Abstract
Background
A comprehensive evaluation of the burden of inflammation bowel disease (IBD) is important for identifying potential strategies to control the disease. We present results from the Global Burden of Diseases (GBD) 2017 of IBD at the national level, the trends in disease burden and its epidemiological features in China.
Methods
Using the methods and results from GBD 2017, we describe the IBD burden based on the prevalence, incidence, mortality, years of lost (YLLs), the years of life lived with disability (YLDs) and disability-adjusted life years (DALYs) in China estimated using DisMod-MR 2·1. We additionally evaluated the rate of DALYs at national locations in 2017.
Findings
From 1990 to 2017, the cases, deaths, YLLs, YLDs and DALYs for IBD in China were from 1,047,991 to 2,665,081, from 5701 to 5198, from 188,814 to 107,373, from 157,581 to 394,887, from 346,396 to 502,260, respectively. Increasing trends were observed in prevalence (APC: 2·9%), incidence (APC: 1·1%), DALYs (APC: 0·8%) and YLDs (APC:2·9%). There were decreasing trends in mortality (APC: -1·0%) and YLLs (APC: -2·7%). As to the age-standardized rates of DALYs, it observed a decreasing trend (APC: -0·78%). Similar trends were observed in men and women. The age-standardized APCs in incidence, mortality and rate of YLLs among women were higher than those among men. The age-standardized rate of DALYs was 27·51 per 100,000 in 2017.
Interpretation
Between 1990 and 2017, China experienced a decrease in the age-standardized DALYs, mortality rates and YLLs due to IBD, despite an increase in the age-standardized rate of prevalence, incidence and YLDs. China is still one of the low endemic areas.
Funding
This work had no supporting funding.
Research in context.
Evidence before this study
Inflammatory bowel disease is a chronic incurable disease. It has high burden in western countries. At the turn of 21st century, IBD has been a global disease with rising prevalence in newly industrialized countries in Asia. Up to now, disease burden of IBD has been reported in Japan, India, Korea. However, few studies were reported in prevalence and incidence of IBD in China. Little is known about the mortality, DALYs, YLLs and YLDs of IBD in China.
Added value of this study
To evaluate the IBD burden among larger populations at the national level in China, this study will describe the burden trend of prevalence, incidence, mortality, DALYs, YLLs and YLDs of IBD from 1990 to 2017. Additionally, the rate of DALYs was evaluated at national locations in 2017.
Implications of all the available evidence
China is still one of the low endemic areas. Considering an increase in the age standardized rate of prevalence, incidence and YLDs in IBD and the massive population, China should take measures to reduce IBD burden.
Alt-text: Unlabelled box
1. Introduction
Inflammatory bowel disease (IBD) is a chronic incurable disease which comprises ulcerative colitis (UC) and Crohn's disease (CD). It can impede career aspirations, instill social stigma and impair quality of life in patients [1].
IBD used to be more common in Western countries during the industrial revolution but was rarely reported in Asia, Africa and Latin America for a long period [2]. In China, the first case of UC was reported in 1936 and the first case of CD was described in approximately 19503. As the gastroenterologists were not familiar with IBD, and their diagnostic pathway was one of exclusion. The prevalence and incidence of IBD remained low for quite a long period in China. While IBD has steadily increased in the western world such as North America, Europe, Australia and New Zealand since the middle of 20th century. At the turn of 21st century, IBD has become a global disease with rising prevalence in newly industrialized countries in Asia, South America and Middle East. China was included as one of the newly industrialized countries in Asia [4]. As IBD has an unpredictable relapsing and remitting course, complications, hospitalizations, surgeries and use of expensive therapies, its increasing prevalence will lead to a substantial increase in the disease burden [4].
However, most literatures related to the burden of IBD was reported in western countries [1,2,[5], [6], [7]] few were reported on the national burden of IBD in newly industrialized countries, particularly in China [8,9] Due to the lack of a nationwide registration system, it was not abundant for published national, population-based epidemiological data of IBD in China. Only few studies were reported on the incidence and prevalence of IBD in a few regions of China [10], [11], [12]. Xue Li et al. reported the incidence rate of IBD was 1·74 (95% CI: 1·08; 2·40) per 100,000 person years in China [8]. As the data in their studies were only collected from hospitals, some bias may exist. It could potentially result in the underestimation of the true incidence. As a result, comprehensive long-term assessments of IBD burden among larger populations at the national level are required. To address the above need, this study provides an overview of the trends in the disease burden of IBD from 1990 to 2017 from the Global Burden of Disease (GBD) 2017 in China.
2. Methods
2.1. Overview
The GBD study provides a standardized approach for estimating prevalence, incidence, deaths, years of life lost (YLLs), the years of life lived with disability (YLDs) and disability-adjusted life years (DALYs) by cause, age, sex, year and location. The institutional review board of the First Affiliated Hospital of Zhejiang University in Zhejiang Province, Hangzhou, China, determined that the study did not need approval because it used publicly available data. This study complied with the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) recommendations [13].
