Abstract
Introduction
In addition to the directly attributed mortality, COVID-19 is also likely to increase mortality indirectly. In this systematic review, we investigate the direct and indirect effects of COVID-19 on out-of-hospital cardiac arrests.
Methods
We searched PubMed, BioMedCentral, Embase and the Cochrane Central Register of Controlled Trials for studies comparing out-of-hospital cardiac arrests occurring during the pandemic and a non-pandemic period. Risk of bias was assessed with the ROBINS-I tool. The primary endpoint was return of spontaneous circulation. Secondary endpoints were bystander-initiated cardiopulmonary resuscitation, survival to hospital discharge, and survival with favourable neurological outcome.
Results
We identified six studies. In two studies, rates of return of spontaneous circulation and survival to hospital discharge decreased significantly during the pandemic. Especially in Europe, bystander-witnessed cases, bystander-initiated cardiopulmonary resuscitation and resuscitation attempted by emergency medical services were reduced during the pandemic. Also, ambulance response times were significantly delayed across all studies and patients presenting with non-shockable rhythms increased in two studies. In 2020, 3.9–5.9% of tested patients were SARS-CoV-2 positive and 4.8–26% had suggestive symptoms (fever and cough or dyspnoea).
Conclusions
Out-of-hospital cardiac arrests had worse short-term outcomes during the pandemic than a non-pandemic period suggesting direct effects of COVID-19 infection and indirect effects from lockdown and disruption of healthcare systems. Patients at high risk of deterioration should be identified outside the hospital to promptly initiate treatment and reduce fatalities.
Study registration PROSPERO CRD42020195794.
Keywords: Out-of-hospital cardiac arrest, COVID-19, Cardiopulmonary resuscitation
Introduction
Since December 2019, several cases of atypical pneumonia caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) were reported in Wuhan, China.1 This novel coronavirus is currently responsible for the coronavirus disease 2019 (COVID-19) pandemic that rapidly spread in Europe and worldwide. As of November 4, 2020, SARS-CoV-2 infected more than 47 million individuals globally, causing more than 1 million deaths.2 The COVID-19 pandemic may also be responsible for excess deaths in individuals not directly affected by SARS-CoV-2 infection. An increase in indirect mortality may arise from altered access to healthcare services secondary to the profound reorganization of hospitals3 and the effects of lockdown on physical, psychological, and social wellbeing. Moreover, lockdown and the fear of contracting the infection in hospitals could have prevented patients from calling emergency medical services (EMS) or presenting to emergency departments.4
In Lombardy, Northern Italy,5, 6 Paris, France,7 and New York City, USA,8 the incidence of out-of-hospital cardiac arrest (OHCA) during the COVID-19 pandemic markedly increased compared with previous years and was associated with high mortality. In contrast, other areas of Northern Italy9 and the USA10 did not experience the same variations. Although causes are still unclear, these findings suggest that incidence and outcomes of OHCA might be directly or indirectly affected by the COVID-19 pandemic. While COVID-19 is often a self-limited lower respiratory tract illness, patients may suffer from a rapidly worsening hypoxic respiratory failure, eventually leading to cardiac arrest if not promptly treated. COVID-19 might also cause cardiac arrest due to SARS-CoV2 infection causing vascular inflammation, myocardial injury,11 arrhythmias, and thromboembolism12 leading to myocardial infarction or pulmonary embolism. Delays in treating time-dependent conditions, such as acute coronary syndromes,13 may lead to cardiac arrests as most OHCA are related to myocardial ischemia.14 Moreover, overall survival after OHCA might be affected by fear of infection, reducing rates of bystander-initiated cardiopulmonary resuscitation (CPR),15 and overload of emergency medical services (EMS)16 causing delays in ambulance arrival.
We conducted a systematic review to ascertain the direct and indirect effects of the COVID-19 pandemic on the incidence, treatment, and outcomes of OHCA.
Methods
This systematic review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines,17, 18 and the protocol was registered in PROSPERO (CRD42020195794).19 We used the PICO (Population, Intervention or exposure, Comparison, Outcome) framework to frame the review question: Among adults with OHCA (P), does the COVID-19 pandemic, compared with a non-pandemic period (C), affect ROSC, bystander-CPR, survival to hospital discharge or 30 days, and survival with favourable neurological outcome (O)?
