Highlights
-
•
More people died from Covid in countries or states with higher rates of intergenerational co-residence.
-
•
The positive correlation persists even when controlling for demographic characteristics, economic factors, and anti-Covid measures.
-
•
The positive association between co-residence and fatalities is led by the US.
-
•
Intergenerational co-residence and Covid detected cases are also positively correlated.
Keywords: Covid-19, Intergenerational co-residence, Mortality, Family arrangements
Abstract
We study how patterns of intergenerational residence possibly influence fatalities from Covid-19. We use aggregate data on Covid-19 deaths, the share of young adults living with their parents, and a number of other statistics, for 29 European countries associated with the European Union and all US states. Controlling for population size, we find that more people died from Covid in countries or states with higher rates of intergenerational co-residence. This positive correlation persists even when controlling for date of first death, presence of lockdown, Covid tests per capita, hospital beds per capita, proportion of elderly, GDP per capita, government’s political orientation, percentage urban, and rental prices. The positive association between co-residence and fatalities is led by the US.
1. Introduction
Covid is a relatively deadly epidemic (Yang et al., 2020) that is particularly likely to kill older people (Abdulamir and Hafidh, 2020). It is also very contagious (Wu et al., 2020). One strategy that individuals and policy-makers have used to protect the more vulnerable elderly from the virus is to minimize contacts between older adults and younger people (Koh, 2020). Intergenerational co-residence makes it harder to avoid such intergenerational contacts. This paper’s main goal is to test whether intergenerational co-residence is positively associated with Covid fatalities. To our knowledge there is limited research assessing the association between mortality from Covid and co-residence of older and younger adults based on international comparisons and across US states. Some recent studies examining the question by comparing various regions of European countries have not established a positive association between intergenerational co-residence and fatalities from Covid (e.g. Belloc et al., 2020; Arpino et al., 2020). Tests are performed using data from 29 countries associated with the European Union (EU) as well as the fifty states of the USA, which adds up to 79 areas (countries or US states).1
By studying 79 geographic areas associated with only two federations (the EU and the USA) we add to previous cross-country or cross-region studies of the association between intergenerational co-residence and Covid fatalities in multiple ways. First, we expand on Bayer and Kuhn’s (2020) study based on data from 24 countries from four continents; our sample is a more homogeneous set of 79 countries associated with the EU or part of the USA. 2 Second, our period of observation is longer than most other studies, including Bayer and Kuhn (2020): we collected number of deaths from February 15 (first death in France) to August 3 2020, one hundred and twelve days after the first Covid death was reported in Wyoming. Third, as pointed out by Belloc et al. (2020), Bayer and Kunz pull together countries at different stages of their epidemic curve. In contrast, we analyze cumulative fatalities attributed to Covid measured at fixed intervals after an area’s onset of the epidemic: 20, 40, 60, 80 and 100 days after the area’s first death. We investigate not only whether intergenerational co-residence contributes to deaths from Covid-19 but also whether such contribution (if positive) varies with the timing of the epidemic’s onset.
Many cross-country studies of fatalities from Covid such as Bayer and Kuhn (2020) and Sorci et al. (2020) have used variation in CFR (case fatality rate) as their measure of mortality. This requires data on both Covid cases and fatalities. Our fourth contribution is that we use cumulative fatalities as our principal COVID outcome. We complement it using cumulative confirmed cases but we place more emphasis on explaining cumulative deaths, as it minimizes measurement error coming from differences in country data publishing methods and testing behavior. In our sample number of tests per capita after 86 days ranged from 0.01 in Bulgaria to 0.18 in Rhode Island and New Mexico.
Fifth, we make a methodological contribution to the literature on fatalities and intergenerational co-residence by controlling for the following variables: test rates per capita measured 14 days prior to the dates at which fatalities are measured, number of days separating the first death in France 3 from the onset date in a state or country, number of hospital beds, and a number of other economic, demographic and political factors likely to be associated with Covid fatalities.
We find that intergenerational co-residence, defined as the share of 18−34 years old living with their parents, is associated with more cumulative deaths after 20, 40, 60, 80 and 100 days. For example, an extra one percentage point in such co-residence is associated with 4% more cumulative deaths from Covid 40 days after the area’s onset of the epidemic, 3.5 % more cumulative deaths 60 days after onset and 3% more Covid deaths at either 80 or 100 days after onset. We find that the association between co-residence and cumulative deaths is larger for US states than for EU countries. Lovett et al. (2020) have suggested that in the USA the association between co-residence and deaths is related to a urban/rural divide, with multi-generational co-residence being more common in rural areas. We don’t find that.
We also explore whether one of the channels that links intergenerational co-residence and cumulative death rates is an association between intergenerational co-residence and number of cases. We find that co-residence rates are also positively associated with cumulative cases, a proxy for the number of infected individuals.
Even though it was not our primary goal, our study also offers a more sophisticated comparison of fatalities due to Covid in the US and the EU than a simple comparison between European countries and the USA as one country. From a statistical point of view it may be incorrect to pool all the states of the US.4
We check the robustness of our results by controlling for different social distance measures, not only lockdowns, and using a 16 days difference between tests and deaths instead of a 14 days difference.
The next section discusses the models and data used in this study. Results are presented in Section 3 and Section 4 concludes.
2. Empirical set-up
2a. The model. Our main variables of interest are cumulative Covid-caused deaths and intergenerational co-residence rates. We estimate the conditional correlation of Covid deaths and intergenerational co-residence rates using log-linear regressions, with log of number of deaths being the left-hand side variable. We use a logarithmic transformation, for logarithms allow us to interpret coefficients in percentage terms which favors comparability across areas (countries and states) that are highly heterogeneous.5 This leads to the following estimating equation:
| (1) |
where Deaths are the number of cumulative Covid-caused deaths 20, 40, 60, 80, or 100 days after the first death in area r, and Co-resid is the proportion of 18–34 years old individuals living with their parents in that area. X is a vector of variables related to Covid and Z is a vector of demographic and other controls.
Vector X includes a dummy equal to one if the government imposed a lockdown and days from first death to lockdown: imposition of a lockdown and the speed at which a lockdown was imposed have been associated with lower death rates from Covid (e.g. Friedson et al., 2020; Huber and Langen, 2020). We also control for number of tests per capita 14 days prior to the day deaths were measured and for number of days that elapsed between onset of the epidemic in France and in each country/state.6 For example, for deaths at 20 days we include tests per capita at 6 days past onset; for deaths at 100 days past onset, we include tests 86 days past onset.
Vector Z includes demographic variables, starting with total population in the country/state. Population’s effect may be mechanical: more people implies a potential for more deaths. In addition, it is possible that population affects number of deaths because it affects population density. In turn, such density may facilitate the spread of infections such as Covid. It is not just the total population that matters, but also the share of individuals over age 65 who are more likely to die from Covid (Abdulamir and Hafidh, 2020). We thus add proportion of individuals over 65 as a control. Furthermore, our regressions control for proportion urban: density in large cities may be particularly conducive to Covid infections and fatalities (Florida, 2020).7
Furthermore, vector Z includes a control for whether the area is a US state. We control for hospital beds per capita and for whether an area has a government leaning to the left (in the case of European countries based on party classifications; in the case of the US based on whether the state’s governor is affiliated with the Democratic party). Political variables have helped explain cross-country variation in Covid deaths in previous studies. For example, a study of 103 countries by Sorci et al. (2020) found that democracies suffer from a higher mortality burden than autocratic regimes. Our controls include a dummy for US and an interaction between leftist government and US.
Two economic variables are included in Z as well. First, GDP (Gross Domestic Product or its equivalent in the case of US states, Gross State Product or GSP) per capita,8 for it may influence the spread of Covid (e.g. through exposure to foreigners) and how fatal it is via a number of channels, including quality of health care and degree of lockdown. Rent, a major determinant of the price of housing, is included in the controls, in part due to its influence on individual and policy-makers options to separate those who are sick from those have not yet caught the virus.
We subject our estimates to the Oster (2019) test for selection on unobservables
Oster (2019) develops a methodology to evaluate the possible degree of omitted variable bias under the assumption that the selection on the observed controls is proportional to the selection on the unobserved controls. We use it to compute the value of the relative degree of selection that would be necessary to explain our coefficient for the share of young individuals living with their parents.
2b. The data. The European data we use are limited to 29 countries, of which 26 currently belong to the European Union (EU). 9 For the US we include the 50 states. Table 1 contains links to our data sources, the year they were measured, and the dates they were downloaded. Data on daily Covid-caused deaths were extracted from the European Centre for Disease Prevention and Control in the case of European countries and from the New York Times github page in the case of US states. We then computed cumulative number of deaths at 20-day intervals starting from the onset of a country/state’s Covid epidemic. A limitation of this study follows from the lack of comparability of data on fatalities across different countries and states.10
Table 1.
