Abstract
Purposes
Evidence suggests evening-type individuals have a higher risk of reporting psychological distress than morning-type individuals. However, less is known regarding the underlying processes that might mediate or moderate this association among Chinese rural population. This study aimed to evaluate the prevalence of psychological distress, investigate whether sleep quality would mediate the association between chronotype and psychological distress and explore whether age would moderate the direct or indirect effect of the mediation model.
Methods
The cross-sectional study utilized a sample of 884 rural residents from rural regions in Anqing City, Anhui Province, China. Morningness-Eveningness Questionnaire (MEQ), Pittsburgh Sleep Quality Index (PSQI) and 21-item Depression Anxiety Stress Scale (DASS-21) were used to measure chronotype, sleep quality and psychological distress, respectively. MacKinnon’s four-step procedure was employed to examine the mediation effect, while Hayes PROCESS macro (model 59) was used to perform the moderated mediation analysis.
Results
The prevalence of psychological distress among Chinese rural population was 33.4%. The association between chronotype and psychological distress was partially mediated by sleep quality (indirect effect = - 0.05, 95% CI = [-0.08, -0.03]). In addition, age moderated the first stage (sleep quality–psychological distress) of the indirect effect, with the indirect effect being attenuated for older rural residents. As suggested by Johnson-Neyman technique, the association between sleep quality and psychological distress was only significant when the age of the participant was lower than 48.59.
Conclusions
The incidence of psychological distress among Chinese rural residents cannot be neglected. Interventions for the enhancement of sleep quality to prevent and reduce psychological distress should be prioritized to rural residents who are prone to eveningness, especially those who are younger.
Introduction
With the sustained rapid social and economic development, there has been an increasing focus on psychological distress [1]. Psychological distress is a broad term that refers to a non-specific syndrome with anxiety and depression posited as the core symptoms [2, 3], and as the level of psychological distress enhances, the likelihood of the person with symptoms capable of meeting the diagnostic criteria of mental disorders increases [4]. The comorbid association between psychological distress and physical conditions could lead to poorer quality of life, reduced workplace productivity, increased utilization of healthcare resources, higher healthcare costs, and prolonged disability [4–7]. The prevention of psychological distress beforehand is a priority agenda for health.
The disruption of circadian rhythms is regarded as a risk factor in various mood-related problems encompassing depression and anxiety [8]. Previous literature suggested circadian clock-related genes might predispose individuals to anxiety disorders [9]. Likewise, the changes in the secretion of diurnal cortisol have been presented to be implicated in anxiety [10, 11] and the decrease in melatonin has been linked to affective disorders [12]. In addition, participants from anxiety and depression groups were more likely to report delayed sleep onset and offset time than those from the control group [13]. Chronotype as an indicator of circadian rhythms represents a continuous spectrum ranging from eveningness to morningness [14, 15]. Evening-type individuals are more active and perform better in the evening than in the morning and circadian processes (such as cortisol and body temperature) peaks in the evening, while it is vice versa for morning-type individuals [16]. More importantly, evening-type individuals are more likely to suffer from the desynchrony between circadian rhythms and environmental demands [14]. Considerable studies supported the evidence for the relation between eveningness and mood fluctuation based on healthy population [17, 18]. Thus, it is highly possible chronotype is linked to psychological distress in non-clinical samples.
Compared with urban residents, rural dwellers are more likely to be socio-economically disadvantaged and less educated, live in poorer social and physical environment, and have less access to health care services [19–21], which makes them more vulnerable to psychological distress. In China, the prevalence of depression in rural areas was 1.5 times higher than that in urban areas [22]. Additionally, there was a big difference in the occupational routines of the rural and urban populations [23]. For rural residents, there was no great disparity in the starting and finishing time of work. Furthermore, rural residents reported less recreational and communicative leisure activities than their urban counterparts [24]. Thus, the work obligations and the participation in leisure activities might also exert a regulatory effect on circadian rhythm among rural residents [25]. Although there are great discrepancies in lifestyles between urban and rural residents, the majority of previous literature on the associations between chronotype and psychological distress was only based on urban areas. To date, no study has explored the effect of chronotype on psychological distress in rural China. Given that rural residents accounted for approximately 43% of the total population in China [26], ongoing efforts are in need to further explore the association between chronotype and psychological distress among rural dwellers in China. In addition, there is an enormous explanatory gap in potential mechanisms underlying the association, which is vital to advance our understanding of psychological distress among Chinese rural dwellers.
The mediating role of sleep quality
Accumulating evidence is emerging regarding the relation between chronotype and quality of sleep [27, 28] due to social jetlag which is defined as the misalignment of social time and chronotype [29]. Social jetlag presents to be higher in evening-type individuals. Previous study claimed evening chronotype was the most influential risk factor for poor quality of sleep [30]. Additionally, sleep quality is essential for optimal physical and psychological health [31]. Prior research showed the negative association between sleep quality and psychological distress [32]. According to the literature review, sleep quality might mediate the association between chronotype and psychological distress among Chinese rural dwellers.
The moderating role of age
Existing literature has indicated the age differences in the association between chronotype and depressive symptoms among a rural population, suggesting a more prominent relation in participants aged 31–40 years [33]. Nevertheless, a more previous study reported the totally different findings that the association between chronotype and depressive symptoms was stronger in younger (aged≤ 20 years) or older (aged ≥50 years) participants [34]. Despite the inconsistent findings from literature review, they reached the consensus on the moderating role of age in the mechanisms through which chronotype influences psychological distress. A meta-analysis conducted by Au and Reece [35] summarized 36 studies and revealed the research concerning the moderating role of age in the relation between chronotype and mood symptoms was too few to ascertain the relationship.
The present study
The primary objective of the present study was to estimate the prevalence of psychological distress among rural dwellers in rural China, while the second objective was to shed light on “how” and “for whom” chronotype would be associated with psychological distress through a moderated mediation model (see Fig 1). We hypothesized that sleep quality might serve as a mediator to bridge the link between chronotype and psychological distress. In addition, age would moderate the direct and/or indirect effect (including chronotype—sleep quality path and sleep quality–psychological distress path) of chronotype on psychological distress.
Fig 1. Conceptual model.
