Abstract
All-trans retinoic acid (atRA) has a dramatic impact on the survival of patients with acute promyelocytic leukemia, but its therapeutic value in other types of acute myeloid leukemia (AML) has so far remained unclear. Given that AML is a stem cell-driven disease, recent studies have addressed the effects of atRA on leukemic stem cells (LSCs). atRA promoted stemness of MLL-AF9-driven AML in an Evi1-dependent manner but had the opposite effect in Flt3-ITD/Nup98-Hoxd13-driven AML. Overexpression of the stem cell-associated transcription factor EVI1 predicts a poor prognosis in AML, and is observed in different genetic subtypes, including cytogenetically normal AML. Here, we therefore investigated the effects of Evi1 in a mouse model for cytogenetically normal AML, which rests on the combined activity of Flt3-ITD and Npm1c mutations. Experimental expression of Evi1 on this background strongly promoted disease aggressiveness. atRA inhibited leukemia cell viability and stem cell-related properties, and these effects were counteracted by overexpression of Evi1. These data further underscore the complexity of the responsiveness of AML LSCs to atRA and point out the need for additional investigations which may lay a foundation for a precision medicine-based use of retinoids in AML.
Keywords: AML, leukemia stem cells, all-trans retinoic acid, FLT3-ITD, EVI1, MECOM
1. Introduction
Acute myeloid leukemia (AML) is an aggressive hematopoietic malignancy whose incidence increases with age [1,2]. Even though the number of genetic lesions per individual is low compared to other cancers [3], its genetic causes are complex and heterogeneous [4,5,6,7,8]. A number of recurrent chromosome rearrangements and point mutations have been described, among them the translocation t(8;21) which gives rise to the acute myeloid leukemia 1—eight-twentyone (AML1-ETO) fusion gene, 11q23 rearrangements involving the mixed lineage leukemia (MLL) gene, nucleoporin 98 (NUP98) fusions, nucleophosmin 1 (NPM1) mutations, and fms related receptor tyrosine kinase 3 internal tandem duplications (FLT3-ITD) [4,5,6,9,10]. Further, aberrant expression of genes, including that encoding the transcription factor Ecotropic Viral Integration site 1 (EVI1), is a typical feature of AML [4,7,11,12,13]. Many molecular and genetic aberrations have prognostic value and/or represent potential or actual targets for rationally designed therapeutics [4,5,6,7,12,13,14]. Indeed, several targeted drugs were recently approved for use in AML and will complement standard chemotherapy for selected groups of patients [14]. However, acute promyelocytic leukemia (APL), characterized by rearrangements of the retinoic acid receptor alpha (RARA) gene, has benefited more than any other AML subtype from targeted therapies: addition of the RARA ligand all-trans retinoic acid (atRA) to its therapy has greatly improved APL patient survival for the last few decades [15,16,17]. Despite the striking success of atRA in APL, and even though atRA also causes blast differentiation and sensitization to chemotherapy in other types of AML in vitro [18,19,20,21,22,23,24,25,26,27], clinical benefit of atRA in non-APL AML has not been consistently demonstrated so far [20,27,28,29,30,31]. Further, attempts to identify genetically defined subgroups of patients that may respond to atRA-containing therapy have yielded contradictory results [20,27,29,30,31,32].
Both normal and leukemic hematopoiesis are organized in a hierarchical manner, and emanate from mostly quiescent stem cells (hematopoietic stem cells, HSCs, or leukemic stem cells, LSCs, respectively) that reside in a specialized niche in the bone marrow (BM) [33,34,35]. These stem cells give rise to highly proliferative progenitors, which in normal hematopoiesis differentiate into non-dividing functional blood cells, but in malignant hematopoiesis form the bulk of the only partially differentiated leukemic cell mass [33,34,35]. LSCs play key roles not only in leukemia emergence, but also in chemotherapy resistance and relapse [33]. Therefore, determining the effect of a potential therapeutic on LSCs may be pivotal to understanding its clinical effectiveness [33]. Some recent studies investigated the impact of atRA on AML LSCs, with divergent results [27]. atRA inhibited stem cell abundance and activity in a mouse model of AML driven by a Nup98-Hoxd13 fusion gene together with an FLT3-ITD [36]. By contrast, atRA promoted serial replating ability—considered as a readout of stem cell activity—in AML1-ETO-expressing murine BM cells [21]. Similarly, in an MLL-AF9-driven mouse model of AML, atRA augmented stem cell abundance, quiescence, and activity in a manner that was dependent on the expression of Evi1 [37]. EVI1 and atRA also collaborated to promote stem cell-related properties in human AML cell lines and primary samples [37].
In the present study, we asked whether EVI1 would also interact with atRA to alter LSC-related properties on the background of different genetic driver lesions. Since 21% of EVI1-overexpressing AMLs are cytogenetically normal [13], we sought to employ a model for cytogenetically normal AML. The most frequent mutations in cytogenetically normal AML affect the FLT3 and NPM1 genes (the latter lead to a predominantly cytoplasmic localization of the chaperone protein NPM1, hence are referred to as “NPM1c”) [4,5,6], and mice whose hematopoietic cells carry a Flt3-ITD and an Npm1c allele develop an aggressive, AML-like disease [38]. The Flt3-ITD/Npm1c model was therefore used in the current study. We found that atRA inhibited leukemia cell (LC) viability as well as LSC-related properties in Evi1low Flt3-ITD/Npm1c-driven AML, but these effects were counteracted by experimental Evi1 expression.
2. Experimental Section
2.1. Ethics Approval
Animal experiments were approved by the Animal Ethics Committee of the Medical University of Vienna and the Austrian Federal Ministry of Education, Science, and Research (GZ66.009/0309-WF/V/3b/2015, 3 November 2015). Federation of European Laboratory Animal Science Associations and Austrian guidelines to minimize animal distress and suffering were followed.