The GBD 2017 used multiple methods to integrate a large number of available data sources with the specific epidemiology of each disease, and the Bayesian meta-regression tool DisMod-MR V.2·1 was used as the main method of estimation [14]. Detailed information about data resources, definitions, statistical modeling and efforts to improve data quality have been previously reported [[14], [15], [16], [17]].
We extracted GBD 2017 data on IBD in China from 1990 to 2017 using the Global Health Data Exchange (GHDx) [18]. The variables obtained from these data included year, age, sex and location. The incidence, prevalence, mortality and DALYs were used as the primary metrics to assess the impacts on health within population. The total number of IBD cases and rates of each metrics were provided by the GBD 2017. Prevalence rate (per 100 000) was defined as aggregated cases (including new cases and previously diagnosed cases) divided by the population size; incidence rate (per 100 000) was defined as the number of new cases divided by the population size; mortality rate (per 100 000) was defined as the number of annual deaths divided by the total population size; YLLs were calculated as the sum of each death multiplied by the standard life expectancy at each age and DALYs were summed by YLLs and YLDs.
2.2. Statistical analysis
Analyses were completed using Stata version 13·1, Python version 2·7, or R version 3·3 [14]. All rates are expressed as age-standardized based on the GBD reference population unless otherwise specified. Uncertainty is estimated with each metrics and propagated throughout the GBD modeling process. 95% uncertainty intervals (95% UIs) are calculated by the 2·5th and 97·5th percentiles of the draw-level values (1000 draws for each metric) [19]. The annual percentage change (APC) were extracted from GHDx to evaluate trends in disease burden [18]. As the 95% Confidence Interval (95%CI) related to APC extracted was missing, Joinpoint Regression Program (Version 4.7.0.0, February 2019) was used to calculate the average annual percentage change. The values of APC were calculated as [(Exp(bi)−1)] × 100, where bi represents the slope of the period segment. The Z test was used to assess whether an APC was different from zero. The terms ‘increase’ and ‘decrease’ were used when the slope of the trend was statistically significant, while ‘stable’ referred to a non-significant trend.
Role of Funding Source: Not applicable.
3. Results
In China, there were 1·04 million (95%UI 0·96, 1·12) new cases in 2017 and 5198 (95%UI 4842, 6382) deaths due to IBD. Age-standardized rates of prevalence, incidence, mortality, DALYs, YLDs and YLLs for IBD in 2017 were 136·25 cases (95%UI 125·37, 147·4) per 100 000, 60·37 new cases (95% UI 56·06, 65·36) per 100 000, 0·33 deaths (95% UI 0·31, 0·41) per 100 000, 27·51 DALYs (95% UI 21·10, 34·95) per 100 000, 20.37 YLDs (95% UI: 13·87, 27·70) per 100 000 and 7·14 YLLs (95% UI 6·44, 8·00) per 100 00 (table 1).
Table 1.
Number and Age-standardized Rates of Prevalence, Incidence, Deaths, YLLs, YLDs, and DALYs in 2017 for IBD in China.
| Measure | All-ages cases | age-standardized rates per 100 000 |
|---|---|---|
| Prevalence | 2,665,081·31 (2,433,418·64,2,900,745·26) | 136·25 (125·37, 147·44) |
| Incidence | 1,035,160·80 (955,409·19,1,121,047·12) | 60·37 (56·06,65·36) |
| Deaths | 5198·80 (4842·48,6382·74) | 0·33 (0·31,0·41) |
| DALYs | 502,260·64 (380,117·22,646,617·71) | 27·51 (21·10,34·95) |
| YLDs | 394,887·43 (269,861·71,538,490·11) | 20·37 (13·87,27·70) |
| YLLs | 107,373·21 (98,982·88,122,574·72) | 7·14 (6·44,8·00) |
YLLs=years of life lost, YLDs=years lived with disability, DALYs=disability-adjusted life-years.