Methods
Participants and procedures
The cross-sectional study was conducted in the rural regions of Anqing City, Anhui Province, China, from December, 2019 to January, 2020. Participants were recruited through cluster sampling procedures. The inclusion criteria were a) aged between 18 and 54, and b) having a rural Hukou. The exclusion criteria were: a) participants with missing values on any of the dependent, independent and control variables, b) those whose answer time was less than 8 minutes and c) those who reported longer sleep duration than time in bed, which caused the sleep efficiency (sleep duration/time in bed) was more than 1. Finally, 884 participants were included in the analysis.
Before completing the survey, all participants were given informed written consent, which claimed the participation was voluntary and anonymous and could be withdrawn at any time. The research ethics committee of Naval Medical University approved the study.
Measures
Sociodemographic characteristics
Self-reported age, gender, marital status, educational level, the status of having siblings and family structure were collected. Marital status was grouped into unmarried (single, divorced and widowed) and married. Educational level was categorized as primary school or below, junior high school, and senior high school or above. Family structure was classified into two groups: intact and non-intact.
Chronotype
Chronotype was assessed by Morningness-Eveningness Questionnaire (MEQ) developed by Horne and Ostberg [36], which is the most widely used instrument for the identification of circadian preference [37]. The total score of 19-item scale ranges from 16 to 86 points, with a higher score denoting the tendency to morning activities. The Chinese version scale has been consolidated as a reliable and valid instrument [38, 39].
Sleep quality
The Chinese version of Pittsburgh Sleep Quality Index (PSQI) was used to measure sleep quality [40]. Although the scale contains 24 items, only 19 items are used to calculate sleep quality. The 19 questions scored on a 3-point Likert scale in the reference period of “past 1 month” were grouped into 7 dimensions: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleep medications and daytime dysfunction. The total score is generated by the sum of the scores of the 7 components ranging from 0 to 21 with a lower score indicating higher sleep quality. The Chinese version of PSQI has shown impressive reliability and sufficient validity [41].
Psychological distress
Psychological distress was measured by 21-item Depression Anxiety Stress Scale (DASS-21) developed by Lovibond and Lovibond [42] in its Chinese version, which is a common instrument for screening emotional distress symptoms during the past week [43]. The scale contains three subscales: Depression, anxiety and stress. Each subscale consists of 7 items and participants rated each item on a 4-point Likert scale from 0 (“did not apply to me at all”) to 4 (“apply to me very much”). The range of the total scores for each subscale is 0–42. Zanon and colleagues [44] based on eight countries including China examined the dimensionality of DASS-21 and suggested that DASS-21 would be best utilized as a unidimensional distress scale rather than three separate components of depression, anxiety and stress. In addition, the combination of 21 items presented the optimal sensitivity (79.1%) and specificity (77.0%) at the cut-off point of ≥34 of the total scale to screen psychological distress compared with any of the subscales or the combination of any two subscales [45]. The Chinese version scale has presented excellent reliability and good validity [46].
Statistical analysis
Descriptive statistics, independent t-test and one-way analysis of variance (ANOVA) were performed for the description of demographic characteristics and group comparisons of MEQ, PSQI and DASS-21 scores. Pearson correlation analyses were conducted to calculate the bivariate correlations between the variables of interest. Then, the current study examined the mediation effect through MacKinnon’s four-step procedure [47]. Four criteria need to be satisfied to verify the mediation effect. Firstly, the association between chronotype and psychological distress would be significant. Secondly, the relation between chronotype and sleep quality would be significant. Thirdly, the relationship between sleep quality and psychological distress would still be significant when controlling for chronotype. Lastly, the coefficient for the indirect pathway between chronotype and psychological distress via sleep quality would be significant, which would be tested by the bias-corrected percentile bootstrap method using Hayes’s [48] PROCESS macro (Model 4). The last condition would be met if the 95% bias-corrected confidence interval (CI) calculated with 5000 resamples excluded zero. Finally, Model 59 would be performed to test the moderated mediation model, that was, whether age would moderate the direct and the indirect effects of chronotype on psychological distress. Likewise, if the 95% bias-corrected CI of the interaction did not include zero, the moderating effect of age would be established. Bootstrap method would be conducted to reveal the conditional effect at different values of age (1 SD below the mean, at the mean, and 1SD above the mean). Furthermore, we plotted the conditional effects and confidence bonds according to Johnson-Neyman technique [49]. All statistical analyses were performed by SPSS 25.0 and a two-tailed P-value less than 0.05 indicated statistical significance. All the study variables were standardized and all models were controlled for gender, marital status, the status of having siblings, educational level and family structure.
Results
Demographic characteristics and psychological distress
In the present study, 884 participants from rural areas had a mean age of 36.7 (SD = 7.1), ranging from 18 to 54. Table 1 shows the detailed information. Most participants were females (63.0%), married (92.9%), having siblings (95.7%), reported junior high school education (57.8%) and intact family structure (87.0%). The prevalence of psychological distress among rural dwellers was 33.4%. According to the comparison of the means, males presented higher DASS-21 scores than females (t = 17.02, P < 0.001). Significant differences in MEQ and DASS-21 scores were found across marital status (t = 6.18, P = 0.013 and t = 6.98, P = 0.008). Educational level has a significant effect on MEQ scores (t = 8.39, P < 0.001). LSD post hoc test presented that participants with an educational level of primary school or below had higher MEQ scores than the other two groups (junior high school: mean difference = 1.43, P = 0.011; senior high school or above: mean difference = 2.61, P < 0.001). Those who had an educational level of junior high school presented higher scores of MEQ than the senior high school or above group (mean difference = 1.19, P = 0.016).
