Abstract
As our understanding of the complications of coronavirus disease-2019 (COVID-19) evolve, subclinical cardiac pathology such as myocarditis, pericarditis, and right ventricular dysfunction in the absence of significant clinical symptoms represents a concern. The potential implications of these findings in athletes are significant given the concern that exercise, during the acute phase of viral myocarditis, may exacerbate myocardial injury and precipitate malignant ventricular arrhythmias. Such concerns have led to the development and publication of expert consensus documents aimed at providing guidance for the evaluation of athletes after contracting COVID-19 in order to permit safe return to play. Cardiac imaging is at the center of these evaluations. This review seeks to evaluate the current evidence regarding COVID-19–associated cardiovascular disease and how multimodality imaging may be useful in the screening and clinical evaluation of athletes with suspected cardiovascular complications of infection. Guidance is provided with diagnostic “red flags” that raise the suspicion of pathology. Specific emphasis is placed on the unique challenges posed in distinguishing athletic cardiac remodeling from subclinical cardiac disease. The strengths and limitations of different imaging modalities are discussed and an approach to return to play decision making for athletes post–COVID-19, as informed by multimodality imaging, is provided.
Key Words: athlete, COVID-19, multimodality imaging, myocardial injury, myocarditis, return to play
Abbreviations and Acronyms: CMR, cardiac magnetic resonance; CTA, computed tomography angiography; cTn, cardiac troponin; CV, cardiovascular; COVID-2019, coronavirus disease-2019; ECG, electrocardiogram; ECV, extracellular volume; EF, ejection fraction; EICR, exercise-induced cardiac remodeling; GLS, global longitudinal strain; hs-cTn, high-sensitivity cardiac troponin; LGE, late gadolinium enhancement; LV, left ventricle/ventricular; POCUS, point-of-care ultrasound; PET, positron emission tomography; RTP, return to play; RV, right ventricle/ventricular; TTE, transthoracic echocardiography
Central Illustration
As the global coronavirus disease-2019 (COVID-19) pandemic progresses there has been increased concern for potential long-term cardiopulmonary complications in athletes. Recognizing the potential for cardiac morbidity, in May 2020, the American College of Cardiology Sports and Exercise Cardiology Council and others published return-to-play (RTP) recommendations for previously infected athletes (1, 2, 3). Lately, as schools, colleges, and professional organizations seek to restart competitive sports, there has been renewed focus on the potential cardiac risk to recovered athletes. This has been due, in part, to the public acknowledgment of COVID-19–induced cardiac injury in some high-profile athletes and newer data suggesting higher than expected incidences of myocardial inflammation in recovered nonathletic and athletic populations (4,5).
Myocardial injury, defined as a cardiac troponin (cTn) level greater than the 99th percentile upper reference limit, has been reported frequently in hospitalized patients with COVID-19 and is associated with progressive heart failure, arrhythmia, and death (6). There are multiple mechanisms of myocardial injury including direct myocardial invasion by the virus resulting in myocarditis (7,8). Prior to the COVID-19 pandemic, myocarditis accounted for 7% to 20% of sudden cardiac death in young athletes (9,10). At present, data on the prevalence of myocardial injury, pericarditis, or myocarditis in athletes recovering from COVID-19 are limited to very small observational case series (5,11,12).
Athletes recovering from COVID-19 present some unique challenges. There is concern that exercise during the acute phase of viral myocarditis may exacerbate or prolong the illness or serve as a trigger for serious arrhythmias (13, 14, 15). Furthermore, the diagnosis of acute myocarditis or subsequent pathological remodeling can be difficult to differentiate from the physiological exercise-induced cardiac remodeling (EICR) commonly seen as part of the healthy “athletes’ heart” phenotype. This challenge requires specific knowledge of contemporary multimodality imaging in the athletic context.
The aims of this expert consensus document are to:
-
•
Define the potential latent cardiac complications of COVID-19 infection and how these are relevant for the athlete.
-
•
Provide guidance on how to differentiate potential COVID-19–related cardiac complications from athletes’ heart.
-
•
Identify “red flags” in the clinical evaluation of athletes that require further testing and provide guidance on appropriate downstream imaging.
-
•
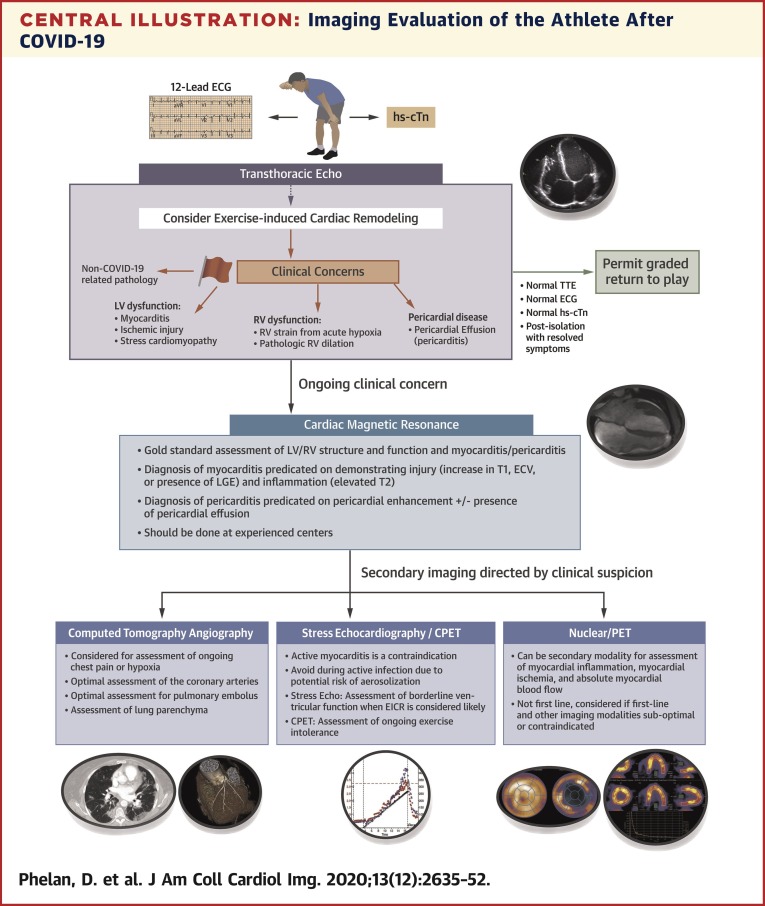
Define the utility and limitations in the various imaging modalities to assess for COVID-19–related cardiac complications (Central Illustration ).
Central Illustration.
Imaging Evaluation of the Athlete After COVID-19
Considerations and proposed cardiac imaging algorithm for the athlete after coronavirus disease-2019 (COVID-19). CPET = cardiopulmonary test; ECG = electrocardiogram; ECV = extracellular volume; EICR = exercise-induced cardiac remodeling; hs-cTn = high-sensitivity cardiac troponin; LGE = late gadolinium enhancement; LV = left ventricle; PET = positron emission tomography; RV = right ventricle; TTE = transthoracic echocardiography.
COVID-19–Related Myocardial Injury
Transmitted primarily via droplets but also probably aerosols, severe acute respiratory syndrome coronavirus 2 virus enters the body via human angiotensin-converting enzyme 2, a receptor expressed not only in the lungs but also in the myocardium and throughout the cardiovascular (CV) system (7,8). Up to one-quarter of hospitalized patients with COVID-19 exhibit myocardial injury with some developing significant cardiac complications, including biventricular heart failure, arrhythmias, and occasionally cardiogenic shock and death (16,17). A multifactorial mechanism is likely, including cytokine-mediated cardiomyopathy, endothelial inflammation and microemboli, acute coronary events, pulmonary emboli, right ventricular (RV) strain, and myocarditis (7,8). Recent data from Linder et al. (18) demonstrating severe acute respiratory syndrome coronavirus 2 viral presence in the myocardium (24 of 39 autopsy cases, 61.5%) with evidence of active viral replication suggest that direct viral invasion may be more common than previously appreciated. These findings have primarily been derived from studying hospitalized patients. Their applicability to younger populations, including athletes, has not been elucidated. Despite the fact that hospitalization for acute infection is uncommon in young, healthy individuals, there is concern that significant subclinical myocardial injury may be prevalent and that this may manifest as protracted malaise or, more concerningly, may represent a substrate for arrhythmias and sudden death (4,5,19). These concerns have guided the CV RTP recommendations in athletes who have recovered from COVID-19 (1,2,20).
Current Screening Strategies in Athletes After COVID-19
Pre-participation physical evaluation is routinely practiced in many places throughout the world, but its extended application to the evaluation of the athlete post–COVID-19 is a new challenge. Currently, there are very limited available data on the prevalence of COVID-19 cardiac involvement in athletes, and on the diagnostic performance of the recommended testing modalities included in consensus screening guidelines. Given that the efficacy of a screening program hinges on these factors, it is expected that screening recommendations will continue to evolve in parallel with available data on COVID-19 illness in athletes.
