The impressive results of the RECOVERY trial established that a moderate dose of dexamethasone (6 mg daily for 10 days) reduced mortality in hospitalised patients with COVID-19 and respiratory failure who required therapy with supplemental oxygen or mechanical ventilation.1 The data also indicated that dexamethasone might increase mortality in hospitalised patients who were not receiving oxygen. This landmark trial and the subsequent practice guidelines from several academic and health organisations recommending dexamethasone use in patients with severe COVID-19 have changed clinical practice for hospitalised patients on supplemental oxygen or mechanical ventilation.2 These favourable findings are supported by three other trials3, 4, 5 of glucocorticoids for COVID-19, which stopped enrolment in early June, 2020, when the RECOVERY trial results were released. Each of these trials showed some evidence of benefit, although none had completed enrolment. A prospective meta-analysis of these and other trials, totalling 1703 participants (1007 [59%] from the RECOVERY trial), confirmed a reduction in 28-day mortality (summary odds ratio [OR] 0·66, 95% CI 0·53–0·82; p<0·001), with minimal heterogeneity across studies.6 While confirming beneficial effects of corticosteroids for critically ill hospitalised patients with COVID-19, some unanswered questions and issues remain that deserve discussion and should be addressed in future research.
Because the design of the largest trial, RECOVERY, was pragmatic, data were scarce in some domains. For example, physicians were able to exclude patients from the trial whom they determined should not be a candidate for treatment with dexamethasone, but reasons for exclusion were not recorded. Thus, we do not know why 1707 patients were unsuitable for randomisation. Patients might have been excluded because of perceived contraindications, including uncontrolled diabetes, acute delirium, underlying malignancy, immunosuppression, or other conditions in which corticosteroids might have harmful effects. Therefore, the benefit–risk profile of corticosteroids across the full spectrum of patients with critical COVID-19 and a range of comorbidities remains uncertain.
A second limitation of the RECOVERY trial is that no data are available on the level of oxygen support. In retrospect, this was an important omission from the database. Such data might have revealed differential benefit or harm with dexamethasone treatment according to level of oxygen supplementation. Moreover, the need for higher levels of oxygen might have been a good indicator that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection had caused some degree of lung injury and that these patients were likely to benefit from dexamethasone therapy.
A third limitation is that the vast majority of patients in these trials were not receiving remdesivir. Although monotherapy with remdesivir does not reduce mortality,7, 8 it is conceivable that the beneficial effects of dexamethasone in patients on supplemental oxygen or mechanical ventilation might be attenuated by the administration of an effective antiviral agent. There might also be an additive benefit of both remdesivir and dexamethasone if remdesivir enhances viral clearance and dexamethasone further decreases the injurious effects of the inflammatory responses to COVID-19.
A fourth limitation is the lack of any data on viral clearance, which is likely to be an important factor in determining harm versus benefit of dexamethasone.9 The normal response to viral infection requires transcriptional upregulation of interferons and recruitment of host inflammatory cells, but corticosteroids in the earlier phase of viral infection can suppress host antiviral responses, potentially leading to more severe lung injury. However, if corticosteroids are administered when viral control has been achieved, they can have a beneficial effect by reducing inflammation and the severity of acute lung injury. Since most of the RECOVERY trial patients treated with oxygen support or mechanical ventilation received dexamethasone more than 7 days since sympton onset, it is possible that viral replication had declined in most patients, particularly since some evidence suggests that SARS-CoV-2 infection, unlike influenza, might be largely cleared in most patients within 7 days.10 Nevertheless, this is an important and unmeasured variable in the RECOVERY trial.
What steps need to be taken to learn more about the effects of dexamethasone in hospitalised patients with COVID-19? More studies on viral clearance and endogenous immune responses,11 both before and after dexamethasone administration, could provide insights into potential beneficial and harmful effects. COVID-19 mortality has been found to be related to impaired interferon responses and dysregulated endogenous proinflammatory responses,12 variables that could be measured in circulating blood samples both before and after dexamethasone treatment. More detailed studies of dexamethasone in hospitalised patients receiving different levels of oxygen support (from low-flow oxygen to high-flow nasal oxygen), along with detailed respiratory and microbiological data, could help to determine whether the benefit of dexamethasone is dependent on the level of oxygen support and other respiratory variables. This information is needed because it is not entirely clear what level of illness should prompt treatment with dexamethasone in non-mechanically ventilated patients with COVID-19. All of these future studies are likely to include remdesivir, which could be an important cofactor that was not part of the RECOVERY trial. Finally, beneficial new therapeutics for COVID-19 are being tested, including monoclonal antibodies, anticoagulation strategies, and additional treatments to block specific arms of the inflammatory cascade, as well as additional antiviral agents. Thus, an ongoing assessment of the interaction of dexamethasone with other therapeutics will be needed as new findings emerge.