Data Definitions and Sources.
| Variable | EU countries | US states | Year Measured |
Downloaded on |
|---|---|---|---|---|
| Covid deaths | https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases | https://github.com/nytimes/covid-19-data/blob/master/us-states.csv | 2020 | August 3, 2020 |
| Intergenerational co-residence | http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset = ilc_lvps08& | https://data.census.gov/cedsci/table?q = Young%20Adults,%2018−34%20Years%20Old,%20Living%20At%20Home%20by%20state&g = 0100000US.04000.001&hidePreview = true&tid = ACSDT1Y2018.B09021&vintage = 2018&layer = VT_2018_040_00_PY_D1&cid = B09021_008E | 2018 | April 23, 2020 |
| COVID-RELATED VARIABLES | ||||
| Number of tests* | https://ourworldindata.org/grapher/full-list-total-tests-for-covid-19 | https://covidtracking.com/api | 2020 | August 3, 2020 |
| Days from 1 st death to lockdown | https://github.com/OlivierLej/Coronavirus_CounterMeasures | https://github.com/OlivierLej/Coronavirus_CounterMeasures | 2020 | April 25, 2020 |
| Days post France** | Same source as above | Same source as above | 2020 | Same as above |
| DEMOGRAPHICS | ||||
| Total population, and % over 65 | https://appsso.eurostat.ec.europa.eu/nui/submitViewTableAction.do | https://data.census.gov/cedsci/table?q = S0102&tid = ACSST1Y2018.S0102 | 2018 | May 11, 2020 |
| % Urban population | https://population.un.org/wup/DataQuery/ | https://www.icip.iastate.edu/tables/population/urban-pct-states | 2010 | May 16, 2020 |
| OTHER VARIABLES | ||||
| Hospital beds (per 1000 inhabitants)*** | https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2019_4dd50c09-en | http://ghdx.healthdata.org/record/united-states-hospital-beds-1000-population-state | 2017 | June 25, 2020 |
| Government political orientation | https://en.wikipedia.org/wiki/List_of_ruling_political_parties_by_country; https://europarl.europa.eu/election-results-2019/en/breakdown-national-parties-political-group/2019−2024/ |
https://en.wikipedia.org/wiki/List_of_United_States_governors | 2020 | May 27, 2020 |
| Rental Prices | https://www.ubs.com/microsites/prices-earnings/en/ | https://www.zillow.com/research/data/ | 2020 | May 8, 2020 |
| Gross Domestic or State Product in dollars (per capita) | https://data.worldbank.org/indicator/NY.GDP.PCAP.CD | https://www.bea.gov/ https://www2.census.gov/programs-surveys/popest/tables/2010−2016/state/totals/nst-est2016−01.xlsx | 2018 | April 29, 2020 |
*The number of tests was measured 14 days prior to the number of fatalities.
**Number of days from February 15, when the first Covid death in our sample was reported in France, to the first death in a particular country.
***Data for Bulgaria, Croatia, Romania and Serbia is from https://ourworldindata.org/.
Regarding the Covid-related controls, information on lockdown measures was collected by Olivier Lejeune for both the EU and the US. The number of tests in EU countries comes from the University of Oxford while information on tests in US states is from the COVID Tracking Project (The Atlantic). This data also allowed us to calculate “Days post France”, the number of days that elapsed between the first death in France and the first death in a particular area which we define as the onset of the epidemic in an area (country or state).
Demographic information (i.e. the share of 18−34 years old living with their parents, total population and the share of individuals over age 65) comes from Eurostat for EU countries and from the American Community Survey for US states. In both cases the information is for 2018. The share of population living in urban areas was extracted from the United Nations (UN) Population Division for EU countries (World Urbanization Prospects) and from the Iowa Community Indicators Program of Iowa State University for US states. The UN data define ‘urban’ according to the criteria used by each country. The US data is based on the 2010 Census and defines urban as “densely settled territory with specific population thresholds and urban clusters (each with their own population size and density thresholds).”
Data on hospital beds were obtained from the OECD for the EU and from the Global Health Data Exchange webpage for the US. In both cases, the information is for 2017. We gathered information on the government in power in the EU countries based on the last elections as reported in Wikipedia. Most countries who are members of the EU have governments based on what parties won a majority of seats in the last election. We considered as left-wing those parties belonging to the Greens-European Free Alliance, European United Left-Nordic Green Left, and Progressive Alliance of Socialists and Democrats groups.11 For US states, we refer to the party of the state’s governor and we classified Democrats as left-wing. Rental prices come from Statista and Zillow for EU countries and US states, respectively, and were collected for 2020. We collected 2018 data on per capita GDP from the World Bank (for EU countries) and from the U.S. Bureau of Economic Analysis (for US states). All data can be found in the Appendix.
Table 2 reports descriptive statistics for our sample of 29 European nations/states and 50 US states. For simplicity, in the rest of this paper they are all called ‘areas’. It can be seen from Table 2A that for the average ‘area’ cumulative deaths went up from 224 after 20 days to 3709 at 100 days after the first death in that area. Table 2B breaks these statistics down by continent. Mean cumulative deaths at 100 days after onset amounted to 2413 per US state and to 5943 per EU country. The tables also report on average fatality rates per capita. For the combined sample they started at 27 deaths pc after 20 days and reached 329 deaths after 100 days (Table 2A). The corresponding numbers for the US (EU) were 33 (18) when measured 20 days after the onset of an area’s epidemic and 407 (194) after 100 days. At both these time intervals standard deviations in the US were roughly double those in the EU, which confirms Baker (2020)’s observation that death rates varied more in the US than in Europe.
Table 2A.
Descriptive Statistics for Complete Sample (EU + US).
| mean | Sd | min | max | |
|---|---|---|---|---|
| US | 0.633 | 0.485 | 0 | 1 |
| Deaths 20 | 223.506 | 543.999 | 1 | 3716 |
| Deaths 40 | 1515.076 | 3733.115 | 7 | 20,212 |
| Deaths 60 | 2723.848 | 6159.075 | 8 | 29,446 |
| Deaths 80 | 3398.203 | 7500.756 | 10 | 37,297 |
| Deaths 100 | 3709.215 | 8011.994 | 14 | 41,800 |
| Deaths 20 pc | 27.244 | 37.580 | 0.104 | 248.931 |
| Deaths 100 pc | 328.737 | 417.310 | 5.137 | 2072.24 |
| Co-residence | 37.644 | 13.729 | 14.543 | 75 |
| Tests pc 6 | 0. 003 | 0.004 | 3.08e-07 | 0.017 |
| Tests pc 26 | 0.014 | 0.010 | 0.0004 | 0.053 |
| Tests pc 46 | 0.030 | 0.019 | 0.004 | 0.105 |
| Tests pc 66 | 0.053 | 0.028 | 0.009 | 0.144 |
| Tests pc 86 | 0.081 | 0.040 | 0.013 | 0.178 |
| Days to lockdown | 6.430 | 8.308 | −16 | 31 |
| No lockdown | 0.304 | 0.463 | 0 | 1 |
| Days post France | 31.772 | 8.961 | 0 | 58 |
| Population | 9.852 | 15.981 | 0.431 | 83.019 |
| % over 65 | 0.176 | 0.024 | 0.111 | 0.228 |
| % urban | 72.784 | 13.711 | 38.7 | 97.7 |
| Hospital beds pc | 3.481 | 1.624 | 1.7 | 8 |
| Leftist gov. | 0.392 | 0.491 | 0 | 1 |
| GDP or GSP pc | 51375.47 | 20545.45 | 7246.192 | 116597.3 |
| Rental prices | 1543.3 | 628.7 | 521.4 | 2990 |
Notes: Data sources: see Table 1. Deaths20, Deaths30 etc refer to cumulative deaths 20, 30, etc days after the first death in the country/state. Co-residence using the share of 18−34 year-olds living with their parents. “Days post France” is the number of days between first death in France and first death in country/state. Days to lockdown reflects the number of days from the first COVID-related death to lockdown. It is missing for those countries/states without lockdown. Population is expressed in millions of citizens.
Table 2B.
Separate Descriptive Statistics for US States and EU Countries.
| US States | EU Countries | |||
|---|---|---|---|---|
| Mean | Std Dev | Mean | Std Dev | |
| Deaths 20 | 179.5 | 531.069 | 299.310 | 566.944 |
| Deaths 40 | 1011.34 | 2923.496 | 2383.586 | 4757.184 |
| Deaths 60 | 1710.18 | 4120.074 | 4471.552 | 8424.321 |
| Deaths 80 | 2144.4 | 4598.357 | 5559.931 | 10586.66 |
| Deaths 100 | 2413.38 | 4833.187 | 5943.414 | 11391.78 |
| Deaths 20 pc | 32.875 | 43.804 | 17.535 | 20.541 |
| Deaths 100 pc | 406.989 | 479.538 | 193.820 | 230.031 |
| Co-residence | 31.217 | 6.190 | 48.724 | 16.035 |
| Tests pc 6 | 0.002 | 0.003 | 0.003 | 0.004 |
| Tests pc 26 | 0.013 | 0.008 | 0.013 | 0.011 |
| Tests pc 46 | 0.031 | 0.018 | 0.025 | 0.017 |
| Tests pc 66 | 0.057 | 0.026 | 0.040 | 0.026 |
| Tests pc 86 | 0.091 | 0.035 | 0.056 | 0.036 |
| Days to lockdown | 7.68 | 8.479 | 4.276 | 7.671 |
| No lockdown | 0.12 | 0.328 | 0.621 | 0.494 |
| Days post France | 33.48 | 7.517 | 28.828 | 10.519 |
| Population | 4.908 | 5.535 | 18.377 | 23.215 |
| % over 65 | 0.165 | 0.019 | 0.194 | 0.021 |
| % urban | 73.59 | 14.565 | 71.393 | 12.219 |
| Hospital beds pc | 2.63 | 0.719 | 4.948 | 1.710 |
| Leftist gov. | 0.48 | 0.505 | 0.241 | 0.435 |
| GDP or GSP pc | 58721.74 | 11067.72 | 38709.49 | 26438.62 |
| Rental prices | 1642.54 | 577.254 | 1372.266 | 685.502 |
Our principal explanatory variable of interest is co-residence of young adults (ages 18−34) with their parents. On average, among the 79 areas in our sample 37.6 % of 18−34 year-olds live with their parents. For European countries this average is 49 % and for US states 31 %. The standard deviations are quite high: 16.0 in the EU and 6.2 in the US. Croatia has the highest co-residence rate in Europe (75 %); Denmark the lowest (18.8 %). In the US co-residence rates range between 14.5 % (North Dakota) and 46.25 % (New Jersey).
From Table 2A it can be seen that tests per capita grew considerably over time: from an average of 0.003 per capita 6 days after onset to an average of 0.081 86 days after onset in a particular area. Initially EU countries had more tests per capita than US states, but this reversed at 46 days past onset. For example, at 86 days EU countries on average had 0.056 such tests versus 0.91 for the US (see Table 2B). It can also be seen that 30 % of all areas did not have a lockdown, implying that a lockdown was imposed in 70 % of the areas. EU countries were less likely to have a lockdown than US states: 62 % of EU countries did not have a lockdown, but this was only the case with 12 % of US states. On average it took an area 6.4 days from onset to lockdown. The first COVID-related death in the EU or US was reported in France on February 15. “Days post France” reports the number of days from February 15 to the first death in a particular area. That day points to the onset of the epidemic in that country or state. On average, an area experienced its first Covid-caused death 32 days after France. On average EU countries had an earlier onset: after 29 days compared to 33 days later for US states. Days between onset in France and other areas lie in a range between zero and 58. Slightly less than 10 million individuals live in the average area.
