Abstract
A primigravid woman with Covid-19 related respiratory insufficiency was admitted into a tertiary Intensive Care Unit at 23 3/7 weeks’ gestation. Highly sensitive flow cytometry of peripheral leukocytes indicated significantly suppressed naïve T- and B-cell compartments. The suppressed immune cell responses led us keep the initially started administration of corticosteroids for fetal and maternal indication at a low dose. After three weeks her B-cell response peaked, SARS-CoV-2 was cleared and clinical improvement ensued a week later. At 28 weeks’ gestation, a son of 1570 g was born by cesarean section. She was extubated two days postpartum and discharged from hospital 5.5 weeks postpartum.
Keywords: Covid-19, Pregnancy, Immune monitoring, Flow cytometry
1. Introduction
Cases of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) increase, but data on pregnant women with Covid-19 remain sparse. The vast majority of pregnant women seem to experience mild disease. In the United Kingdom, estimated incidence of hospital admission with confirmed Covid-19 in pregnancy was 4.9 per 1000 maternities, and 10 % of women require respiratory support. (Knight et al., 2020) Pathophysiological mechanisms leading to severe disease, and particularly the role of the immune system, remain largely unknown, both during and outside pregnancy. Here, we describe an exceptional sentinel case of a healthy pregnant woman who developed critical Covid-19. Detailed flow-cytometric immune monitoring informed clinical decision making and may provide clues into disease pathways.
1.1. Case
A 30-year-old primigravid Caucasian women with an unremarkable medical history (except for subclinical hypothyroidism) and a body mass index of 18.2 kg/m² was admitted into a secondary hospital with a deteriorating respiratory condition and fever at 23 week’s gestation (detailed clinical parameters are shown in the Supplementary material). Chest radiography showed bilateral pneumonia. Suspected SARS-CoV-2 infection was confirmed with polymerase chain reaction (PCR). Her condition rapidly deteriorated. At 23 3/7 weeks’ gestation (hospital day 4), she was transferred to a tertiary medical center, with neonatal intensive care support available from the national threshold of 24 weeks’ gestation onwards. She was admitted into the ICU and intubated due to threatening respiratory failure. Corticosteroids for fetal lung maturation were not administered at that time, considering potential risks of negatively affecting the maternal immune response (this moment was two months prior to publication of the preliminary report of the RECOVERY trial showing that dexamethasone reduces mortality among Covid-19 patients receiving mechanical ventilation (Horby et al., 2020)).
In the following week, her pulmonary parameters stabilized and chest radiography showed some signs of improvement. However, on hospital day 15, her respiratory condition deteriorated with increased oxygen demand. Viral load came back high and a CT-scan showed 80 % reduced translucency of pulmonary tissue. The following day remdesivir therapy was started and she was ventilated in prone position for two days with minimal response. It was deemed increasingly likely that her condition could benefit from ending the pregnancy, and based on expert opinion combined with emerging evidence that corticosteroids were not detrimental to clearance of SARS-CoV-2, she was administered corticosteroids for fetal lung maturation (intramuscular betamethasone injection of 11.4 mg for two days) at 25 3/7 weeks’ gestation (hospital days 18 and 19). The day after, oral prednisolone 60 mg daily was started, in order to suppress the maternal inflammatory response.
On hospital day 30 (27 1/7 weeks’ gestation), her respiratory condition improved and SARS-CoV-2 PCRs were negative for the fourth consecutive day (and would remain negative throughout the rest of admission). Ultrasonographic examination revealed a normal fetal biophysical profile, with an estimated fetal weight on the 91st percentile. As her condition had improved considerably, it was decided not to end the pregnancy at that time, hypothesizing that risks of surgery outweighed benefits to her clinical condition.
On hospital day 37 (28 1/7 weeks’ gestation) fever occurred. Two days later, temperature and CRP-levels had continued to rise, while no explanation could be identified. It was decided to perform cesarean section because of potential compromise of the pregnancy on maternal recovery. During surgery, there were no signs of intrauterine infection. A son was born with a birth weight of 1570 g (96th percentile) and Apgar score of 9/8/7. The day after, the clinical status of the woman improved markedly. She responded by opening her eyes to light and speech, with normalization of body temperature and improved respiratory function. Two days after cesarean section, she was extubated. She was discharged from ICU on hospital day 47 (7 days postpartum). After four weeks in inpatient care she was discharged to rehabilitation care, suffering from mild critical illness neuropathy. Directly after birth, her son was admitted into the neonatal intensive care unit (NICU) and stayed there for six weeks, with morbidity resulting from preterm birth.
2. Materials and methods
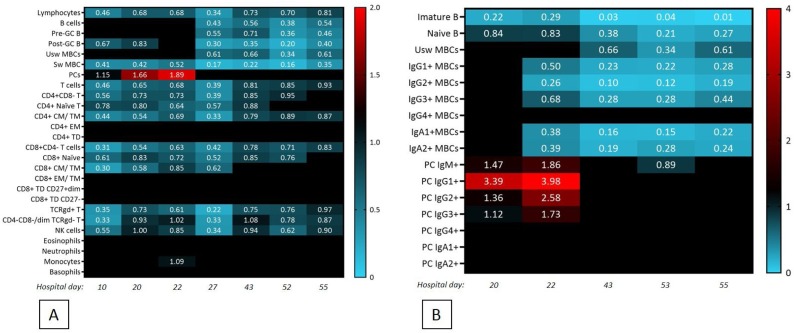
Flow cytometric strategies have been developed for rapid and detailed immune profiling. The EuroFlow consortium (www.euroflow.org) has established a standardized and extensive panel of immune monitoring tubes, able to detect subsets in the full leukocyte repertoire. The panels used were: the standardized Primary Immunodeficiency Orientation Tube (PIDOT) consisting of an 8-colour, 12-antibody combination (van der Burg et al., 2019) and an adaptation of the B-cell tube (Blanco et al., 2019) consisting of 16-colour, 23-antibodies, enabling deep analysis of B-cell and plasma cell subsets (≥100), detection of small clonal B-cell populations, main leukocyte and lymphoid subsets and main maturation T-cell stages. Up to ten million leukocytes are analyzed per panel and time point. Measurements were performed on the following hospital days: 10, 20, 22, 27, 43, 52 and 55 for the PIDOT and 20, 22, 43, 52 and 55 for the B-cell tube. Outcomes of measurements can be compared to established EuroFlow age-matched reference values (Blanco et al., 2019; van der Burg et al., 2019). This technique enables detection of small deviations in the immune repertoire, which may be subclinical under normal circumstances.
