et des situations d’urgence. Available through: https://www.legifrance.gouv.fr/eli/loi/2004/8/9/2004-806/jo/article 20.
- 3.Décret n° 2020-293 du 23 mars 2020 prescrivant les mesures générales nécessaires pour faire face à l’épidémie de covid-19 dans le cadre de l’état d’urgence sanitaire. Available through: https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000041746694&categorieLien=id.
- 4.Loi n° 2020-290 du 23 mars 2020 d’urgence pour faire face à l’épidémie de covid-19. Available through: https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000041746313&dateTexte=20200325.
- 5.Informations coronavirus Covid-19. Available through: https://www.gouvernement.fr/info-coronavirus#xtor=SEC-3-GOO-[%7Badgroup%7D]-[425081976934]-search-[site%20du%20gouvernement.
- 6.Ducournau F., Arianni M., Awwad S., Baur E.M., Beaulieu J.Y., Bouloudhnine M., et al. COVID-19: initial experience of an international group of hand surgeons. Hand Surg Rehabil. 2020;39:159–166. doi: 10.1016/j.hansur.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Informations coronavirus Covid-19. Available through: https://www.gouvernement.fr/infocoronavirus?fbclid=IwAR1KSoRVvlYnUjRZA34jU7E6byyZZOWV7qlDAJc3rK_fsL8iyYVq4LzlqUE.
- 8.Article 47 (article R.4127-47 du code de la santé publique). Available through: https://www.conseil-national.medecin.fr/code-deontologie/devoirs-patients-art-32-55/article-47-continuite-soins.
- 9.Témoignage — Coronavirus: “Les gars faut faire quelque chose”, Philippe Liverneaux, chirurgien à Strasbourg. Available through: https://france3-regions.francetvinfo.fr/grand-est/bas-rhin/strasbourg-0/temoignage-coronavirus-gars-faut-faire-quelque-chose-philippe-liverneaux-chirurgien-strasbourg-1818280.html.
- 10.Huh S. How to train the health personnel for protecting themselves from novel coronavirus (COVID-19) infection during their patient or suspected case care. J Educ Eval Health Prof. 2020;17:10. doi: 10.3352/jeehp.2020.17.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fathizadeh H., Maroufi P., Momen-Heravi M., Dao S., Köse S., Ganbarov K., et al. Protection and disinfection policies against SARS-CoV-2 (COVID-19) Infez Med. 2020;28:185–191. [PubMed] [Google Scholar]
- 12.Ağalar C., Öztürk Engin D. Protective measures for COVID-19 for healthcare providers and laboratory personnel. Turk J Med Sci. 2020;50:578–584. doi: 10.3906/sag-2004-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chirico F., Nucera G., Magnavita N. COVID-19: protecting healthcare workers is a priority. Infect Control Hosp Epidemiol. 2020;1(April) doi: 10.1017/ice.2020.148. [Published online ahead of print, 17 April 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coronavirus: en quoi consiste le stade 3 de l’épidémie? Available through: http://www.leparisien.fr/societe/coronavirus-en-quoi-consiste-le-stade-3-de-l-epidemie-06-03-2020-8273916.php.
- 15.Attestation de déplacement. Available through: https://www.gouvernement.fr/sites/default/files/cfiles/attestation-deplacement-fr-20200324.pdf.
- 16.Décret n° 2020-260 du 16 mars 2020 portant réglementation des déplacements dans le cadre de la lutte contre la propagation du virus covid-19. Available through: https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000041728476&categorieLien=id.
- 17.Décret n° 2020-264 du 17 mars 2020 portant création d’une contravention réprimant la violation des mesures destinées à prévenir et limiter les conséquences des menaces sanitaires graves sur la santé de la population. Available through: https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000041731767&categorieLien=id.
- 18.Coronavirus. Foire aux questions pour les agents hospitaliers Sur les sujets RH récurrents. Available through: https://solidarites-sante.gouv.fr/IMG/pdf/covid-19_faq_hospitaliers_sujetsrh.pdf.
- 19.Hong Y.R., Lawrence J., Williams D., Jr, Mainous A., III Population-level interest and telehealth capacity of US hospitals in response to COVID-19: cross-sectional analysis of Google Search and National Hospital Survey data. JMIR Public Health Surveill. 2020;6 doi: 10.2196/18961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Télésoin: c’est (enfin) parti! Available through: https://www.kineactu.com/article/11857-telesoin-c-est-enfin-parti.
- 21.Covid-19 — Ordre des masseurs-kinésithérapeutes. Available through: http://www.ordremk.fr/actualites/kines/covid-19.
- 22.Arrêté du 14 avril 2020 complétant l’arrêté du 23 mars 2020 prescrivant les mesures d’organisation et de fonctionnement du système de santé nécessaires pour faire face à l’épidémie de covid-19 dans le cadre de l’état d’urgence sanitaire. Available through: https://www.has-sante.fr/upload/docs/application/pdf/2020-04/arrete_du_14_avril_2020_completant_larrete_du_23_mars_2020.pdf.
- 23.Telemedicine has a big role in the coronavirus fight, but doctors say the laws remain murky. Available through: https://www.cnbc.com/2020/03/18/telemedicine-has-role-to-play-in-covid-19-fight-but-laws-are-murky.html.
- 24.Bachireddy C., Chen C., Dar M. Securing the safety net and protecting public health during a pandemic: Medicaid’s response to COVID-19. JAMA. 2020;323:2009–2010. doi: 10.1001/jama.2020.4272. [DOI] [PubMed] [Google Scholar]
- 25.Buvik A., Bugge E., Knutsen G., Småbrekke A., Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res. 2016;16:483. doi: 10.1186/s12913-016-1717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]