Abstract
Background
COVID-19 pandemic has created a need to identify potential predictors of severe disease. We performed a systematic review and meta-analysis of gastrointestinal predictors of severe COVID-19.
Methods
An extensive literature search was performed using PubMed, Embase, Web of Science and Cochrane. Odds ratio (OR) and mean difference (MD) were calculated for proportional and continuous outcomes using a random-effect model. For each outcome, a 95% confidence interval (CI) and P-value were generated.
Results
A total of 83 studies (26912 patients, mean age 43.5±16.4 years, 48.2% female) were included. Gastrointestinal predictors of severe COVID-19 included the presence of diarrhea (OR 1.50, 95%CI 1.10-2.03; P=0.01), elevated serum aspartate aminotransferase (AST) (OR 4.00, 95%CI 3.02-5.28; P<0.001), and elevated serum alanine aminotransferase (ALT) (OR 2.54, 95%CI 1.91-3.37; P<0.001). Significantly higher levels of mean AST (MD 14.78 U/L, 95%CI 11.70-17.86 U/L; P<0.001), ALT (MD 11.87 U/L, 95%CI 9.23-14.52 U/L; P<0.001), and total bilirubin (MD 2.08 mmol/L, 95%CI 1.36-2.80 mmol/L; P<0.001) were observed in the severe COVID-19 group compared to non-severe COVID-19 group.
Conclusion
Gastrointestinal symptoms and biomarkers should be assessed early to recognize severe COVID-19.
Keywords: SARS-CoV-2, COVID-19, diarrhea, severe COVID-19, predictors
Introduction
COVID-19, caused by SARS-CoV-2, has become a worldwide pandemic imposing a significant burden on healthcare systems around the globe. The virus causes a variety of manifestations, including pneumonia, acute respiratory distress syndrome, shock, sepsis, and death [1]. Currently, no specific therapy (preventive or therapeutic) is available for this disease [2].
Symptomatically, the virus leads to fever, fatigue, cough, shortness of breath, myalgias, arthralgias, nasal congestion, runny nose, sore throat, nausea/vomiting, and diarrhea [1]. The virus further causes laboratory abnormalities, including derangements of white cell count, platelet count, C-reactive protein, procalcitonin, lactate dehydrogenase, aspartate aminotransferase (AST), alanine aminotransferase (ALT), total bilirubin (TB), creatinine, and D-dimer [1]. The pandemic nature of this disease necessitates emergent and early recognition of symptomatic patients to identify those at most severe risk and to provide supportive measures as needed, up to and including mechanical ventilation.
Gastrointestinal parameters (symptoms and laboratory findings) have been reported in the literature among patients with COVID-19 [3], but there is little comprehensive information regarding gastrointestinal symptoms in these patients. We performed a systematic review and meta-analysis to evaluate whether gastrointestinal symptoms and abnormal laboratory findings predict disease severity.
Materials and methods
A comprehensive literature search was performed from January 1st, 2020, to May 31st, 2020, using the following databases: PubMed/Medline, Embase, Cochrane, Web of Science. The search strategy, using a predeveloped vocabulary for COVID-19 [4], was created by an experienced librarian (WLS) and crosschecked by another reviewer (MA). An example search strategy using EMBASE is highlighted in Supplementary Table 1 (421.2KB, pdf) . Article screening and data extraction was performed by 2 independent reviewers (MA and HH) and any discrepancies in screening/extraction were resolved through mutual discussion. Interobserver agreement was evaluated using % of agreement and Cohen’s Kappa (Κ) statistic. Articles were selected if they reported data on COVID-19 patients with respect to gastrointestinal symptoms (diarrhea, abdominal pain, and nausea/vomiting) or laboratory findings (serum AST, ALT, or TB). We excluded articles if the data of interest were not reported or the article had not undergone a peer-review process. We further excluded case reports and retrospective studies/case series reporting <10 cases. We used the bibliography of the finalized articles to further broaden our literature search. We did not restrict our search according to language.
Severe COVID-19 was defined as respiratory distress (rate ≥30 /min, oxygen saturation ≤93% at rest and/or PaO2/FiO2 ≤300 mmHg) [1], intensive care unit (ICU) admission, and/or death. Laboratory data (mean serum AST, ALT and TB) were reported based on the local laboratory’s reference parameters for each study. Symptoms (diarrhea and nausea/vomiting) were reported based on initial presentation.
Statistical analysis
Data extraction was performed using Microsoft Excel (Microsoft, Redmond, Wash, USA). Continuous variables (using mean and standard deviation [SD]) and proportional variables (using event and total patients) were compared using the DerSimonian-Laird approach or a random-effects model. The fixed effect model was used as a sensitivity tool; however, given the presumed heterogeneity of study data from diverse sources and clinical settings, the random-effects model was considered more appropriate and results were reported using that approach [5,6]. The mean and SD were calculated from median and interquartile range where applicable. Results are displayed using forest plots for each summary estimate, i.e., mean difference (MD) and odds ratio (OR) for continuous and proportional variables, respectively. A 95% confidence interval (CI), P-value (<0.05 was considered statistically significant), and study heterogeneity using I2 statistic (>50% was considered as substantial heterogeneity) were calculated for each outcome [7]. Subgroup analysis was performed based on the definition of severe COVID-19 (respiratory distress, ICU admission, and death) if at least 3 studies reported the outcome. Sensitivity analysis using leave-one-out meta-analysis was performed and point estimates were generated. Meta-regression was attempted to assess the impact of moderator variables on study outcomes. The moderator variables assessed included female proportions in each study, region of study (Asia, Europe, North America, South America), and number of centers in each study (single center, dual center, multicenter). The statistical analysis was performed using Open Meta Analyst (CEBM, University of Oxford, Oxford, United Kingdom) and Comprehensive Meta-Analysis (BioStat, Englewood, NJ, USA).
We utilized the Quality in Prognostic Studies (QUIPS) tool for assessing the risk of bias in the observational studies [8]. Publication bias was assessed qualitatively by visualizing the funnel plot and quantitatively using Egger’s regression analysis. We adhered to “preferred reporting items for systematic reviews and meta-analyses (PRISMA)” guidelines for the purposes of this manuscript.
Results
Literature search
Using the search strategy defined above, a total of 1525 records were generated. After the inclusion/exclusion criteria had been applied, a total of 83 published studies (all observational) remained that reported data on gastrointestinal symptoms and/or laboratory findings (Fig. 1) [1,3,9-89]. All studies included laboratory-confirmed COVID-19 patients. The percentage of agreement was >90% for both screening and data extraction and corresponding Κ values of 0.72 and 0.69 (substantial agreement), respectively, were noted. Of the 83 included studies, 42 reported data on disease severity with respect to symptoms and/or lab findings.
Figure 1.
