ABSTRACT
SARS-CoV2 is a novel coronavirus responsible for causing COVID-19, first identified in the city of Wuhan, China and officially declared a pandemic by the World Health Organization. SARS-CoV2 expresses high affinity to human ACE2 receptors, including within the gastrointestinal tract. Patients with COVID-19 exhibit a wide spectrum of GI symptoms including anorexia, nausea, vomiting, abdominal pain, and abnormal liver function tests. Pathogenesis behind gastrointestinal symptoms caused by SARS-CoV2 has been postulated to be multifactorial including disruption of the intestinal mechanical barrier integrity, alteration of the gut microbiome and systemic inflammatory response to the virus. SARS-CoV-2 RNA has also been found in stool samples of infected patients for a significantly longer period than in nasopharyngeal samples, though the implication of this finding is unclear at this time. Liver injury in patients with COVID-19 is usually mild, stemming from immune-mediated damage, drug induced hepatotoxicity, or ischemia from sepsis. Patients with pre-existing liver disease may be at a higher risk for hospitalization and mortality. Given the high degree of infectivity of this disease, healthcare providers will need to remain watchful for resurgence of this virus. Strict protocols should be implemented regarding hand hygiene, isolation, personal protective equipment, and appropriate disposal of waste. It is also imperative to identify patients with gastrointestinal symptoms at an early stage as these patients may have a prolonged course between symptom onset and viral clearance.
KEYWORDS: SARS-COV2, Covid-19, pathophysiology, liver injury, gastroenterology
1. Introduction
SARS-CoV2 is a novel coronavirus believed to have originated in Wuhan, China, and primarily causes respiratory symptoms. The virus spread rapidly worldwide, and the outbreak was officially declared a pandemic by the World Health Organization, on 11 March 2020. To date, over nine million confirmed cases have been detected worldwide, with the USA continuing to lead with over two million confirmed cases and over one hundred thousand deaths. The virus, like other coronaviruses, was initially noted to cause severe respiratory symptoms, however given the sudden emergence of this virus, there is only a cursory understanding of the breadth of its presentation. Recently there has been a focus on non-respiratory symptoms, including gastrointestinal manifestations. A wide variation in gastrointestinal symptoms has been reported ranging from anorexia to diarrhea. Here we will review the pathophysiology, gastrointestinal and hepatobiliary manifestations, and clinical implications of COVID-19.
2. Epidemiology and virology
Coronaviruses (CoV) are enveloped, positive sense, single stranded RNA with the largest known viral genome (Figure 1). Taxonomically it is a member of the Betacoronavirus genus. The name Coronavirus was derived from Latin; corona meaning the ‘crown’. Under the electron microscope the viral envelope appears crown-like due to the projections formed by the spike (S) protein on the membrane of the virus. There are seven strains of coronaviruses that infect humans. Four of these strains 229E, NL63, OC43 and HKU1 are known to cause mild symptoms and non-severe acute respiratory syndrome. The other three strains are highly pathogenic and cause fatal human disease: Severe Acute respiratory Syndrome (SARS) CoV discovered in November 2002, Middle Eastern respiratory syndrome CoV, discovered in June 2012 and the SARS-CoV-2 (that causes COVID-19), first identified in December 2019 [1]. Based on results from genomic sequencing and evolutionary analysis, bats are suspected to be the natural reservoir of this virus. SARS-CoV-2 might have been transmitted from bats to humans via unknown intermediate hosts [2]. The evolution of this virus is not clear and there remains controversy regarding if the current pathogenic state of the virus evolved de novo in its natural reservoir or occurred after transmission to humans [3].
Figure 1.