Table 1. Demographic characteristics and group comparisons of MEQ, PSQI and DASS-21 scores (n = 884).
| No. (%) | MEQ Scores | PSQI Scores | DASS-21 Scores | ||||
|---|---|---|---|---|---|---|---|
| M ± SD | P | M ± SD | P | M ± SD | P | ||
| Gender | 0.156 | 0.771 | <0.001 | ||||
| Male | 327 (37.0) | 62.1 ± 5.8 | 4.9 ± 3.0 | 32.9 ± 29.7 | |||
| Female | 557 (63.0) | 61.5 ± 6.3 | 4.8 ± 3.1 | 25.4 ± 23.5 | |||
| Marital status | 0.013 | 0.237 | 0.008 | ||||
| Unmarried | 63 (7.1) | 59.9 ± 7.4 | 5.3 ± 3,2 | 36.5 ± 28.7 | |||
| Married | 821 (92.9) | 61.8 ±6.0 | 4.8 ± 3.1 | 27.5 ± 25.9 | |||
| The status of having siblings | 0.651 | 0.679 | 0.376 | ||||
| No | 38 (4.3) | 61.3 ± 5.1 | 4.7 ± 3.3 | 31.8 ± 26.0 | |||
| Yes | 846 (95.7) | 61.7 ± 6.2 | 4.9 ± 3.1 | 28.0 ± 26.2 | |||
| Educational level | <0.001 | 0.316 | 0.700 | ||||
| Primary school or below | 155 (17.5) | 63.2 ± 5.5 | 5.2 ± 3.0 | 27.7 ± 23.3 | |||
| Junior high school | 511 (57.8) | 61.7 ± 6.1 | 4.8 ± 3.0 | 27.7 ± 25.7 | |||
| Senior high school or above | 218 (24.7) | 60.6 ± 6.3 | 4.8 ± 3.3 | 29.5 ± 29.2 | |||
| Family structure | 0.999 | 0.717 | 0.259 | ||||
| Intact | 769 (87.0) | 61.7 ± 6.2 | 4.8 ± 3.1 | 28.5 ± 26.8 | |||
| Non-intact | 115 (13.0) | 61.7 ± 5.9 | 5.0 ± 3.1 | 25.6 ± 21.7 | |||
Bivariate analyses
Table 2 presents the means, SD and correlations between the study variables. The results showed that chronotype was negatively correlated with PSQI scores, DASS-21 and its three subscales (all P < 0.05), and positively associated with age (P < 0.001). PSQI scores were positively related to DASS-21 and its three subscales (all P < 0.001).
Table 2. Bivariate correlations among chronotype, PSQI scores, age, psychological distress and its subscales (n = 884).
| Mean | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|
| 1. Chronotype | 61.7 ± 6.1 | ||||||
| 2. PSQI scores | 4.9 ± 3.1 | -0.239*** | |||||
| 3. Age | 36.7 ± 7.1 | 0.219*** | 0.004 | ||||
| 4. Depression subscale of DASS-21 | 7.7 ± 9.4 | -0.124*** | 0.173*** | -0.023 | |||
| 5. Anxiety subscale of DASS-21 | 9.3 ± 9.0 | -0.080* | 0.189*** | -0.014 | 0.879*** | ||
| 6. Stress subscale of DASS-21 | 11.2 ± 9.0 | -0.137*** | 0.268*** | -0.023 | 0.857*** | 0.879*** | |
| 7. DASS-21 | 28.2 ± 26.2 | -0.119*** | 0.219*** | -0.021 | 0.955*** | 0.961*** | 0.953*** |
*P<0.05.
**P<0.01.
***P<0.001.
Testing for mediation effect
As multiple regression analysis showed, chronotype was negatively associated with psychological distress (β = -0.13, P<0.001) (see Model 1 in Table 3). Chronotype was also negatively correlated with PSQI scores (β = -0.27, P<0.001) (see Model 2 in Table 3), which indicated chronotype positively predicted sleep quality. In addition, PSQI score was positively associated with psychological distress while controlling for chronotype (β = 0.20, P<0.001) (see Model 3 in Table 3), which showed the negative association between sleep quality and psychological distress was significant when controlling for chronotype. Finally, the results of bias-corrected percentile bootstrap method presented that the indirect path between chronotype and psychological distress via PSQI scores (sleep quality) was significant (ab = -0.05, SE = 0.01, 95% CI = [-0.08, -0.03]). The mediation effect explained 39.9% of the total effect. Taken together, all four conditions of MacKinnon’s four-step procedure (2008) were satisfied, which supported the mediation effect.
Table 3. Mediation analysis (n = 884).
| Variables | Model 1(Psychological distress) | Model 2 (PSQI Scores) | Model 3(Psychological distress) | |||
|---|---|---|---|---|---|---|
| β | t | β | t | β | t | |
| Chronotype | -0.13*** | -3.70 | -0.27*** | -7.57 | -0.08* | -2.20 |
| PSQI Scores | 0.20*** | 5.88 | ||||
| R2 | 0.04*** | 0.07*** | 0.08*** | |||
| F | 5.42 | 8.82 | 9.25 | |||
Note: controlling for gender, marital status, the status of having siblings, educational level and family structure.
**P<0.01.
***P<0.001.
Testing for moderated mediation effect
The results of the moderated mediation model are presented in Table 4. We expected that age would moderate the association between chronotype and psychological distress either both or separately in the direct effect (chronotype–psychological distress) and indirect effect (path a: chronotype–sleep quality and path b: sleep quality and psychological distress). Nonetheless, age did not moderate the direct effect of chronotype on psychological distress (chronotype * age: β = 0.040, 95% CI = [-0.169, 0.090]). The results revealed that only the first stage of the indirect effect of chronotype on psychological distress through sleep quality (PSQI scores) was moderated by age (chronotype–PSQI scores: β = 0.066, 95% CI = [0.006, 0.260]; PSQI scores–psychological distress: β = -0.008, 95% CI = [-0.121, 0.106]), indicating that the mediation effect of sleep quality on the relation between chronotype and psychological distress was moderated by age among the Chinese rural dwellers.
