Abstract
Liver fibrosis, a reversible pathological process of inflammation and fiber deposition caused by chronic liver injury and can cause severe health complications, including liver failure, liver cirrhosis, and liver cancer. Traditional diagnostic methods and drug-based therapy have several limitations, such as lack of precision and inadequate therapeutic efficiency. As a medical application of nanotechnology, nanomedicine exhibits great potential for liver fibrosis diagnosis and therapy. Nanomedicine enhances imaging contrast and improves tissue penetration and cellular internalization; it simultaneously achieves targeted drug delivery, combined therapy, as well as diagnosis and therapy (i.e., theranostics). In this review, recent designs and development efforts of nanomedicine systems for the diagnosis, therapy, and theranostics of liver fibrosis are introduced. Relative to traditional methods, these nanomedicine systems generally demonstrate significant improvement in liver fibrosis treatment. Perspectives and challenges related to these nanomedicine systems translated from laboratory to clinical use are also discussed.
Keywords: nanomedicine, liver fibrosis, diagnosis, therapy, theranostics, targeted drug delivery
1. Introduction
Liver fibrosis is an important pathological and repair process in chronic liver disease, which is caused by chronic viral hepatitis, alcohol, and non-alcoholic steatohepatitis (NASH), and autoimmune liver disease [1,2,3]. It has been reported that liver diseases caused 4.6% of all deaths in the Asia-Pacific region, 2.7% in the USA, and 2.1% in Europe in 2015. The Asia-Pacific region holds more than half of the global population and accounted for 62.6% of all deaths due to liver diseases globally in 2015. Chronic hepatitis B virus (HBV) infection caused more than half of the deaths due to cirrhosis and other chronic liver diseases, followed by alcohol consumption, non-alcoholic fatty liver disease, and chronic infection with hepatitis C virus [4]. With persistent damage, live fibrosis develops into cirrhosis and, even to hepatocellular carcinoma, together with a series of complications, including hepatic encephalopathy, hepatic failure, and portal hypertension [5,6].
Liver fibrosis is currently diagnosed based on ultrasound imaging and blood testing, both of which lack precision [7]. Chemical drugs [8], Chinese herbal medicines [9], and monoclonal antibodies [10] are also being developed for the treatment of liver fibrosis. These approaches aim to remove injurious stimuli, suppress hepatic inflammation, down regulate hepatic stellate cell (HSC) activation, and promote matrix degradation [11]. However, these approaches exhibit limited therapeutic efficiency and have side effects. Therapeutic methods with enhanced therapeutic efficiency and targeted capabilities need to be developed. Precise diagnostic methods are also needed to monitor the progression of the disease.
Nanomedicine involves the design and application of nanoparticles (NPs) in the diagnosis and treatment of diseases [12,13,14]. As an important area of nanotechnology research, nanomedicine has greatly contributed to biomedicine in recent decades. Finely designed nanostructures have been fabricated as effective therapeutic agents for liver fibrosis with specific site-targeting abilities [15,16,17]. Nanostructures have also been developed as nanoagents for contrast enhancement or nanoprobes for the diagnosis of liver fibrosis [18]. Numerous inorganic or organic NPs have thus far been extensively investigated for the diagnosis and treatment of liver fibrosis, including metal oxide NPs [18], metal NPs [19], lipid NPs [20], polymer NPs [21], and protein NPs [22]. The various composition, controllable shape, size, and modifiable surface properties of NPs provide to them superior advantages, including controlled drug release, cell-tissue gap penetration, high contrast, prolonged duration in the bloodstream, improvement of the pharmacokinetics of drugs, and reduction of toxic side effects [23]. A greater significance of such systems is that they allow the integration of diagnosis and therapy in one nanoplatform [24].
The current review summarizes potential targets and the application of emerging nanomedicine systems for liver fibrosis diagnosis and therapy, including liposomes, polymer NPs, protein NPs, inorganic NPs, and hybrid NPs. Major research gaps, challenges, and coping strategies for the treatment of liver fibrosis by using nanomedicine are also discussed.
2. Potential Targets of Liver Fibrosis
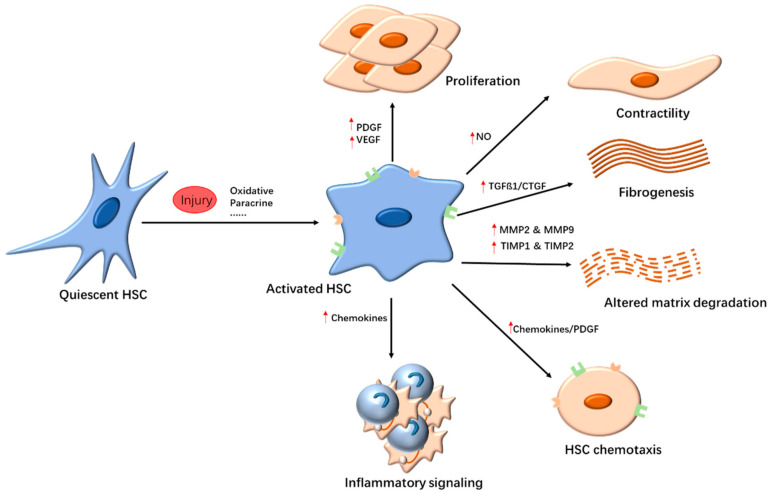
Activated HSCs are involved in the inflammatory response, fibrogenesis, and angiogenesis in liver fibrosis (Figure 1). They are at the center of liver fibrosis. Therefore, HSC-targeted strategies can be developed for the treatment of liver fibrosis. Alternative strategies include anti-inflammatory agents and inhibition of collagen deposition.
Figure 1.
Hepatic stellate cell (HSC) activation. The pathways of HSC activation include initiation and perpetuation stages. Initiation is stimulated by reactive oxygen species (ROS), paracrine stimuli, and so on. The continuous stimulation could induce HSCs into myofibroblast cells, and the perpetuation phase occurs, which is involved in the change of HSC behavior, including proliferation, contractility, fibrogenesis, altered matrix degradation, chemotaxis, and inflammatory signaling. Abbreviations: CTGF, connective tissue growth factor; HSC, hepatic stellate cell; MMP, matrix metalloproteinase; NO, nitric oxide; PDGF, platelet-derived growth factor; TGF-β1, transforming growth factor β1; TIMP, tissue inhibitor of metalloproteinase; VEGF, vascular endothelial growth factor.
2.1. Targeting HSCs
Comprising about 13% of total liver cells, HSCs exist in the sinus space and come in direct contact with hepatic epithelial cells and endothelial cells [25]. In their normal state, HSCs are quiescent and mainly participate in vitamin A (VA) metabolism and fat storage. If the liver suffers from injuries, HSCs are activated and transformed into myofibroblasts. Activation of HSCs is a hallmark of liver fibrosis. Activated HSCs typically express smooth muscle actin (α-SMA); in addition, they synthesize and secrete the extracellular matrix (ECM). ECM deposition changes the structure and function of liver tissue, which is the root cause of liver fibrosis [26,27]. Therefore, activated HSCs are among the important targets for liver fibrosis therapy. Numerous signaling molecules are involved in the activation of HSCs, with TGF-β and PDGF being the important ones [27,28,29]. Therefore, blocking the TGF-β or PDGF signaling pathways is an effective strategy for the treatment of liver fibrosis. Protease inhibitors, such as camostat mesilate (FOY305), can neutralize TGF-β [30]. As a multi-target receptor tyrosine kinase inhibitor, sorafenib, targets the Raf/ERK signaling pathways and PDGF receptor and can effectively attenuate experimental liver fibrosis, inflammation, and angiogenesis [31]. Moreover, many anti-fibrosis drugs, such as the semisynthetic analog of fumagillin-TNP-470 [32] and the fungal metabolite-OPC-15161 [33], suppress the activation and proliferation of HSCs. Moreover, ROS contributes to liver fibrosis by promoting the activation and proliferation of fibroblasts and myofibroblasts, as well as the activating the TGF-β pathway in an autocrine manner [34]. Antioxidants, such as vitamin E [35], silymarin [36], N-acetylcysteine [8], resveratrol [37], quercetin [9], phosphatidylcholine [38], and glutathione [39], can inhibit the activation of HSCs and reduce liver fibrosis. These drugs benefit patients with alcoholic liver disease and NASH.
HSCs are also involved in hepatic angiogenesis and hepatic sinus vascular remodeling. When stimulated by inflammatory factors or hypoxia, HSCs can directly express VEGF and angiopoietin-1, influencing angiogenesis in the liver [40,41]. Pathological angiogenesis is related to the process of liver fibrosis and cirrhosis [42]. During liver fibrosis, fibrous scar tissue presses against the portal vein and central vein, leading to increased intrahepatic resistance. Simultaneously, liver sinus capillarization and fibrous scar obstruction also increase the resistance of blood flow and oxygen diffusion. These processes result in low oxygen conditions in the liver and gene expression, which are sensitive to oxygen concentration such as hypoxia-inducible factors (HIFs). Pathological angiogenesis cannot improve the oxygen level in the liver because of the high permeability of new blood vessels induced by VEGF. Therefore, pathologic angiogenesis and hypoxemia interfere with normal tissue repair and promote the development of liver fibrosis [43]. Pathological angiogenesis plays an important role in liver fibrosis and thus has been considered as an important therapeutic target for the reversal of liver fibrosis. One study found that the knockout of HIF-1α in rats significantly ameliorated liver fibrosis, indicating that improving intrahepatic hypoxia could effectively treat such a disease [44].
2.2. Anti-Inflammatory Response
An inflammatory response to autocrine or paracrine stimulation prompts HSC activation and proliferation. HSC activation consists of two stages: initiation and perpetuation [25,27]. Early changes in gene expression and phenotype represent the initiation stage. Initiation is mainly induced by cytokines, or other stimuli from cells around HSCs and act as paracrine pathways [27]. Reactive oxygen species (ROS) released from Kupffer cells can directly stimulate and activate HSCs [45]. By cascade amplification of inflammatory response, a large number of inflammatory cells infiltrate the damaged sites, and secrete inflammatory cytokines, leading to HSC activation and proliferation [46]. Continuous stimulation can induce HSCs into myofibroblast cells, inducing the perpetuation stage. The activated HSCs subsequently release chemokines, further aggravating the inflammatory response. In this stage, HSC promotes inflammation, fibrosis, and cell proliferation in the autocrine and/or paracrine pathway. Therefore, the inflammation response plays an important role in liver fibrosis. Anti-inflammatory drugs such as corticosteroids [47], colchicine [48], and ursodeoxycholic acid [49] have been used to treat liver fibrosis. Another anti-inflammatory strategy involves the application of specific receptor antagonists to neutralize inflammatory cytokines. In one study, the antifibrotic and anti-inflammatory effects of IL-10 were observed in patients infected with hepatitis C [50]. Moreover, hepatic macrophages participate in the pathogenesis of liver fibrosis by the secretion of inflammatory factors. Targeting hepatic macrophages is also an effective anti-inflammatory technique for the treatment of liver fibrosis [51].
