Abstract
The aim of this study was to assess the levels of self-perceived burden (SPB) and self-management behavior in elderly stroke survivors during the first 3 months after acute stroke, and to explore the correlation between them.
A total of 203 consecutive hospitalized elderly patients diagnosed with stroke were recruited. Self-perceived Burden Scale and Stroke Self-management Scale in 1 month (T1) and 3 months (T2) post-stroke were assessed and compared.
The score of SPB in elderly stroke survivors was 28.96 ± 5.50 and 27.25 ± 6.17 at T1 and T2, respectively. Stroke self-management scale scored 165.93 ± 9.82 at T1 and 167.29 ± 10.60 at T2. In the first 3 months post-stroke, the physical burden was dominant (T1 14.73 ± 3.07, T2 14.40 ± 3.13), and the behavior of stroke symptoms and signs monitoring (T1 27.58 ± 6.56, T2 28.64 ± 6.43) and rehabilitation exercise management (T1 21.40 ± 3.28, T2 20.74 ± 3.15) was the worst. SPB was negatively correlated with self-management behavior (T1 r = -.202, T2 r = -.511).
Elderly stroke survivors experienced a medium level of SPB and self-management behavior in the first 3 months post-stroke. There is a positive relationship between reduced SPB and improved self-management behavior. Addressing the characteristics and correlations as well as development of targeted interventions for SPB decreasing is beneficial to improving self-management behavior for elderly survivors.
Keywords: elderly, longitudinal study, self-management, self-perceived burden, stroke survivor
1. Introduction
Stroke is a major life-threatening cerebrovascular disease event. It is a leading cause of long-term disability, with recent projections forecasting a worldwide rise to 200 million disability-adjusted life years lost per annum by 2030.[1–3] In China, there are about 5 to 6 million stroke patients, and more than 3/4 of them suffer from chronic neurological or cognitive impairment.[4,5] The average age of the first stroke attack is 60.9∼63.4 years.[6] For elderly stroke survivors, especially those with a disabling condition, the receiving care imposes high level of self-perceived burden (SPB).[7] Jiang et al reported 99.0% stroke survivors experienced a mild-moderated level of SPB.[8] SPB is defined as “empathic concern engendered from the impact on others of one's illness and care needs, resulting in guilt, distress, feelings of responsibility, and diminished sense of self”. SPB has a negative influence on patients’ quality of life, which may threaten individuals’ self-management and continued progress following stroke.[9]
Self-management is a care approach that enables individuals to solve problems as they arise, practice new health behaviors, and gain emotional stability.[10] It has been identified as 1 of the key strategies to address stroke patients’ managing their condition more effectively.[11] High self-management behavior enables patients to generate better coping behavior that might improve their recovery.[12] Mu et al study found patients with first stroke seriously lacked disease and rehabilitation management behavior.[13]
In China, the National Stroke Registry reported stroke occurred in more than 7 million Chinese people in 2011, and many survivors suffered constant difficulty with daily tasks.[14] To date, there is a great amount of evidence that functional stroke outcome in terms of motor recovery is influenced and can be predicted by a variety of variables related to metabolic homeostasis,[15] inflammatory activity,[16,17] immune response,[18,19] and perfusion pressure.[20,21] However, no data exists about the correlation between such variables and SPB and self-management behavior in stroke survivors. Especially, studies on the correlation between typical stroke predictors, self-management and SPB in elderly stroke patients are inadequate. Thus, through the longitudinal observation, this study aimed at assessing the levels of SPB and self-management in elderly stroke survivors during the first 3 months post-stroke, and determining the correlation between them.
2. Methods
2.1. Design and participants
This was a longitudinal observational study. The consecutive inpatients with stroke were recruited from neurological department of 3 hospitals in Xi’an between January and September 2017. The inclusion criteria were:
-
(1)
diagnosed with acute stroke and confirmed the disease by CT or MRI examination;
-
(2)
being eligible to participate the study and follow up after discharge;
-
(3)
age 18 years or older.
Exclusion criteria were:
-
(1)
having cognitive impairment, dementia, and psychiatric illness;
-
(2)
suffering from deafness, aphasia or other language barriers;
-
(3)
having serious complications such as severe heart, liver, and kidney diseases.
The study was carried out in accordance with the recommendations of the ethics committee of the 3 hospitals under study. A written informed consent was obtained from each participant.
2.2. Measures
The demographic and disease characteristics included patient's age, gender, marital status, educational level, category of medical expenses, self-evaluated economic pressure, times of stroke, and type of stroke.
