Highlights
-
•
A review of COVID-19 guidelines ensures the need of disruptive technologies.
-
•
COVID-19 enforces healthcare system to find alternatives for patients' treatment.
-
•
The disruptive technologies used to analyze and to restrict the spread of COVID-19.
-
•
The study aids healthcare team to detect the plan of treatment remotely and safely.
-
•
The analysis of COVID-19 patients ensures the importance of intelligent framework.
Keywords: Covid-19, Blockchain, Internet of medical things (iomt), Industry 4.0, Healthcare, 5 G
Abstract
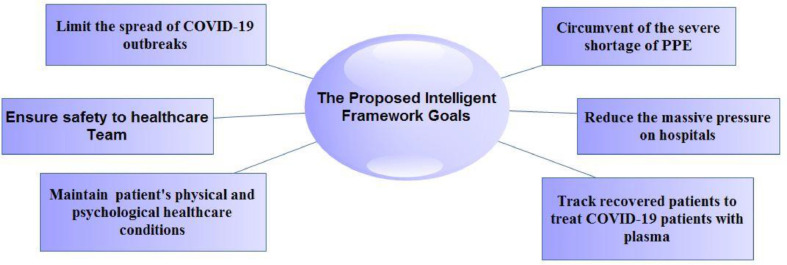
This paper describes a framework using disruptive technologies for COVID-19 analysis. Disruptive technologies include high-tech and emerging technologies such as AI, industry 4.0, IoT, Internet of Medical Things (IoMT), big data, virtual reality (VR), Drone technology, and Autonomous Robots, 5 G, and blockchain to offer digital transformation, research and development and service delivery. Disruptive technologies are essential for Industry 4.0 development, which can be applied to many disciplines. In this paper, we present a framework that uses disruptive technologies for COVID-19 analysis. The proposed framework restricts the spread of COVID-19 outbreaks, ensures the safety of the healthcare teams and maintains patients' physical and psychological healthcare conditions. The framework is designed to deal with the severe shortage of PPE for the medical team, reduce the massive pressure on hospitals, and track recovered patients to treat COVID-19 patients with plasma. The study provides oversight for governments on how to adopt technologies to reduce the impact of unprecedented outbreaks for COVID-19. Our work illustrates an empirical case study on the analysis of real COVID-19 patients and shows the importance of the proposed intelligent framework to limit the current outbreaks for COVID-19. The aim is to help the healthcare team make rapid decisions to treat COVID-19 patients in hospitals, home quarantine, or identifying and treating patients with typical cold or flu.
1. Introduction
The coronavirus disease (COVID-19) is denoted to a severe acute respiratory syndrome coronavirus 2 SARS-CoV-2. It was reported in Wuhan, China, in December 2019 with unexplained phenomena for cases (Wang et al., 2020a; Bai et al., 2020). The COVID-19 has been widespread for 213 countries worldwide, with a total of 41,908,988 confirmed cases, 1141,130 deaths and 31,100,678 recovered on 22 October 2020 (coronavirus, 2020). Unlike Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS), COVID-19 can be transmitted rapidly through contact human and infected surfaces (Mallapaty, 2020). Additionally, COVID-19 is very dangerous for patients with weak immune systems, the elderly, chronic disease (Tuli et al., 2020). The governments globally realized to take immediate procedures in many vital aspects to govern the crisis of COVID-19 outbreaks (Martin et al., 2020; Gharehgozli et al., 2020). The WHO assigns guidelines for COVID-19 cases include confirmed cases, probable cases, suspect cases, and contract cases. The confirmed cases are people with lab affirmation to the COVID-19 epidemic regardless of clinical signs and syndrome. The possible examples are suspect cases for whom testing for the COVID-19 virus is indecisive or whose trial could not be operated for any causes. The suspect cases are patients with an acute respiratory illness who are in contact with confirmed or probable COVID-19 cases in the last 14 days before symptom onset.
Every country in the world is under the threat of infection with COVID-19, especially the healthcare team and their families. There is no reassuring procedure evidence for any improvement in the next day (Jason et al., 2020). Due to the urgent need to analyze COVID-19, disruptive technologies are required to provide efficient, effective and low-cost analysis. These key technologies include artificial intelligence (AI), industry 4.0, Internet of Things (IoT), Internet of Medical Things (IoMT), big data, virtual reality (VR), Drone technology and Autonomous Robots, 5 G, and blockchain to achieve specific goals. In order to answer the questions on what are disruptive technologies and how they can be used, Table 1 presents the effective disruptive technologies that can be applied to limit the COVID-19 outbreaks based on literature (Lasi et al., 2014; Koro, 2015; Alladia et al., 2019 a; 2019 b; S Chen et al., 2020; Chamola et al., 2020; Javaid et al., 2019; 2020; Nabeeh et al., 2019a; R.P.. Singh et al., 2020) and our analysis. Additionally, the following disruptive technologies can be used jointly to meet the criteria for having an intelligent framework used in COVID-19 analysis.
Table 1.
The disruptive technologies used to limit the COVID-19 outbreaks.
| Technologies | Explanations | Benefits |
| 1. Artificial Intelligence (AI) | AI is a powerful tool and technique that makes computers to learn and think. AI can make predictions of patterns. | The AI can be used to predict the outbreak for COVID-19. The AI has analysis models to test the validity of the statistical data about COVID-19, consequently remove unwanted data. The AI develops robots to burden from the healthcare team some duties to perform the medical examination of patients. |
| 2. Industry 4.0 | Industry 4.0 augments industry advancements based on the focus on environmental conditions and the development of related technologies (Lasi et al., 2014). Industry 4.0 relied on the technology of IoT that provides organizations with resilient services. (Abdel-Basset et al., 2019) |
Industry 4.0 developed many applications for the sake of solving healthcare problems. Industry 4.0 can analyze the patients' real data with various technological methods to increase the accuracy of the rapid and accurate diagnosis and treatment (Javaid et al., 2019). Industry 4.0 can be useful in following up on the first vital signs for COVID-19 hospitalized patients or home quarantine patients. |
| 3. Internet of Things (IoT) | The connection between objects over a specific network without human intervene. People could access the needed content remotely from anywhere to attain the proper medical service (Nabeeh et al., 2019a). The IoT, an essential part of the revolution of Industry 4.0, is the connection between services and semantics via wireless protocols (Koro, 2015) . |
IoT is a useful technology to prevent COVID-19 outbreaks. The sensors can make a periodic follow up for hospitalized patients or home quarantine patients (Ting et al., 2020). IoT can ensure that the healthcare team is taking the PEE right conditions. The IoT can be used to trace the contact people with COVID-19 patients. |
| 4. Internet of Medical Things (IoMT) | IoMT is a contemporary mean for connecting the medical sensor devices and the associated applications with healthcare technology systems via networks connectivity (R.P.. Singh et al., 2020) | The IoMT takes the medical team's burden to perform data sharing, monitor patient reports, track patients and contact, gather vital signs, etc. (R.P.. Singh et al., 2020). The use of IoMT can enhance the physical and psychological healthcare of hospitalized patients or home quarantine patients due to the feeling of confidence that everything can be under control with the medical team quickly. Moreover, the comfortability for the medical team and the presentation for the severe shortage of PPE. |
| 5. Big Data | Big data is a discipline that analyzes and extracts information and features from large and complex data that cannot be traditionally processed with application software. | The big data can make a practical analysis of the data generated from sensors and healthcare databases to produce many statistics about the COVID-19 outbreaks and other reports to limit the effect of pandemic across the world (S Chen et al., 2020). |
| 6. Virtual Reality (VR) | VR is a technology used in a computer program to create a suitable simulated environment. People can participate in work in real-time through a distributed whiteboard. | VR offers an appropriate environment for a video call between the healthcare team with patients in hospitals or in-home quarantine. The VR can improve patients' psychological side, especially the home quarantine patients, to make them feel that the healthcare team follows up on all the vital signs and any consequence complications of COVID-19 (Manto et al., 2020). |
| 7. Drone technology and Autonomous Robots | Drone technology is a flying robot controlled by a software application. Like drone technology, the autonomous robot has the capability to carry out specific responsibilities without the intervention of external agencies (Chamola et al., 2020). | Drone technology can be used to reach specific areas in the infected country and minimize human interaction (Chamola et al., 2020). The robot can take many responsibilities from the healthcare team to track and manage some medical care services to patients in hospitals or in-home quarantine |
| 8. 5G | The fifth-generation technology can support global mobile networks (Qualcomm et al., 2020). The 5 G provides more excellent characteristics than 3 G and 4 G. | The 5 G can cooperate with the pandemic of COVID-19 by providing the healthcare team rapid speed communication between assistance to improve the track of COVID-19 and continuously monitoring and analyzing the patients' cases. |
| 9. Blockchain | Blockchain is a transaction record between two parties (Alladia et al., 2019 a). The recorded transaction was used to verify the actions that happened. The blockchain has various applications in different life aspects. |
The blockchain can be used to limit the pandemic of COVID—19 by making the integration of different data sources (Alladi et al., 2019 b) The integrated source can be statistically analyzed to extract essential features for the healthcare team and governments. |
Hence, the use of disruptive technologies reduces the burden of the healthcare team in the COVID-19 pandemic. The use of smart technologies can observe the patients affected by COVID-19. The public healthcare organizations recommend the vital role for disruptive technologies to public health for COVID-19.
The rest of this study is structured as follows. Section 2 presents the related work with the current COVID-19 review and motivation of our work. Section 3 describes our intelligent framework using disruptive technologies in detail for COVID-19 analysis. Section 4 illustrates an empirical case study to show the importance of the proposed intelligent framework. Section 5 explains the results and how disruptive technologies and methods offer better COVID-19 analysis. Section 6 presents two topics for discussion. Section 7 sums up the conclusion and future work.
2. Related work
This section presents the related work for the current COVID-19 status and the framework using disruptive technologies for COVID-19 analysis.
