Abstract
This cohort study examines the association between surgical technical skill and overall survival following colectomy for colon cancer.
Surgical technique is presumed to be an important determinant of patient outcomes. Surgical technical skill, measured by video review, has been associated with postoperative morbidity and histopathologic outcomes.1,2,3 However, it is unknown whether technical skill is associated with long-term survival. Our objective was to assess the association between surgical technical skill and overall survival following colectomy for colon cancer.
Methods
Surgeons were recruited from the Illinois Surgical Quality Improvement Collaborative in 2016 for a video-based technical skills assessment program.4 Each surgeon submitted 1 representative video of a laparoscopic right hemicolectomy that they performed. Videos were reviewed by 12 or more surgeons, including 2 colorectal surgeons with video evaluation experience. Skill scores were assigned using the American Society of Colon & Rectal Surgeons Video Assessment Tool, and the mean score from all raters was used.2,5 Skill score was analyzed separately by terciles and as a continuous variable.
Patients who underwent any minimally invasive colectomy for stage I to III epithelial-origin colon cancer were identified in the National Cancer Database.6 Patients with operations performed from 2012 to 2017 by participating surgeons were identified by National Provider Identifier numbers, which are maintained internally by the American College of Surgeons. The primary outcome was overall survival after surgery, and the secondary outcome was the number of lymph nodes harvested. This study was deemed exempt by the Northwestern University institutional review board, and the need for informed consent was waived because of the minimal risks of linking data from a quality improvement effort with a deidentified clinical registry.
Survival was estimated using the Kaplan-Meier method, with differences among terciles assessed by the log-rank test. Hazard ratios (HRs) for death were estimated using a multivariable Cox proportional hazards regression, and a multivariable linear regression was used to evaluate the association of skill with the number of lymph nodes harvested. Significance tests were 2-sided with a threshold of P < .05. Analyses were performed using SAS, version 9.4 (SAS Institute).
Results
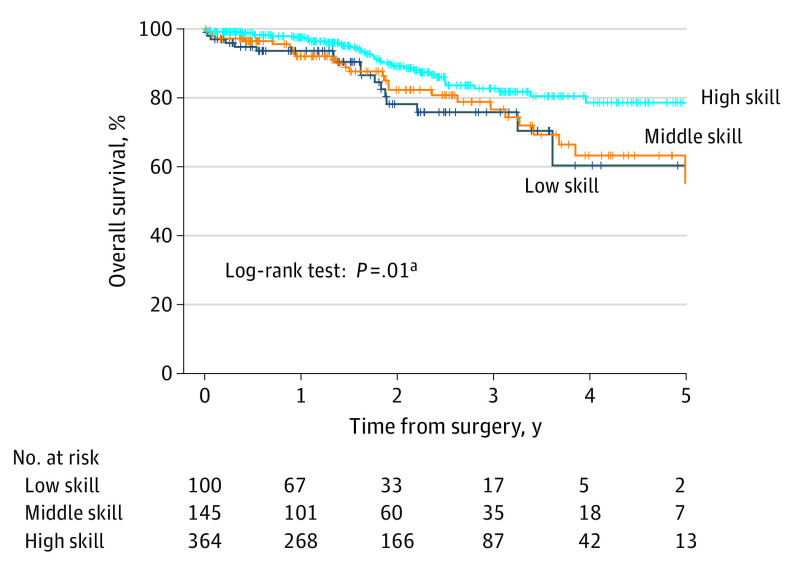
In total, 609 patients underwent laparoscopic colectomy at 11 hospitals performed by 1 of 15 participating surgeons (9 colorectal [60%]; 6 general [40%]). Overall survival differed among skill terciles (5-year survival: 79% for high-skill, 55% for medium-skill, and 60% for low-skill; P = .01 for log-rank test; Figure). Adjusting for patient characteristics, survival was improved for the high-skill vs low-skill tercile (HR, 0.31; 95% CI, 0.18-0.54; P < .001; Table). Each 0.1-point skill score increment was associated with a higher likelihood of survival (HR, 0.90; 95% CI, 0.84-0.97; P = .01). A sensitivity analysis excluding 90-day mortalities demonstrated similar results.
Figure. Patient Overall Survival After Surgery by Surgeon Skill.