Table 4. Conditional process analysis (n = 884).
| β | SE | LLCI | ULCI | |
|---|---|---|---|---|
| Mediator variable model (Outcome: PSQI scores) | ||||
| Chronotype | -0.264*** | 0.036 | -0.334 | -0.194 |
| Age | 0.066 | 0.068 | -0.067 | 0.199 |
| Chronotype * Age | 0.066* | 0.065 | 0.006 | 0.260 |
| Dependent variable model (Outcome: Psychological distress) | ||||
| Chronotype | -0.075* | 0.036 | -0.146 | -0.003 |
| PSQI score | 0.198*** | 0.034 | 0.132 | 0.264 |
| Age | -0.053 | 0.067 | -0.185 | 0.079 |
| Chronotype * Age | -0.040 | 0.066 | -0.169 | 0.090 |
| PSQI scores * Age | -0.008 | 0.058 | -0.121 | 0.106 |
| β | Boot SE | BootLLCI | BootULCI | |
| Conditional indirect effect analysis | ||||
| 1 SD below the mean | -0.068 | 0.019 | -0.108 | -0.034 |
| Mean | -0.052 | 0.011 | -0.076 | -0.032 |
| 1 SD above the mean | -0.037 | 0.013 | -0.065 | -0.014 |
Outcome variable: Psychological distress
Note: controlling for gender, marital status, the status of having siblings, educational level and family structure.
* p<0.05
** p<0.01
*** p<0.001
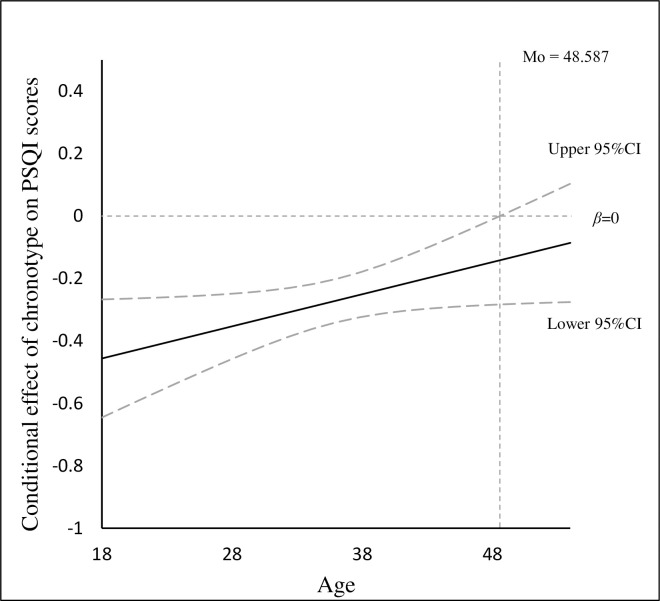
The conditional indirect effect of chronotype on psychological distress via sleep quality (PSQI scores) at different levels of age was performed by bootstrap method. The indirect effect was evaluated at 1 SD below the mean, the mean, and 1SD above the mean (see Table 4). The mediation effect of sleep quality on the association between chronotype and psychological distress became attenuated at 1SD above the mean of age (β = -0.037, 95% CI = [-0.065, -0.014]) than 1SD below the mean of age (β = -0.068, 95% CI = [-0.108, -0.034]). Moreover, the Johnson-Neyman technique (see Fig 2) showed that age could moderate the association between chronotype and sleep quality (PSQI scores) when the age of the participant was lower than 48.59 since the 95% confidence interval did not contain zero.
Fig 2. The conditional effect of chronotype on PSQI scores.
Discussion
In the present research, the prevalence of psychological distress among rural residents from Anhui Province was 33.4%, which is slightly higher than that (33%) of the rural residents in Shangdong Province, China and that (31%) in rural communities in Australia [50, 51]. Earlier literature showed that the rates of psychological distress for famers and non-farmers in rural China were 31.13% and 30.01%, respectively [52]. The discrepancy might be attributed to different measurements and regional differences. In addition, the literature regarding the prevalence of psychological distress among urban population was 15.8–27.8% [53–55]. This is consistent with the previous study regarding the difference in psychological distress between urban and rural regions based on 9 countries, which suggested participants living in village presented higher odds of suffering from psychological distress than those in the cities [56]. Moreover, prior study reported the population-level prevalence of psychological distress in Australia and Canada were 11.1% and 12.0%, suggesting lower rates than our result. This indicated that compared with developed countries, Chinese rural population might be more likely to suffer from psychological distress on account of low income, educational level and poor mental health services [52]. In sum, the prevalence of psychological distress among rural Chinese residents could not be neglected and more attention should be paid to address this issue.
The current study showed males had significant higher scores of psychological distress than females, which contradicted with existing findings [57–60]. The participants in the current analysis were those with rural Hukou from Anhui Province where considerable rural residents migrated to seek work [61]. According to National Bureau of Statistics of China [62], the majority of rural migrant workers were males, accounting for 65.2% of the total migrant workers. Thus, males had a higher tendency to suffer from prolonged working hours, poor living circumstance, experiences of stigma and social inequity [63, 64], which indicated they were more likely to experience distress. Furthermore, this might also be attributed to the cultural value of work. In traditional Chinese society, males were anticipated to play the role of financial supporters of the whole family, and male migrant workers were more likely to expect or be expected to send money back home [61]. All these might explain why males presented higher levels of psychological distress than females in rural China. The present study also showed that unmarried rural residents presented higher levels of psychological distress compared to married residents. This is consistent with the previous findings [65]. Married people have more social support, which plays a critical role in the mitigation of negative emotions. Our results also suggested married rural dwellers and those with lower levels of education presented to be prone to morningness.
Consistent with previous studies [8, 66], the results found the significant association between chronotype and psychological distress among rural residents. This could be explained by Social Zeitgeber Theory [67]. Stressful life events would result in the alterations in the social zeitgebers including sleep-wake schedules. This would contribute to the change of molecular and cellular rhythms, which might further trigger the onset of negative emotions. As mentioned earlier, CLOCK gene variations might exert an influence on the structure of brain, which might be associated with both circadian regulation and emotion [68]. In addition, a recent study conducted by Horne and Norbury [69] revealed that eveningness was related to the increase of amygdala response to negative faces and was more likely to suffer from impaired emotion regulation. Thus, evening-type rural residents might be more likely to report psychological distress.