2.1. The current COVID-19 status
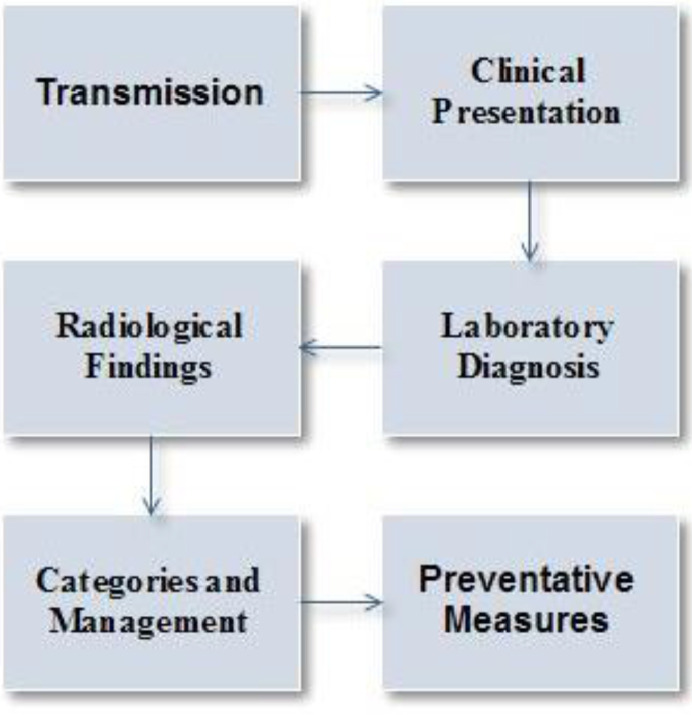
The best practice approaches are suitable for many disciplines, particularly for health, since they can reduce risk and improve efficiency (Melnyk and Fineout-Overholt, 2011). The medical best approach provides a brief review for COVID-19 about the way of transmission, clinical presentation, Laboratory Diagnosis, Radiological findings, Categories and Management, and preventative measures presented in Fig.1 with details as follows:
-
I.
Transmission
There are several studies on the pathophysiological properties and the propagation mechanism for COVID-19 (Chamola et al., 2020). Initially, COVID-19 infected people interacted directly with infected animals. Nowadays, rapidly the outbreaks of COVID-19 are transmitted directly from human to human. The transmission mechanisms between human to human are classified as follows.-
a.Respiratory transmissionThe SARS-CoV-2 is a respiratory virus that is mainly transmitted across the respiratory droplets. The CDC advises people to maintain at least a 6-foot distance between people. Since at least 25% of people may be asymptomatic at a time (CDC, 2020).
-
b.Aerosol transmissionThe SARS-CoV-2 remains viable in aerosols for three hours, according to the experiment (MD, 2020). Los Angeles Times reported that 45 people became infected with COVID-19 and at least two people died with the aerosol transmission (MD, 2020).
-
c.Contact transmissionThe contact transition occurs when the viral particles are emitted from the respiratory tract from an infected person on the surface. Consequently, another person touches the surface, and the personal touch nose, mouth, or eye. According to Wang et al. (2020a) and Read (2020), COVID-19 is more stable on plastic than copper and cardboard.
-
a.
-
II.
Clinical presentation
The incubation period for COVID-19 extended to fourteen days, with a median of four to five days from exposition to symptoms onset (Guan et al., 2020; Lauer et al., 2020). Guan et al. (2020) announced that 97.5% of people infected with COVID-19 who develop symptoms would do so during 11.5 days of SARS-CoV-2 infection. The manifestation of infected people with COVID-19 will experience the following symptoms in Table 2 (Leiwen et al., 2020; Chen et al., 2019; Huang et al., 2020; Xu et al., 2020; Wu et al., 2020; L. Pan et al., 2020).
-
III.
Laboratory Diagnosis
The most frequent abnormalities in COVID-19 are lymphopenia, increased values of C-Reactive Protein (CRP), lactic dehydrogenase (LDH), erythrocyte sedimentation rate (ESR) and d-dimer, as well as low concentrations of serum albumin and hemoglobin, less common low platelet, increase Serum Creatinine Kinase (CK), Alanine aminotransferase (ALT), Aspartate Aminotransferase (AST) (Giuseppe and Plebani, 2020).
-
IV.
Diagnostic Testing
The respiratory samples are endorsed from the lower respiratory tract, including sputum, bronchoalveolar lavage, and tracheal aspirate (when possible). When it is not possible, samples from the upper respiratory tract are also adequate. Generally, the collection of a combined nasopharyngeal swab and the oropharyngeal swab is recommended (Pan American Health Organization (PAHO), 2020).
The molecular method relied on the disclosure of COVID-19 virus nucleic acid RNA by real-time polymerase chain reaction (RT-PCR) assays. RNA extracted from samples using any standard extraction protocols or kits.
-
V.
Radiological findings
The imaging radiology indicates that in a patient with COVID-19 and worsening respiratory status (Rubin Geoffrey, 2020). The imaging may be a chest X-ray or CT chest. The chest x-ray shows airspace opacities (Wong et al., 2019) and 1) ground-glass opacities; 2) abnormal paving appearance; 3) air space consolidation; 4) bronchovascular thickening in the lesion and 5) traction bronchiectasis (Wang et al., 2020a; Javaid et al., 2020; L. Pan et al., 2020; Shi et al., 2020; Lee et al., 2020):
-
VI.
Categories and Management
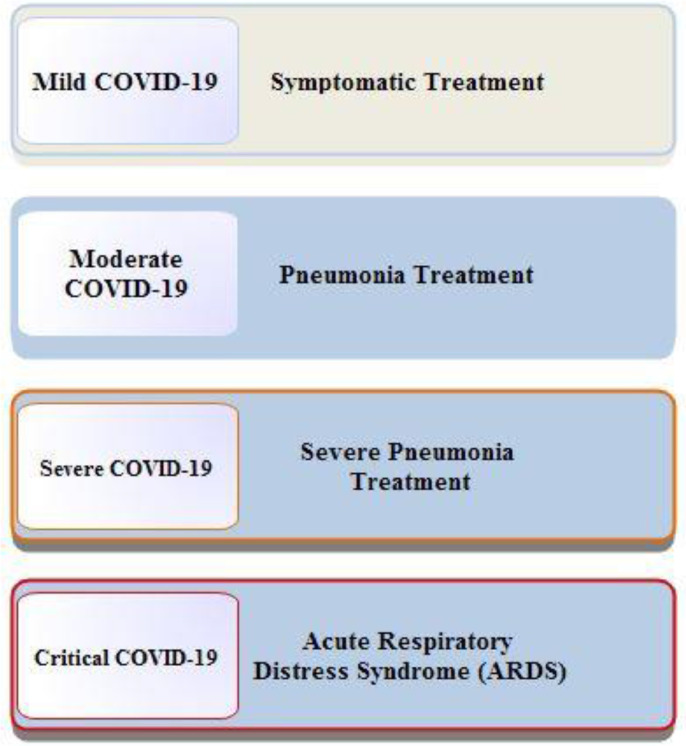
The COVID-19 are classified into five main categories and modeled in Fig.2. The description of types are mentioned as follows (Zhoa et al., 2020; Clinical Management of Covid-19, 2020):-
1.Mild COVID-19: Symptomatic treatmentWHO (2020) advice infected people with COVID-19 with complete isolation and take symptomatic treatment. e.g., antipyretics to treat fever and pain, appropriate nutrition, and suitable rehydration
-
2.Moderate COVID-19: Pneumonia treatmentWHO (2020) advises moderate COVID-19 patients with complete isolation and recommends a close monitor for moderate patients to detect signs and symptoms of progress or deterioration. The urgent provision techniques should be carefully performed to monitor a close follow up to determine the escalation of medical care.
-
3.Severe COVID-19: Severe pneumonia treatmentThe severe COVID-19 patients could be treated by equipped with pulse oximeters, functioning oxygen systems and disposable, single-use, oxygen-delivering interfaces (nasal cannula, Venturi mask, and mask with reservoir bag). WHO (2020) advises the rapid administration of supplemental oxygen therapy to any patient with emergency signs and any patients without emergency signs and oxygen saturation (SpO2) < 90%.
-
4.Critical COVID-19: Acute Respiratory Distress Syndrome (ARDS)The patients with critical COVID-19 treated by a trial of high-flow nasal oxygen HFNO, non-invasive ventilation – continuous positive airway pressure (CPAP), bilevel positive airway pressure (BiPAP) may be used.
-
1.
-
VII.
Preventive measures
The public health recommendations for the prevention of the spread of COVID-19 guidelines are recommended as follows (Clinical Management of Covid-19, 2020):
Keep on personnel preventive measures (e.g., hand hygiene, respiratory etiquette and face covers, environmental disinfection).
Keep on social distances between people in work, governmental agencies, etc..
Keep on the safety of people by staying at home and close non-essential business closure (Yoo et al., 2020; Nakamura et al., 2020).
Apply restrictions on public communications.
Apply travel restrictions with the screening of travelers.
Identify and isolate infected cases with COVID-19.
Keep contact tracing for people to limit the pandemic of COVID-19 outbreaks.
Table. 2.