Search strategy and study selection
We systematically searched PubMed, BioMedCentral, EMBASE and the Cochrane Central Register of Controlled Trials (CENTRAL) for pertinent studies from the earliest publication date available through September 6th, 2020 (Supplemental Table 3). We also reviewed the references of articles identified by this search strategy and selected those we considered relevant. We considered eligible randomized controlled trials, prospective and retrospective observational studies, and case series published in peer-reviewed journals comparing OHCAs occurring during the COVID-19 pandemic and a non-pandemic period as defined by study authors. We excluded systematic reviews, editorials, and literature reviews. After the removal of duplicates, eligibility assessment at the title/abstract level was performed by two investigators. The final selection of included articles was based on complete manuscripts with disagreements resolved by agreement under the supervision of one investigator (GL).
Data collection and presentation
Data were independently extracted by two authors using a standardized form with disagreements resolved by discussion and involving a third reviewer. Extracted data included first author, publication year, country, study period, number of OHCAs and COVID-19 cases, rates of bystander-CPR, return of spontaneous circulation (ROSC), and survival, characteristics of patients, pre-hospital interventions, arrival time of EMS, and risk of bias using the tool Risk Of Bias In Nonrandomized Studies–of Interventions (ROBINS-I).20 Study authors were contacted to obtain missing data. The pre-specified primary endpoint was ROSC. Secondary pre-specified endpoints were bystander-CPR, survival to hospital discharge or 30 days, and survival with favourable neurological outcome. Also, patients characteristics (age and sex), presenting rhythm, location, bystander witnessed, bystander-CPR, COVID-19 status (positive or suspected), EMS response time, resuscitation attempted by EMS, and orotracheal intubation were post-hoc analysed.
When only a median and interquartile range (IQR) were available, we estimated mean and standard deviation (SD) according to the method by Wan et al.21 Pre-specified subgroup analysis was performed for geographical location. Due to an important clinical heterogeneity secondary to differences between systems and the impact of COVID-19 itself on these systems, we did not report a pooled estimate and we used forest plots with RevMan Version 5.3 to display results of individual studies.
Results
Study characteristics
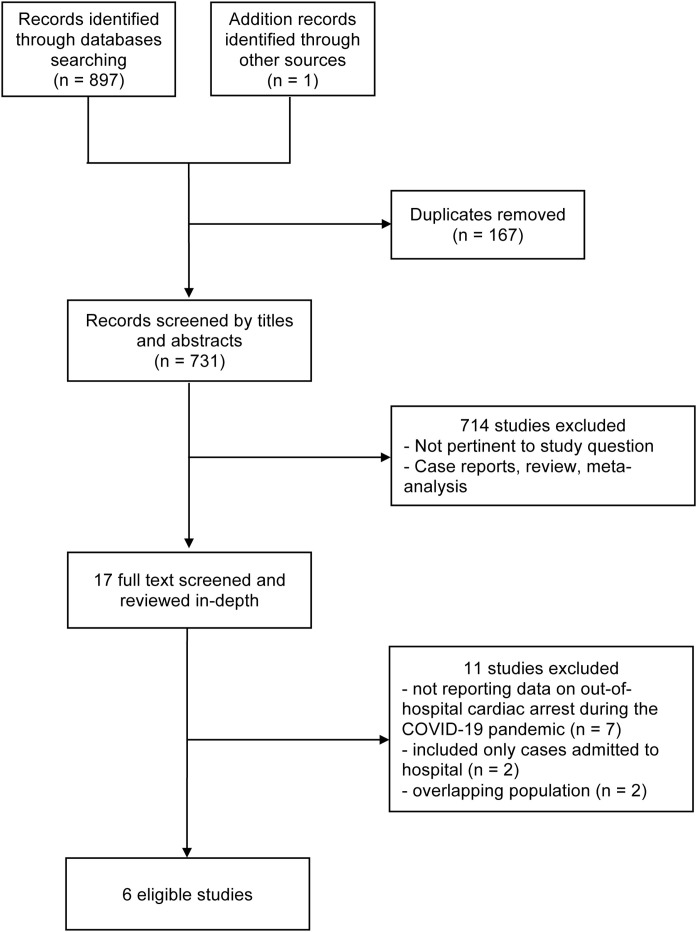
Our search strategy yielded a total of 898 articles. After removing duplicates and non-pertinent articles examined at the title and abstract level, we retrieved 17 studies as full text for detailed assessment and six studies were finally included (Fig. 1 ). Details of excluded studies are available in Supplemental Table 1. Three studies were conducted in Europe,6, 7, 9 two in the USA,8, 10 and one in Asia.23 Main characteristics of included studies are described in Table 1 .
