Abstract
Background:
Inconsistent results have been obtained regarding postoperative pain control using local infiltration and epidural analgesia for patients after total knee or hip arthroplasty (TKA and THA). We therefore conducted a meta-analysis of randomized controlled trials (RCTs) to assess the efficacy and safety of local infiltration vs epidural analgesia for TKA and THA.
Methods:
Electronic searches were conducted on PubMed, EmBase, and the Cochrane library to identify eligible RCTs conducted up to February 2020. Weighted mean difference (WMD) and relative risk with 95% confidence interval (95%CI) were applied to calculate pooled effect estimates between local infiltration and epidural analgesia using the random-effects model.
Results:
Seven RCTs including a total of 412 TKA patients, and three RCTs including a total of 200 THA patients were selected for this meta-analysis. We noted that local infiltration was associated with lower visual analog scale (VAS) scores at rest after 48 hours (WMD: −1.31; 95%CI: −2.44 to −0.18; P = .024) and 72 hours (WMD: −0.95; 95%CI: −1.39 to −0.52; P < .001) for patients with TKA, while local infiltration significantly reduced VAS scores at rest after 12 hours for patients with THA (WMD: −1.00; 95%CI: −1.49 to −0.51; P < .001). Moreover, local infiltration was associated with lower VAS scores during movement after 48 hours in TKA patients (WMD: −1.08; 95%CI: −1.86 to −0.29; P = .007), while there were higher VAS scores during movement after 24 hours for patients with THA (WMD: 1.06; 95%CI: 0.67 to 1.45; P < .001). Furthermore, we noted that local infiltration was associated with higher flexion angles compared with epidural analgesia after 24 hours (WMD: 7.11; 95%CI: 2.30–11.93; P = .004), 48 hours (WMD: 6.69; 95%CI: 3.78 to 9.59; P < .001), and 72 hours (WMD: 5.19; 95%CI: 0.95–9.44; P = .016). There were no significant differences between local infiltration and epidural analgesia for the length of hospital stay, nausea, or wound infection.
Conclusions:
Local infiltration is superior to epidural analgesia for postoperative pain control after TKA, whereas for THA patients inconsistent results were obtained at various times.
Keywords: analgesia, arthroplasty, epidural, hip, knee, meta-analysis, pain, postoperative, replacement
1. Introduction
Total joint arthroplasty is a common orthopedic operation, and total knee arthroplasty (TKA) and total hip arthroplasty (THA) are 2 types of successful surgical intervention for improving the quality of life of patients with end-stage osteoarthritis.[1,2] The rates of TKA and THA are increasing worldwide, by an estimated 100% and 30% between 2000 and 2015, respectively, and the rate is expected to increase 4-fold by 2030.[3,4] Although the overall patient satisfaction is high for patients after TKA and THA, these patients often experience severe pain. Therefore, effective pain control plays an important role in early ambulation and results in better functional outcomes.[5] Moreover, effective pain control could increase overall patient satisfaction and decrease the economic costs owing to shorter hospital stays.[6,7]
Epidural infusion using catheters placed on the subarachnoid space and the peripheral nerves are widely used for patients with acute or chronic pain.[8] Continuous epidural infusion is an effective approach for postoperative pain control and applies low doses of medication, which reduces the potential adverse events.[8] However, the benefits of epidural infusion are balanced by the increased risks of urinary retention, hypotension, pruritus, and motor block.[9,10] Currently, local infiltration containing various constituents are widely used for postoperative pain control, giving sufficient pain control without interfering with lower extremity motor strength.[11] The use of local infiltration to the surgical site could therefore achieve effective analgesia for the treatment of postoperative pain.[12] However, inconsistent results have been observed regarding postoperative pain control after TKA and THA between local infiltration and epidural analgesia. Therefore, we conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) to assess the efficacy and safety of local infiltration vs epidural analgesia for patients after TKA or THA.
2. Methods
2.1. Ethics approval
Not applicable for a meta-analysis study.
2.2. Search strategy and selection criteria
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis Statement was applied to guide this systematic review and meta-analysis.[13] Studies designed as RCTs and ones that compared the treatment effectiveness between local infiltration and epidural analgesia after TKA or THA were included in this study. We systematically searched the PubMed, EmBase, and the Cochrane library to identify trials conducted up to February 2020, using the following core terms: “local infiltration” OR “periarticular injection” OR “intra-articular injection” AND “knee arthroplasty” OR “knee replacement” OR “hip arthroplasty” OR “hip replacement.” Studies that had been completed but not yet published were searched from the website http://clinicaltrials.gov/ (US NIH) and the meta Register of Controlled Trials. We also reviewed the reference lists of the identified studies to identify any new RCTs that met the inclusion criteria.
The details regarding the inclusion criteria were as follows:
-
(1)
Patients: after TKA or THA;
-
(2)
Intervention: local infiltration;
-
(3)
Control: epidural analgesia;
-
(4)
Outcomes: visual analog scale (VAS) score at rest or during movement after 12 hours, 24 hours, 48 hours, and 72 hours; flexion angle after 24 hours, 48 hours, and 72 hours; length of hospital stay, nausea, and wound infection; and
-
(5)
Study design: RCT.
The study selection process was carried out by 2 reviewers, and any conflict between the 2 reviewers was resolved by an additional reviewer's evaluation of the full-text of the article.