On average, 17.5 % of individuals are older than 65 and almost 73 % of an area’s population lives in cities. There are significantly fewer hospital beds per capita in the US than in the EU, but the standard deviation is more than twice as large in the EU than in the US. 48 % of US governors are democrats and we define 24 % of European governments as left-wing. An area’s average GDP per capita is 51,375 (with an average of 58,722 for US states and 38,709 for EU countries).
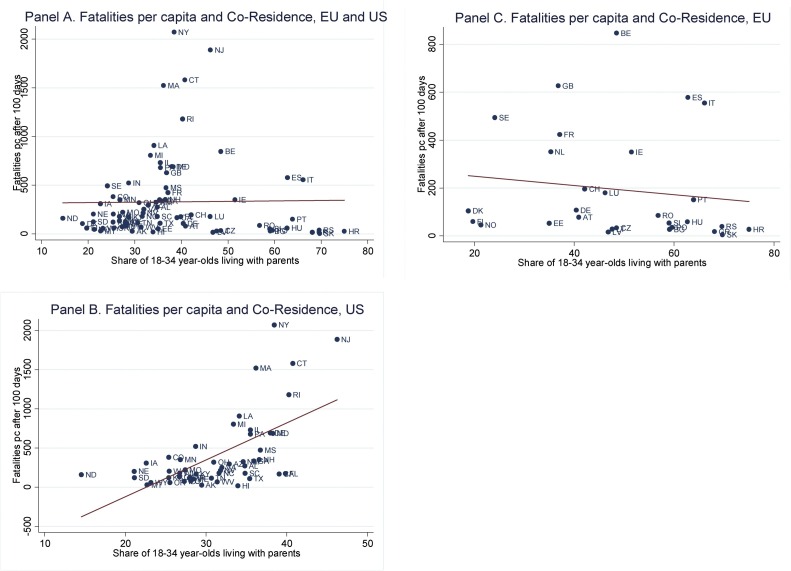
Fig. 1 plots per capita number of deaths 100 days after onset and share of 18−34 year olds living with parents for all 79 areas (European countries and US states). In Panel A all 79 areas are included; Panel B is for US states only; and Panel C for countries associated with the EU. The simple correlation between these two variables is barely positive when all areas are included and it is negative for the European countries. In contrast, there is a clearly positive slope in Panel B: fatalities per capita and co-residence of young adult children and their parents are positively associated when comparing US states. The states driving this association include Connecticut, Massachusetts, New Jersey, New York, and Rhode Island, where both fatalities per capita and co-residence rates are relatively high. Some European countries with high co-residence have high fatalities per capita, as in the case of Spain and Italy, but others with even higher co-residence rates, such as Croatia and Slovakia, have very low fatalities.
Fig. 1.
Fatalities per capita 100 Days after Onset and Share of 18-34 Year Olds Living with Parents.
Notes: Fatalities 100 days after the first death in a given country; pc: per capita. For data sources see Table 1; for acronyms for country or US state see below.
| Name | Name | Name | Name | ||||
|---|---|---|---|---|---|---|---|
| Alabama | AL | Greece | GR | Mississippi | MS | Romania | RO |
| Alaska | AK | Hawaii | HI | Missouri | MO | Serbia | RS |
| Arizona | AZ | Hungary | HU | Montana | MT | Slovakia | SK |
| Arkansas | AR | Idaho | ID | Nebraska | NE | Slovenia | SI |
| Austria | AT | Illinois | IL | Netherlands | NL | S. Carolina | SC |
| Belgium | BE | Indiana | IN | Nevada | NV | S. Dakota | SD |
| Bulgaria | BG | Iowa | IA | New Hampshire | NH | Spain | ES |
| California | CA | Ireland | IE | New Jersey | NJ | Sweden | SE |
| Colorado | CO | Italy | IT | New Mexico | NM | Switzerland | CH |
| Connecticut | CT | Kansas | KS | New York | NY | Tennessee | TN |
| Czechia | CZ | Kentucky | KY | North Carolina | NC | Texas | TX |
| Croatia | HR | Latvia | LV | North Dakota | ND | United Kingdom | GB |
| Delaware | DE | Lithuania | LT | Norway | NO | Utah | UT |
| Denmark | DK | Louisiana | LA | Ohio | OH | Vermont | VT |
| Estonia | EE | Luxembourg | LU | Oklahoma | OK | Virginia | VA |
| Finland | FI | Maine | ME | Oregon | OR | Washington | WA |
| Florida | FL | Maryland | MD | Pennsylvania | PA | West Virginia | WV |
| France | FR | Massachusetts | MA | Poland | PO | Wisconsin | WI |
| Georgia | GA | Michigan | MI | Portugal | PT | Wyoming | WY |
| Germany | DE | Minnesota | MN | Rhode Island | RI |
We now proceed to the regression analysis allowing us to examine the partial association between fatalities and co-residence, after controlling for many other relevant factors.
3. Findings and discussion
Main findings. Table 3 contains the results of the main estimations of Eq. 1 for the combined sample of 29 countries associated with the EU and 50 US states. Cumulative deaths are measured either after 20, 40, 60, 80 or 100 days. Given that the function we estimate is a logarithmic transformation, it follows from the first coefficient in Column 1 that one extra percentage point in the share of young individuals living with their parents is associated with 2.4 % more cumulative deaths from Covid 20 days after an area’s first death. However, this coefficient is not statistically significant. Columns 2–5 indicate that one extra percentage point in the share of individuals age 18−34 living with their parents is associated with 4 % more deaths after 40 days, 3.5 % more deaths after 60 days, 3.2 % after 80 days, and 3.1 % after 100 days. Starting at 40 days, all associations between deaths and co-residence are highly significant statistically.
Table 3.
Log of Cumulative Covid-19 Deaths and Intergenerational Co-residence Rates.
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| VARIABLES | Deaths20 | Deaths40 | Deaths60 | Deaths80 | Deaths100 |
| Co-residence | 0.0241 | 0.0396** | 0.0345** | 0.0319** | 0.0307** |
| (0.0168) | (0.0160) | (0.0150) | (0.0149) | (0.0146) | |
| COVID-RELATED | |||||
| Tests pc | −252.8*** | −18.78 | −0.614 | 5.903 | 4.590 |
| (61.69) | (19.51) | (8.342) | (6.644) | (5.255) | |
| Days to lockdown | −0.0294 | 0.00218 | 0.0104 | 0.0156 | 0.0156 |
| (0.0314) | (0.0343) | (0.0328) | (0.0326) | (0.0326) | |
| No lockdown | −0.283 | 0.136 | 0.200 | 0.247 | 0.253 |
| (0.462) | (0.505) | (0.503) | (0.505) | (0.506) | |
| Days Post France | 0.0696 | −0.0367 | −0.0661** | −0.0787** | −0.0788** |
| (0.0442) | (0.0384) | (0.0329) | (0.0319) | (0.0309) | |
| DEMOGRAPHIC | |||||
| Population | 0.0427*** | 0.0449*** | 0.0469*** | 0.0472*** | 0.0473*** |
| (0.0105) | (0.0114) | (0.0110) | (0.0106) | (0.0104) | |
| % over 65 | 6.679 | 4.701 | 3.444 | 2.721 | 1.646 |
| (7.481) | (9.350) | (9.617) | (9.626) | (9.359) | |
| % Urban | 0.0185 | 0.0277** | 0.0288** | 0.0285** | 0.0301** |
| (0.0115) | (0.0131) | (0.0136) | (0.0135) | (0.0133) | |
| OTHER | |||||
| US | −0.946 | 0.239 | 0.671 | 0.816 | 0.925 |
| (0.741) | (0.657) | (0.600) | (0.594) | (0.633) | |
| Hospital beds | −0.359** | −0.196 | −0.133 | −0.129 | −0.115 |
| (0.166) | (0.174) | (0.170) | (0.168) | (0.167) | |
| Leftist gov. | 0.291 | 0.346 | 0.237 | 0.164 | 0.150 |
| (0.571) | (0.584) | (0.655) | (0.679) | (0.691) | |
| Leftist*US | −0.114 | −0.0572 | −0.0789 | −0.0390 | −0.103 |
| (0.641) | (0.662) | (0.707) | (0.721) | (0.717) | |
| GDP pc | 2.48e-05** | 1.59e-05 | 6.65e-06 | −3.57e-07 | −3.05e-06 |
| (1.21e-05) | (1.36e-05) | (1.37e-05) | (1.40e-05) | (1.35e-05) | |
| Rental Prices | −0.000245 | 5.55e-05 | 0.000270 | 0.000332 | 0.000350 |
| (0.000315) | (0.000350) | (0.000309) | (0.000301) | (0.000293) | |
| Constant | 0.0910 | 1.822 | 2.989 | 3.671 | 3.890 |
| (3.023) | (3.432) | (3.527) | (3.562) | (3.492) | |
| Observations | 79 | 79 | 79 | 79 | 79 |
| R-squared | 0.500 | 0.594 | 0.646 | 0.657 | 0.664 |
Notes: For definitions see Table 2A. Robust standard errors in parentheses. *** p < 0.01, ** p < 0.05, * p < 0.1.
The magnitude of the estimated associations between the logarithms of deaths at different time intervals and co-residence rates is similar. This may be attributed to the similar distributions of the five logarithmic dependent variables. Averages range between 4.2–6.6 and standard deviations grow from 1.5 to 1.9. Also the supports overlap significantly (values go from 0 to 10.6). Moreover, the five dependent variables are very highly correlated: correlations range from 0.802 for log of deaths at 20 and 100 days to almost one for log of deaths at 60 and 80 days, log of deaths at 60 and 100 days, and log of deaths at 80 and 100 days.