Fig. 1.
Selection of included studies.
Table 1.
Characteristics of studies included ordered by first author.
| Study | Geographical area of study | OHCA patients included | COVID-19 pandemic (1) and non-pandemic (2) period | COVID-19 casesb | COVID-19 prevalence among OHCAs |
|---|---|---|---|---|---|
| Baldi et al., 20206 | Lombardy (provinces of Lodi, Cremona, Pavia, and Mantua), Italy | All cases | (1) Feb. 21 – April 20, 2020 (2) Feb. 21 – April 21, 2019 |
14,785 | 26% with symptomsa 3.9% with confirmed diagnosis |
| Cho et al., 202021 | Daegu, South Korea | EMS-treated adults of presumed medical aetiology | (1) Feb. 17 – March 31, 2020 (2) Feb. 17 – March 31, 2018 |
6719 | 17.5% with symptomsa 5.9% with confirmed diagnosis |
| Lai et al., 20208 | New York City, USA | EMS-treated, adults (≥18 years) cases | (1) March 1 – April 25, 2020 (2) March 1 – April 25, 2019 |
159,851 | n/a |
| Marijon et al., 20207 | Paris and its suburbs, France | Non-traumatic, adults (≥18 years) cases | (1) March 16 – April 26, 2020 (2) Weeks 12-17, 2012-19 |
7587 | 8.1% with symptomsa 4.8% with confirmed diagnosis |
| Paoli et al., 20209 | Province of Padua, Italy | All cases | (1) March 1 – April 30, 2020 (2) March 1 – April 30, 2019 |
3851 | n/a |
| Sayre et al., 202010 | Seattle and King County, USA | All cases | (1) Feb. 26 – April 15, 2020 (2) Jan. 1 – Feb. 25, 2020 |
4873 | 4.8% with symptomsa 4.3% with confirmed diagnosis |
Abbreviations: OHCA = out-of-hospital cardiac arrest, EMS = emergency medical services.
Fever associated with cough or dyspnoea.
During the study period.
Risk of bias
All included studies were assessed as being at an overall serious risk of bias. The most common sources of bias were reporting results not adjusted for confounding factors, participant selection, missing data, and outcome measurement. There was low to moderate risk of bias from reporting of result and intervention classification or deviation (Supplemental Table 2).
Return of spontaneous circulation and survival at hospital discharge
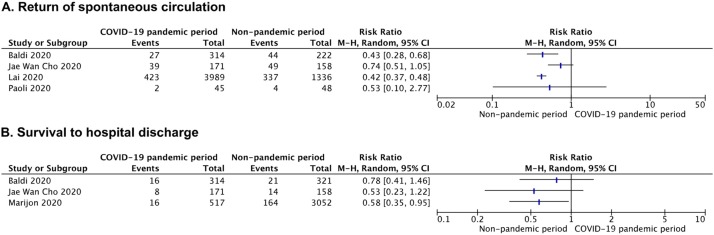
We identified four studies reporting ROSC.6, 8, 9, 23 Two studies, one conducted in Italy and one in the USA, observed significantly lower rates of ROSC in victims of OHCA during the COVID-19 pandemic when compared with victims of the non-pandemic period.6, 8 In Northern Italy, ROSC rates declined from 20% to 8.6% (P < 0.001) during the pandemic6 and from 35% to 18% in New York City.8 A multivariate analysis confirmed that patients with OHCA during the COVID-19 pandemic were 41% less likely to achieve ROSC (OR, 0.59; 95% CI, 0.50–0.70; P < 0.001) in New York City.8 The other two studies reported a non-statistically significant reduction in ROSC rates during the pandemic9, 23 (Fig. 2A).