Until such data are available, general principles from the implementation of the pre-pandemic pre-participation physical evaluation serve a foundation for current recommendations. First, a focused medical history and examination are a commonsense launching point. Many athletes may be asymptomatic or experience nonspecific symptoms that they do not recognize as being associated with COVID-19 and will remain entirely asymptomatic at the time of RTP evaluation. Other athletes may have nonspecific malaise, reduced exercise tolerance, recurrent chest pain, dyspnea, or palpitations at the time of illness, which may persist into convalescence. The evaluation of athletes with persistent symptoms after recovery from acute COVID-19 will be guided by the nature of the symptoms, whereas the evaluation of the asymptomatic athlete will be oriented around screening for subclinical pathology.
Second, data from the pre-pandemic pre-participation physical evaluation suggest the inclusion of additional testing above the most basic tests will invariably improve the sensitivity of screening. However, the addition of more layers to screening in athletes post–COVID-19, specifically the widespread use of more advanced imaging, may come at the cost of reduced specificity for identification of clinically meaningful pathology, particularly if there is a paucity of experience in identifying what constitutes normal, adaptive cardiac remodeling in an athlete. A more comprehensive strategy inclusive of advanced imaging modalities, such as cardiac magnetic resonance (CMR) imaging, also calls into question the practical issues of health care expenditures, qualified technical expertise, and unproven clinical efficacy.
Although there have been some variations and updates in the published RTP CV screening recommendations, a moderately conservative approach that accounts for these practical issues has generally been recommended (1, 2, 3,20,21) with the combination of an electrocardiogram (ECG), cardiac biomarker assessment, and imaging with transthoracic echocardiography (TTE) generally accepted as a reasonable risk stratification RTP strategy in certain athletes depending on their perceived risk (1,20). This testing strategy also aligns with published recommendations for testing in the evaluation of suspected myocarditis (22). Because available health care resources and expenditures must also be appreciated, RTP without CV risk stratification in clearly identified, low-risk cases of COVID-19 may be reasonable, so long as clinical observation is easily accessible and physical training resumes in a progressive and deliberate manner.
Key points:
-
•
Evaluation of the athlete with symptoms should follow a targeted approach based on the presence and nature of symptoms.
-
•
In asymptomatic athletes and mildly symptomatic athletes’ recent recommendations suggest that cardiovascular testing prior to RTP may not be necessary.
-
•
The role of screening athletes is evolving. Until it has been established that complications of COVID-19 are rare in athletes who experience prolonged or more than mild symptoms, current recommendations suggest a prudent exclusion of complications with a combination of ECG, biomarkers and echocardiography.
Practical Issues for the Screening of Athletes After Recovery From COVID-19
Considerations for use of the 12-lead ECG after recovery from COVID-19
The 12-lead ECG is the simplest diagnostic tool in cardiology, and it is effective in detecting conditions linked with sudden cardiac death. Described abnormalities related to myocarditis include frequent or multiform premature ventricular beats or arrhythmias, ST- and T-wave changes, left bundle branch block, and atrioventricular block (23). However, the sensitivity for detecting myopericarditis with these changes is as low as 47% (23). Furthermore, over 70% of athletes have repolarization anomalies characterized by J-point elevation, ascending concave ST segments in the inferior or lateral leads, and tall T waves that may be confused with myopericarditis (Figure 1 ). The specificity of ECG changes in diagnosing myocarditis has not been defined but might be expected to be low. In such circumstances, comparison with previous ECGs is invaluable to minimize the need for conducting unnecessary investigations.
Figure 1.
Challenges With ECG Screening in Athletes Post–COVID-19
Electrocardiograms (ECGs) performed on 2 athletes highlighting challenges with differentiating normal changes associated with athletic training and pathology. (A) Normal healthy endurance athlete’s ECG showing diffuse ST-segment elevation because of early repolarization (blue arrows). (B) An ECG from a 23-year-old soccer player presenting with positional pleuritic chest pain, elevated high-sensitivity troponin (>5,000 ng/l) with confirmed myopericarditis on cardiac magnetic resonance; the ECG also shows diffuse ST-segment elevation (blue arrows) and also subtle PR depression (red arrow). COVID-19 = coronavirus disease-2019.
Considerations for troponin testing after recovery from COVID-19
cTn testing in contemporary clinical practice has evolved with substantial improvements in assay sensitivity and precision. COVID-19 RTP considerations have recommended assessment of the biochemical presence of myocardial injury with quantification of high-sensitivity cTn (hs-cTn) to assess for subclinical myocardial injury (1,3,21). Where hs-cTn is not available, earlier-generation troponin assays can be considered as alternatives.
In competitive athletics, the impact of prolonged strenuous exercise on the release of cTns must be considered (24). The kinetics of troponin release in the setting of strenuous exercise differentiates from pathologicAL troponin release related to myocardial injury and is characterized by a peak and resolution to baseline by ∼24 to 48 h after strenuous exercise (25,26). It is therefore recommended that any RTP assessment inclusive of hs-cTn not be performed within ∼24 to 48 h of exercise.
Additional uncertainties, including a lack of established hs-cTn reference ranges for athletes should be acknowledged. Furthermore, the prognostic significance of elevated hs-cTn less than the 99th percentile has been demonstrated, which emphasizes that “normal” values may not exclude the presence of subclinical myocardial injury (6,27). It therefore remains prudent that biomarker assessment must be considered in combination with additional criteria obtained as part of the risk stratification process.
Considerations for echocardiography after recovery from COVID-19
As hs-cTn and ECG changes may normalize after the athlete has clinically recovered from COVID-19 despite myocardial injury during the acute illness, inclusion of cardiac imaging using TTE for athletes who had symptoms during the acute phase of COVID-19 has been suggested in RTP strategies (1,2,20,21). TTE is a logical primary imaging modality due to its widespread availability and its excellent diagnostic capabilities. The routine use of echocardiography in athletes returning to play after COVID-19 may be challenged by cost and access considerations, especially in regions where the disease has been prevalent and the number of athletes requiring evaluation is large.
Potential role of point-of-care ultrasound
Point-of-care ultrasound (POCUS) has been found useful in the assessment of patients acutely ill with COVID-19, as it conserves personal protective equipment and reduces the risk of contagion (28). It is generally aimed at triaging patients with severe abnormalities, rather than diagnosing subtle abnormalities. Current POCUS technology cannot assess diastolic function or strain, and imaging assessment of the RV can be challenging. It is the opinion of this writing group that POCUS should not replace TTE imaging in the evaluation of recovered athletes.
Potential risks of screening athletes
When designing a program that is meant for widespread screening, especially in asymptomatic individuals, it is important to appreciate the potential costs and harms of testing. These can include financial costs as well as strain on resource-limited health care systems, particularly in regions with higher COVID-19 prevalence. There are also potential harms to the athlete from screening. Extensive use of advanced imaging will predictably discover “gray-zone” cases in which differentiating between expected athletic cardiac remodeling and mild pathology is difficult. Such cases test reasonable management and treatment decisions, and the result may be exclusion from sports participation on the basis of minor deviations from “normal.” Although multimodality clinical assessments may lead to appropriate outcomes in difficult cases, it is also essential for practitioners to appreciate the potential deleterious effects of undue, unnecessary, and excessive testing of athletes. It is important to consider that a screening program that might be the ideal fit for one group (e.g., a professional league) may be quite poorly designed for others (e.g., club-level sport, masters athletes). The optimal screening algorithm will take consideration of the specific risk of the population to be screened, local expertise, and available resources.
Key points:
-
•
ECG is a useful adjunct in the RTP algorithm, but in isolation it lacks sensitivity for myocarditis.
-
•
Troponin assays lack standardization in athletes but are recommended as part of the RTP risk stratification algorithm.
-
•
Echocardiographic techniques are currently considered first line in the imaging of an athlete post–COVID-19.
-
•
Remain cautious of unnecessary testing and appreciate that screening protocols may vary according to athletic discipline and setting.
Imaging Athletes’ Hearts and COVID-19 Considerations
Intensive exercise is associated with the generation of a 5- to 6-fold increase in cardiac output that is achieved via augmentation of stroke volume through a combination of increased venous return to the ventricles, rapid ventricular filling, and a marked reduction in systemic vascular resistance, plus an increased heart rate. Exercise that requires a prolonged and sustained increase in cardiac output necessitates a physiological increase in cardiac dimensions. The magnitude of EICR is governed by age, sex, size, ethnicity, and the intensity and type of sport (29). Endurance athletes reveal the largest cardiac dimensions, whereas Black male athletes may exhibit the greatest increase in left ventricular (LV) wall thickness (29). Adolescent athletes (30) and female athletes (31) generally exhibit less remodeling, although marked athletic changes may still be encountered. Differentiating pathology from EICR can be very challenging, particularly in the persistently symptomatic athlete post-COVID-19 (Figure 2 ).
Figure 2.