The presentation for symptoms of COVID-19.
| COVID-19 Symptoms | Percentages |
| Fever | 83%-99% |
| Dry Cough | 59%-82% |
| Fatigue | 44%-70% |
| Anorexia | 40%-84% |
| Shortness of breath | 31%-40% |
| Sputum production | 28%-33% |
| Myalgias | 11%-35% |
| Headache, confusion, rhinorrhea, sore throat, hemoptysis, vomiting, and diarrhea | <10% |
| Loss of smell (anosmia) | Variable/undetermined |
| Loss of taste (ageusia) | Variable/undetermined |
The influence of COVID-19 on the healthcare team's first-line defense, the patient's physical and psychological healthcare conditions, the severe shortage of (PPE) for the medical team, and massive pressure on hospitals can impose a hazardous consequence. Since March 2020, WHO officially declared COVID-19 as a pandemic. The outbreaks cause the symptoms of discomfort, disappointment, and disquieted not only for ordinary people but also for medical service providers (Montemurro, 2020). Li et al. (2020) stated that medical staff members bear Vicarious traumatization (VT) of non-front-line medical staff is more earnest than that of front-line medical staff. The outbreaks for COVID-19 placed a handicap on healthcare with an improbable workload and provision of all means of PPE. Indeed, the COVID-19 pandemic has spread in a frightening way around the world, which leads to a severe shortage of medical team care and PPE. For patients and the healthcare team, psychiatric symptoms without a mental illness may occur and distress the caregivers of affected individuals (Kelvin et al., 2020). Unfortunately, most healthcare givers in isolation units in COVID-19 do not receive any preceded preparation or training or give proper mental healthcare (Lima et al., 2020). In Barbisch et al. (2015), the pandemic of COVOD-19 leads the healthcare givers to a sense of collective hysteria that leads to despairing and hopeless measures. In India, suicidal cases were recorded. Additionally, two nurses in Italy committed suicide due to the volume of workloads and fear of outbreaks of COVID-19 to patients (Goyal et al., 2020). A devoted national suicide prevention lifeline was stimulated for emotional adversity for the pandemic COVID-19 to prohibit suicide cases in the US.
The healthcare team noticed that patients who suffered from the COVID-19 pandemic are subjected to anxiety and panic attacks, which leads to the need for medical and psychological support (Katafuchi et al., 2020). According to NICE guideline [NG163], (2020):
-
1.
Explore the causes of anxiety.
The health care team directly contacts patients to decrease and to talk about his/her anxiety and provide effective communication and orientation for patients—the provider of adequate ways for rest (e.g., adequate light brightens, bed, etc.). Moreover, health workers provide explanations to the caregivers on how they can help patients physically and emotionally.
-
2.
Medically, patients can take some drugs. e.g., Benzodiazepine can be tried to relieve anxiety.
As a result of the need for direct communication between the healthcare team and infected patients, the infection control recommended for the healthcare team to use fitted respirator masks (e.g., N95 respirators, FFP2), moreover to the other PPE to assure the safety and to prevent the COVID-19 outbreaks (Jason et al., 2020). The outbreak of COVID-19 in 213 countries leads to a severe shortage of PPE and healthcare teams, which encourage technological solutions to decrease the pandemic crisis consequent on humanity. The study addressed the main milestones for COVID-19.
2.2. The motivation and rationale of using a framework approach
This section describes the motivation and rationale to adopt our framework using disruptive technologies for COVID-19 analysis. In short, an intelligent framework is proposed since it can blend different types of disruptive technologies to conduct an effective COVID-19 research analysis. The intelligent framework concerns keeping the healthcare team healthy, keeping the physical and psychological healthcare of patients, and preventing the severe shortage of PPE, reducing the burden in hospitals tracking recovered patients to treat COVID-19 patients with plasma. The intelligent framework adopts the use of leading technologies of AI, industry 4.0, IoT, IoMT, big data, virtual reality (VR), Drone technology and Autonomous Robots, 5 G, and blockchain to achieve the proper goals.
The proposed intelligent framework is designed to accommodate the COVID-19 crisis that affected human survival worldwide. The aim is to help governments with pandemic management. The intelligent framework is focused on limiting the spread of COVID-19 outbreaks, providing a safe environment for the medical team and health caregivers, and maintaining the patient's physical and psychological healthcare. The framework also manages the severe shortage of PPE, reduces the massive pressure on hospitals, and tracks recovered patients to treat COVID-19 patients, as mentioned in Fig.3.
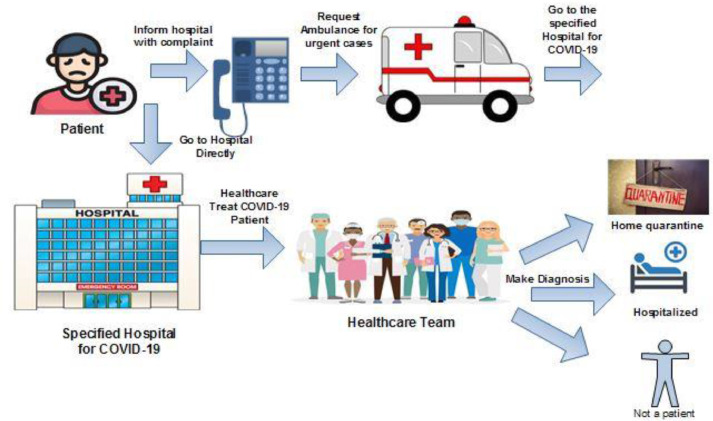
3. The framework using disruptive technologies for COVID-19 analysis
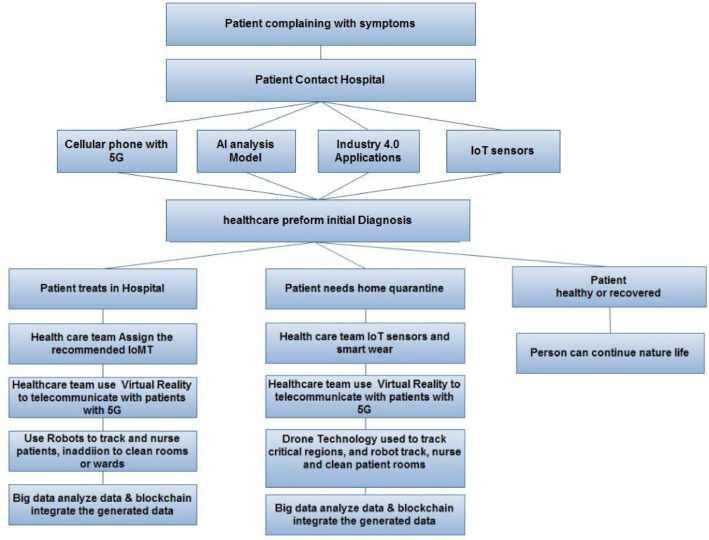
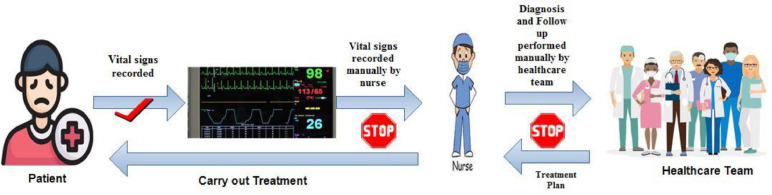
This section describes our intelligent framework using disruptive technologies for COVID-19 analysis. Our study focuses on traditional procedures without using the intelligent framework to illustrate the importance of research concerning the framework goals. The conventional procedures are presented started from patient requests for help or complaint until the healthcare team makes a diagnosis for the patient to be hospitalized, home quarantine, or healthy, as mentioned in Fig.4.
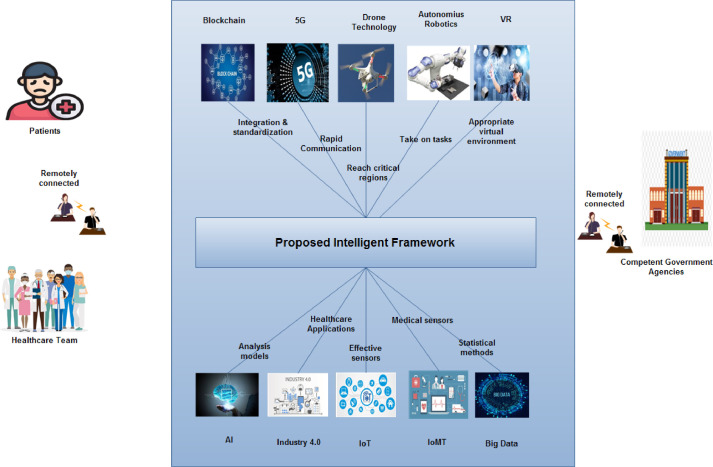
In order to achieve study goals, a general framework is proposed to include technologies of AI, industry 4.0, IoT, IoMT, big data, VR, drone and robotics technology, 5 G, and blockchain modeled in Fig.5. In Fig. 5, the proposed intelligent framework focused on three main actors: 1) Patients, 2) Healthcare team and 3) Competent government agencies. The three main actors can remotely connect with the intelligent framework to take the proper services. The patients can remotely diagnose, treated, and monitored. The healthcare team can perform medical services to patients remotely. The competent governmental agencies can remotely monitor and retrieve required data on time for urgent and regular situations. The proposed intelligent framework adopted: 1) AI with analytical models for the healthcare system, 2) Industry 4.0 with medical applications, 3) IoT with effective sensors to help patient and healthcare team, 4) IoMT with medical sensors with hospitalized and home quarantine patients, 5) Big data used statistical methods to perform an operation on healthcare system data, 6) VR provided healthcare team and patients with appropriate virtual environment, 7) Autonomous robotics and drone technology take on critical tasks from humanity, 8) 5 G used in rapid communication between healthcare system actors and patients, and 9) Blockchain applied integration and standardization for the healthcare system.
Fig. 5.
The general intelligent framework proposed to limit the pandemic of COVID-19.
The intelligent framework proposed systematic procedures to achieve the study goals, as mentioned in Fig. 6. The systematic procedures are presented to patients that have complained about COVID-19 symptoms. The patient can contact the hospital according to available technologies, e.g., cellular phones, industry 4.0 applications, IoT sensors, or AI analysis models. The healthcare team receives a complaint to address patients to a suitable disease category. The healthcare team can decide to treat the patient in-home quarantine, hospital, or treat patients with typical cold or flu. For hospitalized patients, the healthcare team assigns suitable IoMT according to the patient category. The healthcare team can remotely communicate and treat patients with virtual reality and robot technologies. For home quarantine patients, the healthcare system assigns the available and suitable IoT sensors, e.g., smart wears, to monitor and track patients' vital signs and locations. The healthcare team can monitor and treat home quarantine patients according to the current readings for vital signs of IoT sensors. In addition, drone technology and robotics are assessed to track, nurse, and clean patient rooms. The healthcare system data can be integrated and analyzed with the aim of big data and blockchain technologies. For patients, recovered or healthy, have treated with some medical advice or guidelines.