Next, we assess whether the association between mortality and co-residence is more applicable to the US or to Europe. In particular, we test the hypothesis that the relationship between co-residence and Covid fatalities for US states differs from that for countries associated with the EU. This involves testing whether the coefficient of the interaction of co-residence and the US dummy ( equals zero in the following equation:
| (2) |
where the coefficient of co-residence ( now refers to EU countries only. As shown in Table 4 takes values between 6 and 11 % and is statistically significant in all regressions. In contrast, ranges between 1 and 2% and is not statistically different from zero. Hence, we conclude that US states lead our estimated relationship between co-residence and COVID fatalities. The total association between co-residence and fatalities in the US is calculated by adding up the two coefficients of co-residence and co-residence*US. Consider deaths at 100 days after onset (col. 5 in Table 4). We add up 0.109 and 0.00852 which equals 0.11752, implying that a one extra percentage point in the share of co-residence in the US (let us say from the mean of 37.5 % co-residing in the state to 38.5 %) is associated with an increase in deaths at 100 days of 11.8 percent. This sum is significantly different from zero and is economically significant. Our conclusions are robust to an alternative estimation strategy in which we run separate regressions for subsamples of US states and EU countries.12 All results remain invariant if we use population over 65 instead of overall population.
Table 4.
Log of Cumulative Covid-19 Deaths and Intergenerational Co-residence rates, separating EU Countries and US States.
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| VARIABLES | Deaths20 | Deaths40 | Deaths60 | Deaths80 | Deaths100 |
| Co-residence | 0.00863 | 0.0151 | 0.00935 | 0.00951 | 0.00842 |
| (0.0183) | (0.0158) | (0.0149) | (0.0150) | (0.0150) | |
| Coresidence*US | 0.0648* | 0.0984*** | 0.114*** | 0.111*** | 0.109*** |
| (0.0333) | (0.0336) | (0.0348) | (0.0353) | (0.0342) | |
| Observations | 79 | 79 | 79 | 79 | 79 |
| R-squared | 0.524 | 0.662 | 0.696 | 0.695 | 0.699 |
Notes: All other controls reported in Table 3 are included. Robust standard errors in parentheses. *** p < 0.01, ** p < 0.05, * p < 0.1.
In our main specification we accounted for days since onset of the epidemic to lockdown and absence of lockdown. Lockdown implies that the government requires citizens to shelter in place all day long and that they are allowed to come out only to buy essential items. We used these extreme limitations on social activities because with 79 observations we need to limit the number of controls. However, governments changed social distancing rules as the epidemic progressed and measures softer than lockdowns were often introduced. In additional regressions, we included dummies for each separate limitation (no social events, no schools, no shops, partial lockdown and lockdown) being in place at the time that deaths were measured.13 We also include number of days from the first death to the implementation of each type of limitation. Results in Table 5 show that coefficients of co-residence remain mostly unaltered.
Table 5.
Log of Cumulative Covid-19 Deaths and Intergenerational Co-residence rates, accounting for Different Social Distance Measures.
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| VARIABLES | Deaths20 | Deaths40 | Deaths60 | Deaths80 | Deaths100 |
| Co-residence | 0.0180 | 0.0377** | 0.0331** | 0.0309** | 0.0294** |
| (0.0160) | (0.0151) | (0.0146) | (0.0145) | (0.0142) | |
| Days No social events | −0.00414 | −0.00257 | 0.00124 | 0.00135 | 0.000841 |
| (0.0120) | (0.0122) | (0.0124) | (0.0125) | (0.0127) | |
| Days No schools | −0.0149* | −0.0195** | −0.0176** | −0.0155* | −0.0143* |
| (0.00777) | (0.00861) | (0.00781) | (0.00779) | (0.00775) | |
| Days No shops | 0.00286 | 0.0227 | 0.0243 | 0.0244 | 0.0280 |
| (0.0323) | (0.0376) | (0.0402) | (0.0406) | (0.0407) | |
| DaysPartial lockdown | −0.0533** | −0.0404 | −0.0304 | −0.0223 | −0.0147 |
| (0.0224) | (0.0254) | (0.0245) | (0.0237) | (0.0243) | |
| Days Full lockdown | −0.0290 | 0.00279 | 0.0203 | 0.0283 | 0.0299 |
| (0.0236) | (0.0312) | (0.0331) | (0.0342) | (0.0343) | |
| No social events | 1.987 | ||||
| (1.449) | |||||
| No schools | −0.483 | −0.310 | 0.731 | 0.956 | 1.113 |
| (0.980) | (0.800) | (0.866) | (0.898) | (0.891) | |
| No shops | 1.329 | 0.914 | 0.265 | −0.0404 | −0.196 |
| (0.943) | (0.769) | (0.910) | (0.965) | (0.960) | |
| Partial lockdown | 0.294 | −0.398 | −0.370 | −0.300 | −0.309 |
| (0.479) | (0.424) | (0.452) | (0.460) | (0.462) | |
| Full lockdown | −0.158 | −0.119 | −0.220 | −0.258 | −0.216 |
| (0.470) | (0.573) | (0.571) | (0.585) | (0.584) | |
| Observations | 79 | 79 | 79 | 79 | 79 |
| R-squared | 0.601 | 0.643 | 0.677 | 0.682 | 0.687 |
Notes: All other controls reported in Table 3 are included. Robust standard errors in parentheses. *** p < 0.01, ** p < 0.05, * p < 0.1.
Our estimates pass the Oster (2019) test for selection on unobservables. In particular, we obtain a measure of the extent of selection on unobservables relative to selection on observables (delta) equal to 1.55. This value implies that selection on unobservables would have to be 1.55 times larger than selection on observables to explain the observed correlation between intergenerational co-residence and Covid-related deaths. This threshold exceeds the rule-of thumb cutoff of 1 in observational studies.
Throughout our analysis we treat states/countries as independent statistical units. However, our variables of interest are characterized by significant spatial autocorrelations (Miron, 1984). We present some evidence related to these autocorrelations. We first calculated average COVID fatalities and average co-residence rates in neighboring states/countries (those countries/states that share a border) for each country/state. For instance, to the state of Kansas we assigned the average values for the states of Colorado, Nebraska, Missouri, and Oklahoma. We then computed correlations between COVID fatalities in a particular area and average COVID fatalities in neighboring states/countries as well as between between co-residence rate in a particular area and average co-residence rate in neighboring countries/states. Our sample size is reduced to 77 because Alaska and Hawaii do not have neighboring states. All the correlations are high: those between fatality rates are between 0.38 and 0.54, depending on the days since onset, and that between co-residence rates is 0.88. The spatial correlations may be due to a significant amount of individuals commuting across borders or to the fact that areas that are geographically close tend to share cultural and institutional traits. These high correlations imply that the joint analysis of deaths and co-residence in a state/country and in its neighboring states/countries is problematic.14 To circumvent this problem we performed regressions substituting an area’s co-residence rate by its neighbors’ average co-residence rates and found that the association between deaths and neighboring co-residence rates ranges from 4% to 5.6 %, depending on the time interval at which deaths were measured. These numbers are not substantially different from the estimates reported in Table 3. We interpret this as additional evidence that co-residence is strongly related to COVID deaths, for average co-residence rates of neighboring states/countries constitute a good proxy for actual co-residence rates. Results are available from the authors upon request.
Discussion of the main findings: Our cross-country and cross-state analysis confirms a finding first reported by Bayer and Kuhn (2020) based on data for 24, mostly European, countries: more people die from Covid where intergenerational co-residence is more common. Our finding is based on regressions controlling for multiple factors that may influence fatalities (their only control variable is an East Asia dummy) and on a larger sample of 79 areas, of which 29 are European countries associated with the UE and 50 are US states. While we find that the association between Covid deaths and intergenerational co-residence across European countries is positive, we find that it is weak and not significant statistically, which is consistent with analyses by Belloc et al. (2020) and Arpino et al. (2020) at either the cross-country level, the European regional level or based on an analysis of Italian regions.
A surprising result is that the positive association between intergenerational co-residence and Covid fatalities is considerably larger in the US than in Europe, and in contrast to our results for European countries, it is statistically significant. This was already apparent from simple correlations presented graphically in Fig. 1B and C. After controlling for many factors likely to influence fatalities from Covid our regression results indicate that across US states cumulative deaths vary positively with share of individuals age 18−34 living with their parents, while this not the case across EU countries. For example, in the US a one extra percentage point in the share of co-residence is associated with an 11.8 percent increase in cumulative deaths from Covid 100 days after the onset of the pandemic in that state
As for the meaning of this positive association between fatalities and intergenerational co-residence, we are reluctant to jump to conclusions about causality based on this limited evidence. A possible interpretation is that when adult children live with their parents this exposes more vulnerable populations to a dangerous virus, but it is certainly premature to conclude that some deaths could be avoided if older adults and their adult children live in separate households rather than share the same residence.
It is possible that more people die from Covid when more young adults live with their parents because this raises the likelihood that a household is exposed to Covid (see Harris, 2020b for some possible evidence about this). If so, we should find that this type of co-residence is also associated with more Covid cases. In Table 6 we present regressions of cumulative cases at the same intervals used in Table 3, Table 4, Table 5: 20, 40, 60, 80 and 100 days after onset in a particular state or country. The magnitude of the coefficients shows that one additional percentage point in the share of co-residents is associated with a 4.6 % increase in the number of cumulative cases 40 days after onset, a 3.5 % increase at 60 days past onset, and a 3% increase at 80 and 100 days after onset.
Table 6.
Log of Cumulative Covid-19 Cases and Intergenerational Co-residence Rates.
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| VARIABLES | Cases20 | Cases40 | Cases60 | Cases80 | Cases100 |
| Co-residence | 0.0394 | 0.0462* | 0.0348* | 0.0306** | 0.0295** |
| (0.0330) | (0.0256) | (0.0178) | (0.0140) | (0.0133) | |
| Observations | 79 | 79 | 79 | 79 | 79 |
| R-squared | 0.431 | 0.291 | 0.567 | 0.789 | 0.845 |
Notes: All other controls reported in Table 3 are included. Robust standard errors in parentheses. *** p < 0.01, ** p < 0.05, * p < 0.1.
Next, we list a number of alternative interpretations of the positive deaths/co-residence association.