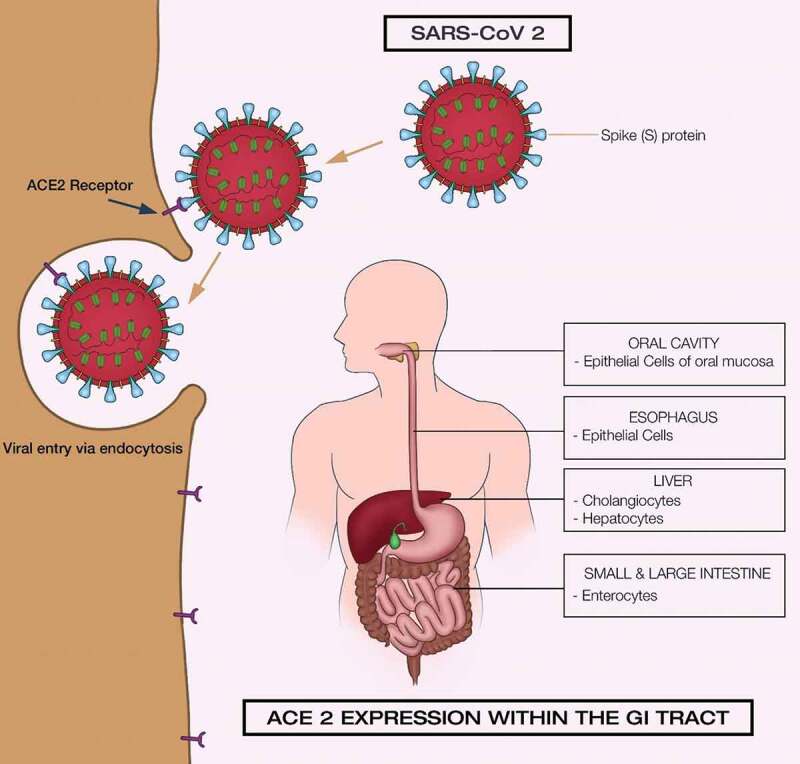
SARS-CoV2 and ACE2 Expression within the Gastrointestinal tract.
The S protein of the SARS-CoV2 plays a crucial role in the receptor selectivity, tissue tropism, and cellular attachment. It is also a main target for neutralizing antibodies and vaccine design [4]. Each monomer of S protein contains two subunits – S1 and S2 – which mediate attachment and membrane fusion via endocytosis. Priming and cleavage of CoV (S) proteins by one of several host proteases including furin, trypsin, cathepsins, transmembrane protease serine protease-2 & 4 (TMPRSS-2 & 4) are essential for viral entry into the cell [5–7].
Strong scientific evidence and data suggest a higher affinity of the SARS-Cov2 (S) protein to the human angiotensin converting enzyme 2 receptors (ACE2). High ACE2 expression was identified within the oral cavity, type II pulmonary alveolar cells (AT2), ileal, and colonic enterocytes, myocardial cells, vascular endothelium, proximal tubule and bladder urothelial cells [8–12]. ACE2 expression within the GI tract was primarily mapped to the luminal surface of small intestinal epithelial cells, with lower expression within crypt cells and colon [13]. Within the hepatobiliary system high ACE2 expression was found in cholangiocytes when compared to hepatocytes [14,15]. These findings indicate that tissue with high ACE2-expression could be at higher risk for viral shedding.
3. Pathogenesis of SARS CoV2 causing GI symptoms
The mechanism by which SARS-CoV2 causes gastrointestinal symptoms is not well defined however there have been several mechanisms put forward.
3.1. Disruption of the mechanical barrier integrity
The gastrointestinal tract is the body’s largest interface between the host and the external environment. ACE2 receptors are highly expressed within the gut lining and the virus itself can cause direct damage to the intestinal mucosa. This can lead to increased intestinal permeability to foreign pathogens by compromising the intestinal barrier function resulting in diarrhea and malabsorption [16].
3.2. Alteration of the gut microbiome
The gut microbiome refers to the collective genomes of the microorganisms including bacteria, fungi, viruses, etc., in the GI tract and plays an important role in the host immune and metabolic function. ACE2 has been reported to have a renin-angiotensin system independent function and was identified as a key regulator of neutral amino acid transporter in the small intestine. Impaired amino acid absorption can in turn lead to a decreased expression of antimicrobial peptides which result in an altered composition of gut microbiota. Hence, the down regulation of ACE2 after SARS-CoV-2 infection can provide a molecular explanation of how amino acid malnutrition can cause intestinal inflammation and diarrhea [13,17–19].
3.3. Systemic inflammatory and immune response
Critically ill patients with COVID-19 infection may develop excessive activated immune response with uncontrolled production and release of cytokines, sometimes referred to as ‘cytokine storm’ which can lead to multi-organ dysfunction including involvement of the gastrointestinal tract. A recent study found high expression of granulocyte macrophage colony stimulating factors (GM-CSF) and Interleukin 6 in patients with COVID-19. GM-CSF is produced from a variety of cell types including macrophages, T cells, fibroblasts, endothelial cells, etc., which are all heavily laden within the GI tract [20,21].