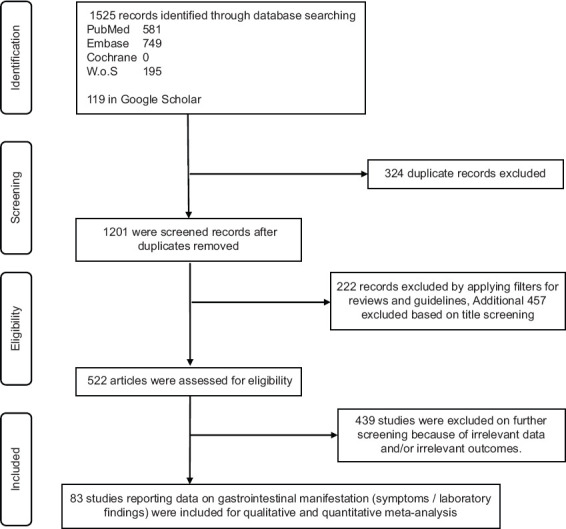
PRISMA diagram
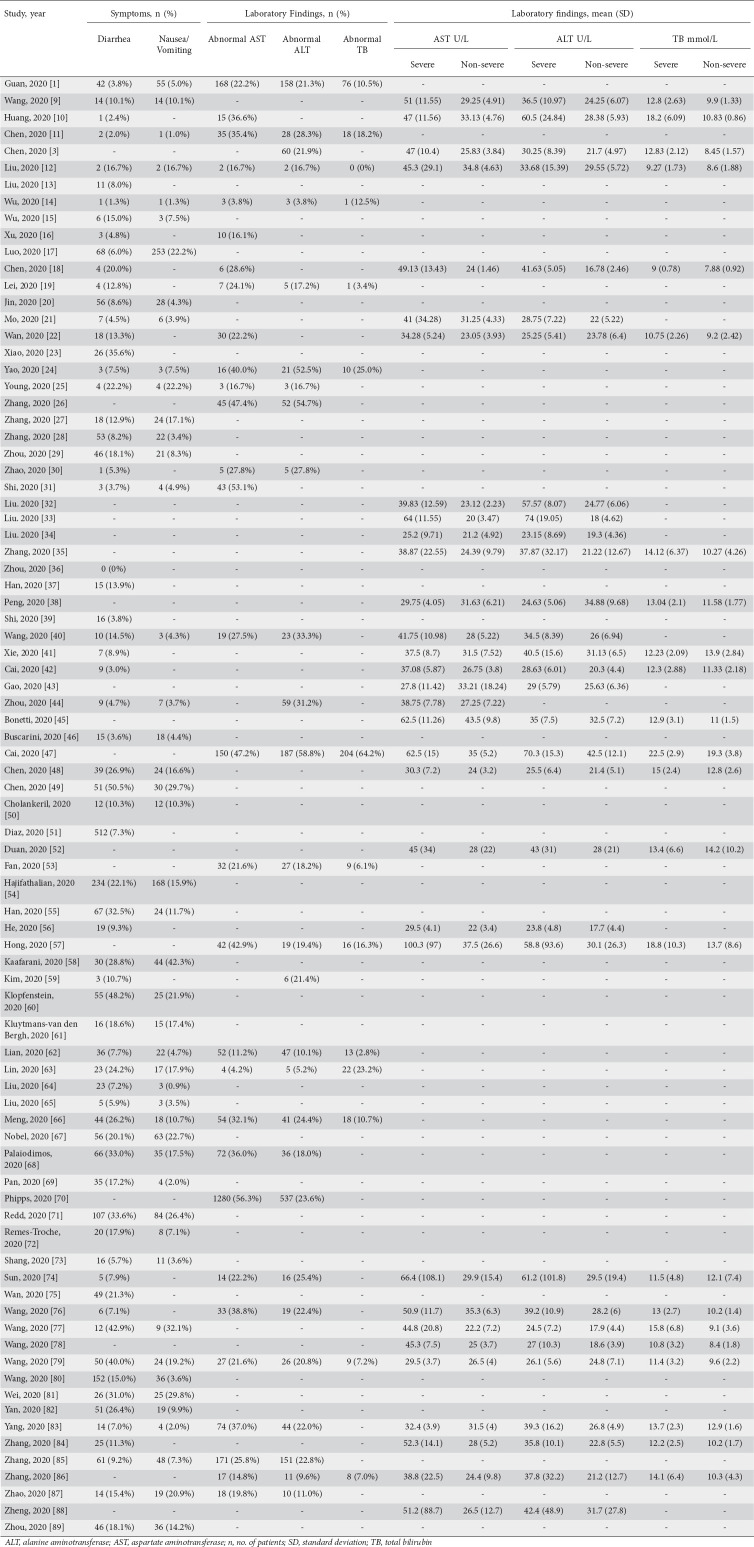
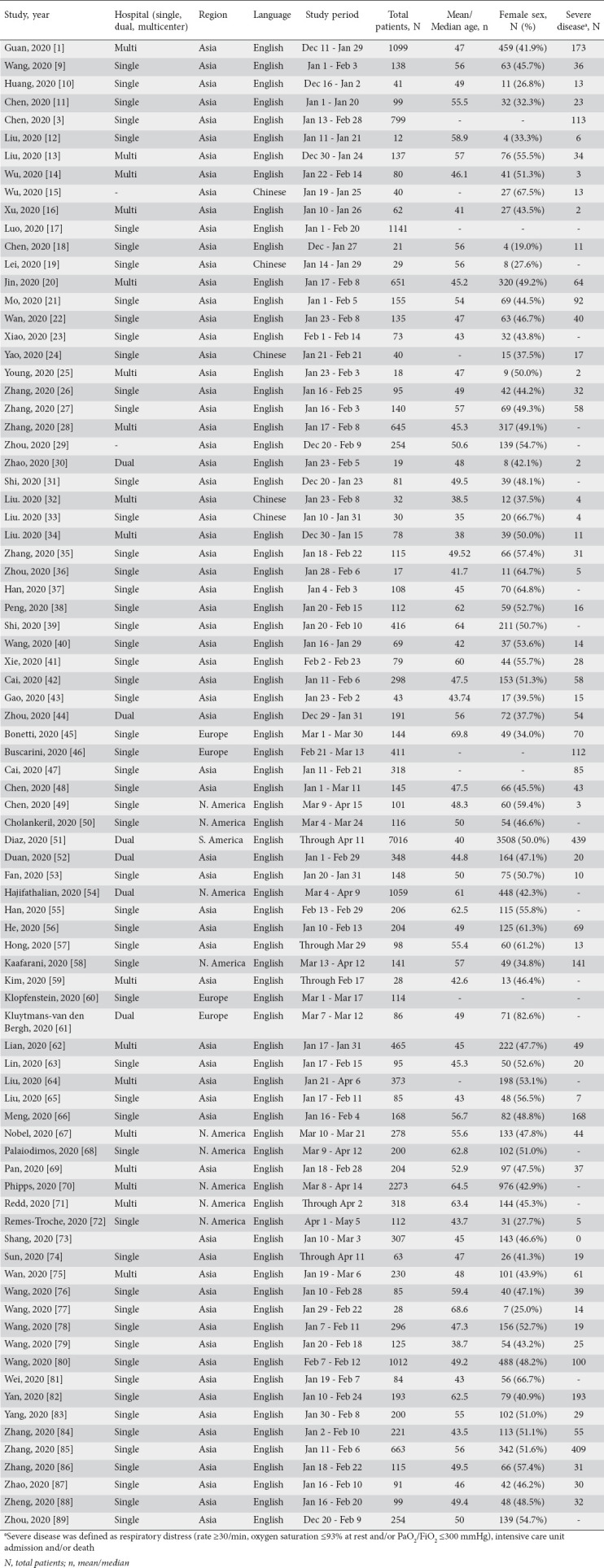
Characteristics of the included studies
Study details and demographics of included patients are highlighted in Table 1. Based on region, 70 studies originated from Asia, 8 from North America, 1 from South America, and 4 from Europe. The study duration was from December 11th through May 5th, 2020. Based on the number of centers reporting data, 17 studies were multicenter, 6 were dual-center, 57 were single-center, and 3 studies failed to mention the center from where the data originated. A total of 26,912 patients were included across these 83 studies. The patients’ mean age was 43.5±16.4 years and the female proportion was 48.2%.