2.3. Inhibition of Collagen Deposition
The main clinical feature of liver fibrosis is the excessive deposition of ECM, particularly collagen. Collagen I is the main component in ECM, and the cross-linking of collagen I is significantly increased in liver fibrosis. Therefore, collagen I reduction has been adopted to treat liver fibrosis. In one study, the monoclonal antibody AB0023, which is an inhibitor of the matrix remodeling enzyme LOXL2, inhibited liver fibrosis by regulating the cross-linking of collagen I [52]. In another study, the human monoclonal antibody GS-6624 was used for the treatment of NASH-induced liver fibrosis [11].
3. Nanomedicine in Liver Fibrosis Diagnosis
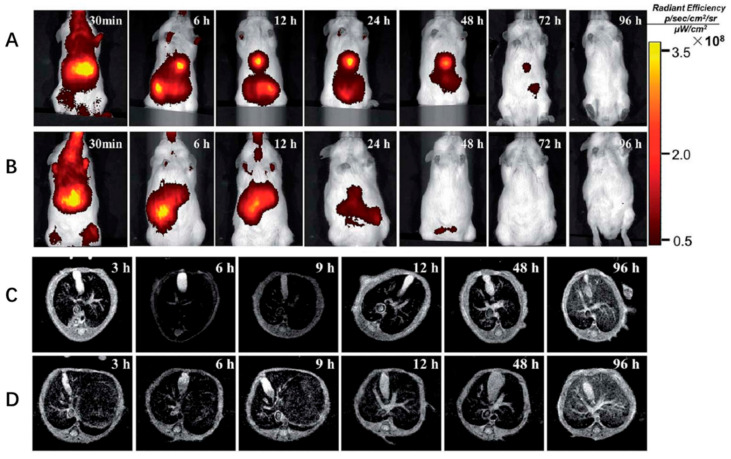
For liver diseases, early detection of liver fibrosis would be helpful for treatment. Unfortunately, most cases of liver disease are diagnosed late because of no symptoms. Current strategies for the diagnosis of liver fibrosis rely on an invasive biopsy which would cause damage for the patients [53]. Recently, magnetic resonance imaging (MRI) has been developed as a method with high diagnostic accuracy for the detection of fibrosis [54]. Magnetic NPs play an important role in the diagnosis and imaging of liver fibrosis [55]. For example, dextran stabilized superparamagnetic iron oxide NPs (D-SPIONs) with high blood compatibility and low cytotoxicity was used as an MRI contrast agent for liver fibrosis detection [56]. D-SPIONs enhanced image contrast of tissue and led to a 55% decrease in the pixel intensity, and therefore improved the contrast difference between the fibrotic tissue and the rest of the extracellular matrix rich hepatic parenchyma at the fibrosis stage significantly. Citrate-coated ultrasmall iron oxide NPs were also shown to provide a good MRI of liver fibrosis [57]. In one study, Fe3O4 NPs coated with SiO2 and then coupled with indocyanine green (ICG) and arginine–glycine–aspartic acid (SPIO@SiO2–ICG–RGD) were constructed for HSC targeting and early detection of liver fibrosis (Figure 2) [18]. Fe3O4 NPs and ICG as the photographic developers for T2 MRI and near-infrared (NIR) imaging, respectively. NIR fluorescence (NIR) and MRI revealed that SPIO@SiO2–ICG–RGD could elicit accurate identification of fibrotic regions in the liver. These NIR hybrid NPs combined imaging and MRI and provided higher sensitivity and spatial resolution for liver fibrosis detection, compared with MRI alone.
Figure 2.
In vivo optical imaging and MRI of liver fibrosis using SPIO@SiO2–ICG–RGD. (A,C) A model of hepatic fibrosis in mice. (B,D) Healthy mouse model (control). Adapted with permission from [18]. Copyright RSC publishing, 2018.
Furthermore, zero-valent iron (ZVI)-based NPs were also fabricated as novel contrast agents for MRI. After functionalized with liver specific polysaccharide pullulan and fluorescent carbon dots, a dual imaging contrast agent (P@ZVI-Cdts) was obtained. The efficiency of the developed systems for targeted liver imaging and optical imaging has been successfully demonstrated in vivo. The high r1 relaxivity enables ZVI NPs to be a competent T1 MRI contrast agent for various clinical applications including diagnosis of liver fibrosis [58].
In addition to MRI, the combination of an ultrasound agent with a targeting peptide has been reported for the early and non-invasive diagnosis of liver fibrosis. One study found that core–shell perfluorooctyl bromide (PFOB) coated with poly(lactic-co-glycolic acid) (PLGA) polymers and modified with a cyclic RGD (cRGD–PLGA–PFOB NPs) exhibited powerful ultrasound molecular imaging features, including high-contrast imaging among liver fibrotic stages and adjacent tissues [59].
4. Nanomedicine for Liver Fibrosis Therapy
4.1. NPs as Therapeutic Agents
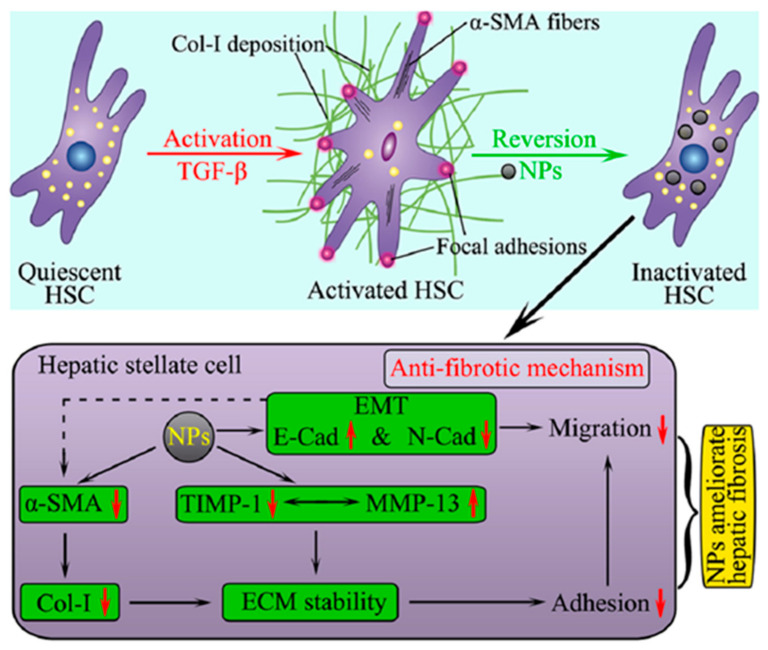
Owing to their distinctive bioactive properties, inorganic NPs alone can be used as therapeutic agents for liver fibrosis therapy [60,61,62]. Both titanium dioxide NPs (TiO2 NPs) and silicon dioxide NPs (SiO2 NPs) can inhibit the expression of collagen I and α-SMA. They also facilitate collagen I degradation by upregulating matrix metalloproteinases (MMPs) and downregulating tissue inhibitors of metalloproteinases (TIMPs), indicating the potential antifibrotic activities of TiO2 NPs and SiO2 NPs in vitro [63]. These NPs further exhibit anti-adhesive and anti-migratory effects by regulating epithelial−mesenchymal transition (EMT) gene expression and revert TGF-β-activated HSCs to a quiescent state (Figure 3). Owing to their anti-inflammatory properties, cerium oxide NPs reduce liver steatosis, portal hypertension, and liver fibrosis in rats [64]. Oral exposure of citrate-functionalized Mn3O4 NPs can protect the liver from carbon tetrachloride (CCl4)-induced cirrhosis, fibrosis, and oxidative stress because of the increased antioxidant properties of Mn3O4 NPs upon acid treatment in the stomach [65]. ZnO NPs also ameliorate liver fibrosis by reducing lipid peroxidation, oxidative stress, and inflammation in dimethylnitrosamine-induced liver damage [66].
Figure 3.
Model for TiO2 NPs and SiO2 NPs ameliorated fibrosis, adhesion and migration of HSCs. TiO2 NPs and SiO2 NPs can suppress the expression of α-SMA and deposition of Col-I induced by TGF-β. ECM was degraded by upregulating MMP-13 and downregulating TIMP-1. Therefore, adhesion of LX-2 cells was reduced. Furthermore, NPs stimulated the expression of E-Cad and reduced the expression of N-Cad, and, therefore, aggravated the migratory phenotype. Reproduced with permission from [63]. Copyright American Chemical Society, 2018.
In addition to metal oxide NPs, other types of inorganic NPs are also used to treat liver fibrosis. A study found that gold NPs reduced liver fibrosis in a rat model of ethanol- and methamphetamine-induced liver injury by inhibiting the activity of Kupffer cells and HSCs [67]. The mechanism involves the regulation of AKT/PI3K and MAPK signaling pathways by gold NPs, thereby reducing pro-inflammatory cytokine secretion and oxidative stress. Another study reported that vitamin E-modified selenium NPs can attenuate liver fibrosis by reducing oxidative stress [68].
4.2. NPs as Drug Carriers without Targeting Ligand for the Treatment of Liver Fibrosis
The liver is the main metabolic and excretory organ in the body in which NPs can accumulate and accomplish passive targeting because of their size. Thus, NPs have been widely used as drug carriers for the treatment of liver fibrosis. Lipid-based NPs have been recognized as the most powerful vehicles because of their good biocompatibility and low toxicity (Table 1) [69]. CCAAT/enhancer-binding protein alpha (CEBPA), a master transcriptional factor in the liver, resets the natural gene regulatory mechanism of hepatocytes to reduce fibrosis and reverse liver dysfunction. Small activating RNA oligonucleotide therapy (CEBPA-51) formulated in liposome NPs can upregulate CEBPA, thereby reducing fibrosis [70]. After Cur-mNLCs treatment, pro-inflammatory cytokines, collagen fibers and α-SMA were reduced, while hepatocyte growth factors (HGF) and MMP2 were increased. Cationic lipid NPs loaded with small interfering RNA to the procollagen α1(I) gene (LNP-siCol1α1) can be retained in the liver of fibrotic mice and accumulate in nonparenchymal liver cells, specifically blocking procollagen α1(I) expression and inhibiting liver fibrosis progression without noticeable side effects [20].
Table 1.