Challenges in Differentiating Exercise-Induced Cardiac Remodeling and Myocardial Injury Secondary to COVID-19: The Utility of Multimodality Imaging
A 23-year-old male elite rower presented with 3 months of exercise intolerance following a mild coronavirus disease-2019 (COVID-19) illness (polymerase chain reaction confirmed). His peak oxygen consumption had reduced by approximately 20 ml/min/kg but in the setting of complete detraining. The possibility of myocardial dysfunction secondary to COVID-19 myocarditis was considered. His high-sensitivity troponin was normal. Echocardiography revealed symmetrical dilation of all 4 cardiac chambers, but low-normal function of the left ventricle (LV). (A) Global longitudinal strain was –16% and (B) LV ejection fraction was 52%. (C) Right ventricular strain was synchronous and normal (–27%) and (D) RV fractional area change of 48% was also normal. The low-normal LV functional measures are common in endurance athletes, but given the persisting clinical uncertainty, a cardiac magnetic resonance scan was performed. (E) There was no enhancement post–gadolinium contrast administration and both (F) T1 and (G) T2 mapping values were normal. The rower was reassured and encouraged to make a graduated return to training and competition.
Echocardiography
Non–COVID-19 myocarditis has been reported to mimic dilated, hypertrophic (owing to edema), and restrictive cardiomyopathies and can present with global or regional LV dysfunction or with diastolic dysfunction with preserved LV ejection fraction (LVEF) (32). However, a clear understanding of the spectrum of echocardiographic findings in the context of COVID-19 is still evolving. Systematic studies describing the frequency of COVID-19–related abnormalities are available but are generally reported in severely ill and hospitalized patients. In a cohort of 100 patients with COVID-19, Szekely et al. (33) reported not only that LV systolic function was more often preserved, but also that LV diastolic dysfunction and impairments of RV systolic function were common. Importantly, in patients with clinical deterioration, acute RV dysfunction, with or without deep venous thrombosis, was the most common functional abnormality present. Inciardi et al. (34) similarly demonstrated that LVEF did not differ between COVID-19 patients with and those without underlying cardiac disease. Data from Churchill et al. (35) further affirmed that LVEF was normal or hyperdynamic in most patients with COVID-19. Diminished RV performance appears to be the most common echocardiographic finding in patients with COVID-19 (36). Advanced echocardiographic measures of RV function, including RV longitudinal strain, predict mortality in patients with COVID-19. Li et al. (37) analyzed 150 consecutive patients with COVID-19 and found that lower RV longitudinal strain most accurately predicted a higher risk for mortality. Currently, there are no studies of TTE findings in athletes recovering from COVID-19. However, with TTE generally accepted and utilized in current COVID-19 RTP screening protocols (1), we anticipate data describing TTE findings in athletes recovered from COVID-19 to be forthcoming. At present, specific recommendations for the assessment of the LV, RV, and pericardium are described subsequently.
Recommendations for echocardiographic assessment of the athlete’s left heart
Increases in LV wall thickness associated with COVID myocarditis should be distinguished from athletes in whom such changes are due to athletic conditioning. It is uncommon for young White athletes to exhibit hypertrophy >12 mm, and those few (<2%) that do are mostly highly trained male endurance athletes whose sport requires a mix of high-endurance and strength components (38). A significantly larger proportion of Black male athletes, particularly those participating in explosive sports, may demonstrate greater hypertrophy but it rarely exceeds 15 mm (39). Changes in LV cavity dimensions and volumes are more significant, with 14% of male athletes demonstrating LV cavity dimensions between 60 and 70 mm (38). In a small proportion of ostensibly healthy male elite endurance athletes, markedly enlarged LV volumes and mildly reduced EFs have been observed (40). This is particularly relevant for post-COVID assessments when similar changes would raise concern of active or recovering myocarditis (Figure 2). Other than elite endurance athletes, it is rare to see a reduction in EF (29,41) such that an EF <50% should raise the possibility of pathology and trigger further evaluation. It may also be useful to use exercise as a means of discrimination in ambiguous cases after active myocarditis has been ruled out by other means. Healthy athletes demonstrate good myocardial contractile reserve, as evidenced by an increase in LVEF of at least 10% following exercise or achieving a maximal LVEF >63% (42,43). Similar principles apply for female athletes. Although less extensively studied, there is evidence that EICR is slightly less and that female athletes rarely exhibit an LV cavity >60 mm (31,38). However, impressive cardiac dilation can still be observed in some highly trained women.
Assessment of the LV should include all standard views of the LV to assess size, EF, and wall thickness according to American Society of Echocardiography guidelines (44). Table 1 describes expected TTE findings in an athlete and “red flags”—findings that are not attributable to EICR and that may warrant further testing. If 2 or more contiguous segments cannot be adequately visualized, ultrasound enhancing agents should be used (44). As mentioned, repetitive volume challenges from endurance training results in a relatively balanced dilation of all 4 chambers. Isolated LV enlargement is not a characteristic feature of EICR. Regional wall motion abnormalities of the LV are always abnormal and should mandate further testing. As mentioned previously, with the exception of some elite endurance athletes, a normal EF can be expected despite LV enlargement (29,41).
Table 1.
Comparison of Typical Athletic Remodeling Versus “Red Flag” Findings That Increase Suspicion for COVID-19–Related Myocardial Disease on Echocardiography
| Athletic Remodeling∗ | “Red Flags” That Increase Suspicion for Pathology |
|---|---|
| LV | |
| Symmetric dilation of all 4 cardiac chambers | Disproportionate or severe LV dilation (LVEDD >70 mm in men and >60 mm in women) |
| No regional structural or functional wall motion abnormalities | Segmental wall motion abnormality |
| Symmetric wall thickening <12 mm (<15 mm in black male athletes) | Asymmetric regional wall thickening |
| Normal or low-normal EF | LVEF <50% |
| Normal or supranormal tissue-Doppler myocardial velocities | Low tissue-Doppler e′ myocardial velocities for age or raised E/e′ |
| Augmentation of low-normal LVEF ≥10% with exercise | Failure to augment low-normal LVEF with exercise |
| Global longitudinal strain ranges from –16% to –22%. | Abnormal global longitudinal strain† |
| Compliant LA with normal reservoir function | Increased atrial stiffness |
| RV | |
| Similar degree of RV dilation to that of the LV | RV-to-LV basal end-diastolic diameter ratio (apical view) >1.0 |
| Usually no more than moderate dilation | RV end-diastolic area >15 cm2/m2 or RV end-diastolic volumes >260 ml |
| Coordinated and consistent regional wall motion and deformation | Segmental wall motion abnormalities |
| Normal or low-normal systolic function | Fractional area change <35% or 3-dimensional RVEF <44% |
| Good augmentation of RV function with exercise | Reduced RV augmentation with exercise (RV fractional area change or strain) |
| Coordinated RV contraction | RV mechanical dyssynchrony >40 ms |
COVID-19 = coronavirus disease 2019; LA = left atrium; LV = left ventricle/ventricular; LVEDD = left ventricular end-diastolic diameter; LVEF = left ventricular ejection fraction; RV = right ventricle/ventricular; RVEF = right ventricular ejection fraction.
See text regarding how athletic remodeling may vary based on sport, gender, ethnicity, and body size.
Ensure good image quality with appropriate tracking. Normal ranges may vary—see text for further details.
Thorough assessment of diastolic function is mandatory. Normal or “supranormal” diastolic function is the rule, especially among endurance athletes characterized by rapid mitral annular tissue Doppler velocities and S < D in the pulmonary vein flow due to robust lusitropy (29). Tissue Doppler data should be interpreted in the context of the age of the athletes, their medical history, and their sport type and compared with published normative data (45).
Strain imaging is evolving to become part of the standard TTE and has proven utility in the detection of LV systolic dysfunction in the context of a normal EF (46). Global longitudinal strain (GLS) has been proven to be a robust prognostic marker in a multitude of disease processes. A study by Janus et al. (47) reported on 35 patients with COVID-19 and highlighted that worsening GLS was associated with adverse outcomes. In the context of the current data in COVID-19 reporting that most patients with documented myocardial injury have normal LVEF, GLS may be a robust tool in identifying subclinical LV dysfunction. The presence of a normal global LV longitudinal strain (GLS >17%) is therefore reassuring. Normal GLS values in athletes are not well defined, ranging from –16% to –22% in published data (29). GLS is dependent on multiple factors, including image quality, and an isolated abnormal result should result in reviewing the primary data to ensure accuracy and integration of the echocardiographic data before proceeding with additional confirmatory tests. A value worse than –16% should raise concern for myocardial pathology.
Assessment of atrial function may help differentiate athletes’ heart from pathology, although again there are important overlapping features (48). In general, exercise-induced preload results in augmented reservoir and conduit function, while left atrial active emptying tends to be lower in athletes manifested by a small A-wave across the mitral inflow (49). In athletes, reduced reservoir function is unusual and pathology should be considered.
Key points:
-
•
Myocarditis can cause regional wall motion abnormalities, global LV systolic dysfunction, isolated diastolic dysfunction, and regional increased wall thickness due to edema.
-
•
Balanced 4-chamber enlargement and symmetrical (usually eccentric) hypertrophy are common EICR findings in endurance and mixed-sport athletes.
-
•
Ejection fraction is usually normal in athletes—elite endurance athletes rarely express a mild reduction in EF at rest, but this is associated with normal diastolic function and normal augmentation of EF and supranormal functional capacity with exercise.
-
•
Reduced LV systolic function or the presence of diastolic dysfunction is suspicious for occult myocardial involvement.