Table 1.
Study characteristics and baseline demographic data for included patients
Prevalence of gastrointestinal parameters on admission
Symptoms
The overall prevalence of diarrhea on admission among the study population was 13.0% (95%CI 10.8-15.5%; I2=95.1%). Based on region, the following prevalences were noted: Europe 16.8% (95%CI 2.9-57.8%; I2=98.0%), North America 26.2% (95%CI 20.1-33.3%; I2=90.6%), and Asia 11.5% (95%CI 9.5-13.9%; I2=91.8%). The overall prevalence of nausea/vomiting on admission among the study population was 9.5% (95%CI 7.9-11.4%; I2=92.6%). Based on region, the following prevalences were noted: Europe 8.9% (95%CI 2.1-30.4%; I2=94.1%), North America 18.7% (95%CI 14.6-23.6%; I2=83.9%), and Asia 7.7% (95%CI 5.9-9.9%; I2=91.6%).
Laboratory abnormalities
The prevalence of abnormal AST findings on admission was 27.1% (95%CI 21.7-33.2%; I2=95.9%). Based on region, the following prevalences were noted: North America 46.3% (95%CI 27.7-66.0%; I2=96.6%), and Asia 26.3% (95%CI 22.1-31.0%; I2=89.3%). The prevalence of abnormal ALT findings on admission was 22.3% (95%CI 18.4-26.7%; I2=92.3%). Based on region, the following prevalences were noted: North America 21.4% (95%CI 16.5-27.4%; I2=69.1%), and Asia 22.1% (95%CI 17.4-27.6%; I2=92.7%). The prevalence of abnormal TB levels on admission was 10.6% (95%CI 5.0-21.0%; I2= 97.1%). All studies that reported abnormal TB were from Asia.
Gastrointestinal predictors of severe COVID-19
Symptoms
The odds of patients with diarrhea having severe disease were significantly greater compared to those without diarrhea (26 studies, OR 1.50, 95%CI 1.10-2.03; P=0.01; I2=54.1%) (Fig. 2A). Leave-one-out meta-analysis demonstrated consistent results, with a point estimate (OR) ranging between 1.46-1.74. A subgroup analysis of 17 studies that defined disease severity in terms of respiratory distress also showed consistent results (OR 1.62, 95%CI 1.11-2.37; P=0.01; I2=54.1%). Subgroup analysis based on ICU admission (5 studies) did not demonstrate increased odds of severe disease (OR 1.39, 95%CI 0.70-2.73; P=0.35; I2=27.1%). Meta-regression did not demonstrate any significant moderating impact of female proportion (P=0.39) or the number of centers involved in the study (P=0.89).
Figure 2.
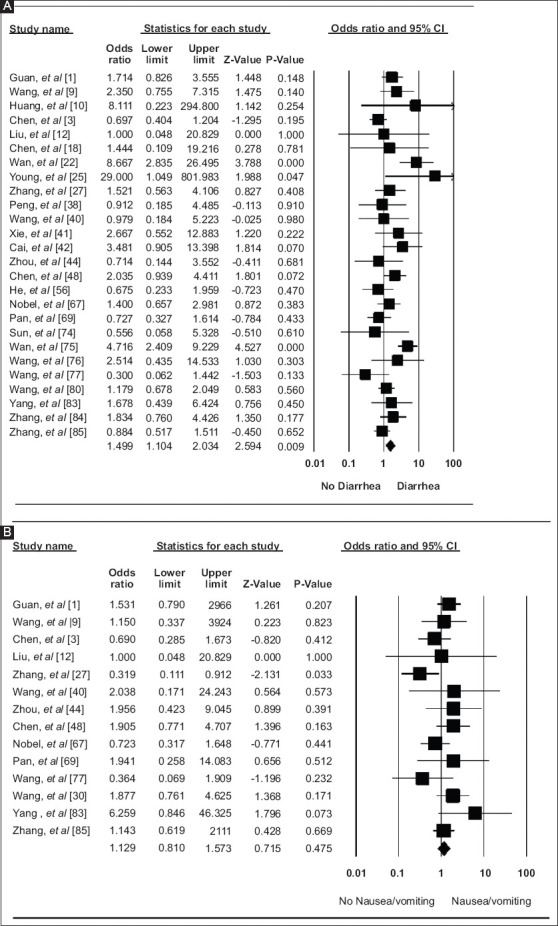
Forest plot demonstrating (A) severe disease in diarrhea vs. no diarrhea, and (B) severe disease in nausea/vomiting vs. no nausea/vomiting
Fourteen studies evaluated nausea/vomiting and disease severity and no significant association was found (OR 1.13, 95%CI 0.81-1.57; P=0.48; I2=22.6%) (Fig. 2B). Consistent results were obtained on leave-one-out meta-analysis (OR 1.07-1.24). The subgroup analysis also did not demonstrate a significant association when severity was classified on the basis of respiratory distress (8 studies, OR 1.27, 95%CI 0.84-1.90; P=0.26; I2=21.2%) or ICU admission (4 studies, OR 0.98, 95%CI 0.41-2.35; P=0.97; I2=42.1%). Meta-regression did not reveal any moderating impact of variables on outcomes, i.e., female proportion (P=0.20), region of study (P=0.19), or number of centers (P=0.33).
Laboratory abnormalities
Elevated serum AST levels in patients were evaluated in 16 studies and greater odds of disease severity were noted compared to patients without elevated AST (OR 4.00, 95%CI 3.02-5.28; P<0.001; I2=40.4%) (Fig. 3A). The results were consistent on leave-one-out meta-analysis (OR 3.64-4.14) as well as subgroup analysis for disease severity defined based on respiratory distress (11 studies, OR 3.80, 95%CI 2.77-5.22; P<0.001; I2=38.7%), and ICU admission (3 studies, OR 5.69, 95%CI 2.01-16.09; P=0.001; I2=45.8%). On meta-regression, the proportion of females in the study inversely correlated with the odds of having greater disease severity (P=0.04).