Fig. 6.
Procedures for the proposed intelligent framework to limit the COVID-19 outbreaks.
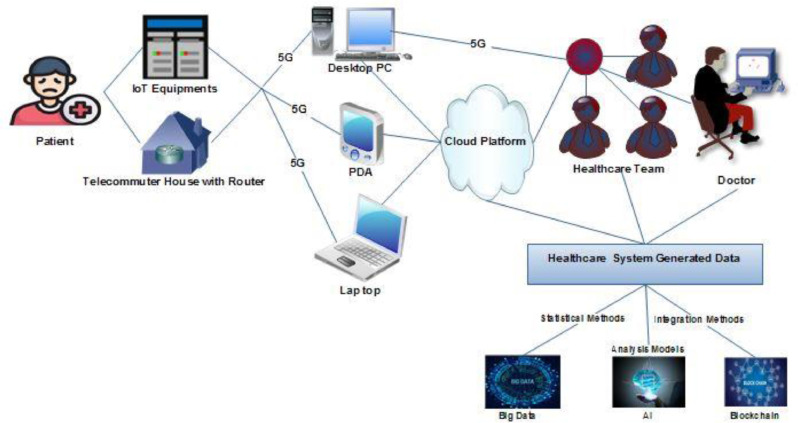
The AI can be useful for the monitoring and prediction for COVID-19 patients and the outbreaks curve. The neural networks and data mining can be developed to extract main features for the COVID-19 and provide daily solutions for the pandemic (Vaishya et al., 2020). Industry 4.0 is an automatic solution for manufacturing purposes. Industry 4.0 can easily use digital information to gather, transmit, store, analyze, and monitor the healthcare system. The technology of industry 4.0 is a novel method to isolate COVID-19 patients to reduce the high death rate, improve drug production, and enhance treatment of COVID-19 (Javaid et al., 2020). The IoT provided useful technological sensors to help fight the current crisis, especially to patients for home quarantine treatment. Fig. 7 illustrates the importance of using IoT technologies to support the proposed framework. The IoT technology, especially for home quarantine, aided the COVID-19 patients to remotely transfer the complaint and vital symptoms to the healthcare system across the IoT equipment and network with a cellular phone or any communication to inform the healthcare team and to receive remote diagnosis and treatment.
Fig. 7.
The proposed intelligent framework treatment using IoT technologies.
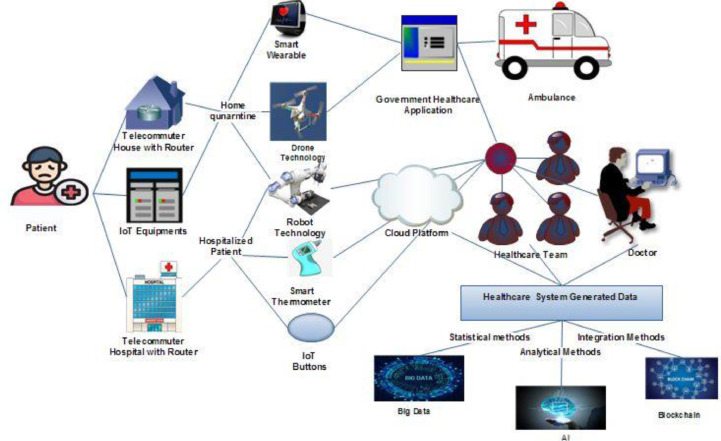
The IoMT denoted the use of IoT in the field of medical healthcare. The IoMT in the COVID-19 pandemic used medical instruments and applications to provide healthcare services to patients in hospitals or under home quarantine, in addition to producing valuable big data for healthcare systems and related governmental sectors. Nowadays, most people are using smartphones for different purposes; the IoMT is proposed a possible number of available medical application services (Hassija e al., 2019). The IoMT provides potential applications in healthcare that can significantly serve in the pandemic of COVID-19. The applications include smart healthcare, patient tracking, remote health monitoring, Emergency cautions, and Wearable devices (R.P.. Singh et al., 2020). The integrated technologies in IoMT are presented in the proposed intelligent framework as follows (Chamola et al., 2020):
-
1.
Smart thermometers
Kinas, a US technology manufacture, developed a smart thermometer to scan people's temperature. During the COVID-19 pandemic, the intelligent thermostat has been connected to mobile applications to make the patients' data available for the related governmental sectors, e.g., the healthcare system. The Kinsa's maps regarded toe be consistent in identifying the high spotted areas for COVIID_19 outbreaks (Mcneil, 2020)
-
2.
IoT buttons
Many hospitals in Canada use IoT buttons to ensure cleaning standards and reduce hospital-acquired infection (HAIs) numbers (Watson et al., 2020). The main advantage of the IoT buttons is the adequality to be attached to any superficies (D'mello et al., 2020).
-
3.
Telemedicine
It provides the healthcare team the ability to remotely diagnose and treat patients in various locations using IoMT technology. Various telemedicine applications are evolved, e.g., teleconsultation software, etc. (Chamola et al., 2020). While aiming to get accurate representation, an integrated framework of intelligent methods should be presented using robotic and drone technology, 5 G, smartwatches, and blockchain.
In Fig.8, the data generated from the IoMT sensors classified according to the place of treatment, either hospitalized or home quarantine. The IoMT sensors of smart wearable, robot technology, and drone technology in-home quarantine treatment associated with governmental healthcare applications to direct the non-emergent data to the healthcare system. The IoMT sensors can send data to emergency agencies, such as calling an ambulance to COVID-19 patients based on tracking the patient's location according to police regulations to ensure that patient does not move and break out the home quarantine. For hospitalized patients, the smart hospital can send patients data to the healthcare team to be monitored, diagnosed, and treated. The data generated from the IoMT sensors and healthcare systems can be managed and analyzed with significant big data, AI techniques, and big data to make useful reports for governments and society (AMD Telemedicine., 2020; Nathali et al. 2020). In addition to the track, COVID-19 outbreak experts and decision-makers can use the generated data to aid researchers in applying MCDM methods with neutrosophic theory to produce efficient and accurate decisions for the COVID-19 pandemic (Nabeeh et al., 2019b; Nabeeh, 2020, 2020a; Nabeeh et al., 2020b). Fig. 8 illustrates the importance of IoMT with the proposed intelligent framework to achieve study goals.
Fig. 8.
The proposed intelligent framework treatment using IoMT technologies.
Virtual reality is extended to the proposed intelligent framework to ensure patients' physiological support in hospitals or in-home quarantine patients. The patients' ambition to allow the healthcare team to manage or intervene any time improves the healing rates, especially for mild and moderate COVID-19 patients. Drone technology is useful in cases of quarantine patients because it can make the full map for the hotspot cases and help decision-makers make decisions with such emerged cases—moreover, drone technology aid police in reaching to handle emergent situations (Cyient, 2020). Robotics technology is a mild stone for the proposed intelligent framework since the robot can take a burden from the healthcare team. For patients in hospitals, robots can visit patients and track their development and cases. On another side, the physiological support for patients will provide many improvement signs in physical healthcare. The robot technology can be beneficial in cleaning teams and services from the people responsible for cleaning the patient's wards and rooms. Regarding the mild and moderate COVID-19 patients, the study recommends that robots visit patients instead of the healthcare team, provide patients with the first aids, and provide vital responsibilities to remove the burden of cleaning and to cook healthy food from COVID-19 patients. The robot can maintain the healthcare for patients' physical and psychological healthcare conditions, decrease the direct contact between healthcare and COVID-19 patients, and limit the decrease of outbreaks aiding governments in reducing hospitals' massive pressure. The 5 G as a speed communication can maintain direct contact between the healthcare team and patients in the case of new cases and work as an efficient link between intelligent framework methods. The blockchain is used to ensure the standardizations for the various healthcare systems and is used as a single and consistent block.
4. An empirical case study
The primary objective of the empirical case study is to highlight how the intelligent framework can be applied with respect to the real situations in the daily healthcare organization. As mentioned in Fig. 2 , which describes the categories for COVID-19 patients, the case study performs a numerical description according to specific clinical parameters (Clinical Management of Covid-19, 2020). The COVID-19 has many symptoms, as mentioned in table1. The severity of the disease can be categorized according to the following clinical parameters mentioned in table 3 . The numerical parameters are described in decimals or percentages. The binary parameters are denoted as 0 (not found), 1 (found). The descriptive parameters are described in the text. The descriptive parameter of the Chest x-ray imaging category is mentioned as follows:
-
1.
Mild Covid-19 patients: No evidence for pneumonia, as mentioned in Fig. 9 and denoted to be symbolled with 0.
-
2.
Moderate Covid-19 patients: They have pneumonia symptoms, as mentioned in Fig. 10 and denoted to be symbolled with 1.
-
3.
Severe Covid-19 patients: They have severe pneumonia symptoms, as mentioned in Fig. 11 and denoted to be symbolled with 2.
-
4.
Critical Covid-19 patients: Bilateral opacities and lung collapse may occur, as mentioned in Fig. 12 and denoted to be symbolled with 1.
Fig. 1.
Guidelines for the basic information about COVID-19 (Clinical Management of Covid-19, 2020).
Fig. 3.
The main goals for the proposed intelligent framework.
Fig. 4.
Traditional Procedures for COVID-19 patient's treatment.
Fig. 2.
The workflow for the main categories affected COVID-19 patients.
Table. 3.
The data type for differentiation of COVID-19 patients' categories.
| Numerical parameters | Binary parameters | Descriptive parameters |
| Fever | Cough |
Chest x-ray |
| Respiratory rate | Dyspnea | |
| Oxygen saturation | Mechanical Ventilations |
Fig. 9.

The chest X-ray for mild COVID-19 patients.