Recommendations for echocardiographic assessment of the athlete’s right heart
Although there is insufficient evidence to guide strict recommendations on post-COVID RV assessment in athletes, we believe that this deserves specific comment for 2 reasons: 1) RV dysfunction is one of the more prevalent abnormalities described in COVID-19 patients; and 2) RV assessment is difficult in athletes and there is potential for physiological changes to be confused with pathology.
RV dysfunction is an expected complication in COVID-19 heart disease (36) due to the fact that pulmonary and pulmonary-vascular complications dominate the clinical picture of acute COVID-19 illness. Any resulting increase in pulmonary vascular resistance can promote RV dysfunction. The RV is more load dependent than the LV; thus, assessment of pulmonary artery pressures is of great importance, particularly in COVID-19 patients.
The assessment of RV structure and function in athletes is complex, particularly in the endurance athlete. RV dilation combined with low-normal or mildly abnormal measures of RV systolic function are common among healthy endurance athletes (50,51). Thus, the confident diagnosis of pathology often requires a series of complementary abnormal results, identification of regional abnormalities, or association with strong clinical suspicion.
Qualitative assessment should include an assessment of RV size and wall motion in parasternal short- and long-axis views as well as in apical views. This is an important start to RV assessment but should not be relied on in isolation.
Reference ranges for quantification need to be tailored to the degree of athletic conditioning, ethnicity, and sex. Unfortunately, reference ranges are not established for all combinations. An alternate strategy is to reference the RV to LV size. This assumes symmetrical remodeling, a finding that has been repeatedly demonstrated to hold true. Using a ratio of basal end-diastolic diameters, the RV-to-LV internal diameter ratio has been demonstrated to be slightly greater in athletes (50) (consistent with the finding of greater RV-to-LV volume ratios), but because of the lunar shape of the RV, the linear dimensions are typically less than the LV. For the normal athlete, the RV-to-LV end-diastolic diameter is typically 0.8 ± 0.1 and 0.6 ± 0.1 in the long- and short-axis views, respectively (24,50,51). See Table 1 for suggested red flags to be considered in clinical decision making.
RV areas should be carefully measured with rotation of the probe to maximize RV area in an apical long-axis view. Measures of RV end-diastolic area, RV end-systolic area, and calculation of fractional area change [(RV end-diastolic area − RV end-systolic area) / RV end-diastolic area] are simple and useful. These measures should be considered in the context of expected athletic remodeling; greater RV areas and slightly reduced RV fractional area change are common. RV volumes can be performed using 3-dimensional echocardiography or, more accurately, using CMR. Using either modality, it is again useful to consider the RV-to-LV ratio to “normalize” for athletic remodeling. Consistently, RV-to-LV volume ratios of 1.1 ± 0.1 have been documented.
Tricuspid annular plane systolic excursion and tricuspid annular systolic velocities (RVs) are commonly used measures for estimation of RV function, although findings regarding accuracy are inconsistent. In athletes, there are several additional factors that also challenge these measures, particularly related to the curvature of the RV free wall and resulting difficulties in alignment of the RV free wall with the ultrasound beam. Two-dimensional deformation measured as longitudinal strain addresses some of these limitations and likely represents a better measure of longitudinal deformation (strain) and deformation rate (strain rate).
Substantial challenges in recognizing subtle pathology remain. In cases in which uncertainty persists, CMR is an appropriate next step to assist with more accurate quantification of volumes, assessment of regional abnormalities, and tissue characterization. Although assessment of enhancement of the thin RV wall is not a reliable estimation, abnormalities in the LV myocardium can assist in the clinical and risk assessment. A complementary strategy is to employ advanced echocardiographic techniques, such as exercise imaging. Given the disproportionate increase in RV work during exercise (relative to LV work), exercise testing may elucidate subtle abnormalities but should only be done after active myocarditis has been ruled out (52). An additional technique of novel interest is “mechanical desynchrony,” referring to increased temporal spread of peak deformation. In athletic studies, this has been applied not only to the LV, but also more recently to the RV (53).
Key points:
-
•
RV pathology is frequently seen after severe COVID-19 infection.
-
•
The RV is load sensitive and EICR can be challenging to differentiate from pathology.
-
•
A combination of qualitative and quantitative assessment should be employed in the assessment of the RV.
-
•
In athletes, the ratio of RV-to-LV end-diastolic diameter (apical view) is typically 0.8 ± 0.1 and it is uncommon to exceed 1.0.
-
•
CMR is a useful adjunct to ensure accurate RV characterization beyond TTE assessment.
Recommendations for the assessment of the pericardium
Pericardial disease, including acute pericarditis and pericardial effusion, appear to be common manifestations of COVID-19 cardiac injury (4,12). Puntmann et al. (4) recently reported that >33% of patients convalescing from COVID-19 had isolated pericardial enhancement either with or without underlying myocarditis. In a study by Brito et al. (12), 41% of athletes who had recovered from COVID-19 who underwent screening CMR had evidence of pericardial hyperenhancement with associated pericardial effusions. However, in the absence of residual symptoms and normal biomarkers of inflammation, the clinical implications of these findings remain unresolved. Characteristic symptoms or ECG changes should raise suspicion of pericarditis and trigger further testing (Figure 3 ).
Figure 3.
Pericardial Complications of COVID-19 in an Athlete
A 24-year-old elite female basketball player, coronavirus disease 2019 (COVID-19) polymerase chain reaction–positive 4 weeks prior, presented for cardiovascular risk stratification. Previous symptoms included temperature to 100.1°F, chills, and positional chest tightness, now all resolved for 21+ days. Current vital signs were stable and a 12-lead electrocardiogram showed normal sinus rhythm without ST-segment deviations. (A) Transthoracic echocardiography parasternal basal short-axis view (arrow; small localized posterior effusion); (B) cardiac magnetic resonance short-axis noncontrast steady-state free precession visualizing effusion (arrow); (C) cardiac magnetic resonance short-axis phase-sensitive inversion recovery late gadolinium enhancement demonstrating localized, probably healing and subacute pericarditis (arrow).
TTE is the first-line imaging modality for the evaluation for pericardial pathology, although normal TTE findings do not exclude the presence of acute pericarditis without significant effusion (54). The echocardiogram should include a complete evaluation of the pericardium. Effusions are usually circumferential but may be localized.
Key points:
-
•
COVID-19 pathological cardiac sequalae include pericarditis with or without pericardial effusion.
-
•
TTE is the first-line imaging in most cases. CMR can further delineate pericardial enhancement or coexisting myocarditis.
CMR Imaging
CMR represents an important diagnostic tool in the work-up of myocarditis associated with COVID-19. Recently, CMR-specific investigations have demonstrated an alarming prevalence of cardiac involvement in patients who have recovered from COVID-19. In a German cohort of 100 middle-aged patients recovered from COVID-19 (median 71 days post-diagnosis), Puntmann et al. (4) reported that 78% of the population had evidence of myocardial injury on CMR. The most common abnormal findings were elevated native T1 (73%) and elevated T2 signals (60%). Nearly one-third had late gadolinium enhancement (LGE). There were relatively mild decreases in LVEF and RVEF in comparison with healthy control subjects. There was a broad spectrum of acute COVID-19 illness severity in this study: 18% were asymptomatic, ∼50% recovered at home with mild to moderate symptoms, and one-third required hospitalization. Inaccurate data analysis metrics and inconsistencies of the reported data that led to the subsequent publication of a revised manuscript are noteworthy limitations of this study. A retrospective study from Wuhan, China, of 26 patients recovering from moderate-to-severe COVID-19 pneumonia (median 47 days post-diagnosis) demonstrated a high prevalence of globally increased T1, T2, and extracellular volume (ECV), and 31% had small LGE in a pattern consistent with myocarditis (55). RV systolic function was reduced in comparison with healthy control subjects, with no reduction in LV systolic function.
Several recently published studies evaluated cardiac abnormalities by CMR in athletes recovered from COVID-19 infection. CMR imaging in 26 athletes (mean 19 years of age) who were asymptomatic or mildly symptomatic with normal ECG, hs-cTn, and echocardiogram determined that 46% had LGE and 15% had CMR evidence of myocarditis (5). Although these results appear alarming, significant limitations should be noted. This investigation was published as a research letter with limited CMR data analysis details provided. Image interpretation bias is likely in this study given the absence of a control group that may limit accuracy of distinguishing small regions of scarring from artifact on LGE imaging. A second observational case series of 46 collegiate athletes (mean 19 years of age) who had recovered from COVID-19 infection included screening CMR (12). In contrast to the prior study, 41% of athletes were reported to have pericardial hyperenhancement, while only 1 athlete was determined to have myocardial LGE and none had abnormal native T2 values. In contrast to the prior 2 studies of athletes recovered from COVID-19 infection, a CMR investigation of 12 Hungarian athletes (median 23 years of age) demonstrated no evidence of myocardial injury or inflammation (11). The compilation of current data underscores the need for more robust, multicenter data, inclusion of appropriate control subjects, and the blinded assessments of reproducibility between observers and between imaging centers. Our understanding of COVID-19–associated cardiac disease continues to evolve, and these studies raise several unanswered critical questions:
-
1.
What are the clinical predictors of myocardial injury on CMR?
