Abstract
Simple Summary
DUX4-rearrangement (DUX4r) is a recently discovered recurrent genomic lesion reported in 4–7% of childhood B cell acute lymphoblastic leukaemia (B-ALL) cases. This subtype has favourable outcomes, especially in children and adolescents treated with intensive chemotherapy. The fusion most commonly links the hypervariable IGH gene to DUX4 a gene located within the D4Z4 macrosatellite repeat on chromosome 4. DUX4r is cryptic to most standard diagnostic techniques, and difficult to identify even with next generation sequencing assays. This review summarises the clinical features and molecular genetics of DUX4r B-ALL and proposes prospective new diagnostic methods.
Abstract
DUX4-rearrangement (DUX4r) is a recently discovered recurrent genomic lesion reported in 4–7% of childhood B cell acute lymphoblastic leukaemia (B-ALL) cases. This subtype has favourable outcomes, especially in children and adolescents treated with intensive chemotherapy. The fusion most commonly links the hypervariable IGH gene to DUX4 a gene located within the D4Z4 macrosatellite repeat on chromosome 4, with a homologous polymorphic repeat on chromosome 10. DUX4r is cryptic to most standard diagnostic techniques, and difficult to identify even with next generation sequencing assays. This review summarises the clinical features and molecular genetics of DUX4r B-ALL and proposes prospective new diagnostic methods.
Keywords: acute lymphoblastic leukaemia, DUX4, ERG, molecular subtype
1. Introduction
B-cell acute lymphoblastic leukaemia (B-ALL) is a malignant disorder of the bone marrow resulting in over proliferation of immature B lymphoblasts. The disease can manifest at any age but the majority of patients are children, making B-ALL the most common childhood malignancy [1]. This heterogeneous disease is characterised by a variety of different genomic alterations including changes in chromosome number, chromosomal translocations and single nucleotide variants (SNV). Detection of the underlying genomic alterations assists clinical risk stratification and therapeutic triage. Cytogenetic analysis has proven adept at identifying several recurrent genomic alterations which result in diseases with distinct gene expression profiles (GEP) and defined prognosis. This includes high hyperdiploidy, hypodiploidy, and the translocations t(12;21) [ETV6-RUNX1], t(9;22) BCR-ABL1, t(1;19) TCF3-PBX1 and alterations of chromosome 11q23 resulting in rearrangement of KMT2A/MLL. These alterations account for approximately 60% of pediatric B-ALL cases [2,3]. Remaining patients were historically classified as B-other and demonstrated highly variable prognosis and treatment response.
Molecular studies involving GEP and next-generation sequencing (NGS) have subsequently identified a number of additional recurrent molecular alterations not detectable with standard cytogenetics, several of which may be targetable by precision medicine approaches. This includes the newly recognized subtype of Philadelphia chromosome-like (Ph-like) ALL characterized by a gene expression profile similar to cases with a BCR-ABL1 translocation, but instead carrying one of multiple kinase activating lesions. One example is rearrangement of the cytokine receptor gene CRLF2 (CRLF2r), commonly with concurrence of Janus Kinase 2 (JAK2) mutations [4,5], affecting 5–7% of children with B-ALL [3]. NGS has also recently identified a rearrangement of the homeodomain encoding the Double Homeobox 4 (DUX4) transcription factor with the immunoglobulin heavy chain (IGH) locus which results in a distinct genetic subtype.
As early as 2002 researchers identified a novel B-ALL subtype, with a distinct microarray GEP, not associated with any known recurrent genomic alterations, that appeared to confer a good prognosis. Interrogation of overexpressed genes in these patients failed to uncover a causative lesion [6]. Follow-up studies involving copy number alteration (CNA) analysis revealed many of the patients with the distinct expression profile also demonstrated deletion of the ERG gene (ETS transcription factor ERG), a genomic alteration absent in almost all other subtypes. ERG deletion was consequently proposed as the driving lesion in this subtype [7,8]. Multiple studies have subsequently demonstrated that monoallelic deletion of ERG is observed in only a subset of patients demonstrating this GEP. Furthermore, ERG deletions were subclonal in several patients at diagnosis and either altered or absent at relapse [9,10,11].
In 2016, two independent studies identified rearrangement of the DUX4 locus (DUX4r), most commonly partnered with IGH, present in patients with the previously detected GEP [12,13]. Transduction of the DUX4 fusion transcript into NIH3T3 fibroblasts resulted in cellular transformations, demonstrating the oncogenic potential of this alteration [12]. Multiple studies have subsequently confirmed the unique GEP of DUX4r cases and identified the rearrangement in 4–7% of B-ALL patients [9,14,15,16,17,18,19], as well as within the NALM6 cell line [12]. Leukaemic cells carrying the DUX4r also display a unique methylation profile, associated with widespread hypomethylation [15,20,21], and express a specific non coding RNA signature [16,21]. Consequently, DUX4r, also reported in the literature as DUX4/ERG, has increasingly been accepted as a distinct molecular subtype in B-ALL. In this review, we present the current understanding of the molecular structure and biological effects of the DUX4r. We further explore the continued difficulties associated with detection of this alteration in new patient samples and discuss the impact this may have on the accurate assessment of prognosis and subsequent therapy options.
2. Description of the DUX4 Rearrangement
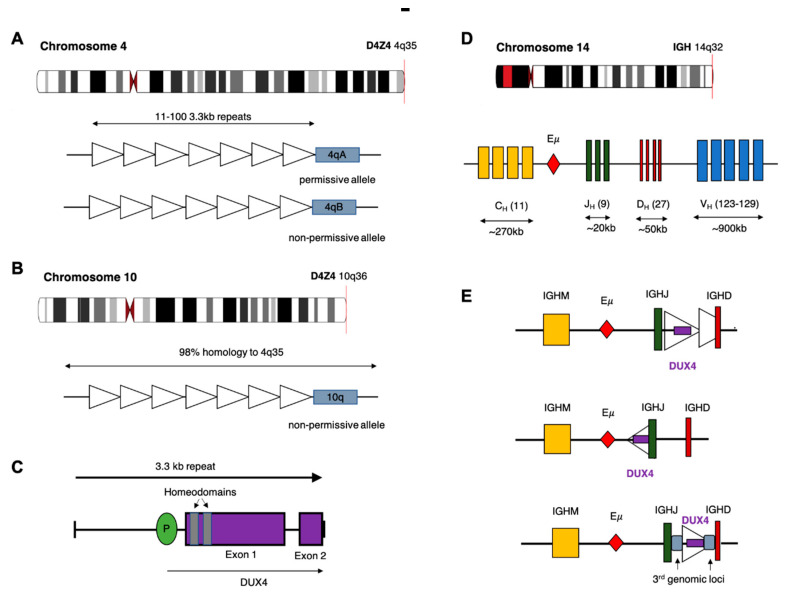
The DUX4 gene is present within each repeat of the D4Z4 tandem array located in the subtelomeric region of chromosome 4q [22], with an almost identical locus (>98% nucleotide identity) on 10q [23,24]. The D4Z4 array is polymorphic in length containing between 11–100 copies of the 3.3 kb repeat in healthy adults (Figure 1) [25]. In healthy tissue, transcription of DUX4 is restricted to germline cells of the testes. Transcription has also been observed in induced pluripotent stem cells, suggesting a role for DUX4 in germline development [26,27]. Expression of the full-length DUX4 transcript is epigenetically silenced in somatic tissue [27]. Only the first exon of the spliced transcript contains a coding sequence for the protein which consists of two N-terminal homeodomains capable of DNA binding [28] and a C-terminal transactivation domain [29]. The DUX4 protein is capable of binding to, and upregulating expression of, multiple genes as well as initiating expression from alternate promoters, producing non-canonical transcript isoforms [29].
Figure 1.
Potential chromosomal rearrangements involving IGH and DUX4. (A) Ideogram of chromosome 4 indicating location of the D4Z4 array and a depiction of the two alleles which vary in the sequence distal to the final repeat (repeat indicated by open triangles). This includes the permissive 4qA allele which can result in FSHD when contracted to fewer than 10 repeats. (B) Ideogram of chromosome 10 indicating location of the homologous D4Z4 array with 98% identical sequence. This chromosome is associated with a non-permissive allele which does not result in FSHD. (C) Schematic diagram of the repeat 3.3 kb repeat sequence indicating location and exons of the DUX4 gene. (D) Ideogram of chromosome 14 and depiction of the IGH locus indicating constant (CH), joining (JH), diversity (DH) and variable (VH) alleles (E) Schematic diagram depicting possible rearrangements as a result of cryptic insertion of DUX4 from either chromosome 4 or 10 into the IGH locus. DUX4 can be inserted in either orientation, include only a partial or one complete and one partial copy of the repeat array and also be inserted with sequence from a third genomic location.
