Abstract
To investigate the incidence of skin diseases, the factors affecting the life quality, anxiety, and depression of patients with skin diseases and the correlation among the 3.
A total of 1127 patients with skin diseases were selected online from March 2018 to June 2018. Logistic regression was used to analyze the factors influencing life quality, anxiety, and depression. Spearman rank correlation was used to analyze the correction among the life quality, anxiety, and depression.
There was no significant difference in ethnicity, education, and time of question among patients (P > .05). Sex ratio, age, marital status, and occupation were statistically significant difference among patients with different skin diseases (P < .05). The life quality index of patients with psoriasis, atopic dermatitis, acne, steroid-dependent dermatitis, and alopecia were 11.96 ± 6.74, 9.84 ± 6.99, 11.57 ± 6.85, 13.86 ± 6.31, 7.86 ± 6.82, respectively. The differences were statistically significant (P < .05). The main factors affecting quality of life included age, family history, and types of skin diseases. The age, ethnicity, education, and family history of skin diseases were the main factors affecting anxiety of patients with different skin diseases. Additionally, sex, marital status, education, and family history of skin diseases were the main factors influencing depression. Spearman rank correlation analysis showed that the life quality, anxiety, and depression were positively correlated.
Psoriasis, atopic dermatitis, acne, steroid-dependent dermatitis, and alopecia have a certain impact on the life quality of most patients, and may cause different degrees of anxiety and depression.
Keywords: anxiety, depression, life quality, skin diseases
1. Introduction
Skin diseases are common conditions and often accompanied by flushing, itching, desquamation, pain, and burning of epidermis or mucosa. Compared with other diseases, skin diseases are more likely to cause psychological problems.[1,2] Certain chronic skin diseases significantly reduce the quality of life of patients.[3] For example, psoriasis is mainly characterized by itchy, which affects the work, life, study, and sleep of patients, and seriously affects the quality of life of patients. Acne, hair loss, and atopic dermatitis affect physical appearance of the patient and have a great psychological impact on emotional, psychological, and social situations of patients.[4,5] At the same time, some skin diseases may cause allergies, infections, and dietary contraindications. Skin diseases are risk factors for mood disorders and acute anxiety disorders, which can affect the course of the disease and the therapeutic effect. Study has shown that more than 10 kinds of skin diseases such as psoriasis, acne, and alopecia are closely related to psychological problems.[6] People with chronic skin diseases can become depressed because of the difficulty in treating the disease,[7] and depression can seriously decrease the quality of life of patients.
The prevalence of skin diseases is on the rise in recent years. Compared with healthy people, patients with acne, atopic dermatitis, psoriasis, steroid-dependent dermatitis, and alopecia usually have different degrees of depression or anxiety, and severe cases even have suicidal tendencies.[8–10] Poor emotional state can also aggravate existing symptoms, and have an important impact on the patient's prognosis, thus forming a vicious circle.[11] Based on the bio-psychological-social model,[12] some skin diseases have been attributed to psychosomatic medicine, and psychological intervention has become an important means of dermatological adjuvant therapy.[13] However, previous studies have focused on the relationship between a single skin disease and psychological state. Studies on the horizontal comparison of psychological states among different skin diseases are rare.[14–16]
To understand the prevalence and distribution of common skin diseases and the psychological impact of skin diseases on patients of north and east regions in Xinjiang, we conducted a skin disease survey of some regions in Xinjiang from March to June 2018. The depression and anxiety in patients with 5 common skin diseases including psoriasis, atopic dermatitis, acne, steroid-dependent dermatitis, and alopecia were evaluated and the differences were identified. This provides a preliminary theoretical basis for targeted psychological intervention.