Fig. 2.
Forest plot for return of spontaneous circulation (A) and survival to hospital discharge (B). M–H = Mantel–Haenszel, CI = confidence interval.
Survival at hospital discharge was reported in three studies6, 7, 23 and survival with good neurologic outcome only in one.23 In France, patients suffering an OHCA during the COVID-19 pandemic were less likely to survive: rates of survival at hospital discharge declined from 5.4% to 3.1% (P < 0.001).7 A non-statistically significant reduction in survival rate was observed in Italy6 and South Korea23 (Fig. 2B). Patients treated during the COVID-19 pandemic who survived to hospital discharge with a good neurological outcome were 2.9% vs. 5.7% during the non-pandemic period in South Korea (P = 0.09).23
Characteristics of patients
Baseline characteristics of patients with OHCA during the COVID-19 pandemic were similar to those of non-pandemic periods except for New York City where patients with OHCA were older, less likely to be white, and more likely to have comorbidities (hypertension, diabetes, and physical limitations)8 (Supplemental Figs. 1 and 2). OHCAs during the COVID-19 pandemic were more likely to occur at home in Italy (90% during the pandemic vs. 83% in the non-pandemic period; P = 0.005)6 and France (90% vs. 77%; P < 0.001)7 while in the other studies were similar9, 10, 23 (Supplemental Fig. 3). The proportion of patients presenting with non-shockable rhythms (pulseless electrical activity or asystole) during the pandemic increased by 10% in New York City8 and Paris.7 A similar increase was also seen in Italy6 and South Korea,23 even if this difference was not statistically significant (Supplemental Fig. 4).
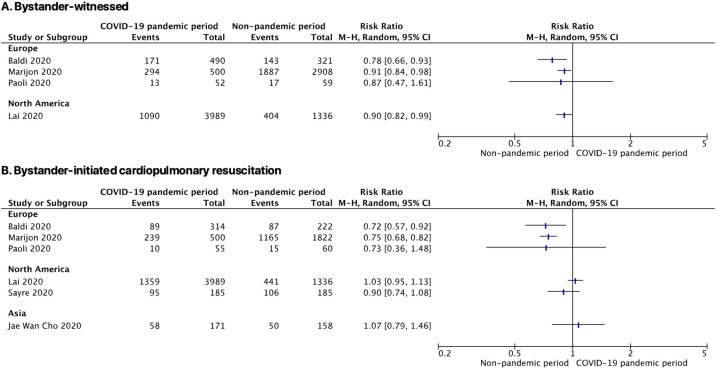
During the pandemic, OHCAs were less likely to be witnessed in Italy,5 France,7 and the USA8 (Fig. 3 A). Similarly, important reductions in bystander-CPR during the pandemic were observed in Italy (35% vs. 45%, P = 0.02)6 and France (48% vs. 64%, P < 0.001)7 while in studies conducted in the USA8, 10 and South Korea23 remained similar (Fig. 3B). Patients with COVID-19 symptoms were less likely to receive bystander-CPR (-19%) when compared with patients not diagnosed or suspected in Italy.6
Fig. 3.
Forest plot for rates of bystander-witnessed out-of-hospital cardiac arrests (A) and bystander-initiated cardiopulmonary resuscitation (B) with subgroup analysis by continent. M–H = Mantel–Haenszel, CI = confidence interval.