Contraction of the D4Z4 region resulting in fewer than 10 repeats is associated with facioscapulohumeral muscular dystrophy (FSHD) [25,30], a genetically inherited disorder that initially manifests as progressive weakening of the facial, shoulder and upper arm muscles [31]. Partial deletion of the D4Z4 array is associated with hypomethylation and loss of repressive histone modifications that are believed to reduce chromatin packing of the subtelomeric region allowing DUX4 expression [32,33]. Intriguingly, FSHD only manifests in patients who demonstrate D4Z4 contraction on chromosome 4q and not the homologous array on chromosome 10q. Furthermore, contraction of an alternative chromosome 4q allele (4qB) [24], does not result in disease. Sequencing efforts have subsequently revealed that the permissive 4qA allele carries a polymorphism in the region immediately distal to the final repeat of the array (Figure 1). This polymorphism creates a canonical polyadenylation signal in the 3’UTR of DUX4 enabling expression of a stable mRNA transcript [34]. The translated protein then binds multiple target genes resulting in widespread changes in gene expression that are ultimately cytotoxic [26].
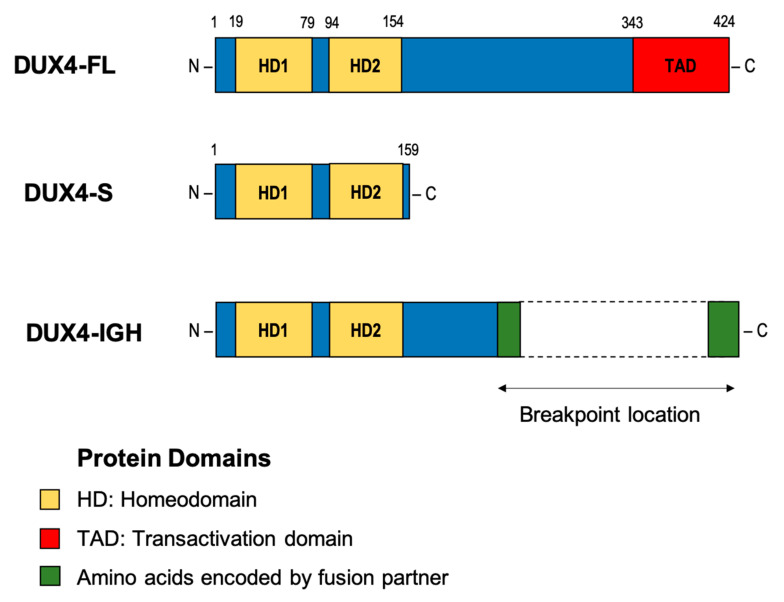
DUX4 has also been implicated in several cancers involving rearrangements that produce chimeric proteins with altered transcriptional activity [35,36]. For example, a recurrent translocation between Capicua Transcriptional Repressor (CIC) and DUX4 occurs in a proportion of patients with Ewing-like sarcoma. This chromosomal rearrangement produces an in-frame transcript containing the first 20 exons of CIC but replacing the terminal exons with the 3’ portion of DUX4. Translation of the chimeric transcript produces a protein that retains the majority of CIC, including the N-terminal DNA binding domains, but replaces the C-terminus with the DUX4 transactivation domain. As a result, the chimeric CIC-DUX4 protein acts as an oncogenic transcriptional activator [37]. In B-ALL, translocation of DUX4 results in a different chimeric protein, but one that again acts as an oncogenic transcriptional activator. In all but one reported case, the 5’ coding sequence of DUX4 is cryptically inserted into an alternate genomic location, resulting in expression of a chimeric transcript which retains sequence containing the N-terminus of DUX4 but replacing the 3’ coding sequence (Figure 2). While multiple potential fusion partners have been identified, including ERG, DUX4 is most commonly inserted into the IGH locus [9,12,13,17].
Figure 2.
Deduced proteins of the various forms of DUX4. Full-length DUX4 (DUX4-FL) and truncated DUX4 (DUX4-S) generated from an alternatively spliced transcript of DUX4 (DUX4-s) lacking the C-terminal transactivation domain. Putative DUX4-IGH chimeric protein in which the C-terminal portion of DUX4 containing the transactivation domain is replaced with amino acid sequence encoded by the genomic location into which DUX4 was inserted. Length of the C-terminal portion of the chimeric protein can vary between patients, depending on the breakpoint location within exon 1 of DUX4.
Multiple rearrangements of IGH (IGHr) have been reported in B-ALL resulting in expression or overexpression of genes with oncogenic potential. The most common of these is a translocation between chromosome 14 and CRLF2 of the pseudoautosomal region of chromosome X/Y resulting in increased expression of cytokine receptor-like factor 2 [4,38]. In the case of DUX4, most analyses report that the rearrangement involves a portion of the D4Z4 array on 4q or the homologous region on 10q, consisting of either a partial copy of DUX4 or one complete and one partial D4Z4 repeat, being inserted into the IGH locus, placing them close to the IGH enhancer (E) [12]. As with other IGHr, the presence of the enhancer induces expression of the translocated gene [38]. Repeats containing DUX4 can be inserted in either orientation resulting in expression from the positive or negative strand. In some cases, a more complex rearrangement involving sequences from a third genomic location have been reported (Figure 1C) [12,15]. Alternatively, Hi-C data performed on the NALM6 cell line suggest that a reciprocal translocation can occur in which the telomeric ends of 4/10q are exchanged with 14q [39].
IGH breakpoints are enriched in the 3.5 kb region preceding the IGHM constant allele and overlapping the IGH D-J junctions but can occur throughout the locus [9]. Breakpoint locations for the DUX4 gene are harder to define given the repetitive nature of the D4Z4 array, but most commonly occur within the 5’ region upstream of DUX4 and within the 3’ coding region of exon1. This results in a DUX4 transcript which maintains the homeodomains encoded at the 5’ end of the transcript fused to sequence, usually from IGH-JH or IGH-DH regions, but can also be another genomic location [9,12,13,40]. The resulting protein thus maintains its ability to bind DUX4 targets but possesses a truncated C-terminus with inclusions of some amino acids encoded by the alternate locus. As the genomic breakpoints for this rearrangement are highly variable, the resultant length and amino acid sequence the C-terminal domain of the DUX4-fusion varies considerably between patients but consistently retains the DNA binding homeodomains (Figure 2) [9,12,39].
3. Disease Model
DUX4r B-ALL results in high-level expression of DUX4 [9,12]. Paradoxically, over-expression of wild-type DUX4 (WT DUX4) in a variety of cell types results in apoptosis [12,41]. To reconcile this paradox Yasuda et al. [12] suggest that the altered C-terminus of DUX4 which occurs due to the cryptic insertion results in a variant of the DUX4 transcription factor that is capable of binding DNA and altering transcription but does not lead to apoptosis. Follow up experiments conducted by Tanaka et al [42] support this hypothesis. Chromatin immunoprecipitation followed by sequencing (ChIP-seq) performed on the NALM6 cell line confirmed that DUX4-IGH binds to 97% of the same gene targets as WT DUX4. However, experiments involving inducible vectors led to up-regulation of significantly fewer genes by DUX4-IGH than WT DUX4. Additionally, luciferase reporter assays utilising the ZSCAN4 promoter, a well-known target of DUX4, indicated that DUX4-IGH demonstrates decreased transcriptional activity compared to DUX4 [42]. Similar experiments conducted with Reh cells transfected with patient-derived constructs of the DUX4-IGH fusion confirm this finding [43] and suggest that alteration of the C-terminus of DUX4-IGH attenuates the transcription inducing ability compared to WT DUX4.