2.3. Data collection and quality assessment
The following information was abstracted independently by 2 reviewers: first author's name, publication year, country, sample size, percentage male, mean age, type of operation, anesthesia, intervention, control, and investigated outcomes. Any disagreement between reviewers was settled by discussion until a consensus was reached. The study quality was assessed using the JADAD scale, on the basis of randomization, blinding, allocation concealment, withdrawals and dropouts, and use of intention-to-treat analysis.[14] The scoring system ranged from 0 to 5, and studies scoring 4 or 5 were considered high quality.
2.4. Statistical analysis
The treatment effectiveness between local infiltration and epidural analgesia for VAS score at rest or during movement, flexion angle, and the length of hospital stay were assigned as continuous data, and the weighted mean difference (WMD) with its 95% confidence interval (CI) was calculated for each trial. The risk of nausea and wound infection were assigned as categories data, and relative risk (RR) with 95%CI was calculated for each trial before data pooling. The pooled analyses for investigated outcomes were conducted using the random-effects model.[15,16] Heterogeneity across included studies were assessed by I2 and Q statistics, and significant heterogeneity was defined as I2 > 50% or P < .10.[17,18] Subgroup analyses were also conducted on the basis of time endpoints and the type of operation. Publication biases for investigated outcomes were assessed by Egger and Begg tests.[19,20] The inspection level for pooled results are 2-sided, and P < .05 was regarded as statistically significant. The STATA software (Version 10.0; StataCorp, Texas, United States of America) was applied to conduct all statistical analyses in this study.
3. Results
3.1. Literature search
A total of 1432 records were identified by electronic searches, and 950 studies were retained after duplicate records were excluded. A further 903 studies were excluded because they reported irrelevant titles or were not RCT design. The remaining 47 studies were retrieved for further full-text evaluations, and a total of 10 RCTs were selected for final quantitative analysis.[21–30] No new study met the inclusion criteria by reviewing the reference lists of retrieved studies and the website http://clinicaltrials.gov/ (US NIH) and the meta Register of Controlled Trials (Fig. 1).
Figure 1.
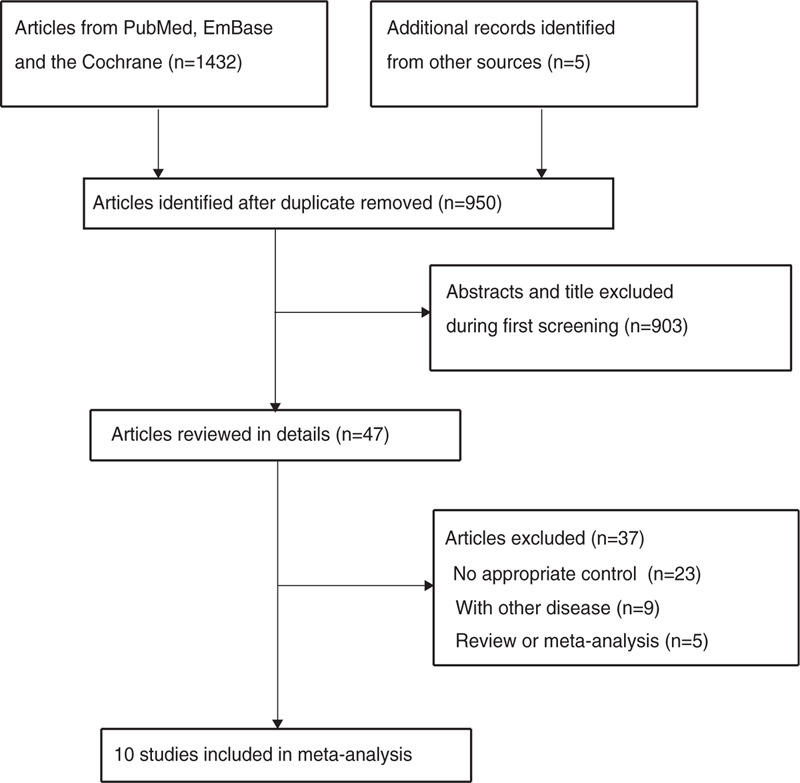
PRISMA flowchart showing the study selection process.
3.2. Study characteristics
The baseline characteristics of the identified studies and included patients are presented in Table 1. Seven of the RCTs included 412 TKA patients, and the remaining 3 trials included 200 THA patients. Nine trials applied spinal anesthesia, and the remaining trial used combined anesthesia. Five studies were conducted in Europe, 3 trials were conducted in Asia, 1 study was conducted in Turkey, and the remaining study was conducted in the USA. Study quality was assessed using the JADAD scale: 2 studies scored 5, 1 study scored 4, 6 studies scored 3, and the remaining study scored 2.
Table 1.
The baseline characteristics of included studies and patients.