SARS-CoV-2 positive patients among OHCAs were 3.9%, 4.3%, 4.8%, and 5.9% in Italy, South Korea, France, and USA, respectively.6, 7, 10, 23 COVID-like symptoms such as fever associated with cough or dyspnoea were documented in 26%, 18%, 8.1%, and 4.8% of patients with OHCA during the pandemic, respectively.6, 7, 10, 23
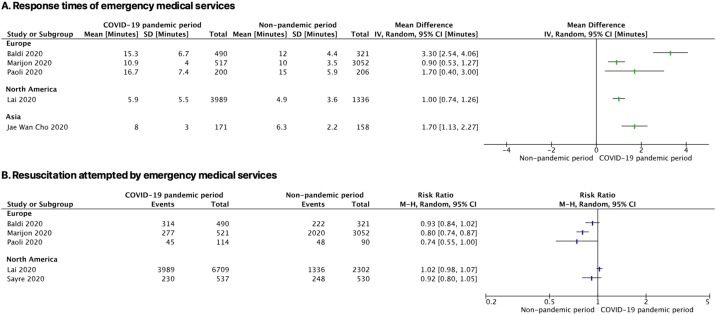
Emergency medical services
Compared to a non-pandemic period, EMS response times to OHCAs were significantly delayed during the COVID-19 pandemic across all studies,6, 7, 8, 9, 23 in particular important delays were observed in Italy (+1 and 3 min.)6, 9 and South Korea (+1 min.)23 (Fig. 4 A). Proportion of cases where pre-hospital resuscitation manoeuvres were initiated by EMS providers was significantly reduced during the pandemic in one study conducted in Italy (39% vs. 53%; P = 0.048) and in France (53% vs. 66%, P < 0.001) while two further studies reported a non-statistically significant reduction in EMS-initiated resuscitations6, 10 (Fig. 4B).
Fig. 4.
Forest plot of the response times of emergency medical services (A) and proportion of patients with out-of-hospital cardiac arrest where resuscitation was attempted by emergency medical services (B). SD = standard deviation, IV = inverse variance, M–H = Mantel–Haenszel, CI = confidence interval.
One study in New York City reported that orotracheal intubation (−28%) and ventilation through bag valve mask (−7,4%) were performed less frequently by EMS during the COVID-19 pandemic. This observation was coupled with an increase (+20%) in the use of supraglottic airway devices.8
Discussion
This is the first systematic review examining the impact of COVID-19 pandemic on incidence, treatment and outcomes of OHCAs compared to a non-pandemic period. The general direction of effect indicates that OHCAs occurring during the COVID-19 pandemic had delayed EMS arrival times, were less likely to present in a shockable rhythm and had lower rates of ROSC and survival to hospital discharge. Identified studies suggest that COVID-19 may have the potential to reduce bystander-witnessed OHCAs and the proportion of cases where bystander-CPR is started, especially in Europe. Also, OHCAs occurred more frequently at home and EMS attempted less frequently resuscitation manoeuvres.
In the early phase of the pandemic, the incidence of OHCA increased by 58% in Lombardy, Italy.5 Such a markedly increase was significantly correlated to the incidence of COVID-19 cases in the first 60 days after the outbreak.6 Similar patterns were reported in New York City8 and in Paris7 where OHCAs doubled and decreased towards non-pandemic levels in parallel with COVID-19 hospital admissions. On the contrary, other studies in Northern Italy9 and in Seattle, USA,10 did not observe an increased incidence and this might be related to the prevalence of COVID-19 in the communities.
Two studies reported that patients presenting with non-shockable rhythms significantly increased during the pandemic.7, 8 Hypoxia is one of the common causes of non-shockable rhythms and it is also characterized by worse outcomes. Therefore, acute hypoxemic respiratory failure in non-hospitalized COVID-19 patients likely occurred, eventually evolving to cardiac arrest and contributing to increase OHCA incidence with worse short-term outcomes. Also, myopericarditis, arrhythmias, and thromboembolism11, 12 are all possible direct complications of COVID-19, leading to cardiac arrest, especially if not timely treated. The proportion of excess OHCAs directly attributable to COVID-19 was 74% in Lombardy, Italy,6 and 33% in Paris, France.7 Indirect effects might be responsible for the remaining cases. Patients with acute coronary syndromes were not timely seeking medical attention,13, 24 mainly due to fear and anxiety caused by the pandemic. Considering that most OHCAs are secondary to myocardial ischemia,14 the decreased hospital admissions for acute coronary syndromes may account for part of excess OHCAs. Lockdown, social distancing, and altered access to healthcare services (hospital overload and suspension of elective activity and inpatient visits) probably contributed.