2.2. Ex Vivo Culture of Cells from Flt3-ITD/Npm1c-Driven Murine AML and Evi1 Overexpression
Spleen cells from C57BL/6 mice that had succumbed to AML following transplantation with Flt3-ITD/Npm1c-transformed hematopoietic cells [38] were cultured in IMDM medium (Thermo Fisher Scientific, Waltham, MA, USA) containing 10% fetal bovine serum (Thermo Fisher Scientific), 1% L-glutamine (Thermo Fisher Scientific), 50 ng/mL mSCF (Peprotech, Hamburg, Germany), 10 ng/mL mIL-3 (Peprotech), and 10 ng/mL mIL-6 (BioLegend, San Diego, CA, USA). To generate Evi1high and Evi1low variants of Flt3-ITD/Npm1c-driven AML, these cells were transduced either with a vector encoding an epitope-tagged version of murine Evi1 (pMYs_FLAG-Evi1_IRES_GFP, kindly provided by Dr. Takuro Nakamura, Cancer Institute of JFCR, Tokyo, Japan) or with empty vector as a control. In brief, vectors were transfected into Platinum-E cells, along with the ecotropic packaging plasmid psi2 (containing the gag, pol, and env genes) using a standard calcium chloride protocol. Virus-containing supernatants were harvested after 48–96 h, filtered (0.45 µm pore size), and supplemented with polybrene (4 μg/mL). Cells were spinoculated with retroviral supernatant for 60 min at 1300 rpm and 34 °C. The process was repeated with fresh retroviral supernatant after 24 and 48 h. Five days after the last transduction, Flt3-ITD/Npm1c_Evi1 and Flt3-ITD/Npm1c_vec cells were sorted for GFP positivity and expanded in the above-described medium. For transplantation, 6–8-week-old female C57BL/6 recipient mice were sub-lethally irradiated (5 Gy). On the next day, mice were anesthetized by i.p. injection of 100 µL Ketasol/Rompun solution (18.5 mg/mL Ketasol (AniMedica, Senden, Germany), 1.5 mg/mL Rompun (Bayer, Leverkusen, Germany), and 0.9% sodium chloride (Braun, Kronberg, Germany)) followed by retro-orbital injection of 400,000 Flt3-ITD/Npm1c_Evi1 or Flt3-ITD/Npm1c_vec cells. Mice were monitored for signs of disease (immotility, hunched posture, scrubby fur, loss of body weight), and sacrificed when terminally ill. Their BM and spleen cells were collected and vitally frozen. The GFP-positive fractions of these cells were considered as LCs, and are referred to as LCFlt3-ITD/Npm1c_Evi1 and LCFlt3-ITD/Npm1c_vec, respectively. For ex vivo experiments, cells were thawed and maintained in the medium described at the beginning of this chapter.
2.3. Drug Treatment, Cell Viability (Metabolic Activity), and Apoptosis Assays
For cell viability and apoptosis assays, BM LCFlt3-ITD/Npm1c_vec and LCFlt3-ITD/Npm1c_Evi1 were seeded at 200 cells/µL and incubated with various concentrations of atRA (Sigma-Aldrich, St. Louis, MO, USA) or with solvent for 48 h. Metabolic activity as a proxy for cell viability was determined in white-walled 96-well-plates (Greiner Bio-One, Kremsmuenster, Austria) using the CellTiter-Glo® Luminescent Cell Viability Assay (Promega, Madison, WI, USA). Luminescence was measured using the Varioskan LUX microplate reader with SkanIt Software for Microplate Readers RE, Version 5.0.0.42. (Thermo Fisher Scientific).
Annexin V assays were performed to quantify the proportions of apoptotic cells after drug treatment. Thus, cells were stained with 2 µL of Annexin V-APC (BD Biosciences, Franklin Lakes, NJ, USA) in 100 µL Annexin V binding buffer (10 mM HEPES (Sigma-Aldrich), pH 7.4, 140 mM NaCl (Carl Roth, Karlsruhe, Germany), and 2.5 mM CaCl2 (Sigma-Aldrich)) for 15 min at room temperature, and analyzed by flow cytometry (LSR Fortessa, BD Biosciences). Annexin V− cells were classified as viable and Annexin V+ as apoptotic.
2.4. Determination of Myeloid Differentiation by Flow Cytometry
To analyze myeloid differentiation, BM cells from leukemic mice were treated with 1 µM atRA (Sigma-Aldrich) or the corresponding amount of solvent for 72 h. Afterwards, 500,000 cells per sample were washed once with PBS and stained with 1 µL of CD11b (clone M1/70, BioLegend) and Gr-1 (clone RB6-8C5, BioLegend) antibodies in 100 µL 2% fetal bovine serum/PBS for 30 min. Cells were washed again and analyzed by flow cytometry (LSR Fortessa, BD Biosciences). Analyses were restricted to leukemic cells by gating on the GFP-positive population.
2.5. Serial Replating Assays
For serial replating assays, BM LCFlt3-ITD/Npm1c_vec and LCFlt3-ITD/Npm1c_Evi1 were treated with 1 µM atRA or the corresponding amount of solvent for 72 h. Thereafter, 3000 cells were plated per well of a six-well plate in MethoCult GF M3434 (Stemcell Technologies, Vancouver, Canada). Every seven days, the numbers of colonies were quantified, and 3000 cells were used for replating.
2.6. Quantitative RT-PCR
Total RNA was extracted using Trizol (Thermo Fisher Scientific) and reverse-transcribed using random hexamer primers (Thermo Fisher Scientific) and M-MLV reverse transcriptase (Thermo Fisher Scientific). Quantitative RT-PCR (qRT-PCR) was performed on a Step One Plus Real Time PCR system (Thermo Fisher Scientific) using GoTaq qPCR Master Mix (Promega) and the following primers: Evi1 (fwd: 5′-CTCGAAGCCTTCAGGAACAC-3′, rev: 5′-AGCTTCAAGCGGGTCAGTTA-3′), ß-2-microglobulin (fwd: 5′-CCTTCAGCAAGGACTGGTCT-3′, rev: 5′-TGTCTCGATCCCAGTAGACG-3′). Assays were performed in triplicate, and Evi1 expression was normalized to ß-2-microglobulin expression using the ΔΔCT method [39].