NPs as drug carriers without targeting ligands in liver fibrosis treatment.
| Nanoparticle Systems | NPs Formulation | Delivered Drug | Reference |
|---|---|---|---|
| Lipid-based NPs | RNA oligonucleotide-liposomal | MTL-CEBPA | [70] |
| Cationic lipid NPs | small interfering RNA to the procollagen 1(I) gene | [20] | |
| Dexamethasone-liposomes | dexamethasone | [71] | |
| Polymer-based NPs | Cationic nanohydrogel particles | anti-Col1α1 siRNA | [72] |
| Ketal cross-linked cationic nanohydrogel | Cy5-labeled anti-col1α1 siRNA | [73] | |
| PLGA | phyllanthin | [74] | |
| PEG-PLGA or PEG-PLGA/PLGA NPs | sorafenib | [75] | |
| Eudragit(R) RS100 NPs (SMnps) | silymarin | [76] | |
| Inorganic NPs | Rhodamine B (RhB)-mesoporous silica NPs (MSNs-RhB | salvianolic acid B | [77] |
| Mesoporous silica NPs | siTnC | [78] | |
| PEG-AuNPs | hesperetin | [79] | |
| AuNPs and SiNPs | NO donors | [80] | |
| PtNPs | Curcumin | [81] | |
| Calcium phosphate NPs (CaP@BSA NPs) | TSG-6 | [82] | |
| Graphene nanostars linked to PAMAM-GS dendrimer | Plasmid | [83] | |
| Protein NPs | Zein nanospheres | Curcumin | [84] |
| Glucose modify albumin NPs | Berberine | [85] | |
| Albumin NPs | Bexamethasone | [22] | |
| Polyavidin-based NPs | Dexamethasone | [86] |
Polymer-based NPs have been fabricated as drug carriers for the treatment of liver fibrosis (Table 1). In one study, ketal cross-linked cationic nanohydrogel particles were synthesized to deliver Cy5-labeled anti-col1α1 siRNA, which enhanced carrier and payload accumulation in the fibrotic tissue and prevented fibrosis progression [73]. PLGA and eudragit have also been employed as drug carriers. In one study, phyllanthin was carried by PLGA to reduce liver marker enzymes, namely alanine aminotransferase and aspartate aminotransferase, as well as collagen [74]. In another study, silymarin was delivered by eudragit NPs for the treatment of liver fibrosis by decreasing the expression of TNF-α, TGF-β1, TIMP-1, and CK-19. Moreover, nanoformulations were also found to increase HGF and MMP-2 expression and the MMP-2/TIMP-1 ratio [76].
In addition, inorganic NPs such as silica-based NPs were prepared as drug carriers because of their porous structures (Table 1). Salvianolic acid B (SAB) loaded rhodamine B covalently grafted mesoporous silica NPs (SAB@MSNs-RhB) were prepared for liver fibrosis therapy through the [77]. The SAB@MSNs-RhB formulation exhibited improved cellular uptake, sustained drug release, and enhanced efficacy in anti-ROS/hepatic fibrosis. Small interfering tenascin-C was delivered by mesoporous silica NPs to reduce the expression of TnC, an ECM glycoprotein, consequently reducing the secretion of inflammatory cytokines and hepatocyte migration [78]. Compared with hesperetin alone, hesperetin loaded on PEGylated gold NPs showed higher antioxidative, anti-inflammatory, anti-proliferative, and anti-fibrotic activities in diethylnitrosamine-induced hepatocarcinogenesis in rats [79]. Graphene nanostars conjugated with a PAMAM-G5 dendrimer were prepared for the selective targeting and delivery of a plasmid expressing collagenase metalloproteinase 9 under the CD11b promoter into inflammatory macrophages in cirrhotic livers. The nanoformulations promoted the macrophage switch from inflammatory M1 to proregenerative M2 and reduced selectively and locally the presence of collagen fibers in fibrotic tracts [83].
Protein-based NPs currently show great potential as drug carriers for the treatment of liver fibrosis because of their biocompatibility and low immunogenicity (Table 1) [87]. Algandaby et al. reported that curcumin-loaded zein nanospheres showed high efficiency in attenuating the hepatic gene expression of collagen I, the tissue inhibitor of MMP2, and TGF-β, as well as downregulating MMP2 expression [84]. Moreover, compared with free berberine, berberine entrapped in glucose-modified albumin NPs more efficiently inhibited the growth of the human hepatic stellate cell line LX-2 and reduced liver fibrosis in vivo [85]. Human serum albumin-dexamethasone NPs were also fabricated to deliver dexamethasone to non-parenchymal hepatic cells, which play an important role in the pathogenesis of liver fibrosis. This treatment efficiently inhibited TNF-α production, hence the significant decrease in fibrosis relative to that in rats treated with free dexamethasone treatment [22]. Another study reported on the preparation of avidin-nucleic-acid-nano-assemblies (ANANAS), which are NPs based on polyavidin. These NPs were generated from a nucleic acid filament and avidin, a protein in egg whites. These NPs were designed to selectively deliver dexamethasone to the liver, particularly to the liver immunocompetent cells, and thereby improve the therapeutic efficacy by reducing interlobular collagen I deposition and MMP13 [86].
4.3. NPs as Drug Carriers with Targeting Ligands for the Treatment of Liver Fibrosis
Non-specific drug disposition limits the effective clinical use of traditional anti-fibrotic drugs. Targeting drug delivery to the fibrotic region can thus far be achieved using nanoformulations. As the sole hepatic VA storage cells with a crucial role in liver fibrosis, HSCs have been actively targeted by conjugating NPs with VA.
Liposomes loaded with drugs and HSC targeting components have been developed to target HSCs for the treatment of liver fibrosis (Table 2). In one study, VA-coupled liposomes were prepared to deliver imatinib. The hepatic accumulation of imatinib increased by about 13.5-fold, compared with imatinib treatment alone [88]. The nanoformulations not only inhibited the expression of phosphorylated PDGFR-β but also reduced the expression of profibrotic mediators such as hydroxyproline, TGF-β, and MMP2 with fewer adverse effects. In another study, VA-coupled liposomes were used to deliver valsartan, an angiotensin II receptor antagonist [89]. The nanoformulations increased the expression of hepatic Mas-receptor and PPAR-γ and potently normalized the level of fibrogenic mediators by improving the permeability and efficacy of valsartan.
Table 2.
NPs used in active targeting therapy of liver fibrosis.
| Nanoparticle Systems | NPs Formulation | Delivered Drugs | Targeted Ligand | Targeted Structures | Reference |
|---|---|---|---|---|---|
| Lipid-based NPs | VA-liposomes | Imatinib | VA | HSC | [88] |
| VA-liposomes | Valsartan | VA | HSC | [89] | |
| pPB-modified liposomes | Recombinant human TRAIL | pPB | HSC | [90] | |
| AMD3100-liposomes | Antiangiogenic siRNA | VEGF siRNAs | HSC | [91] | |
| M6P-bovine serum albumin (BSA)-conjugated-liposomes | Hesperidin | M6P | HSC | [92] | |
| VA-coupled liposomes | BMP4-siRNA | VA | HSC | [93] | |
| Cationic liposomes | Artificial microRNA | microRNA | CTGF | [94] | |
| Chol-PEG-VA-amphiphilic cationic hyperbranched lipoid (C15-PA) | SiCol I α1 and siTIMP-1 | VA | HSC | [95] | |
| pPB-modified stable nucleic acid lipid | siRNAs against heat shock protein 47 | pPB | HSC | [96] | |
| Galactosamine-phospholipid NPs | siRNA targets CTGF | galactosamine | hepatocytes and renal tubular epithelial cells | [97] | |
| SP94-LCPP (lipid/calcium/phosphate/protamine) nanoparticle | TRAIL plasmid DNA | hepato-cellular carcinoma (HCC)-targeting peptide (SP94) | hepatocellular carcinoma (HCC) cells | [98] | |
| Phosphatidylserine-modified nanostructured lipid NPs | Curcumin | phosphatidylserine | macrophage | [99] | |
| Polymer-based NPs | VA-collagenase I-poly-(lactic-co-glycolic)-b-poly (ethylene glycol)-maleimide (PLGA-PEG-Mal) (named CRM) micelle | Nilotinib | VA | HSC | [100] |
| Poly (lactide-co-glycolide)-polyspermine-poly (ethylene glycol)-vitamin A (PLGA-PSPE-PEG-VA) self-assembled into core-shell polymeric micelles (PVMs) | Silibinin genetic (siCol1 alpha 1) drugs | VA | HSC | [101] | |
| Retinoic acid-chondroitin sulfate micells | Doxorubicin | VA | HSC | [102] | |
| POEGMA-b-PVDM -VA micelle | NO | VA | HSC | [19] | |
| Retinol-conjugated polyetherimine (RcP) nanoparticle | Antisense oligonucleotide (ASO) | RcP | HSC | [103] | |
| PLGA NPs | R406 | R406 | Macrophages | [104] | |
| retinol-chitosan NPs | JQ1 and atorvastatin | VA | HSC | [105] | |
| Inorganic NPs | pPB-MSNP | Erlotinib | pPB | PDGFRB | [106] |
Abbreviations: VA, vitamin A; TRAIL, TNF-related apoptosis-inducing ligand; HSC, hepatic stellate cell; CTGF, connective tissue growth factor; MMP, matrix metalloproteinase; NO, nitric oxide; VEGF, vascular endothelial growth factor.