Delays in EMS response occurred during the pandemic and may be another reason for the increased non-shockable rhythms25 and decreased ROSC and survival.26 Overload of emergency systems and changes in protocols and practices is the most likely cause. In Northern Italy, the culprit intervals were the time needed for call taking, dispatching, and departure.9 These delays can be explained respectively by the need to ask questions about COVID-19 status (tested positive or COVID-like symptoms), the increased dispatchers’ workload due to increased volume of calls received,4, 16 and wearing personal protective equipment (PPE). Interestingly, the time between departure and arrival was significantly lower,9 likely due to road traffic reduction during the lockdown. Another report from Northern Italy found that arrival time was longer only for OHCAs involving patients suspected or diagnosed with COVID-19,6 supporting that wearing PPE may prolong response times.
The community response in OHCA is pivotal for survival and, with the current pandemic, its fragility emerged. Concerns of contracting an infection is often cited as a barrier preventing bystanders from starting CPR. During the early phases of the pandemic, a dangerous effect on bystander-CPR rates was hypothesized.15 In Europe, we observed a decline in bystander-CPR6, 7 that may have affected short-term outcomes. In Italy, a decline in bystander-CPR was observed only among patients diagnosed or suspected of COVID-19.6 It is unclear why the effect was more evident in Europe. One possible explanation is that the pandemic reached European countries first after China and were subjected to an unprecedented situation characterized by fear and uncertain (e.g., Italy experienced a 19% reduction in bystander-CPR6). Also, the increase in non-witnessed OHCAs occurring at home due to lockdown and smart work policies and variations in training and motivation in performing CPR among citizens of different countries might account for these differences. Although the situation might improve with the gradual improvement of the pandemic,27 our findings are alarming as there is risk that all the progresses made in optimising the chain of survival chain are lost.
The risk of contracting the disease during resuscitation manoeuvres depends on the COVID-19 prevalence in OHCAs and the probability of transmission to rescuers. We found a non-negligible prevalence of COVID-19 among OHCAs: 3.9–5.9% of tested patients were SARS-CoV-2 positive and 4.8–26% had suggestive symptoms (fever and cough or dyspnoea).6, 7, 10, 23 As highlighted by the International Liaison Committee on Resuscitation, bystanders are likely to already be exposed to COVID-19 when a cardiac arrest occurs at home if the victim was infected.28 Public campaigns promoting the safety of chest-compression only CPR compared to certain death if resuscitation is not performed might reduce some reluctance among laypeople. Furthermore, smartphone applications to alerts citizens first responders29 were suspended in Paris, France and Switzerland due to the absence of PPE.30, 31
For EMS personnel, the correct use of PPE is of paramount importance to safely perform resuscitation manoeuvres. Despite the use of PPE, fear of contracting the infection may persist. It is important to balance the potential risks of infection and the harm of delaying or withholding a resuscitation. During the pandemic, two studies conducted in Europe reported that EMS providers were less likely to start resuscitation manoeuvres.7, 9 In New York City, there was a marked reduction in endotracheal intubations, coupled with increased use of supraglottic airway devices.8 Such geographically limited results may find an explanation by considering the EMS system of the affected countries, for example in France and Italy, OHCAs are attended by an EMS physician. Another possible explanation is a less optimistic approach limiting resuscitation efforts to OHCAs with higher odds of positive outcomes such as bystander-witnessed, bystander-CPR, and shockable rhythms. All factors that, according to our findings, were reduced during the pandemic. Also, the perceptions that hospital and intensive care units were overwhelmed may have played a role.
Limitations
Our conclusions and overall description of effects are based only on published data in this short period of time. Thus, countries reached later by the pandemic or hit in a different extent were not included due to the absence of data, leading to the underrepresentation of other regions of the world. Moreover, included studies carried a high risk of bias, mainly due to inadequate adjustment for known confounders, and we performed post-hoc analysis for some outcomes (e.g., characteristic of patients and OHCA event). Also, differences between countries in healthcare services, EMS system, education in CPR, and clinical practice should be considered. Aspects with limited data such as long-term effects, definitive cause of OHCA, and characteristics and outcomes in other regions should be addressed in future studies to understand more clearly the relative impact of direct or indirect effects. Also, a more in-depth investigation of the prevalence of COVID-19 among OHCAs could be useful to guide resuscitation guidelines.