2.7. Immunoblot Analysis
Preparation of protein lysates from spleen LCs, SDS-PAGE, transfer to PVDF membranes (Hybond-P; Amersham, Amersham, United Kingdom), and antibody incubations were performed using standard procedures. The following antibodies were used: anti-FLAG (clone M2; Sigma-Aldrich; 1:1000) and anti-GAPDH (clone 14C10; Cell Signaling Technologies, Danvers, MA, USA; 1:50,000). Blots were developed using SuperSignal West Femto or Pico Chemiluminescent Substrate (both from Thermo Fisher Scientific) and scanned using a ChemiDoc Touch Imaging System (Bio-Rad Laboratories, Hercules, CA, USA).
2.8. Statistical Analyses of Experimental Data
Significance of differences between multiple groups was determined by 2-way ANOVA followed by Bonferroni’s post hoc test. In serial replating assays, numbers of colonies were expressed relative to LCFlt3-ITD/Npm1c_vec -atRA in each round of plating; significance was assessed using the one-sample t-test for comparisons with the control and Student’s t-test for other comparisons. The log-rank test was used to evaluate survival differences between groups of mice. Two-sided p-values < 0.05 were considered statistically significant. Analyses were performed using GraphPad Prism 6 (San Diego, CA, USA) software.
3. Results
3.1. Experimental Expression of Evi1 in Flt3-ITD/Npm1c-Driven Murine AML Decreases Disease Latency
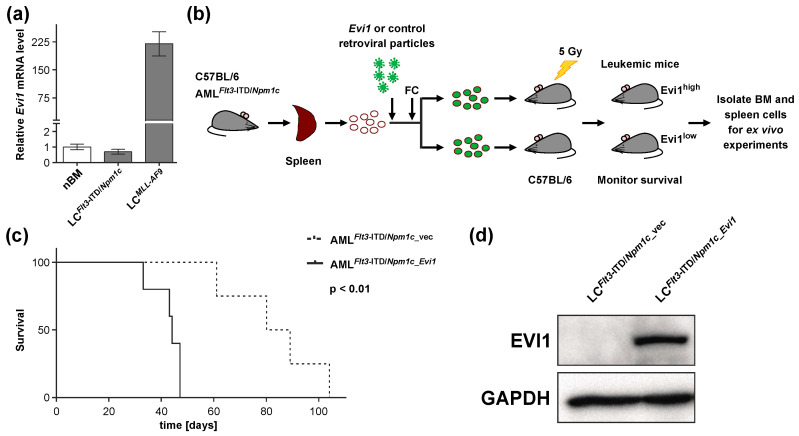
Human patients with cytogenetically normal AML may overexpress EVI1 or not [12,13,40]. We therefore determined the expression of Evi1 in Flt3-ITD/Npm1c-driven murine AML [38] using qRT-PCR. Evi1 mRNA levels in BM from Flt3-ITD/Npm1c mice were comparable to those in normal mouse BM, and substantially lower than in BM from mice with MLL-AF9-driven AML (Figure 1a). Therefore, LCs from Flt3-ITD/Npm1c mice were transduced with a vector encoding an epitope-tagged version of murine Evi1 (pMYs_FLAG-Evi1_IRES_GFP) or with empty vector as a control, and sorted for GFP positivity to yield Flt3-ITD/Npm1c_Evi1 and Flt3-ITD/Npm1c_vec cells, respectively. These were transplanted into sub-lethally irradiated C57BL/6 recipient mice (400,000 cells/mouse; Figure 1b and Figure S1). In agreement with earlier observations [41,42], Evi1 up-regulation dramatically decreased time to disease onset (Figure 1c; median survival, 84 and 44 days for recipients of Flt3-ITD/NPM1c_vec and Flt3-ITD/NPM1c_Evi1 cells, respectively, p < 0.01). The presence of the EVI1 protein in LCFlt3-ITD/Npm1c_Evi1, but not LCFlt3-ITD/Npm1c_vec, obtained from terminally ill recipient mice was confirmed by immunoblot analysis using a FLAG antibody (Figure 1d).
Figure 1.
Experimental expression of Evi1 decreases the latency of Flt3-ITD/Npm1c-driven murine AML. (a) Relative Evi1 mRNA levels in normal murine bone marrow cells (nBM) and in leukemic cells from bone marrow (BM) of mice with Flt3-ITD/Npm1c- and MLL-AF9-driven AML (LCFlt3-ITD/Npm1c and LCMLL-AF9, respectively; n = 3). (b) Schematic of experimental design. Spleen cells from mice terminally ill with Flt3-ITD/Npm1c-driven AML (AMLFlt3-ITD/Npm1c) were transduced with pMSCV_FLAG-Evi1_IRES_GFP or with empty vector as a control. GFP-positive cells were sorted and transplanted into sub-lethally irradiated recipient mice. FC, flow cytometry; BM, bone marrow. (c) Kaplan–Meier plot of mice transplanted with Flt3-ITD/Npm1c_vec and Flt3-ITD/Npm1c_Evi1 cells (400,000 cells/mouse). n = 4 (AMLFlt3-ITD/Npm1c_vec group), n = 5 (AMLFlt3-ITD/Npm1c_Evi1 group). (d) Immunoblot analysis of FLAG-EVI1 expression in spleen LCFlt3-ITD/Npm1c_Evi1 and LCFlt3-ITD/Npm1c_vec from terminally ill recipient mice. GAPDH was used as a loading control.