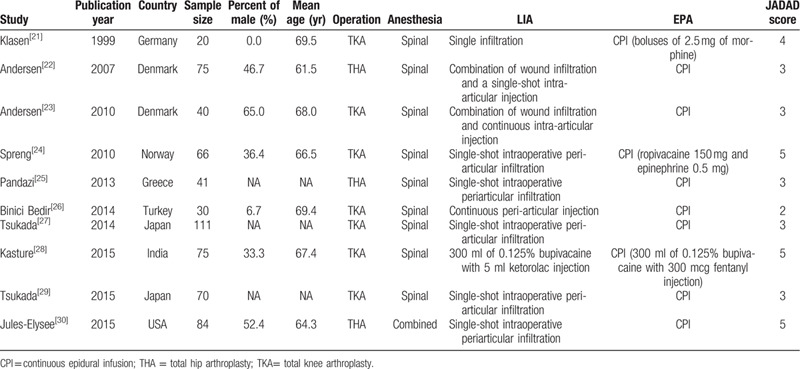
3.3. Visual analog scale scores at rest
The breakdown number of studies for the effects between local infiltration and epidural analgesia in patients after TKA on VAS scores at rest after 12 hours, 24 hours, 48 hours, and 72 hours were 4, 6, 4, and 4, respectively (Fig. 2A). We noted that local infiltration significantly reduced the at rest VAS score after 48 hours (WMD: −1.31; 95%CI: −2.44 to −0.18; P = .024; I2 = 80.5%; Pheterogeneity = .002) and 72 hours (WMD: −0.95; 95%CI: −1.39 to −0.52; P < .001; I2 = 0.0%; Pheterogeneity = .515) compared with epidural analgesia, whereas there were no significant differences between local infiltration and epidural analgesia for at rest VAS scores after 12 hours (WMD: −0.13; 95%CI: −0.92 to 0.66; P = .749; I2 = 63.3%; Pheterogeneity = .043) or 24 hours (WMD: −0.45; 95%CI: −1.21 to 0.31; P = .249; I2 = 87.4%; Pheterogeneity < .001). Furthermore, although the Begg test found no significant publication bias for the at rest VAS score after TKA (P = .495), the Egger test indicated significant publication bias for at rest VAS scores after TKA (P = .008). These conclusions were not altered after adjustment using the trim and fill method.[31]
Figure 2.
Local infiltration vs epidural analgesia on visual analog scale pain scores at rest for total knee arthroplasty (A) and total hip arthroplasty (B) patients.
The breakdown number of studies for the effects between local infiltration and epidural analgesia in patients after THA on at rest VAS score after 12 hours, 24 hours, 48 hours, and 72 hours were 1, 3, 2, and 2, respectively (Fig. 2B). We noted that local infiltration was associated with a lower at rest VAS score after 12 hours (WMD: −1.00; 95%CI: −1.49 to −0.51; P < .001) as compared with epidural analgesia, whereas there were no significant differences between local infiltration and epidural analgesia for at rest VAS scores after 24 hours (WMD: 0.43; 95%CI: −0.24 to 1.10; P = .205; I2 = 73.6%; Pheterogeneity = .023), 48 hours (WMD: −0.63; 95%CI: −1.60 to 0.34; P = .202; I2 = 61.4%; Pheterogeneity = .107), or 72 hours (WMD: −0.62; 95%CI: −1.60 to 0.36; P = .216; I2 = 86.2%; Pheterogeneity = .007). There was no significant publication bias for the at rest VAS scores after THA (PEgger = .824; PBegg = .711).
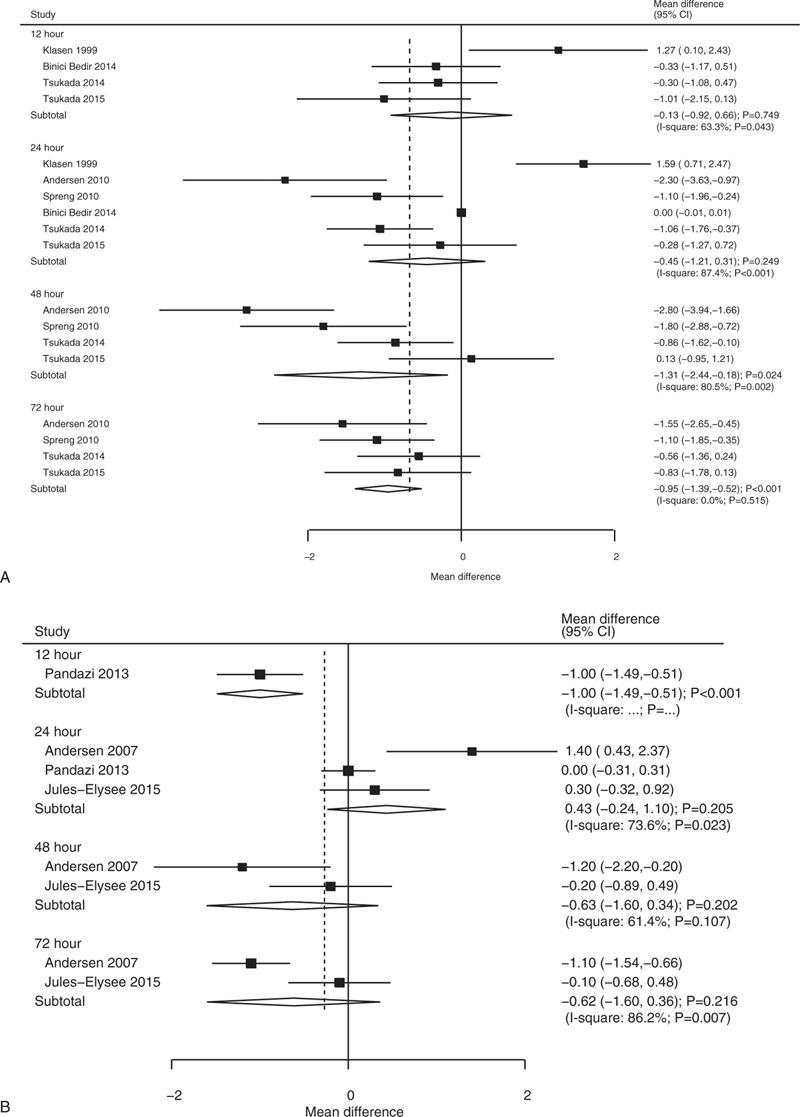
3.4. Visual analog scale scores during movement
The breakdown number of studies for the effects between local infiltration and epidural analgesia in patients after TKA on VAS scores during movement after 24 hours, 48 hours, and 72 hours were 3, 3, and 3, respectively (Fig. 3A). We noted that local infiltration significantly reduced VAS scores during movement after 48 hours (WMD: −1.08; 95%CI: −1.86 to −0.29; P = .007; I2 = 31.9%; Pheterogeneity = .230) compared with epidural analgesia, while there were no significant differences between groups for VAS scores during movement after 24 hours (WMD: −0.56; 95%CI: −1.93 to 0.80; P = .419; I2 = 73.9%; Pheterogeneity = .022) or 72 hours (WMD: −1.25; 95%CI: −2.55 to 0.05; P = .060; I2 = 78.2%; Pheterogeneity = .010). We noted significant publication bias for VAS scores during movement for patients after TKA (PEgger = .015; PBegg = .076). This conclusion was not changed after adjustment using the trim and fill method.[31]
Figure 3.