Conclusions
The COVID-19 pandemic is responsible not only for deaths among infected individuals, but also for the excess number of OHCAs coupled with lower rates of ROSC and survival to hospital discharge. Although part of this finding may be direct consequences of COVID-19, lockdown, social distancing and reorganization of healthcare systems may had contributed by increasing time of EMS arrival, unwitnessed OHCAs occurring at home, and reducing bystander-CPR. Our findings highlight the need for systems to monitor their performance in order to detect critical variations and take adequate countermeasures. Monitoring through remote and telemedicine systems32 may allow early identification of patients at higher risk of out-of-hospital death and reduce excess mortality during a pandemic. Further research on the topic should focus on long-term effects of COVID-19 pandemic on OHCA and in developing effective public health interventions to prevent such effects in case of recurring pandemics.
Conflict of interest
None.
Authors’ contribution
Design of the study: Scquizzato T, Landoni G, Paoli A, Lembo R, Fominskiy E, Kuzovlev A, Likhvantsev V, Zangrillo A. Data collection: Scquizzato T, Landoni G, Paoli A, Lembo R, Fominskiy E, Kuzovlev A, Likhvantsev V, Zangrillo A. Statistical analysis: Scquizzato T, Lembo R, Landoni G. Manuscript draft and critical review: Scquizzato T, Landoni G, Paoli A, Lembo R, Fominskiy E, Kuzovlev A, Likhvantsev V, Zangrillo A. Administrative support: Landoni G, Zangrillo A.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.resuscitation.2020.10.020.
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- 1.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Worldometer . 2020. COVID-19 coronavirus pandemic. Available from: https://www.worldometers.info/coronavirus/ [Google Scholar]
- 3.Zangrillo A., Beretta L., Silvani P., Colombo S., Scandroglio A.M., Dell’Acqua A., Fominskiy E., Landoni G., Monti G., Azzolini M.L., Monaco F., Oriani A., Belletti A., Sartorelli M., Pallanch O., Saleh O., Sartini C., Nardelli P., Lombardi G., Morselli F., Scquizzato T., Frontera A., Ruggeri A., Scotti R., Assanelli A., Dagna L., Rovere-Querini P., Castagna A., Scarpellini P., Di Napoli D., Ambrosio A., Ciceri F., Tresoldi M. Fast reshaping of intensive care unit facilities in a large metropolitan hospital in Milan, Italy: facing the COVID-19 pandemic emergency. Crit Care Resusc. 2020;22(2):91–94. doi: 10.51893/2020.2.pov1. Epub ahead of print. PMID: 32227819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stella F., Alexopoulos C., Scquizzato T., Zorzi A. Impact of the COVID-19 outbreak on emergency medical system missions and emergency department visits in the Venice area. Eur J Emerg Med. 2020;27:298–300. doi: 10.1097/MEJ.0000000000000724. [DOI] [PubMed] [Google Scholar]
- 5.Baldi E., Sechi G.M., Mare C., et al. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020 doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baldi E., Sechi G.M., Mare C., et al. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020:ehaa508. doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marijon E., Karam N., Jost D., et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30117-1. S2468266720301171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lai P.H., Lancet E.A., Weiden M.D., et al. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York city. Med Hist. 2020;10 doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paoli A., Brischigliaro L., Scquizzato T., Favaretto A., Spagna A. Out-of-hospital cardiac arrest during the COVID-19 pandemic in the Province of Padua, Northeast Italy. Resuscitation. 2020 doi: 10.1016/j.resuscitation.2020.06.031. S0300957220302690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sayre M.R., Barnard L.M., et al. Prevalence of COVID-19 in out-of-hospital cardiac arrest: implications for bystander CPR. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.048951. [DOI] [PubMed] [Google Scholar]
- 11.Bonow R.O., Fonarow G.C., O’Gara P.T., Yancy C.W. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1105. [DOI] [PubMed] [Google Scholar]