The C-terminal transactivation domain of WT DUX4 associates with p300/CBP which act as co-activators of transcription [29]. Loss of the C-terminus is therefore predicted to prevent recruitment of p300/CBP and reduce the ability of DUX4-IGH to upregulate expression. This hypothesis is supported by studies showing clear differences between the GEP generated in cells transduced to express a full-length DUX4 transcript (DUX4-fl) and those expressing a truncated form of DUX4 (DUX4-s) lacking the C-terminal transactivation domain (Figure 2) [26,44]. Induced expression of DUX4-fl results in upregulated expression of several hundred genes, many of which normally function in germline or early stem cells. Only a subset of these genes is upregulated in cells expressing C-terminally truncated forms of DUX4. Furthermore, expression of DUX4-s does not result in cell death [26]. Additional research is needed, however, both to understand how dysregulated expression induced by DUX4-IGH results in leukaemic transformation and to determine how patient specific variation in the C-terminal portion of DUX4-IGH affects disease progression.
4. Genomic Landscape of DUX4r Leukaemia
Multiple genomic alterations are highly associated with the DUX4r subtype, the most prevalent of which is deletion or alteration of ERG. ERG is a transcription factor from the ETS family involved in the regulation of hematopoietic stem cell maintenance and differentiation [45,46]. Monoallelic intragenic deletions of ERG, most commonly involving deletion of exons 3–7 or exons 3–9, is observed in 3–5% of B-ALL cases, and almost exclusively in DUX4r [47,48]. ERG deletion was initially proposed to be the key mechanism for ERG deregulation [7], but is absent in 20–40% of patients with DUX4r. Furthermore, these deletions are often subclonal and the deletion breakpoint can vary between diagnosis and relapse indicating that ERG deletion is a secondary event in disease progression [10,47].
DUX4r patients have also been shown to express an alternative transcript isoform of ERG in which transcription is initiated at a non-canonical exon present in intron 6. This alternate ERG transcript (ERGalt) produces a truncated C-terminal ERG protein with an N-terminal encoded by 7 amino acids from the non-canonical exon 6, that acts as a competitive inhibitor of wild-type ERG [9]. DUX4-IGH has been shown to bind to an alternative transcription initiation site of within intron 6 of ERG, inducing expression of ERGalt [9]. Efforts to correlate the presence of ERG deletion with the expression of ERGalt show that levels of the ERGalt transcript are higher in patients with a detected monoallelic deletion [10]. Given that these deletions remove intron 6 where transcription of the alternative isoform is initiated, this increased expression must be occurring on the non-deleted allele, potentially resulting in further impairment of wild-type ERG transcription [9]. The role of ERGalt in disease progression, however, remains to be fully elucidated.
Patients with ERG deletion, even those with subclonal deletions, demonstrate good prognosis [10,47]. ERG has been shown in vivo and in mouse models to increase cell proliferation and is believed to be crucial for maintenance of human leukaemia [45]. In acute myeloid leukaemia (AML), duplication of ERG is significantly related with higher levels of expression and lower overall survival [49] while high ERG expression has been reported as a poor risk indicator in T-cell acute lymphoblastic leukaemia (T-ALL) [50]. Deletion or inhibition of ERG in B-ALL may therefore attenuate this effect. Cell line experiments investigating the role of ERG in leukaemogenesis have shown that short hairpin RNA (shRNA) knockdown of wild-type ERG led to inhibition of cell growth [45]. Together this data supports the observation that ERG deregulation offers a protective effect that may result in improved patient outcome.
Deletion of the transcription factor IKAROS Family Zinc Finger 1 (IKZF1), particularly the intragenic exon 4–7 deletion producing a dominant-negative isoform of Ikaros, have also been observed in a proportion of patients with DUX4r [8,19,47,48]. IKZF1 deletion has been reported in a variety of B-ALL subtypes but occurs with greater frequency in patients with the BCR-ABL1 translocation or Ph-like subtype [4,51]. Studies assessing the effect of co-occurring copy number alterations have demonstrated that IKZF1 deletion is an independent indicator of poor prognosis [52,53] except when observed in combination with ERG deletion [54]. This may explain why the presence of IKZF1 deletion does not translate into poorer outcomes for DUX4r patients [47,48]. Additional genomic alterations reported in DUX4r include deletion, or less commonly mutation of the lymphoid transcription factor, PAX5, and deletion of the cell cycle regulator CDKN2A or the paralogous gene CDKN2B [8,9,16,19]. Mutations in other transcriptional regulators not commonly affected in B-ALL, such as MYC, MYCBP2, and ZEB2 are less frequently observed, while mutations affecting Ras signaling, as well as epigenetic modifiers KMT2D [15], SETD2 and NCOR1 have also been reported [9,18]. Given that DUX4r is itself capable of inducing oncogenesis the role and significance of these additional mutations is as yet unclear.
5. Detecting DUX4r
Early research predominantly relied on the detection of intragenic ERG deletion as a marker for DUX4r [47], using Multiplex ligation-dependent probe amplification (MLPA) [55], SNP array [8,47] or genomic PCR using primers specific for the suspected deletion [10]. Genomic PCR showed higher sensitivity than MLPA [10] but neither was able to detect all cases with DUX4r as indicated by GEP [9,10,47]. While previously used as a surrogate of DUX4r, ERG deletion is now recognized as a secondary alteration and no longer relied upon for the detection of DUX4r. The expression of the ERGalt transcript produced in the presence of the DUX4-chimeric protein has also been suggested as a surrogate marker for DUX4r [9]. However, studies have shown that ERGalt can be expressed, albeit at lower levels, in other B-ALL subtypes. Furthermore, ERGalt expression may not be detected in all DUX4r patient samples and thus does not constitute an accurate or sensitive marker for subtype determination [10,15].
Diagnostic techniques for the detection of chromosomal translocations typically involve cytogenetic analysis, including G-banded karyotyping, fluorescence in situ hybridisation (FISH), or reverse transcriptase polymerase chain reaction (RT-PCR) for the detection of gene fusions with well-characterised breakpoints [56]. However, all of these techniques fail to conclusively detect fusions involving DUX4. DUX4r are cytogenetically cryptic due to the small size of the repeat sequence that is inserted into the IGH locus or [9], in the case of a reciprocal translocation, the fact that both DUX4 and IGH are located in subtelomeric regions [39]. Even though FISH has been highly effective at detecting other ALL specific translocations undetectable by karyotyping [57,58], the design of fluorescent probes to indicate the DUX4r is difficult for two reasons. Firstly, the repetitive nature of the D4Z4 array means that probes binding to this location will bind to multiple loci both on 4q and 10q. They could potentially cross-hybridize with additional highly homologous regions present on the short arms of all acrocentric and pericentromeric regions of multiple other chromosomes [59]. Secondly, the highly variable sequence and positions of breakpoints both within IGH and DUX4 make the design of break-apart fluorescent probes difficult.
Immunophenotyping has been employed for the prediction of some subtype defining genomic lesions in ALL [60]. Whilst surface expression of CRLF2 lends itself to flow cytometric detection of patients with CRLF2r [61], the detection of DUX4r is reliant upon expression of the cell surface antigen CD371 (CLL-1). This antigen is encoded by CLEC12A, known to be upregulated by DUX4 expression, and was detected on blast cells of DUX4r cases but shown to be almost absent in all other analysed subtypes in one study [62]. The few non-DUX4r samples with CD371 expression were shown to contain alternate subtype-specific lesions detectable by standard cytogenetics. Aberrant expression of CD2 has also been observed in patients with DUX4r [7,55] including patients who demonstrate monocytic lineage switch [55,63] and the combination of CD371 and CD2 has recently been suggested as a strong marker for DUX4r [60,62]. Additional studies are needed to confirm this finding and validate immunophenotyping as an accurate method for detection of DUX4r patients.
To date detection of the DUX4r subtype has been dependent almost exclusively upon NGS. Whole genome sequencing (WGS) has proven effective at detecting DUX4r, including determination of the breakpoint locations [13], but given its high cost is infrequently employed and not amenable as a diagnostic technique. Long read sequencing has been successfully performed on the NALM6 cell line characterised by the DUX4-IGH rearrangement in order to clarify genomic breakpoints and determine the full-length fusion transcript [12,39]. However, this form of sequencing has not been applied outside of research. More recently, genomic capture high throughput sequencing (gc-HTS) was utilised in a research setting for detection of clonal rearrangement of the IGH/TR- loci used for MRD monitoring. This sequencing approach was not only effective at detecting IGH and TRD rearrangements but also detected the presence of rearrangements involving the IGH locus (IGHr) including 10 BCP-ALL cases with IGH-DUX4. Authors reported that gc-HTS was a robust method for detecting IGHr requiring only a small amount of diagnostic material [40]. Further validation of this technique in a clinical setting is pending, though unless probes are designed to capture DUX4, this assay will miss DUX4r that does not involve IGH.