4. GI symptoms in COVID-19
With the continuing evolution of COVID-19 and growing understanding of its presentation, there has been a shift in emphasis to its gastrointestinal manifestations from respiratory symptoms. In fact, the very first case of confirmed COVID-19 in the USA was of a 35-year-old male who in addition to respiratory symptoms also had nausea, vomiting, diarrhea and abdominal discomfort [21].
Table 1 summarizes multiple studies that have reported diverse GI symptoms of COVID-19 patients and the percentage of the study population that exhibited these symptoms. A few of the studies that reported clinical characteristics and outcomes in COVID −19 patients with GI symptoms are discussed below.
Table 1.
Clinical features and laboratory findings in confirmed COVID-19 patients
| Study (N) |
Median Age (years) |
Nausea/vomiting (%) |
Diarrhea (%) |
Abdominal pain (%) |
Elevated AST (%) |
Elevated ALT (%) |
Elevated Total Bilirubin (%) |
|---|---|---|---|---|---|---|---|
| Richardson et al[41]; (n = 5700) |
63 | NA | NA | NA | 58.4 | 39 | NA |
| Guan et al[29]; (n = 1099) |
47 | 5 | 3.8 | NA | 22.2 | 21.3 | 10.5 |
| Quingxian et al[42]; (n = 417) |
50 | NA | NA | NA | 18.23 | 12.95 | 23.19 |
| Xiao et al[22]; (n = 168) |
53.8 | 73 | 37 | 25 | 65 | 66 | NA |
| Zhou et al[23]; (n = 191) |
56 | 4% | 5% | NA | NA | 31 | NA |
| Wang et al[24]; (n = 138) |
56 | 10.1 | 10.1 | 2.2 | 22.46 | 17.39 | 7.1 |
| Chen et al[25]; (n = 99) |
55.5 | 1 | NA | NA | 28 | 35 | 18 |
| Zhang et al[26]; (n = 139) |
57 | 17.3 | 12.9 | 5.8 | NA | NA | NA |
| Jian et al[27]; (n = 80) |
46 | 1.25 | 1.25 | NA | 24 | 30 | 6.6 |
| Pan et al[17]; (n = 204) | 52.9 | 3.9 | 34 | 1.9 | 21.5 | 26.3 | NA |
| Xi et al[28]; (n = 74) |
46.14 | 71.62 | 14.8 | NA | 26.87 | 23.25 | 9.8 |
AST-Aspartate transaminase
ALT- Alanine transaminase
A study from Zhejiang province analyzed 74 confirmed COVID-19 cases with GI symptoms (from a total of 651 enrolled patients) and concluded that these patients had a higher rate of fever (>38.5 C), fatigue, headache, dyspnea, family clustering and critical illness/ICU admissions, compared to those without GI symptoms [28].
Another study on 1099 patients from 552 hospitals that identified clinical characteristics of COVID-19 in China, reported nausea or vomiting in 55 (5%) and diarrhea in 42 (3.8%) of the patients. The study also revealed that although 2.3% of the patients were suffering from pre-existing liver disease, aspartate aminotransferase (AST) was elevated (>40 U/L) in 22.2% and alanine aminotransferase (ALT) was elevated (>40 U/L) in 21.3% of the patient population [29].
A cross-sectional, multi-center study on 204 COVID-19 patients from Hubei, China conducted by Pan et al., aimed to investigate the prevalence and outcomes of those patients with digestive symptoms. The study reported GI symptoms in 50.5% of the patients, which included loss of appetite in 78.6%, diarrhea in 34%, vomiting in 3.9%, and abdominal pain in 1.9% of cases. It also demonstrated that patients with digestive symptoms had a longer time from onset of symptoms to admission, higher liver enzyme levels and a longer prothrombin time than patients without GI symptoms [17].
A study on 206 COVID-19 patients by Han et al., compared 117 patients with GI symptoms (48 of which had only digestive symptoms and 69 had both respiratory and digestive symptoms) with 89 patients with respiratory symptoms alone. The results of this study reported that patients with GI symptoms had a late presentation for care and had a longer duration between symptom onset and viral clearance. These patients were also more likely to have a positive viral RNA in stool (73.3% vs 14.3%, p = 0.033) than those with respiratory symptoms [30].