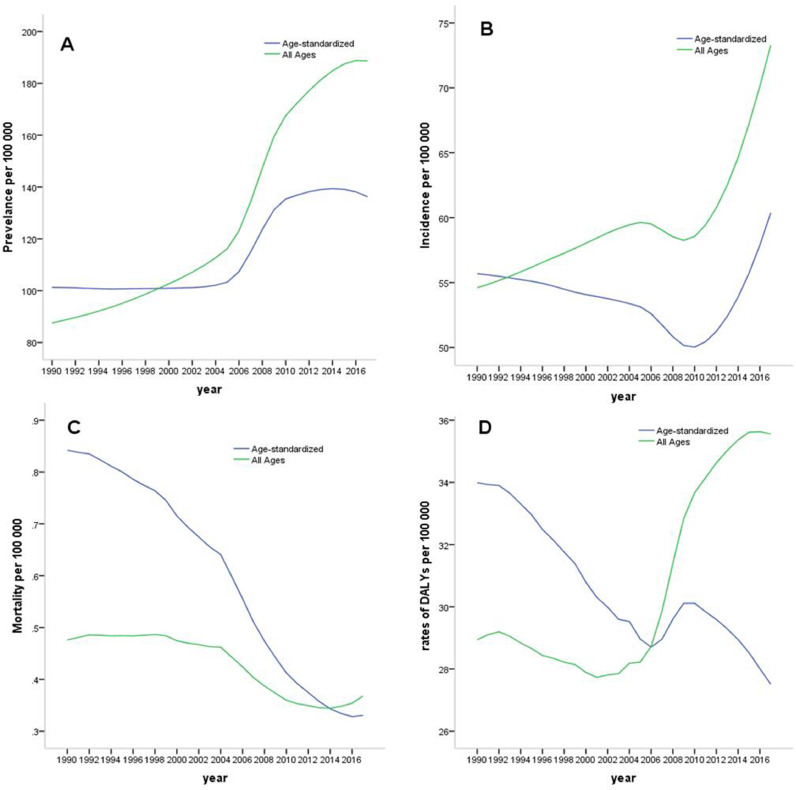
As shown in table 2 and Fig. 1, there were increasing trends from 1990 to 2017 in prevalence (APC: 2·9%), incidence (APC: 1·1%), DALYs (APC: 0·8%) and YLDs (APC:2·9%). There were decreasing trends from 1990 to 2017 in mortality (APC: −1·0%) and YLLs (APC: −2·7%). Surprisingly, it observed a decreasing trend for the age-standardized rates of DALYs (APC: −0·8%) from 1990 to 2017.
Table 2.
all-age and age-standardized annual percentage changes between 1990 and 2017.
| Measure | All ages |
Age standardized |
||||
|---|---|---|---|---|---|---|
| Total | Male | Female | Total | Male | Female | |
| Prevalence | 2·9% (2·7%,3·1%) | 2·9% (2·8%,2·9%) | 2·9% (2·8%,3·0%) | 1·2% (1·0%,1·3%) | 1·2% (1·1%,1·3%) | 1·1% (0·9%,1·2%) |
| Incidence | 1·1% (1·0%,1·2%) | 0·9% (0·9%,1·0%) | 1·2% (1·1%,1·3%) | 0·3% (0·2%,0·3%) | 0·2% (0·1%,0·2%) | 0·4% (0·3%,0·4%) |
| Deaths | −1·0% (−1·2%,−0·8%) | −0·5% (−0·6%,−0·3%) | −1·5% (−1·8%,−1·3%) | −3·5% (−3·6%,−3·3%) | −2·9% (−3·0%,−2·8%) | −3·9% (−4·1%,−3·8%) |
| DALYs | 0·8% (0·6%,0·9%) | 0·6% (0·4%,0·7%) | 0·9% (0·8%,1·0%) | −0·8% (−0·9%,−0·6%) | −0·9% (−1·0%,−0·7%) | −0·7% (−0·8%,−0·6%) |
| YLLs | −2·7% (−3·0%,−2·4%) | −2·2% (−2·4%,−2·1%) | −3·3% (−3·5%,−3·0%) | −3·6% (−3·7%,−3·4%) | −3·6% (−4·0%,−3·2%) | −4·1% (−4·3%,−4·0%) |
| YLDs | 2·9% (2·6%,3·1%) | 2·8% (2·7%,2·9%) | 2·9% (2·8%,3·0%) | 1·1% (1·0%,1·2%) | 1·2% (1·1%,1·2%) | 1·1% (1·0%,1·2%) |
DALYs=disability-adjusted life years, YLLs=years of life lost, YLDs=years lived with disability.
Fig. 1.
Observed and age-standardized rates (ARs) of IBD from 1990 to 2017 in China. (A) Observed and ARs of the prevalence; (B) Observed and ARs of the incidence; (C) Observed and ARs of the mortality; (D) Observed and ARs of the DALYs. DALYs=disability-adjusted life years.