More commonly, research groups have relied upon transcriptome sequencing for analysis and detection of patients with DUX4r. Transcriptome sequencing allows for detection of transcribed gene fusions as well as GEP. Both direct detection of DUX4r through the identification of paired-end reads linking IGH and DUX4 [9,12,13,14,17,18,19], as well as the detection of the distinct expression profile characteristic of this subtype [14,17,18,19], are possible with RNA sequencing (RNA-seq) data. A variety of different fusion calling algorithms have been employed for direct detection of DUX4 and its fusion partner, including fusionCatcher [64], TopHat-fusion [65], defuse [66] and Cicero [67]. However, these algorithms do not consistently detect a fusion involving DUX4 in all cases where a DUX4r has been indicated by GEP [14,18,19]. Alternatively, direct detection and comparison of expression levels of DUX4 can be used to infer the presence of a DUX4r since DUX4 is not expressed in healthy somatic tissue or leukaemic cells other than those with the rearrangement [12]. However, accurate quantification of DUX4 expression requires consideration of the potential for short sequenced reads from the chimeric DUX4 transcript to align to multiple locations in the human reference genome [9].
Given the highly distinct GEP observed in patients with DUX4r [6,8], hierarchical clustering of expression data can reliably identify patients with this subtype. This can be performed using gene sets reported in the literature as being associated with the DUX4r subtype [14], or alternatively by performing unsupervised hierarchical clustering utilising the top 5–10% of genes with the highest variability in expression across a large cohort of ALL samples [17,18,19]. In both instances, RNA-seq data from a large number of samples is typically required and is thus difficult to perform outside of a research context. To attempt to resolve this issue, Brown et al. [68] have developed a random forest classifier trained on RNA-seq data from two published cohorts for detection of DUX4r and other B-ALL subtypes. However, the classifier has not yet been tested on a large validation cohort containing multiple DUX4r samples.
6. Clinical Presentation
DUX4r leukaemia has been reported in 4–7% of pediatric (<18 years) B-ALL patients [6,9,19], and has been associated with an older age of onset [13,47,48]. For example, Lilljebjörn et al, [13] report a median age of 6.5 years at time of diagnosis for paediatric DUX4r patients compared with 4 years for other B-ALL patients, while Marincervic-Zuniga et al, [15] report a median age of 9.3 compared to 4.5 years in their cohort. Studies investigating B-ALL in the adolescent and young adult population (16–39 years) suggest an enrichment in the proportion of DUX4r patients [12] although the lesion is observed across all age groups [17,18] (Table 1). At diagnosis, patients frequently present with lower white cell counts (WCC) compared with other B-ALL subtypes [16,48]. Immunophenotypic data indicates that DUX4r is exclusively associated with a B cell immunophenotype although aberrant expression of CD2, a T-lineage restricted cell marker, has been reported in a proportion of cases [7,48]. Patients have also been associated with lineage switching after the onset of treatment in which samples coexpress markers of both B lymphocyte and monocyte lineage. In addition, analysis of B-ALL samples which display lineage switching (swALL) show enrichment for DUX4r. This is observed as coexpression of CD19 and CD34 as well as CD33 and CD14. Not all DUX4r samples demonstrate swALL but those that do are reported to have poorer treatment response [63] and a higher rate of relapse [20] than non-swALL DUX4r.
Table 1.
Summary of findings from published studies identifying DUX4r subtype.
| Reference | Detection Method | Cohort (Age Range in Years) |
Frequency DUX4r | Additional Alterations | Prognosis | |||
|---|---|---|---|---|---|---|---|---|
| ERG | IKZF1 | PAX5 | CDKN2A | |||||
| Yeoh et al. 2002; [6] | Microarray GEP | Paediatric ALL (<19) | 14/327 (4.3%) | — | — | — | — | — |
| Mullighan et al. 2007; [7] | Microarray GEP | B-ALL | 19/218 (8.7%) | 13/19 (68.4%) | — | — | — | — |
| Harvey et al. 2010; [8] | Microarray GEP | HR * B-ALL (1–20) | 21/207 (10.1%) | 8/21 (38.1%) | 6/21 (28.6%) | 3/21 (14.3%) | 5/21 (23.8%) | 4-yr RFS 94% ± 5.1 |
| HR * B-ALL (validation cohort) | 5/99 (5.1%) | — | — | — | — | 1/5 (20%) relapse | ||
| Zhang et al. 2016; [9] | Microarray GEP RNA-seq (n=175) |
Paediatric B-ALL (0–15) | 94/1347 (7.0%) | 54/91 (59.3%) | 17/91 (18.7%) | 3/91 (3.3%) | — | — |
| Adolescent B-ALL (16–20) | 38/395 (9.62%) | 23/38 (60.5%) | 19/38 (50%) | 6/38 (15.8%) | — | — | ||
| Young Adult B-ALL (21–39) | 9/171 (5.3%) | 3/9 (33.3%) | 3/9 (33.3%) | 2/9 (22.2%) | — | — | ||
| Yasuda et al. 2016; [12] | RNA-seq | AYA Ph-negative B-ALL (15–39) | 12/62 (19.4%) | — | — | — | — | 8 CR; 1 CR after SCT; 1 Early mortality; 2 NA |
| Lilljebjörn et al. 2016; [13] | RNA-seq | Paediatric B-ALL (<18) | 8/195 (4%) | 5/8 (62.5%) | — | — | — | No observed relapses |
| Paediatric B-Other ^ (2–15) | 20/49 (40.8%) | 10/20 (50%) | — | — | — | 4/20 (20%) relapse | ||
| Liu et al. 2016; [19] | RNA-seq | Children (<18) | 6/94 (6.4%) | — | 3/6 (50%) | 4/6 (66.7%) | 3/6 (50%) | 5-yr OS 100% |
| Adult (>18) | 5/78 (6.4%) | — | 1/5 (20%) | 3/5 (60%) | 3/5 (60%) | 5-yr OS 53% | ||
| Vendramini 2017; [16] | Microarray GEP | Paediatric B-Other ^ (<18) | 35/143 (24.5%) | 14/34 (41.2%) | 12/34 (35.3%) | 4/34 (11.8%) | 5/34 (14.7%) | 5-yr EFS 91.1% 4.9 |
| Marincevic-Zuniga 2017 [15] | RNA-seq | Paediatric B-ALL (<18) | 9/116 (7.8%) | 7/9 (77.8%) | — | — | — | 1/9 (11.1%) relapses |
| Li et al. 2018; [18] | RNA-seq | Children (<18) | 50/906 (5.5%) | — | — | — | — | — |
| Adult (>18) | 13/258 (5.0%) | — | — | — | — | — | ||
| Zur Stadt et al. 2019; [40] | gc-HTS | B-ALL (excludes ETV6-RUNX1, KMT2Ar and Ph+ALL) | 10/164 (6.1%) | 2/10 (20%) | — | — | — | — |
| Zaliova et al. 2019; [14] | RNA-seq | Paediatric B-Other ^ (1–18) | 30/110 (27%) | 19/30 (63%) | 6/30 (20%) | 6/30 (20%) | 9/30 (30%) | — |
| Gu et al. 2019; [17] | RNA-seq | Paediatric (0.2–15) | 61/1191 (5.1%) | — | 2/35 (5.7%) | — | — | Child (<18) 5-yr EFS and OS 93.2% ± 3.8 Adult (>18) 5-yr EFS 84.6% ± 10; 5-yr OS 85.7% ± 9.4 |
| AYA B-ALL (16–39) | 33/419 (7.9%) | — | 3/18 (16.7%) | — | — | |||
| Adult B-ALL (40–79) | 12/378 (3.2%) | — | — | — | — | |||
Abbreviations: GEP (gene expression profiling); RFS (relapse free survival); HR (high-risk); CR (complete remission); SCT (stem-cell transplant); EFS (event free survival); OS (overall survival).— Indicates data not provided in the cited study; * Determination of high-risk (HR) status based on high white cell count (WCC), older age of disease onset, and lack of favourable genetic features (ETV6-RUNX1 or trisomy of chromosomes 4/10). ^ B-Other refers to B-ALL patients that do not belong to one of the following recognized subtypes: ETV6-RUNX1, BCR-ABL1, TCF3-PBX1, KMT2Ar, hyperdiploidy or hypodiploidy.