Local infiltration vs epidural analgesia on visual analog scale pain scores during movement for total knee arthroplasty (A) and total hip arthroplasty (B) patients.
The breakdown number of studies for the effects between local infiltration and epidural analgesia in patients after THA on VAS scores during movement after 24 hours, 48 hours, and 72 hours were 3, 2, and 2, respectively (Fig. 3B). We noted that local infiltration was associated with higher VAS scores during movement after 24 hours (WMD: 1.06; 95%CI: 0.67 to 1.45; P < .001; I2 = 0.0%; Pheterogeneity = .407) compared with epidural analgesia, while there were no significant differences between groups for VAS scores during movement after 48 hours (WMD: −0.33; 95%CI: −2.48 to 1.82; P = .766; I2 = 82.0%; Pheterogeneity = .019) or 72 hours (WMD: −0.99; 95%CI: −3.74 to 1.75; P = .478; I2 = 94.5%; Pheterogeneity < .001). No significant publication bias for VAS scores during movement for patients after THA was detected (PEgger = .247; PBegg = .133).
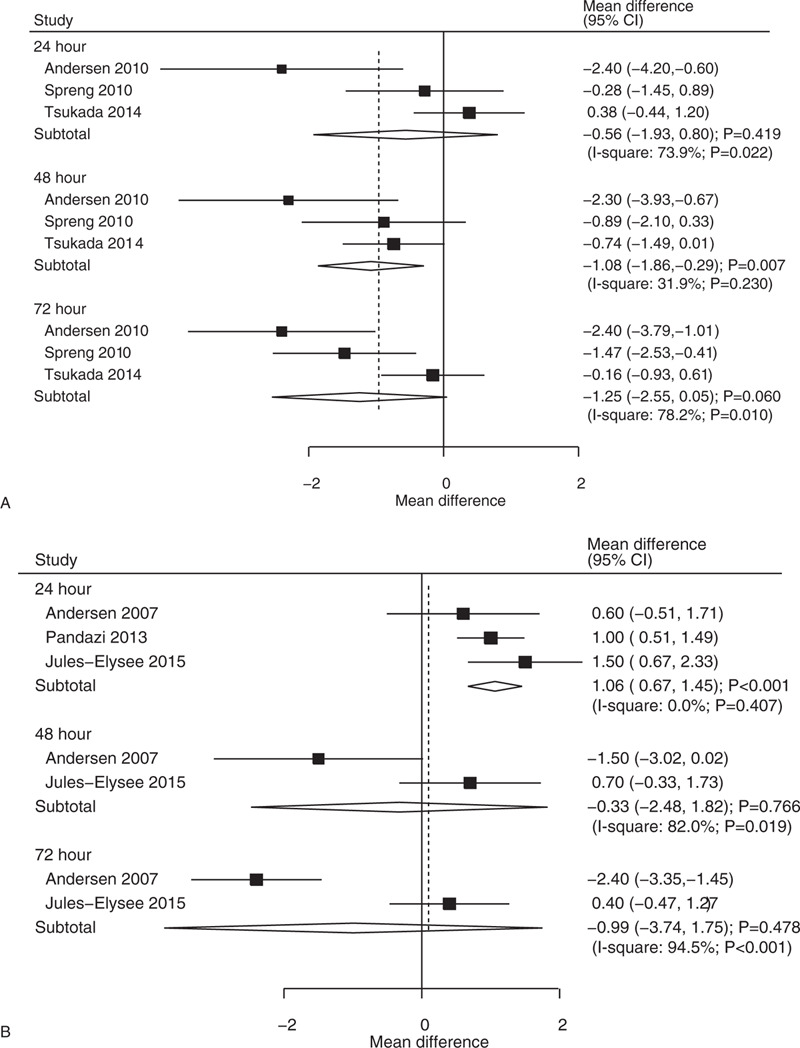
3.5. Flexion angle
The breakdown number of studies for the effects between local infiltration and epidural analgesia in patients after TKA on flexion angle after 24 hours, 48 hours, and 72 hours were 3, 3, and 3, respectively (Fig. 4). We noted local infiltration was associated with higher flexion angles after 24 hours (WMD: 7.11; 95%CI: 2.30–11.93; P = .004; I2 = 28.7%; Pheterogeneity = .246), 48 hours (WMD: 6.69; 95%CI: 3.78–9.59; P < .001; I2 = 0.0%; Pheterogeneity = .754), or 72 hours (WMD: 5.19; 95%CI: 0.95–9.44; P = .016; I2 = 53.9%; Pheterogeneity = .114) compared to epidural analgesia. No significant publication bias for flexion angle for patients after TKA was detected (PEgger = .466; PBegg = .175).