- 12.Ciceri F., Beretta L., Scandroglio A.M., Colombo S., Landoni G., Ruggeri A., Peccatori J., D'Angelo A., De Cobelli F., Rovere-Querini P., Tresoldi M., Dagna L., Zangrillo A. Microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS): an atypical acute respiratory distress syndrome working hypothesis. Crit Care Resusc. 2020;22(2):95–97. doi: 10.51893/2020.2.pov2. Epub ahead of print. PMID: 32294809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Filippo O., D’Ascenzo F., Angelini F., et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020 doi: 10.1056/NEJMc2009166. NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Larsen J.M., Ravkilde J. Acute coronary angiography in patients resuscitated from out-of-hospital cardiac arrest – a systematic review and meta-analysis. Resuscitation. 2012;83:1427–1433. doi: 10.1016/j.resuscitation.2012.08.337. [DOI] [PubMed] [Google Scholar]
- 15.Scquizzato T., Olasveengen T.M., Ristagno G., Semeraro F. The other side of novel coronavirus outbreak: fear of performing cardiopulmonary resuscitation. Resuscitation. 2020;150:92–93. doi: 10.1016/j.resuscitation.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Semeraro F., Gamberini L., Tartaglione M., et al. An integrated response to the impact of coronavirus outbreak on the Emergency Medical Services of Emilia Romagna. Resuscitation. 2020;151:1–2. doi: 10.1016/j.resuscitation.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liberati A., Altman D.G., Tetzlaff J., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moher D., Liberati A., Tetzlaff J., Altman D.G., The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scquizzato T., Lembo R., Fominskiy E., Landoni G., Zangrillo A. 2020. Effects of COVID-19 pandemic on out-of-hospital cardiac arrest: a systematic review and meta-analysis PROSPERO. CRD42020195794. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020195794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sterne J.A., Hernán M.A., Reeves B.C., et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wan X., Wang W., Liu J., Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cho J.W., Jung H., Lee M.J., et al. Preparedness of personal protective equipment and implementation of new CPR strategies for patients with out-of-hospital cardiac arrest in the COVID-19 era. Resusc Plus. 2020;3:100015. doi: 10.1016/j.resplu.2020.100015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garcia S., Albaghdadi M.S., Meraj P.M., et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Waalewijn R.A., Nijpels M.A., Tijssen J.G., Koster R.W. Prevention of deterioration of ventricular fibrillation by basic life support during out-of-hospital cardiac arrest. Resuscitation. 2002;54:31–36. doi: 10.1016/s0300-9572(02)00047-3. [DOI] [PubMed] [Google Scholar]
- 26.Vukmir R.B. Survival from prehospital cardiac arrest is critically dependent upon response time. Resuscitation. 2006;69:229–234. doi: 10.1016/j.resuscitation.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 27.Ciceri F., Ruggeri A., Lembo R., Puglisi R., Landoni G., Zangrillo A. COVID-BioB Study Group. Decreased in-hospital mortality in patients with COVID-19 pneumonia. Pathog Glob Health. 2020;114(6):281–282. doi: 10.1080/20477724.2020.1785782. Epub 2020 Jun 25. PMID: 32584660; PMCID: PMC7480486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nolan J.P., Monsieurs K.G., Bossaert L., et al. European resuscitation council COVID-19 guidelines executive summary. Resuscitation. 2020 doi: 10.1016/j.resuscitation.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scquizzato T., Pallanch O., Belletti A., et al. Enhancing citizens response to out-of-hospital cardiac arrest: a systematic review of mobile-phone systems to alert citizens as first responders. Resuscitation. 2020;152:16–25. doi: 10.1016/j.resuscitation.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jost D., Derkenne C., Kedzierewicz R., et al. The need to adapt the rescue chain for out-of-hospital cardiac arrest during the COVID-19 Pandemic: experience from the Paris fire brigade basic life support and advanced life support teams. Resuscitation. 2020 doi: 10.1016/j.resuscitation.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Momentum – Sospensione allarmi DAE Informazione Coronavirus; 2020. Available from: https://fr.momentum.dos-group.com/news/show/110/sospensione-allarmi-dae (accessed 05.07.20).
- 32.Semeraro F., Scquizzato T., Scapigliati A., et al. New Early Warning Score: off-label approach for Covid-19 outbreak patient deterioration in the community. Resuscitation. 2020;151:24–25. doi: 10.1016/j.resuscitation.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.