7. Prognosis and Treatment
As DUX4r is a recently described molecular lesion, there is currently no available data from prospective trials demonstrating its utility as an independent marker for risk stratification. This is hampered by difficulty in case ascertainment, as the lesion cannot be detected with standard diagnostic techniques. Patients with DUX4r have been reported to have higher levels of MRD throughout induction [14,40,48] and slower response to treatment [47]. Consequently, many patients within the DUX4r subtype are classified as intermediate or high risk based upon treatment response [14,40,47]. However, early reports investigating DUX4r subtype suggested that patients demonstrated excellent prognosis, particularly in paediatric patients who received intensive chemotherapy for remission induction [6,8].
Yasuda et al. [12] reported that patients with DUX4r demonstrated longer disease free survival after complete remission (CR) was achieved in adolescent and young adult patients; while Harvey et al. [8] reported significantly superior outcomes with 94% 4-year event free survival (EFS), though in the context of intensive chemotherapy given for high risk stratification (Table 1). Some studies have also reported good response to prednisolone in a majority of DUX4r cases [16,48]. Indeed the NALM6 cell line which demonstrates high expression of PDGFRA, a hallmark of ERG-deleted cases, was shown to be more sensitive to prednisolone than patients with low expression of PDGFRA [69].
Reports from more recent studies are varied and indicate differences in prognosis between pediatric and adult patients [19]. For example, in a study of 1988 B-ALL patients conducted by Gu et al. [17], DUX4r was associated with 93% EFS and overall survival (OS) in pediatric patients (<18) but 86% EFS and 84% OS in adults. Overall, it appears that presence of the fusion is associated with favourable outcomes, at least in the context of intensive chemotherapy applied as part of a risk-adapted approach to therapy. However, additional research on large uniformly treated cohorts is needed to confirm this finding. The reported protective effects of ERG deletion, and any other cooperating lesions, also requires further investigation to determine if this may enable stratification of patient risk within the DUX4r subtype [10,16].
Several B-ALL translocations, particularly those resulting in the production of chimeric kinases, have been shown to be targetable with precision medicine approaches [70]. DUX4r may constitute another B-ALL subtype which would be amenable to targeted therapy. Knock-down experiments utilising shRNA targeting the DUX4 fusion transcript have been effective at reducing cell proliferation [12]. Furthermore, mutations targeting the homeodomains of DUX4 can reduce DNA-binding activity of the transcription factor and abrogate the altered GEP of DUX4r [71]. This suggests that patients harbouring a DUX4r may be amenable to small molecule inhibitors that impede DNA binding. While there are currently no DUX4 inhibitor molecules available or in clinical trials, pre-clinical validation of a potential DUX4-IGH inhibitor is underway that could potentially lower treatment toxicity associated with intensive chemotherapy [72].
8. Conclusions
DUX4r represents a distinct subtype of B-ALL affecting 4–7% of pediatric patients, and a higher proportion of adolescents and young adults. Patients typically exhibit favourable outcomes in the context of intensive chemotherapy, but conjecture does exist and additional studies in large cohorts of uniformly treated patients are needed to confirm this finding. To this end the development of a specific and sensitive assay for detection of either DUX4 expression or the DUX4-fusion at diagnosis is essential. Early identification of patients with DUX4r as well as accurate identification of co-occurring alterations would enable studies to determine if secondary alterations such as ERG deletion are in themselves offering protective benefit, or if all patients with DUX4r subtype demonstrate good outcomes. Additional research into the mechanism of disease is also needed, specifically the impact of patient-specific variation in the DUX4-fusion and a greater understanding of the role of ERG deregulation in disease progression.
Acknowledgments
We would like to acknowledge the ongoing support of SAHMRI, NHMRC, The Cancer Council of South Australia and The Leukeamia Foundation Australia.
Author Contributions
Conceptualization, overall supervision and coordination of the manuscript preparation D.T.Y.; writing—original draft preparation, J.A.R., M.J.O. and D.T.Y.; Generation of table and figures J.A.R.; writing—review and editing, all authors. All authors have read and agreed to the published version of the manuscript.
Funding
This work is supported in part by grants from the National Health and Medical Research Council (NHMRC), South Australian Cancer Council Beat Cancer Project, The Leukaemia Foundation and Bristol-Meyers Squibb Company (to D.L.W.). J.R. is supported by a scholarship from the University of Adelaide. D.T.Y. is an NHMRC Early Career Fellow.
Conflicts of Interest
D.L.W. receives research support from BMS, and Honararia from BMS and Amgen. D.T.Y. receives research support from BMS & Novartis, and Honararia Amgen, BMS, Novartis, Takeda and Pfizer. None of these agencies have had a role in the preparation of this manuscript. All other authors declare no conflict of interest.
References
- 1.Inaba H., Greaves M., Mullighan C.G. Acute lymphoblastic leukaemia. Lancet. 2013;381:1943–1955. doi: 10.1016/S0140-6736(12)62187-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tasian S.K., Loh M.L., Hunger S.P. Childhood acute lymphoblastic leukemia: Integrating genomics into therapy. Cancer. 2015;121:3577–3590. doi: 10.1002/cncr.29573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hunger S.P., Mullighan C.G. Redefining ALL classification: Toward detecting high-risk ALL and implementing precision medicine. Blood. 2015;125:3977–3987. doi: 10.1182/blood-2015-02-580043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harvey R.C., Mullighan C.G., Chen I.-M., Wharton W., Mikhail F.M., Carroll A.J., Kang H., Liu W., Dobbin K.K., Smith M.A., et al. Rearrangement of CRLF2 is associated with mutation of JAK kinases, alteration of IKZF1, Hispanic/Latino ethnicity, and a poor outcome in pediatric B-progenitor acute lymphoblastic leukemia. Blood. 2010;115:5312–5321. doi: 10.1182/blood-2009-09-245944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mullighan C.G., Collins-Underwood J.R., Phillips L.A.A., Loudin M.G., Liu W., Zhang J., Ma J., Coustan-Smith E., Harvey R.C., Willman C.L., et al. Rearrangement of CRLF2 in B-progenitor-and Down syndrome-associated acute lymphoblastic leukemia. Nat. Genet. 2009;41:1243–1246. doi: 10.1038/ng.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yeoh E.-J., Ross M.E., Shurtleff S.A., Williams W.K., Patel D., Mahfouz R., Behm F.G., Raimondi S.C., Relling M.V., Patel A., et al. Classification, subtype discovery, and prediction of outcome in pediatric acute lymphoblastic leukemia by gene expression profiling. Cancer Cell. 2002;1:133–143. doi: 10.1016/S1535-6108(02)00032-6. [DOI] [PubMed] [Google Scholar]