3.2. atRA Reduces Viability and Stem Cell Related Properties in LCs from Flt3-ITD/Npm1c-Driven AML, but Experimental Expression of Evi1 Counteracts These Effects
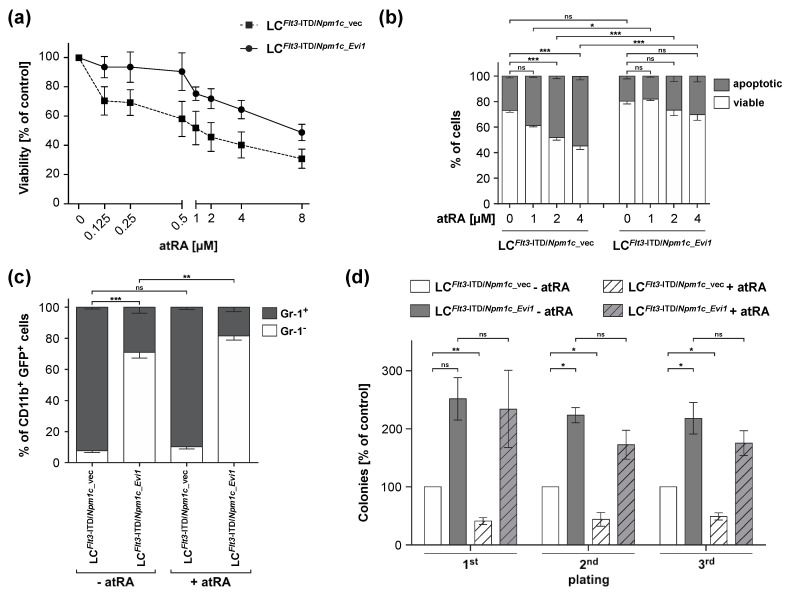
To determine the effects of atRA, and its interactions with the expression of Evi1, on viability, apoptosis, differentiation, and stem cell-related properties of LCs from Flt3-ITD/Npm1c-driven AML, BM LCFlt3-ITD/Npm1c_vec and LCFlt3-ITD/Npm1c_Evi1 were treated with atRA or solvent and subjected to appropriate assays. A three-day ex vivo incubation with atRA decreased the viability of LCFlt3-ITD/Npm1c_vec in a dose-dependent manner, while experimental expression of Evi1 reduced the sensitivity towards atRA in this assay (IC50, 1.12 µM for LCFlt3-ITD/Npm1c_vec and 2.95 µM for LCFlt3-ITD/Npm1c_Evi1; Figure 2a). LCFlt3-ITD/Npm1c_Evi1 also exhibited a slightly lower rate of basal apoptosis than LCFlt3-ITD/Npm1c_vec, and had a strongly and significantly diminished response to the cell death-promoting effect of atRA (Figure 2b and Figure S2a). Further underscoring the increased aggressiveness of AML with Evi1 overexpression, LCFlt3-ITD/Npm1c_Evi1 contained a much higher proportion of immature (Gr-1−) cells within the myeloid (CD11b+) compartment than LCFlt3-ITD/Npm1c_vec (Figure 2c and Figure S2b). atRA slightly increased the proportion of immature myeloid cells among LCFlt3-ITD/Npm1c_Evi1 but had no significant effect on LCFlt3-ITD/Npm1c_vec (Figure 2c and Figure S2b). Finally, Evi1 overexpression increased the serial replating efficiency, an indicator of LSC activity, of Flt3-ITD/Npm1c-driven AML cells (Figure 2d and Figure S2c). Importantly, atRA reduced the replating ability of LCFlt3-ITD/Npm1c_vec, but had no significant effect on that of LCFlt3-ITD/Npm1c_Evi1 (Figure 2d and Figure S2c).
Figure 2.
Experimental expression of Evi1 counteracts the anti-leukemic and stem cell inhibitory effects of atRA in Flt3-ITD/Npm1c-driven murine AML. (a,b) Bone marrow LCFlt3-ITD/Npm1c_vec and LCFlt3-ITD/Npm1c_Evi1 were treated with the indicated concentrations of atRA or with solvent for 48 h. (a) Cell viability was determined using metabolic activity as a proxy (Cell-Titer Glo® assay). n = 4. (b) Apoptosis was determined through Annexin V staining followed by flow cytometry. n = 2–4. (c) Myeloid differentiation. Bone marrow cells from leukemic mice were treated with 1 µM atRA or the corresponding amount of solvent for 72 h, stained with CD11b and Gr-1 antibodies, and subjected to flow cytometry. Analyses were restricted to leukemia cells (LCs) by gating on GFP-positive cells. n = 3. (d) Serial replating activity. Bone marrow LCFlt3-ITD/Npm1c_vec and LCFlt3-ITD/Npm1c_Evi1 were treated with 1 µM atRA or the corresponding amount of solvent for 72 h. A total of 3000 cells were plated per well of a six-well plate in MethoCult GF M3434. Every seven days, the numbers of colonies were quantified, and 3000 cells were re-plated. Numbers of colonies are expressed relative to those obtained with solvent-treated LCFlt3-ITD/Npm1c_vec in each round of plating. n = 3. (a–d) *, p < 0.05; **, p < 0.01; ***, p < 0.001; ns, not significant.
In summary, our results demonstrate anti-leukemic effects of atRA towards LCs and LSCs from Flt3-ITD/Npm1c-driven AML. These effects were counteracted by experimental expression of Evi1. These data confirm the earlier noted genetic and molecular complexity of the responsiveness of AML LSCs to atRA [27,37].