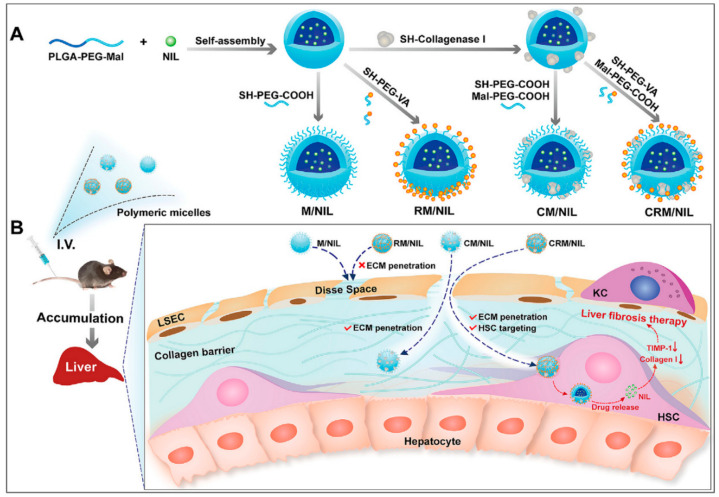
Polymer-based NPs have also been fabricated to target HSCs by coupling with VA for liver fibrosis therapy (Table 2). An article reported on the preparation of retinol and collagenase I co-decorated polymeric micelles (CRM) based on PLGA-b-poly(ethylene glycol)-maleimide (PLGA-PEG-Mal) to be used as HSC-targeting nanodrug delivery systems for liver fibrosis therapy [100]. In the current study, the decoration of collagenase I could facilitate the nanocarrier penetration of the fibrotic liver. Consistent with this finding, CRMs were found to efficiently degrade pericellular collagen I and exhibit excellent accumulation in the fibrotic liver and accurate targeting of activated HSCs in a mouse hepatic fibrosis model. CRM/NIL loaded with nilotinib (NIL), a second-generation tyrosine kinase inhibitor used for the treatment of liver fibrosis, showed excellent antifibrotic efficiency (Figure 4). In addition, polymeric micelles (PVMs) formed with PLGA-polyspermine-PEG-VA were used to target HSCs and deliver the chemical drug silibinin and genetic drug siCol1α1 to the liver fibrosis site [101]. The double-loaded polymer micelle more efficiently reduced collagen I and ameliorated liver fibrosis, compared with the PVMS loaded with either the chemical drug only or genetic drug only. Chondroitin sulfate micelles coupled with retinoic acid and doxorubicin (DOX) (DOX + RA–CS micelles) were selectively taken up in activated HSCs and hepatoma cells, but not in normal hepatocytes (LO2) [102]. DOX + RA–CS micelles preferentially accumulated in the Golgi apparatus, destroyed the Golgi structure, and ultimately downregulated collagen I production in vitro and exerted synergistic antifibrotic effects on CCl4-induced fibrotic rat models.
Figure 4.
Extracellular matrix-penetrating polymeric micelles for liver fibrosis therapy. (A) Schematic illustration of the preparation of four different polymeric micelles. (B) Schematic illustration of the proposed destiny of the four different polymeric micelles in vivo. The CRM/NIL is able to penetrate the collagen barrier and target activated HSCs. Internalization of CRM/NIL allows the release of NIL, which reduces expression of the metallopeptidase inhibitor, TIMP-1, which in turn enhances collagen I degradation, thereby exerting therapeutic action against liver fibrosis. Reproduced with permission from [100]. Copyright Elsevier, 2020.
Apart from polymeric micelles, other polymer nanoformulations have also been constructed for the delivery of drugs, nucleic acid and other therapeutic moieties for the treatment of liver fibrosis (Table 2). In one study, retinol-conjugated polyetherimine NPs adsorbed plasma proteins, particularly retinol-binding protein 4 (RBP), forming a protein-coated complex [103]. The adsorbed RBP could direct the NPs into HSCs. After being loaded with antisense oligonucleotides, NPs effectively suppressed the expression of collagen I, consequently ameliorating hepatic fibrosis. Hassan et al. reported that chitosan NPs loaded with JQ1 (a small molecule that could abrogate the cytokine-induced activation of HSCs and reverse fibrotic response in animal models) and atorvastatin and further conjugated with retinol could target and prevent HSC activation [105].
In addition to VA, cyclic peptide pPB can particularly recognize PDGFRβ on the surface of HSCs (Table 2). A study used pPB-modified liposomes to deliver recombinant human tumor necrosis factor-related apoptosis-inducing ligand (rhTRAIL) to the HSC membrane, prolonging rhTRAIL circulation in vivo and alleviating fibrosis both in vitro and in vivo [90]. Similarly, the CXCR4 antagonist AMD3100 could target HSCs [91]. AMD3100-conjugated liposomes efficiently delivered therapeutic VEGF siRNAs to activate CXCR4-overexpressed HSCs both in vitro and in vivo. The nanoformulations downregulated the expression of VEGF, reduced the mean vessel density, and normalized the hepatic vascular structure in the livers of mice with CCl4-induced liver fibrosis. Moreover, AMD3100 encapsulated in liposomes also exhibited antifibrotic effects by suppressing the proliferation and activation of HSCs. Mannose 6-phosphate (M6P)/insulin-like growth factor-II receptor, overexpressed in HSCs, was also used as the targeting site. Conjugation of M6P-modified albumin to hesperidin-loaded liposomes improved the efficacy of chemical drugs and attenuated liver fibrosis [92].
Hepatic macrophages play important roles in the pathogenesis of liver fibrosis and act as target sites for the treatment of liver fibrosis (Table 2). Scavenger receptors expressed on liver endothelial cells and Kupffer cells have also been targeted using nanoformulations. For instance, phosphatidylserine (PS), which acts as a specific recognition signal for the phagocytosis of apoptotic cells, can target macrophages. Wang et al. showed that PS-modified lipid carriers containing curcumin (Cur–mNLCs) exhibited enhanced retention time, bioavailability, and delivery efficiency of payload, as well as reduced liver damage and fibrosis in vivo [99].
5. Nanomedicine in Liver Fibrosis Theranostics
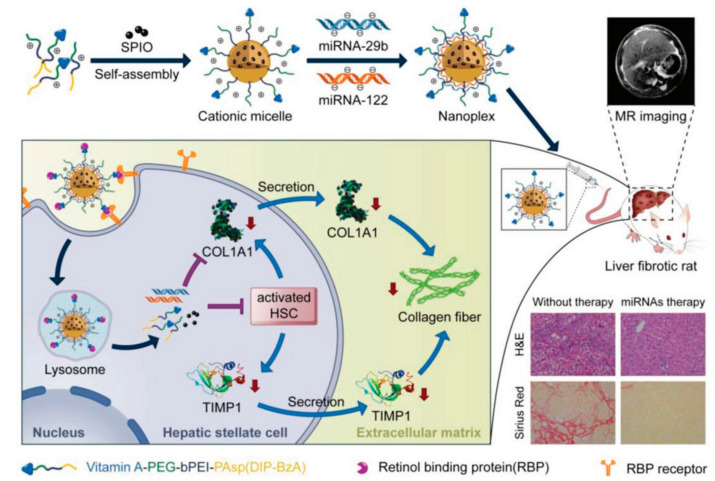
“Theranostics”, a portmanteau word of “therapeutics” and “diagnostics”, is achieved by incorporating diagnostic and therapeutic functions into a single nanoplatform. Theranostics has been proposed as a new and revolutionary therapeutic concept in several types of disease therapy, including that for liver fibrosis [107]. This strategy allows simultaneous diagnosis and treatment response by using personalized medicine with high accuracy and specificity. In one study, Hepatitis B core protein nanocages coated with RGD-targeting ligands (RGD–HBc/QR) exhibited selectivity to activated HSCs by targeting integrin αvβ3 and efficiently inhibited the proliferation and activation of HSCs both in vitro and in vivo [108]. By encapsulating a quercetin–gadolinium complex and/or labeling it with NIR fluorescent probes (Cy5.5), the resulted nanoformulations (RGD–HBc/QGd) showed great potential as MRI contrast agents and NIR fluorescent agents for liver fibrosis diagnosis in vivo. Another study reported that relaxin-conjugated PEGylated superparamagnetic iron oxide NPs (RLX-SPIONs) showed specific binding and uptake in TGFβ-activated HSCs, as well as strongly attenuated cirrhosis and showed enhanced contrast in MRI [20]. Micelles coupled with inorganic materials were also developed for theranostics to treat liver fibrosis. A pH-sensitive and VA-conjugated copolymer cationic micelle that was coupled with a superparamagnetic iron oxide nanoparticle could transport miRNA-29b and miRNA-112 to HSCs in an MRI-visible manner. Synergistic antifibrotic therapeutic efficacy was achieved by downregulating the expression of fibrosis-related genes, including collagen Iα1, α-SMA, and a tissue inhibitor of MMP1 (Figure 5) [109].
Figure 5.
Vitamin A–decorated pH-sensitive and SPIO-loaded nanocomplex T-PBP@miRNA/SPIO (T-miRNA/S) for miRNA targeting delivery in the therapy of liver fibrosis. Expression of liver fibrosis-related genes for alleviating liver fibrosis were synergistically downregulated. The red arrows indicate the reduction of COL1A1, TIMP1, and collagen fiber. Abbreviations: COL1A1, collagen type I alpha 1 protein; TIMP1, tissue inhibitor of metalloproteinase 1; SPIO, superparamagnetic iron oxide. Reproduced with permission from [109]. Copyright John Wiley and Sons, 2019.
6. Conclusions and Future Perspectives
This review summarizes the strategies being used to develop novel methods for the treatment of liver fibrosis on the basis of multifunctional NPs. The application of nanomedicine systems in the diagnosis and treatment of liver fibrosis is widely reported in the literature and continues to be a rapidly growing research field, with emphasis on active targeted drug delivery and theranostics. Numerous types of inorganic and organic NPs have been extensively investigated, including metal oxide NPs, metal NPs, liposomes, polymer NPs, dendrimers, protein NPs, and organic–inorganic hybrid NPs. Each type has its advantages disadvantages. Inorganic NPs are intrinsically robust with relatively low manufacturing costs, but their design flexibility and functionality are limited. Organic NPs possess broad design flexibility for integrating multiple functions into one platform but show structural instability and involve high manufacturing cost and fabrication complexity. Organic–inorganic hybrid NPs combine the advantages of organic NPs and inorganic NPs and thus are preferred in the development of theranostic platforms.
Although NPs have shown great potential for liver fibrosis therapy, they also exhibit hepatotoxicity [110,111,112,113,114]. The long-term hepatotoxicity of NPs should be carefully and systemically evaluated, particularly when they are used in patients with liver disease. Patients are more sensitive to NPs because of reduced self-protective mechanisms, decreased immune function, and lack of ability for self-repair. Studies have shown that exposure to NPs increases pathological damage [115,116,117]. Therefore, the health risks involved in the use of NPs for liver fibrosis therapy should be given significant attention.
Until now, lipid-based NPs were the only nanomedicine system that in the clinical stages of studies for the treatment of liver fibrosis. Lipid NPs delivering siRNA against heat shock protein 47 were developed to target HSCs and treat advanced liver fibrosis caused by NASH or hepatitis C virus infection. This nanomedicine system was in clinical phase 1b/2 and study results were safe and effective [118,119]. To improve the clinical applicability of nanomedicine systems in the future, the following directions should be considered: (1) Developing stimuli-responsive nanomedicine systems with high sensitivity, which can intelligently respond to endogenous or exogenous stimuli and release payload at targeting sites. (2) Employing an “all-in-one” strategy to develop smart nanomedicine systems that combine multiple functionalities, including targeted delivery, prolonged blood retention, enhanced tissue penetration and cellular internalization, responsiveness to stimuli, and disease progressive monitoring. (3) Systematic evaluation of long-term toxicity, immunogenicity, and pharmacokinetics of medicine systems. Notably, from the clinical use of the reported nanomedicine systems, only one example was performed. All obstacles should be overcome by designing and fabricating nanomedicine systems with appropriate components, surface chemistry, sizes, payloads, and specific target ligands before clinical translation.