- 7.Mullighan C.G., Miller C.B., Su X., Radtke I., Dalton J., Song G., Zhou X., Pui C.-H., Shurtleff S.A., Downing J.R. ERG Deletions Define a Novel Subtype of B-Progenitor Acute Lymphoblastic Leukemia. Blood. 2007;110:691. doi: 10.1182/blood.V110.11.691.691. [DOI] [Google Scholar]
- 8.Harvey R.C., Mullighan C.G., Wang X., Dobbin K.K., Davidson G.S., Bedrick E.J., Chen I.-M., Atlas S.R., Kang H., Ar K., et al. Identification of novel cluster groups in pediatric high-risk B-precursor acute lymphoblastic leukemia with gene expression profiling: Correlation with genome-wide DNA copy number alterations, clinical characteristics, and outcome. Blood. 2010;116:4874–4884. doi: 10.1182/blood-2009-08-239681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang J., McCastlain K., Yoshihara H., Xu B., Chang Y., Churchman M.L., Wu G., Li Y., Wei L., Iacobucci I., et al. Deregulation of DUX4 and ERG in acute lymphoblastic leukemia. Nat. Genet. 2016;48:1481–1489. doi: 10.1038/ng.3691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zaliova M., Potuckova E., Hovorkova L., Musilova A., Winkowska L., Fiser K., Stuchly J., Mejstrikova E., Starkova J., Zuna J., et al. ERG deletions in childhood acute lymphoblastic leukemia with DUX4 rearrangements are mostly polyclonal, prognostically relevant and their detection rate strongly depends on screening method sensitivity. Haematologica. 2019;104:1407–1416. doi: 10.3324/haematol.2018.204487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Potuckova E., Zuna J., Hovorkova L., Starkova J., Stary J., Trka J., Zaliova M. Intragenic ERG Deletions Do Not Explain the Biology of ERG-Related Acute Lymphoblastic Leukemia. PLoS ONE. 2016;11:e0160385. doi: 10.1371/journal.pone.0160385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yasuda T., Tsuzuki S., Kawazu M., Hayakawa F., Kojima S., Ueno T., Imoto N., Kohsaka S., Kunita A., Doi K., et al. Recurrent DUX4 fusions in B cell acute lymphoblastic leukemia of adolescents and young adults. Nat. Genet. 2016;48:569–574. doi: 10.1038/ng.3535. [DOI] [PubMed] [Google Scholar]
- 13.Lilljebjörn H., Henningsson R., Hyrenius-Wittsten A., Olsson L., Orsmark-Pietras C., von Palffy S., Askmyr M., Rissler M., Schrappe M., Cario G., et al. Identification of ETV6-RUNX1-like and DUX4-rearranged subtypes in paediatric B-cell precursor acute lymphoblastic leukaemia. Nat. Commun. 2016;7:11790. doi: 10.1038/ncomms11790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zaliova M., Stuchly J., Winkowska L., Musilova A., Fiser K., Slamova M., Starkova J., Vaskova M., Hrusak O., Sramkova L., et al. Genomic landscape of pediatric B-other acute lymphoblastic leukemia in a consecutive European cohort. Haematologica. 2019;104:1396–1406. doi: 10.3324/haematol.2018.204974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marincevic-Zuniga Y., Dahlberg J., Nilsson S., Raine A., Nystedt S., Lindqvist C.M., Berglund E.C., Abrahamsson J., Cavelier L., Forestier E., et al. Transcriptome sequencing in pediatric acute lymphoblastic leukemia identifies fusion genes associated with distinct DNA methylation profiles. J. Hematol. Oncol. 2017;10:148. doi: 10.1186/s13045-017-0515-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vendramini E., Giordan M., Giarin E., Michielotto B., Fazio G., Cazzaniga G., Biondi A., Silvestri D., Valsecchi M.G., Muckenthaler M.U., et al. High expression of miR-125b-2 and SNORD116 noncoding RNA clusters characterize ERG-related B cell precursor acute lymphoblastic leukemia. Oncotarget. 2017;8:42398–42413. doi: 10.18632/oncotarget.16392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gu Z., Churchman M.L., Roberts K.G., Moore I., Zhou X., Nakitandwe J., Hagiwara K., Pelletier S., Gingras S., Berns H., et al. PAX5-driven subtypes of B-progenitor acute lymphoblastic leukemia. Nat. Genet. 2019;51:296–307. doi: 10.1038/s41588-018-0315-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li J.F., Dai Y.T., Lilljebjörn H., Shen S.H., Cui B.W., Bai L., Liu Y.F., Qian M.X., Kubota Y., Kiyoi H., et al. Transcriptional landscape of B cell precursor acute lymphoblastic leukemia based on an international study of 1,223 cases. Proc. Natl. Acad. Sci. USA. 2018;115:E11711–E11720. doi: 10.1073/pnas.1814397115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu Y.-F., Wang B.-Y., Zhang W.-N., Huang J.-Y., Li B.-S., Zhang M., Jiang L., Li J.-F., Wang M.-J., Dai Y.-J., et al. Genomic Profiling of Adult and Pediatric B-cell Acute Lymphoblastic Leukemia. EBioMedicine. 2016;8:173–183. doi: 10.1016/j.ebiom.2016.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schroeder M.P., Bastian L., Eckert C., Gökbuget N., James A.R., Tanchez J.O., Schlee C., Isaakidis K., Häupl B., Baum K., et al. Integrated analysis of relapsed B-cell precursor Acute Lymphoblastic Leukemia identifies subtype-specific cytokine and metabolic signatures. Sci. Rep. 2019;9:4188. doi: 10.1038/s41598-019-40786-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.James A.R., Schroeder M.P., Neumann M., Bastian L., Eckert C., Gökbuget N., Tanchez J.O., Schlee C., Isaakidis K., Schwartz S., et al. Long non-coding RNAs defining major subtypes of B cell precursor acute lymphoblastic leukemia. J. Hematol. Oncol. 2019;12:8. doi: 10.1186/s13045-018-0692-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Winokur S.T., Bengtsson U., Feddersen J., Mathews K.D., Weiffenbach B., Bailey H., Markovich R.P., Murray J.C., Wasmuth J.J., Altherr M.R. The DNA rearrangement associated with facioscapulohumeral muscular dystrophy involves a heterochromatin-associated repetitive element: Implications for a role of chromatin structure in the pathogenesis of the disease. Chromosome Res. 1994;2:225–234. doi: 10.1007/BF01553323. [DOI] [PubMed] [Google Scholar]
- 23.Cacurri S., Piazzo N., Deidda G., Vigneti E., Galluzzi G., Colantoni L., Merico B., Ricci E., Felicetti L. Sequence homology between 4qter and 10qter loci facilitates the instability of subtelomeric KpnI repeat units implicated in facioscapulohumeral muscular dystrophy. Am. J. Hum. Genet. 1998;63:181–190. doi: 10.1086/301906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Geel M., Dickson M.C., Beck A.F., Bolland D.J., Frants R.R., van der Maarel S.M., de Jong P.J., Hewitt J.E. Genomic analysis of human chromosome 10q and 4q telomeres suggests a common origin. Genomics. 2002;79:210–217. doi: 10.1006/geno.2002.6690. [DOI] [PubMed] [Google Scholar]
- 25.van Deutekom J.C., Wijmenga C., van Tienhoven E.A., Gruter A.M., Hewitt J.E., Padberg G.W., van Ommen G.J., Hofker M.H., Frants R.R. FSHD associated DNA rearrangements are due to deletions of integral copies of a 3.2 kb tandemly repeated unit. Hum. Mol. Genet. 1993;2:2037–2042. doi: 10.1093/hmg/2.12.2037. [DOI] [PubMed] [Google Scholar]
- 26.Geng L.N., Yao Z., Snider L., Fong A.P., Cech J.N., Young J.M., van der Maarel S.M., Ruzzo W.L., Gentleman R.C., Tawil R., et al. DUX4 activates germline genes, retroelements, and immune mediators: Implications for facioscapulohumeral dystrophy. Dev. Cell. 2012;22:38–51. doi: 10.1016/j.devcel.2011.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Snider L., Geng L.N., Lemmers R.J.L.F., Kyba M., Ware C.B., Nelson A.M., Tawil R., Filippova G.N., van der Maarel S.M., Tapscott S.J., et al. Facioscapulohumeral dystrophy: Incomplete suppression of a retrotransposed gene. PLoS Genet. 2010;6:e1001181. doi: 10.1371/journal.pgen.1001181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gabriëls J., Beckers M.C., Ding H., De Vriese A., Plaisance S., van der Maarel S.M., Padberg G.W., Frants R.R., Hewitt J.E., Collen D., et al. Nucleotide sequence of the partially deleted D4Z4 locus in a patient with FSHD identifies a putative gene within each 3.3 kb element. Gene. 1999;236:25–32. doi: 10.1016/S0378-1119(99)00267-X. [DOI] [PubMed] [Google Scholar]