Figure 4.
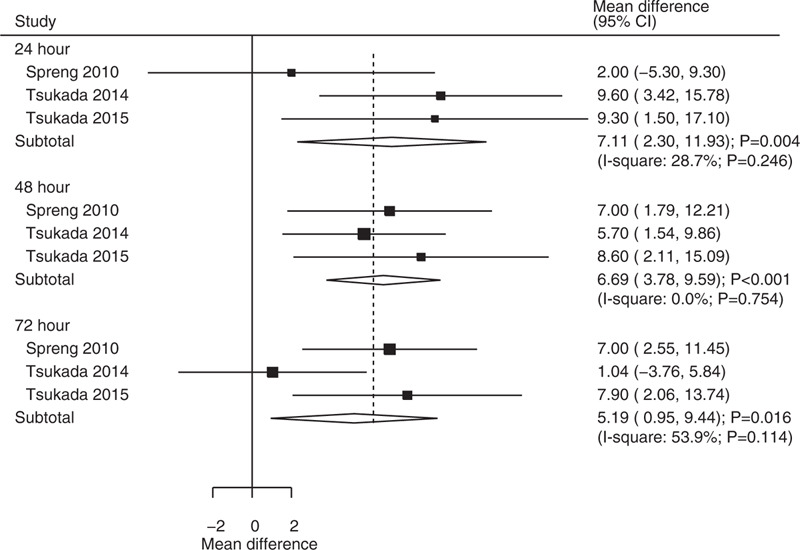
Local infiltration vs epidural analgesia on flexion angles for total knee arthroplasty patients.
3.6. Length of hospital stay
Data for the effect of local infiltration vs epidural analgesia on the length of hospital stay were available in five studies. We noted local infiltration was not associated with the length of hospital stay as compared with epidural analgesia (WMD: −0.83; 95%CI: −1.67 to 0.00; P = .051; I2 = 95.0%; Pheterogeneity < .001; Fig. 5). Subgroup analyses indicated no significant differences between local infiltration and epidural analgesia for patients after TKA (WMD: −0.61; 95%CI: −1.95 to 0.74; P = .376) or THA (WMD: −1.25; 95%CI: −3.55 to 1.06; P = .289). There was no significant publication bias for the length of hospital stay (PEgger = .108; PBegg = .462).
Figure 5.
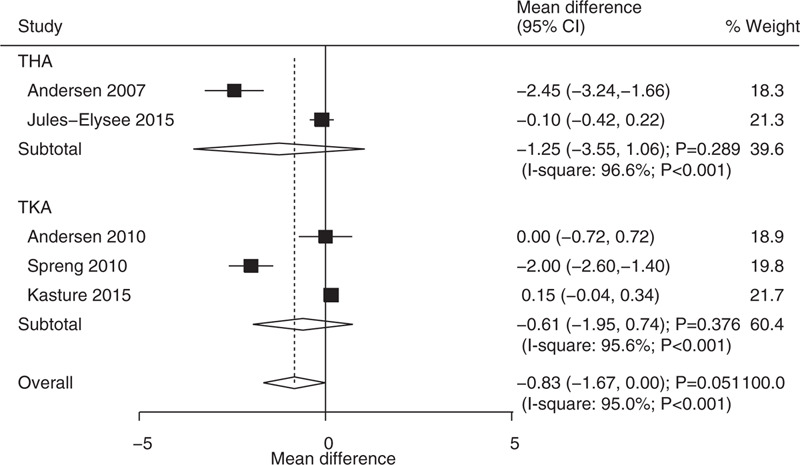
Local infiltration vs epidural analgesia on the length of hospital stay.
3.7. Adverse events
Data for the effects of local infiltration vs epidural analgesia on the risk of nausea and wound infection were available in 6 and 4 studies, respectively. The pooled RR indicated that local infiltration was associated with a lower risk of nausea compared to epidural analgesia (RR: 0.47; 95%CI: 0.24–0.93; P = .030; I2 = 81.4%; Pheterogeneity < .001; Fig. 6). Moreover, there were no significant differences between local infiltration and epidural analgesia on the risk of wound infection (RR: 2.05; 95%CI: 0.43–9.80; P = .370; I2 = 0.0%; Pheterogeneity = .634; Fig. 7). The results of the subgroup analyses did not find any significant differences between local infiltration and epidural analgesia for the risk of nausea or wound infection. There was no significant publication bias for nausea (PEgger = .180; PBegg = .260) and wound infection (PEgger = .409; PBegg = 1.000).