-
2.
What are the temporal characteristics of CMR markers of COVID-19–induced myocardial injury and inflammation?
-
3.
Are similar levels of myocardial injury and inflammation observed in patients recovering from influenza, enteroviruses, or other respiratory viral illnesses?
-
4.
Are CMR abnormalities observed in recovered COVID-19 patients associated with long-term adverse outcomes?
-
5.
Are there factors other than differences in study design and patient populations that can explain the marked variance in prevalence of myocardial injury and inflammation on CMR imaging in the studies published thus far?
Suggested indications to consider CMR in athletes post COVID-19 are presented in Table 2 .
Table 2.
Indications: Consider Addition of CMR to the Evaluation of Athletes Post–COVID-19
|
|
|
|
|
|
|
|
|
CMR = cardiac magnetic resonance; ECG = electrocardiogram; TTE = transthoracic echocardiogram; other abbreviations as in Table 1.
Utility, strengths, and limitations of CMR
CMR is the gold-standard imaging modality for regional and global ventricular function and is uniquely positioned to evaluate ventricular inflammation, edema, and scarring from myocarditis due to its ability to provide myocardial tissue characterization (Figure 4 ). LGE has been an important component of CMR tissue characterization for 20 years, as it provides a precise assessment of the presence, location, and transmural extent of myocardial scarring and fibrosis (56). A mid-myocardial or subepicardial non–coronary artery disease hyperenhancement pattern on LGE is frequently observed in acute myocarditis associated with significant troponin elevation. Multiple studies have demonstrated that the presence of LGE is a powerful marker of adverse cardiac prognosis (heart failure, ventricular arrhythmic events, and mortality) in patients with myocarditis (57,58). Recently, in a subgroup of 187 patients from the ITAMY (ITAlian study in MYocarditis) registry in Italy, evidence of persistent LGE (particularly in the mid-wall septum) at 6 months was the strongest independent predictor of long-term adverse cardiac events at follow-up (median 7 years) (59). It is important to note that in order to differentiate small regions of scarring from artifact, experienced CMR imagers pursue patient-specific adjustments (e.g., change field of view, swap phase encoding direction, adjust inversion time, employ novel black blood or multiple averaged, motion-corrected LGE sequences) of LGE imaging.
Figure 4.
Cardiac Magnetic Resonance Imaging in a Woman With COVID-19 Myocarditis
A 31-year-old woman presented 20 days after the onset of cough, fever, diarrhea, and malaise with subsequent onset of dyspnea and was diagnosed with congestive heart failure upon hospital admission. Cardiac B-type natriuretic peptide was elevated at 2,646 pg/ml, and high-sensitivity troponin I was 110 ng/l. There was mild global reduction in left ventricular (54%) and right ventricular (53%) ejection fraction. Native T1, T2, and late gadolinium enhancement cardiac magnetic resonance images were obtained. (A, B) Myocardial mapping demonstrating significant diffuse elevation of native T1 (1,110 ms) and increased T2 of the lateral wall (69 ms). (C, D) Late gadolinium enhancement imaging demonstrates subepicardial hyperenhancement of the basal and mid lateral wall (blue arrows). In addition, there is a small pericardial effusion and small bilateral pleural effusions are present. COVID-19 = coronavirus disease 2019.
Parametric mapping has greatly expanded the ability of CMR to enhance myocardial tissue characterization. CMR parametric mapping (native T1, T2, and ECV) provides both visual and quantitative data of T1 and T2 relaxation times to accurately evaluate for the presence and extent of myocarditis. Although CMR parametric mapping techniques have been demonstrated to be highly valuable for the diagnosis and prognosis of a wide range of inflammatory, fibrotic, and infiltrative conditions that can affect the myocardium, there are important caveats to be aware of to ensure accurate and consistent CMR mapping data. There are multiple pulse sequences and vendor-specific image acquisition and evaluation techniques for CMR mapping that are not yet standardized. Local consistency in T1 and T2 mapping pulse sequences and parameters employed, data analysis, and reporting are imperative. Ideally, normal reference range data should be obtained locally from each CMR program. As the magnitude of T1 or T2 abnormalities for athletes with suspected COVID-19 myocarditis is likely to be modest, at least 30 to 50 healthy subjects should comprise each institution’s reference range to ensure a higher level of accuracy. Given these nuances, we recommend that such studies be performed only in centers with appropriate experience and proficiency in CMR.
Elevation of native T1 mapping can reflect any myocardial pathological process that affects intracellular, extracellular, or both compartments of the myocardium. T2 mapping is commonly used to evaluate myocardial inflammation, as it becomes elevated in the presence of myocardial edema. Owing to the frequent patchy nature of myocarditis, long-axis (4-chamber) and mid and basal short-axis images should be obtained for both T1 and T2 mapping. It is acknowledged that precise cutoff values for defining “abnormal” native T1, T2, and ECV are not available due to the aforementioned variability of parametric mapping methodologies (60). Balancing adequate sensitivity and specificity accuracy, we suggest that a native T1 or T2 >2 SDs above the local normal reference mean can be used as an abnormal threshold for athletes with suspected COVID-19 myocarditis.
ECV calculation is abnormal for disease states that involve the myocardial interstitial and extracellular space. To calculate ECV, a second T1 mapping acquisition from the same slice locations are obtained 10 to 30 min post–gadolinium contrast administration. A hematocrit obtained within 24 h of the CMR examination is needed for ECV calculation. We suggest using an ECV >30% as an abnormal threshold for athletes with suspected COVID-19 myocarditis. Please refer to the Society for Cardiovascular Magnetic Resonance Consensus Statement on CMR Mapping for further details regarding optimal performance of parametric mapping (61).
The 2018 Lake Louise Criteria for the CMR diagnosis of myocarditis emphasize the presence of an abnormality reflecting myocardial injury (regional or global increase in T1, elevated ECV, or the presence of LGE) and myocardial edema (regional or global increase in T2) to support a clinical diagnosis of myocarditis, as a singular CMR abnormality may not be sufficiently accurate (62). Regional or global ventricular systolic dysfunction and pericardial abnormalities (effusion, pericardial hyperenhancement) are supportive findings for the diagnosis of myocarditis.
The timing of obtaining a CMR study for an athlete with suspected COVID-19 myocarditis is important. CMR during the acute stage of illness should only be performed in cases in which immediate and compelling patient management decisions are anticipated in order to reduce the risk of exposure to hospital and cardiac magnetic resonance staff (63). Ideally, the CMR study should be obtained >10 days from the time of initial diagnosis.
Key points:
-
•
Recent studies employing CMR have identified a high prevalence of cardiac abnormalities in patients recovering from COVID-19. The long-term prognosis associated with these abnormalities is unknown.
-
•
The presence of LGE is associated with an adverse cardiac prognosis in patients with non–COVID-19 myocarditis.
-
•
Steady-state free precession cine imaging, parametric mapping (native T1, T2, and ECV), and LGE imaging should be performed at experienced CMR centers for all athletes undergoing a CMR study in cases of suspected COVID-19 myocarditis.
-
•
Local consistency and proficiency in T1 and T2 mapping pulse sequences and parameters employed, data analysis, and reporting with normal reference ranges are important.
-
•
A CMR abnormality of native T1 or T2 (>2 SDs above local normal reference mean), ECV (>30%), or any LGE can support a clinical diagnosis of myocarditis.
-
•
The CMR study should be obtained >10 days from the time of initial diagnosis.
Computed Tomography Angiography
In the athlete who has ongoing chest pain after COVID-19 or other concerns for ischemic myocardial damage, coronary computed tomography angiography (CTA) may be preferred because of its the excellent negative predictive value. Coronary CTA is also an optimal test for delineating the origin and course of anomalous coronary arteries, which can be a cause of ischemic chest pain, especially in a younger patient population with a lower likelihood of having atherosclerotic disease (64).
Coronary CTA may also reveal important noncoronary cardiac and vascular findings attributable to COVID-19. Patients with active pericarditis can have pericardial thickening and hyperattenuation (65). Moreover, COVID-19 has been associated with an increased incidence of venous thromboembolism, and coronary CTA may reveal pulmonary embolisms, though contrast timing and acquisition parameters are not optimized for pulmonary embolism evaluation (66). Features of RV dysfunction may also be present, including right-sided chamber enlargement and flattening of the interventricular septum. More recently, CT has been used to assess myocardial perfusion, scar, and extracellular volume (67, 68, 69) These assessments are not routine in clinical practice and involve additional contrast and radiation exposure. Therefore, if myocarditis is suspected clinically, dedicated imaging with echocardiography or CMR is suggested.
Coronary CTA can provide some evaluation of the lung parenchyma, although they are typically incompletely visualized, as the field of view is limited to the heart. In COVID-19, a “one-stop-shop” approach includes imaging of the entire thorax as well as evaluation of coronary, aortic, pulmonary artery, and myocardial pathology (70). In the acute phase of COVID-19, when the extent of related complications may be uncertain and there is a need to minimize exposure of health care personnel, this approach may be reasonable. Once recovered, however, CT testing should be optimized to best address the clinical question of interest.
Key points:
-
•
Coronary CTA may be helpful in the individualized secondary risk stratification of athletes who have recovered from COVID-19, particularly in those with ongoing symptoms.