The mediating role of sleep quality
The study also found sleep quality of rural residents partially meditated the association between chronotype and psychological distress, which was in line with our hypothesis and previous literature [70]. Although Smidt and colleagues [71] reported opposite findings, the research only had 52 participants and only abstract was published. Therefore, the quality of the research might be questioned. Evening-type individuals have a higher tendency to drink caffeinated beverage, eat snacks at midnight and suffer from internet addiction [72, 73]. A recent study reported the problematic smartphone use contributed to the enhanced risk of poor sleep quality, anxiety and depression [74]. Another study provided support regarding the positive correlations between PSQI scores and DASS-21 based on a non-clinical sample [75]. In sum, rural dwellers who were prone to eveningness tended to have poorer sleep quality, which further resulted in psychological distress. Thus, enhancing sleep quality might help reduce psychological distress among rural residents, especially those who are prone to eveningness. Prior literature has documented that sleep quality would benefit from exercise, mindfulness and music therapy [76–78], which would further contribute to the decrease in psychological distress.
The moderating role of age
The results presented that age only moderated the association between chronotype and sleep quality among Chinese rural residents. Our findings suggested the association was attenuated in older rural dwellers than younger rural dwellers. As Johnson-Neyman technique presented, with the increase in age, the association between chronotype and sleep quality became weakened. When the age of the participants enhanced to 48.59 and over, the effect of chronotype on sleep quality became insignificant. Sleep problems are more normative as getting older [79] since there were many other influential factors that could disturb sleep, such as the loss and atrophy of neurons, reduced cerebral blood flow and neurotransmitter defects [80]. Thus, the effect of chronotype on sleep quality became weakened for middle-aged rural residents in comparison to younger rural residents.
Contrary to our expectations, age did not moderate the direct effect of chronotype on psychological distress and the association between sleep quality and psychological distress. This expanded the previous literature by uncovering age moderated the relationship between chronotype and psychological distress through moderating the first stage (chronotype—sleep quality) of the indirect path. Taken together, the moderated mediation model has profound implications. The interventions regarding the improvement of sleep quality should be prioritized for rural residents who are prone to eveningness and younger.
Limitations and strengths
Some limitations must be addressed. Firstly, we employed a cross-sectional design, which cannot infer the causal relationship. In the future, longitudinal research could be conducted to validate the results of our study. Secondly, research data were collected through participants’ self-report, which might be subjective and lead to self-reported bias. Further study might benefit from collecting data from various informants (e.g., friends). Thirdly, the participants in our study were all from the rural area of Anhui province, which might geographically limit a wider generalization. Further research could collect data from various regions to ensure a broader generalization. Lastly, psychological distress as a complex concept could be influenced by considerable factors. Only part of psychological distress could be explained by chronotype and sleep quality. Also, there are other variables possibly explaining the associations between chronotype and psychological distress, such as emotional processing [81] and clock genes [82]. A more integrated model with more variables is suggested for further investigation in order to more comprehensively understand psychological distress among rural population.
Despite several limitations, the study adds knowledge to the previous literature, both theoretically and practically. Theoretically, the study sheds light on the potential mechanisms underlying the association between chronotype and psychological distress with the mediating and moderating effects of sleep quality and age, respectively. Practically, the study enlightens the interventions for the prevention and reduction of psychological distress among rural residents.
Conclusion
To our knowledge, this is the first study to explore the relationship between chronotype and psychological distress among Chinese rural population through a moderated mediation model. The prevalence of psychological distress was 33.4% in the study. Sleep quality mediated the association between chronotype and psychological distress. Additionally, age moderated the strength of the mediating effect with the indirect association being attenuated in older Chinese rural residents. For Chinese rural residents who are prone to eveningness, especially those who are younger, it might be essential to design the interventions concerning the enhancement of sleep quality to prevent and decrease psychological distress.
Supporting information
(ZIP)
Acknowledgments
The authors would like to acknowledge all participants and Dr Ye Hong who helped recruit participants and collect data.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Berkanovic E, Hurwicz ML, Landsverk J. Psychological distress and the decision to seek medical care. Social science & medicine (1982). 1988;27(11):1215–21. 10.1016/0277-9536(88)90351-6 [DOI] [PubMed] [Google Scholar]
- 2.Massé R, Poulin C, Dassa C, Lambert J, Bélair S, Battaglini A. The Structure of Mental Health: Higher-Order Confirmatory Factor Analyses of Psychological Distress and Well-Being Measures. Social Indicators Research. 1998;45:475–504. [Google Scholar]
- 3.Dunleavy G, Bajpai R, Tonon AC, Cheung KL, Thach T-Q, Rykov Y, et al. Prevalence of psychological distress and its association with perceived indoor environmental quality and workplace factors in under and aboveground workplaces. Building and Environment. 2020;175:106799. [Google Scholar]
- 4.Holden L, Scuffham P, Hilton M, Vecchio N, Whiteford H. Psychological distress is associated with a range of high-priority health conditions affecting working Australians. Australian and New Zealand journal of public health. 2010;34(3):304–10. 10.1111/j.1753-6405.2010.00531.x [DOI] [PubMed] [Google Scholar]