Figure 3.
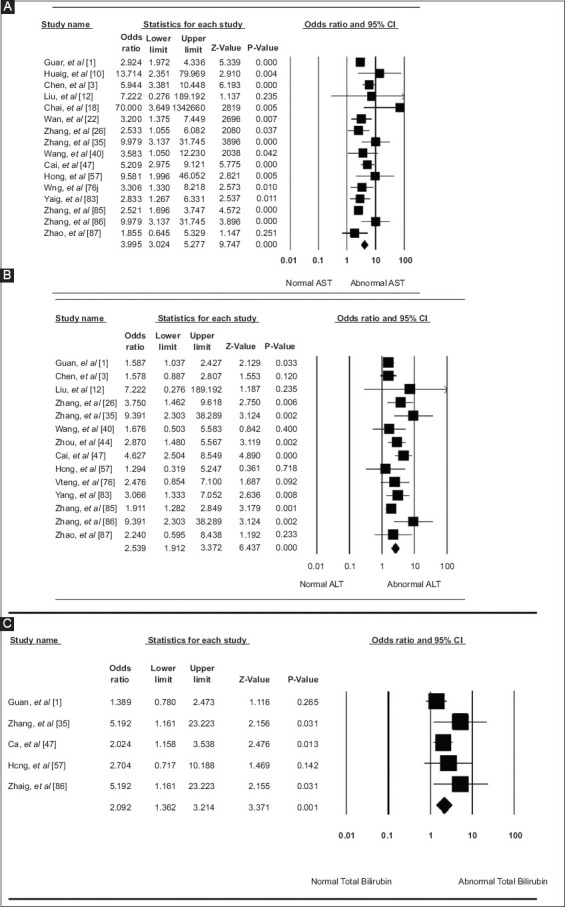
Forest plot demonstrating (A) severe disease in elevated AST vs, normal AST, (B) severe disease in elevated ALT vs. normal ALT, and (C) severe disease in elevated TB vs. normal TB
AST, aspartate aminotransferase; ALT, alanine aminotransferase; TB, total bilirubin
Elevated serum ALT levels on admission were evaluated in 14 studies and greater odds of disease severity were noted compared to patients with normal ALT (OR 2.54, 95%CI 1.91-3.37; P<0.001; I2=39.3%) (Fig. 3B). Similar results were obtained using leave-one-out meta-analysis (OR 2.28-2.73) and subgroup analysis for disease severity based on respiratory distress (9 studies, OR 2.93, 95%CI 1.92-4.48; P<0.001; I2=55.9%). No significant moderating impact of female proportion (P=0.35) or number of centers (P=0.24) was noted.
Only 5 studies evaluated elevated serum TB levels in association with disease severity, and elevated TB was associated with severe disease (OR 2.09, 95%CI 1.36-3.21; P=0.001; I2=17.5%) (Fig. 3C). Leave-one-out meta-analysis demonstrated a consistent association (OR 1.89-2.51). A subgroup analysis and meta-regression were not possible because of the low number of studies.
Mean laboratory findings and severe COVID-19
The mean serum AST level was significantly higher in the severe group compared to the non-severe group (32 studies, MD 14.78 U/L, 95%CI 11.70-17.86 U/L; P<0.001; I2=97.5%) (Fig. 4A). The leave-one-out meta-analysis was consistent with a point estimate (MD) ranging from 13.70-15.32 U/L. Subgroup analysis was performed on the basis of severity and significantly higher mean AST levels were noted for the severe group, defined in terms of ICU admission (5 studies, MD 20.49 U/L, 95%CI 7.60-33.39 U/L; P=0.002; I2=98.03%), death (4 studies, MD 18.01 U/L; 95%CI 13.62-22.41 U/L; P<0.001; I2=93.7%), and respiratory distress (20 studies, MD 13.60 U/L, 95%CI 9.95-17.24 U/L; P<0.001; I2=96.9%). Meta-regression did not reveal any moderating impact of region of study (P=0.89) or number of centers (P=0.94).
Figure 4.
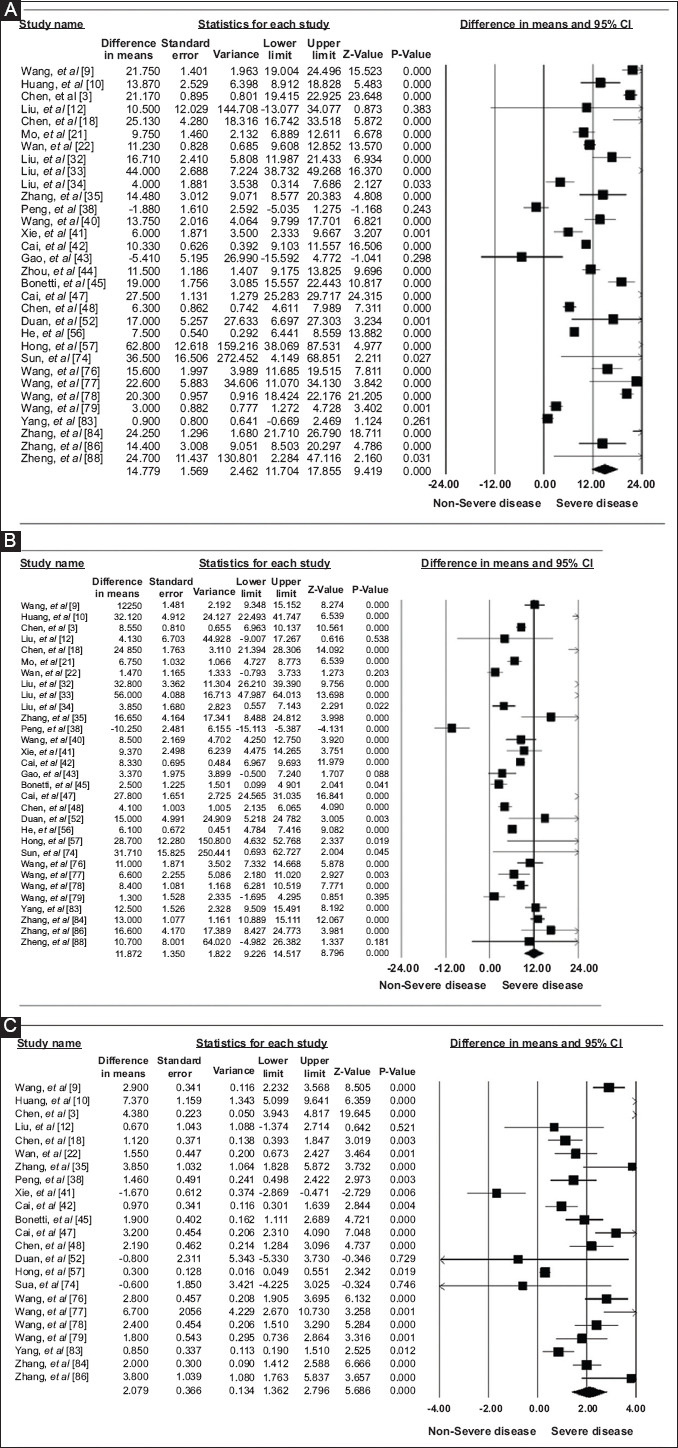
Forest plot demonstrating (A) mean serum AST in severe vs. non-severe disease, (B) mean serum ALT in severe vs. non-severe disease, and (C) mean serum TB in severe vs. non-severe disease
AST, aspartate aminotransferase; ALT, alanine aminotransferase; TB, total bilirubin
The mean serum ALT level was also significantly higher for the severe group compared to the non-severe group (31 studies, MD 11.87 U/L, 95%CI 9.23-14.51 U/L; P<0.001; I2=95.5%) (Fig. 4B). The results were consistent on leave-one-out meta-analysis (MD 11.14-12.61 U/L) and subgroup analysis for severity based on respiratory distress (20 studies, MD 13.01 U/L, 95%CI 8.84-17.17 U/L; P<0.001; I2=96.7%), ICU admission (5 studies, MD 14.78 U/L, 95%CI 9.20-20.37 U/L; P<0.001; I2 = 83.7%), and death (3 studies, MD 6.56 U/L, 95%CI 3.00-10.13 U/L; P<0.001; I2=89.3%). On meta-regression, female proportions were inversely correlated with disease severity on the basis of mean ALT level (P=0.04).