2. Materials and methods
2.1. Subjects
In total 1127 outpatients and inpatients from March to June 2018 were selected from 12 hospitals in Xinjiang, including Xinjiang Uygur Autonomous Region Chinese Medicine Hospital, Hami City Xinshi Skin Hospital, Altay Regional People's Hospital, Jixian People's Hospital, Midong District People's Hospital, Yili State Hospital of Traditional Chinese Medicine, Karamay People's Hospital, Changji People's Hospital, Fuhai County Chinese Medicine Hospital, Tacheng City Traditional Chinese Medicine Hospital, Dushanzi Central Hospital, and Fukang Chinese Medicine Hospital. The inclusion criteria were as follows: Voluntary participation; patients who can correctly read and understand the questionnaire; patients who met 1 of the 5 diagnostic criteria for skin diseases in China Clinical Dermatology.[17] Exclusion criteria were as follows: patients who had concurrent other skin diseases; patients who had serious physical and mental illnesses; pregnant women; patients who were alcohol and drug dependence. Written and informed consent were obtained from every patient and the study was approved by the ethics review board of Xinjiang Uygur Autonomous Region Chinese Medicine Hospital.
2.2. Questionnaires
The “Skin Disease Questionnaire” was designed by our lab. The general information of the questionnaire included the ethnicity, age, sex, marital status, education, occupation, time of question, and body mass index. The dermatology life quality index (DLQI), Self-Rating Depression Scale (SDS), and self-rating anxiety scale (SAS) scales were used.
The DLQI[18] scale was used. The scale consists of 10 items. Each item was rated from 0 to 4. The total score of the scale was equal to the sum of the scores of items. SDS scale revised by Self-Rating Depression Scale and Depression Status Inventory was used.[19] It consists of 20 items. Each item was rated from 1 to 4. The total score was equal to 1.25 times of the sum of the scores of items. The reliability and validity met the measurement requirements.
SAS scale[20] consists of 20 items. Each item was rated from 1 to 4. The total score of the questionnaire was 25 to 100 points, equal to 1.25 times of the sum of the scores of items.
2.3. Questionnaire collection
In March 2018, the questionnaire was issued through the online platform and the QR code of the questionnaire was generated. The survey respondents were determined by cluster sampling. The respondents filled in the questionnaires through the web link or mobile phone after scanning the WeChat QR code.
2.4. Statistical analyses
Statistical analysis was performed using SAS JMP10.0. Quantitative data (age, body mass index, time of question and DLQI score) were expressed as the mean± standard deviation. One-way ANOVA were used for comparison among groups followed by least significant difference for comparison between groups. Qualitative data (ethnicity, sex, marital status, education, occupation, family history of skin diseases, and disease course) were expressed as absolute numbers and composition ratios and analyzed with the χ2test. Logistic regression was performed to determine the factors affecting life quality. Spearman rank correlation analysis was used to analyze the correlation among the life quality, anxiety degree, and depression degree. The test level was set at α = 0.05 (2-side). The comparison between the 2 groups was corrected according to the number of comparisons α = 0.05/n.
3. Results
3.1. Basic information of the respondents
In this study, in total 1127 patients were enrolled, including 159 patients with psoriasis, 572 patients with atopic dermatitis, 277 patients with acne, 50 patients with steroid-dependent dermatitis, and 114 patients with alopecia patients. Among them, 373 patients were males and 754 were females. There were 962 Han and 165 Minority patients. As shown in Table 1, there was no significant difference in ethnicity, education, and time of question among different skin disease patients (P > .05). Meanwhile, the factors of sex ratio, age, marital status, and occupation among different skin disease patients were significantly different (P < .05). After correction of α = 0.05/10 = 0.005, the proportion of men with psoriasis was higher than that of atopic dermatitis, acne, and steroid-dependent dermatitis, respectively (P < .05); the average age of psoriasis patients was higher than that of atopic dermatitis and acne patients, respectively (P < .05); the average age of patients with atopic dermatitis, steroid-dependent dermatitis, and alopecia was higher than that of acne patients, respectively (P < .05); proportion of unmarried psoriasis patients was higher than that of atopic dermatitis, steroid-dependent dermatitis, and alopecia patients, respectively (P < .05); proportion of unmarried acne patients was lower than that of atopic dermatitis, steroid-dependent dermatitis, and alopecia patients, respectively (P < .05); proportion of student alopecia patients was higher than that of psoriasis, atopic dermatitis, acne, steroid-dependent dermatitis patients, respectively (P < .05). Additionally, there was significant difference in family history and disease course among different skin disease patients. Psoriasis patients had a higher family history than atopic dermatitis patients (P < .05); the proportion of psoriasis patients with disease course more than 5 years was higher than that of atopic dermatitis, acne, steroid-dependent dermatitis, and alopecia patients, respectively (P < .05). These indicate that sex, age, marriage, occupation, family history, and disease course are different among different patients with different skin diseases.