Fig. 10.

The chest X-ray for moderate COVID-19 patients.
Fig. 11.

The chest X-ray for severe COVID-19 patients.
Fig. 12.
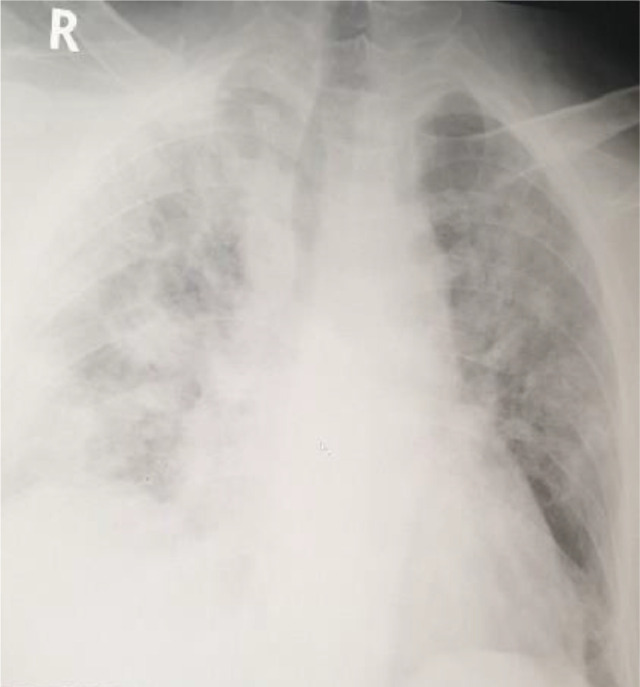
The chest X-ray for critical COVID-19 patients.
The numerical case study can be applied to Mansoura University Hospitals Quarantine. The healthcare team provides research with samples of 20 patients with corresponding clinical parameters and the healthcare team suggestions treatment for COVID-19 patients. Table 4 mentions the main guidelines to address patients to their suitable category. Indeed, there are many clinical varieties in the cases of COVID-19. Table 5 presents real data for COVID-19 cases, and the diagnosis may be variant from one case to another. The severity of cases can be determined with the most commonly used parameter results aggregated in table 5. Table 5 shows the final diagnosis for COVID-19 patients as mild, moderate, severe, or critical. Each category can be treated according to guidelines mentioned in Fig.2.
Table. 4.
Definitions for different COVID-19 patient's categories according to clinical parameters.
| Categories | Fever | Cough | Dyspnea | Fast Breathing | Chest X-ray | Oxygen Saturation | Mechanical ventilation |
| Mild | × | × (Respiratory rate<22 breath per min) | No evidence of pneumonia | >94% | × | ||
| Moderate | (Respiratory rate<30 breath per min) | Evidence of pneumonia (not severe) | 90%-94% | × | |||
| Severe | (Respiratory rate> 30 breath per min | Evidence of severe pneumonia. | < 90% | × | |||
| Critical | (Respiratory rate> 30 breath per min | Bilateral opacities, lung collapse, may occur | <85% |
Table 5.
Clinical parameters for samples of COVID-19 patients.
| Patients | Fever (Temperature) | Cough | Dyspnea | Respiratory rate |
Chest X-ray |
Oxygen Saturation | Mechanical ventilation | Category |
| 1 | 38.1 | 1 | 0 | 27 | 0 | 92% | 0 | Moderate |
| 2 | 37.7 | 1 | 0 | 20 | 0 | 97% | 0 | Mild |
| 3 | 38 | 1 | 1 | 29 | 1 | 93% | 0 | Moderate |
| 4 | 39.2 | 1 | 1 | 39 | 3 | 81% | 1 | Critical |
| 5 | 37.5 | 1 | 0 | 19 | 0 | 99% | 0 | Mild |
| 6 | 38.9 | 1 | 1 | 34 | 2 | 89% | 0 | Severe |
| 7 | 39.4 | 1 | 1 | 41 | 3 | 78% | 1 | Critical |
| 8 | 38.2 | 1 | 1 | 29 | 1 | 94% | 0 | Moderate |
| 9 | 39 | 1 | 1 | 36 | 2 | 88% | 0 | Severe |
| 10 | 37.7 | 1 | 0 | 22 | 0 | 97% | 0 | Mild |
| 11 | 39.2 | 1 | 1 | 32 | 2 | 90% | 0 | Severe |
| 12 | 38.4 | 1 | 1 | 28 | 1 | 93% | 0 | Moderate |
| 13 | 39.7 | 1 | 1 | 37 | 3 | 83% | 1 | Critical |
| 14 | 37.6 | 1 | 0 | 18 | 0 | 99% | 0 | Mild |
| 15 | 39 | 1 | 1 | 31 | 2 | 87% | 0 | Severe |
| 16 | 38.3 | 1 | 1 | 24 | 1 | 94% | 0 | Moderate |
| 17 | 39.5 | 1 | 1 | 37 | 3 | 80% | 1 | Critical |
| 18 | 39.8 | 1 | 1 | 41 | 3 | 79% | 1 | Critical |
| 19 | 37.6 | 1 | 0 | 21 | 0 | 98% | 0 | Mild |
| 20 | 38.4 | 1 | 1 | 32 | 2 | 89% | 0 | Severe |
The case study shows the direct interaction between the healthcare team and patients, which leads to the great importance for the proposed framework. Some hospitals have an electronic monitor to read the vital signs for patients and other hospitals, depending on human intervention in all medical processes. Hospitals have a monitor to record vital signs (Ammenwerth et al., 2007). However, reading results cannot be transferred automatically to the healthcare system. The healthcare team (e.g., nurses) must save the monitor readings and transform the results into the proper format to the healthcare team (e.g., Doctors). The systematic procedures for the traditional use of monitor are presented in Fig. 13 . The procedures are automatically performed to record vital signs with a monitor. However, the other procedures need humans to intervene such that way, and the nurse needs to record the patient's vitals manually and inform doctors with clinical parameters. The healthcare diagnosis the category of disease and puts the treatment plan. The nursing team carries out the treatment plan to patients.
Fig. 13.
The traditional procedures for the use of monitor in hospitals.
The intelligent framework limits the spread of COVID-19 outbreaks provides a safe environment for the medical team and health caregivers and maintains the patient's physical and psychological healthcare. The framework also manages the severe shortage of PPE, reduces the massive pressure on hospitals, and tracks recovered patients to treat COVID-19 patients.
In the light of Fig.12, the stop symbols can be handled remotely with the proposed intelligent framework. The initial diagnosis can be applied with disruptive technologies of an intelligent framework using AI, IoT, and IoMT technologies via 5 G and cloud platforms. The medical healthcare team can decide to treat patients in-home quarantine, hospitalized, or identify or treat patients with typical cold or flu. The drone technology can scan critical regions with emitted people to limit the COVID-19 outbreaks regions. The robot technology takes a massive burden from the healthcare team and government and can treat and track COVID-19 patients. In addition, they are taking cleaning and cooking duties from patients and healthcare givers. The healthcare system data can be processed to produce valuable and predictive results via AI models, big data, blockchain. Finally, the proposed intelligent framework can be a safe environment for COVID-19 patients to be remotely monitored, diagnosed, and treated.
5. Results and how disruptive technologies and methods offer better COVID-19 analysis
5.1. Neutrosophic and multiple-criteria decision-making (MCDM) methods
The proposed intelligent framework is aimed to limit the COVID-19 outbreaks. An innovative breakthrough in current disruptive technologies and its offering can become essential for making better COVID-19 analysis. The contemporary literature presented in Table 1 does not include Neutrosophic and Multiple-criteria decision-making (MCDM) methods (Abdel-basset and Mohamed. R., 2020a; Abdel-Basset et al., 2020a). Therefore, the framework offers something new to demonstrate how our work.
While aiming to show the applicability of the proposed study, real data are collected from Jaber Alahmad Al-Sabah Hospital Kuwait for COVID-19 patients. Real data are collected from the healthcare system, healthcare teams, and healthcare givers to provide the decision-makers of the healthcare team to categorize patients with their symptoms to be hospitalized, home quarantine, normal cold, flu, or healthy person. The study adopts the neutrosophic theory with the MCDM method of TOPSIS. Since the pandemic of COVID-19 is a complex problem with various alternatives and criteria with conditions of uncertainty.
In results and discussion, the study applies the neutrosophic theory with TOPSIS (Abdelbasset et al., 2019; Nabeeh et al., 2019a, Nabeeh et al., 2019b). The study regards four decision-makers from the healthcare team to record their perspectives about the COVID-19 symptoms, patients' symptoms, and recovery steps. The research includes 20 patients as alternatives and 16 common symptoms recommended with the studies (Leiwen et al., 2020; Chen et al., 2019; Huang et al., 2020; Xu et al., 2020; Wu et al., 2020; L. Pan et al., 2020) as criteria. The results provide the healthcare team with neutrosophic weighted criteria according to AHP procedures and ranked symptoms of patients according to TOPSIS. The requirements are considered, as mentioned in Table 6 . The alternatives are considered 20 patients from A1 to A20 with details in the Appendix A.
Table 6.
The criterions considered in discussion and results.
| Criteria | Symptoms |
| C1 | Dry Cough |
| C2 | Fever |
| C3 | Fatigue |
| C4 | Shortness of breath |
| C5 | Anorexia |
| C6 | Sputum production |
| C7 | Headache |
| C8 | Myalgias |
| C9 | Confusion |
| C10 | Rhinorrhea |
| C11 | Sore throat |
| C12 | Vomiting |
| C13 | Diarrhea |
| C14 | Hemoptysis |
| C15 | Loss of smell (anosmia) |
| C16 | Loss of taste (ageusia) |
The results and discussions show the priorities of patients according to the weighted results of recommended symptoms. The results take a massive burden from the healthcare team. The healthcare team can do a quick review in the light of results to decide to treat patients in hospitals, quarantine at home, or identifying and treating patients with typical cold or flu.