The mean serum TB level was evaluated in 26 studies and a significantly higher level was found in severe COVID-19 patients compared to the non-severe group (MD 2.08 mmol/L, 95%CI 1.36-2.80 mmol/L; P<0.001; I2=94.2%) (Fig. 4C). Consistent results were obtained using leave-one-out meta-analysis (MD 1.89-2.15 mmol/L) and subgroup analysis based on the severity criteria of ICU admission (5 studies, MD 2.91 mmol/L, 95%CI 1.24-4.58 mmol/L; P=0.001; I2=95.7%), death (3 studies, MD 2.92 mmol/L, 95%CI 1.20-4.64 mmol/L; P<0.001; I2=94.6%), and respiratory distress (14 studies, MD 1.62 mmol/L, 95%CI 0.92-2.33 mmol/L; P<0.001; I2=80.7%). On meta-regression, female proportions were inversely correlated with disease severity on the basis of mean TB level (P=0.03).
Risk of bias
Based on QUIPS tools, most of the studies (n=63) were at risk of bias for failing to account for confounders, while the remaining (n=20) accounted for some confounders. Twenty studies lacked details of the statistical design (Supplementary Table 2 (421.2KB, pdf) ). Visible asymmetry was observed on a funnel plot based on the symptom of diarrhea; however, Egger’s regression did not reveal a significant publication bias (P=0.76) (Supplementary Fig. 1).
Discussion
Our meta-analysis demonstrated significant correlations between gastrointestinal parameters (diarrhea, elevated serum ALT, AST and TB) and severe disease outcomes, i.e., respiratory distress, ICU admission, and/or death. Although the most frequent manifestation of COVID-19 is pneumonia, gastrointestinal signs/symptoms are seen in a significant number of patients and can be the presenting manifestations of the disease [90]. A systematic review by Cheung et al reported diarrhea and nausea/vomiting in 13% and 10% of COVID-19 patients, respectively [91]. We demonstrated a similar prevalence of diarrhea (13%) and nausea/vomiting (9.5%). We believe that the reported prevalence of diarrhea and nausea/vomiting is somewhat lower than in reality, as some of these patients only present with these symptoms and may not undergo COVID-19 testing because they do not fulfill local hospital or laboratory criteria.
The mechanism behind gastrointestinal symptoms is thought to be secondary to viral attachment and entry via angiotensin-converting enzyme 2 (ACE2), readily expressed in ileal and colonic epithelium [92]. This can explain symptoms such as diarrhea and nausea/vomiting. Furthermore, researchers have also identified viral RNA in the stool of patients infected with COVID-19, making diarrhea not only a marker for disease severity but a potential route of contagion [22]. Given the association of diarrhea with severe COVID-19 disease, based on our meta-analysis results, COVID-19 patients with diarrhea should be stratified into a high-risk group for developing severe disease as described above and managed accordingly.
Table 2.
Admission symptoms and laboratory findings on admission
Several mechanisms have been postulated to explain the hepatotoxicity seen in COVID-19 patients. One possible mechanism of hepatotoxicity of COVID-19 is immune system activation. It has been shown that many of the respiratory viruses, including COVID-19, lead to an activation of cytotoxic T cells and Kupffer cells in the liver that eventually damage hepatocytes [93]. Another mechanism is the triggering of a “cytokine storm,” leading to a massive surge in mediators such as interleukin-6, associated with sepsis, multiorgan dysfunction and death [8,94,95]. Direct viral entry through the intestines and invasion of the portal system and, subsequently, cholangiocytes, is another hypothesized mechanism [96]. Lastly, drug-induced hepatotoxicity should also be considered, as currently researchers are investigating all possible therapeutic options [97]. We demonstrated significantly increased elevation of ALT, AST and TB in patients with severe COVID-19 compared to non-severe patients, which can be attributed to some or all of the aforementioned mechanisms.
Several limitations exist with our analysis. The most notable was the lack of high quality randomized controlled trials and cohort studies. We relied on data from observational studies that reported admission data. Observational studies have their own inherent biases that limit data interpretation, including selection, recall, and confounding bias. It is difficult to establish a temporal relation between cause and event using observational studies, as there is no follow up. However, as we reported admission data, we propose screening and risk-stratifying individuals, based on their admission laboratory findings and symptoms, into severe and non-severe categories. We were not able to account for factors such as comorbidities, timing of hospitalization and routine home medications. We were also not able to account for these related gastrointestinal symptoms due to lack of stratified data. Lastly, given that the major manifestations of COVID-19 are respiratory symptoms (cough, shortness of breath, sputum production) and fever, gastrointestinal symptoms may have been underreported.
Despite the limitations, our analysis combines data from a large number of studies with a robust number of patients. We used admission data to avoid potential heterogeneity introduced by other factors, such as in-hospital medications, nosocomial infections, intubation, etc. The results of our study were consistent on both subgroup and sensitivity analysis. Furthermore, we provided subgroup prevalence based on region, i.e., Asia, Europe and North America where applicable.
In conclusion, patients presenting with diarrhea or elevated ALT, AST and/or TB and diagnosed with COVID-19 should be stratified into a high-risk group for developing severe disease outcomes (i.e., respiratory distress, ICU admission, and/or death) and managed appropriately.
Summary Box.