Figure 6.
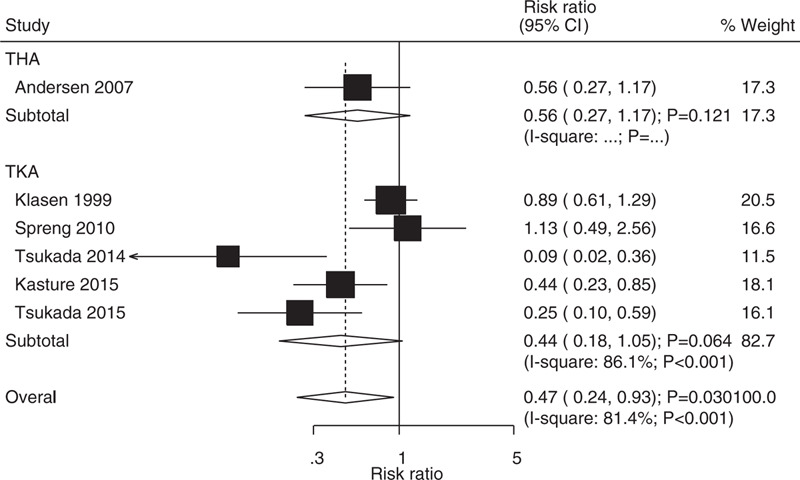
Local infiltration vs epidural analgesia on the risk of nausea.
Figure 7.
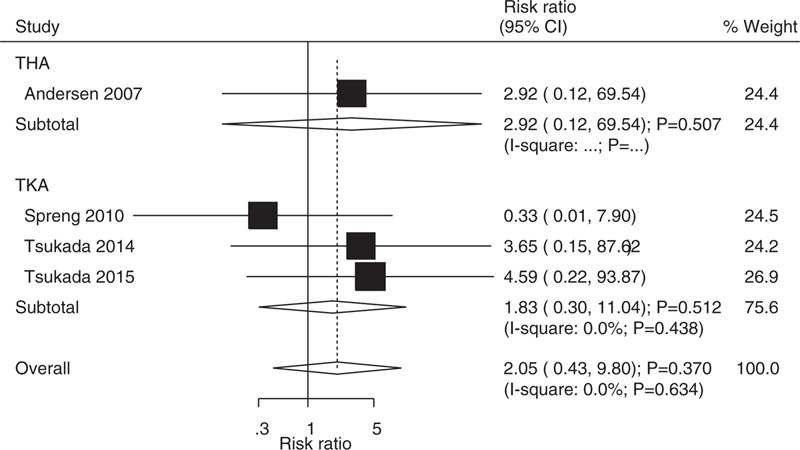
Local infiltration vs epidural analgesia on the risk of wound infection.
4. Discussion
The current systematic review and meta-analysis was based on RCTs and compared the efficacy and safety of local infiltration vs epidural analgesia for patients after TKA or THA. This study included a total of 412 TKA patients and 200 THA patients from 7 and 3 RCTs, respectively. The findings of this study revealed that local infiltration showed lower VAS scores at rest compared to epidural analgesia after 48 hours and 72 hours for TKA patients, while local infiltration was associated with lower VAS scores at rest after 12 hours for THA patients. Moreover, local infiltration was associated with lower VAS scores during movement after 48 hours for TKA patients, whereas local infiltration was associated with higher VAS scores at movement after 24 hours for THA patients. Furthermore, the levels of flexion angle after 24 hours, 48 hours, and 72 hours for TKA patients who received local infiltration were significantly higher than for patients who received epidural analgesia. Finally, patients who received local infiltration had a reduced risk of nausea as compared with those who received epidural analgesia.
Several systematic reviews and meta-analyses have already compared the treatment effectiveness between local infiltration and epidural analgesia for patients after TKA or THA. A meta-analysis conducted by Yan et al suggested that local infiltration provides better pain relief and a larger range of motion in TKA patients, while local infiltration did not yield significant effects on the length of hospital stay and complications.[32] Moreover, they pointed out that local infiltration was associated with poor pain relief during movement at 24 hours. Li et al conducted a meta-analysis of 7 RCTs and found that local infiltration did not give better pain control after TKA as compared with epidural analgesia, but that local infiltration was associated with a better range of motion, shorter hospital stay, and lower risk of nausea.[33] However, the analyses for other results were not stratified by time endpoints and the type of operation, and several other trials were not included. Therefore, we conducted a systematic review and meta-analysis to compare the treatment effectiveness between local infiltration and epidural analgesia for patients after TKA or THA.
The results summary revealed that local infiltration was associated with lower VAS scores at rest after 48 hours and 72 hours for patients after TKA. Although most included trials reported similar results or trends, a study conducted by Tsukada et al found no significant difference between local infiltration and epidural analgesia.[29] This result could explained by the fact that this study compared the efficacy of periarticular injection with epidural analgesia for patients after TKA, and ignored other regional analgesia regimens or intravenous patient-controlled analgesia regimens. Furthermore, although we noted that local infiltration significantly reduced VAS scores at rest after 12 hours for THA patients, this result was based on only 1 included trial,[25] causing the pooled conclusion to be variable and requiring further verification. Finally, local infiltration was associated with lower VAS scores during movement after 48 hours in TKA patients, and all included trials reported a similar trend. Notably, local infiltration was associated with higher VAS scores during movement after 24 hours for THA patients. This result could be attributed to the various analgesia regimens employed.