-
•
CT should be optimized to address specific clinical questions and not used routinely as a “a one-stop shop” in the athlete recovering from COVID-19.
Stress Echocardiography and Cardiopulmonary Exercise Testing
Exercise testing can play important diagnostic and prognostic roles in the management of the athlete after COVID-19. Importantly, exercise testing should be avoided during the acute phase of infection, given the risk to staff from contamination of lab space and possible aerosol generation (71) and for excess risk to the patients, particularly those with active myocarditis, as this is an absolute contraindication to exercise testing (72). Once the athlete is no longer infectious and active myocarditis is ruled out, exercise testing should be considered if the athlete has new or persistent symptoms during physical exertion. The addition of gas exchange measurements (i.e., cardiopulmonary exercise testing) may be particularly valuable in those athletes presenting with undifferentiated dyspnea or exertional intolerance, as cardiopulmonary exercise testing can identify both cardiac and pulmonary sequelae of COVID-19 illness. Exercise testing should also be performed in athletes with established COVID-19–associated myocarditis after a 3- to 6-month period of convalescence as part of RTP risk stratification, recommended by guidelines (73). The primary goal of such testing is to identify clinically significant ventricular arrhythmia. Although exercise stress echocardiography has been shown to be helpful in the evaluation of borderline LVEF in athletes (42,43), its role as first-line imaging is limited in this specific setting, given the predominant concern is active myocarditis, and alternative imaging (i.e., CMR) is better suited for this diagnostic purpose. The best choice of exercise testing modality will ultimately depend both on the specifics of the athlete’s presentation and the available resources.
Key point:
-
•
Exercise testing should be considered in the secondary risk stratification of athletes, after strict public health isolation, and based on findings from the initial risk stratification algorithm.
Nuclear and Positron Emission Tomography
For decades, single-photon emission CT and positron emission tomography (PET) myocardial perfusion imaging have been established modalities for the assessment of suspected or known coronary artery disease, and similarly, radionuclide ventriculography has been used to assess LV volumes and EF (65). More recently, dynamic imaging with PET has been used clinically to quantify absolute myocardial blood flow, and 18F-fluorodeoxyglucose PET has assisted in the assessment of myocardial inflammation (74,75). However, in the athlete who has recovered from COVID-19, these modalities are considered second line, given that ionizing radiation should be minimized, especially in a younger patient population. In addition, echocardiography provides a superior hemodynamic assessment, and CMR is the primary modality for the characterization of myocardial tissue.
Therefore, nuclear imaging should be reserved for specific scenarios in which first-line imaging is suboptimal or contraindicated. When pursued, PET myocardial perfusion imaging may be preferred over single-photon emission CT due to more rapid acquisition and lower radiation exposure. Furthermore, in a patient with COVID-19 and suspected microvascular ischemia, quantification of myocardial blood flow with PET may aid in the diagnosis (76). Finally, 18F-fluorodeoxyglucose PET is occasionally a useful adjunct for assessing focal myocarditis (77).
Key point:
-
•
PET should be considered a second-line investigation in the setting of continued clinical concern when echocardiography and CMR are suboptimal or contraindicated.
RTP Considerations for Athletes With Abnormal Findings on Imaging and Recommendations for Follow-Up Testing
Myocarditis
During the active inflammatory phase of myocarditis, athletes should not participate in any sporting activities due to the risk of exercise-induced disease progression and potential to precipitate a malignant arrhythmia in an electrically unstable myocardium (13,14). Owing to the difficulty in clearly defining when active inflammation has resolved, recommendations suggest restriction from competition and strenuous training for 3 to 6 months. After this period, athletes may RTP if they fulfill the following criteria: 1) normalization of LV systolic function; 2) normalization of serum biomarkers of myocardial injury and inflammation; and 3) absence of clinically relevant arrhythmias. Testing should include measurement of cardiac and inflammatory biomarkers, an echocardiogram, a graded exercise ECG, and a Holter monitor (13,14). The use of serial CMR to evaluate for residual scarring has not been well defined, but as previously discussed, residual LGE after the acute phase of myocarditis may be associated with worse outcomes. The 2019 European recommendations suggest that it is reasonable to participate in competitive sports in the context of normal LV function and in the absence of arrhythmia (13). A shared decision-making strategy should be adopted and at least annual clinical surveillance employed.
Acute pericarditis
For most etiologies of acute pericarditis, the natural history is benign, although a small subset may progress to more serious complications, including significant pericardial effusion with tamponade, recurrent pericarditis, and pericardial constriction. The long-term effect of COVID-19–related pericarditis is unknown. Treatment of pericarditis includes exercise restriction as exercise appears to exacerbate inflammation in the pericardium and to precipitate recurrences (54). Athletes with pericarditis should avoid competitive sports during the acute phase. Current recommendations indicate that athletes may return to full activity after normalization of serum inflammatory biomarkers and resolution of any effusion on echocardiography (14). Athletes with concomitant myocardial involvement should follow the recommendations for myocarditis.
RV dysfunction
The underlying cause of RV dysfunction usually determines RTP recommendations. If the RV dysfunction is due to myocarditis or pulmonary emboli, then the guidelines would be made based on these diagnoses and consequences of treatment (e.g., anticoagulation) on sports participation. An important consideration independent of etiology-based guidelines is that RV dysfunction can be associated with an increased risk of arrhythmias in several conditions, including an association between RV dysfunction and arrhythmias in athletes (78). Whether this is relevant to those convalescing from COVID-19 is yet to be determined, but it would seem sensible to exercise caution and be vigilant for palpitations, arrhythmias, and syncope when RV dysfunction is present.
Future Directions
Prospectively collected clinical and imaging data are paramount in order to provide evidenced-based care to those with prior COVID-19 and to determine the safety of return to exercise. Furthermore, the true prevalence of cardiac involvement in athletes with or without COVID-19 symptoms remains unknown. Developing best management practices and clarifying long-term CV sequelae will not be possible without collection and scrutinization of rigorous and carefully obtained data. Athletic registry data will further define best practices for multimodality imaging in COVID-19 for diagnosis, prognosis, and management.
Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
Carl Lavie, MD, served as the Guest Editor for this paper.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Phelan D., Kim J.H., Chung E.H. A game plan for the resumption of sport and exercise after coronavirus disease 2019 (COVID-19) infection. JAMA Cardiol. 2020;5:1085–1086. doi: 10.1001/jamacardio.2020.2136. [DOI] [PubMed] [Google Scholar]
- 2.Schellhorn P., Klingel K., Burgstahler C. Return to sports after COVID-19 infection. Eur Heart J. 2020 May 20 doi: 10.1093/eurheartj/ehaa448. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baggish A., Drezner J.A., Kim J., Martinez M., Prutkin J.M. Resurgence of sport in the wake of COVID-19: cardiac considerations in competitive athletes. Br J Sports Med. 2020;54:1130–1131. doi: 10.1136/bjsports-2020-102516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Puntmann V.O., Carerj M.L., Wieters I. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 Jul 27 doi: 10.1001/jamacardio.2020.3557. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rajpal S., Tong M.S., Borchers J. Cardiovascular magnetic resonance findings in competitive athletes recovering from COVID-19 infection. JAMA Cardiol. 2020 Sep 11 doi: 10.1001/jamacardio.2020.4916. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sandoval Y., Januzzi J.L., Jr., Jaffe A.S. Cardiac troponin for the diagnosis and risk-stratification of myocardial injury in COVID-19: JACC Review Topic of the Week. J Am Coll Cardiol. 2020;76:1244–1258. doi: 10.1016/j.jacc.2020.06.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Libby P. The heart in COVID-19: primary target or secondary bystander? J Am Coll Cardiol Basic Trans Science. 2020;5:537–542. doi: 10.1016/j.jacbts.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Atri D., Siddiqi H.K., Lang J., Nauffal V., Morrow D.A., Bohula E.A. COVID-19 for the cardiologist: a current review of the virology, clinical epidemiology, cardiac and other clinical manifestations and potential therapeutic strategies. J Am Coll Cardiol Basic Trans Science. 2020;5:518–536. doi: 10.1016/j.jacbts.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Phillips M., Robinowitz M., Higgins J.R., Boran K.J., Reed T., Virmani R. Sudden cardiac death in Air Force recruits. A 20-year review. JAMA. 1986;256:2696–2699. [PubMed] [Google Scholar]