First, the association could indicate an income effect not captured by the inclusion of area-level Gross Product and average rent in the regressions. Other income, wealth, or cost-of-living components associated with intergenerational co-residence could simultaneously affect fatalities and co-residence. Lovett et al. (2020) noted the association between multigenerational co-residence and high fatality rates in poverty-stricken parts of the US such as Indian reservations. That many of the US states with above-average co-residence also have above-average state income (as in the case of New Jersey and Connecticut) suggests that poverty is not a major factor here, but the possible association between co-residence and poverty is worthy of further investigation based on more detailed individual or regional data.
Second, intergenerational co-residence may reflect a more widespread presence of active religious communities encouraging physical contacts conducive to the spread of Covid-19. A carefully designed study of 312 areas in Germany with varying proportions of Catholics found that Covid fatalities were higher in areas with higher proportions of Catholics (Laliotis and Minos, 2020). The authors hypothesize that Catholics may have stronger social and family networks, which e.g. may be associated with higher rates of intergenerational co-residence. For example, inter-generational co-residence is more common in predominantly Catholic countries such as Italy and Spain. However, as pointed out by Arpino et al. (2020), some of the lowest case levels of Covid were recorded in Portugal and Slovenia, two other countries where the Catholic Church is the largest Christian denomination. Whether our findings result from differences in religious affiliation is also worthy of further investigation based on more detailed data.15
Third, given the high percentage of the US population that either immigrated or are children of immigrants one may also want to investigate whether our US findings are related to cross-state variation in the presence of immigrants from certain countries, either in the respondents’ generation or in their ancestors’, and frequency of intergenerational co-residence in the countries of emigration.
Fourth, intergenerational co-residence is just one measurable component of the broader concept of intergenerational relationships, as proposed by Arpino et al. (2020). Other components of such intergenerational relationships include geographic proximity, contact frequency and provision of grandchild care. Future research may want to estimate how geographic variations in Covid fatalities also vary with these other dimensions of intergenerational relationships.
Fifth, intergenerational co-residence may indicate psychological dispositions such as perceived sociability, as suggested by Oksanen et al. (2020). They showed that Covid mortality was significantly positively associated with such sociability. It could be that countries with cultures that encourage sociability also have higher rates of intergenerational co-residence. This interpretation is reinforced by Albertini et al. (2020) simulation experiments suggesting that high intergenerational connectedness alone is not sufficient to rapidly contaminate a large fraction of the elderly, and thus cause high fatalities. Only when they introduce social connectedness among the elderly do they find that a virus infects large fractions of the elderly.
Other findings: The regression results reported in Table 3 confirm that extent of testing helps explain variation in deaths from Covid, in line with previous research e.g. by Sung and Kaplan (2020) and Terriau et al. (2020). We find that a 1 percentage point increase in tests per capita 6 days after the epidemic’s onset is associated with a 253 % reduction in fatalities after 20 days. Associations between tests per capita and fatalities become statistically insignificant starting at 40 days past onset. Associations between our measures of lockdown and fatalities are mostly statistically insignificant. As for hospital beds, it also shows a large negative association with deaths at 20 days past onset: the magnitude of the coefficient implies that one more bed per 1000 inhabitants is associated with 36 % fewer Covid deaths 20 days after onset. However, number of beds per capita does not seem to matter much at 40 days or later.
We also include days it took for the epidemic to reach a country or state after the epidemic’s onset in France on February 15 (the variable is called Days Post France in Table 3) and find that once an area has passed 60 days since onset, the more time elapsed between a state or country’s epidemic and the onset in France, the smaller the number of fatalities. At 80 days or 100 days past onset cumulative fatalities are 7.9 % lower for every extra day between the onset in a particular area and the onset in France. This possibly indicates that countries or states that started their COVID pandemic later may have learned considerably from the experience of countries who got hit by the pandemic at an earlier date. For example, they could have adopted better techniques and strategies in taking care of patients, as suggested by Landoni et al. (2020).
Deaths are higher in more urban states or countries 40 days or longer after the local onset of the epidemic. For example, at 40 days after the first death one extra percentage point in percent urban is associated with 2.8 % more cumulative deaths from Covid. As the pandemic progresses urban areas suffer slightly more: 100 days after onset cumulative deaths are 3% higher for every point increase in percent urban.
Not surprisingly, the larger its population the more deaths are recorded in a country or state. As for Gross Domestic Product or Gross State Product, it is associated positively with cumulative deaths for deaths at 20 days (perhaps because people travel more and have more visitors).
4. Conclusion
We find that intergenerational co-residence is associated with a higher number of deaths from Covid using a sample of 29 European countries and 50 US states. This finding is applicable to cross-state comparisons in the US more than to cross-country comparisons in the EU.
If the association is causal, it implies that reductions in such co-residential arrangements may protect an area’s inhabitants from dying of Covid-19. However, we are not able to establish such causality.
Further research is needed that will include better statistics on deaths from Covid, a longer period for the measurement of cumulative deaths, and more countries. It would also be useful to further explore the question we address using more detailed data, such as US counties, European provinces, or other sub-national data.
Footnotes
We thank Jan Fidrmuc, Francois Lagunas, and Joseph Sabia for help in gathering the data, useful comments, and suggestions. We also thank an anonymous referee, Cynthia Bansak, and Maurice Schiff for very helpful comments.
We limited our study to Europe and the USA to minimize the number of unobservables possibly influencing the results. We include 26 of the 28 members of the European Union (Malta and Cyprus were dropped due to missing data). We also include the UK (since it belonged to the EU up to recently), Switzerland (a country associated with the EU through a series of bilateral treaties), and Serbia, currently in negotiations with the EU. Serbia is expected to complete its negotiations by the end of 2024, allowing it to join the Union by 2026. For simplicity we call our sample of European countries EU countries. We are not aware of another Covid study based on pooled data from European countries and US states.
The countries they selected had at least 200 diagnosed cases by March 15, 2020, and include Australia, Austria, Belgium, Canada, Switzerland, Denmark, Spain, France, Germany, Italy, Japan, the Netherlands, Norway, Singapore, South Korea, Sweden, the United Kingdom, and the United States.
The first death from Covid in Europe was recorded in France.
This may be considered as another application of Simpson’s paradox, as pointed out in this twitter thread by Miles Beckett https://twitter.com/mbeckett/status/1278750652160634880.
Based on data from Los Angeles and New Jersey, Harris (2020a) estimates that, on average, it took 16 days from a test-based COVID diagnosis to death. He presumes that during the worst phase of the epidemic in Italy the time from diagnosis to death was shorter (Harris, personal communication). We measure tests 14 days prior to the time we measure deaths, which is reasonable if many of those tested already have severe symptoms. However, if tests are widely available and many of those tested are asymptomatic it may take more than 16 days from test time to death. Results remain invariant when we use 16 days leads in our regressions.
However, intergenerational rural families could also facilitate the spread of Covid. Covid-19 Stalks Large Families in Rural America https://www.wsj.com/articles/Covid-19-households-spread-coronavirus-families-navajo-california-second-wave-11591553896?shareToken=st88d807a0fa83404080f6766404ad8496&reflink=article_email_share
GDP is expressed in dollar terms for both US states and EU countries.
A list of all the countries can be found in the appendix. Two EU countries, Malta and Cyprus, were dropped due to missing data. We include the UK since it belonged to the EU up to recently; Switzerland given its economic associations with major EU countries; and Serbia, as it is likely to join the Union by 2026. For simplicity we call our sample of European countries EU countries.
For more on that topic, see https://analysis.Covid19healthsystem.org/index.php/2020/06/04/how-comparable-is-Covid-19-mortality-across-countries/. According to Coleman et al (2020) statistics on Covid-caused deaths reported by country/state may not be accurate indications of the actual number of deaths due to the Covid virus. Unfortunately, we did not have data on excess mortality for each area in our data set. An example of a study based on excess mortality after Covid limited to a particular country is Laliotis and Minos (2020).
The latest elections were held in Ireland on February 8, 2020, and Slovakia on February 29, 2020. The elections were either pre-Covid or at the very beginning of Covid, so in all cases we classified the government’s leaning in light of the latest election results responsible for the formation of a national government.
We do not include them in the paper since the regressions for EU countries are based on few observations which harms inference. They are available upon request.
We classify various degrees of lockdown and limitations following Olivier Lejeune (https://github.com/OlivierLej/Coronavirus_CounterMeasures).
We thank an anonymous referee for pointing this out.
In the USA official data don’t specify respondents’ religion, so it may be a problem for researchers to analyze this question adequately.