Acknowledgments
This research was funded by the National Natural Science Foundation of China (21677090, 22076085).
Author Contributions
X.B., G.S. and S.Z. designed this work of review. X.B. and G.S. performed the literature search of the databases. X.B. and G.S. wrote the manuscript. G.S. and S.Z. revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Lee Y.A., Wallace M.C., Friedman S.L. Pathobiology of liver fibrosis: A translational success story. Gut. 2015;64:830–841. doi: 10.1136/gutjnl-2014-306842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baffy G., Brunt E.M., Caldwell S.H. Hepatocellular carcinoma in non-alcoholic fatty liver disease: An emerging menace. J. Hepatol. 2012;56:1384–1391. doi: 10.1016/j.jhep.2011.10.027. [DOI] [PubMed] [Google Scholar]
- 3.Mieli-Vergani G., Vergani D., Czaja A.J., Manns M.P., Krawitt E.L., Vierling J.M., Lohse A.W., Montano-Loza A.J. Autoimmune hepatitis. Nat. Rev. Dis. Primers. 2018;4:18017. doi: 10.1038/nrdp.2018.17. [DOI] [PubMed] [Google Scholar]
- 4.Sarin S.K., Kumar M., Eslam M., George J., Al Mahtab M., Akbar S.M.F., Jia J., Tian Q., Aggarwal R., Muljono D.H., et al. Liver diseases in the Asia-Pacific region: A Lancet Gastroenterology & Hepatology Commission. Lancet Gastroenterol. Hepatol. 2020;5:167–228. doi: 10.1016/S2468-1253(19)30342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trautwein C., Friedman S.L., Schuppan D., Pinzani M. Hepatic fibrosis: Concept to treatment. J. Hepatol. 2015;62:S15–S24. doi: 10.1016/j.jhep.2015.02.039. [DOI] [PubMed] [Google Scholar]
- 6.Zhang D.Y., Friedman S.L. Fibrosis-dependent mechanisms of hepatocarcinogenesis. Hepatology. 2012;56:769–775. doi: 10.1002/hep.25670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manning D.S., Afdhal N.H. Diagnosis and Quantitation of Fibrosis. Gastroenterology. 2008;134:1670–1681. doi: 10.1053/j.gastro.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 8.De Oliveira C.P.M.S., Stefano J.T., De Siqueira E.R.F., Silva L.S., De Campos Mazo D.F., Lima V.M.R., Furuya C.K., Mello E.S., Souza F.G., Rabello F., et al. Combination of N-acetylcysteine and metformin improves histological steatosis and fibrosis in patients with non-alcoholic steatohepatitis. Hepatol. Res. 2008;38:159–165. doi: 10.1111/j.1872-034X.2007.00215.x. [DOI] [PubMed] [Google Scholar]
- 9.Peres W., Tuñón M.J., Collado P.S., Herrmann S., Marroni N., González-Gallego J. The flavonoid quercetin ameliorates liver damage in rats with biliary obstruction. J. Hepatol. 2000;33:742–750. doi: 10.1016/S0168-8278(00)80305-0. [DOI] [PubMed] [Google Scholar]
- 10.Ogawa S., Ochi T., Shimada H., Inagaki K., Fujita I., Nii A., Moffat M.A., Katragadda M., Violand B.N., Arch R.H., et al. Anti-PDGF-B monoclonal antibody reduces liver fibrosis development. Hepatol. Res. 2010;40:1128–1141. doi: 10.1111/j.1872-034X.2010.00718.x. [DOI] [PubMed] [Google Scholar]
- 11.Schuppan D., Kim Y.O. Evolving therapies for liver fibrosis. J. Clin. Investig. 2013;123:1887–1901. doi: 10.1172/JCI66028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Silva C., Pinho J., Lopes J.M., Almeida A.J., Reis C.P. Current Trends in Cancer Nanotheranostics: Metallic, Polymeric, and Lipid-Based Systems. Pharmaceutics. 2019;11:22. doi: 10.3390/pharmaceutics11010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pucek A., Tokarek B., Waglewska E., Bazylińska U. Recent Advances in the Structural Design of Photosensitive Agent Formulations Using “Soft” Colloidal Nanocarriers. Pharmaceutics. 2020;12:587. doi: 10.3390/pharmaceutics12060587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wawrzyńczyk D., Cichy B., Zaręba J.K., Bazylińska U. On the interaction between up-converting NaYF4:Er3+,Yb3+ nanoparticles and Rose Bengal molecules constrained within the double core of multifunctional nanocarriers. J. Mater. Chem. C. 2019;7:15021–15034. doi: 10.1039/C9TC04163J. [DOI] [Google Scholar]
- 15.Doane T.L., Burda C. The unique role of nanoparticles in nanomedicine: Imaging, drug delivery and therapy. Chem. Soc. Rev. 2012;41:2885–2911. doi: 10.1039/c2cs15260f. [DOI] [PubMed] [Google Scholar]
- 16.Surendran S.P., Thomas R.G., Moon M.J., Jeong Y.Y. Nanoparticles for the treatment of liver fibrosis. Int. J. Nanomed. 2017;12:6997–7006. doi: 10.2147/IJN.S145951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reddy L.H., Couvreur P. Nanotechnology for therapy and imaging of liver diseases. J. Hepatol. 2011;55:1461–1466. doi: 10.1016/j.jhep.2011.05.039. [DOI] [PubMed] [Google Scholar]
- 18.Li Y., Shang W., Liang X., Zeng C., Liu M., Wang S., Li H., Tian J. The diagnosis of hepatic fibrosis by magnetic resonance and near-infrared imaging using dual-modality nanoparticles. RSC Adv. 2018;8:6699–6708. doi: 10.1039/C7RA10847H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duong H.T., Dong Z., Su L., Boyer C., George J., Davis T.P., Wang J. The use of nanoparticles to deliver nitric oxide to hepatic stellate cells for treating liver fibrosis and portal hypertension. Small Weinh. Der Bergstr. Ger. 2015;11:2291–2304. doi: 10.1002/smll.201402870. [DOI] [PubMed] [Google Scholar]
- 20.Calvente C.J., Sehgal A., Popov Y., Kim Y.O., Zevallos V., Sahin U., Diken M., Schuppan D. Specific hepatic delivery of procollagen α1(I) small interfering RNA in lipid-like nanoparticles resolves liver fibrosis. Hepatology. 2015;62:1285–1297. doi: 10.1002/hep.27936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li L., Wang H., Ong Z.Y., Xu K., Ee P.L.R., Zheng S., Hedrick J.L., Yang Y.-Y. Polymer- and lipid-based nanoparticle therapeutics for the treatment of liver diseases. Nano Today. 2010;5:296–312. doi: 10.1016/j.nantod.2010.06.007. [DOI] [Google Scholar]
- 22.Melgert B.N., Olinga P., Jack V.K., Molema G., Meijer D.K.F., Poelstra K. Dexamethasone coupled to albumin is selectively taken up by rat nonparenchymal liver cells and attenuates LPS-induced activation of hepatic cells. J. Hepatol. 2000;32:603–611. doi: 10.1016/S0168-8278(00)80222-6. [DOI] [PubMed] [Google Scholar]
- 23.Petros R.A., DeSimone J.M. Strategies in the design of nanoparticles for therapeutic applications. Nat. Rev. Drug Discov. 2010;9:615–627. doi: 10.1038/nrd2591. [DOI] [PubMed] [Google Scholar]
- 24.Nagórniewicz B., Mardhian D.F., Booijink R., Storm G., Prakash J., Bansal R. Engineered Relaxin as Theranostic nanomedicine to diagnose and ameliorate liver cirrhosis. Nanomed. Nanotechnol. Biol. Med. 2019;17:106–118. doi: 10.1016/j.nano.2018.12.008. [DOI] [PubMed] [Google Scholar]
- 25.Yin C., Evason K.J., Asahina K., Stainier D.Y.R. Hepatic stellate cells in liver development, regeneration, and cancer. J. Clin. Investig. 2013;123:1902–1910. doi: 10.1172/JCI66369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hernandez-Gea V., Friedman S.L. Pathogenesis of Liver Fibrosis. Annu. Rev. Pathol. Mech. Dis. 2011;6:425–456. doi: 10.1146/annurev-pathol-011110-130246. [DOI] [PubMed] [Google Scholar]
- 27.Tsuchida T., Friedman S.L. Mechanisms of hepatic stellate cell activation. Nat. Rev. Gastroenterol. Hepatol. 2017;14:397–411. doi: 10.1038/nrgastro.2017.38. [DOI] [PubMed] [Google Scholar]
- 28.Meng X.-M., Nikolic-Paterson D.J., Lan H.Y. TGF-β: The master regulator of fibrosis. Nat. Rev. Nephrol. 2016;12:325–338. doi: 10.1038/nrneph.2016.48. [DOI] [PubMed] [Google Scholar]
- 29.Kocabayoglu P., Lade A., Lee Y.A., Dragomir A.-C., Sun X., Fiel M.I., Thung S., Aloman C., Soriano P., Hoshida Y., et al. β-PDGF receptor expressed by hepatic stellate cells regulates fibrosis in murine liver injury, but not carcinogenesis. J. Hepatol. 2015;63:141–147. doi: 10.1016/j.jhep.2015.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Okuno M., Moriwaki H., Muto Y., Kojima S. Protease inhibitors suppress TGF-β generation by hepatic stellate cells. J. Hepatol. 1998;29:1031–1032. doi: 10.1016/S0168-8278(98)80136-0. [DOI] [PubMed] [Google Scholar]
- 31.Wang Y., Gao J., Zhang D., Zhang J., Ma J., Jiang H. New insights into the antifibrotic effects of sorafenib on hepatic stellate cells and liver fibrosis. J. Hepatol. 2010;53:132–144. doi: 10.1016/j.jhep.2010.02.027. [DOI] [PubMed] [Google Scholar]
- 32.Wang Y.Q., Ikeda K., Ikebe T., Hirakawa K., Sowa M., Nakatani K., Kawada N., Kaneda K. Inhibition of hepatic stellate cell proliferation and activation by the semisynthetic analogue of fumagillin TNP-470 in rats. Hepatology. 2000;32:980–989. doi: 10.1053/jhep.2000.18658. [DOI] [PubMed] [Google Scholar]