There is one more issue to be considered. Should the favourable results of the RECOVERY trial prompt a reconsideration of dexamethasone treatment for acute respiratory distress syndrome (ARDS) due to other causes? This is a key question, as recent work suggests that both classical ARDS and its major risk factor, sepsis, have identifiable subtypes with differential responses to therapy. For example, in one sepsis subtype, randomisation to corticosteroids was associated with increased mortality (OR 7·9, 95% CI 1·6–39·9; pinteraction=0·02).13 A Spanish open-label, randomised, multicentre trial in 277 patients with moderate-to-severe non-COVID-19-related ARDS found a 15% absolute reduction in 60-day mortality (36% to 21%; p=0·0047) in dexamethasone-treated patients.14 This study had important limitations, including the open-label design and the modest overall number of participants (the trial was stopped for low enrolment after 5 years, 2013–18). Nevertheless, we believe that it is reasonable to consider a prospective double-blind, randomised trial design for classical ARDS that will include a sufficient number of patients to be adequately powered for 90-day mortality. Because COVID-19 and classical ARDS have considerable heterogeneity, future trials should incorporate plans for both understanding heterogeneity and prospectively identifying treatment-responsive subgroups of patients.15
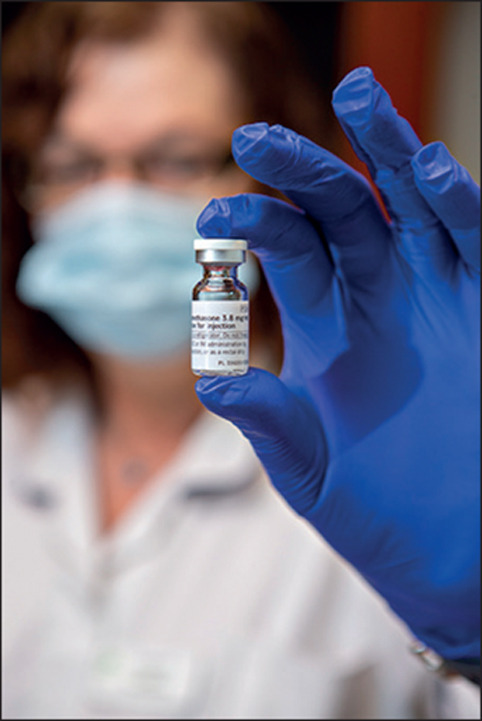
© 2020 Lewis Houghton/Science Photo Library
Acknowledgments
MAM reports grants from the US National Heart, Lung, and Blood Institute and the US National Institutes of Health, the US Department of Defense, the California Institute of Regenerative Medicine, and Roche-Genentech; and consultancy fees from Citius Pharmaceuticals and Novartis, outside of the submitted work. BTT reports consulting fees for Bayer, Thetis, and Novartis, outside of the submitted work.
References
- 1.The Recovery Collaborative Group. Horby P, Lim WS. Dexamethasone in hospitalized patients with Covid-19—preliminary report. N Engl J Med. 2020 doi: 10.1056/NEJMoa2021436. published online July 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lamontagne F, Agoritsas T, Macdonald H. A living WHO guideline on drugs for covid-19. BMJ. 2020;370 doi: 10.1136/bmj.m3379. [DOI] [PubMed] [Google Scholar]
- 3.Dequin PF, Heming N, Meziani F. Effect of hydrocortisone on 21-day mortality or respiratory support among critically ill patients with COVID-19: a randomized clinical trial. JAMA. 2020;324:1298–1306. doi: 10.1001/jama.2020.16761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tomazini BM, Maia IS, Cavalcanti AB. Effect of dexamethasone on days alive and ventilator-free in patients with moderate or severe acute respiratory distress syndrome and COVID-19: the CoDEX randomized clinical trial. JAMA. 2020;324:1307–1316. doi: 10.1001/jama.2020.17021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Angus DC, Derde L, Al-Beidh F. Effect of hydrocortisone on mortality and organ support in patients with severe COVID-19: the REMAP-CAP COVID-19 corticosteroid domain randomized clinical trial. JAMA. 2020;324:1317–1329. doi: 10.1001/jama.2020.17022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA. 2020;324:1330–1341. doi: 10.1001/jama.2020.17023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beigel JH, Tomashek KM, Dodd LE. Remdesivir for the treatment of Covid-19—final report. N Engl J Med. 2020 doi: 10.1056/NEJMoa2007764. published online Oct 8. [DOI] [PubMed] [Google Scholar]
- 8.WHO SOLIDARITY Trial Consortium. Pan H, Peto R. Repurposed antiviral drugs for COVID-19—interim WHO SOLIDARITY trial results. medRxiv. 2020 doi: 10.1101/2020.10.15.20209817. published online Oct 15. (preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matthay MA, Wick KD. Corticosteroids, COVID-19 pneumonia and acute respiratory distress syndrome. J Clin Invest. 2020 doi: 10.1172/JCI143331. published online Sept 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lane HC, Fauci AS. Research in the context of a pandemic. N Engl J Med. 2020 doi: 10.1056/NEJMe2024638. published online July 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuri-Cervantes L, Pampena MB, Meng W. Comprehensive mapping of immune perturbations associated with severe COVID-19. Sci Immunol. 2020;5 doi: 10.1126/sciimmunol.abd7114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hadjadj J, Yatim N, Barnabei L. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science. 2020;369:718–724. doi: 10.1126/science.abc6027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Antcliffe DB, Burnham KL, Al-Beidh F. Transcriptomic signatures in sepsis and a differential response to steroids. Am J Respir Crit Care Med. 2019;199:980–986. doi: 10.1164/rccm.201807-1419OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Villar J, Ferrando C, Martínez D. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir Med. 2020;8:267–276. doi: 10.1016/S2213-2600(19)30417-5. [DOI] [PubMed] [Google Scholar]
- 15.Harhay MO, Casey JD, Clement M. Contemporary strategies to improve clinical trial design for critical care research: insights from the First Critical Care Clinical Trialists Workshop. Intensive Care Med. 2020;46:930–942. doi: 10.1007/s00134-020-05934-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