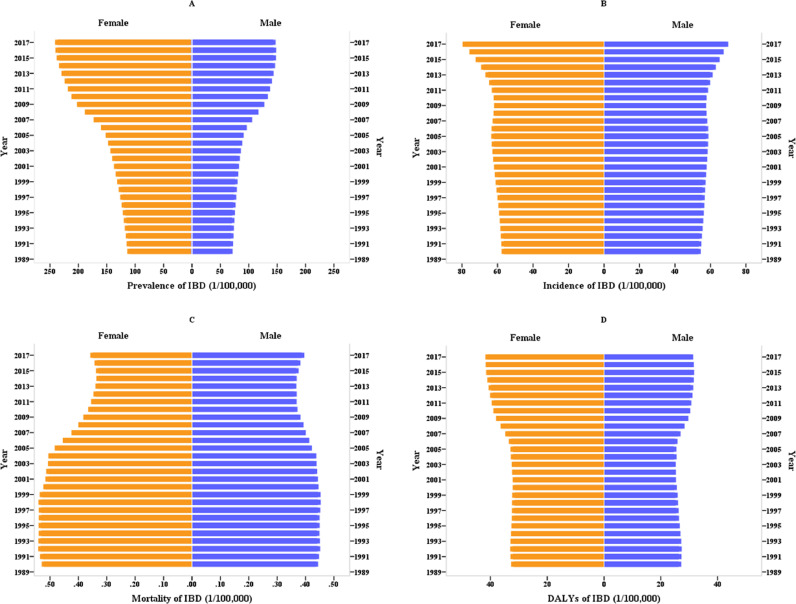
Increasing trends in prevalence, incidence, DALYs and YLDs were seen among females and males for all ages (APC: 2·9%, 1·2%, 0·9% and 2.9% in female, 2·9%, 0·9%, 0·6% and 2·8% in male, respectively). A decreasing trend was observed in mortality and YLLs among females and males (APC: −1·5% and −3·3% in female, −0·5% and −2·2% in male, respectively). The all-ages annual percentage changes in prevalence, incidence, mortality and rate of DALYs among females were higher than those among males (Fig. 2). As to the prevalence, DALYs and YLDs, the age-standardized annual percentage changes was higher in males than females, while the incidence, deaths and YLLs was higher in females than males (table 2).
Fig. 2.
Disease burden of IBD among different sex groups from 1990 to 2017 in China. (A) The differences in prevalence between males and females; (B) the differences in incidence between males and females; (C) the differences of mortality between males and females; (D) the differences in DALYs between males and females. DALYs=disability-adjusted life years.
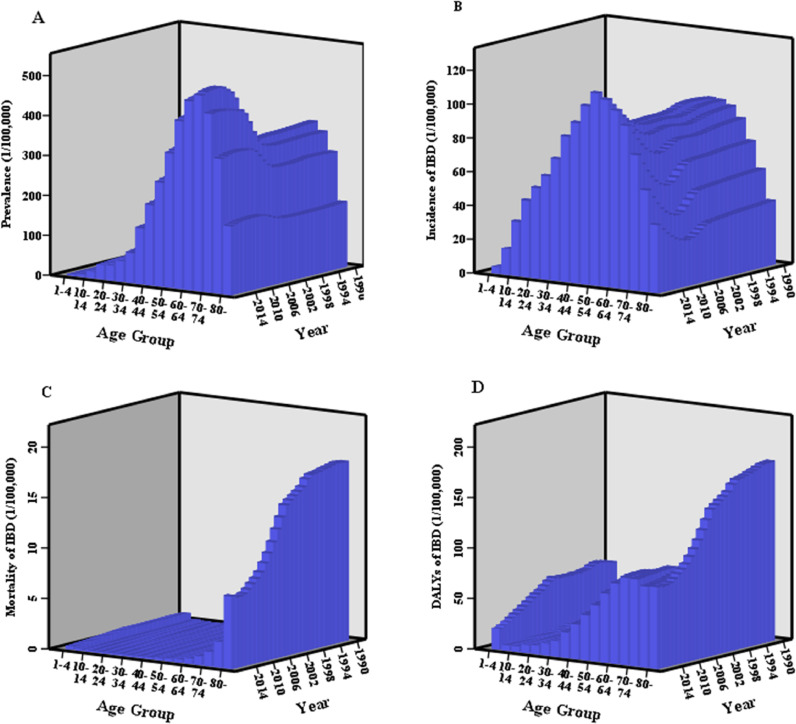
Fig. 3 shows the rates of IBD among different age groups. IBD of over 100/100 000 rate was more prevalent among individuals aged over 35 and increased rapidly between the ages of 30 and 69. The highest prevalence rate was observed in those aged 65–69. Similar tendency was observed in incidence with highest rate among those aged 50–55. The incidence was observed over 20/100 000 in those aged over 15. The mortality began to increase rapidly from the age of 60 with rates that were consistently high among those aged over 80. The rate of DALYs was over 50/100 000 among those aged over 50.
Fig. 3.
Disease burden of IBD among different age groups from 1990 to 2017 in China. (A) The changes in prevalence of IBD among different age groups; (B) the changes in incidence of IBD among different age groups; (C) the changes in mortality of IBD among different age groups; (D) the changes in rates of DALYs for IBD among different age groups. DALYs=disability-adjusted life years.