On pairwise comparison of survival using the log-rank test with Šidák correction for multiple comparisons.
aLog-rank test for overall comparison high vs low skill, P > .99 for middle vs low skill, and P = .04 for high vs middle skill.
Table. Patients, Surgeons, Process Measures, and Outcomes by Surgical Skill Tercile.
| Characteristic | No. (%) | P valuea | ||
|---|---|---|---|---|
| Low skill | Middle skill | High skill | ||
| Surgeon characteristics | ||||
| Surgeons | 5 (33) | 5 (33) | 5 (33) | NA |
| Patients | 100 | 145 | 364 | |
| Annual surgical volume, mean (SD)b | 20.0 (5.3) | 29.0 (12.8) | 72.8 (55.1) | |
| Technical skill score, mean (SD) [range]c | 3.2 (0.2) [3.0 to 3.4] | 3.7 (0.1) [3.5 to 3.8] | 4.2 (0.3) [4.0 to 4.6] | |
| Patient characteristics | ||||
| Age, mean (SD), y | 64.5 (13.4) | 66.4 (13.8) | 66.9 (13.1) | .32 |
| Sex | ||||
| Male | 43 (43) | 82 (57) | 178 (49) | .10 |
| Female | 57 (57) | 63 (43) | 186 (51) | |
| Race/ethnicity | ||||
| Non-Hispanic White | 65 (65) | 106 (73) | 295 (81) | <.001 |
| Non-Hispanic Black | 25 (25) | 32 (22) | 35 (10) | |
| Hispanic | 8 (8) | 4 (3) | 13 (4) | |
| Other | 2 (2) | 3 (2) | 21 (6) | |
| Primary payer | ||||
| Uninsured/unknown | 7 (7) | 9 (6) | 17 (5) | .42 |
| Private insurance | 24 (24) | 45 (31) | 122 (34) | |
| Governmentd | 69 (69) | 91 (63) | 225 (62) | |
| Charlson/Deyo score, mean (SD)e | 0.42 (1.00) | 0.57 (0.92) | 0.46 (0.96) | .06 |
| Stage | ||||
| I | 33 (33) | 36 (25) | 123 (34) | .26 |
| II | 35 (35) | 48 (33) | 117 (32) | |
| III | 32 (32) | 61 (42) | 124 (34) | |
| Operation type | ||||
| Partial colectomy | 96 (96) | 133 (92) | 344 (95) | .33 |
| Total colectomy | 4 (4) | 12 (8) | 20 (5) | |
| Process measures | ||||
| Lymph node harvest | ||||
| Nodes examined, mean (SD) | 20.3 (9.2) | 21.2 (10.5) | 23.9 (12.1) | .003 |
| Adjusted difference, β (95% CI)f | 0 [Reference] | +1.0 (−2.4 to 4.3) | +4.0 (−0.5 to 8.4) | NA |
| P valuef | NA | .56 | .08 | NA |
| Adjuvant chemotherapy | ||||
| No. of recipients/No. of stage III patients (%)g | 24/31 (77) | 49/59 (83) | 100/123 (81) | .81 |
| Days from surgery to treatment, mean (SD) | 48.9 (15.5) | 52.8 (34.7) | 47.0 (18.8) | .60 |
| Survival outcomes | ||||
| Overall survival, HR (95% CI)h | 1 [Reference] | 0.51 (0.23-1.15) | 0.31 (0.18-0.54) | NA |
| Deaths within 90 d excluded, HR (95% CI) | 1 [Reference] | 0.56 (0.29-1.06) | 0.35 (0.22-0.58) | |
| Stratified by stage, HR (95% CI) | ||||
| I | 1 [Reference] | 0.62 (0.10-4.03) | 0.22 (0.04-1.10) | NA |
| II | 1 [Reference] | 0.12 (0.04-0.39) | 0.14 (0.07-0.30) | |
| III | 1 [Reference] | 1.00 (0.49-2.04) | 0.54 (0.30-0.95) | |
| Open approach, HR (95% CI) | 1 [Reference] | 0.41 (0.23-0.72) | 0.41 (0.18-0.90) | NA |
Abbreviations: HR, hazard ratio; NA, not applicable.
Associations between skill tercile and patient characteristics evaluated using 1-way analysis of variance, Kruskal-Wallis, and χ2 tests.