3. Results and discussion
The patient was lymphopenic during all measurements, with absolute lymphocyte counts below the 5th percentile of normal range (Fig. 1 and Supplementary material). A major increase in monocytes was observed between hospital day 20 and hospital day 22. Total B-cells, T-cells and NK-cells were low across all time points. Because a gradual increase in the number of plasma cells compared to age-matched controls was seen (van der Burg et al., 2019), suggesting the beginning of an adaptive immune response, administration of corticosteroids was limited to prednisolone (methylprednisolone was considered potentially too detrimental to the maternal immune response) and kept at a low dose. Indeed the increase in plasma cells continued after initiation of prednisolone (at 60 mg/day on hospital day 20–26, 30 mg/day on hospital day 27–30 and 15 mg/day on hospital day 31–34). Eventually, the use of prednisolone led to a decrease in plasma cell peak. However, the first neutralizing antibodies were found, albeit still with low titers. The delayed immunoglobulin (Ig) response was reflected by a low number of Ig-switched B cells. T cells were also low, both CD4+ and CD8+, Th1 and Th2 and importantly also the follicular T helper cells that are responsible for inducing the germinal center reaction leading to class-switched B cells. This may be the reason why mostly IgG3 (which can cross epithelial barriers to some extent) rather than IgAs (the major Ig isotype capable of crossing epithelial barriers) were produced. Naïve T cells remained low throughout the clinical course, while increased neutrophils and a transient monocyte peak were apparent, although not above reference values. We assessed the composition of the naïve B cell compartment, since the size of this compartment represents the number of newly formed B cells and hence gives an impression of the diversity of the B cell repertoire (Fig. 1B). Within the naïve compartment, various sub-compartments can be identified based on the expression of CD5, hence only the immature naïve B cells, are recent bone marrow emigrants. The size of this compartment was very small in this woman compared to age-matched controls, suggesting a minute B cell repertoire diversity.
Fig. 1.
Numerical deviations of circulating leukocyte subsets.
Successful clearance of any viral infection requires CD8 + T cell-mediated killing and CD4 + T cell-mediated help to cognate B cells to produce neutralizing antibodies. Clearly also innate cells are important, as well as soluble immune mediators (cytokines, antibodies, complement factors). It is the combination of these different effector mechanisms that determines viral clearance or persistence. The seemingly contradicting processes of hyperinflammation, immune suppression and viral activity inevitably lead to dilemmas for treating physicians, especially at the ICU, particularly in a pregnant women where the fetus also is at risk with most therapeutics used.
To gain insight into biomarkers with predictive power to assist clinical decision, we decided to perform state-of-the-art immune monitoring with as widely as possible assessment of the adaptive and innate immune system. These studies have led to the notion that the size of naive T and B cell compartment and thereby the diversity of the T cell receptor (TR) and Ig repertoires are critical determinants of clinical outcome. In the case reported here, at all time points a very small naïve T and B cell compartment was found, even smaller than in most elderly people who generally have small compartments. Nevertheless, eventually a productive plasma cell peak, which preceded the antibody serum peak, was observed. Although corticosteroids were indicated and administered, this was done at low dosage, based on the immune monitoring indicating an emerging Ig response.
We had obtained blood samples from the woman shortly before she got pregnant showing leukopenia and severe lymphopenia prior to pregnancy. It is therefore tempting to speculate that she had sustained low naïve T and B cell numbers for a while, irrespective of pregnancy. Hence we postulate that the patient’s pregnancy has unlikely contributed to the severe clinical course, although mechanical compression resulting from third-trimester pregnancy may have contributed to the maternal respiratory compromise.
Informed consent statement
The patient provided written informed consent to publish this article.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
None.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.jri.2020.103243.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Blanco E., et al. Defects in memory b-cell and plasma cell subsets expressing different immunoglobulin-subclasses in patients with cvid and immunoglobulin subclass deficiencies. J. Allergy Clin. Immunol. 2019;144:809–824. doi: 10.1016/j.jaci.2019.02.017. [DOI] [PubMed] [Google Scholar]
- Horby P., et al. Effect of dexamethasone in hospitalized patients with covid-19: preliminary report. medRxiv. 2020 2020.06.22.20137273. [Google Scholar]
- Knight M., et al. Characteristics and outcomes of pregnant women admitted to hospital with confirmed sars-cov-2 infection in uk: national population based cohort study. BMJ. 2020;369 doi: 10.1136/bmj.m2107. m2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Der Burg M., et al. The euroflow pid orientation tube for flow cytometric diagnostic screening of primary immunodeficiencies of the lymphoid system. Front. Immunol. 2019;10:246. doi: 10.3389/fimmu.2019.00246. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.