What is already known:
Gastrointestinal manifestations (diarrhea, nausea/vomiting, abnormal aspartate aminotransferase [AST], abnormal alanine aminotransferase[ALT], and abnormal total bilirubin [TB]) have been demonstrated in several studies in patients with COVID-19
A recent meta-analysis accounted for these manifestations in the form of pooled analysis
What the new findings are:
We performed a comprehensive systematic review and meta-analysis of the available literature through May 31st, 2020 to assess these manifestations with respect to disease severity
Our results indicate that diarrhea, abnormal ALT, AST and TB were associated with severe disease (intensive care unit admission, respiratory distress, and/or mortality)
Based on the current study results, patients with these manifestations should be stratified as high-risk and managed appropriately
Biography
University of Toledo Medical Center, Toledo, Ohio; The Wright Center for Graduate Medical Education, Scranton, Pennsylvania, USA
Footnotes
Conflict of Interest: None
References
- 1.Guan WJ, Ni ZY, Hu Y, et al. China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ding S, Liang TJ. Is SARS-CoV-2 also an enteric pathogen with potential fecal-oral transmission? A COVID-19 virological and clinical review. Gastroenterology. 2020;159:53–61. doi: 10.1053/j.gastro.2020.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ket JCF, Otten RHJ, Van Dusseldorp I. [Accessed 3 July 2020];KNVI biomedische informatie search blocks/Zoekblokken. Available from: https://blocks.bmi-online.nl/catalog/397 . [Google Scholar]
- 5.DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. 2015;45:139–145. doi: 10.1016/j.cct.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 7.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158:280–286. doi: 10.7326/0003-4819-158-4-201302190-00009. [DOI] [PubMed] [Google Scholar]
- 9.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu Y, Yang Y, Zhang C, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020;63:364–374. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu K, Fang YY, Deng Y, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl) 2020;133:1025–1031. doi: 10.1097/CM9.0000000000000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu J, Liu J, Zhao X, et al. Clinical characteristics of imported cases of COVID-19 in Jiangsu province: a multicenter descriptive study. Clin Infect Dis. 2020;71:706–712. doi: 10.1093/cid/ciaa199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu WS, Li YG, Wei ZF, et al. Investigation and analysis on characteristics of a cluster of COVID-19 associated with exposure in a department store in Tianjin. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:489–493. doi: 10.3760/cma.j.cn112338-20200221-00139. [DOI] [PubMed] [Google Scholar]
- 16.Xu XW, Wu XX, Jiang XG, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606. doi: 10.1136/bmj.m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Luo S, Zhang X, Xu H. Don't overlook digestive symptoms in patients with 2019 novel Coronavirus disease (COVID-19) Clin Gastroenterol Hepatol. 2020;18:1636–1637. doi: 10.1016/j.cgh.2020.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen G, Wu D, Guo W, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130:2620–2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen L, Liu HG, Liu W, et al. [Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia] Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:E005. doi: 10.3760/cma.j.issn.1001-0939.2020.0005. [DOI] [PubMed] [Google Scholar]
- 20.Jin X, Lian JS, Hu JH, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69:1002–1009. doi: 10.1136/gutjnl-2020-320926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mo P, Xing Y, Xiao Y, et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis. 2020 Mar 16;:ciaa270. [Online ahead of print]. doi: 10.1093/cid/ciaa270. [Google Scholar]
- 22.Wan S, Xiang Y, Fang W, et al. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J Med Virol. 2020;92:797–806. doi: 10.1002/jmv.25783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158:1831–1833. doi: 10.1053/j.gastro.2020.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yao N, Wang SN, Lian JQ, et al. Clinical characteristics and influencing factors of patients with novel coronavirus pneumonia combined with liver injury in Shaanxi region. Zhonghua Gan Zang Bing Za Zhi. 2020;28:234–239. doi: 10.3760/cma.j.cn501113-20200226-00070. [DOI] [PubMed] [Google Scholar]
- 25.Young BE, Ong SWX, Kalimuddin S, et al. Singapore 2019 Novel Coronavirus Outbreak Research Team. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA. 2020;323:1488–1494. doi: 10.1001/jama.2020.3204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang G, Zhang J, Wang B, Zhu X, Wang Q, Qiu S. Analysis of clinical characteristics and laboratory findings of 95 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a retrospective analysis. Respir Res. 2020;21:74. doi: 10.1186/s12931-020-01338-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75:1730–1741. doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 28.Zhang X, Cai H, Hu J, et al. Epidemiological, clinical characteristics of cases of SARS-CoV-2 infection with abnormal imaging findings. Int J Infect Dis. 2020;94:81–87. doi: 10.1016/j.ijid.2020.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhou Z, Zhao N, Shu Y, Han S, Chen B, Shu X. Effect of gastrointestinal symptoms in patients with COVID-19. Gastroenterology. 2020;158:2294–2297. doi: 10.1053/j.gastro.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhao D, Yao F, Wang L, et al. A comparative study on the clinical features of COVID-19 pneumonia to other pneumonias. Clin Infect Dis. 2020;316:F889–F897. doi: 10.1093/cid/ciaa247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu C, Jiang ZC, Shao CX, et al. Preliminary study of the relationship between novel coronavirus pneumonia and liver function damage: a multicenter study. Zhonghua Gan Zang Bing Za Zhi. 2020;28:107–111. doi: 10.3760/cma.j.issn.1007-3418.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 33.Liu M, He P, Liu HG, et al. Clinical characteristics of 30 medical workers infected with new coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:E016. doi: 10.3760/cma.j.issn.1001-0939.2020.0016. [DOI] [PubMed] [Google Scholar]
- 34.Liu W, Tao ZW, Wang L, et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J (Engl) 2020;133:1032–1038. doi: 10.1097/CM9.0000000000000775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang Y, Zheng L, Liu L, Zhao M, Xiao J, Zhao Q. Liver impairment in COVID-19 patients: a retrospective analysis of 115 cases from a single centre in Wuhan city, China. Liver Int. 2020;40:2095–2103. doi: 10.1111/liv.14455. [DOI] [PubMed] [Google Scholar]
- 36.Zhou Y, Zhang Z, Tian J, Xiong S. Risk factors associated with disease progression in a cohort of patients infected with the 2019 novel coronavirus. Ann Palliat Med. 2020;9:428–436. doi: 10.21037/apm.2020.03.26. [DOI] [PubMed] [Google Scholar]
- 37.Han R, Huang L, Jiang H, Dong J, Peng H, Zhang D. Early clinical and CT manifestations of coronavirus disease 2019 (COVID-19) pneumonia. AJR Am J Roentgenol. 2020;215:338–343. doi: 10.2214/AJR.20.22961. [DOI] [PubMed] [Google Scholar]