- 33.Sugawara H., Ueno T., Torimura T., Inuzuka S., Tanikawa K. Inhibitory effect of OPC-15161, a component of fungus Thielavia minor, on proliferation and extracellular matrix production of rat cultured hepatic stellate cells. J. Cell. Physiol. 1998;174:398–406. doi: 10.1002/(SICI)1097-4652(199803)174:3<398::AID-JCP14>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 34.Morry J., Ngamcherdtrakul W., Yantasee W. Oxidative stress in cancer and fibrosis: Opportunity for therapeutic intervention with antioxidant compounds, enzymes, and nanoparticles. Redox Biol. 2017;11:240–253. doi: 10.1016/j.redox.2016.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hickman I., Macdonald G. Is vitamin E beneficial in chronic liver disease? Hepatology. 2007;46:288–290. doi: 10.1002/hep.21834. [DOI] [PubMed] [Google Scholar]
- 36.Sukalingam K., Ganesan K., Xu B. Protective Effect of Aqueous Extract from the Leaves of Justicia tranquebariesis against Thioacetamide-Induced Oxidative Stress and Hepatic Fibrosis in Rats. Antioxidants. 2018;7:78. doi: 10.3390/antiox7070078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Di Pascoli M., Diví M., Rodríguez-Vilarrupla A., Rosado E., Gracia-Sancho J., Vilaseca M., Bosch J., García-Pagán J.C. Resveratrol improves intrahepatic endothelial dysfunction and reduces hepatic fibrosis and portal pressure in cirrhotic rats. J. Hepatol. 2013;58:904–910. doi: 10.1016/j.jhep.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 38.Mezey E. Prevention of alcohol-induced hepatic fibrosis by phosphatidylcholine. Gastroenterology. 1994;106:257–259. doi: 10.1016/S0016-5085(94)96015-1. [DOI] [PubMed] [Google Scholar]
- 39.Hirano A., Kaplowitz N., Tsukamoto H., Kamimura S., Fernandez-Checa J.C. Hepatic mitochondrial glutathione depletion and progression of experimental alcoholic liver disease in rats. Hepatology. 1992;16:1423–1427. doi: 10.1002/hep.1840160619. [DOI] [PubMed] [Google Scholar]
- 40.Ankoma-Sey V., Wang Y., Dai Z. Hypoxic stimulation of vascular endothelial growth factor expression in activated rat hepatic stellate cells. Hepatology. 2000;31:141–148. doi: 10.1002/hep.510310122. [DOI] [PubMed] [Google Scholar]
- 41.Aleffi S., Petrai I., Bertolani C., Parola M., Colombatto S., Novo E., Vizzutti F., Anania F.A., Milani S., Rombouts K., et al. Upregulation of proinflammatory and proangiogenic cytokines by leptin in human hepatic stellate cells. Hepatology. 2005;42:1339–1348. doi: 10.1002/hep.20965. [DOI] [PubMed] [Google Scholar]
- 42.Fernández M., Semela D., Bruix J., Colle I., Pinzani M., Bosch J. Angiogenesis in liver disease. J. Hepatol. 2009;50:604–620. doi: 10.1016/j.jhep.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 43.Taura K., De Minicis S., Seki E., Hatano E., Iwaisako K., Osterreicher C.H., Kodama Y., Miura K., Ikai I., Uemoto S., et al. Hepatic Stellate Cells Secrete Angiopoietin 1 That Induces Angiogenesis in Liver Fibrosis. Gastroenterology. 2008;135:1729–1738. doi: 10.1053/j.gastro.2008.07.065. [DOI] [PubMed] [Google Scholar]
- 44.Moon J.-O., Welch T.P., Gonzalez F.J., Copple B.L. Reduced liver fibrosis in hypoxia-inducible factor-1α-deficient mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2009;296:G582–G592. doi: 10.1152/ajpgi.90368.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sánchez-Valle V., Chávez-Tapia N.C., Uribe M., Méndez-Sánchez N. Role of oxidative stress and molecular changes in liver fibrosis: A review. Curr. Med. Chem. 2012;19:4850–4860. doi: 10.2174/092986712803341520. [DOI] [PubMed] [Google Scholar]
- 46.Seki E., Schwabe R.F. Hepatic inflammation and fibrosis: Functional links and key pathways. Hepatology. 2015;61:1066–1079. doi: 10.1002/hep.27332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Anand L., Choudhury A., Bihari C., Sharma B.C., Kumar M., Maiwall R., Tan S.S., Shah S.R., Hamid S., Butt A.S., et al. Flare of Autoimmune Hepatitis Causing Acute on Chronic Liver Failure: Diagnosis and Response to Corticosteroid Therapy. Hepatology. 2019;70:587–596. doi: 10.1002/hep.30205. [DOI] [PubMed] [Google Scholar]
- 48.Morgan T.R., Weiss D.G., Nemchausky B., Schiff E.R., Anand B., Simon F., Kidao J., Cecil B., Mendenhall C.L., Nelson D., et al. Colchicine treatment of alcoholic cirrhosis: A randomized, placebo-controlled clinical trial of patient survival. Gastroenterology. 2005;128:882–890. doi: 10.1053/j.gastro.2005.01.057. [DOI] [PubMed] [Google Scholar]
- 49.Cheng K., Ashby D., Smyth R.L. Ursodeoxycholic acid for cystic fibrosis-related liver disease. Cochrane Database Syst. Rev. 2017;2017:CD000222. doi: 10.1002/14651858.CD000222.pub4. [DOI] [PubMed] [Google Scholar]
- 50.Nelson D.R., Lauwers G.Y., Lau J.Y.N., Davis G.L. Interleukin 10 treatment reduces fibrosis in patients with chronic hepatitis C: A pilot trial of interferon nonresponders. Gastroenterology. 2000;118:655–660. doi: 10.1016/S0016-5085(00)70134-X. [DOI] [PubMed] [Google Scholar]
- 51.Heide D.v.d., Weiskirchen R., Bansal R. Therapeutic Targeting of Hepatic Macrophages for the Treatment of Liver Diseases. Front. Immunol. 2019;10:2852. doi: 10.3389/fimmu.2019.02852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Van Bergen T., Spangler R., Marshall D., Hollanders K., Van de Veire S., Vandewalle E., Moons L., Herman J., Smith V., Stalmans I. The Role of LOX and LOXL2 in the Pathogenesis of an Experimental Model of Choroidal Neovascularization. Investig. Ophthalmol. Vis. Sci. 2015;56:5280–5289. doi: 10.1167/iovs.14-15513. [DOI] [PubMed] [Google Scholar]
- 53.Yoshio S., Atsushi N., Yoshito I. Limitations of liver biopsy and non-invasive diagnostic tests for the diagnosis of nonalcoholic fatty liver disease/ nonalcoholic steatohepatitis. World J. Gastroenterol. 2014;20:475–485. doi: 10.3748/wjg.v20.i2.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dulai P.S., Sirlin C.B., Loomba R. MRI and MRE for non-invasive quantitative assessment of hepatic steatosis and fibrosis in NAFLD and NASH: Clinical trials to clinical practice. J. Hepatol. 2016;65:1006–1016. doi: 10.1016/j.jhep.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sun C., Lee J.S.H., Zhang M. Magnetic nanoparticles in MR imaging and drug delivery. Adv. Drug Deliv. Rev. 2008;60:1252–1265. doi: 10.1016/j.addr.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Saraswathy A., Nazeer S.S., Nimi N., Arumugam S., Shenoy S.J., Jayasree R.S. Synthesis and characterization of dextran stabilized superparamagnetic iron oxide nanoparticles for in vivo MR imaging of liver fibrosis. Carbohydr. Polym. 2014;101:760–768. doi: 10.1016/j.carbpol.2013.10.015. [DOI] [PubMed] [Google Scholar]
- 57.Saraswathy A., Nazeer S.S., Jeevan M., Nimi N., Arumugam S., Harikrishnan V.S., Varma P.R., Jayasree R.S. Citrate coated iron oxide nanoparticles with enhanced relaxivity for in vivo magnetic resonance imaging of liver fibrosis. Colloids Surf. B Biointerfaces. 2014;117:216–224. doi: 10.1016/j.colsurfb.2014.02.034. [DOI] [PubMed] [Google Scholar]
- 58.Nimi N., Saraswathy A., Nazeer S.S., Francis N., Shenoy S.J., Jayasree R.S. Multifunctional hybrid nanoconstruct of zerovalent iron and carbon dots for Magnetic Resonance Angiography and Optical Imaging: An In vivo study. Biomaterials. 2018;171:46–56. doi: 10.1016/j.biomaterials.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 59.Xuan J., Chen Y., Zhu L., Guo Y., Ao M. Ultrasound molecular imaging with cRGD-PLGA-PFOB nanoparticles for liver fibrosis staging in a rat model. Oncotarget. 2017;8:108676–108691. doi: 10.18632/oncotarget.21358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Anselmo A.C., Mitragotri S. A Review of Clinical Translation of Inorganic Nanoparticles. AAPS J. 2015;17:1041–1054. doi: 10.1208/s12248-015-9780-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Xu Z.P., Zeng Q.H., Lu G.Q., Yu A.B. Inorganic nanoparticles as carriers for efficient cellular delivery. Chem. Eng. Sci. 2006;61:1027–1040. doi: 10.1016/j.ces.2005.06.019. [DOI] [Google Scholar]
- 62.Tee J.K., Peng F., Ho H.K. Effects of inorganic nanoparticles on liver fibrosis: Optimizing a double-edged sword for therapeutics. Biochem. Pharmacol. 2019;160:24–33. doi: 10.1016/j.bcp.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 63.Peng F., Tee J.K., Setyawati M.I., Ding X., Yeo H.L.A., Tan Y.L., Leong D.T., Ho H.K. Inorganic Nanomaterials as Highly Efficient Inhibitors of Cellular Hepatic Fibrosis. ACS Appl. Mater. Interfaces. 2018;10:31938–31946. doi: 10.1021/acsami.8b10527. [DOI] [PubMed] [Google Scholar]
- 64.Oró D., Yudina T., Fernández-Varo G., Casals E., Reichenbach V., Casals G., González de la Presa B., Sandalinas S., Carvajal S., Puntes V., et al. Cerium oxide nanoparticles reduce steatosis, portal hypertension and display anti-inflammatory properties in rats with liver fibrosis. J. Hepatol. 2016;64:691–698. doi: 10.1016/j.jhep.2015.10.020. [DOI] [PubMed] [Google Scholar]