Table 1.
Basic information of the respondents.

3.2. DLQI score of each skin disease and its effect on life quality of patients
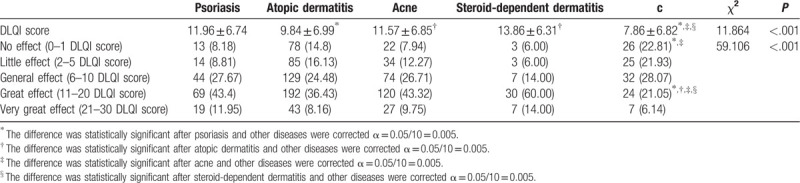
To assess the life quality of patients, the DLQI Questionnaire was used. The DLQI score of psoriasis was 11.96 ± 6.74, of atopic dermatitis was 9.84 ± 6.99, of acne was 11.57 ± 6.85, of steroid-dependent dermatitis was 13.86 ± 6.31, and of alopecia was 7.86 ± 6.82 (Table 2). DLQI score of psoriasis, atopic dermatitis, and alopecia patients was significantly lower than that of acne and steroid-dependent dermatitis patients, respectively (P < .05). Then, the DLQI score of each patient was rated from 0 to 30, indicating no effect (0–1), little effect (2–5), general effect (6–10), great effect (11–20), and very great effect (21–30). There was a statistically significant difference in the life quality among the different skin disease patients (Table 2). The proportion of no effect on life quality in alopecia patients was higher than that in psoriasis and acne patients, respectively (P < .05). Patients with psoriasis, atopic dermatitis, acne, and steroid-dependent dermatitis had a great effect on the life quality. The life quality of the above patients was higher than that of alopecia patients, respectively (P < .05). These demonstrate that skin diseases have a certain impact on the quality of life of patients.
Table 2.
The DLQI score of each skin disease and its effect on life quality of patients.
3.3. Factors affecting the life quality of patients
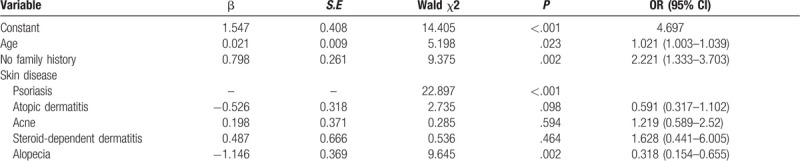
Factors affecting the quality of life of patients with different skin diseases were analyzed. Multivariate regression analysis of logistic regression was performed. The age, family history, and types of skin disease were used as independent variables. The effect on life quality was used as dependent variables. The results showed that the age, family history, and types of skin disease were the main factors affecting life quality (Table 3). For each additional year of age, the probability of affecting life quality was 1.021 (95% CI 1.003–1.039) times of the previous year; patients with a family history were more likely to affect life quality for 2.221 (95% CI 1.333–3.703) times than those without family history; the possibility of alopecia patients affecting life quality was 0.318 (95% CI 0.154–0.655) times of psoriasis patients. The effect of steroid-dependent dermatitis on life quality was 1.628 (95% CI 0.441–6.005) times than psoriasis; that of acne on life quality was 1.219 (95% CI 0.589–2.52) times than psoriasis; that of atopic dermatitis on life quality was 0.591 (95% CI 0.317–1.102) times than psoriasis; that of alopecia on life quality was 0.318 (95% CI 0.154–0.655) times than psoriasis. These results show that age, family history, and types of skin diseases are the main factors affecting quality of life.