- 38.Peng YD, Meng K, Guan HQ, et al. Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48:E004. doi: 10.3760/cma.j.cn112148-20200220-00105. [DOI] [PubMed] [Google Scholar]
- 39.Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang Z, Yang B, Li Q, Wen L, Zhang R. Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. 2020;71:769–777. doi: 10.1093/cid/ciaa272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xie H, Zhao J, Lian N, Lin S, Xie Q, Zhuo H. Clinical characteristics of non-ICU hospitalized patients with coronavirus disease 2019 and liver injury: a retrospective study. Liver Int. 2020;40:1321–1326. doi: 10.1111/liv.14449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cai Q, Huang D, Ou P, et al. COVID-19 in a designated infectious diseases hospital outside Hubei Province, China. Allergy. 2020;75:1742–1752. doi: 10.1111/all.14309. [DOI] [PubMed] [Google Scholar]
- 43.Gao Y, Li T, Han M, et al. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J Med Virol. 2020;92:791–796. doi: 10.1002/jmv.25770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bonetti G, Manelli F, Patroni A, et al. Laboratory predictors of death from coronavirus disease 2019 (COVID-19) in the area of Valcamonica, Italy. Clin Chem Lab Med. 2020;58:1100–1105. doi: 10.1515/cclm-2020-0459. [DOI] [PubMed] [Google Scholar]
- 46.Buscarini E, Manfredi G, Brambilla G, et al. GI symptoms as early signs of COVID-19 in hospitalised Italian patients. Gut. 2020;69:1547–1548. doi: 10.1136/gutjnl-2020-321434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cai Q, Huang D, Yu H, et al. COVID-19: Abnormal liver function tests. J Hepatol. 2020;73:566–574. doi: 10.1016/j.jhep.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen Q, Zheng Z, Zhang C, et al. Clinical characteristics of 145 patients with corona virus disease 2019 (COVID-19) in Taizhou, Zhejiang, China. Infection. 2020;48:543–551. doi: 10.1007/s15010-020-01432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen A, Agarwal A, Ravindran N, To C, Zhang T, Thuluvath PJ. Are gastrointestinal symptoms specific for COVID-19 infection? a prospective case-control study from the United States. Gastroenterology. 2020;159:1161–1163.e2. doi: 10.1053/j.gastro.2020.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cholankeril G, Podboy A, Aivaliotis VI, et al. High prevalence of concurrent gastrointestinal manifestations in patients with SARS-CoV-2: early experience from California. Gastroenterology. 2020;159:775–777. doi: 10.1053/j.gastro.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Díaz LA, García-Salum T, Fuentes-López E, et al. Contributors. Symptom profiles and risk factors for hospitalization in patients with SARS-CoV-2 and COVID-19: a large cohort from South America. Gastroenterology. 2020;159:1148–1150. doi: 10.1053/j.gastro.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Duan J, Wang X, Chi J, et al. Correlation between the variables collected at admission and progression to severe cases during hospitalization among patients with COVID-19 in Chongqing. J Med Virol. 2020;92:2616–2622. doi: 10.1002/jmv.26082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fan Z, Chen L, Li J, et al. Clinical Features of COVID-19-related liver functional abnormality. Clin Gastroenterol Hepatol. 2020;18:1561–1566. doi: 10.1016/j.cgh.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hajifathalian K, Krisko T, Mehta A, et al. WCM-GI research group. Gastrointestinal and hepatic manifestations of 2019 novel coronavirus disease in a large cohort of infected patients from New York: clinical implications. Gastroenterology. 2020;159:1137–1140.e2. doi: 10.1053/j.gastro.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Han C, Duan C, Zhang S, et al. Digestive symptoms in COVID-19 patients with mild disease severity: clinical presentation, stool viral RNA testing, and outcomes. Am J Gastroenterol. 2020;115:916–923. doi: 10.14309/ajg.0000000000000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.He R, Lu Z, Zhang L, et al. The clinical course and its correlated immune status in COVID-19 pneumonia. J Clin Virol. 2020;127:104361. doi: 10.1016/j.jcv.2020.104361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hong KS, Lee KH, Chung JH, et al. Clinical features and outcomes of 98 patients hospitalized with SARS-CoV-2 infection in Daegu, South Korea: a brief descriptive study. Yonsei Med J. 2020;61:431–437. doi: 10.3349/ymj.2020.61.5.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kaafarani HMA, Moheb ME, Hwabejire JO, et al. Gastrointestinal complications in critically ill patients with COVID-19. Ann Surg. 2020;272:e61–e62. doi: 10.1097/SLA.0000000000004004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kim ES, Chin BS, Kang CK, et al. Korea National Committee for Clinical Management of COVID-19. Clinical course and outcomes of patients with severe acute respiratory syndrome coronavirus 2 infection: a preliminary report of the first 28 patients from the Korean cohort study on COVID-19. J Korean Med Sci. 2020;35:e142. doi: 10.3346/jkms.2020.35.e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Klopfenstein T, Kadiane-Oussou NJ, Royer PY, Toko L, Gendrin V, Zayet S. Diarrhea: An underestimated symptom in Coronavirus disease 2019. Clin Res Hepatol Gastroenterol. 2020;44:282–283. doi: 10.1016/j.clinre.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kluytmans-van den Bergh MFQ, Buiting AGM, Pas SD, et al. Prevalence and clinical presentation of health CareWorkers with symptoms of Coronavirus disease 2019 in 2 Dutch hospitals during an early phase of the pandemic. JAMA Netw Open. 2020;3:e209673. doi: 10.1001/jamanetworkopen.2020.9673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lian J, Jin X, Hao S, et al. Epidemiological, clinical, and virological characteristics of 465 hospitalized cases of coronavirus disease 2019 (COVID-19) from Zhejiang province in China. Influenza Other Respir Viruses. 2020;14:564–574. doi: 10.1111/irv.12758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lin L, Jiang X, Zhang Z, et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020;69:997–1001. doi: 10.1136/gutjnl-2020-321013. [DOI] [PubMed] [Google Scholar]