4. Discussion
atRA in combination with chemotherapy and, more recently, arsenic trioxide has greatly improved the outcome of APL [15,16,17]. In contrast, the success of atRA in non-APL AML has been limited so far [31]. Further, the sensitivity of certain molecularly or genetically defined AML subgroups (defined by MN1 expression or NPM1 mutations, respectively) was not confirmed in subsequent studies [20,27,29,30,31,32]. Nevertheless, atRA and other retinoids remain attractive options for the treatment of AML because of their low toxicity and abundant preclinical data suggesting their possible effectiveness in this disease [18,19,20,21,22,23,24,25,26,27,36]. The ongoing clinical interest in the use of atRA in AML is indicated by recent publications [43,44] and the fact that several trials are currently recruiting (www.clinicaltrials.gov).
Surprisingly, even though AML is well established as a stem cell-driven disease [33], to date very few studies have addressed the effect of atRA on AML LSCs. In AML1-ETO-expressing murine BM cells, atRA increased serial replating ability and led to the formation of larger and more immature colonies [21], suggesting that atRA promoted LSC activity on this genetic background. Similarly, atRA promoted leukemic stemness in an MLL-AF9-driven mouse model of AML in a manner dependent on the expression of Evi1 [37]. MLL rearrangements are frequently associated with EVI1 overexpression in human AML [45,46], and this is reflected in the corresponding mouse model [37,47]. In BM cells from MLL-AF9 leukemic mice, atRA promoted the abundance and quiescence of an immunophenotypically defined LSC-enriched cell population and enhanced the activity of LSCs as determined by serial replating and in vivo limiting dilution assays. These effects of atRA were abolished by knock-down of Evi1 [37]. Correspondingly, an RAR antagonist decreased LSC-related properties in an Evi1-dependent manner in vitro and in vivo, and prolonged survival of both of primary treated and secondary recipient mice with Evi1high, MLL-AF9-driven AML. Confirmatory results were obtained with both human AML cell lines and with primary AML samples [37].
In sharp contrast to the observations with the AML1-ETO and MLL-AF9 models, atRA inhibited LSC activity in an AML mouse model driven by an Flt3-ITD in combination with a Nup98-Hoxd13 fusion gene [36]. Treatment of primary mice with atRA alone or in combination with the tyrosine kinase inhibitor sorafenib prolonged time to disease onset in secondary recipients. Moreover, an in vivo limiting dilution assay with cells from the treated mice revealed ~9-fold, ~500-fold, and >12,000-fold reductions in LSC frequencies upon treatment with atRA, sorafenib, and atRA + sorafenib, respectively [36]. The present study corroborates the notion that the Flt3-ITD—which in this case was combined with an Npm1 mutation in order to reveal its leukemogenic potential—renders AML LSCs sensitive to the inhibitory effects of atRA. Furthermore, we show that overexpression of Evi1 abolishes the inhibitory effect of atRA on Flt3-ITD/Npm1c-bearing LSCs. Together, these data suggest that complex genetic and molecular interactions determine the response of AML LSCs to atRA. Further underscoring this, and in sharp contrast to its role in AML, on the background of the APL-typical PML-RARA fusion, the Flt3-ITD mutation reduced the inhibitory effect of atRA on the ability to initiate leukemia in secondary recipients [48].
The molecular and genetic complexity determining the atRA responsiveness of AML LSCs may explain, to some extent, why it has been difficult to identify patient groups benefitting from atRA in non-APL AML. Other aspects that warrant consideration are the identity of the drugs used in conjunction with atRA, as well as the timing and duration of treatment. Different trials assessing the efficacy of atRA in AML were based on different chemotherapeutics. atRA was initiated at different time points relative to the start of chemotherapy, and was included in the maintenance therapy in some studies but not others [31]. Prolonged administration of atRA may be of particular importance in cases where atRA inhibits LSCs. On the other hand, in AML with aberrations rendering their LSCs positively responsive to atRA, there might even be a therapeutic role for RAR antagonists, even though the effects of atRA on normal HSCs [49,50,51,52] need to be carefully considered in this context. Other aspects concerning the identity of the retinoids themselves also warrant attention. Certain synthetic retinoids are resistant to degradation by CYP26 [53], which may increase their clinical effectiveness. Moreover, atRA mediates its effects through different nuclear receptor isoforms that can be targeted by specific agonists and antagonists. Among these isoforms, RARA and RARG were reported to promote myeloid differentiation [21,51,53] and HSC activity [51], respectively. The identity of the isoforms mediating the activity of atRA towards LSCs has been queried only in the context of AML1-ETO, with complex results: only the combination of a RARA and a RARG agonist reproduced the LSC-promoting effects of atRA [21].
Further research is needed to carefully dissect which patient subgroups may benefit from which type of retinoid, and how retinoids can be combined with other drugs to maximize anti-leukemic effects. An enhanced understanding of the effects of retinoids on LSCs may ultimately facilitate the development of precision medicine-based retinoid therapy for certain subgroups of AML.
Acknowledgments
pMYs_FLAG-Evi1_IRES_GFP was kindly provided by Takuro Nakamura, The Cancer Institute, Tokyo. Open Access Funding by the Austrian Science Fund (FWF).
Supplementary Materials
Supplementary materials can be found at https://www.mdpi.com/2227-9059/8/10/385/s1.