Table 3.
Logistic regression analysis of factors affecting life quality.
3.4. Influential factors of moderate–severe anxiety
Logistic regression was used to analyze the influencing factors of anxiety in patients with different skin diseases. Patients were grouped into anxiety group and nonanxiety group based on SAS score. The SAS score <50 points was defined as nonanxiety whereas that >50 points was defined as anxiety. As shown in Table 4, ethnicity, marital status, education, family history, DLQI score, and SAS score were statistically significant between the nonanxiety group and the anxiety group, respectively (P < .05). The DLQI score, SDS score, divorce rate, and proportions of patients with family history or received secondary education were higher in the anxiety group than those in the nonanxiety group, respectively (P < .05). The college/university degree proportion was lower in the anxiety group than that in the nonanxiety group (P < .05).
Table 4.
Influential factors of moderate–severe anxiety.
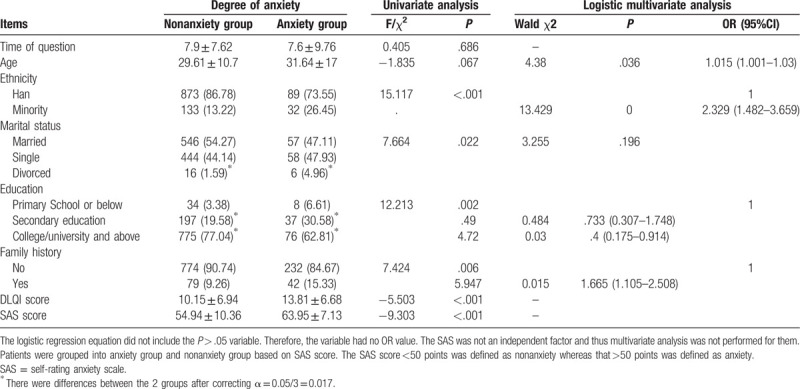
Logistic regression was performed using anxiety as the dependent variable (0 = none or mild, 1 = moderate–severe) and the aforementioned possible influencing factors as independent variables. The results showed that age, ethnicity, education, family history were the main factors of moderate–severe anxiety in patients with skin disease. For each additional year of age, the probability of moderate–severe anxiety was 1.015 (1.001–1.030) times of the previous year; the possibility of moderate–severe anxiety in minority patients was 2.329 (1.482–3.659) times of Han patients; the probability of moderate–severe anxiety in patients with college/university or above was 0.400 (0.175–0.914) times that of primary school; the probability of moderate–severe anxiety in patients with family history was 2.221 (1.333–3.703) times than that without family history. These demonstrate that age, ethnicity, education, and family history of skin diseases are the main factors of moderate–high anxiety in patients with different skin diseases.
3.5. Influential factors of moderate–severe depression
Logistic regression analysis was used to analyze the influencing factors of depression in patients with different skin diseases. Patients were grouped into depression group and nondepression group based on SDS score. The SDS score < 50 points was defined as nondepression whereas that > 50 points was defined as depression. As shown in Table 5, time of question, age, sex, marital status, education, disease course, family history, DLQI score, and SDS score were statistically significant between the nondepression group and the depression group, respectively (P < .05).
Table 5.
Influencing factors of moderate–severe depression.