The Chinese version of SPB Scale (SPBS) was used to evaluate patients’ burden.[22] SPBS was originally developed by Cousineau.[23] The SPBS used in this study is a 10-item self-report measure. It includes 3 subscales: physical burden (PB), emotional burden (EmB), and economic burden. It uses a 5-point Likert scale to indicate the degree of SPB. Higher scores indicate greater perceived burden. According to the score, patients’ SPB was divided into 3 levels. Due to the difference of item numbers in each dimension, the item average score was employed to compare the level of each dimension.
The self-management behavior of stroke patients was assessed by Stroke Self-management Scale. It was developed by Wang et al.[24] The Cronbach's α coefficient of the scale is .835 and the content validity is .95. The scale contains fifty items. It has seven dimensions, named symptoms and signs monitoring, medication management, diet management, daily life management, emotion management, social function and interpersonal relationship management, and rehabilitation exercise management (REM). It uses a 5-point Likert scale to indicate the degree of self-management behavior. Higher scores indicate better self-management behavior.
Patient's ability to perform activities of daily living (ADL) was measured using Barthel Index (BI).[25] It has 10 items, each scores from 0 to 15. Total scores range from 0 (total dependence) to 100 (total independence). A higher BI indicates a higher level of ADL. For a better interpretation, its scores have been grouped into 4 categories: severe disability (BI ≤40), moderate disability (BI: 41–60), mild disability (BI: 61–99) and no disability (BI = 100). BI is widely used for stroke patients in China.[26] The scale has a good reliability with Cronbach's alpha of .96.
2.3. Procedure
Participants’ sociodemographic and disease data and BI were collected by face-to face interview on the discharge day. At 1 month and 3 months after discharge, participants’ SPB and self-management behavior were assessed by telephone or WeChat platform.
2.4. Statistical analysis
Epidata version 3.0 was used to input the data. Statistical analyses were performed using the SPSS 19.0 statistics package. The statistical significance for all test was set at P<.05. Descriptive analysis was conducted using percentage and frequency for categorical variables, and mean and standard deviation for continuous variables. Bivariate Pearson correlations were used to test the correlations between the variables.
3. Results
3.1. Characteristics of participants
A total of 217 patients in the acute phase of stroke were recruited to participate in the study and completed the baseline data. Of 217 patients, 203 last followed up at 3 months after discharge. Figure 1 shows the number of patients who were surveyed, and the number of patients who completed the survey at 1 and 3 months after stroke. In the present study, 203 patients who responded to both the 1 month and 3 months survey were included. Of the 203 participants, there were 132 (65.0%) males and 71 (35.0%) females. The mean age was 69.69 years (standard deviation = 6.95, range 60–89 years). The characteristics of the participants are presented in Table 1.
Figure 1.
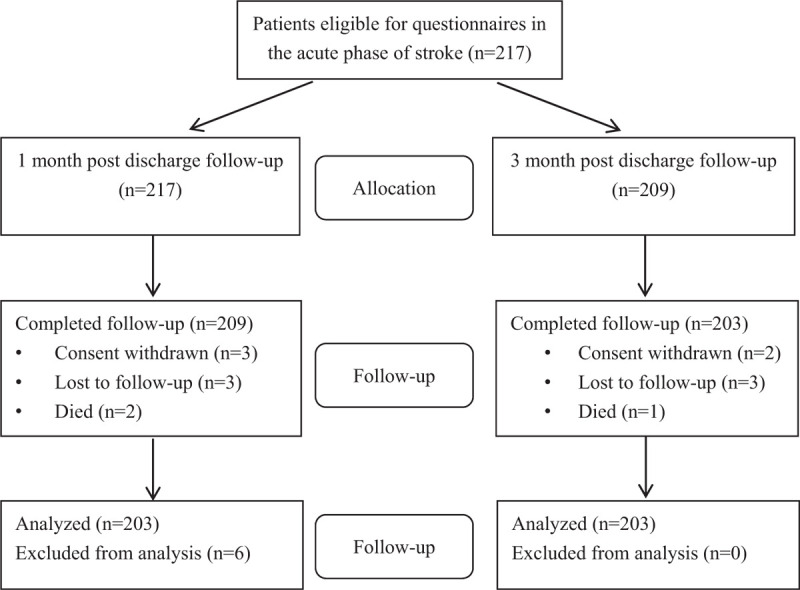
Flow-chart of the study.
Table 1.
Characteristics of participants (n = 203).

3.2. Patients’ SPB
Differences in SPBS scores between 1 month and 3 month are detailed in Table 2 and Figure 2. Of the 3 dimensions of SPBS, PB scored the highest at both 1 and 3 months post-stroke. Except the economic burden, the total score of SPBS and scores of PB and EmB declined significantly at 3 months compared to 1 month (P < .05).