- 10.Maron B.J., Haas T.S., Ahluwalia A., Murphy C.J., Garberich R.F. Demographics and epidemiology of sudden deaths in young competitive athletes: from the United States National Registry. Am J Med. 2016;129:1170–1177. doi: 10.1016/j.amjmed.2016.02.031. [DOI] [PubMed] [Google Scholar]
- 11.Vago H., SL, Dohy Z., Merkely B. Cardiac magnetic resonance findings in patients recovered from COVID-19: initial experiences in elite athletes. J Am Coll Cardiol Img. 2020 doi: 10.1016/j.jcmg.2020.11.014. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brito D., Meester S, Yanamala N. High prevalence of pericardial involvement in college student-athletes recovering from COVID-19. J Am Coll Cardiol Img. 2020 doi: 10.1016/j.jcmg.2020.10.023. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pelliccia A., Solberg E.E., Papadakis M. Recommendations for participation in competitive and leisure time sport in athletes with cardiomyopathies, myocarditis, and pericarditis: position statement of the Sport Cardiology Section of the European Association of Preventive Cardiology (EAPC) Eur Heart J. 2019;40:19–33. doi: 10.1093/eurheartj/ehy730. [DOI] [PubMed] [Google Scholar]
- 14.Maron B.J., Udelson J.E., Bonow R.O. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task Force 3: Hypertrophic Cardiomyopathy, Arrhythmogenic Right Ventricular Cardiomyopathy and Other Cardiomyopathies, and Myocarditis: a Scientific Statement from the American Heart Association and American College of Cardiology. Circulation. 2015;132:e273–e280. doi: 10.1161/CIR.0000000000000239. [DOI] [PubMed] [Google Scholar]
- 15.Kiel R.J., Smith F.E., Chason J., Khatib R., Reyes M.P. Coxsackievirus B3 myocarditis in C3H/HeJ mice: description of an inbred model and the effect of exercise on virulence. Eur J Epidemiol. 1989;5:348–350. doi: 10.1007/BF00144836. [DOI] [PubMed] [Google Scholar]
- 16.Driggin E., Madhavan M.V., Bikdeli B. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lindner D., Fitzek A., Bräuninger H. Association of cardiac infection with SARS-CoV-2 in confirmed COVID-19 autopsy cases. JAMA Cardiol. 2020 Jul 27 doi: 10.1001/jamacardio.2020.3551. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lechien J.R., Chiesa-Estomba C.M., Place S. Clinical and epidemiological characteristics of 1420 European patients with mild-to-moderate coronavirus disease 2019. J Intern Med. 2020;288:335–344. doi: 10.1111/joim.13089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wilson M.G., Hull J.H., Rogers J. Cardiorespiratory considerations for return to play in elite athletes after COVID-19 infection: a practical guide for sport and exercise medicine physicians. Br J Sports Med. 2020;54:1157–1161. doi: 10.1136/bjsports-2020-102710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baggish A.L., Levine B.D. Icarus and sports after COVID 19: too close to the sun? Circulation. 2020;142:615–617. doi: 10.1161/CIRCULATIONAHA.120.048335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Caforio A.L., Pankuweit S., Arbustini E. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34:2636–2648, 2648a–d. doi: 10.1093/eurheartj/eht210. [DOI] [PubMed] [Google Scholar]
- 23.Morgera T., Di Lenarda A., Dreas L. Electrocardiography of myocarditis revisited: clinical and prognostic significance of electrocardiographic changes. Am Heart J. 1992;124:455–467. doi: 10.1016/0002-8703(92)90613-z. [DOI] [PubMed] [Google Scholar]
- 24.La Gerche A., Burns A.T., Mooney D.J. Exercise-induced right ventricular dysfunction and structural remodelling in endurance athletes. Eur Heart J. 2012;33:998–1006. doi: 10.1093/eurheartj/ehr397. [DOI] [PubMed] [Google Scholar]
- 25.Donnellan E., Phelan D. Biomarkers of cardiac stress and injury in athletes: what do they mean? Curr Heart Fail Rep. 2018;15:116–122. doi: 10.1007/s11897-018-0385-9. [DOI] [PubMed] [Google Scholar]
- 26.Kleiven O., Omland T., Skadberg O. Race duration and blood pressure are major predictors of exercise-induced cardiac troponin elevation. Int J Cardiol. 2019;283:1–8. doi: 10.1016/j.ijcard.2019.02.044. [DOI] [PubMed] [Google Scholar]
- 27.Bardaji A., Bonet G., Carrasquer A. Prognostic implications of detectable cardiac troponin I below the 99th percentile in patients admitted to an emergency department without acute coronary syndrome. Clin Chem Lab Med. 2018;56:1954–1961. doi: 10.1515/cclm-2017-1140. [DOI] [PubMed] [Google Scholar]
- 28.Johri A.M., Galen B., Kirkpatrick J.N., Lanspa M., Mulvagh S., Thamman R. ASE statement on point-of-care ultrasound during the 2019 novel coronavirus pandemic. J Am Soc Echocardiogr. 2020;33:670–673. doi: 10.1016/j.echo.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baggish A.L., Battle R.W., Beaver T.A. Recommendations on the use of multimodality cardiovascular imaging in young adult competitive athletes: a report from the American Society of Echocardiography in Collaboration with the Society of Cardiovascular Computed Tomography and the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2020;33:523–549. doi: 10.1016/j.echo.2020.02.009. [DOI] [PubMed] [Google Scholar]
- 30.Sharma S., Maron B.J., Whyte G., Firoozi S., Elliott P.M., McKenna W.J. Physiologic limits of left ventricular hypertrophy in elite junior athletes: relevance to differential diagnosis of athlete's heart and hypertrophic cardiomyopathy. J Am Coll Cardiol. 2002;40:1431–1436. doi: 10.1016/s0735-1097(02)02270-2. [DOI] [PubMed] [Google Scholar]
- 31.Rawlins J., Carre F., Kervio G. Ethnic differences in physiological cardiac adaptation to intense physical exercise in highly trained female athletes. Circulation. 2010;121:1078–1085. doi: 10.1161/CIRCULATIONAHA.109.917211. [DOI] [PubMed] [Google Scholar]
- 32.Felker G.M., Boehmer J.P., Hruban R.H. Echocardiographic findings in fulminant and acute myocarditis. J Am Coll Cardiol. 2000;36:227–232. doi: 10.1016/s0735-1097(00)00690-2. [DOI] [PubMed] [Google Scholar]
- 33.Szekely Y., Lichter Y., Taieb P. Spectrum of cardiac manifestations in COVID-19: a systematic echocardiographic study. Circulation. 2020;142:342–353. doi: 10.1161/CIRCULATIONAHA.120.047971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Inciardi R.M., Adamo M., Lupi L. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur Heart J. 2020;41:1821–1829. doi: 10.1093/eurheartj/ehaa388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Churchill T.W., Bertrand P.B., Bernard S. Echocardiographic features of COVID-19 illness and association with cardiac biomarkers. J Am Soc Echocardiogr. 2020;33:1053–1054. doi: 10.1016/j.echo.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mahmoud-Elsayed H.M., Moody W.E., Bradlow W.M. Echocardiographic findings in patients with COVID-19 pneumonia. Can J Cardiol. 2020;36:1203–1207. doi: 10.1016/j.cjca.2020.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li Y., Li H., Zhu S. Prognostic value of right ventricular longitudinal strain in patients with COVID-19. J Am Coll Cardiol Img. 2020 Aug 31 doi: 10.1016/j.jcmg.2020.04.014. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pelliccia A., Culasso F., Di Paolo F.M., Maron B.J. Physiologic left ventricular cavity dilatation in elite athletes. Ann Intern Med. 1999;130:23–31. doi: 10.7326/0003-4819-130-1-199901050-00005. [DOI] [PubMed] [Google Scholar]
- 39.Sheikh N., Sharma S. Impact of ethnicity on cardiac adaptation to exercise. Nat Rev Cardiol. 2014;11:198–217. doi: 10.1038/nrcardio.2014.15. [DOI] [PubMed] [Google Scholar]
- 40.Abergel E., Chatellier G., Hagege A.A. Serial left ventricular adaptations in world-class professional cyclists: implications for disease screening and follow-up. J Am Coll Cardiol. 2004;44:144–149. doi: 10.1016/j.jacc.2004.02.057. [DOI] [PubMed] [Google Scholar]
- 41.Utomi V., Oxborough D., Whyte G.P. Systematic review and meta-analysis of training mode, imaging modality and body size influences on the morphology and function of the male athlete's heart. Heart. 2013;99:1727–1733. doi: 10.1136/heartjnl-2012-303465. [DOI] [PubMed] [Google Scholar]
- 42.Claessen G., Schnell F., Bogaert J. Exercise cardiac magnetic resonance to differentiate athlete's heart from structural heart disease. Eur Heart J Cardiovasc Imaging. 2018;19:1062–1070. doi: 10.1093/ehjci/jey050. [DOI] [PubMed] [Google Scholar]
- 43.Millar L.M., Fanton Z., Finocchiaro G. Differentiation between athlete's heart and dilated cardiomyopathy in athletic individuals. Heart. 2020;106:1059–1065. doi: 10.1136/heartjnl-2019-316147. [DOI] [PubMed] [Google Scholar]