- 5.Baune BT, Adrian I, Jacobi F. Medical disorders affect health outcome and general functioning depending on comorbid major depression in the general population. Journal of psychosomatic research. 2007;62(2):109–18. 10.1016/j.jpsychores.2006.09.014 [DOI] [PubMed] [Google Scholar]
- 6.Doherty AM, Gaughran F. The interface of physical and mental health. Social psychiatry and psychiatric epidemiology. 2014;49(5):673–82. 10.1007/s00127-014-0847-7 [DOI] [PubMed] [Google Scholar]
- 7.Nordstoga AL, Vasseljen O, Meisingset I, Nilsen TIL, Unsgaard-Tøndel M. Improvement in Work Ability, Psychological Distress and Pain Sites in Relation to Low Back Pain Prognosis: A Longitudinal Observational Study in Primary Care. Spine. 2019;44(7):E423–e9. 10.1097/BRS.0000000000002860 [DOI] [PubMed] [Google Scholar]
- 8.McClung CA. How Might Circadian Rhythms Control Mood? Let Me Count the Ways. Biological Psychiatry. 2013;74(4):242–9. 10.1016/j.biopsych.2013.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sipilä T, Kananen L, Greco D, Donner J, Silander K, Terwilliger J, et al. An Association Analysis of Circadian Genes in Anxiety Disorders. Biological psychiatry. 2010;67:1163–70. 10.1016/j.biopsych.2009.12.011 [DOI] [PubMed] [Google Scholar]
- 10.Greaves-Lord K, Ferdinand R, Oldehinkel A, Sondeijker F, Ormel J, Verhulst F. Higher cortisol awakening response in young adolescents with persistent anxiety problems. Acta psychiatrica Scandinavica. 2007;116:137–44. 10.1111/j.1600-0447.2007.01001.x [DOI] [PubMed] [Google Scholar]
- 11.Vreeburg S, Hoogendijk W, Derijk R, van Dyck R, Smit J, Zitman F, et al. Salivary cortisol levels and the 2-year course of depressive and anxiety disorders. Psychoneuroendocrinology. 2013;38 10.1016/j.psyneuen.2012.12.017 [DOI] [PubMed] [Google Scholar]
- 12.Carpenter J, Abelmann A, Hatton S, Robillard R, Hermens D, Bennett M, et al. Pineal volume and evening melatonin in young people with affective disorders. Brain imaging and behavior. 2016;11. [DOI] [PubMed] [Google Scholar]
- 13.Robillard R, Hermens D, Naismith S, White D, Rogers N, Ip T, et al. Ambulatory sleep-wake patterns and variability in young people with emerging mental disorders. Journal of psychiatry & neuroscience: JPN. 2014;39:130247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Duffy JF, Rimmer DW, Czeisler CA. Association of intrinsic circadian period with morningness–eveningness, usual wake time, and circadian phase. Behavioral Neuroscience. 2001;115(4):895–9. 10.1037//0735-7044.115.4.895 [DOI] [PubMed] [Google Scholar]
- 15.Bailey S, Heitkemper M. Circadian rhythmicity of cortisol and body temperature: Morningness-eveningness effects. Chronobiology international. 2001;18:249–61. 10.1081/cbi-100103189 [DOI] [PubMed] [Google Scholar]
- 16.Nikhil J, K N M, Prabhu P P. Diurnal changes in differential sensitivity and temporal resolution in morning-type and evening-type individuals with normal hearing. 2018;4:229–33. 10.1016/j.wjorl.2017.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Park CI, An SK, Kim HW, Koh MJ, Namkoong K, Kang JI, et al. Relationships between chronotypes and affective temperaments in healthy young adults. Journal of Affective Disorders. 2015;175:256–9. 10.1016/j.jad.2015.01.004 [DOI] [PubMed] [Google Scholar]
- 18.Jeong H, Moon E, Park J, Lee B, Lee YM, Choi Y, et al. The relationship between chronotype and mood fluctuation in the general population. Psychiatry research. 2015;229. [DOI] [PubMed] [Google Scholar]
- 19.Wang H, Stokes JE. Trajectories of rural-urban disparities in biological risks for cardiovascular disease among Chinese middle-aged and older adults. Health & Place. 2020;64:102354 10.1016/j.healthplace.2020.102354 [DOI] [PubMed] [Google Scholar]
- 20.Stickley A, Koyanagi A, Roberts B, McKee M. Urban–rural differences in psychological distress in nine countries of the former Soviet Union. Journal of Affective Disorders. 2015;178:142–8. 10.1016/j.jad.2015.02.020 [DOI] [PubMed] [Google Scholar]
- 21.Vlahov D, Galea S, Freudenberg N. The urban health "advantage". Journal of urban health: bulletin of the New York Academy of Medicine. 2005;82(1):1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu Y, Lei P, Ye R, Sunil TS, Zhou H. Prevalence and risk factors of depression in middle-aged and older adults in urban and rural areas in China: a cross-sectional study. The Lancet. 2019;394:S53. [Google Scholar]
- 23.Kawasaki T, Cugini P, Itoh K, Uezono K, Ogaki T, Yoshimizu Y, et al. Circadian rhythm of blood pressure and life style: a study of clinically healthy subjects living in rural and industrialized countries. Journal of human hypertension. 1996;10(5):281–5. [PubMed] [Google Scholar]
- 24.Hu R, Gong C. Leisure difference between urban and rural residents and its influencing factors. Journal of Guizhou Normal University (Social Science). 2018;2:41–9. [Google Scholar]
- 25.de Souza CM, Hidalgo MP. The midpoint of sleep on working days: a measure for chronodisruption and its association to individuals' well-being. Chronobiology international. 2015;32(3):341–8. 10.3109/07420528.2014.979941 [DOI] [PubMed] [Google Scholar]
- 26.Lee Y, Kim J, Han ES, Chae S, Ryu M, Ahn KH, et al. Changes in physical activity and cognitive decline in older adults living in the community. Age (Dordrecht, Netherlands). 2015;37(2):20 10.1007/s11357-015-9759-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee C-Y, Chen H-C, Tseng M-C, Lee H-C, Huang L-H. The Relationships among sleep quality and chronotype, emotional disturbance, and insomnia vulnerability in shift nurses. The journal of nursing research: JNR. 2015;23:225–35. 10.1097/jnr.0000000000000095 [DOI] [PubMed] [Google Scholar]
- 28.Rique GLN, Fernandes Filho GMC, Ferreira ADC, de Sousa-Muñoz RL. Relationship between chronotype and quality of sleep in medical students at the Federal University of Paraiba, Brazil. Sleep Science. 2014;7(2):96–102. 10.1016/j.slsci.2014.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiology international. 2006;23:497–509. 10.1080/07420520500545979 [DOI] [PubMed] [Google Scholar]
- 30.Yun J-A, Ahn Y-S, Jeong K-S, Joo E-J, Choi K-S. The relationship between chronotype and sleep quality in Korean firefighters. Clinical Psychopharmacology and Neuroscience. 2015;13:201–8. 10.9758/cpn.2015.13.2.201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kohn TP, Kohn JR, Haney NM, Pastuszak AW, Lipshultz LI. The effect of sleep on men’s health. Translational Andrology and Urology. 2019:S178–S85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jamieson D, Beaudequin D, McLoughlin L, Parker M, Lagopoulos J, Hermens D. Associations between sleep quality and psychological distress in early adolescents 2019. [DOI] [PubMed] [Google Scholar]