The results summary revealed that local infiltration was associated with higher flexion angles after 24 hours, 48 hours, and 72 hours in TKA patients. These results could be explained by the pain scores in the local infiltration group being lower than that for epidural analgesia. The use of methylprednisolone acetate could extend pain control and aid flexion.[34] Local infiltration affects only the surgical area, and does not interfere with the muscle strength of the lower limbs.[11] Several other characteristics assigned to local infiltration and epidural analgesia could affect the treatment effects of total joint arthroplasty, which should be addressed in further large-scale studies.[35–40] In addition, although the pooled results showed no significant differences between groups for the length of hospital stay, for either TKA or THA patients, a lower trend was detected for patients who received local infiltration. Local infiltration may protect against the risk of nausea as compared with epidural analgesia, whereas there was no significant difference between groups for the risk of wound infection. These results were analyzed on the basis of a small number of included studies, and the conclusions are not stable.
Several limitations of this study should be acknowledged:
-
(1)
most of the included trials investigated the treatment effectiveness between local infiltration and epidural analgesia for TKA patients, and only 3 trials included THA patients, affecting the robustness of the pooled results for THA patients;
-
(2)
the heterogeneity was not fully explained through the stratified analyses based on the type of operation and time endpoints;
-
(3)
the analgesia regimens differed across the included trials, which could affect the treatment effectiveness between local infiltration and epidural analgesia, and contribute to potential heterogeneity across the included trials;
-
(4)
the analysis of this study was based on published articles, and publication bias is therefore an inevitable limitation.
This study found that local infiltration gave a better or equivalent efficacy for pain control as compared with epidural analgesia for TKA patients, while the treatment effectiveness between local infiltration and epidural analgesia for patients after THA remains inconclusive. Moreover, the flexion angle in patients who received local infiltration was significantly higher than those who received epidural analgesia. Furthermore, the risk of nausea for patients who received local infiltration was reduced when compared with epidural analgesia. Further high quality RCTs should be conducted to compare the treatment effectiveness between local infiltration and epidural analgesia for patients after THA.
Author contributions
XXXX.
Footnotes
Abbreviations: CI = confidence interval, RCTs = randomized controlled trials, RR = relative risk, THA = total hip arthroplasty, TKA = total knee arthroplasty, WMD = weighted mean difference.
How to cite this article: Liu X, Zhang H, Zhang H, Guo M, Gao Y, Du C. Local infiltration vs epidural analgesia for postoperative pain control after total knee or hip arthroplasty: a meta-analysis of randomized controlled trials. Medicine. 2020;99:44(e22674).
XL and HZ are co-first authors and contributed equally to this study.
The authors have no conflicts of interests to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Harris WH. The first 50 years of total hip arthroplasty: lessons learned. Clin Orthop Relat Res 2009;467:28–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Ritter MA, Harty LD. Debate: simultaneous bilateral knee replacements: the outcomes justify its use. Clin Orthop Relat Res 2004. 84–6. [PubMed] [Google Scholar]
- [3].OECD. Health at a Glance 2017; 2017. [Google Scholar]
- [4].Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780–5. [DOI] [PubMed] [Google Scholar]
- [5].Soffin EM, Wu CL. Regional and multimodal analgesia to reduce opioid use after total joint arthroplasty: a narrative review. HSS J 2019;15:57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Andersen LO, Kehlet H. Analgesic efficacy of local infiltration analgesia in hip and knee arthroplasty: a systematic review. Br J Anaesth 2014;113:360–74. [DOI] [PubMed] [Google Scholar]
- [7].Affas F. Local infiltration analgesia in knee and hip arthroplasty efficacy and safety. Scand J Pain 2016;13:59–66. [DOI] [PubMed] [Google Scholar]
- [8].Wiebalck A, Brodner G, Van Aken H. The effects of adding sufentanil to bupivacaine for postoperative patient-controlled epidural analgesia. Anesth Analg 1997;85:124–9. [DOI] [PubMed] [Google Scholar]
- [9].Choi PT, Bhandari M, Scott J, et al. Epidural analgesia for pain relief following hip or knee replacement. Cochrane Database Syst Rev 2003. CD003071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Tang R, Evans H, Chaput A, et al. Multimodal analgesia for hip arthroplasty. Orthop Clin North Am 2009;40:377–87. [DOI] [PubMed] [Google Scholar]
- [11].Kerr DR, Kohan L. Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery: a case study of 325 patients. Acta Orthop 2008;79:174–83. [DOI] [PubMed] [Google Scholar]
- [12].Elder JB, Hoh DJ, Wang MY. Postoperative continuous paravertebral anesthetic infusion for pain control in lumbar spinal fusion surgery. Spine (Phila Pa 1976) 2008;33:210–8. [DOI] [PubMed] [Google Scholar]
- [13].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Controlled Clin Trials 1996;17:1–2. [DOI] [PubMed] [Google Scholar]
- [15].DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clin Trials 1986;7:177–88. [DOI] [PubMed] [Google Scholar]