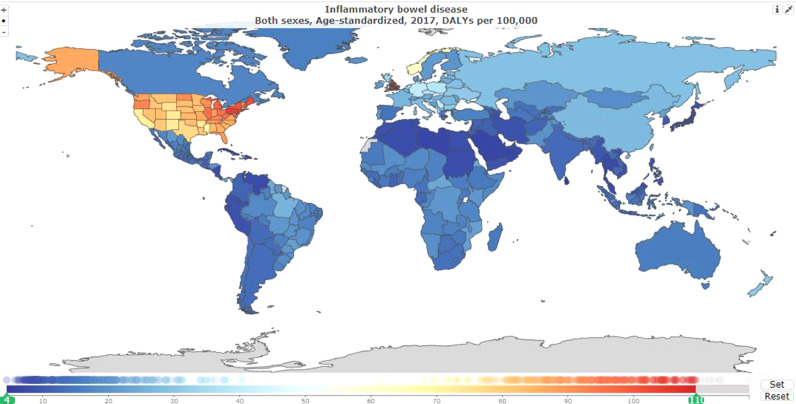
Fig. 4 illustrates the rate of DALYs in IBD by GBD country and sub-national locations in 2017 for both sexes combined. The geographical variation in IBD of DALYs across countries is shown: the age-standardized rate of DALYs with over 100 per 100,000 was seen in 11 of 195 countries and territories, including Connecticut, Maine, Massachusetts, New Hampshire, New York, Pennsylvania, Rhode Island, North East England, North West England, East of England and South West England. The age-standardized rate of DALYs with 51~100 per 100,000 was seen in 51 of 195 countries and territories. The age-standardized rate of DALYs with below 50 per 100,000 was seen in other countries and territories, and in China it was 27·51 (95%UI: 21·1, 34·95) per 100,000.
Fig. 4.
Age-standardized rate of DALYs per 100,000 for IBD by location for both sexes, 2017.
4. Discussion
This study described the disease burden of IBD in China, revealing that the prevalence, incidence and YLDs persisted to increase between 1990 and 2017. As IBD is the product of industrialization, it is easily to understand the increasing trend due to the rapidly expanding urbanization and developing industry occurring in China. Similar increasing trends were seen in Hong Kong from 1991 to 2006 [20,21], Taiwan from 1998 to 2008 [22], Brail from 1988 to 2012 [23], Malaysia from 1990 to 2013 [24], Tuzla from 1995 to 2006 [25,26], Songpa from 1991 to 2005 [27]. However, some reports showed declining incidence of IBD in parts of North America and Europe [4]. Despite the incidence in parts of North America had declining trend, there were still approximate more than two million North Americans live with IBD today, and that population is forecasted to be approaching four million by 2030 [1,28,29].
Although the incidence of IBD increased between 1990 and 2017, the burden in terms of mortality and YLLs improved. It is not surprising that China has experienced a rapid social and economic development over the past three decades. Transformation of the social economy has accelerated the process of industrialization and health political developments, including China's social health insurance programs. For instance, the urban employee-based basic medical insurance program (UEBMI) was launched in 1998, the rural new cooperative medical program (NCMS) was launched in 2003 and the urban resident-based basic medical insurance program (URBMI) was launched in 2007 [30]. With these developments, the general population had enough public health insurance, leading to pay more attention to their own health. In addition, increasing clinicians had been trained to have adequate experience in the diagnosis and treatment of IBD [31].
In Western countries, it showed an equal gender distribution for UC and a slight female predominance for CD [[32], [33], [34]]. In contrast, data from Asian countries showed male predominance for CD and an equal gender distribution for UC [35,36]. In China, the male-to-female ratio is around 2·32:1 in CD and 1·53:1 in UC [10]. The reason remained unexplained for this difference in gender ratio between Asian and Western populations. Smoking could explain the male predominance in IBD incidence [37]. Although the smoking rate is much higher in men (50%) than that in women (11%) [38], some held the view that smoking could not fully explain the difference in CD prevalence between gender distribution [39]. However, there was a paradox that the male-to female ratio was 0·6:1 in IBD prevalence and incidence (data could be obtained in GHDx) [18]. The possible reason was that sample in the GBD 2017 was larger and more reliable than that in Jiang L's study [10]. Similar to the total trends, the prevalence, incidence, DALYs and YLDs among males and females for all-ages increased, while the mortality and YLLs decreased from 1990 to 2017.
Although IBD was primarily diagnosed at middle age, the prevalence rate was on the rise among the elderly for the aging population increasing worldwide. Due to the longer disease duration, the mortality began to increase at the age of 60 with highest rates at age of over 80. In addition, the results in this study was in consistent with the previous literature, which reported that the proportion diagnosed was rising among the children and adolescents [40]. According to the China Statistical Yearbook 2017, children and adolescents aged <14 accounted for 16.8% at the end of 2017 [41]. It could explain why IBD was less prevalent among individuals aged <14. Data from the West showed that IBD is characterized by a bimodal age distribution with peaks at age groups 20–39 and 60–79 years [42]. In this study, the peak of IBD incidence rate was observed at age groups 50–55.