Appendix A. Raw Data
Main variables
| Country/State | Deaths 20 | Deaths 40 | Deaths 60 | Deaths 80 | Deaths 100 | Coresid. Rate |
|---|---|---|---|---|---|---|
| Austria | 146 | 463 | 620 | 668 | 688 | 40.9 |
| Belgium | 1118 | 6327 | 8735 | 9464 | 9704 | 48.5 |
| Bulgaria | 8 | 43 | 91 | 140 | 193 | 59.1 |
| Croatia | 25 | 79 | 99 | 107 | 110 | 75 |
| Czechia | 129 | 240 | 306 | 328 | 349 | 48.5 |
| Denmark | 161 | 403 | 538 | 580 | 603 | 18.8 |
| Estonia | 31 | 55 | 64 | 69 | 69 | 35 |
| Finland | 48 | 211 | 304 | 324 | 328 | 19.7 |
| France | 7 | 1331 | 15,729 | 25,201 | 28,367 | 37.1 |
| Germany | 455 | 4294 | 7369 | 8450 | 8856 | 40.4 |
| Greece | 49 | 116 | 151 | 175 | 189 | 68.1 |
| Hungary | 34 | 262 | 442 | 534 | 573 | 62.7 |
| Ireland | 71 | 687 | 1458 | 1650 | 1714 | 51.5 |
| Italy | 1268 | 13,917 | 25,085 | 30,911 | 33,475 | 66.1 |
| Latvia | 11 | 19 | 24 | 30 | 30 | 46.8 |
| Lithuania | 15 | 45 | 60 | 71 | 78 | 47.6 |
| Luxembourg | 31 | 83 | 103 | 110 | 110 | 46.2 |
| Netherlands | 434 | 3134 | 5168 | 5830 | 6059 | 35.3 |
| Norway | 32 | 163 | 224 | 236 | 244 | 21.3 |
| Poland | 43 | 401 | 811 | 1064 | 1346 | 59.6 |
| Portugal | 311 | 928 | 1203 | 1465 | 1549 | 63.9 |
| Romania | 282 | 744 | 1151 | 1360 | 1651 | 56.8 |
| Serbia | 66 | 173 | 234 | 250 | 270 | 69.6 |
| Slovakia | 18 | 28 | 28 | 28 | 28 | 69.7 |
| Slovenia | 30 | 82 | 103 | 108 | 111 | 59 |
| Spain | 2696 | 17,489 | 25,428 | 28,752 | 27,136 | 62.8 |
| Sweden | 180 | 1580 | 3225 | 4395 | 5053 | 24.1 |
| Switzerland | 103 | 900 | 1476 | 1641 | 1676 | 42.1 |
| United Kingdom | 878 | 14,927 | 29,446 | 37,297 | 41,800 | 36.8 |
| Alabama | 114 | 298 | 551 | 773 | 1006 | 34.8 |
| Alaska | 7 | 8 | 8 | 10 | 14 | 29.5 |
| Arizona | 89 | 308 | 704 | 1052 | 1594 | 32.9 |
| Arkansas | 30 | 76 | 115 | 176 | 279 | 28.0 |
| California | 52 | 725 | 2235 | 3768 | 4986 | 39. 1 |
| Colorado | 80 | 484 | 986 | 1445 | 1647 | 25.4 |
| Connecticut | 277 | 2012 | 3408 | 4055 | 4307 | 40.7 |
| Delaware | 46 | 187 | 332 | 422 | 512 | 38.0 |
| Florida | 29 | 613 | 1470 | 2251 | 2930 | 39.8 |
| Georgia | 154 | 810 | 1420 | 2019 | 2602 | 35.9 |
| Hawaii | 10 | 17 | 17 | 17 | 19 | 33.9 |
| Idaho | 41 | 66 | 79 | 88 | 94 | 27.3 |
| MAIN VARIABLES (CONT.) | ||||||
| Country/State | Deaths 20 | Deaths 40 | Deaths 60 | Deaths 80 | Deaths 100 | Coresid. Rate |
| Illinois | 309 | 1943 | 4149 | 5834 | 7024 | 35.5 |
| Indiana | 151 | 897 | 1691 | 2231 | 2578 | 28.7 |
| Iowa | 44 | 184 | 446 | 650 | 719 | 22.6 |
| Kansas | 11 | 107 | 174 | 211 | 257 | 25.4 |
| Kentucky | 44 | 208 | 343 | 469 | 561 | 28.8 |
| Louisiana | 370 | 1599 | 2381 | 2835 | 3117 | 34.1 |
| Maine | 27 | 62 | 79 | 101 | 109 | 28.4 |
| Maryland | 104 | 945 | 1992 | 2740 | 3142 | 38.3 |
| Massachusetts | 503 | 3405 | 5938 | 7353 | 8060 | 36.2 |
| Michigan | 845 | 3406 | 4891 | 5894 | 6138 | 33.4 |
| Minnesota | 57 | 343 | 786 | 1228 | 1470 | 26.8 |
| Mississippi | 67 | 239 | 528 | 817 | 1035 | 36.7 |
| Missouri | 80 | 296 | 601 | 823 | 1019 | 27.4 |
| Montana | 7 | 16 | 17 | 19 | 23 | 22.7 |
| Nebraska | 24 | 85 | 160 | 226 | 285 | 21.1 |
| Nevada | 46 | 206 | 345 | 429 | 494 | 31.8 |
| New Hampshire | 23 | 84 | 204 | 308 | 373 | 36.6 |
| New Jersey | 199 | 4202 | 9116 | 11,531 | 12,800 | 46.2 |
| New Mexico | 36 | 156 | 317 | 431 | 511 | 34.6 |
| New York | 3716 | 20,212 | 27,448 | 29,847 | 30,934 | 38.5 |
| North Carolina | 116 | 454 | 771 | 1135 | 1413 | 31.6 |
| North Dakota | 9 | 31 | 54 | 77 | 89 | 14.5 |
| Ohio | 213 | 937 | 1720 | 2404 | 2807 | 31.0 |
| Oklahoma | 79 | 207 | 288 | 348 | 384 | 26.7 |
| Oregon | 22 | 83 | 134 | 157 | 192 | 25.5 |
| Pennsylvania | 241 | 1946 | 4504 | 5986 | 6625 | 35.5 |
| Rhode Island | 118 | 388 | 655 | 865 | 960 | 40.3 |
| South Carolina | 44 | 166 | 380 | 525 | 683 | 34.8 |
| South Dakota | 1 | 7 | 34 | 59 | 78 | 21.1 |
| Tennessee | 104 | 200 | 309 | 430 | 585 | 30.7 |
| Texas | 136 | 662 | 1300 | 1793 | 2292 | 35.4 |
| Utah | 18 | 46 | 92 | 128 | 172 | 28.1 |
| Vermont | 23 | 46 | 54 | 55 | 56 | 27.9 |
| Virginia | 46 | 375 | 927 | 1407 | 1620 | 32.0 |
| Washington | 83 | 456 | 805 | 1042 | 1168 | 25.4 |
| West Virginia | 18 | 52 | 74 | 88 | 95 | 31.4 |
| Wisconsin | 107 | 300 | 459 | 648 | 786 | 26.7 |
| Wyoming | 7 | 12 | 18 | 20 | 25 | 23.2 |
Control variables
| Country/State | Date 1 st death | Days 1 st death in France | Day lock-down | Beds | Population | GDP pc | % over 65 | Leftist gov. | % Urban |
|---|---|---|---|---|---|---|---|---|---|
| Austria | 13/03 | 27 | 0 | 7.37 | 8,858,775 | 51,500 | 0.188 | 0 | 57.4 |
| Belgium | 12/03 | 26 | 7 | 5.76 | 11,455,519 | 47,472 | 0.189 | 0 | 97.7 |
| Bulgaria | 12/03 | 26 | 0 | 7.45 | 7,000,039 | 9272 | 0.213 | 0 | 72.3 |
| Croatia | 25/03 | 39 | 0 | 5.54 | 4,076,246 | 14,915 | 0.206 | 0 | 55.2 |
| Czechia | 24/03 | 37 | 0 | 6.63 | 10,649,800 | 23,069 | 0.196 | 0 | 73.3 |
| Denmark | 16/03 | 30 | 0 | 2.61 | 5,806,081 | 61,391 | 0.196 | 1 | 86.8 |
| Estonia | 26/03 | 40 | 0 | 4.69 | 1,324,820 | 23,247 | 0.198 | 0 | 68.1 |
| Finland | 22/03 | 36 | 0 | 3.28 | 5,517,919 | 50,175 | 0.218 | 1 | 83.8 |
| France | 15/02 | 0 | 31 | 5.98 | 67,012,883 | 41,470 | 0.201 | 0 | 78.4 |
| Germany | 10/03 | 24 | 0 | 8.00 | 83,019,213 | 47,616 | 0.215 | 0 | 77 |
| Greece | 12/03 | 26 | 11 | 4.21 | 10,724,599 | 20,317 | 0.220 | 0 | 76.3 |
| Hungary | 16/03 | 30 | 12 | 7.02 | 9,772,756 | 16,151 | 0.193 | 0 | 68.9 |
| Ireland | 12/03 | 26 | 16 | 2.96 | 4,904,240 | 78,583 | 0.141 | 0 | 61.5 |
| Italy | 23/02 | 8 | 19 | 3.18 | 60,359,546 | 34,489 | 0.228 | 1 | 68.3 |
| Latvia | 04/04 | 49 | 0 | 5.57 | 1,919,968 | 17,855 | 0.203 | 0 | 67.8 |
| Lithuania | 21/03 | 35 | 0 | 6.56 | 2,794,184 | 19,071 | 0.198 | 0 | 66.8 |
| Luxembourg | 15/03 | 29 | 1 | 4.66 | 613,894 | 116,597 | 0.144 | 1 | 88.5 |
| Netherlands | 07/03 | 21 | 0 | 3.32 | 17,282,163 | 53,022 | 0.192 | 0 | 87.1 |
| Norway | 13/03 | 27 | 0 | 3.60 | 5,328,212 | 81,734 | 0.172 | 0 | 79.1 |
| CONTROL VARIABLES (CONT.) | |||||||||
| Country/State | Date 1 st death | Days 1 st death in France | Day lock-down | beds | Population | GDP pc | % over 65 | Leftist gov. | % Urban |
| Poland | 13/03 | 27 | 12 | 6.62 | 37,972,812 | 15,422 | 0.177 | 0 | 60.9 |
| Portugal | 18/03 | 32 | 0 | 3.39 | 10,276,617 | 23,403 | 0.218 | 1 | 60.6 |
| Romania | 23/03 | 37 | 2 | 6.89 | 19,414,458 | 12,306 | 0.185 | 0 | 53.8 |
| Serbia | 21/03 | 35 | 0 | 5.61 | 6,963,764 | 7246 | 0.204 | 0 | 55 |
| Slovakia | 07/04 | 52 | 1 | 5.82 | 5,450,421 | 19,444 | 0.160 | 0 | 54.7 |
| Slovenia | 18/03 | 32 | 0 | 4.50 | 2,080,908 | 26,042 | 0.198 | 0 | 52.7 |
| Spain | 05/03 | 19 | 11 | 2.97 | 46,937,060 | 30,324 | 0.194 | 1 | 78.4 |
| Sweden | 12/03 | 26 | 0 | 2.22 | 10,230,185 | 54,651 | 0.199 | 1 | 85.1 |
| Switzerland | 06/03 | 20 | 0 | 4.53 | 8,544,527 | 82,829 | 0.185 | 0 | 73.6 |
| United Kingdom | 07/03 | 21 | 0 | 2.54 | 66,647,112 | 42,962 | 0.184 | 0 | 81.3 |