- 33.Levandovski R, Dantas G, Fernandes L, Caumo W, Torres I, Roenneberg T, et al. Depression scores associate With chronotype and social jetlag in a rural population. Chronobiology international. 2011;28:771–8. 10.3109/07420528.2011.602445 [DOI] [PubMed] [Google Scholar]
- 34.Kim S, Lee Y, Kim H, Cho I, Lee J-Y, Cho S-J. Age as a moderator of the association between depressive symptoms and morningness-eveningness. Journal of psychosomatic research. 2010;68:159–64. 10.1016/j.jpsychores.2009.06.010 [DOI] [PubMed] [Google Scholar]
- 35.Au J, Reece J. The relationship between chronotype and depressive symptoms: A meta-analysis. Journal of Affective Disorders. 2017;218:93–104. 10.1016/j.jad.2017.04.021 [DOI] [PubMed] [Google Scholar]
- 36.Horne JA, Ostberg O. A self sssessment questionnaire to determine morningness eveningness in human circadian rhythms. International journal of chronobiology. 1976;4:97–110. [PubMed] [Google Scholar]
- 37.Sun J, Chen M, Cai W, Wang Z, Wu S, Sun X, et al. Chronotype: implications for sleep quality in medical students. Chronobiology International. 2019;36:1–9. 10.1080/07420528.2018.1513943 [DOI] [PubMed] [Google Scholar]
- 38.Zhang B, Hao Y-l, Rong R-g. The reliability and validity of Chinese version morningness/eveningness questionnaire. Chinese Journal of Behavioral Medical Science. 2006;15(9):856–8. [Google Scholar]
- 39.Li S, Li Q-q, Wang X-F, Liu L-J, Liu Y, Zhang L-X, et al. Preliminary test for the Chinese version of the Morningness–Eveningness Questionnaire. Sleep and Biological Rhythms. 2011;9 10.1111/j.1479-8425.2010.00461.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Buysse D, Reynolds C, Monk T, Berman S, Kupfer D. The Pittsburgh Sleep Quality Index—A new instrument For psychiatric practice and research. Psychiatry research. 1989;28:193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 41.Zheng B, Li M, Wang K, Lv J. Analysis of the reliability and validity of the Chinese version of Pittsburgh sleep quality index among medical college students. Journal of Peking University Health sciences. 2016;48:424–8. [PubMed] [Google Scholar]
- 42.Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33(3):335–43. 10.1016/0005-7967(94)00075-u [DOI] [PubMed] [Google Scholar]
- 43.Lovibond SH, Lovibond PF. Manual for the Depression, Anxiety and Stress Scales (DASS) 1995. [DOI] [PubMed] [Google Scholar]
- 44.Zanon C, Brenner R, Baptista M, Vogel D, Rubin M, Al-Darmaki F, et al. Examining the dimensionality, reliability, and invariance of the Depression, Anxiety, and Stress Scale–21 (DASS-21) across eight countries. Assessment. 2020:107319111988744. [DOI] [PubMed] [Google Scholar]
- 45.Tran TD, Tran T, Fisher J. Validation of the depression anxiety stress scales (DASS) 21 as a screening instrument for depression and anxiety in a rural community-based cohort of northern Vietnamese women. BMC Psychiatry. 2013;13(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang K, Shi H, Geng F, Zou L-q, Tan S, Wang Y, et al. Cross-Cultural validation of the Depression Anxiety Stress Scale-21 in China. Psychological assessment. 2015;28. [DOI] [PubMed] [Google Scholar]
- 47.MacKinnon D. An Introduction to statistical mediation analysis. 2008:245. [Google Scholar]
- 48.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. 2013. [Google Scholar]
- 49.Hayes AF, Rockwood N. Regression-based statistical mediation and moderation analysis in clinical research:Observations, recommendations, and implementation. Behaviour Research and Therapy. 2016;98. [DOI] [PubMed] [Google Scholar]
- 50.Feng D, Ji L, Xu L. The influence of social support, lifestyle and functional disability on psychological distress in rural China: Structural equation modelling. Australian Journal of Rural Health. 2013;21(1):13–9. 10.1111/ajr.12009 [DOI] [PubMed] [Google Scholar]
- 51.Kilkkinen A, Kao‐Philpot A, O’Neil A, Philpot B, Reddy P, Bunker S, et al. Prevalence of psychological distress, anxiety and depression in rural communities in Australia. Australian Journal of Rural Health. 2007;15:114–9. 10.1111/j.1440-1584.2007.00863.x [DOI] [PubMed] [Google Scholar]
- 52.Feng D, Ji L, Xu L. Effect of subjective economic status on psychological distress among farmers and non-farmers of rural China. Australian Journal of Rural Health. 2015;23(4):215–20. 10.1111/ajr.12187 [DOI] [PubMed] [Google Scholar]
- 53.Bourbonnais R, Moisan J, Vézina M. Job strain and psychological distress in white-collar workers. Scandinavian journal of work, environment & health. 1996;22:139–45. 10.5271/sjweh.122 [DOI] [PubMed] [Google Scholar]
- 54.Firdaus G. Increasing rate of psychological distress in urban households: How does income matter? Community Mental Health Journal. 2017;54. [DOI] [PubMed] [Google Scholar]
- 55.Lee S, Leung C, Kwok K, Ng K. A community-based study of the relationship between somatic and psychological distress in Hong Kong. Transcultural psychiatry. 2015;52 10.1177/1363461515569756 [DOI] [PubMed] [Google Scholar]
- 56.Stickley A, Koyanagi A, Roberts B, McKee M. Urban–rural differences in psychological distress in nine countries of the former Soviet Union. Journal of Affective Disorders. 2015;178 10.1016/j.jad.2015.02.020 [DOI] [PubMed] [Google Scholar]
- 57.Zhang M, Zhang J, Zhang F, Zhang L, Feng D. Prevalence of psychological distress and the effects of resilience and perceived social support among Chinese college students: Does gender make a difference? Psychiatry Research. 2018;267:409–13. 10.1016/j.psychres.2018.06.038 [DOI] [PubMed] [Google Scholar]
- 58.Masood A, Masud Y, Mazahir S. Gender differences in resilience and psychological distress of patients with burns. Burns. 2016;42(2):300–6. 10.1016/j.burns.2015.10.006 [DOI] [PubMed] [Google Scholar]
- 59.Chung R, Bemak F, Kagawa Singer M. Gender differences in psychological distress among southeast asian refugees. The Journal of nervous and mental disease. 1998;186:112–9. 10.1097/00005053-199802000-00007 [DOI] [PubMed] [Google Scholar]
- 60.Matud M, Bethencourt-Pére J, ibañez I. Gender differences in psychological distress in Spain. The International Journal of social psychiatry. 2014;61 10.1177/0020764014564801 [DOI] [PubMed] [Google Scholar]
- 61.Wong D, Song H. The resilience of migrant workers in Shanghai China: the roles of migration stress and meaning of migration. The International journal of social psychiatry. 2008;54:131–43. 10.1177/0020764007083877 [DOI] [PubMed] [Google Scholar]
- 62.National Bureau of Statistics of China. Report on monitoring and investigation of migrant workers in 2018. 2019 April 29 [Cited 2020 April 20]. Available from: http://www.stats.gov.cn/tjsj/zxfb/201904/t20190429_1662268.html.