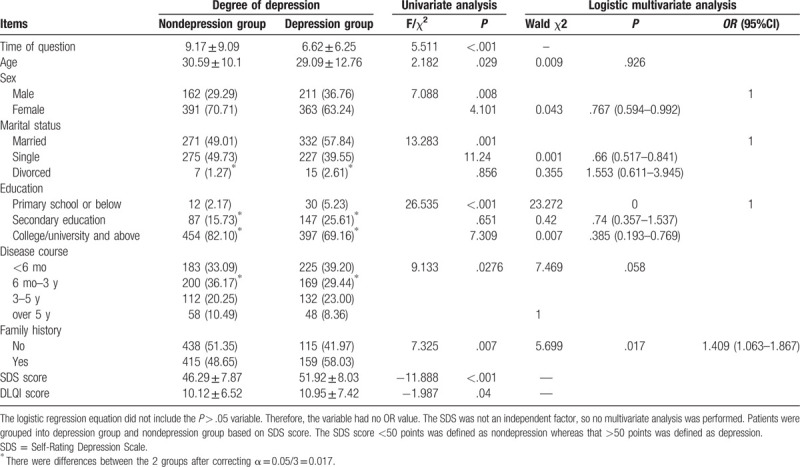
Logistic regression was performed using depression as the dependent variable (0 = none or mild, 1 = moderate–severe) and the aforementioned possible influencing factors as independent variables. The results showed that sex, marital status, education, and family history were the main factors of moderate–severe depression in patients with skin disease. The possibility of moderate–severe depression in female patients was 0.767 (0.594–0.992) times of male patients; the possibility of moderate–severe depression in unmarried patients was 0.660 (0.517–0.841) times of married patients; the probability of moderate–severe depression in patients with college/university or above was 0.385 (0.193–0.769) times that of primary school; the probability of moderate–severe depression in patients with family history was 1.409 (1.063–1.867) times than that without family history. These indicate that sex, marital status, education, family history of skin diseases are the main factors of moderate-to-severe depression in patients with dermatosis.
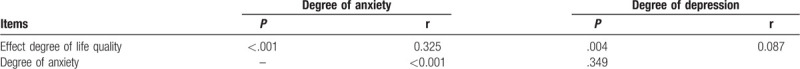
3.6. Correlation analysis among the effect degree on life quality, anxiety, and depression
Spearman rank correlation analysis was performed on the effect degree on life quality of skin disease patients (no effect, little effect, general effect, great effect, and very great effect), degree of anxiety (none, mild, moderate, and severe), and degree of depression (none, mild, moderate, and severe). Results showed that there was a positive correlation among effect on life quality and degrees of anxiety and depression, respectively (Table 6). These data show that the 3 factors interact with each other and are positively correlated.
Table 6.
Spearman rank correlation analysis among the effect degree of life quality, anxiety, and depression.
4. Discussion
Psoriasis, atopic dermatitis, acne, alopecia, and steroid-dependent dermatitis mostly affect the skin of the head and face, while psoriasis and atopic dermatitis can spread to the skin of the trunk and limbs.[21–24] The treatment period is long. These diseases will be seriously affecting the life quality of patients.[25]
In this study, atopic dermatitis had the highest incidence among the investigated patients, followed by acne, psoriasis, alopecia, and steroid-dependent dermatitis. The main influencing factors of various skin diseases were age, sex, occupation, and disease course. Atopic dermatitis, psoriasis, steroid-dependent dermatitis, and alopecia occurred between 30 and 34 years old, and acne occurred around 26 years old; there was no significant difference between male and female. The main skin diseases of student patients were acne and atopic dermatitis, and that of the general staff patients was atopic dermatitis. The disease course of psoriasis patients was usually 3 to 5 years, accounting for 30.19% of all patients, and that of atopic dermatitis patients was generally <6 months, accounting for 45.54% of all patients, which had the highest number of cases. The disease course of acne, steroid-dependent dermatitis, and alopecia patients was 6 months to 3 years, accounting for 41.16%, 46%, and 42.11% of all patients, respectively.