- 29.Choi S.H., Gearhart M.D., Cui Z., Bosnakovski D., Kim M., Schennum N., Kyba M. DUX4 recruits p300/CBP through its C-terminus and induces global H3K27 acetylation changes. Nucleic Acids Res. 2016;44:5161–5173. doi: 10.1093/nar/gkw141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wijmenga C., Hewitt J.E., Sandkuijl L.A., Clark L.N., Wright T.J., Dauwerse H.G., Gruter A.M., Hofker M.H., Moerer P., Williamson R. Chromosome 4q DNA rearrangements associated with facioscapulohumeral muscular dystrophy. Nat. Genet. 1992;2:26–30. doi: 10.1038/ng0992-26. [DOI] [PubMed] [Google Scholar]
- 31.Pandya S., King W.M., Tawil R. Facioscapulohumeral dystrophy. Phys. Ther. 2008;88:105–113. doi: 10.2522/ptj.20070104. [DOI] [PubMed] [Google Scholar]
- 32.Zeng W., de Greef J.C., Chen Y.-Y., Chien R., Kong X., Gregson H.C., Winokur S.T., Pyle A., Robertson K.D., Schmiesing J.A., et al. Specific loss of histone H3 lysine 9 trimethylation and HP1gamma/cohesin binding at D4Z4 repeats is associated with facioscapulohumeral dystrophy (FSHD) PLoS Genet. 2009;5:e1000559. doi: 10.1371/journal.pgen.1000559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Overveld P.G.M., Lemmers R.J.F.L., Sandkuijl L.A., Enthoven L., Winokur S.T., Bakels F., Padberg G.W., van Ommen G.-J.B., Frants R.R., van der Maarel S.M. Hypomethylation of D4Z4 in 4q-linked and non-4q-linked facioscapulohumeral muscular dystrophy. Nat. Genet. 2003;35:315–317. doi: 10.1038/ng1262. [DOI] [PubMed] [Google Scholar]
- 34.Lemmers R.J.L.F., van der Vliet P.J., Klooster R., Sacconi S., Camaño P., Dauwerse J.G., Snider L., Straasheijm K.R., van Ommen G.J., Padberg G.W., et al. A unifying genetic model for facioscapulohumeral muscular dystrophy. Science. 2010;329:1650–1653. doi: 10.1126/science.1189044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dmitriev P., Kairov U., Robert T., Barat A., Lazar V., Carnac G., Laoudj-Chenivesse D., Vassetzky Y.S. Cancer-related genes in the transcription signature of facioscapulohumeral dystrophy myoblasts and myotubes. J. Cell. Mol. Med. 2014;18:208–217. doi: 10.1111/jcmm.12182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dib C., Zakharova V., Popova E., Kiseleva E., Chernyak B., Lipinski M., Vassetzky Y.S. DUX4 Pathological Expression: Causes and Consequences in Cancer. Trends Cancer Res. 2019;5:268–271. doi: 10.1016/j.trecan.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 37.Kawamura-Saito M., Yamazaki Y., Kaneko K., Kawaguchi N., Kanda H., Mukai H., Gotoh T., Motoi T., Fukayama M., Aburatani H., et al. Fusion between CIC and DUX4 up-regulates PEA3 family genes in Ewing-like sarcomas with t(4;19)(q35;q13) translocation. Hum. Mol. Genet. 2006;15:2125–2137. doi: 10.1093/hmg/ddl136. [DOI] [PubMed] [Google Scholar]
- 38.Dyer M.J.S., Akasaka T., Capasso M., Dusanjh P., Lee Y.F., Karran E.L., Nagel I., Vater I., Cario G., Siebert R. Immunoglobulin heavy chain locus chromosomal translocations in B-cell precursor acute lymphoblastic leukemia: Rare clinical curios or potent genetic drivers? Blood. 2010;115:1490–1499. doi: 10.1182/blood-2009-09-235986. [DOI] [PubMed] [Google Scholar]
- 39.Tian L., Shao Y., Nance S., Dang J., Xu B., Ma X., Li Y., Ju B., Dong L., Newman S., et al. Long-read sequencing unveils IGH-DUX4 translocation into the silenced IGH allele in B-cell acute lymphoblastic leukemia. Nat. Commun. 2019;10:2789. doi: 10.1038/s41467-019-10637-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zur Stadt U., Alawi M., Adao M., Indenbirken D., Escherich G., Horstmann M.A. Characterization of novel, recurrent genomic rearrangements as sensitive MRD targets in childhood B-cell precursor ALL. Blood Cancer J. 2019;9:96. doi: 10.1038/s41408-019-0257-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kowaljow V., Marcowycz A., Ansseau E., Conde C.B., Sauvage S., Mattéotti C., Arias C., Corona E.D., Nuñez N.G., Leo O., et al. The DUX4 gene at the FSHD1A locus encodes a pro-apoptotic protein. Neuromuscul. Disord. 2007;17:611–623. doi: 10.1016/j.nmd.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 42.Tanaka Y., Kawazu M., Yasuda T., Tamura M., Hayakawa F., Kojima S., Ueno T., Kiyoi H., Naoe T., Mano H. Transcriptional activities of DUX4 fusions in B-cell acute lymphoblastic leukemia. Haematologica. 2018;103:e522–e526. doi: 10.3324/haematol.2017.183152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dong X., Zhang W., Wu H., Huang J., Zhang M., Wang P., Zhang H., Chen Z., Chen S.-J., Meng G. Structural basis of DUX4/IGH-driven transactivation. Leukemia. 2018;32:1466–1476. doi: 10.1038/s41375-018-0093-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mitsuhashi H., Ishimaru S., Homma S., Yu B., Honma Y., Beermann M.L., Miller J.B. Functional domains of the FSHD-associated DUX4 protein. Biol. Open. 2018;7:bio033977. doi: 10.1242/bio.033977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tsuzuki S., Taguchi O., Seto M. Promotion and maintenance of leukemia by ERG. Blood. 2011;117:3858–3868. doi: 10.1182/blood-2010-11-320515. [DOI] [PubMed] [Google Scholar]
- 46.Taoudi S., Bee T., Hilton A., Knezevic K., Scott J., Willson T.A., Collin C., Thomas T., Voss A.K., Kile B.T., et al. ERG dependence distinguishes developmental control of hematopoietic stem cell maintenance from hematopoietic specification. Genes Dev. 2011;25:251–262. doi: 10.1101/gad.2009211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Clappier E., Auclerc M.F., Rapion J., Bakkus M., Caye A., Khemiri A., Giroux C., Hernandez L., Kabongo E., Savola S., et al. An intragenic ERG deletion is a marker of an oncogenic subtype of B-cell precursor acute lymphoblastic leukemia with a favorable outcome despite frequent IKZF1 deletions. Leukemia. 2014;28:70–77. doi: 10.1038/leu.2013.277. [DOI] [PubMed] [Google Scholar]
- 48.Zaliova M., Zimmermannova O., Dörge P., Eckert C., Möricke A., Zimmermann M., Stuchly J., Teigler-Schlegel A., Meissner B., Koehler R., et al. ERG deletion is associated with CD2 and attenuates the negative impact of IKZF1 deletion in childhood acute lymphoblastic leukemia. Leukemia. 2014;28:182–185. doi: 10.1038/leu.2013.282. [DOI] [PubMed] [Google Scholar]
- 49.Nibourel O., Guihard S., Roumier C., Pottier N., Terre C., Paquet A., Peyrouze P., Geffroy S., Quentin S., Alberdi A., et al. Copy-number analysis identified new prognostic marker in acute myeloid leukemia. Leukemia. 2017;31:555–564. doi: 10.1038/leu.2016.265. [DOI] [PubMed] [Google Scholar]
- 50.Baldus C.D., Martus P., Burmeister T., Schwartz S., Gökbuget N., Bloomfield C.D., Hoelzer D., Thiel E., Hofmann W.K. Low ERG and BAALC expression identifies a new subgroup of adult acute T-lymphoblastic leukemia with a highly favorable outcome. J. Clin. Oncol. 2007;25:3739–3745. doi: 10.1200/JCO.2007.11.5253. [DOI] [PubMed] [Google Scholar]