5.2. How AI can impact COVID-19 research
Healthcare services are demonstrated with continuous challenges due to the prospect of the appearance of variant types of bacteria, viruses, and diseases (Chang, 2018). The case of COVID-19 is studying from all governmental aspects, trying to reach solutions to save humanity. This section illustrates how disruptive technologies and applications from the literature can be practically applied to the proposed intelligent framework.
The core applications and technologies of AI for COVID-19 are concluded by Vaishya et al. (2020) as follows:
-
1.
Early disease detection and diagnosis
The AI can be used to make analysis with irregular symptoms and produce an alarm to the healthcare system. The AI can be valuable in the COVID-19 diagnosis of patients with medical image technologies such as Computed tomography (CT), Magnetic resonance imaging (MRI) scan to patients.
-
2.
Observation and management
The AI can apply neural networks to monitor and to treat COVID-19 patient to produce remote solutions to limit the pandemic of COVID-19 outbreak (Haleem et al., 2019; Biswas and Sen, 2020; Chen S et al., 2020)
-
3.
Follow contact with the patients.
The hotspot can be helpful to monitor and to predict disease categories to make rapid diagnosis and treatment.
-
4.
Projection of infected person & mortality prediction
The technology can monitor and follow-up the evolution of the diseases from available governmental, social, media data and platforms to limit the outbreaks. AI applications can predict COVID-19 patients and the death rate.
-
5.
Medications and vaccines development
The technologies and applications can analyze data using statistical methods and algorithms. The AI can be helpful to rapid vaccine development to make diagnostic tests vaccination progress (Ren et al., 2020).
-
6.
Disease prevention
The AI technologies and applications can provide updated and analyzed data to governmental issues to provide more preventive healthcare services.
5.3. How other disruptive technologies can impact COVID-19 research
The vital applications and technologies of industry 4.0 for COVID-19 can provide day-to-day digital results to manage the pandemic of COVID-19 outbreaks (Javaid et al., 2020). Industry 4.0 can offer various innovations to the digital technology of media platforms to achieve unusual information. Industry 4.0 can achieve better risk management for emergent healthcare conditions of COVID-19 outbreaks (Yang et al., 2020). The IoT application and technology provides smart healthcare with important opportunities to manage the crisis of COVID-19 on humanity. The IT sensors can perform automatic processes and communication between patient and healthcare systems (Swayamsiddha and Mohanty, 2020). The IoMT, an extensive for IoT, provides remote medical services for hospitalized or home quarantine patients (Chenghu et al., 2020). The generated data can help build a medical platform to be analyzed further to achieve valuable statistical results. In (R.P.. Singh et al., 2020), big data integrate a heterogeneous form of data to rapidly acquire the data to provide to governmental aspects to limit the widespread pandemic of COVID-19 outbreaks.
Mashamba and Crayton (2020) provide digital solutions to limit the pandemic of COVID-19. The tracking of high-risk COVID-19 patients with digital DH1S2 based solutions defined as a standalone package for disease surveillance systems, international and national dashboards, and drones for surveillance. In addition to telemedicine applications to categorize patients of COVID-19 as follows: virtual chatbots and web bots to take follow up with virtual visits, telemedical robot cards, electronic intensive care units, and virtual visits to patients' rooms. For home quarantine, Mashamba and Crayton (2020) adopt some valuable applications such as the Apple health check app, Siri gives me guidance and Alexa daily check. Bakken et al. (2020) provided a community based on blockchain and AI technologies linked with self-testing and tracking system for urgent infectious diseases. In Chamola et al. (2020), the proposed technology is used in China to improve communication between the healthcare team to improve the track and monitor for patients and viruses.
5.4. How predictive modeling can provide possible solutions and recommendations on the proposed intelligent framework?
Predictive modeling can predict outcomes using data and statistics. The intelligent framework can be extended with predictive data modeling features to estimate the predictions for the spread of COVID-19 to inform the competent authorities to take preventive methods. Koutsellis et al. (2020) used predictive modeling to predict the spread of COVID-19 outbreaks in the United States and European countries. Ghosh (2020) applied analysis and prediction to the spread of COVID-19 and the effect on countries and people. Due to the rising of the death rate of COVID-19 and the unclear risk factors. Ran et al. (2020) applied the regression model of Cox regression models to investigate the risk factors for case fatality and predicted the death probability under specific combinations of key predictors. In addition, Wang et al. (2020b) developed a model to predict the prognosis of COVID-19 to produce a good performance in predicting the outcome of COVID-19. Therefore, predictive modeling can generate possible solutions and recommendations that help countries limit the pandemic for COVID-19 outbreaks.
5.5. How to prove the justification and suitability of the proposed intelligent framework?
Paul et al. (2020) evaluate the justification, suitability, and institutional bottlenecks relative to the framework according to health system building Blocks. The WHO conceptual framework based on six health system building blocks: 1) Health Services, 2) Health workforce, 3) Health information, 4) Medical technologies, 5) health financing and 6) Leadership and governance (WHO, 2020). In order to show the justification and suitability for the proposed intelligent framework, the standard health systems blocks are tested as follows:
-
1.
Health services: The framework can provide medical healthcare services anytime, anywhere, anyplace to the competent authorities with minimum waste of resources.
-
2.
Health workforce: The framework provides complete transparency to the competent authorities and provides the best healthcare services with the available resources and any circumstances.
-
3.
Health Information: The framework supports the competent authorities with on time and well-functioned information to perform analysis to enhance health system performance and status.
-
4.
Medical technologies: The framework can maintain a sustainable health role in developing medical devices and equipment to improve healthcare services.
-
5.
Health Financial: The framework concerned with facilities that can be reflected in healthcare services in the pandemic of COVID-19 to provide incentives for financial funds.
-
6.
Leadership and governance: The framework ensures the strategic policy with effective oversight and attention to system-design and accountability.
6. Discussion
6.1. Managerial insights
The study adopted an intelligent framework that merges smart technological issues to assist governments, especially healthcare disciplines. The intelligent framework takes a considerable burden from the healthcare team to reduce human intervention. The reduction of human intervention should help increase the use of full PPE. The challenges of the COVID-19 pandemic are the rapid spread in 213 counties and most of the manufacturing is a lockdown (Kumar et al., 2020; Mandel et al., 2020), so the production of PPE is limited. The technological capabilities support governments in making home isolation for mild and moderate COVID-19 cases to reduce the massive pressure in hospitals and track recovered patients to treat COVID-19 patients.
The intelligent framework provides patients in-home quarantine with remote connection and telemedicine with robotic and drone technologies to support the physical and physiological healthcare. Some features of the intelligent framework applied in Kuwait include the home quarantine patients who are provided with smartwatch connected with online governmental applications. The aim is to detect the patient location to ensure that the patient would not transfer to another site and spread the COVID-19 and be a cause for more outbreaks. In addition to tracking the emergent case, if patients change location, the system can request a nearby police station to move patients for check-ups. The use of smartwatches provides patients with an excellent physiological condition due to the feel of remote tracking. Besides, in Egypt, Mansoura University is developing a robot model to serve food to patients to reduce the human intervention and give patients feel that systematic procedures are performing to enhance services tracking all patients' vital activities.
By applying the intelligent framework, patients can be monitored with the aid of leading technologies of AI, industry 4.0, IoT, IoMT, big data, VR, Drone technology and Autonomous Robots, 5 G, and blockchain to diagnose the disease, record the health status and receive advice on telemedicine. The system can track the evolution case for patients, served with robots and drones. The combined big data is standardized with blockchain technology to be useful for further analysis purposes applied from the governmental sides. Besides, governments can track the recovered patients to denote with plasma according to certain medical conditions, can be extracted from the medical system, to treat patients of COVID-19. In the cases that patients do not need to denote, the competent authorities, e.g., the ministry of interior affairs, takes appropriate actions.
6.2. Disruptive technologies leading the fight against COVID-19
The disruptive technologies combat against the pandemic of COVID-19. The disruptive technologies can replace the traditional methods in the healthcare system of diagnosis, direct communication between patient and healthcare team, overcrowding in hospitals, shortage of PPE, etc. with intelligent solutions. The use of AI, IoT, and IoMT technologies via 5 G and cloud platforms promote the healthcare system to perform day-to-day routine remotely. The remote services take a large burden from healthcare teams and patients, leading to the limit of the spread of COVID-19. The diagnosis can be remotely detected according to data captured to take the decision to treat patients in-home quarantine, hospitalized, or identify or treat patients with typical cold or flu.
The disruptive technologies fight COVID-19, either for patients treated at home quarantine or hospital using robot or drone technology. The AI, big data, and blockchain models can be used to valuable and predictable analysis results.
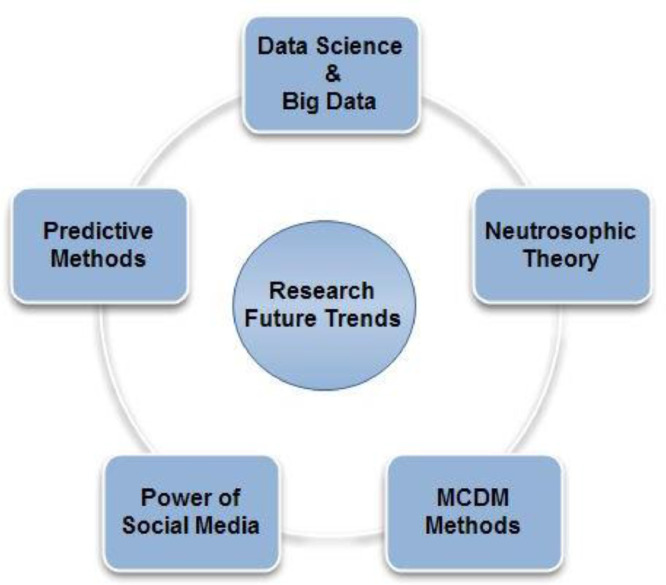
6.3. Future trends and expectations for COVID-19 analysis
The pandemic of COVID-19 provides novel research indications to treat and to limit the negative impact on the economy and humanity. The future research vision is mentioned as follows in the light of the proposed framework technologies, as follows in Fig. 14:
-
1.