Annual volume of colectomy procedures per surgeon.
Skill scores were determined based on the American Society of Colon and Rectal Surgeons Video Assessment Tool, which incorporates assessment of (1) control of the ileocolic vascular pedicle, (2) respect for tissue, (3) time and motion, (4) instrument handling, (5) flow of operation, (6) exposure, (7) tissue planes, (8) completeness of dissection, and (9) overall technical skill.
Includes Medicare, Medicaid, Military, TRICARE, Veterans Affairs, and Indian/Public Health Service.
Excluding cancer.
Multivariable linear regression model estimating the mean number of lymph nodes examined; adjusted for patient age, sex, race/ethnicity, payer, Charlson/Deyo score, stage, operation type, and year of surgery while accounting for surgeon-level clustering.
Excluding patients who received neoadjuvant chemotherapy.
Primary analysis of patients undergoing minimally invasive colectomy for cancer modeled with Cox proportional hazards regression to estimate the hazard of death. Model adjusted for patient age, sex, race/ethnicity, payer, Charlson/Deyo score, stage, operation type, and year of surgery while accounting for surgeon-level clustering. No significant difference was noted on pairwise comparison of the high-skill vs middle-skill tercile.
A stage-stratified sensitivity analysis demonstrated that the association between skill and outcomes was strongest among patients with stage II disease (high vs low skill: HR, 0.14; 95% CI, 0.07-0.30; P < .001; middle vs low skill: HR, 0.12; 95% CI, 0.04-0.39; P < .001; 0.1-point score increment: HR, 0.85; 95% CI, 0.78-0.94; P < .001; Table). In a sensitivity analysis of 307 open procedures, survival was improved for the high-skill (HR, 0.41; 95% CI, 0.18-0.90; P = .03) and middle-skill (HR, 0.41; 95% CI, 0.23-0.72; P = .002) vs the low-skill tercile; however, each 0.1-point skill score increment was not significantly associated with survival (HR, 0.91; 95% CI, 0.80-1.05; P = .20). The mean (SD) number of lymph nodes examined was 23.9 (9.2) for the high-skill tercile, 21.2 (10.5) for the middle-skill tercile, and 20.3 (12.1) for the low-skill tercile, but terciles did not differ significantly on adjusted analysis.
Discussion
This study demonstrates an association between surgical technical skill and long-term survival following cancer surgery. This association persists when excluding early postoperative deaths, suggesting that these findings are not solely attributable to mortality from surgical complications. Study limitations include a small surgeon sample and skill assessment based on a single video. Skill may affect survival through oncologic resection quality (eg, lymph node harvesting) or may reflect surgeon characteristics, such as operative volume or guideline adherence. Additionally, fewer complications might reduce long-term morbidity affecting nutrition and physical function.
References
- 1.Birkmeyer JD, Finks JF, O’Reilly A, et al. ; Michigan Bariatric Surgery Collaborative . Surgical skill and complication rates after bariatric surgery. N Engl J Med. 2013;369(15):1434-1442. doi: 10.1056/NEJMsa1300625 [DOI] [PubMed] [Google Scholar]
- 2.Stulberg JJ, Huang R, Kreutzer L, et al. . Association between surgeon technical skills and patient outcomes. JAMA Surg. 2020. doi: 10.1001/jamasurg.2020.3007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Curtis NJ, Foster JD, Miskovic D, et al. . Association of surgical skill assessment with clinical outcomes in cancer surgery. JAMA Surg. 2020;155(7):590-598. doi: 10.1001/jamasurg.2020.1004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Illinois Surgical Quality Improvement Collaborative ISQIC overview. Accessed April 23, 2020. https://www.isqic.org/about-isqic
- 5.Champagne BJ, Steele SR, Hendren SK, et al. . The American Society of Colon and Rectal Surgeons assessment tool for performance of laparoscopic colectomy. Dis Colon Rectum. 2017;60(7):738-744. doi: 10.1097/DCR.0000000000000817 [DOI] [PubMed] [Google Scholar]
- 6.Bilimoria KY, Stewart AK, Winchester DP, Ko CY. The National Cancer Data Base: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol. 2008;15(3):683-690. doi: 10.1245/s10434-007-9747-3 [DOI] [PMC free article] [PubMed] [Google Scholar]