- 64.Liu J, Chen T, Hwang S. Analysis of imported cases of COVID-19 in Taiwan: a nationwide study. Int J Environ Res Public Health. 2020;17:3311. doi: 10.3390/ijerph17093311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu Z, Ding L, Chen G, et al. Clinical time features and chest imaging of 85 patients with COVID-19 in Zhuhai, China. Front Med (Lausanne) 2020;7:209. doi: 10.3389/fmed.2020.00209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Meng Y, Wu P, Lu W, et al. Sex-specific clinical characteristics and prognosis of coronavirus disease-19 infection in Wuhan, China: a retrospective study of 168 severe patients. PLoS Pathog. 2020;16:e1008520. doi: 10.1371/journal.ppat.1008520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nobel YR, Phipps M, Zucker J, et al. Gastrointestinal symptoms and coronavirus disease 2019: a case-control study from the United States. Gastroenterology. 2020;159:373–375.e2. doi: 10.1053/j.gastro.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Palaiodimos L, Kokkinidis DG, Li W, et al. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism. 2020;108:154262. doi: 10.1016/j.metabol.2020.154262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pan L, Mu M, Yang P, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115:766–773. doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Phipps MM, Barraza LH, LaSota ED, et al. Acute liver injury in COVID-19: prevalence and association with clinical outcomes in a large US cohort. Hepatology. 2020;72:807–817. doi: 10.1002/hep.31404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Redd WD, Zhou JC, Hathorn KE, et al. Prevalence and characteristics of gastrointestinal symptoms in patients with SARS-CoV-2 infection in the United States: a multicenter cohort study. Gastroenterology. 2020;159:765–767.e2. doi: 10.1053/j.gastro.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Remes-Troche JM, Ramos-de-la-Medina A, Manríquez-Reyes M, Martínez-Pérez-Maldonado L, Lara EL, Solís-González MA. Initial gastrointestinal manifestations in patients with SARS-CoV-2 in 112 patients from Veracruz (southeastern Mexico) Gastroenterology. 2020;159:1179–1181. doi: 10.1053/j.gastro.2020.05.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Shang Y, Xu C, Jiang F, et al. Clinical characteristics and changes of chest CT features in 307 patients with common COVID-19 pneumonia infected SARS-CoV-2: a multicenter study in Jiangsu, China. Int J Infect Dis. 2020;96:157–162. doi: 10.1016/j.ijid.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sun Y, Dong Y, Wang L, et al. Characteristics and prognostic factors of disease severity in patients with COVID-19: the Beijing experience. J Autoimmun. 2020;112:102473. doi: 10.1016/j.jaut.2020.102473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wan Y, Li J, Shen L, et al. Enteric involvement in hospitalised patients with COVID-19 outside Wuhan. Lancet Gastroenterol Hepatol. 2020;5:534–535. doi: 10.1016/S2468-1253(20)30118-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang CZ, Hu SL, Wang L, Li M, Li HT. Early risk factors of the exacerbation of Coronavirus disease 2019 pneumonia. J Med Virol. 2020;92:2593–2599. doi: 10.1002/jmv.26071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wang F, Yang Y, Dong K, et al. Clinical characteristics of 28 patients with diabetes and COVID-19 in Wuhan, China. Endocr Pract. 2020;26:668–674. doi: 10.4158/EP-2020-0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wang K, Zuo P, Liu Y, et al. Clinical and laboratory predictors of in-hospital mortality in patients with COVID-19: a cohort study in Wuhan, China. Clin Infect Dis. 2020 May 3;:ciaa538. doi: 10.1093/cid/ciaa538. [Online ahead of print]. doi: 10.1093/cid/ciaa538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wang R, Pan M, Zhang X, et al. Epidemiological and clinical features of 125 hospitalized patients with COVID-19 in Fuyang, Anhui, China. Int J Infect Dis. 2020;95:421–428. doi: 10.1016/j.ijid.2020.03.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wang X, Fang J, Zhu Y, et al. Clinical characteristics of non-critically ill patients with novel coronavirus infection (COVID-19) in a Fangcang Hospital. Clin Microbiol Infect. 2020;26:1063–1068. doi: 10.1016/j.cmi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wei XS, Wang X, Niu YR, et al. Diarrhea is associated with prolonged symptoms and viral carriage in corona virus disease 2019. Clin Gastroenterol Hepatol. 2020;18:1753–1759. doi: 10.1016/j.cgh.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yan Y, Yang Y, Wang F, et al. Clinical characteristics and outcomes of patients with severe covid-19 with diabetes. BMJ Open Diabetes Res Care. 2020;8 doi: 10.1136/bmjdrc-2020-001343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yang L, Liu J, Zhang R, et al. Epidemiological and clinical features of 200 hospitalized patients with corona virus disease 2019 outside Wuhan, China: a descriptive study. J Clin Virol. 2020;129:104475. doi: 10.1016/j.jcv.2020.104475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang G, Hu C, Luo L, et al. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. J Clin Virol. 2020;127:104364. doi: 10.1016/j.jcv.2020.104364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhang J, Wang X, Jia X, et al. Risk factors for disease severity, unimprovement, and mortality in COVID-19 patients in Wuhan, China. Clin Microbiol Infect. 2020;26:767–772. doi: 10.1016/j.cmi.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhang Y, Zheng L, Liu L, Zhao M, Xiao J, Zhao Q. Liver impairment in COVID-19 patients: A retrospective analysis of 115 cases from a single centre in Wuhan city, China. Liver Int. 2020;40:2095–2103. doi: 10.1111/liv.14455. [DOI] [PubMed] [Google Scholar]
- 87.Zhao XY, Xu XX, Yin HS, et al. Clinical characteristics of patients with 2019 coronavirus disease in a non-Wuhan area of Hubei Province, China: a retrospective study. BMC Infect Dis. 2020;20:311. doi: 10.1186/s12879-020-05010-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zheng Y, Xu H, Yang M, et al. Epidemiological characteristics and clinical features of 32 critical and 67 noncritical cases of COVID-19 in Chengdu. J Clin Virol. 2020;127:104366. doi: 10.1016/j.jcv.2020.104366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhou Z, Zhao N, Shu Y, Han S, Chen B, Shu X. Effect of gastrointestinal symptoms in patients with COVID-19. Gastroenterology. 2020;158:2294–2297. doi: 10.1053/j.gastro.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Aziz M, Perisetti A, Lee-Smith WM, Gajendran M, Bansal P, Goyal H. Taste changes (dysgeusia) in COVID-19: a systematic review and metaanalysis. Gastroenterology. 2020;159:1132–1133. doi: 10.1053/j.gastro.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cheung KS, Hung IFN, Chan PPY, et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from a Hong Kong cohort: systematic review and meta-analysis. Gastroenterology. 2020;159:81–95. doi: 10.1053/j.gastro.2020.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhang H, Kang Z, Gong H, et al. The digestive system is a potential route of 2019-nCov infection: a bioinformatics analysis based on single-cell transcriptomes. bioRxiv. 2020 Jan 31; doi: 10.1101/2020.01.30.927806. [Google Scholar]
- 93.Adams DH, Hubscher SG. Systemic viral infections and collateral damage in the liver. Am J Pathol. 2006;168:1057–1059. doi: 10.2353/ajpath.2006.051296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Aziz M, Fatima R, Assaly R. Elevated interleukin-6 and severe COVID-19: a meta-analysis. J Med Virol. 2020;92:2283–2285. doi: 10.1002/jmv.25948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Aziz M, Fatima R, Lee-Smith W, Assaly R. The association of low serum albumin level with severe COVID-19: a systematic review and meta-analysis. Crit Care. 2020;24:255. doi: 10.1186/s13054-020-02995-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yeo C, Kaushal S, Yeo DJTLG. Enteric involvement of coronaviruses: is faecal–oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. 2020;5:335–337. doi: 10.1016/S2468-1253(20)30048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Leise MD, Poterucha JJ, Talwalkar JA. Drug-induced liver injury. Mayo Clin Proc. 2014;89:95–106. doi: 10.1016/j.mayocp.2013.09.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.