Author Contributions
Conceptualization, C.H.N. and R.W.; methodology, C.H.N., A.M.G.; validation, A.M.G.; formal analysis, C.H.N., A.M.G. and G.H.; investigation, C.H.N. and A.M.G.; resources, G.S.V., P.B.S. and R.W.; data curation, C.H.N., G.H. and R.W.; writing—original draft preparation, C.H.N., G.H. and R.W.; writing—review and editing, all authors; visualization, C.H.N. and G.H.; supervision, R.W.; project administration, R.W.; funding acquisition, R.W. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Austrian Science Fund (FWF), project P-28256 to RW.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Almeida A., Ramos F. Acute myeloid leukemia in the older adults. Leuk. Res. Rep. 2016;6:1–7. doi: 10.1016/j.lrr.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sanford D., Ravandi F. Management of Newly Diagnosed Acute Myeloid Leukemia in the Elderly: Current Strategies and Future Directions. Drugs Aging. 2015;32:983–997. doi: 10.1007/s40266-015-0309-2. [DOI] [PubMed] [Google Scholar]
- 3.Lawrence M., Stojanov P., Polak P., Kryukov G., Cibulskis K., Sivachenko A., Carter S., Stewart C., Mermel C., Roberts S., et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature. 2013;499:214–218. doi: 10.1038/nature12213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Network C.G.A.R. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N. Engl. J. Med. 2013;368:2059–2074. doi: 10.1056/NEJMoa1301689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grimwade D., Ivey A., Huntly B. Molecular landscape of acute myeloid leukemia in younger adults and its clinical relevance. Blood. 2016;127:29–41. doi: 10.1182/blood-2015-07-604496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Papaemmanuil E., Gerstung M., Bullinger L., Gaidzik V., Paschka P., Roberts N., Potter N., Heuser M., Thol F., Bolli N., et al. Genomic Classification and Prognosis in Acute Myeloid Leukemia. N. Engl. J. Med. 2016;374:2209–2221. doi: 10.1056/NEJMoa1516192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ng S., Mitchell A., Kennedy J., Chen W., McLeod J., Ibrahimova N., Arruda A., Popescu A., Gupta V., Schimmer A., et al. A 17-gene stemness score for rapid determination of risk in acute leukaemia. Nature. 2016;540:433–437. doi: 10.1038/nature20598. [DOI] [PubMed] [Google Scholar]
- 8.Hackl H., Astanina K., Wieser R. Molecular and genetic alterations associated with therapy resistance and relapse of acute myeloid leukemia. J. Hematol. Oncol. 2017;10:51. doi: 10.1186/s13045-017-0416-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gough S., Slape C., Aplan P. NUP98 gene fusions and hematopoietic malignancies: Common themes and new biologic insights. Blood. 2011;118:6247–6257. doi: 10.1182/blood-2011-07-328880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meyer C., Hofmann J., Burmeister T., Groger D., Park T., Emerenciano M., Pombo de Oliveira M., Renneville A., Villarese P., Macintyre E., et al. The MLL recombinome of acute leukemias in 2013. Leukemia. 2013;27:2165–2176. doi: 10.1038/leu.2013.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wieser R. The oncogene and developmental regulator EVI1: Expression, biochemical properties, and biological functions. Gene. 2007;396:346–357. doi: 10.1016/j.gene.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 12.Haas K., Kundi M., Sperr W., Esterbauer H., Ludwig W., Ratei R., Koller E., Gruener H., Sauerland C., Fonatsch C., et al. Expression and prognostic significance of different mRNA 5’-end variants of the oncogene EVI1 in 266 patients with de novo AML: EVI1 and MDS1/EVI1 overexpression both predict short remission duration. Genes Chromosomes Cancer. 2008;47:288–298. doi: 10.1002/gcc.20532. [DOI] [PubMed] [Google Scholar]
- 13.Groschel S., Lugthart S., Schlenk R., Valk P., Eiwen K., Goudswaard C., van Putten W., Kayser S., Verdonck L., Lubbert M., et al. High EVI1 expression predicts outcome in younger adult patients with acute myeloid leukemia and is associated with distinct cytogenetic abnormalities. J. Clin. Oncol. 2010;28:2101–2107. doi: 10.1200/JCO.2009.26.0646. [DOI] [PubMed] [Google Scholar]
- 14.Bohl S., Bullinger L., Rucker F. New Targeted Agents in Acute Myeloid Leukemia: New Hope on the Rise. Int. J. Mol. Sci. 2019;20:1983. doi: 10.3390/ijms20081983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ablain J., de The H. Retinoic acid signaling in cancer: The parable of acute promyelocytic leukemia. Int. J. Cancer. 2014;135:2262–2272. doi: 10.1002/ijc.29081. [DOI] [PubMed] [Google Scholar]
- 16.Testa U., Lo-Coco F. Targeting of leukemia-initiating cells in acute promyelocytic leukemia. Stem Cell Investig. 2015;2:8. doi: 10.3978/j.issn.2306-9759.2015.04.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sanz M., Fenaux P., Tallman M., Estey E., Lowenberg B., Naoe T., Lengfelder E., Dohner H., Burnett A., Chen S., et al. Management of acute promyelocytic leukemia: Updated recommendations from an expert panel of the European LeukemiaNet. Blood. 2019;133:1630–1643. doi: 10.1182/blood-2019-01-894980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lishner M., Curtis J., Minkin S., McCulloch E. Interaction between retinoic acid and cytosine arabinoside affecting the blast cells of acute myeloblastic leukemia. Leukemia. 1989;3:784–788. [PubMed] [Google Scholar]
- 19.Yang G., Minden M., McCulloch E. Regulation by retinoic acid and hydrocortisone of the anthracycline sensitivity of blast cells of acute myeloblastic leukemia. Leukemia. 1994;8:2065–2075. [PubMed] [Google Scholar]