Little data were available on DALYs in IBD patients in China. Here, we found that the burden of IBD was still low in China, unlike the Western countries with higher DALYs such as the Europe and north America. Given the massive population in China, IBD should be paid more attention. Luckily, the health care delivered improved resulting from the economic progression. The implementation of sigmoidoscopy or colonoscopy enhanced the detection of IBD [25]. In the era of Internet, social media emerged as a group of internet-based applications that allow users to exchange information and create content [43]. In China, there are several IBD-related social media widely used, such as Baidu blog, WeChat, Dingxiang Yisheng and Haodaifu. Among them, WeChat is the most popular mobile app. As a result, increasing IBD patients are inclined to use social media as part of their disease management [31]. They could change their attitude and the way they deal with the illness through seeking information from social media. It was reported that there was 59.3% of IBD patients seeking information from social media [31].
However, there were no predictive forecasting models of the prevalence and economic impact of IBD in China, which should be resolved in the future. Luckily for IBD patients, China Crohn's and Colitis Foundation (CCCF) has been established to improve their quality of life (QOL) through education and training. CCCF is a nonprofit, volunteer-driven organization founded in Hangzhou, China. Now it has a total of 5 programs in action: IBD specialist training programs, IBD patients’ health education programs, health care professionals-patients network project, fundraising program, and volunteer program [31]. According to Kaplan GG, the strategies to reduce burden of IBD included establishing the predictive forecasting models of the prevalence and economic impact of IBD, ensuring the equality and affordability of IBD management, funding research on interactions between genes, the environment and intestinal microbes [1].
There were several limitations in this study. First, general limitations of the GBD 2017 exist and have been illustrated [14,15,19]. One of the main limitations of measuring IBD burden in China was a lack of reliable incidence data. In China, there were no IBD research centers or monitor system. These data may be not nationally representative. The estimates depend on sophisticated statistical modeling to address sparse and inconsistent data, data collection and model selection may cause errors, and which may be addressed in the next iteration of the GBD study. Additionally, our study does not include the differences of IBD incidence and prevalence in Chinese ethic populations or factors related to UC and CD, respectively.
In conclusion, China still experienced an increase in the age-standardized prevalence rate and incidence rate between 1990 and 2017. Due to the improved health care delivery, the age-standardized rate of DALYs, deaths and YLLs due to IBD decreased. Female predominance was in IBD patients. The highest incidence rate was observed at age groups 50–55. China is still one of the low endemic areas of DALYs for IBD. Regarding the massive population, strategies should be considered in the future to reduce the burden of IBD.
Declaration of copeting interests
We declare no competing interests.
Acknowledgments
Author contributions
QY contributed to the concept of the manuscript and completed the first draft of the manuscript. RW, LY, CWE, PXH and RJJ contributed to the discussion part of the manuscript. All authors contributed to the framework construction, results interpretation, manuscript revision, and approved the final version of the manuscript. The corresponding authors attest that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Data sharing statement
All the data may be available from the corresponding author by request or the IHME website (http://ghdx.healthdata.org/gbd-results-tool).
Acknowledgements
Not applicable.
Funding
This work had no supporting funding.
Contributor Information
Xiao-hua Pan, Email: pxh77@qq.com.
Jing-jing Ren, Email: 3204092@zju.edu.cn.
References
- 1.Kaplan G.G. The global burden of IBD: from 2015 to 2025. Nat Rev Gastroenterol Hepatol. 2015;12(12):720–727. doi: 10.1038/nrgastro.2015.150. [DOI] [PubMed] [Google Scholar]
- 2.de Groof E.J., Rossen N.G., van Rhijn B.D., Karregat E.P., Boonstra K., Hageman I. Burden of disease and increasing prevalence of inflammatory bowel disease in a population-based cohort in the Netherlands. Eur J Gastroenterol Hepatol. 2016;28(9):1065–1072. doi: 10.1097/MEG.0000000000000660. [DOI] [PubMed] [Google Scholar]
- 3.Chen M.H., Mao R. Diagnosis and treatment of Chinese inflammatory bowel disease for 100 years. Chin J Dig. 2015;35(1):6–9. [Google Scholar]