Table 2.
Comparison of self-perceived burden scores among elderly patients at 1 and 3 months post-stroke (n = 203, Mean ± SD).

Figure 2.

Changes of Self-perceived Burden Scales total and its 3 dimensions in the first 3 months after stroke.
3.3. Patients’ self-management behavior
Table 3 and Figure 3 shows the scores and their changes of patients’ self-management behavior at 1 and 3 months post-stroke. Compared to 1 month, the total score of stroke self-management had a tendency of increase at 3 months. The score of symptoms and signs monitoring, diet, daily life, and emotional management had statistically increased at 3 months (P < .05). The score of social function and interpersonal relationship management and REM at 3 months decreased by .22 and .08 points compared to 1 month, respectively (P < .05).
Table 3.
Comparison of scores of self-management behavior among elderly patients at 1 and 3 months after stroke (n = 203, Mean ± SD).
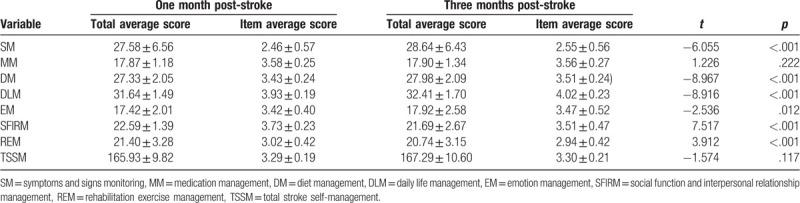
Figure 3.

Changes of Stroke Self-management Scale total and its 7 dimensions in the first 3 months after stroke.
3.4. Correlation between SPB and self-management behavior
Table 4 presents bivariate correlations between SPB and self-management behavior. Except economic burden, the total stroke self-management was found to be negatively associated with physical, EmB and total SPB in the early 3 months after stroke. At 3 months, the correlation coefficients were higher than that of 1 month.
Table 4.
Correlation between self-management behavior and self-perceived burden (n = 203, r).

4. Discussion
4.1. Elderly stroke survivors’ SPB and its change over time
The present study found the overall SPB during the first 3 months after stroke was in the medium level among elderly survivors, and the heaviest burden was PB both at 1 month and 3 months post-stroke. The results are different from Jiang's study.[8] A possible explanation is that at 3 months post-stroke, the majority survivors remained dependent in social function due to paralysis, expressed in terms of impaired ADL, medical problems, and motor impairment.[27] This implies that more attention and support on physical rehabilitation from healthcare professionals might help elderly stroke survivors reduce PB.
Compared to 1 month post-stroke, the overall SPB and physical and EmB had a significant decrease at 3 months. This may due to the improvement of physical function and decrease of dependence on caregivers. For elderly stroke survivors, economic burden didn’t change much within first 3 months post-stroke. This may be caused by expensive costs of stroke sequel treatment and long-term of rehabilitation. The results suggest the importance of disease management in the early care following acute stroke among elderly survivors.
4.2. Elderly stroke survivors’ self-management behavior and its change over time
In the current study, the level of self-management behavior among elderly stroke survivors was moderate in the first 3 months post-stroke. Of seven dimensions, the scores of symptoms and signs monitoring and REM were lowest. Considering the heavy PB for them, the result further implies that it is necessary to provide continued interventions on symptoms and signs monitoring and rehabilitation exercise for elderly stroke survivors.
Compared to 1 month post-stroke, there were no significant changes in the total self-management and medication management at 3 months. Notably, the 2 dimensions’ scores of social function and interpersonal relationship management and REM at 3 months were found to be statistically worse, which may suggest that elderly survivors living with stroke complications can experience a decline in their belief to perform social activities and rehabilitation exercise with confidence over time. The results indicate that elderly survivors’ confidence and motivation of stroke self-management should be stimulated as well as guidance on disease monitoring and rehabilitation in the early phase after stroke.
4.3. Correlation between SPB and self-management behavior
Previous studies found that SPB had negative influence on patients’ rehabilitation and quality of life, which has been identified as putative causes of the desire for suicide.[9,28] Consistent with Du's study, Pearson correlation analysis showed that there was a negative correlation between the total self-management behavior and SPB.[29] With SPB increased, elderly survivors’ self-management behavior decreased. Importantly, the correlation increased at 3 months when compared to 1 month post-stroke. Self-management is a term used to describe an iterative process whereby individual responses and behaviors are used to cope with the physical and psychological consequences of chronic disease.[30] The result indicates that the challenge for self-management intervention is to find an effective method to help patients reduce SPB as soon as possible after acute stroke.