| Alabama | 25/03 | 39 | 10 | 3.10 | 3,683,315 | 45,219 | 0.170 | 0 | 59 |
| Alaska | 27/03 | 41 | 1 | 2.50 | 527,644 | 73,205 | 0.119 | 0 | 66 |
| Arizona | 20/03 | 34 | 11 | 2.00 | 5,373,653 | 48,055 | 0.176 | 0 | 89.8 |
| Arkansas | 24/03 | 38 | 0 | 3.20 | 2,228,521 | 42,454 | 0.168 | 0 | 56.2 |
| California | 04/03 | 18 | 13 | 1.90 | 29,770,454 | 74,205 | 0.143 | 1 | 95 |
| Colorado | 12/03 | 26 | 14 | 1.90 | 4,311,330 | 63,882 | 0.142 | 1 | 86.2 |
| Connecticut | 18/03 | 32 | 5 | 2.00 | 2,726,056 | 76,342 | 0.172 | 1 | 88 |
| CONTROL VARIABLES (CONT.) | |||||||||
| Country/State | Date 1 st death | Days 1 st death in France | Day lock-down | Beds | Population | GDP pc | % over 65 | Leftist gov. | % Urban |
| Delaware | 26/03 | 40 | −2 | 2.20 | 739,890 | 77,253 | 0.187 | 1 | 83.3 |
| Florida | 06/03 | 20 | 28 | 2.60 | 16,652,573 | 48,318 | 0.205 | 0 | 91.2 |
| Georgia | 12/03 | 26 | 22 | 2.40 | 7,756,469 | 55,832 | 0.138 | 0 | 75.1 |
| Hawaii | 31/03 | 45 | −6 | 1.80 | 1,075,189 | 64,096 | 0.184 | 1 | 91.9 |
| Idaho | 26/03 | 40 | −1 | 2.00 | 1,279,758 | 43,430 | 0.159 | 0 | 70.6 |
| Illinois | 17/03 | 31 | 4 | 2.50 | 9,592,941 | 67,268 | 0.156 | 1 | 88.5 |
| Indiana | 16/03 | 30 | 9 | 2.60 | 4,943,116 | 55,172 | 0.157 | 0 | 72.4 |
| Iowa | 24/03 | 38 | 0 | 3.00 | 2,327,434 | 59,977 | 0.170 | 0 | 64 |
| Kansas | 12/03 | 26 | 18 | 3.40 | 2,128,525 | 56,334 | 0.159 | 1 | 74.2 |
| Kentucky | 16/03 | 30 | 0 | 3.20 | 3,332,232 | 46,898 | 0.164 | 1 | 58.4 |
| Louisiana | 14/03 | 28 | 9 | 3.30 | 3,435,023 | 53,589 | 0.155 | 1 | 73.2 |
| Maine | 27/03 | 41 | 6 | 2.50 | 1,055,182 | 47,969 | 0.206 | 1 | 38.7 |
| Maryland | 18/03 | 32 | 12 | 1.90 | 4,567,060 | 68,573 | 0.154 | 0 | 87.2 |
| Massachusetts | 20/03 | 34 | 5 | 2.30 | 5,291,844 | 82,480 | 0.165 | 0 | 92 |
| Michigan | 18/03 | 32 | 7 | 2.50 | 7,612,607 | 53,209 | 0.172 | 1 | 74.6 |
| Minnesota | 21/03 | 35 | 7 | 2.50 | 4,181,203 | 64,675 | 0.158 | 1 | 73.3 |
| Mississippi | 19/03 | 33 | 15 | 4.10 | 2,184,974 | 37,948 | 0.159 | 0 | 49.4 |
| Missouri | 18/03 | 32 | 20 | 3.10 | 4,578,406 | 51,699 | 0.169 | 0 | 70.4 |
| Montana | 27/03 | 41 | 2 | 3.50 | 804,931 | 46,609 | 0.188 | 1 | 55.9 |
| CONTROL VARIABLES (CONT.) | |||||||||
| Country/State | Date 1 st death | Days 1 st death in France | Day lock-down | Beds | Population | GDP pc | % over 65 | Leftist gov. | % Urban |
| Nebraska | 27/03 | 41 | 0 | 3.60 | 1,405,515 | 63,942 | 0.158 | 0 | 73.1 |
| Nevada | 16/03 | 30 | 16 | 2.10 | 2,309,016 | 55,269 | 0.157 | 1 | 94.2 |
| New Hampshire | 23/03 | 37 | 5 | 2.10 | 1,056,256 | 63,067 | 0.181 | 0 | 60.3 |
| New Jersey | 10/03 | 24 | 11 | 2.40 | 6,779,523 | 69,378 | 0.161 | 1 | 94.7 |
| New Mexico | 25/03 | 39 | −1 | 1.80 | 1,573,961 | 46,954 | 0.176 | 1 | 77.4 |
| New York | 14/03 | 28 | 8 | 2.60 | 14,927,812 | 85,746 | 0.164 | 1 | 87.9 |
| North Carolina | 25/03 | 39 | 5 | 2.10 | 7,816,396 | 54,441 | 0.163 | 1 | 66.1 |
| North Dakota | 27/03 | 41 | 0 | 4.30 | 560,687 | 72,597 | 0.153 | 0 | 59.9 |
| Ohio | 20/03 | 34 | 4 | 2.90 | 8,788,823 | 57,492 | 0.171 | 0 | 77.9 |
| Oklahoma | 19/03 | 33 | 11 | 2.90 | 2,879,339 | 50,613 | 0.157 | 0 | 66.2 |
| Oregon | 14/03 | 28 | 9 | 1.70 | 3,233,678 | 56,956 | 0.176 | 1 | 81 |
| Pennsylvania | 18/03 | 32 | 14 | 2.90 | 9,750,990 | 61,594 | 0.182 | 1 | 78.7 |
| Rhode Island | 28/03 | 42 | 0 | 2.00 | 812,775 | 57,852 | 0.173 | 1 | 90.7 |
| South Carolina | 16/03 | 30 | 22 | 2.60 | 3,846,959 | 45,280 | 0.177 | 0 | 66.3 |
| South Dakota | 10/03 | 24 | 0 | 4.80 | 635,152 | 58,624 | 0.166 | 0 | 56.7 |
| Tennessee | 21/03 | 35 | 11 | 3.00 | 5,106,473 | 53,933 | 0.163 | 0 | 66.4 |
| Texas | 16/03 | 30 | 18 | 2.40 | 20,718,514 | 61,167 | 0.125 | 0 | 84.7 |
| Utah | 22/03 | 36 | 12 | 1.90 | 2,184,156 | 55,550 | 0.111 | 0 | 90.6 |
| Vermont | 19/03 | 33 | 6 | 2.00 | 485,556 | 53,523 | 0.198 | 0 | 38.9 |
| CONTROL VARIABLES (CONT.) | |||||||||
| Country/State | Date 1 st death | Days 1 st death in France | Day lock-down | Beds | Population | GDP pc | % over 65 | Leftist gov. | % Urban |
| Virginia | 14/03 | 28 | 16 | 2.20 | 6,408,308 | 62,563 | 0.155 | 1 | 75.5 |
| Washington | 29/02 | 14 | 23 | 1.70 | 5,734,478 | 74,182 | 0.154 | 1 | 84.1 |
| West Virginia | 29/03 | 43 | −5 | 3.80 | 1,396,570 | 43,053 | 0.200 | 0 | 48.7 |
| Wisconsin | 19/03 | 33 | 6 | 2.10 | 4,398,813 | 57,720 | 0.170 | 1 | 70.2 |
| Wyoming | 13/04 | 58 | −16 | 3.60 | 431,046 | 69,900 | 0.167 | 0 | 64.8 |
Number of tests per capita
| Country/State | Tests pc 6 | Tests pc 26 | Tests pc 46 | Tests pc 66 | Tests pc 86 |
|---|---|---|---|---|---|
| Austria | 0.002 | 0.014 | 0.027 | 0.041 | 0.055 |
| Belgium | 0.001 | 0.007 | 0.020 | 0.049 | 0.065 |
| Bulgaria | 0.001 | 0.002 | 0.006 | 0.009 | 0.013 |
| Croatia | 0.002 | 0.007 | 0.011 | 0.016 | 0.018 |
| Czechia | 0.004 | 0.016 | 0.028 | 0.041 | 0.048 |
| Denmark | 0.002 | 0.013 | 0.046 | 0.088 | 0.130 |
| Estonia | 0.012 | 0.033 | 0.049 | 0.064 | 0.078 |
| Finland | 0.004 | 0.011 | 0.022 | 0.033 | 0.041 |
| France | 0.000 | 0.000 | 0.004 | 0.009 | 0.009 |
| Germany | 0.004 | 0.017 | 0.029 | 0.042 | 0.055 |
| Greece | 0.001 | 0.003 | 0.006 | 0.012 | 0.020 |
| Hungary | 0.000 | 0.003 | 0.008 | 0.015 | 0.022 |
| Ireland | 0.001 | 0.010 | 0.030 | 0.059 | 0.074 |
| Italy | 0.000 | 0.003 | 0.014 | 0.027 | 0.042 |
| Latvia | 0.014 | 0.030 | 0.048 | 0.063 | 0.077 |
| Lithuania | 0.002 | 0.017 | 0.056 | 0.098 | 0.131 |
| Luxembourg | 0.009 | 0.048 | 0.075 | 0.106 | 0.158 |
| Netherlands | 0.001 | 0.005 | 0.011 | 0.016 | 0.021 |
| Norway | 0.009 | 0.019 | 0.028 | 0.038 | 0.046 |
| Poland | 0.000 | 0.003 | 0.008 | 0.016 | 0.027 |
| Portugal | 0.003 | 0.019 | 0.045 | 0.073 | 0.097 |
| Romania | 0.001 | 0.005 | 0.012 | 0.021 | 0.030 |
| Serbia | 0.000 | 0.004 | 0.017 | 0.032 | 0.044 |
| Slovakia | 0.006 | 0.018 | 0.029 | 0.036 | 0.039 |
| Slovenia | 0.008 | 0.017 | 0.027 | 0.036 | 0.042 |
| Spain | 0.003 | 0.013 | 0.021 | 0.037 | 0.056 |
| Sweden | 0.002 | 0.006 | 0.012 | 0.021 | 0.031 |
| Switzerland | 0.002 | 0.017 | 0.028 | 0.037 | 0.047 |
| United Kingdom | 0.001 | 0.003 | 0.009 | 0.027 | 0.051 |
| Alabama | 0.002 | 0.012 | 0.035 | 0.058 | 0.090 |
| Alaska | 0.010 | 0.023 | 0.057 | 0.103 | 0.167 |
| Arizona | 0.000 | 0.008 | 0.016 | 0.035 | 0.063 |
| Arkansas | 0.003 | 0.011 | 0.029 | 0.054 | 0.103 |
| California | 0.000 | 0.003 | 0.010 | 0.031 | 0.062 |
| Colorado | 0.000 | 0.006 | 0.015 | 0.029 | 0.048 |
| Connecticut | 0.002 | 0.016 | 0.038 | 0.076 | 0.127 |
| Delaware | 0.006 | 0.021 | 0.043 | 0.082 | 0.125 |
| Florida | 0.000 | 0.004 | 0.017 | 0.034 | 0.061 |
| Georgia | 0.000 | 0.004 | 0.016 | 0.045 | 0.067 |
| Hawaii | 0.013 | 0.026 | 0.038 | 0.049 | 0.067 |
| Idaho | 0.005 | 0.014 | 0.025 | 0.036 | 0.056 |
| Illinois | 0.001 | 0.011 | 0.031 | 0.073 | 0.117 |
| Indiana | 0.000 | 0.008 | 0.020 | 0.041 | 0.065 |