5. Fecal PCR testing
Various studies have reported the detection of stool viral nucleic acid using rRT-PCR in patients with COVID-19. SARS-COV2 RNA was also isolated using endoscopy specimens from the esophagus, stomach, duodenum and rectum [31]. Live virus from stool samples of two patients in the absence of diarrhea was also reported in a study by Wang et al [32]. This provides evidence of viral replication and shedding in the GI tract, though concerning for possible fecal-oral transmission, there have been no documented cases reported to date.
The duration of viral shedding in feces has been reported for as long as 5 weeks after a negative respiratory PCR. Yongjian et al. reported a positive stool PCR in 41 (55%) of 74 patients with a mean of 27.9 days, while their respiratory samples remained positive for a mean of 16.7 days after the onset of symptoms [33]. A comprehensive meta-analytic study reported that the stool PCR may persist for 33 days or more after the onset of illness even after a negative respiratory PCR [34]. Persistent viral shedding in stool detected by RT-PCR was also seen in 8/10 pediatric patients well after a negative respiratory PCR [35].
Of note, some studies investigating viral shedding and fecal PCR in patients with COVID-19 reported a poor correlation between positive stool PCR and degree of gastrointestinal symptoms or disease activity [36,37]. Moreover, it is yet to be determined if every positive stool PCR has a live virus or just fragments of RNA released from the GI tract.
6. COVID-19 and Liver disease
Abnormal liver function tests have been reported not only in SARS-Cov2 but also in SARS-CoV and MERS-CoV [38]. While there are variations observed in liver function tests among studies (Table 1), the elevated LFTs are usually mild and transient, though severe liver damage was reported in some critically ill patients [17,39,40]. Among the elevated liver enzymes, AST was associated with increased risk of mortality [40].
A large study including 5700 confirmed COVID-19 patients from New York City, USA (Table 1) reported an AST elevation (>40 U/L) in 58.4% and ALT elevation (>60 U/L) in 39% of the participants [41].
The exact mechanism of liver injury is not well understood. Given the pattern of elevated liver function tests being mostly hepatocellular rather than cholangitic, it is unclear if SARS-CoV2 causes direct hepatocyte damage. A recent study using single cell RNA-seq data of two independent cohorts, reported a predominance of ACE2 expression in cholangiocytes (59%) compared to hepatocytes (2.6%) [14]. This would suggest a predominant cholangitic pattern, however, based on mice models of liver injury, there was a transient up-regulation of ACE2 expression caused by a compensatory differentiation of cholangiocyte epithelial cells into hepatocytes [43]. Liver histology from positive COVID-19 patients did not show any intracytoplasmic or intranuclear viral inclusion bodies to suggest direct liver damage [36,44]. Immune mediated liver injury may result from abnormal hyperactivated immune response and cytokine (Interleukin 2,6,7,10, tumor necrosis factor alpha, granulocyte colony stimulating factor, etc.) activation. This response is frequently reported in patients with SARS-COV2 and is associated with multiorgan dysfunction. Presence of hypoxia/ischemia from pneumonia and sepsis could also contribute to liver injury in critically ill patients.
Medications used in the treatment of COVID-19, including antibiotics, antivirals and steroids, are known to cause hepatotoxicity. A recent study reported a positive correlation between the use of drugs and elevated liver enzymes [40]. Another study involving COVID-19 patients with a history of pre-existing liver disease, showed that they had an increased risk of hospitalization and mortality, especially in patients with liver cirrhosis [45].
7. Clinical implications
The sudden emergence and rapid spread of COVID-19 have led to significant changes to the normal functioning of hospital systems. At the urging of the Surgeon General, many hospitals across the USA have postponed elective procedures to help prevent spread of COVID-19. The significance of the tropism of COVID-19 to the GI tract and its detection in stool via PCR remains a key area of concern to gastroenterologists. The AASLD, AGA, ACG, ASGE have published a joint statement on 15 March 2020 regarding COVID-19, with general guidelines for clinical practice based on current knowledge as summarized below [46]:
Recommendations:
Postpone elective procedures
Screen all high-risk patients
Ensure adequate personal protective equipment (PPE) is available to providers
and ensure adequate training on use of PPE.
Ensure enough room to allow for adequate social distancing (6 feet apart)
COVID-19 patients should remain in isolation with procedures performed in negative pressure rooms.