- 65.Adhikari A., Polley N., Darbar S., Bagchi D., Pal S.K. Citrate functionalized Mn3O4 in nanotherapy of hepatic fibrosis by oral administration. Future Sci. OA. 2016;2:2056–5623. doi: 10.4155/fsoa-2016-0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rani V., Verma Y., Rana K., Rana S.V.S. Zinc oxide nanoparticles inhibit dimethylnitrosamine induced liver injury in rat. Chem. Biol. Interact. 2018;295:84–92. doi: 10.1016/j.cbi.2017.10.009. [DOI] [PubMed] [Google Scholar]
- 67.De Carvalho T.G., Garcia V.B., de Araújo A.A., da Silva Gasparotto L.H., Silva H., Guerra G.C.B., de Castro Miguel E., de Carvalho Leitão R.F., da Silva Costa D.V., Cruz L.J., et al. Spherical neutral gold nanoparticles improve anti-inflammatory response, oxidative stress and fibrosis in alcohol-methamphetamine-induced liver injury in rats. Int. J. Pharm. 2018;548:1–14. doi: 10.1016/j.ijpharm.2018.06.008. [DOI] [PubMed] [Google Scholar]
- 68.Hamza R.Z., EL-Megharbel S.M., Altalhi T., Gobouri A.A., Alrogi A.A. Hypolipidemic and hepatoprotective synergistic effects of selenium nanoparticles and vitamin. E against acrylamide-induced hepatic alterations in male albino mice. Appl. Organomet. Chem. 2020;34:e5458. doi: 10.1002/aoc.5458. [DOI] [Google Scholar]
- 69.Böttger R., Pauli G., Chao P.-H., Al Fayez N., Hohenwarter L., Li S.-D. Lipid-based nanoparticle technologies for liver targeting. Adv. Drug Deliv. Rev. 2020 doi: 10.1016/j.addr.2020.06.017. in press. [DOI] [PubMed] [Google Scholar]
- 70.Reebye V., Huang K.-W., Lin V., Jarvis S., Cutilas P., Dorman S., Ciriello S., Andrikakou P., Voutila J., Saetrom P., et al. Gene activation of CEBPA using saRNA: Preclinical studies of the first in human saRNA drug candidate for liver cancer. Oncogene. 2018;37:3216–3228. doi: 10.1038/s41388-018-0126-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bartneck M., Scheyda K.M., Warzecha K.T., Rizzo L.Y., Hittatiya K., Luedde T., Storm G., Trautwein C., Lammers T., Tacke F. Fluorescent cell-traceable dexamethasone-loaded liposomes for the treatment of inflammatory liver diseases. Biomaterials. 2015;37:367–382. doi: 10.1016/j.biomaterials.2014.10.030. [DOI] [PubMed] [Google Scholar]
- 72.Kaps L., Nuhn L., Aslam M., Brose A., Foerster F., Rosigkeit S., Renz P., Heck R., Kim Y.O., Lieberwirth I., et al. In Vivo Gene-Silencing in Fibrotic Liver by siRNA-Loaded Cationic Nanohydrogel Particles. Adv. Healthc. Mater. 2015;4:2809–2815. doi: 10.1002/adhm.201500826. [DOI] [PubMed] [Google Scholar]
- 73.Leber N., Kaps L., Aslam M., Schupp J., Brose A., Schäffel D., Fischer K., Diken M., Strand D., Koynov K., et al. SiRNA-mediated in vivo gene knockdown by acid-degradable cationic nanohydrogel particles. J. Control. Release. 2017;248:10–23. doi: 10.1016/j.jconrel.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 74.Krithika R., Vhora I., Verma R.J. Preparation, toxicity analysis and in vivo protective effect of phyllanthin-loaded PLGA nanoparticles against CCl4-induced hepatic fibrosis. J. Drug Deliv. Sci. Technol. 2019;51:364–371. doi: 10.1016/j.jddst.2019.03.019. [DOI] [Google Scholar]
- 75.Lin T.-T., Gao D.-Y., Liu Y.-C., Sung Y.-C., Wan D., Liu J.-Y., Chiang T., Wang L., Chen Y. Development and characterization of sorafenib-loaded PLGA nanoparticles for the systemic treatment of liver fibrosis. J. Control. Release. 2016;221:62–70. doi: 10.1016/j.jconrel.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 76.Younis N., Shaheen M.A., Abdallah M.H. Silymarin-loaded Eudragit® RS100 nanoparticles improved the ability of silymarin to resolve hepatic fibrosis in bile duct ligated rats. Biomed. Pharmacother. 2016;81:93–103. doi: 10.1016/j.biopha.2016.03.042. [DOI] [PubMed] [Google Scholar]
- 77.He Q., Zhang J., Chen F., Guo L., Zhu Z., Shi J. An anti-ROS/hepatic fibrosis drug delivery system based on salvianolic acid B loaded mesoporous silica nanoparticles. Biomaterials. 2010;31:7785–7796. doi: 10.1016/j.biomaterials.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 78.Vivero-Escoto J.L., Vadarevu H., Juneja R., Schrum L.W., Benbow J.H. Nanoparticle mediated silencing of tenascin C in hepatic stellate cells: Effect on inflammatory gene expression and cell migration. J. Mater. Chem. B. 2019;7:7396–7405. doi: 10.1039/C9TB01845J. [DOI] [PubMed] [Google Scholar]
- 79.Krishnan G., Subramaniyan J., Chengalvarayan Subramani P., Muralidharan B., Thiruvengadam D. Hesperetin conjugated PEGylated gold nanoparticles exploring the potential role in anti-inflammation and anti-proliferation during diethylnitrosamine-induced hepatocarcinogenesis in rats. Asian J. Pharm. Sci. 2017;12:442–455. doi: 10.1016/j.ajps.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Das A., Mukherjee P., Singla S.K., Guturu P., Frost M.C., Mukhopadhyay D., Shah V.H., Patra C.R. Fabrication and characterization of an inorganic gold and silica nanoparticle mediated drug delivery system for nitric oxide. Nanotechnology. 2010;21:305102. doi: 10.1088/0957-4484/21/30/305102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yu X., Yuan L., Zhu N., Wang K., Xia Y. Fabrication of antimicrobial curcumin stabilized platinum nanoparticles and their anti-liver fibrosis activity for potential use in nursing care. J. Photochem. Photobiol. B Biol. 2019;195:27–32. doi: 10.1016/j.jphotobiol.2019.03.023. [DOI] [PubMed] [Google Scholar]
- 82.Wang M., Zhang M., Fu L., Lin J., Zhou X., Zhou P., Huang P., Hu H., Han Y. Liver-targeted delivery of TSG-6 by calcium phosphate nanoparticles for the management of liver fibrosis. Theranostics. 2020;10:36–49. doi: 10.7150/thno.37301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Melgar-Lesmes P., Luquero A., Parra-Robert M., Mora A., Ribera J., Edelman E.R., Jiménez W. Graphene–Dendrimer Nanostars for Targeted Macrophage Overexpression of Metalloproteinase 9 and Hepatic Fibrosis Precision Therapy. Nano Lett. 2018;18:5839–5845. doi: 10.1021/acs.nanolett.8b02498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Algandaby M.M., Al-Sawahli M.M., Oaa A., Fahmy U.A., Abdallah H.M., Hattori M., Ashour O.M., Abdel-Naim A.B. Curcumin-Zein Nanospheres Improve Liver Targeting and Antifibrotic Activity of Curcumin in Carbon Tetrachloride-Induced Mice Liver Fibrosis. J. Biomed. Nanotechnol. 2016;12:1746–1757. doi: 10.1166/jbn.2016.2270. [DOI] [PubMed] [Google Scholar]
- 85.Lam P.L., Kok S.H.L., Gambari R., Kok T.W., Leung H.Y., Choi K.L., Wong C.S., Hau D.K.P., Wong W.Y., Lam K.H., et al. Evaluation of berberine/bovine serum albumin nanoparticles for liver fibrosis therapy. Green Chem. 2015;17:1640–1646. doi: 10.1039/C4GC01815J. [DOI] [Google Scholar]
- 86.Violatto M.B., Casarin E., Talamini L., Russo L., Baldan S., Tondello C., Messmer M., Hintermann E., Rossi A., Passoni A., et al. Dexamethasone Conjugation to Biodegradable Avidin-Nucleic-Acid-Nano-Assemblies Promotes Selective Liver Targeting and Improves Therapeutic Efficacy in an Autoimmune Hepatitis Murine Model. ACS Nano. 2019;13:4410–4423. doi: 10.1021/acsnano.8b09655. [DOI] [PubMed] [Google Scholar]
- 87.Hawkins M.J., Soon-Shiong P., Desai N. Protein nanoparticles as drug carriers in clinical medicine. Adv. Drug Deliv. Rev. 2008;60:876–885. doi: 10.1016/j.addr.2007.08.044. [DOI] [PubMed] [Google Scholar]
- 88.El-Mezayen N.S., El-Hadidy W.F., El-Refaie W.M., Shalaby T.I., Khattab M.M., El-Khatib A.S. Hepatic stellate cell-targeted imatinib nanomedicine versus conventional imatinib: A novel strategy with potent efficacy in experimental liver fibrosis. J. Control. Release. 2017;266:226–237. doi: 10.1016/j.jconrel.2017.09.035. [DOI] [PubMed] [Google Scholar]
- 89.El-Mezayen N.S., El-Hadidy W.F., El-Refaie W.M., Shalaby T.I., Khattab M.M., El-Khatib A.S. Oral vitamin-A-coupled valsartan nanomedicine: High hepatic stellate cell receptors accessibility and prolonged enterohepatic residence. J. Control. Release. 2018;283:32–44. doi: 10.1016/j.jconrel.2018.05.021. [DOI] [PubMed] [Google Scholar]
- 90.Li Q., Ding Y., Guo X., Luo S., Zhuang H., Zhou J., Xu N., Yan Z. Chemically modified liposomes carrying TRAIL target activated hepatic stellate cells and ameliorate hepatic fibrosis in vitro and in vivo. J. Cell. Mol. Med. 2019;23:1951–1962. doi: 10.1111/jcmm.14097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Liu C.-H., Chan K.-M., Chiang T., Liu J.-Y., Chern G.-G., Hsu F.-F., Wu Y.-H., Liu Y.-C., Chen Y. Dual-Functional Nanoparticles Targeting CXCR4 and Delivering Antiangiogenic siRNA Ameliorate Liver Fibrosis. Mol. Pharm. 2016;13:2253–2262. doi: 10.1021/acs.molpharmaceut.5b00913. [DOI] [PubMed] [Google Scholar]