- [16].Ades AE, Lu G, Higgins JP. The interpretation of random-effects meta-analysis in decision models. Med Decis Making 2005;25:646–54. [DOI] [PubMed] [Google Scholar]
- [17].Deeks JJ, Higgins JPT, Altman DG. Higgins JGS. Analysing data and undertaking meta-analyses. Cochrane Handbook for Systematic Reviews of Interventions. Oxford, UK: The Cochrane Collaboration; 2008. 243–96. [Google Scholar]
- [18].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ (Clin Res ed) 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clin Res ed) 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088–101. [PubMed] [Google Scholar]
- [21].Klasen JA, Opitz SA, Melzer C, et al. Intraarticular, epidural, and intravenous analgesia after total knee arthroplasty. Acta Anaesthesiol Scand 1999;43:1021–6. [DOI] [PubMed] [Google Scholar]
- [22].Andersen KV, Pfeiffer-Jensen M, Haraldsted V, et al. Reduced hospital stay and narcotic consumption, and improved mobilization with local and intraarticular infiltration after hip arthroplasty: a randomized clinical trial of an intraarticular technique versus epidural infusion in 80 patients. Acta Orthop 2007;78:180–6. [DOI] [PubMed] [Google Scholar]
- [23].Andersen KV, Bak M, Christensen BV, et al. A randomized, controlled trial comparing local infiltration analgesia with epidural infusion for total knee arthroplasty. Acta Orthop 2010;81:606–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Spreng UJ, Dahl V, Hjall A, et al. High-volume local infiltration analgesia combined with intravenous or local ketorolac+morphine compared with epidural analgesia after total knee arthroplasty. Br J Anaesth 2010;105:675–82. [DOI] [PubMed] [Google Scholar]
- [25].Pandazi A, Kanellopoulos I, Kalimeris K, et al. Periarticular infiltration for pain relief after total hip arthroplasty: a comparison with epidural and PCA analgesia. Arch Orthop Trauma Surg 2013;133:1607–12. [DOI] [PubMed] [Google Scholar]
- [26].Binici Bedir E, Kurtulmus T, Basyigit S, et al. A comparison of epidural analgesia and local infiltration analgesia methods in pain control following total knee arthroplasty. Acta Orthop Traumatol Turc 2014;48:73–9. [DOI] [PubMed] [Google Scholar]
- [27].Tsukada S, Wakui M, Hoshino A. Postoperative epidural analgesia compared with intraoperative periarticular injection for pain control following total knee arthroplasty under spinal anesthesia: a randomized controlled trial. J Bone Joint Surg Am 2014;96:1433–8. [DOI] [PubMed] [Google Scholar]
- [28].Kasture S, Saraf H. Epidural versus intra-articular infusion analgesia following total knee replacement. J Orthop Surg 2015;23:287–9. [DOI] [PubMed] [Google Scholar]
- [29].Tsukada S, Wakui M, Hoshino A. Pain control after simultaneous bilateral total knee arthroplasty: a randomized controlled trial comparing periarticular injection and epidural analgesia. J Bone Joint Surg Am 2015;97:367–73. [DOI] [PubMed] [Google Scholar]
- [30].Jules-Elysee KM, Goon AK, Westrich GH, et al. Patient-controlled epidural analgesia or multimodal pain regimen with periarticular injection after total hip arthroplasty: a randomized, double-blind, placebo-controlled study. J Bone Joint Surg Am 2015;97:789–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Duval S, Tweedie R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc 2000;95:89–98. [Google Scholar]
- [32].Yan H, Cang J, Xue Z, et al. Comparison of local infiltration and epidural analgesia for postoperative pain control in total knee arthroplasty and total hip arthroplasty: a systematic review and meta-analysis. Bosn J Basic Med Sci 2016;16:239–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Li C, Qu J, Pan S, et al. Local infiltration anesthesia versus epidural analgesia for postoperative pain control in total knee arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res 2018;13:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Mullaji A, Kanna R, Shetty GM, et al. Efficacy of periarticular injection of bupivacaine, fentanyl, and methylprednisolone in total knee arthroplasty: a prospective, randomized trial. J Arthroplasty 2010;25:851–7. [DOI] [PubMed] [Google Scholar]
- [35].Serbest S, Tiftikci U, Karaaslan F, et al. A neglected case of giant synovial chondromatosis in knee joint. Pan Afr Med J 2015;22:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Tiftikci U, Serbest S, Burulday V. Can Achilles tendon be used as a new distal landmark for coronal tibial component alignment in total knee replacement surgery? An observational MRI study. Ther Clin Risk Manag 2017;13:81–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Ogurel T, Serbest S, Ogurel R, et al. Blood chromium-cobalt levels in patients after total knee arthroplasty and their effect on the retinal nerve fiber layer and macular ganglion cell complex. Retina 2020;40:1200–6. [DOI] [PubMed] [Google Scholar]
- [38].Tosun HB, Uludag A, Serbest S, et al. A rare case of extensive diffuse nonpigmented villonodular synovitis as a cause of total knee arthroplasty failure. Int J Surg Case Rep 2014;5:419–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Serbest S, Tosun HB. Dislocation of a revision total knee arthroplasty: rare but serious complication. Pan Afr Med J 2015;20:193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Tiftikci U, Serbest S. Periprosthetic proximal medial femoral cortical destruction caused by a femoral arterial pseudoaneurysm. Clin Interv Aging 2015;10:1967–70. [DOI] [PMC free article] [PubMed] [Google Scholar]