6.Elective office visits should be offered via telemedicine
In the coming months as shelter in place orders are lifted, guidance from medical societies and the CDC will be critical in deciding the appropriate time to resume regular clinical activity. Use of cost-effective barrier protection will need to be widely adopted to allow for resumption of high-risk medical procedures such as esophagogastroduodenoscopy and colonoscopies while minimizing aerosolization of virus particles. In addition, review of infection control practices including disinfection of instruments as well as disposal of post-procedural waste will need to be updated to ensure safe practice. Reminders not to overlook the biosafety concerning COVID-19 patients’ fecal disposition, stems from lessons learnt during the 2003 SARS outbreak, wherein rapid transmission had occurred due to inadequate sewage disposal from aging buildings in Amoy Gardens, Hong Kong [47].
8. Conclusion
COVID-19 has proven to be one of the most devastating pandemics so far. It is too early to speculate on the duration and course of this outbreak. However, current management strategies are being devised using lessons learned from previous outbreaks, primarily from the 2003 SARS and 2012 MERS, as SARS-CoV2 shares homology with the viruses responsible for these 2 outbreaks. We as medical providers will need to remain vigilant to the possibility of resurgence of this virus. Regardless of what the future holds, it is important to collect, analyze, review, and report the data with respect to the virus’ morphology, pathogenesis, varied presentations, and modes of transmission. This will eventually help, not only in determining protocols for screening, diagnosis and management, but also pave the way for prevention of similar pandemics in the future.
Disclosure statement
Guarantor of the article: Anwaruddin Syed
Specific author contributions:
Anwaruddin Syed: Planning/conducting the study and drafting the manuscript
Arsalan Khan: Drafting the work and revising it
FalgunGosai: Collecting and interpreting data
Abuzar Asif: Collecting and interpreting data; revising the manuscript
Sonu Dhillon: Revising the manuscript; final approval of the version
Disclosure statement
No financial or conflict of interest disclosures for all authors.
References
- [1].Raoult D, Zumla A, Locatelli F, et al. Coronavirus infections: epidemiological, clinical and immunological features and hypotheses. Cell Stress. 2020;4(4):66–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Guo Y-R, Cao Q-D, Hong Z-S, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Mil Med Res. 2020;7(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Andersen KG, Rambaut A, Lipkin WI, et al. The proximal origin of SARS-CoV-2. Nat Med. 2020;26(4):450–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Ortega JT, Serrano ML, Pujol FH, et al. Role of changes in SARS-CoV-2 spike protein in the interaction with the human ACE2 receptor: an in silico analysis. Excli J. 2020;19:410–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ou X, Liu Y, Lei X, et al. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat Commun. 2020;11(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271–280.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Gierer S, Bertram S, Kaup F, et al. The spike protein of the emerging betacoronavirus EMC uses a novel coronavirus receptor for entry, can be activated by TMPRSS2, and is targeted by neutralizing antibodies. J Virol. 2013;87(10):5502–5511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Xu H, Zhong L, Deng J, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12(1):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Zou X, Chen K, Zou J, et al. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front Med. 2020;14(2):185–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Zhao Y, Zhao Z, Wang Y, et al. Single-cell RNA expression profiling of ACE2, the receptor of SARS-CoV-2. Bioinformatics. 2020. DOI: 10.1101/2020.01.26.919985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Zhang H, Kang Z, Gong H, et al. The digestive system is a potential route of 2019-NCov infection: a bioinformatics analysis based on single-cell transcriptomes. Microbiology. 2020. DOI: 10.1101/2020.01.30.927806. [DOI] [Google Scholar]
- [12].Zhang H, Penninger JM, Li Y, et al. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46(4):586–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Hashimoto T, Perlot T, Rehman A, et al. ACE2 links amino acid malnutrition to microbial ecology and intestinal inflammation. Nature. 2012;487(7408):477–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Chai X, Hu L, Zhang Y, et al. Specific ACE2 Expression in cholangiocytes may cause liver damage after 2019-NCoV infection. Genomics. 2020. DOI: 10.1101/2020.02.03.931766. [DOI] [Google Scholar]