For elderly stroke survivors, the total SPB and its 3 dimensions were all negatively correlated with emotion, social function and interpersonal relationship management at 1 and 3 months post-stroke. At 3 months, there was also a negative correlation between SPB and daily life management. The results indicate SPB has negative impact on elderly stroke survivors’ emotional and social function, especially greatly influences daily life. This further explained low and reduced daily life management score at 3 months.
There are limitations in the study. First, the participants were recruited from 3 general hospitals in 1 city, which might limit representation of all stroke patients in other cities in China and internationally. Second, the study evaluated patients’ SPB and self-management behavior during the first 3 months after stroke, which cannot provide evidence of long-term burden of stroke patients. Hence, multicenter longitudinal studies are needed to further investigate correlation between elderly stroke survivors’ SPB and self-management behavior.
5. Conclusions and implications
This study extends knowledge by providing the changes of elderly survivors’ SPB and self-management behavior in the early stage after acute stroke. Elderly survivors experienced moderate SPB and self-management behavior during the first 3 months post-stroke. Over time, SPB and self-management behavior had a tendency of decrease and increase, respectively. In the first 3 months after acute stroke, the PB was dominant, and the behavior of stroke symptoms and signs monitoring and REM was the worst in elderly survivors. SPB was negatively correlated with self-management behavior. Addressing the characteristics and correlations as well as development of targeted interventions for SPB decreasing is beneficial to improving self-management behavior for elderly survivors in the early stage after acute stroke.
Acknowledgments
We thank the grant support from the Department of Science & Technology of Shaanxi Province (Grand No. 2015KW-041 and Grand No. 2017SF-177) and the Fourth Military Medical University (Grand No. 2019XB070).
Author contributions
Conceptualization: Chun-Ping Ni, Hong-Xia Guo, Xiao-Ran Ren, Yuan-Yuan Wei.
Data curation: Xiao-Ran Ren, Yuan-Yuan Wei, Pei Shao, Ting Xiao, Jing Wang.
Formal analysis: Xiang-Ni Su, Yan Hua.
Writing – original draft: Xiao-Ran Ren, Yuan-Yuan Wei.
Writing – review & editing: Chun-Ping Ni, Hong-Xia Guo.
Footnotes
Abbreviations: ADL = activities of daily living, BI = Barthel index, EmB = emotional burden, PB = physical burden, REM = rehabilitation exercise management, SPB = self-perceived burden, SPBS = self-perceived burden scale.
How to cite this article: Ren XR, Wei YY, Su XN, Hua Y, Shao P, Xiao T, Wang J, Ni CP, Guo HX. Correlation between self-perceived burden and self-management behavior in elderly stroke survivors: a longitudinal observational study. Medicine. 2020;99:44(e22862).
C-P N and H-X G contributed equally to this work, and should be considered as the correspondence.
X-R R and Y-Y W contributed equally to this work, and should be considered as the first author.
The authors have no funding and conflicts of interests to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
References
- [1].Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet Glob Health 2014;383:245–55. [Google Scholar]
- [2].Guan T, Ma J, Li M, et al. Rapid transitions in the epidemiology of stroke and its risk factors in China from 2002 to 2013. Neurology 2017;89:53–61. [DOI] [PubMed] [Google Scholar]
- [3].Tsai CF, Thomas B, Sudlow CL. Epidemiology of stroke and its subtypes in Chinese vs white population: a systematic review. Neurology 2013;81:264–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Tian SP. The care of stroke patients. Chin J Pract Nerv Dis 2013;16:89–90. [Google Scholar]
- [5].Deng CY, Zhao Y, Lu Q. The review of stigma in patients with stroke. Chin J Nurs 2016;51:733–7. [Google Scholar]
- [6].Wang LD, Liu JM, Yang Y, et al. The Prevention and Treatment of Stroke Still Face Huge Challenges—Brief Report on Stroke Prevention and Treatment in China 2018. Chin Circ J 2019;34:105–19. [Google Scholar]
- [7].Luo LR, Liu M. Study on the self-perceived burden influencing factors and intervention with elderly stroke patients. Medicine and Philosophy 2013;4:79–81. [Google Scholar]
- [8].Jiang LH, Deng CY, Li ZJ, et al. Analysis on the status of self-perceived burden in stroke patients and its influencing factors. Tianjin Journal of Nursing 2019;27:514–7. [Google Scholar]