- 4.Ng S.C., Shi H.Y., Hamidi N., Underwood F.E., Tang W., Benchimol E.I. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390(10114):2769–2778. doi: 10.1016/S0140-6736(17)32448-0. [DOI] [PubMed] [Google Scholar]
- 5.Rocchi A., Benchimol E.I., Bernstein C.N., Bitton A., Feagan B., Panaccione R. Inflammatory bowel disease: a Canadian burden of illness review. Can J Gastroenterol. 2012;26(11):811–817. doi: 10.1155/2012/984575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coward S., Clement F., Benchimol E.I., Bernstein C.N., Avina-Zubieta J.A., Bitton A. Past and future burden of inflammatory bowel diseases based on modeling of population-based data. Gastroenterology. 2019;156(5):1345–1353. doi: 10.1053/j.gastro.2019.01.002. [DOI] [PubMed] [Google Scholar]
- 7.Burisch J., Jess T., Martinato M., Lakatos P.L. ECCO-EpiCom. The burden of inflammatory bowel disease in Europe. J. Crohn's Colitis. 2013;7(4):322–337. doi: 10.1016/j.crohns.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Li X., Song P., Li J., Tao Y., Li G., Li X. The disease burden and clinical characteristics of inflammatory bowel disease in the Chinese population: a systematic review and meta-analysis. Int J Environ Res Public Health. 2017;14(3):238. doi: 10.3390/ijerph14030238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cui G., Yuan A. A systematic review of epidemiology and risk factors associated with Chinese inflammatory bowel disease. Front Med (Lausanne) 2018;5:183. doi: 10.3389/fmed.2018.00183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jiang L., Xia B., Li J., Ye M., Yan W., Deng C. Retrospective survey of 452 patients with inflammatory bowel disease in Wuhan city, central China. Inflamm Bowel Dis. 2006;12:212–217. doi: 10.1097/01.MIB.0000201098.26450.ae. [DOI] [PubMed] [Google Scholar]
- 11.Zhao J., Ng S.C., Lei Y., Yi F., Li J., Yu L. First prospective, population-based inflammatory bowel disease incidence study in mainland of China: the emergence of “western” disease. Inflamm Bowel Dis. 2013;19(9):1839–1845. doi: 10.1097/MIB.0b013e31828a6551. [DOI] [PubMed] [Google Scholar]
- 12.Zeng Z., Zhu Z., Yang Y., Ruan W., Peng X., Su Y. Incidence and clinical characteristics of inflammatory bowel disease in a developed region of Guangdong Province, China: a prospective population-based study. J Gastroenterol Hepatol. 2013;28(7):1148–1153. doi: 10.1111/jgh.12164. [DOI] [PubMed] [Google Scholar]
- 13.Stevens G.A., Alkema L., Black R.E., Boerma J.T., Collins G.S., Ezzati M. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet. 2016;388:e19–e23. doi: 10.1016/S0140-6736(16)30388-9. [DOI] [PubMed] [Google Scholar]
- 14.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.GBD 2017 Causes of Death Collaborators. Global Regional and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murray C.J., Ezzati M., Flaxman A.D., Lim S., Lozano R., Michaud C. GBD 2010: design, definitions, and metrics. Lancet. 2012;380(9859):2063–2066. doi: 10.1016/S0140-6736(12)61899-6. [DOI] [PubMed] [Google Scholar]
- 17.Murray C.J., Lopez A.D. Measuring the global burden of disease. N Engl J Med. 2013;369:448–457. doi: 10.1056/NEJMra1201534. [DOI] [PubMed] [Google Scholar]
- 18.Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2017 (GBD 2017) Results. http://ghdx.healthdata.org/gbd-results-tool(accessed 3 Oct2019).
- 19.G.B.D. 2017 Mortality Collaborators. Global, regional, and national age-specific mortality and life expectancy, 1950-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392: 1684–735. [DOI] [PMC free article] [PubMed]
- 20.Lok K.H., Hung H.G., Ng C.H., Kwong K.C., Yip W.M., Lau S.F. Epidemiology and clinical characteristics of ulcerative colitis in Chinese population: experience from a single center in Hong Kong. J Gastroenterol Hepatol. 2008;23(3):406–410. doi: 10.1111/j.1440-1746.2007.05079.x. [DOI] [PubMed] [Google Scholar]
- 21.Lok K.H., Hung H.G., Ng C.H., Li K.K., Li K.F., Szeto M.L. The epidemiology and clinical characteristics of Crohn's disease in the Hong Kong Chinese population: experiences from a regional hospital. Hong Kong Med J. 2007;13(6):436–441. [PubMed] [Google Scholar]
- 22.Wei S.C., Lin M.H., Tung C.C., Weng M.T., Kuo J.S., Shieh M.J. A nationwide population-based study of the inflammatory bowel diseases between 1998 and 2008 in Taiwan. BMC Gastroenterol. 2013;13:166. doi: 10.1186/1471-230X-13-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parente J.M., Coy C.S., Campelo V., Parente M.P., Costa L.A., da Silva R.M. Inflammatory bowel disease in an underdeveloped region of northeastern Brazil. World J Gastroenterol. 2015;21(4):1197–1206. doi: 10.3748/wjg.v21.i4.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ng S.C., Tang W., Leong R.W., Chen M., Ko Y., Studd C. Environmental risk factors in inflammatory bowel disease: a population-based case-control study in Asia-Pacific. Gut. 2015;64(7):1063–1071. doi: 10.1136/gutjnl-2014-307410. [DOI] [PubMed] [Google Scholar]