- [15].Ding S, Liang TJ.. Is SARS-CoV-2 also an enteric pathogen with potential fecal–oral transmission? A COVID-19 virological and clinical review. Gastroenterology. 2020;159(1):53–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Gu J, Han B, Wang J.. COVID-19: gastrointestinal manifestations and potential fecal–oral transmission. Gastroenterology. 2020;158(6):1518–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Pan L, Mu M, Yang P, et al. Clinical characteristics of Covid-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Perlot T, Penninger JM.. ACE2 – from the renin–angiotensin system to gut microbiota and malnutrition. Microbes Infect. 2013;15(13):866–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Cole-Jeffrey CT, Liu M, Katovich MJ, et al. ACE2 and microbiota: emerging targets for cardiopulmonary disease therapy. J Cardiovasc Pharmacol. 2015;66(6):540–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Sun X, Wang T, Cai D, et al. Cytokine storm intervention in the early stages of COVID-19 pneumonia. Cytokine Growth Factor Rev. 2020;53:38–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the USA. N Engl J Med. 2020;382(10):929–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Xiao F, Tang M, Zheng X, et al. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158(6):1831–1833.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Luo S, Zhang X, Xu H. Don’t overlook digestive symptoms in patients with 2019 novel coronavirus disease (COVID-19). Clin Gastroenterol Hepatol. Published online March, 2020;S1542356520304018. DOI: 10.1016/j.cgh.2020.03.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Wu J, Liu J, Zhao X, et al. Clinical characteristics of imported cases of coronavirus disease 2019 (COVID-19) in Jiangsu Province: a multicenter descriptive study. Clinl Infect Dis. 2020;71(15):706–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Jin X, Lian J-S, Hu J-H, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69(6):1002–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Zhang -J-J, Dong X, Cao -Y-Y, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75(7):1730–1741. [DOI] [PubMed] [Google Scholar]
- [30].Han C, Duan C, Zhang S, et al. Digestive symptoms in COVID-19 patients with mild disease severity: clinical presentation, stool viral RNA testing, and outcomes. Am J Gastroenterol. 2020;115(6):916–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Lin L, Jiang X, Zhang Z, et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020;69(6):997–1001. [DOI] [PubMed] [Google Scholar]
- [32].Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. Published online March 11, 2020. DOI: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Wu Y, Guo C, Tang L, et al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol. 2020;5(5):434–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Cheung KS, Hung IFN, Chan PPY, et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from the Hong Kong Cohort and systematic review and meta-analysis. Gastroenterology. Published online April, 2020. DOI: 10.1053/j.gastro.2020.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Xu Y, Li X, Zhu B, et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020;26(4):502–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Tian S, Xiong Y, Liu H, et al. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod Pathol. 2020;33(6):1007–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Chen Y, Chen L, Deng Q, et al. The presence of SARS‐CoV‐2 RNA in the feces of COVID‐19 patients. J Med Virol. Published online April 25, 2020:jmv.25825. DOI: 10.1002/jmv.25825. [DOI] [PubMed] [Google Scholar]
- [38].Lee I-C, Huo T-I, Huang Y-H. Gastrointestinal and liver manifestations in patients with COVID-19. J Chin Med Assoc. Published online April, 2020;1. DOI: 10.1097/JCMA.0000000000000319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Zhang C, Shi L, Wang F-S. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020;5(5):428–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Lei F, Liu Y, Zhou F, et al. Longitudinal association between markers of liver injury and mortality in COVID-19 in China. Hepatology. Published online May 2, 2020. DOI: 10.1002/hep.31301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323(20):2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Bezerra J, Pochapin M, El-Serag H, Vargo J. JOINT GI SOCIETY MESSAGE: COVID-19 Clinical Insights for Our Community of Gastroenterologists and Gastroenterology Care Providers [Internet]. Default. 2020 [cited 25 August 2020]. Available from: https://www.asge.org/home/joint-gi-society-message-covid-19 [Google Scholar]
- [43].Guan GW, Gao L, Wang JW, et al. [Exploring the mechanism of liver enzyme abnormalities in patients with novel coronavirus-infected pneumonia]. Zhonghua Gan Zang Bing Za Zhi. 2020;28(2):E002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Singh S, Khan A. Clinical characteristics and outcomes of COVID-19 among patients with pre-existing liver disease in USA: a multi-center research network study. Gastroenterology; Published online May 2020. DOI: 10.1053/j.gastro.2020.04.064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].El-Serag H. Joint GI society message: COVID-19 clinical insights for our community of gastroenterologists and gastroenterology care providers. Am Gastroenterol Ass. May 2020. [Google Scholar]
- [47].Li LY, Wu W, Chen S, et al. Digestive system involvement of novel coronavirus infection: prevention and control infection from a gastroenterology perspective. J Dig Dis. 2020;21(4):199–204. [DOI] [PMC free article] [PubMed] [Google Scholar]