- 44.Lang R.M., Badano L.P., Mor-Avi V. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39.e14. doi: 10.1016/j.echo.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 45.La Gerche A., Taylor A.J., Prior D.L. Athlete's heart: the potential for multimodality imaging to address the critical remaining questions. J Am Coll Cardiol Img. 2009;2:350–363. doi: 10.1016/j.jcmg.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 46.Collier P., Phelan D., Klein A. A test in context: myocardial strain measured by speckle-tracking echocardiography. J Am Coll Cardiol. 2017;69:1043–1056. doi: 10.1016/j.jacc.2016.12.012. [DOI] [PubMed] [Google Scholar]
- 47.Janus S.E., Hajjari J., Karnib M., Tashtish N., Al-Kindi S.G., Hoit B.D. Prognostic value of left ventricular global longitudinal strain in COVID-19. Am J Cardiol. 2020;131:134–136. doi: 10.1016/j.amjcard.2020.06.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Trivedi S.J., Claessen G., Stefani L. Differing mechanisms of atrial fibrillation in athletes and non-athletes: alterations in atrial structure and function. Eur Heart J Cardiovasc Imaging. 2020 Aug 5 doi: 10.1093/ehjci/jeaa183. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 49.D'Ascenzi F., Anselmi F., Focardi M., Mondillo S. Atrial enlargement in the athlete's heart: assessment of atrial function may help distinguish adaptive from pathologic remodeling. J Am Soc Echocardiogr. 2018;31:148–157. doi: 10.1016/j.echo.2017.11.009. [DOI] [PubMed] [Google Scholar]
- 50.Teske A.J., Prakken N.H., De Boeck B.W. Echocardiographic tissue deformation imaging of right ventricular systolic function in endurance athletes. Eur Heart J. 2009;30:969–977. doi: 10.1093/eurheartj/ehp040. [DOI] [PubMed] [Google Scholar]
- 51.Zaidi A., Sheikh N., Jongman J.K. Clinical differentiation between physiological remodeling and arrhythmogenic right ventricular cardiomyopathy in athletes with marked electrocardiographic repolarization anomalies. J Am Coll Cardiol. 2015;65:2702–2711. doi: 10.1016/j.jacc.2015.04.035. [DOI] [PubMed] [Google Scholar]
- 52.Claeys M., Claessen G., Claus P. Right ventricular strain rate during exercise accurately identifies male athletes with right ventricular arrhythmias. Eur Heart J Cardiovasc Imaging. 2020;21:282–290. doi: 10.1093/ehjci/jez228. [DOI] [PubMed] [Google Scholar]
- 53.Lie O.H., Klaboe L.G., Dejgaard L.A. Cardiac phenotypes and markers of adverse outcome in elite athletes with ventricular arrhythmias. J Am Coll Cardiol Img. 2020 Oct 27 doi: 10.1016/j.jcmg.2020.07.039. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 54.Klein A.L., Abbara S., Agler D.A. American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr. 2013;26:965–1012.e15. doi: 10.1016/j.echo.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 55.Huang L., Zhao P., Tang D. Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. J Am Coll Cardiol Img. 2020;13:2330–2339. doi: 10.1016/j.jcmg.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kim R.J., Fieno D.S., Parrish T.B. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation. 1999;100:1992–2002. doi: 10.1161/01.cir.100.19.1992. [DOI] [PubMed] [Google Scholar]
- 57.Grun S., Schumm J., Greulich S. Long-term follow-up of biopsy-proven viral myocarditis: predictors of mortality and incomplete recovery. J Am Coll Cardiol. 2012;59:1604–1615. doi: 10.1016/j.jacc.2012.01.007. [DOI] [PubMed] [Google Scholar]
- 58.Grani C., Eichhorn C., Biere L. Prognostic value of cardiac magnetic resonance tissue characterization in risk stratifying patients with suspected myocarditis. J Am Coll Cardiol. 2017;70:1964–1976. doi: 10.1016/j.jacc.2017.08.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Aquaro G.D., Ghebru Habtemicael Y., Camastra G. Prognostic value of repeating cardiac magnetic resonance in patients with acute myocarditis. J Am Coll Cardiol. 2019;74:2439–2448. doi: 10.1016/j.jacc.2019.08.1061. [DOI] [PubMed] [Google Scholar]
- 60.Nagel E., Kwong R.Y., Chandrashekhar Y.S. CMR in nonischemic myocardial inflammation: solving the problem of diagnosing myocarditis or still diagnostic ambiguity? J Am Coll Cardiol Img. 2020;13:163–166. doi: 10.1016/j.jcmg.2019.10.023. [DOI] [PubMed] [Google Scholar]
- 61.Messroghli D.R., Moon J.C., Ferreira V.M. Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2∗ and extracellular volume: a consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI) J Cardiovasc Magn Reson. 2017;19:75. doi: 10.1186/s12968-017-0389-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ferreira V.M., Schulz-Menger J., Holmvang G. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol. 2018;72:3158–3176. doi: 10.1016/j.jacc.2018.09.072. [DOI] [PubMed] [Google Scholar]
- 63.Han Y., Chen T., Bryant J. Society for Cardiovascular Magnetic Resonance (SCMR) guidance for the practice of cardiovascular magnetic resonance during the COVID-19 pandemic. J Cardiovasc Magn Reson. 2020;22:26. doi: 10.1186/s12968-020-00628-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cheezum M.K., Liberthson R.R., Shah N.R. Anomalous aortic origin of a coronary artery from the inappropriate sinus of Valsalva. J Am Coll Cardiol. 2017;69:1592–1608. doi: 10.1016/j.jacc.2017.01.031. [DOI] [PubMed] [Google Scholar]
- 65.Cremer P., Hachamovitch R., Tamarappoo B. Clinical decision making with myocardial perfusion imaging in patients with known or suspected coronary artery disease. Semin Nucl Med. 2014;44:320–329. doi: 10.1053/j.semnuclmed.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Burris A.C., 2nd, Boura J.A., Raff G.L., Chinnaiyan K.M. Triple rule out versus coronary CT angiography in patients with acute chest pain: results from the ACIC consortium. J Am Coll Cardiol Img. 2015;8:817–825. doi: 10.1016/j.jcmg.2015.02.023. [DOI] [PubMed] [Google Scholar]
- 67.Lubbers M., Coenen A., Kofflard M. Comprehensive cardiac CT with myocardial perfusion imaging versus functional testing in suspected coronary artery disease: the multicenter, randomized CRESCENT-II trial. J Am Coll Cardiol Img. 2018;11:1625–1636. doi: 10.1016/j.jcmg.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 68.Esposito A., Palmisano A., Antunes S. Cardiac CT with delayed enhancement in the characterization of ventricular tachycardia structural substrate: relationship between CT-segmented scar and electro-anatomic mapping. J Am Coll Cardiol Img. 2016;9:822–832. doi: 10.1016/j.jcmg.2015.10.024. [DOI] [PubMed] [Google Scholar]
- 69.Bandula S., White S.K., Flett A.S. Measurement of myocardial extracellular volume fraction by using equilibrium contrast-enhanced CT: validation against histologic findings. Radiology. 2013;269:396–403. doi: 10.1148/radiology.13130130. [DOI] [PubMed] [Google Scholar]
- 70.Pontone G., Baggiano A., Conte E. “Quadruple rule-out” with computed tomography in a COVID-19 patient with equivocal acute coronary syndrome presentation. J Am Coll Cardiol Img. 2020;13:1854–1856. doi: 10.1016/j.jcmg.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Faghy M.A., Sylvester K.P., Cooper B.G., Hull J.H. Cardiopulmonary exercise testing in the COVID-19 endemic phase. Br J Anaesth. 2020;125:447–449. doi: 10.1016/j.bja.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fletcher G.F., Ades P.A., Kligfield P. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation. 2013;128:873–934. doi: 10.1161/CIR.0b013e31829b5b44. [DOI] [PubMed] [Google Scholar]
- 73.Maron B.J., Udelson J.E., Bonow R.O. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task Force 3: Hypertrophic Cardiomyopathy, Arrhythmogenic Right Ventricular Cardiomyopathy and Other Cardiomyopathies, and Myocarditis: a Scientific Statement From the American Heart Association and American College of Cardiology. J Am Coll Cardiol. 2015;66:2362–2371. doi: 10.1016/j.jacc.2015.09.035. [DOI] [PubMed] [Google Scholar]
- 74.Ziadi M.C., Dekemp R.A., Williams K.A. Impaired myocardial flow reserve on rubidium-82 positron emission tomography imaging predicts adverse outcomes in patients assessed for myocardial ischemia. J Am Coll Cardiol. 2011;58:740–748. doi: 10.1016/j.jacc.2011.01.065. [DOI] [PubMed] [Google Scholar]
- 75.Blankstein R., Osborne M., Naya M. Cardiac positron emission tomography enhances prognostic assessments of patients with suspected cardiac sarcoidosis. J Am Coll Cardiol. 2014;63:329–336. doi: 10.1016/j.jacc.2013.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Taqueti V.R., Di Carli M.F. Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC State-of-the-Art Review. J Am Coll Cardiol. 2018;72:2625–2641. doi: 10.1016/j.jacc.2018.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Palmisano A., Vignale D., Peretto G. Hybrid FDG-PET/MR or FDG-PET/CT to detect disease activity in patients with persisting arrhythmias after myocarditis. J Am Coll Cardiol Img. 2020 Aug 31 [E-pub ahead of print] [Google Scholar]
- 78.Heidbuchel H., La Gerche A. The right heart in athletes. Evidence for exercise-induced arrhythmogenic right ventricular cardiomyopathy. Herzschrittmacherther Elektrophysiol. 2012;23:82–86. doi: 10.1007/s00399-012-0180-3. [DOI] [PubMed] [Google Scholar]