- [9].McPherson CJ, Wilson KG, Chyurlia L, et al. The balance of give and take in caregiver–partner relationships: An examination of self-perceived burden, relationship equity, and quality of life from the perspective of care recipients following stroke. Rehabil Psychol 2010;55:194–203. [DOI] [PubMed] [Google Scholar]
- [10].Lorig KR, Holman HR. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 2003;26:1–7. [DOI] [PubMed] [Google Scholar]
- [11].Jordan JE, Osborne RH. Chronic disease self-management education programs: challenges ahead. Med J Aust 2007;186:84–7. [DOI] [PubMed] [Google Scholar]
- [12].Li X, Sun XJ. A study on the relationship between self-perceived burden and self-management behavior among maintenance hemodialysis patients. Chinese Journal of Nursing 2016;51:562–6. [Google Scholar]
- [13].Mu X, Li J, Liu RR, et al. The current status and influencing factors of self-management behaviors in patients with first stroke. Chinese Journal of Nursing 2016;51:289–93. [Google Scholar]
- [14].Wang YL, Li XL, Zhao XQ, et al. Using recombinant tissue plasminogen activator to treat acute ischemic stroke in China: analysis of the results from the Chinese National Stroke Registry (CNSR). Stroke 2011;42:1658–64. [DOI] [PubMed] [Google Scholar]
- [15].Lattanzi S, Bartolini M, Provinciali L, et al. Glycosylated hemoglobin and functional outcome after acute ischemic stroke. J Stroke Cerebrovasc Dis 2016;25:1786–91. [DOI] [PubMed] [Google Scholar]
- [16].Lattanzi S, Di Napoli M, Ricci S, et al. Matrix metalloproteinases in acute intracerebral hemorrhage. Neurotherapeutics 2020;17:484–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Di Napoli M, Slevin M, Popa-Wagner A, et al. Monomeric C-reactive protein and cerebral hemorrhage: from bench to bedside. Front Immunol 2018;9:1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Lattanzi S, Brigo F, Trinka E, et al. Neutrophil-to-lymphocyte ratio in acute cerebral hemorrhage: a system review. Transl Stroke Res 2019;10:137–45. [DOI] [PubMed] [Google Scholar]
- [19].Zangari R, Zanier ER, Torgano G, et al. Early ficolin-1 is a sensitive prognostic marker for functional outcome in ischemic stroke. J Neuroinflammation 2016;13:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Divani AA, Liu X, Di Napoli M. Blood pressure variability predicts poor in-hospital outcome in spontaneous intracerebral hemorrhage. Stroke 2019;50:2023–9. [DOI] [PubMed] [Google Scholar]
- [21].Buratti L, Cagnetti C, Balucani C, et al. Blood pressure variability and stroke outcome in patients with internal carotid artery occlusion. J Neurol Sci 2014;339:164–8. [DOI] [PubMed] [Google Scholar]
- [22].Wu Y, Jiang Y. Investigation and analysis of the self-perceived burden among cancer patients. Journal of Nursing Administration 2010;10:405–7. [Google Scholar]
- [23].Cousineau N, McDowell I, Hotz S, et al. Measuring chronic patients’ feelings of being a burden to their caregivers development and preliminary validation of a scale. Med Care 2003;41:110–8. [DOI] [PubMed] [Google Scholar]
- [24].Wang YQ, Jiang YL, Wang Y, et al. Survey of status quo of related knowledge level and self-management behavior of stroke patients at convalescence. Chinese nursing research 2013;27:3090–2. [Google Scholar]
- [25].Manhoey FI, Barthel DW. Functional evaluation: the barthel index. Md State Med J 1965;14:61–5. [PubMed] [Google Scholar]
- [26].He Y, Wu YY, Yan TB. Study on validity and reliability of Chinese version of Barthel index in assessing the activities of daily living in stroke patients. Chinese Journal of Physical Medicine and Rehabilitation 2008;30:185–9. [Google Scholar]
- [27].Rachpukdee S, Howteerakul N, Suwannapong N, et al. Quality of life of stroke survivors: a 3-month follow-up study. J Stroke Cerebrovasc Dis 2013;22:e70–8. [DOI] [PubMed] [Google Scholar]
- [28].Wilson KG, Chochinov HM, McPherson CJ, et al. Desire for euthanasia or physician-assisted suicide in palliative cancer care. Health Psychol 2007;26:314–23. [DOI] [PubMed] [Google Scholar]
- [29].Du J. Study on relation of health self- management skills and self- perceived burden of patients with chronic diseases. Medical Journal of Chinese Peoples’ Health 2015;27:1–4. [Google Scholar]
- [30].McCorkle R, Ercolano E, Lazenby M, et al. Self-management: enabling and empowering patient living with cancer as a chronic illness. Cancer J Clin 2011;61:50–62. [DOI] [PMC free article] [PubMed] [Google Scholar]