- 51.Mullighan C.G., Miller C.B., Radtke I., Phillips L.A., Dalton J., Ma J., White D., Hughes T.P., Le Beau M.M., Pui C.-H., et al. BCR-ABL1 lymphoblastic leukaemia is characterized by the deletion of Ikaros. Nature. 2008;453:110–114. doi: 10.1038/nature06866. [DOI] [PubMed] [Google Scholar]
- 52.Boer J.M., van der Veer A., Rizopoulos D., Fiocco M., Sonneveld E., de Groot-Kruseman H.A., Kuiper R.P., Hoogerbrugge P., Horstmann M., Zaliova M., et al. Prognostic value of rare IKZF1 deletion in childhood B-cell precursor acute lymphoblastic leukemia: An international collaborative study. Leukemia. 2016;30:32–38. doi: 10.1038/leu.2015.199. [DOI] [PubMed] [Google Scholar]
- 53.Mullighan C.G., Su X., Zhang J., Radtke I., Phillips L.A.A., Miller C.B., Ma J., Liu W., Cheng C., Schulman B.A., et al. Deletion of IKZF1 and prognosis in acute lymphoblastic leukemia. N. Engl. J. Med. 2009;360:470–480. doi: 10.1056/NEJMoa0808253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stanulla M., Dagdan E., Zaliova M., Möricke A., Palmi C., Cazzaniga G., Eckert C., Te Kronnie G., Bourquin J.-P., Bornhauser B., et al. IKZF1plus Defines a New Minimal Residual Disease-Dependent Very-Poor Prognostic Profile in Pediatric B-Cell Precursor Acute Lymphoblastic Leukemia. J. Clin. Oncol. 2018;36:1240–1249. doi: 10.1200/JCO.2017.74.3617. [DOI] [PubMed] [Google Scholar]
- 55.Slamova L., Starkova J., Fronkova E., Zaliova M., Reznickova L., van Delft F.W., Vodickova E., Volejnikova J., Zemanova Z., Polgarova K., et al. CD2-positive B-cell precursor acute lymphoblastic leukemia with an early switch to the monocytic lineage. Leukemia. 2014;28:609–620. doi: 10.1038/leu.2013.354. [DOI] [PubMed] [Google Scholar]
- 56.Akkari Y.M.N., Bruyere H., Hagelstrom R.T., Kanagal-Shamanna R., Liu J., Luo M., Mikhail F.M., Pitel B.A., Raca G., Shago M., et al. Evidence-based review of genomic aberrations in B-lymphoblastic leukemia/lymphoma: Report from the cancer genomics consortium working group for lymphoblastic leukemia. Cancer Genet. 2020;243:52–72. doi: 10.1016/j.cancergen.2020.03.001. [DOI] [PubMed] [Google Scholar]
- 57.Harrison C.J., Moorman A.V., Barber K.E., Broadfield Z.J., Cheung K.L., Harris R.L., Jalali G.R., Robinson H.M., Strefford J.C., Stewart A., et al. Interphase molecular cytogenetic screening for chromosomal abnormalities of prognostic significance in childhood acute lymphoblastic leukaemia: A UK Cancer Cytogenetics Group Study. Br. J. Haematol. 2005;129:520–530. doi: 10.1111/j.1365-2141.2005.05497.x. [DOI] [PubMed] [Google Scholar]
- 58.Russell L.J., Capasso M., Vater I., Akasaka T., Bernard O.A., Calasanz M.J., Chandrasekaran T., Chapiro E., Gesk S., Griffiths M., et al. Deregulated expression of cytokine receptor gene, CRLF2, is involved in lymphoid transformation in B-cell precursor acute lymphoblastic leukemia. Blood. 2009;114:2688–2698. doi: 10.1182/blood-2009-03-208397. [DOI] [PubMed] [Google Scholar]
- 59.Hewitt J.E., Lyle R., Clark L.N., Valleley E.M., Wright T.J., Wijmenga C., van Deutekom J.C., Francis F., Sharpe P.T., Hofker M. Analysis of the tandem repeat locus D4Z4 associated with facioscapulohumeral muscular dystrophy. Hum. Mol. Genet. 1994;3:1287–1295. doi: 10.1093/hmg/3.8.1287. [DOI] [PubMed] [Google Scholar]
- 60.Ohki K., Takahashi H., Fukushima T., Nanmoku T., Kusano S., Mori M., Nakazawa Y., Yuza Y., Migita M., Okuno H., et al. Impact of immunophenotypic characteristics on genetic subgrouping in childhood acute lymphoblastic leukemia: Tokyo Children’s Cancer Study Group (TCCSG) study L04-16. Genes Chromosomes Cancer. 2020;59:551–561. doi: 10.1002/gcc.22858. [DOI] [PubMed] [Google Scholar]
- 61.Tasian S.K., Doral M.Y., Borowitz M.J., Wood B.L., Chen I.-M., Harvey R.C., Gastier-Foster J.M., Willman C.L., Hunger S.P., Mullighan C.G., et al. Aberrant STAT5 and PI3K/mTOR pathway signaling occurs in human CRLF2-rearranged B-precursor acute lymphoblastic leukemia. Blood. 2012;120:833–842. doi: 10.1182/blood-2011-12-389932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schinnerl D., Mejstrikova E., Schumich A., Zaliova M., Fortschegger K., Nebral K., Attarbaschi A., Fiser K., Kauer M.O., Popitsch N., et al. CD371 cell surface expression: A unique feature of DUX4-rearranged acute lymphoblastic leukemia. Haematologica. 2019;104:e352–e355. doi: 10.3324/haematol.2018.214353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Novakova M., Vakrmanova B., Slamova L., Musilova A., Brüggemann M., Ritgen M., Fronkova E., Kalina T., Trka J., Stary J., et al. Switching Towards Monocytic Lineage and Discordancy between Flow Cytometric and PCR Minimal Residual Disease Results Is a Hallmark Feature of DUX4 Rearranged B-Cell Precursor Acute Lymphoblastic Leukemia. Blood. 2018;132:2825. doi: 10.1182/blood-2018-99-116575. [DOI] [Google Scholar]
- 64.Nicorici D., Şatalan M., Edgren H., Kangaspeska S., Murumägi A., Kallioniemi O., Virtanen S., Kilkku O. FusionCatcher—A tool for finding somatic fusion genes in paired-end RNA-sequencing data. bioRxiv. 2014:011650. [Google Scholar]
- 65.Kim D., Salzberg S.L. TopHat-Fusion: An algorithm for discovery of novel fusion transcripts. Genome Biol. 2011;12:R72. doi: 10.1186/gb-2011-12-8-r72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.McPherson A., Hormozdiari F., Zayed A., Giuliany R., Ha G., Sun M.G.F., Griffith M., Heravi Moussavi A., Senz J., Melnyk N., et al. deFuse: An algorithm for gene fusion discovery in tumor RNA-Seq data. PLoS Comput. Biol. 2011;7:e1001138. doi: 10.1371/journal.pcbi.1001138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tian L., Li Y., Edmonson M.N., Zhou X., Newman S., McLeod C., Thrasher A., Liu Y., Tang B., Rusch M.C., et al. CICERO: A versatile method for detecting complex and diverse driver fusions using cancer RNA sequencing data. Genome Biol. 2020;21:126. doi: 10.1186/s13059-020-02043-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Brown L.M., Lonsdale A., Zhu A., Davidson N.M., Schmidt B., Hawkins A., Wallach E., Martin M., Mechinaud F.M., Khaw S.L., et al. The application of RNA sequencing for the diagnosis and genomic classification of pediatric acute lymphoblastic leukemia. Blood Adv. 2020;4:930–942. doi: 10.1182/bloodadvances.2019001008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jerchel I.S., Chatzivasileiou D., Hoogkamer A.Q., Boer J.M., Beverloo H.B., Pieters R., den Boer M.L. High PDGFRA expression does not serve as an effective therapeutic target in ERG-deleted B-cell precursor acute lymphoblastic leukemia. Haematologica. 2018;103:e73–e77. doi: 10.3324/haematol.2017.171702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Roberts K.G., Li Y., Payne-Turner D., Harvey R.C., Yang Y.-L., Pei D., McCastlain K., Ding L., Lu C., Song G., et al. Targetable kinase-activating lesions in Ph-like acute lymphoblastic leukemia. N. Engl. J. Med. 2014;371:1005–1015. doi: 10.1056/NEJMoa1403088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dong X., Zhang H., Cheng N., Li K., Meng G. DUX4HD2-DNAERG structure reveals new insight into DUX4-Responsive-Element. Leukemia. 2019;33:550–553. doi: 10.1038/s41375-018-0273-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Salome’ M., Caronni C., Runfola V., Giambruno R., Campolungo D., Ghirardi C., Gabellini D. PB1661 Characterization of a DUX4-IGH inhibitor as a possible treatment for acute lymphoblastic leukemia. HemaSphere. 2019;3:768. doi: 10.1097/01.HS9.0000564892.23559.d7. [DOI] [Google Scholar]