This study shows that DLQI score for psoriasis, acne, and steroid-dependent dermatitis were in the range of 11 to 20, which has a great impact on quality of life. DLQI scores in patients with atopic dermatitis and alopecia were in the range of 6 to 10, which has a certain impact on the quality of life. Multivariate regression analysis of logistic regression showed that types of skin disease were independent factors affecting life quality. Steroid-dependent dermatitis may have relatively higher effect on life quality than alopecia. This may be because that the treatment cycle of psoriasis, atopic dermatitis, acne, and steroid-dependent dermatitis is long, and the recurrence rate is high, which affects the external beauty, thereby aggravating the patient's psychological burden and stress, leading to disordered endocrine function, and causing dysfunction of skin function and repeated skin disease.[26,27] Alopecia also causes certain psychological stress, which aggravates repeated illnesses, but the impact was relatively lower as compared with the other 4 skin diseases. However, the sample sizes of different disease types in the present study were different, which may affect the solidity of the results. Further studies with larger and balanced sample sizes are needed to verify our results.
There were significant differences in anxiety and depression among patients with various skin diseases, indicating that different skin diseases have different degrees of psychological damage to patients. The recurrent episodes and the low cure rate of skin diseases make patients vulnerable to adverse emotions. These also imply that patients with skin diseases are prone to be in a bad state of mind and are closely related to psychological disorders. Moderate-to-severe anxiety and depression suggest that patients need professional psychological intervention.[28] Therefore, dermatologists should pay attention to check the bad moods of patients with skin diseases, increase psychological treatment in time, and establish a mind–body medical concept. On the other hand, dermatologists should guide the patients with skin diseases to take the initiative to adjust their emotions and reduce mental burden while taking the prescribed medicine. Furthermore, dermatologists should strengthen family support and offer individualized patient education.
This study is limited in that the data of lifestyle habits, eating habits, and hospital visits that may have effect on depression and anxiety were not collected or analyzed.
5. Conclusions
In conclusion, psoriasis, atopic dermatitis, acne, steroid-dependent dermatitis, and alopecia can affect the life quality of most patients, and may cause different degrees of anxiety and depression. Our findings may provide evidence for clinical psychotherapy of anxiety and depression in patients with skin diseases.
Author contributions
Conceptualization: Fei Guo, Hongxia Liu.
Data curation: Qin Yu, Zhaoxia Liu, Chenghui Zhang, Pengying Li, Youlu Xu, Yongjie Zuo, Guirong Zhang, Yuanyuan Li.
Formal analysis: Yuanyuan Li.
Funding acquisition: Hongxia Liu.
Writing – original draft: Fei Guo.
Footnotes
Abbreviations: BMI = body mass index, DLQI = dermatology life quality index, SAS = self-rating anxiety scale, SDS = Self-Rating Depression Scale.
How to cite this article: Guo F, Yu Q, Liu Z, Zhang C, Li P, Xu Y, Zuo Y, Zhang G, Li Y, Liu H. Evaluation of life quality, anxiety, and depression in patients with skin diseases. Medicine. 2020;99:44(e22983).
This work was supported by National Natural Science Foundation of China grant (No. 81660840).