- 25.Pavlovic-Calic N., Salkic N.N., Gegic A., Smajic M., Alibegovic E. Crohn's disease in Tuzla region of Bosnia and Herzegovina: a 12-year study (1995-2006) Int J Colorectal Dis. 2008;23(10):957–964. doi: 10.1007/s00384-008-0493-1. [DOI] [PubMed] [Google Scholar]
- 26.Salkic N.N., Pavlovic-Calic N., Gegic A., Jovanovic P., Basic M. Ulcerative colitis in the Tuzla region of Bosnia and Herzegovina between 1995 and 2006: epidemiological and clinical characteristics. Eur J Gastroenterol Hepatol. 2010;22(3):346–353. doi: 10.1097/MEG.0b013e32832bfe05. [DOI] [PubMed] [Google Scholar]
- 27.Yang S.K., Yun S., Kim J.H., Park J.Y., Kim H.Y., Kim Y.H. Epidemiology of inflammatory bowel disease in the Songpa Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008;14(4):542–549. doi: 10.1002/ibd.20310. [DOI] [PubMed] [Google Scholar]
- 28.Ananthakrishnan A.N. Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol. 2015;12(4):205–217. doi: 10.1038/nrgastro.2015.34. [DOI] [PubMed] [Google Scholar]
- 29.Coward S., Clement F., Benchimol E.I., Bernstein C.N., Bitton A., Carroll M. Analyzing the rising prevalence of IBD: predicting the prevalence in 2030 by age group. Gastroenterology. 2018;154(6):S992–S993. [Google Scholar]
- 30.Meng Q., Fang H., Liu X., Yuan B., Xu J. Consolidating the social health insurance schemes in China: towards an equitable and efficient health system. Lancet. 2015;386(10002):1484–1492. doi: 10.1016/S0140-6736(15)00342-6. [DOI] [PubMed] [Google Scholar]
- 31.Chen Y. Perspectives of IBD China: is Crohn's and Colitis Foundation Model a Solution to Health Care Issues for the Country? Inflamm Bowel Dis. 2018;24(5):925–929. doi: 10.1093/ibd/izy056. [DOI] [PubMed] [Google Scholar]
- 32.Bernstein C.N., Wajda A., Svenson L.W., MacKenzie A., Koehoorn M., Jackson M. The epidemiology of inflammatory bowel disease in Canada: a population-based study. Am J Gastroenterol. 2006;101(7):1559–1568. doi: 10.1111/j.1572-0241.2006.00603.x. [DOI] [PubMed] [Google Scholar]
- 33.Vind I., Riis L., Jess T., Knudsen E., Pedersen N., Elkjaer M. Increasing incidences of inflammatory bowel disease and decreasing surgery rates in Copenhagen City and County, 2003-2005: a population-based study from the Danish Crohn colitis database. Am J Gastroenterol. 2006;101(6):1274–1282. doi: 10.1111/j.1572-0241.2006.00552.x. [DOI] [PubMed] [Google Scholar]
- 34.Jr Loftus EV. Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology. 2004;126(6):1504–1517. doi: 10.1053/j.gastro.2004.01.063. [DOI] [PubMed] [Google Scholar]
- 35.Cosnes J., Gower-Rousseau C., Seksik P., Cortot A. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011;140(6):1785–1794. doi: 10.1053/j.gastro.2011.01.055. [DOI] [PubMed] [Google Scholar]
- 36.Hou J.K., El-Serag H., Thirumurthi S. Distribution and manifestations of inflammatory bowel disease in Asians, Hispanics, and African Americans: a systemic review. Am J Gastroenterol. 2009;104(8):2100–2109. doi: 10.1038/ajg.2009.190. [DOI] [PubMed] [Google Scholar]
- 37.Ng S.C., Bernstein C.N., Vatn M.H., Lakatos P.L., Jr Loftus EV, Tysk C. Geographical variability and environmental risk factors in inflammatory bowel disease. Gut. 2013;62(4):630–649. doi: 10.1136/gutjnl-2012-303661. [DOI] [PubMed] [Google Scholar]
- 38.Giovino G.A., Mirza S.A., Samet J.M., Gupta P.C., Jarvis M.J., Bhala N. Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys. Lancet. 2012;380(9842):668–679. doi: 10.1016/S0140-6736(12)61085-X. [DOI] [PubMed] [Google Scholar]
- 39.Yang S.K. How Does the Epidemiology of Inflammatory Bowel Disease Differ between East and West? A Korean Perspective. Inflamm Intest Dis. 2017;2(2):95–101. doi: 10.1159/000454712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Armitage E., Drummond H.E., Wilson D.C., Ghosh S. Increasing incidence of both juvenile-onset Crohn's disease and ulcerative colitis in Scotland. Eur J Gastroenterol Hepatol. 2001;13(12):1439–1447. doi: 10.1097/00042737-200112000-00007. [DOI] [PubMed] [Google Scholar]
- 41.National bureau of statistics of China. China Stat Yearb. 2018 http://www.stats.gov.cn/tjsj/ndsj/2018/indexeh.htm (access on 12 Dec, 2019) [Google Scholar]
- 42.Kedia S., Ahuja V. Epidemiology of IBD in India: the Great Shift East. Inflamm Intest Dis. 2017;2(2):102–115. doi: 10.1159/000465522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guo L., Reich J., Groshek J., Farraye F.A. Social media use in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016;22(5):1231–1238. doi: 10.1097/MIB.0000000000000713. [DOI] [PubMed] [Google Scholar]