- 63.Chen L, Li W, He J, Wu L, Yan Z, Tang W. Mental health, duration of unemployment, and coping strategy: a cross-sectional study of unemployed migrant workers in eastern China during the economic crisis. BMC public health. 2012;12:597 10.1186/1471-2458-12-597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zeng C, Li X, Yang X, Du H, Lin D. Experiences of stigma and suicidal behaviors among rural-to-urban migrants: the mechanistic roles of depression and substance use. Psychology, Health & Medicine. 2019;25:1–11. 10.1080/13548506.2019.1687921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Soulsby L, Bennett K. Marriage and psychological wellbeing: the role of social support. Psychology. 2015;6:1349. [Google Scholar]
- 66.Cox RC, Olatunji BO. Differential associations between chronotype, anxiety, and negative affect: A structural equation modeling approach. Journal of Affective Disorders. 2019;257:321–30. 10.1016/j.jad.2019.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ehlers C, Frank E, Kupfer D. Social Zeitgebers and Biological Rhythms: A Unified Approach to Understanding the Etiology of Depression. Archives of general psychiatry. 1988;45:948–52. 10.1001/archpsyc.1988.01800340076012 [DOI] [PubMed] [Google Scholar]
- 68.Bauducco S, Richardson C, Gradisar M. Chronotype, circadian rhythms and mood. Current Opinion in Psychology. 2020;34:77–83. 10.1016/j.copsyc.2019.09.002 [DOI] [PubMed] [Google Scholar]
- 69.Horne CM, Norbury R. Late chronotype is associated with enhanced amygdala reactivity and reduced fronto-limbic functional connectivity to fearful versus happy facial expressions. NeuroImage. 2018;171:355–63. 10.1016/j.neuroimage.2018.01.025 [DOI] [PubMed] [Google Scholar]
- 70.Selvi Y, Boysan M, Kandeger A, Uygur Ö, Sayin A, Akbaba N, et al. Heterogeneity of sleep quality in relation to circadian preferences and depressive symptomatology among major depressive patients. Journal of Affective Disorders. 2018;235 10.1016/j.jad.2018.08.003 [DOI] [PubMed] [Google Scholar]
- 71.Smidt A, Latham MD, Allen N. Do sleep parameters mediate the association between chronotype and mental health? Sleep. 2017;40:A413–A. [Google Scholar]
- 72.Randler C. Association between chronotype and diet in adolescents based on food logs. Eating Behaviors. 2009;10:115–8. 10.1016/j.eatbeh.2009.03.002 [DOI] [PubMed] [Google Scholar]
- 73.Randler C, Wolfgang L, Matt K, Demirhan E, Horzum mb, Beşoluk Ş. Smartphone addiction proneness in relation to sleep and morningness–eveningness in German adolescents. Journal of Behavioural Addictions. 2016;5 10.1556/2006.5.2016.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yang J, Fu X, Liao X, Li Y. Association of problematic smartphone use with poor sleep quality, depression, and anxiety: A systematic review and meta-analysis. Psychiatry Research. 2020;284:112686 10.1016/j.psychres.2019.112686 [DOI] [PubMed] [Google Scholar]
- 75.João K, Jesus S, Carmo C, Pinto P. The impact of sleep quality on the mental health of a non-clinical population. Sleep Medicine. 2018;46 10.1016/j.sleep.2017.12.020 [DOI] [PubMed] [Google Scholar]
- 76.Wang C-F, Sun Y-L, Zang H-X. Music therapy improves sleep quality in acute and chronic sleep disorders: A meta-analysis of 10 randomized studies. International Journal of Nursing Studies. 2014;51(1):51–62. 10.1016/j.ijnurstu.2013.03.008 [DOI] [PubMed] [Google Scholar]
- 77.Lederman O, Ward PB, Firth J, Maloney C, Carney R, Vancampfort D, et al. Does exercise improve sleep quality in individuals with mental illness? A systematic review and meta-analysis. Journal of Psychiatric Research. 2019;109:96–106. 10.1016/j.jpsychires.2018.11.004 [DOI] [PubMed] [Google Scholar]
- 78.Rash JA, Kavanagh VAJ, Garland SN. A meta-analysis of mindfulness-based therapies for insomnia and sleep disturbance: Moving towards processes of change. Sleep Medicine Clinics. 2019;14(2):209–33. 10.1016/j.jsmc.2019.01.004 [DOI] [PubMed] [Google Scholar]
- 79.Sonnega J, Sonnega A. Intermet use and sleep among older adults in the United States. Innovation in Aging. 2018;2:962–3. [Google Scholar]
- 80.Polo-Kantola P. Sleep problems in midlife and beyond. Maturitas. 2011;68(3):224–32. [DOI] [PubMed] [Google Scholar]
- 81.Berdynaj D, Boudissa SN, Grieg MS, Hope C, Mahamed SH, Norbury R. Effect of chronotype on emotional processing and risk taking. Chronobiology International. 2016;33(4):406–18. 10.3109/07420528.2016.1146739 [DOI] [PubMed] [Google Scholar]
- 82.Jankowski KS, Dmitrzak-Weglarz M. ARNTL, CLOCK and PER3 polymorphisms–links with chronotype and affective dimensions. Chronobiology International. 2017;34(8):1105–13. 10.1080/07420528.2017.1343341 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(ZIP)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.