Data Science and big data: apply the power of data science to extract knowledge from big data generated from healthcare systems or smart health care (Stuhler et al., 2020).
-
2.
Predictive methodology: the use of predicting methods to forecast the COVID-19 treatment outbreaks and produce statistical reports (Smailhodzic et al., 2016).
-
3.
The power of social media: the data generated from social media can be analyzed to produce consistent results served by the government to try to manage the crisis efficiently (Ma et al., 2013).
-
4.
Multiple-criteria decision-making (MCDM): the researchers can apply the MCDM to support governments with well-formed decisions (Ma et al., 2013). Neutrosophic theory: as the COVID-19 is a problem definition surrounded by vague impression, inconsistency, and uncertainty, and researchers can help decision-makers with consistent and optimized decisions to manage the current pandemic (Abdel-Basset et al., 2019; Nabeeh et al., 2019a, 2019b; Nabeeh, 2020; Nabeeh et al., 2020a, 2020b).
Fig. 14.
The future trends of research in the light of the proposed intelligent framework.
7. Conclusion and future work
The world is fighting severely with COVID-19; researchers from different disciplines can provide governments with appropriate solutions to restrict the COVID-19 outbreak. The study illustrated a review of COVID-19 guidelines as follows: the explanation for the COVID-19, the transmission mechanisms, clinical presentation, laboratory diagnosis, and categories and management. The study proposed an intelligent framework using disruptive technologies to aid government and humanity during the epidemic to reduce COVID-19 outbreaks. The proposed framework demonstrated five main goals: 1) keeping the medical teams safe; 2) maintaining the patients; physical and psychological healthcare conditions; 3) managing a severe shortage of PPE for the medical team; 4) reducing the massive pressure on hospitals, and 5) tracking recovered patients to treat COVID-19 patients. The proposed framework integrated different disruptive technologies of AI, industry 4.0, IoT, IoMT, big data, VR, Drone technology and Autonomous Robots, 5 G, and blockchain to provide governance with an integrated vision to manage the pandemic of COVID-19. The study showed a numerical of COVID-19 patients to present the importance of the proposed intelligence to limit the current outbreaks for COVID-19. The proposed intelligent framework uses the hybrid methodology of neutrosophic theory with TOPSIS results. The results showed an aided list for the healthcare team to treat COVID-19 patients in the hospital, home quarantine, or identifying and treating with typical cold or flu. Our future work will include the use of pioneering AI and Data Science techniques to explore COVID-19 further and publicize our analysis.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Declaration of Competing Interest
The authors declare that there is no conflict of interest in the research
Acknowledgments
Authors would like to thank Dr. Ahmed Kamal Nabeeh (Medical staff in the corona team of Aljaber Alahmad Alsapah Hospital) for his great support in medical aspects of the COVID-19 regarding the symptoms investigation and results of treatment of the disease. This work is partly supported by VC Research (VCR 0000064).
Biographies
Dr. Mohamed Abdel-Basset received his B.Sc. and M.Sc from Faculty of Computers and Informatics, Zagazig University, Egypt. Received his Ph.D from Faculty of Computers and Informatics, Menoufia University, Egypt. Currently, Mohamed is Associate Professor at Faculty of Computers and Informatics, Zagazig University, Egypt. His current research interests are Optimization, Operations Research, Data Mining, Computational Intelligence, Applied Statistics, Decision support systems, Robust Optimization, Engineering Optimization, Multi-objective Optimization, Swarm Intelligence, Evolutionary Algorithms, and Artificial Neural Networks. He is working on the application of multi-objective and robust meta-heuristic optimization techniques. He is also an/a Editor/reviewer in different international journals and conferences. He holds the program chair in many conferences in the fields of decision making analysis, big data, optimization, complexity and internet of things, as well as editorial collaboration in some journals of high impact.
Prof. Victor Chang is currently a Full Professor of Data Science and Information Systems at the School of Computing, Engineering and Digital Technologies, Teesside University, Middlesbrough, UK, since September 2019. He currently leads the Artificial Intelligence and Information Systems Research Group at Teesside University. He was a Senior Associate Professor, Director of Ph.D. (June 2016- May 2018) and Director of MRes (Sep 2017 - Feb 2019) at International Business School Suzhou (IBSS), Xi'an Jiaotong-Liverpool University (XJTLU), Suzhou, China, between June 2016 and August 2019. He was also a very active and contributing key member at Research Institute of Big Data Analytics (RIBDA), XJTLU. He was an Honorary Associate Professor at University of Liverpool. Previously he was a Senior Lecturer at Leeds Beckett University, UK, between Sep 2012 and May 2016. Within 4 years, he completed Ph.D. (CS, Southampton) and PGCert (Higher Education, Fellow, Greenwich) while working for several projects at the same time. Before becoming an academic, he has achieved 97% on average in 27 IT certifications. He won a European Award on Cloud Migration in 2011, IEEE Outstanding Service Award in 2015, best papers in 2012, 2015 and 2018, the 2016 European special award, Outstanding Young Scientist 2017 and INSTICC Service Award 2017–2020. He is a visiting scholar/Ph.D. examiner at several universities, an Editor-in-Chief of IJOCI & OJBD journals, former Editor of FGCS, Associate Editor of TII, Information Fusion and Information Discovery and Delivery (IDD), founding chair of two international workshops and founding Conference Chair of IoTBDS and COMPLEXIS since Year 2016. He is the founding Conference Chair for FEMIB since Year 2019 and IIoTBDSC since Year 2020. He published 3 books as sole authors and the editor of 2 books on Cloud Computing and related technologies. He gave and was invited to give 22 keynotes at international conferences. He is widely regarded as one of the most active and influential young scientist and expert in IoT/Data Science/Cloud/security/AI/IS, as he has experience to develop 10 different services for multiple disciplines.
Miss Nada A. Nabeh received B.S and M.S in Information Systems from the Faculty of Computers and Information Sciences, Mansoura University, Egypt. Her research interests include cloud computing, big data, smart cities, the Internet of Things, neural networks, artificial intelligence, web service composition and evolutionary algorithms.
Appendix A
This section contains additional literature and analysis related to this research.
In Abdel-Basset et al., (2019); Nabeeh et al., (2019a); (Nabeeh et al., 2019b), a neutrosophic theory is applied to handle the uncertainty conditions to achieve a consistent decision. The decision judgments of the healthcare system, team, and givers are modeled in neutrosophic scale format and integrated. The AHP is used to prioritize weights for criteria as the following consequences: C2→C1→C3→C5→C4→C6→C8→C7→C9→C10→C11→C13→C12→C14→C13→C15→ C16.
The 20 patients, as problem alternatives, are ranked according to the hybrid methodology of neutrosophic and TOPSIS (Nabeeh et al., 2019b). The healthcare system, team, and care giver's perspectives are collected and integrated into the neutrosophic scale. The TOPSIS compares alternatives according to relative closeness concerning the weights for criteria symptoms produced from applying the AHP method. The neutrosophic theory is used to handle uncertainty conditions. The patients are prioritized according to the relative closeness of TOPSIS as follows: A17→A1→A18→A5→A4→A6→A8→A7→A19→A10→A11→A13→A12→A20→A15→A16→A2→A3→A9→A14
In Kapoor et al., (2020), the virtual reality in healthcare for COVID-19 outbreaks adopt eight effective applications which are VR for
Physical therapy,
Management of pain,
Mobile application,
Hospitalized patient,
Physical rehabilitation,
Cognitive rehabilitation,
Distracting patients and
Psychological treatment.
References
- Abdel-Basset M., Mohamed R. A novel plithogenic TOPSIS- CRITIC model for sustainable supply chain risk management. J. Clean. Prod. 2020;247:0959–6526. 119586. [Google Scholar]
- Abdel-Basset M., Nabeeh N.A., El-Ghareeb H.A., Aboelfetouh A. Utilizing neutrosophic theory to solve transition difficulties of iot-based enterprises. Enterprise Information Systems. 2019 [Google Scholar]
- Ammenwerth E., Ehlers F., Hirsch B., Gratl Gordon. HIS-Monitor: an approach to assess the quality of information processing in hospitals. Int J Med Inform. 2007;76:216–225. doi: 10.1016/j.ijmedinf.2006.05.004. Issues 2–3. [DOI] [PubMed] [Google Scholar]
- Bai L.and . Chinese experts’ consensus on the Internet of Things-aided diagnosis and treatment of coronavirus disease 2019. Clinical eHealth. 2020;3:7–15. [Google Scholar]
- Barbisch D., Koenig K.L., Shih F.Y. Is there a case for quarantine? Perspectives from SARS to Ebola. Disas. Med. Publ. Health Prep. 2015;9(5):547–553. doi: 10.1017/dmp.2015.38. [DOI] [PubMed] [Google Scholar]
- Bakken S., Koleck T.A., Dreisbach C., Hickey K.T. Enabling Precision Health Approaches for Symptom Science Through Big Data and Data Science. In: Dorsey S., Starkweather A., editors. Genomics of Pain and Co-Morbid Symptoms. Springer; Cham: 2020. [Google Scholar]
- Biswas K, Sen P. 2020. Space-time dependence of coronavirus (COVID-19) outbreak. arXiv preprint arXiv:2003.03149.
- Chamola V., Hassija V.., Gupta V., Guizani M. A Comprehensive Review of the COVID-19 Pandemic and the Role of IoT, Drones, AI, Blockchain, and 5G in Managing its Impact. IEEE Access. 2020;8:90225–90265. doi: 10.1109/ACCESS.2020.2992341. 2020, doi. [DOI] [Google Scholar]
- Chang V. An overview, examples, and impacts offered by emerging services and analytics in cloud computing virtual reality. Neural Comput & Applic. 2018;29:1243–1256. doi: 10.1007/s00521-017-3000-1. [DOI] [Google Scholar]
- Chenghu, Z., Fenzhen, S., Pei, T.and et al. 2020. COVID-19: challenges to GIS with Big Data, Geography and Sustainability, 1(1).