- 92.Morsy M.A., Nair A.B. Prevention of rat liver fibrosis by selective targeting of hepatic stellate cells using hesperidin carriers. Int. J. Pharm. 2018;552:241–250. doi: 10.1016/j.ijpharm.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 93.Omar R., Yang J., Alrushaid S., Burczynski F.J., Minuk G.Y., Gong Y. Inhibition of BMP4 and Alpha Smooth Muscle Actin Expression in LX-2 Hepatic Stellate Cells by BMP4-siRNA Lipid Based Nanoparticle. J. Pharm. Pharm. Sci. 2018;21:119–134. doi: 10.18433/jpps29584. [DOI] [PubMed] [Google Scholar]
- 94.Yang D., Gao Y.H., Tan K.B., Zuo Z.X., Yang W.X., Hua X., Li P.J., Zhang Y., Wang G. Inhibition of hepatic fibrosis with artificial microRNA using ultrasound and cationic liposome-bearing microbubbles. Gene Ther. 2013;20:1140–1148. doi: 10.1038/gt.2013.41. [DOI] [PubMed] [Google Scholar]
- 95.Qiao J.-B., Fan Q.-Q., Zhang C.-L., Lee J., Byun J., Xing L., Gao X.-D., Oh Y.-K., Jiang H.-L. Hyperbranched lipoid-based lipid nanoparticles for bidirectional regulation of collagen accumulation in liver fibrosis. J. Control. Release. 2020;321:629–640. doi: 10.1016/j.jconrel.2020.02.049. [DOI] [PubMed] [Google Scholar]
- 96.Jia Z., Gong Y., Pi Y., Liu X., Gao L., Kang L., Wang J., Yang F., Tang J., Lu W., et al. pPB Peptide-Mediated siRNA-Loaded Stable Nucleic Acid Lipid Nanoparticles on Targeting Therapy of Hepatic Fibrosis. Mol. Pharm. 2018;15:53–62. doi: 10.1021/acs.molpharmaceut.7b00709. [DOI] [PubMed] [Google Scholar]
- 97.Khaja F., Jayawardena D., Kuzmis A., Önyüksel H. Targeted Sterically Stabilized Phospholipid siRNA Nanomedicine for Hepatic and Renal Fibrosis. Nanomaterials. 2016;6:8. doi: 10.3390/nano6010008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Liu C.-H., Chern G.-J., Hsu F.-F., Huang K.-W., Sung Y.-C., Huang H.-C., Qiu J.T., Wang S.-K., Lin C.-C., Wu C.-H., et al. A multifunctional nanocarrier for efficient TRAIL-based gene therapy against hepatocellular carcinoma with desmoplasia in mice. Hepatology. 2018;67:899–913. doi: 10.1002/hep.29513. [DOI] [PubMed] [Google Scholar]
- 99.Wang J., Pan W., Wang Y., Lei W., Feng B., Du C., Wang X.J. Enhanced efficacy of curcumin with phosphatidylserine-decorated nanoparticles in the treatment of hepatic fibrosis. Drug Deliv. 2018;25:1–11. doi: 10.1080/10717544.2017.1399301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fan Q.-Q., Zhang C.-L., Qiao J.-B., Cui P.-F., Xing L., Oh Y.-K., Jiang H.-L. Extracellular matrix-penetrating nanodrill micelles for liver fibrosis therapy. Biomaterials. 2020;230:119616. doi: 10.1016/j.biomaterials.2019.119616. [DOI] [PubMed] [Google Scholar]
- 101.Qiao J.-B., Fan Q.-Q., Xing L., Cui P.-F., He Y.-J., Zhu J.-C., Wang L., Pang T., Oh Y.-K., Zhang C., et al. Vitamin A-decorated biocompatible micelles for chemogene therapy of liver fibrosis. J. Control. Release. 2018;283:113–125. doi: 10.1016/j.jconrel.2018.05.032. [DOI] [PubMed] [Google Scholar]
- 102.Luo J., Zhang P., Zhao T., Jia M., Yin P., Li W., Zhang Z.-R., Fu Y., Gong T. Golgi Apparatus-Targeted Chondroitin-Modified Nanomicelles Suppress Hepatic Stellate Cell Activation for the Management of Liver Fibrosis. ACS Nano. 2019;13:3910–3923. doi: 10.1021/acsnano.8b06924. [DOI] [PubMed] [Google Scholar]
- 103.Zhang Z., Wang C., Zha Y., Hu W., Gao Z., Zang Y., Chen J., Zhang J., Dong L. Corona-Directed Nucleic Acid Delivery into Hepatic Stellate Cells for Liver Fibrosis Therapy. ACS Nano. 2015;9:2405–2419. doi: 10.1021/nn505166x. [DOI] [PubMed] [Google Scholar]
- 104.Kurniawan D.W., Jajoriya A.K., Dhawan G., Mishra D., Argemi J., Bataller R., Storm G., Mishra D.P., Prakash J., Bansal R. Therapeutic inhibition of spleen tyrosine kinase in inflammatory macrophages using PLGA nanoparticles for the treatment of non-alcoholic steatohepatitis. J. Control. Release. 2018;288:227–238. doi: 10.1016/j.jconrel.2018.09.004. [DOI] [PubMed] [Google Scholar]
- 105.Hassan R., Tammam S.N., Safy S.E., Abdel-Halim M., Asimakopoulou A., Weiskirchen R., Mansour S. Prevention of hepatic stellate cell activation using JQ1- and atorvastatin-loaded chitosan nanoparticles as a promising approach in therapy of liver fibrosis. Eur. J. Pharm. Biopharm. 2019;134:96–106. doi: 10.1016/j.ejpb.2018.11.018. [DOI] [PubMed] [Google Scholar]
- 106.Deshmukh M., Nakagawa S., Higashi T., Vincek A., Venkatesh A., Ruiz de Galarreta M., Koh A.P., Goossens N., Hirschfield H., Bian C.B., et al. Cell type-specific pharmacological kinase inhibition for cancer chemoprevention. Nanomedicine. 2018;14:317–325. doi: 10.1016/j.nano.2017.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gou Y., Miao D.D., Zhou M., Wang L.J., Zhou H.Y., Su G.X. Bio-Inspired Protein-Based Nanoformulations for Cancer Theranostics. Front. Pharmacol. 2018;9:421. doi: 10.3389/fphar.2018.00421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zhang Q., Xu D., Guo Q., Shan W., Yang J., Lin T., Ye S., Zhou X., Ge Y., Bi S., et al. Theranostic Quercetin Nanoparticle for Treatment of Hepatic Fibrosis. Bioconjugate Chem. 2019;30:2939–2946. doi: 10.1021/acs.bioconjchem.9b00631. [DOI] [PubMed] [Google Scholar]
- 109.Wu J., Huang J., Kuang S., Chen J., Li X., Chen B., Wang J., Cheng D., Shuai X. Synergistic MicroRNA Therapy in Liver Fibrotic Rat Using MRI-Visible Nanocarrier Targeting Hepatic Stellate Cells. Adv. Sci. 2019;6:1801809. doi: 10.1002/advs.201801809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Yu Y., Duan J., Li Y., Li Y., Sun Z. Silica nanoparticles induce liver fibrosis via TGF-β1/Smad3 pathway in ICR mice. Int. J. Nanomed. 2017;12:6045–6057. doi: 10.2147/IJN.S132304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Zhang Q., Chang X., Wang H., Liu Y., Wang X., Wu M., Zhan H., Li S., Sun Y. TGF-β1 mediated Smad signaling pathway and EMT in hepatic fibrosis induced by Nano NiO in vivo and in vitro. Environ. Toxicol. 2020;35:419–429. doi: 10.1002/tox.22878. [DOI] [PubMed] [Google Scholar]
- 112.Bo L., Zhang X., Yang J., Zhang Y., Li W., Fan C., Huang Q. Influence of polyethylene glycol coating on biodistribution and toxicity of nanoscale graphene oxide in mice after intravenous injection. Int. J. Nanomed. 2014;9:4697–4707. doi: 10.2147/IJN.S66591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lee I.-C., Ko J.-W., Park S.-H., Shin N.-R., Shin I.-S., Moon C., Kim S.-H., Yun W.-K., Kim H.-C., Kim J.-C. Copper nanoparticles induce early fibrotic changes in the liver via TGF-β/Smad signaling and cause immunosuppressive effects in rats. Nanotoxicology. 2018;12:637–651. doi: 10.1080/17435390.2018.1472313. [DOI] [PubMed] [Google Scholar]
- 114.Wen T., Du L., Chen B., Yan D., Yang A., Liu J., Gu N., Meng J., Xu H. Iron oxide nanoparticles induce reversible endothelial-to-mesenchymal transition in vascular endothelial cells at acutely non-cytotoxic concentrations. Part. Fibre Toxicol. 2019;16:30. doi: 10.1186/s12989-019-0314-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Bartneck M., Ritz T., Keul H.A., Wambach M., Bornemann J., Gbureck U., Ehling J., Lammers T., Heymann F., Gassler N., et al. Peptide-Functionalized Gold Nanorods Increase Liver Injury in Hepatitis. ACS Nano. 2012;6:8767–8777. doi: 10.1021/nn302502u. [DOI] [PubMed] [Google Scholar]
- 116.Jia J., Li F., Zhou H., Bai Y., Liu S., Jiang Y., Jiang G., Yan B. Oral Exposure to Silver Nanoparticles or Silver Ions May Aggravate Fatty Liver Disease in Overweight Mice. Environ. Sci. Technol. 2017;51:9334–9343. doi: 10.1021/acs.est.7b02752. [DOI] [PubMed] [Google Scholar]
- 117.Li J., He X., Yang Y., Li M., Xu C., Yu R. Risk assessment of silica nanoparticles on liver injury in metabolic syndrome mice induced by fructose. Sci. Total Environ. 2018;628:366–374. doi: 10.1016/j.scitotenv.2018.02.047. [DOI] [PubMed] [Google Scholar]
- 118.Soule B., Tirucherai G., Kavita U., Kundu S., Christian R. Safety, tolerability, and pharmacokinetics of BMS-986263/ND-L02-s0201, a novel targeted lipid nanoparticle delivering HSP47 siRNA, in healthy participants: A randomised, placebo-controlled, double-blind, phase 1 study. J. Hepatol. 2018;68:S112. doi: 10.1016/S0168-8278(18)30442-2. [DOI] [Google Scholar]
- 119.Sakamoto N., Ogawa K., Suda G., Morikawa K., Sho T., Nakai M., Suzuki H., Yamagata N., Tanaka Y., Ying W. Clinical phase 1b study results for safety, pharmacokinetics and efficacy of ND-L02-s0201, a novel targeted lipid nanoparticle delivering HSP47 SIRNA for the treatment of Japanese patients with advanced liver fibrosis. J. Hepatol. 2018;68:S242. doi: 10.1016/S0168-8278(18)30701-3. [DOI] [Google Scholar]