| Iowa | 0.003 | 0.011 | 0.031 | 0.063 | 0.104 |
| NUMBER OF TESTS PER CAPITA (CONT.) | |||||
| Country/State | Tests pc 6 | Tests pc 16 | Tests pc 26 | Tests pc 36 | Tests pc 46 |
| Kansas | 0.000 | 0.004 | 0.013 | 0.029 | 0.053 |
| Kentucky | 0.000 | 0.007 | 0.017 | 0.048 | 0.082 |
| Louisiana | 0.000 | 0.025 | 0.046 | 0.081 | 0.129 |
| Maine | 0.006 | 0.017 | 0.022 | 0.047 | 0.077 |
| Maryland | 0.000 | 0.011 | 0.029 | 0.051 | 0.088 |
| Massachusetts | 0.004 | 0.025 | 0.063 | 0.102 | 0.135 |
| Michigan | 0.002 | 0.013 | 0.032 | 0.068 | 0.103 |
| Minnesota | 0.003 | 0.011 | 0.025 | 0.057 | 0.101 |
| Mississippi | 0.001 | 0.017 | 0.036 | 0.063 | 0.098 |
| Missouri | 0.000 | 0.010 | 0.018 | 0.032 | 0.058 |
| Montana | 0.007 | 0.014 | 0.029 | 0.051 | 0.087 |
| Nebraska | 0.003 | 0.012 | 0.034 | 0.074 | 0.110 |
| Nevada | 0.001 | 0.010 | 0.019 | 0.041 | 0.081 |
| New Hampshire | 0.005 | 0.012 | 0.030 | 0.062 | 0.095 |
| New Jersey | 0.000 | 0.012 | 0.032 | 0.068 | 0.127 |
| New Mexico | 0.008 | 0.024 | 0.062 | 0.120 | 0.178 |
| New York | 0.002 | 0.026 | 0.058 | 0.098 | 0.171 |
| North Carolina | 0.003 | 0.010 | 0.025 | 0.052 | 0.091 |
| North Dakota | 0.009 | 0.028 | 0.085 | 0.131 | 0.172 |
| Ohio | 0.002 | 0.008 | 0.018 | 0.038 | 0.062 |
| Oklahoma | 0.000 | 0.010 | 0.022 | 0.056 | 0.086 |
| Oregon | 0.001 | 0.008 | 0.017 | 0.031 | 0.046 |
| Pennsylvania | 0.001 | 0.013 | 0.025 | 0.040 | 0.058 |
| Rhode Island | 0.008 | 0.053 | 0.105 | 0.144 | 0.177 |
| South Carolina | 0.000 | 0.008 | 0.015 | 0.036 | 0.066 |
| South Dakota | 0.001 | 0.009 | 0.025 | 0.043 | 0.083 |
| Tennessee | 0.003 | 0.017 | 0.044 | 0.079 | 0.123 |
| Texas | 0.000 | 0.006 | 0.017 | 0.036 | 0.056 |
| Utah | 0.005 | 0.026 | 0.062 | 0.092 | 0.126 |
| Vermont | 0.004 | 0.021 | 0.035 | 0.059 | 0.103 |
| Virginia | 0.000 | 0.005 | 0.014 | 0.032 | 0.060 |
| Washington | 0.000 | 0.012 | 0.025 | 0.039 | 0.054 |
| West Virginia | 0.006 | 0.021 | 0.049 | 0.074 | 0.111 |
| Wisconsin | 0.002 | 0.010 | 0.021 | 0.046 | 0.094 |
| Wyoming | 0.017 | 0.028 | 0.054 | 0.084 | 0.088 |
References
- Abdulamir A.S., Hafidh R.R. The possible immunological pathways for the variable immunopathogenesis of COVID--19 infections among healthy adults, elderly and children. Electron. J. Gen. Med. 2020;17(4) [Google Scholar]
- Albertini M., Sage L., Scherer S. University of Bologna; WP: 2020. Intergenerational Contacts and Covid-19 Spread: Omnipresent Grannies or Bowling Together? [Google Scholar]
- Arpino B., Bordone V., Pasqualini M. 2020. Are Intergenerational Relationships Responsible for More COVID-19 Cases? A Cautionary Tale of Available Empirical Evidence. SocArXiv, May 6. [DOI] [Google Scholar]
- Baker G. Federalism makes the US unique in its pandemic response. Wall Street J. 2020;30-31:C2. May. [Google Scholar]
- Bayer Christian, Kuhn Moritz. 2020. Intergenerational Ties and Case Fatality Rates: A Cross-Country Analysis. IZA DP No. 13114, April. [Google Scholar]
- Belloc M., Buonanno P., Drago F., Galbiati R., Pinotti P. Cross-country correlation analysis for research on COVID-19. Vox-CEPR Policy Portal. 2020 https://voxeu.org/article/cross-country-correlation-analysis-research-Covid-19 Accessed on June 29, 2020. [Google Scholar]
- Coleman M.P., Di Carlo V., Ashton J.R., Pollock A., Matz M., Allemani C. Reliable, real-world data on excess mortality are required to assess the impact of Covid-19. TheBMJ. 2020 May 7. [Google Scholar]
- Florida Richard. The geography of coronavirus. Bloomberg City Lab. 2020 April 3. [Google Scholar]
- Friedson A., McNichols D., Sabia J., Dave D. 2020. Did California’s Shelter-in-Place Order Work? Early Coronavirus-Related Public Health Benefits. NBER Working Paper w26992, April. [Google Scholar]
- Harris J.E. 2020. Reopening Under COVID-19: What to Watch For. NBER Working Paper No. 27166, May. [Google Scholar]
- Harris J.E. 2020. Data From the COVID-19 Epidemic in Florida suggest That Younger Cohorts Have Been Transmitting Their Infections to Less Socially Mobile Older Adults, Review of Economics of the Household, On-line-first. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber M., Langen H. 2020. The Impact of Response Measures on COVID-19-Related Hospitalization and Death Rates in Germany and Switzerland. arXiv:2005.11278 [q-bio.PE] Last revised May 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh D. Occupational risks for COVID-19 infection. Occupational med. (Oxford, England) 2020;70(1):3. doi: 10.1093/occmed/kqaa036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laliotis I., Minos D. Spreading the disease: the role of culture. COVID Econ. 2020;40:180–210. [Google Scholar]
- Landoni G., Losi D., Fresilli S., Lazzari S., Nardelli P., Puglisi R., Zangrillo A. Is time our ultimate ally in defying the pandemic? Pathog. Glob. Health. 2020 doi: 10.1080/20477724.2020.1785199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovett I., Frosch D., Overberg P. Covid-19 stalks large families in Rural America. Wall Street J. 2020 https://www.wsj.com/articles/Covid-19-households-spread-coronavirus-families-navajo-california-second-wave-11591553896?shareToken=st88d807a0fa83404080f6766404ad8496&reflink=article_email_share June 7. [Google Scholar]
- Miron J. Spatial Statistics and Models. Springer; Dordrecht: 1984. Spatial autocorrelation in regression analysis: a beginner’s guide; pp. 201–222. [Google Scholar]
- Oksanen A., Kaakinen M., Latikka R., Savolainen L., Savela L., Koivula A. Regulation and trust: 3-Month follow-up study on COVID-19 mortality in 25 european countries. JMIR Public Health Surveill. 2020;6(2):e19218. doi: 10.2196/19218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oster Emily Oster. Unobservable selection and coefficient stability: theory and evidence. J. Bus. Econ. Stat. 2019;37(2):187–204. doi: 10.1080/07350015.2016.1227711. [DOI] [Google Scholar]
- Sorci G., Faivre B., Morand S. Why does COVID-19 case fatality rate vary among countries? medRxiv preprint. 2020 doi: 10.1038/s41598-020-75848-2. doi: https://www.medrxiv.org/content/10.1101/2020.04.17.20069393v1 version posted onJune 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung W.Y.Y., Kaplan R.M. Why do countries’ COVID-19 death rates vary so much? Medpage Today. 2020 https://www.medpagetoday.com/infectiousdisease/Covid19/86527 May 15. [Google Scholar]
- Wu J.T., Leung K., Bushman M., Kishore N., Niehus R., de Salazar P.M., Cowling B.J., Lipsitch M., Leung G.M. Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan, China. Nat. Med. 2020;26(4):506–510. doi: 10.1038/s41591-020-0822-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Peng F., Wang R., Guan K., Jiang T., Xu G., Sun J., Chang C. The deadly coronaviruses: the 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. J. Autoimmun. 2020;109 doi: 10.1016/j.jaut.2020.102434. May. [DOI] [PMC free article] [PubMed] [Google Scholar]