- 20.Heuser M., Argiropoulos B., Kuchenbauer F., Yung E., Piper J., Fung S., Schlenk R., Dohner K., Hinrichsen T., Rudolph C., et al. MN1 overexpression induces acute myeloid leukemia in mice and predicts ATRA resistance in patients with AML. Blood. 2007;110:1639–1647. doi: 10.1182/blood-2007-03-080523. [DOI] [PubMed] [Google Scholar]
- 21.Chee L., Hendy J., Purton L., McArthur G. ATRA and the specific RARalpha agonist, NRX195183, have opposing effects on the clonogenicity of pre-leukemic murine AML1-ETO bone marrow cells. Leukemia. 2013;27:1369–1380. doi: 10.1038/leu.2012.362. [DOI] [PubMed] [Google Scholar]
- 22.Steinmetz B., Hackl H., Slabáková E., Schwarzinger I., Smějová M., Spittler A., Arbesu I., Shehata M., Souček K., Wieser R. The oncogene EVI1 enhances transcriptional and biological responses of human myeloid cells to all-trans retinoic acid. Cell Cycle. 2014;13:2931–2943. doi: 10.4161/15384101.2014.946869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.El Hajj H., Dassouki Z., Berthier C., Raffoux E., Ades L., Legrand O., Hleihel R., Sahin U., Tawil N., Salameh A., et al. Retinoic acid and arsenic trioxide trigger degradation of mutated NPM1, resulting in apoptosis of AML cells. Blood. 2015;125:3447–3454. doi: 10.1182/blood-2014-11-612416. [DOI] [PubMed] [Google Scholar]
- 24.Martelli M., Gionfriddo I., Mezzasoma F., Milano F., Pierangeli S., Mulas F., Pacini R., Tabarrini A., Pettirossi V., Rossi R., et al. Arsenic trioxide and all-trans retinoic acid target NPM1 mutant oncoprotein levels and induce apoptosis in NPM1-mutated AML cells. Blood. 2015;125:3455–3465. doi: 10.1182/blood-2014-11-611459. [DOI] [PubMed] [Google Scholar]
- 25.Boutzen H., Saland E., Larrue C., de Toni F., Gales L., Castelli F., Cathebas M., Zaghdoudi S., Stuani L., Kaoma T., et al. Isocitrate dehydrogenase 1 mutations prime the all-trans retinoic acid myeloid differentiation pathway in acute myeloid leukemia. J. Exp. Med. 2016;213:483–497. doi: 10.1084/jem.20150736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verhagen H., Smit M., Rutten A., Denkers F., Poddighe P., Merle P., Ossenkoppele G., Smit L. Primary acute myeloid leukemia cells with overexpression of EVI-1 are sensitive to all-trans retinoic acid. Blood. 2016;127:458–463. doi: 10.1182/blood-2015-07-653840. [DOI] [PubMed] [Google Scholar]
- 27.Nguyen C., Grandits A., Purton L., Sill H., Wieser R. All-trans retinoic acid in non-promyelocytic acute myeloid leukemia: Driver lesion dependent effects on leukemic stem cells. Cell Cycle. 2020:1–16. doi: 10.1080/15384101.2020.1810402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schlenk R., Frohling S., Hartmann F., Fischer J., Glasmacher A., del Valle F., Grimminger W., Gotze K., Waterhouse C., Schoch R., et al. Phase III study of all-trans retinoic acid in previously untreated patients 61 years or older with acute myeloid leukemia. Leukemia. 2004;18:1798–1803. doi: 10.1038/sj.leu.2403528. [DOI] [PubMed] [Google Scholar]
- 29.Burnett A., Hills R., Green C., Jenkinson S., Koo K., Patel Y., Guy C., Gilkes A., Milligan D., Goldstone A., et al. The impact on outcome of the addition of all-trans retinoic acid to intensive chemotherapy in younger patients with nonacute promyelocytic acute myeloid leukemia: Overall results and results in genotypic subgroups defined by mutations in NPM1, FLT3, and CEBPA. Blood. 2010;115:948–956. doi: 10.1182/blood-2009-08-236588. [DOI] [PubMed] [Google Scholar]
- 30.Schlenk R., Lubbert M., Benner A., Lamparter A., Krauter J., Herr W., Martin H., Salih H., Kundgen A., Horst H., et al. All-trans retinoic acid as adjunct to intensive treatment in younger adult patients with acute myeloid leukemia: Results of the randomized AMLSG 07-04 study. Ann. Hematol. 2016;95:1931–1942. doi: 10.1007/s00277-016-2810-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuley-Bagheri Y., Kreuzer K., Monsef I., Lubbert M., Skoetz N. Effects of all-trans retinoic acid (ATRA) in addition to chemotherapy for adults with acute myeloid leukaemia (AML) (non-acute promyelocytic leukaemia (non-APL)) Cochrane Database Syst. Rev. 2018;8:CD011960. doi: 10.1002/14651858.CD011960.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schlenk R., Dohner K., Kneba M., Gotze K., Hartmann F., Del Valle F., Kirchen H., Koller E., Fischer J., Bullinger L., et al. Gene mutations and response to treatment with all-trans retinoic acid in elderly patients with acute myeloid leukemia. Results from the AMLSG Trial AML HD98B. Haematologica. 2009;94:54–60. doi: 10.3324/haematol.13378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stahl M., Kim T., Zeidan A. Update on acute myeloid leukemia stem cells: New discoveries and therapeutic opportunities. World J. Stem Cells. 2016;8:316–331. doi: 10.4252/wjsc.v8.i10.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haas S., Trumpp A., Milsom M. Causes and Consequences of Hematopoietic Stem Cell Heterogeneity. Cell Stem Cell. 2018;22:627–638. doi: 10.1016/j.stem.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 35.Pinho S., Frenette P. Haematopoietic stem cell activity and interactions with the niche. Nat. Rev. Mol. Cell. Biol. 2019;20:303–320. doi: 10.1038/s41580-019-0103-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ma H., Greenblatt S., Shirley C., Duffield A., Bruner J., Li L., Nguyen B., Jung E., Aplan P., Ghiaur G., et al. All-trans retinoic acid synergizes with FLT3 inhibition to eliminate FLT3/ITD+ leukemia stem cells in vitro and in vivo. Blood. 