The authors have no conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Association CM. Clinical application of vitamin and mineral supplements in the prevention and treatment of several common skin diseases: Expert consensus. Chin J Clin Nutrition 2013;21:386–90. [Google Scholar]
- [2].Cui SS, Lu HG, Wang SP, et al. Mental health status of dermatological patients and its influencing factors. Chin J Dermatol 2008;41:758–9. [Google Scholar]
- [3].Jin SM. Talking about the psychological state and nursing of patients with chronic skin diseases. Health Care Guide 2017;50:0090. [Google Scholar]
- [4].Jiang QK. Influencing factors and nursing strategies of medication compliance in patients with chronic skin diseases. Nursing Practice Rese 2010;7:122–4. [Google Scholar]
- [5].Zhang SY, Cai ZL. The influence factors and nursing countermeasures of chronic skin disease patients with poor medication compliance. Nurs Practice Res 2014;11:70–1. [Google Scholar]
- [6].Wang ZM. The influence factors and nursing countermeasures of chronic skin disease patients with poor medication compliance. Everyone's Health 2017;11:236. [Google Scholar]
- [7].Zhu Z, Chen JP, Zhang M. Clinical effect of Jiawei Zhiyang Mixture on chronic pruritic skin disease. Drug Evaluation 2018;15:61–4. [Google Scholar]
- [8].Feng ZQ, Yan AP. Study on psychological factors of the patients with psoriasis vulgaris and nursing intervention. J Dermatol Venereol 2015;31:5–7. [Google Scholar]
- [9].Long YX, Chen C, Zhou YX, et al. Status and relationship of body image and quality of life among patients with acne. J Nurs Sci 2017;32:30–2. [Google Scholar]
- [10].Xu XT, Xu J, Chen B, et al. Analysis of psychological status and related factors in patients with vitiligo. Chin J Leprosy Skin Dis 2015;2015:761–2. [Google Scholar]
- [11].He YM, Zhao GH. Research progress on quality of life in patients with chronic skin diseases. Nurs Practice Res 2013;23:5423–4. [Google Scholar]
- [12].Zhang W. Discussion on a bio-psycho-environmental-humanities medical model. Med Soc (Berkeley) 2011;24:62–4. [Google Scholar]
- [13].Yang XQ. Summarization of psychodermatology. J Clin Dermatol 2004;12:19–20. [Google Scholar]
- [14].Korkoliakou P, Efstathiou V, Giannopoulou I, et al. Psychopathology and alexithymia in patients with psoriasis. An Bras Dermatol 2017;92:510–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kuty-Pachecka M. Psychological and psychopathological factors in alopecia areata. Psychiatr Pol 2015;49:955–64. [DOI] [PubMed] [Google Scholar]
- [16].Sarkar S, Patra P, Mridha K, et al. Personality disorders and its association with anxiety and depression among patients of severe acne: a cross-sectional study from Eastern India. Indian J Psychiatry 2016;58:378–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Zhao B. Chinese Clinical Dermatology. Nanjing: Jiangsu Science and Technology Press; 2010. [Google Scholar]
- [18].Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clinical Exp Dermatol 2010;19:210–6. [DOI] [PubMed] [Google Scholar]
- [19].Shu L. Self-rating depression scale and depression status inventory. Chin J Mental Health 1999;supplementary issue: 194–6. [Google Scholar]
- [20].Tao M, Gao JF. Reliability and validity of the revised Self-rating Anxiety Scale (SAS-CR). Chin J Neuropsychiatric Dis 1994;20:301–3. [Google Scholar]
- [21].Gallitano SM, Berson DS. How acne bumps cause the blues: the influence of acne vulgaris on self-esteem. Int J Womens Dermatol 2017;4:12–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Ko HC, Kim WI, Cho SH, et al. Topical tacrolimus for the treatment of atopic dermatitis with truncal lesion. Ann Dermatol 2018;30:173–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Li SJ, Huang KP, Joyce C, et al. The impact of alopecia areata on sexual quality of life. Int J Trichol 2018;10:271–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Nicholas MN, Gooderham M. Psoriasis, depression, and suicidality. Skin Therapy Lett 2017;22:1–4. [PubMed] [Google Scholar]
- [25].Farzanfar D, Dowlati Y, French LE, et al. Inflammation: a contributor to depressive comorbidity in inflammatory skin disease. Skin Pharmacol Physiol 2018;31:246–51. [DOI] [PubMed] [Google Scholar]
- [26].Luca M, Luca A, Musumeci ML, et al. Psychopathological variables and sleep quality in psoriatic patients. Int J Mol Sci 2016;17:1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Nguyen SH, Nguyen LH, Vu GT, et al. Health-related quality of life impairment among patients with different skin diseases in Vietnam: a cross-sectional study. Int J Environ Res Public Health 2019;16:305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Mattoo SK, Handa S, Kaur I, et al. Psychiatric morbidity in vitiligo: prevalence and correlates in India. J Eur Acad Dermatol Venereol 2002;16:573–8. [DOI] [PubMed] [Google Scholar]