- Chen S, Yang J, Yang W, Wang C, B€arnighausen T. COVID-19 control in China during mass population movements at New Year. Lancet. 2020 doi: 10.1016/S0140-6736(20)30421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clinical Management of Covid-19, interim management 27may 2020, Who organization.
- Cyient. 2020. Cyient provides drone-based surveillance technology to support telangana state police in implementing COVID-19 Lockdown. [Online]. Available: https://www.cyient.com/prlisting/corporate/cyient-provides-drone-based-%surveillance-technology-tosupport-telangana-state-police-in-implementing-covi%d-19-lockdown.
- Gharehgozli O.and . Impact of COVID-19 on the economic output of the US Outbreak's Epicenter. Economics of Disasters and Climate Change. 2020:1–13. doi: 10.1007/s41885-020-00069-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan WJ., Ni Z., Hu Y. .Clinical characteristics of coronavirus disease 2019 in China. The New England J medicine. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuseppe L., Plebani M. Clinical laboratory and SARS-CoV-2 infection: where do we stand? Clinical Chemistry and Laboratory Medicine. 2020 doi: 10.1515/cclm-2020-0372. [DOI] [PubMed] [Google Scholar]
- Goyal K., Chauhan P., Chhikara K., Gupta P., Singh M.P. Fear of COVID 2019: first suicidal case in India! Asian J. Psychiatr. 2020;49 doi: 10.1016/j.ajp.2020.101989. 10.1016/ j.ajp.2020.101989. [Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haleem A, Vaishya R, Javaid M, Khan IH. Artificial Intelligence (AI) applications in orthopaedics: an innovative technology to embrace. J Clin Orthop Trauma. 2019 doi: 10.1016/j.jcot.2019.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X. . Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katafuchi Y., ad Kurita K., Managi S. COVID-19 with stigma: theory and evidence from mobility data. Economics of Disasters and Climate Change (Forthcoming) 2020 doi: 10.1007/s41885-020-00077-w. https://mpra.ub.uni-muenchen.de/102766/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee EYP, Ng M-Y, Khong P-L. 2020 COVID-19 pneumonia: what has CT taught us? Online.thelancet.com. Published: 24 February 2020.
- Lasi, H., H.G. Kemper, P. Fettke, T. Feld, and M. Hoffmann. 2014. “ndustry 4.0.Business Information Systems Engineering 6 (4): 239–242. doi:10.1007/s12599-014-0334-4.
- Lima C.K.T., Carvalho P.M.M., Lima I.A.A.S., Nunes J.V.A.O., Saraiva J.S., de Souza R.I., da Silva C.G.L., Neto M.L.R. The emotional impact of Coronavirus 2019- nCoV (new Coronavirus disease) Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112915. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Ge J., Yang M., Feng J., Qiao M., Jiang R., Bi J., Zhan G., Xu X., Wang L., Zhou Q., Zhou C., Pan Y., Liu S., Zhang H., Yang J., Zhu B., Hu Y., Hashimoto K., Jia Y., Wang H., Wang R., Liu C., Yang C. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.007. piiS0889-1591(20)30309-3. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauer SA., Grantz KH., Bi Q. The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: estimation and Application. Annals of internal medicine. 2020 doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallapaty S. 2020. What the cruise-ship outbreaks reveal about COVID-19. Nature. 2020;580(7801):18. doi: 10.1038/d41586-020-00885-w. [DOI] [PubMed] [Google Scholar]
- Ma B., Tan C., Jiang Z., Deng H. Intuitionistic fuzzy multicriteria group decision for evaluating and selecting information systems projects. Inf. Technol. J. 2013;12(13):2505–2511. 2013. [Google Scholar]
- Manto, M., Dupre, N., Hadjivassiliou, M., Louis, E.D., Mitoma, H., Molinari, M., ... & Schmahmann, J.D. (2020). Management of Patients with Cerebellar Ataxia During the COVID-19 Pandemic: current Concerns and Future Implications. Cerebellum (London, England), 1. [DOI] [PMC free article] [PubMed]
- Martin A. . Socio-Economic Impacts of COVID-19 on Household Consumption and Poverty. Economics of Disasters and Climate Change. 2020:1–27. doi: 10.1007/s41885-020-00070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcneil, D.G.Jr. 2020. Can smart thermometers track the spread of the coronavirus?'' The New York Times. [Online]. Available: https://www.nytimes.com/2020/03/18/health/coronavirusfever-thermometer%s.html\.
- Melnyk B.M., Fineout-Overholt E., editors. Evidence-based Practice in Nursing & healthcare: A guide to Best Practice. Lippincott Williams & Wilkins; 2011. [Google Scholar]
- Montemurro N. The emotional impact of COVID-19: from medical staff to common people, Brain, Behavior, and Immunity. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabeeh N.A. An integrated neutrosophic-TOPSIS approach and its application to personnel selection: a new trend in brain processing and analysis. IEEE Access. 2019;7:29734–29744. 2019. [Google Scholar]
- Nabeeh N.A. A Hybrid Neutrosophic Approach of DEMATEL with AR-DEA in Technology Selection, NSS. 2020;3 https://digitalrepository.unm.edu/nss_journal/vol31/iss1/2 2020. [Google Scholar]
- Nabeeh N.A., Abdel-Monem A., Abdelmouty A. A hybrid approach of neutrosophic with multimoora in application of personnel selection. Neutrosophic Sets and Systems. 2020:1. 2019. [Google Scholar]
- Nabeeh N.A., Abdel-Monem A., Abdelmouty A. A novel methodology for assessment of hospital service according to BWM, MABAC, PROMETHEE II. Neutrosophic Sets and Systems. 2020;31(1):5. 2020. [Google Scholar]
- Nabeeh N.A., Abdel-Basset M., El-Ghareeb H.A., Aboelfetouh A. Neutrosophic multi-criteria decision making approach for IoT-Based Enterprises. IEEE Access. 2019 [Google Scholar]
- Pan L., Mu M., Ren HG. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020 doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan American Health Organization (PAHO), link:https://www.paho.org/en, [online accessed 08/06/2020].
- Paul E., Ndiaye Y., Sall F., L, Fecher F, Porignon D. An assessment of the core capacities of the Senegalese health system to deliver Universal Health Coverage. Health Policy OPEN. 2020;1 doi: 10.1016/j.hpopen.2020.100012. 1000122590-2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh R.P.., Javaid M., . Raju V., Haleem. Abid, Ali S. Internet of Medical Things (IoMT) for orthopaedic in COVID-19 pandemic: roles, challenges, and applications. J Clin Orthop Trauma. 2020 doi: 10.1016/j.jcot.2020.05.011. Elsevier public health emergency collection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ran Wu. . Predictive model and risk factors for case fatality of COVID-19: a Cohort of 21,392 Cases in Hubei, China. The Innovation. 2020;1(2):2666–6758. doi: 10.1016/j.xinn.2020.100022. 100022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read R. A choir decided to go ahead wth rehearsal. Now dozens of mebers have COVID-19 and two are dead. 2020 Seattle burfeau. Los Angeles time. [Google Scholar]
- Ren J., Zhang A., Wang X. Traditional Chinese medicine for COVID-19 treatment. Pharmacol Res. 2020;4 doi: 10.1016/j.phrs.2020.104743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi H, Han X, Jiang N, Cao Y, Osamah A, Gu J, Fan Y, Zheng C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan. China: a descriptive study. 2020 doi: 10.1016/S1473-3099(20)30086-4. [online] thelancet.com 24 February 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smailhodzic, E., Hooijsma, W., Boonstra, A., and et al. 2016. Social media use in healthcare: a systematic review of effects on patients and on their relationship with healthcare. [DOI] [PMC free article] [PubMed]
- Swayamsiddha S., Mohanty C. Application of cognitive Internet of Medical Things for COVID-19 pandemic. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2020;14(5):911–915. doi: 10.1016/j.dsx.2020.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ting D.S.W., Carin L., Dzau V., Wong T.Y. Digital technology and COVID-19. Nat. Med. 2020;26(4):459–461. doi: 10.1038/s41591-020-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuli S., Tuli S., Rakesh Tuli, G. SukhpalSingh. Elsevier, Internet of Things; 2020. Predicting the Growth and Trend of COVID-19 Pandemic Using Machine Learning and Cloud Computing. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaishya R., Javaid M., Haleem-Khan I., Abid-Haleem Artificial Intelligence (AI) applications for COVID-19 pandemic. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2020;14:337e339. doi: 10.1016/j.dsx.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D. . Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, F., and et al. 2020b . Establishing a model for predicting the outcome of COVID-19 based on combination of laboratory tests, Travel Medicine and Infectious Disease, 36, 101782, 1477–8939. [DOI] [PMC free article] [PubMed]
- Wu C., Chen X., Cai Y. . Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson J., Builta J. IoT Set to Play a Growing Role in the COVID-19 Response_Omdia. OMDIA. 2020 Apr. 2020. [Online]. Available: https://technology.informa.com/622426/iot-set-to play-a-growingrole-in%-the-covid-19-response. [Google Scholar]
- Xu XW., Wu XX., Jiang XG. . Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ (Clinical research ed) 2020;368:m606. doi: 10.1136/bmj.m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang T, Gentile M, Shen CF, Cheng CM. Combining point-of-care diagnostics and internet of medical things (IoMT) to combat the COVID-19 pandemic. Diagnostics (Basel) 2020;10(4) doi: 10.3390/diagnostics10040224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo S., Managi S. Global Mortality Benefits of COVID-19 Action. Technological Forecasting & Social Change (forthcoming) 2020 doi: 10.1016/j.techfore.2020.120231. https://www.sciencedirect.com/science/article/pii/S004016252031057X [DOI] [PMC free article] [PubMed] [Google Scholar]