2016;127:2867–2878. doi: 10.1182/blood-2015-05-646786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nguyen C., Bauer K., Hackl H., Schlerka A., Koller E., Hladik A., Stoiber D., Zuber J., Staber P., Hoelbl-Kovacic A., et al. All-trans retinoic acid enhances, and a pan-RAR antagonist counteracts, the stem cell promoting activity of EVI1 in acute myeloid leukemia. Cell Death Dis. 2019;10:944. doi: 10.1038/s41419-019-2172-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mupo A., Celani L., Dovey O., Cooper J., Grove C., Rad R., Sportoletti P., Falini B., Bradley A., Vassiliou G. A powerful molecular synergy between mutant Nucleophosmin and Flt3-ITD drives acute myeloid leukemia in mice. Leukemia. 2013;27:1917–1920. doi: 10.1038/leu.2013.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Livak K., Schmittgen T. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 40.Metzeler K., Hummel M., Bloomfield C., Spiekermann K., Braess J., Sauerland M., Heinecke A., Radmacher M., Marcucci G., Whitman S., et al. An 86-probe-set gene-expression signature predicts survival in cytogenetically normal acute myeloid leukemia. Blood. 2008;112:4193–4201. doi: 10.1182/blood-2008-02-134411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jin G., Yamazaki Y., Takuwa M., Takahara T., Kaneko K., Kuwata T., Miyata S., Nakamura T. Trib1 and Evi1 cooperate with Hoxa and Meis1 in myeloid leukemogenesis. Blood. 2007;109:3998–4005. doi: 10.1182/blood-2006-08-041202. [DOI] [PubMed] [Google Scholar]
- 42.Watanabe-Okochi N., Yoshimi A., Sato T., Ikeda T., Kumano K., Taoka K., Satoh Y., Shinohara A., Tsuruta T., Masuda A., et al. The shortest isoform of C/EBPbeta, liver inhibitory protein (LIP), collaborates with Evi1 to induce AML in a mouse BMT model. Blood. 2013;121:4142–4155. doi: 10.1182/blood-2011-07-368654. [DOI] [PubMed] [Google Scholar]
- 43.Lubbert M., Grishina O., Schmoor C., Schlenk R., Jost E., Crysandt M., Heuser M., Thol F., Salih H., Schittenhelm M., et al. Valproate and Retinoic Acid in Combination With Decitabine in Elderly Nonfit Patients With Acute Myeloid Leukemia: Results of a Multicenter, Randomized, 2 × 2, Phase II Trial. J. Clin. Oncol. 2020;38:257–270. doi: 10.1200/JCO.19.01053. [DOI] [PubMed] [Google Scholar]
- 44.Wass M., Gollner S., Besenbeck B., Schlenk R., Mundmann P., Gothert J., Noppeney R., Schliemann C., Mikesch J., Lenz G., et al. A proof of concept phase I/II pilot trial of LSD1 inhibition by tranylcypromine combined with ATRA in refractory/relapsed AML patients not eligible for intensive therapy. Leukemia. 2020:1–11. doi: 10.1038/s41375-020-0892-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bindels E., Havermans M., Lugthart S., Erpelinck C., Wocjtowicz E., Krivtsov A., Rombouts E., Armstrong S., Taskesen E., Haanstra J., et al. EVI1 is critical for the pathogenesis of a subset of MLL-AF9-rearranged AMLs. Blood. 2012;119:5838–5849. doi: 10.1182/blood-2011-11-393827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Groschel S., Schlenk R., Engelmann J., Rockova V., Teleanu V., Kuhn M., Eiwen K., Erpelinck C., Havermans M., Lubbert M., et al. Deregulated expression of EVI1 defines a poor prognostic subset of MLL-rearranged acute myeloid leukemias: A study of the German-Austrian Acute Myeloid Leukemia Study Group and the Dutch-Belgian-Swiss HOVON/SAKK Cooperative Group. J. Clin. Oncol. 2013;31:95–103. doi: 10.1200/JCO.2011.41.5505. [DOI] [PubMed] [Google Scholar]
- 47.Krivtsov A., Figueroa M., Sinha A., Stubbs M., Feng Z., Valk P., Delwel R., Dohner K., Bullinger L., Kung A., et al. Cell of origin determines clinically relevant subtypes of MLL-rearranged AML. Leukemia. 2013;27:852–860. doi: 10.1038/leu.2012.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Esnault C., Rahme R., Rice K., Berthier C., Gaillard C., Quentin S., Maubert A., Kogan S., de The H. FLT3-ITD impedes retinoic acid, but not arsenic, responses in murine acute promyelocytic leukemias. Blood. 2019;133:1495–1506. doi: 10.1182/blood-2018-07-866095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Purton L., Bernstein I., Collins S. All-trans retinoic acid delays the differentiation of primitive hematopoietic precursors (lin(−)c-kit(+)Sca-1(+)) while enhancing the terminal maturation of committed granulocyte monocyte progenitors. Blood. 1999;94:483–495. doi: 10.1182/blood.V94.2.483. [DOI] [PubMed] [Google Scholar]
- 50.Purton L., Bernstein I., Collins S. All-trans retinoic acid enhances the long-term repopulating activity of cultured hematopoietic stem cells. Blood. 2000;95:470–477. doi: 10.1182/blood.V95.2.470. [DOI] [PubMed] [Google Scholar]
- 51.Purton L., Dworkin S., Olsen G., Walkley C., Fabb S., Collins S., Chambon P. RARgamma is critical for maintaining a balance between hematopoietic stem cell self-renewal and differentiation. J. Exp. Med. 2006;203:1283–1293. doi: 10.1084/jem.20052105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cabezas-Wallscheid N., Buettner F., Sommerkamp P., Klimmeck D., Ladel L., Thalheimer F., Pastor-Flores D., Roma L., Renders S., Zeisberger P., et al. Vitamin A-Retinoic Acid Signaling Regulates Hematopoietic Stem Cell Dormancy. Cell. 2017;169:807–823.e819. doi: 10.1016/j.cell.2017.04.018. [DOI] [PubMed] [Google Scholar]
- 53.Hernandez D., Palau L., Norsworthy K., Anders N., Alonso S., Su M., Petkovich M., Chandraratna R., Rudek M., Smith B., et al. Overcoming microenvironment-mediated protection from ATRA using CYP26-resistant retinoids. Leukemia. 2020:1–5. doi: 10.1038/s41375-020-0790-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.