Abstract
Simple Summary
A growing number of studies suggest that cancer-associated fibroblasts (CAFs) modulate both myeloid and lymphoid cells through secretion of molecules (i.e., chemical function) and production of the extracellular matrix (ECM), i.e., physical function. Even though targeting functions CAFs is a relevant strategy, published clinical trials solely aimed at targeting the stroma showed disappointing results, despite being based on solid preclinical evidence. Our review dissects the interactions between CAFs and immune cells and explains how a deeper understanding of CAF subpopulations is the cornerstone to propose relevant therapies that will ultimately improve survival of patients with cancer.
Abstract
Cancer-associated fibroblasts (CAFs) are prominent cells within the tumor microenvironment, by communicating with other cells within the tumor and by secreting the extracellular matrix components. The discovery of the immunogenic role of CAFs has made their study particularly attractive due to the potential applications in the field of cancer immunotherapy. Indeed, CAFs are highly involved in tumor immune evasion by physically impeding the immune system and interacting with both myeloid and lymphoid cells. However, CAFs do not represent a single cell entity but are divided into several subtypes with different functions that may be antagonistic. Considering that CAFs are orchestrators of the tumor microenvironment and modulate immune cells, targeting their functions may be a promising strategy. In this review, we provide an overview of (i) the mechanisms involved in immune regulation by CAFs and (ii) the therapeutic applications of CAFs modulation to improve the antitumor immune response and the efficacy of immunotherapy.
Keywords: cancer-associated fibroblasts, immunology, tumor microenvironment, cell communication
1. Introduction
Control and elimination of tumor cells by the immune system (also known as immunosurveillance) is a defense system that plays a major role in the prevention of cancers [1]. However, tumor growth in immunocompetent patients indicates that antitumor immunity can be dodged and no longer fulfill its full role. Indeed, modulating immunity toward tumor tolerance and evading the immune system are hallmarks of cancer [2,3].
The tumor microenvironment (TME) is actively involved in immune evasion leading to cancer progression and metastasis [4]. This compartment comprises several cell types, in addition to tumor cells, including pericytes, endothelial cells (venous, arterial and lymphatic), immune cells, nerve cells, adipocytes and cancer-associated fibroblasts (CAFs). CAFs are the most abundant cell type within the TME and play prominent roles by communicating with other cells and by secreting the extracellular matrix (ECM) components [5]. Similar to other cell types, recent studies have revealed that CAFs count multiple subpopulations with different functions [6]. This heterogeneity can be partially explained by the diverse origins of CAFs, ranging from local precursors including fibroblasts [5], pericytes [7], adipocytes [8], epithelial (epithelial-to-mesenchymal transition) [9] and endothelial cells (endothelial-to-mesenchymal transition) [10], to distant precursors such as bone marrow-derived mesenchymal cells [11] and circulating fibrocytes [12]. In noncancerous conditions, resident tissue fibroblasts are quiescent cells acting as sentinels and maintaining tissue homeostasis.
Upon tissue injury, such as in wound healing or in cancer, they differentiate into myofibroblasts (i.e., activated fibroblasts) to repair damaged tissue by secreting the ECM and by interacting with immune cells [13]. These functions are rewired by tumor cells, making CAFs their accomplices [5]. The discovery of the immunogenic role of CAFs has made their study particularly attractive due to potential applications in the field of cancer immunotherapy. A growing number of studies suggest that CAFs modulate both myeloid and lymphoid cells through secretion of molecules (i.e., chemical function) and production of ECM (i.e., physical function). In this review, we provide an overview of (i) the mechanisms involved in the immune regulation by CAFs, and (ii) the therapeutic applications of CAFs modulation to improve the antitumor immune response and the efficacy of immunotherapy.
2. CAFs Constitute A Chemical Immune Barrier
Once activated, CAFs produce several molecules to interact with immune cells, such as growth factors and cytokines [5]. Through these secretions, CAFs affect recruitment and characteristics of both myeloid (Table 1) and lymphoid cells (Table 2) to build a chemical immune barrier and, therefore, create an immunosuppressive TME favorable for cancer progression. CAFs activation is then perpetuated by immune cells through positive feedback loops. Among the cytokines that play a central role in the activation of fibroblasts, transforming growth factor β (TGFβ) is one of the most important [14]. The positive-feedback loop between CAFs and immune cells through TGFβ is well established; both CAFs and immune cells have the ability to secrete and respond to TGFβ [15].
Table 1.
Summary of studies evaluating modulation of myeloid cells by CAFs 1.
| Myeloid Cells | Effect | CAF-Secreted Molecules | Cancer Type | Study |
|---|---|---|---|---|
| TAM | Recruitment Reprogramming to an M2-like phenotype | Chi3L1 | Breast | Cohen et al. [16] |
| Recruitment | CCL2 | Lymphoma | Ren et al. [17] | |
| Recruitment | NA | Pancreas | Gunderson et al. [18] | |
| Recruitment | CCL2 | Breast | Jia et al. [19] | |
| Recruitment | CCL2 | Breast | Ksiazkiewicz et al. [20] | |
| Recruitment Reprogramming to an M2-like phenotype | CXCL12 | Prostate | Comito et al. [21] | |
| Reprogramming to an M2-like phenotype | IL-6 and IL-10 | Pancreas | Mathew et al. [22] | |
| Recruitment | NA | Breast | Liao et al. [23] | |
| MDSC | Recruitment | CCL2 | Colorectal | Chen et al. [24] |
| Recruitment | IL-6 | Skin (squamous) | Ruhland et al. [25] | |
| Recruitment | CCL2 | Biliary tract | Yang et al. [26] | |
| Recruitment | CXCL1 | Lung, colon, melanoma, breast, pancreas, thymoma | Kumar et al. [27] | |
| Recruitment | NA | Breast | Liao et al. [23] | |
| Recruitment Differentiation | CXCL12 | Liver | Deng et al. [28] | |
| Differentiation | IL-6, VEGF, M-CSF, CXCL12 and CCL2 | Pancreas | Mace et al. [29] | |
| DC | Recruitment | NA | Breast | Liao et al. [23] |
| Induction of regulatory DC | IL-6 | Liver | Cheng et al. [30] | |
| Inhibition of differentiation | Kynurenine | Lung | Hsu et al. [31] | |
| Induction of DC promoting Th2 polarization | TSLP | Pancreas | De Monte et al. [32] | |
| TAN | Recruitment | CCL2 | Lymphoma | Ren et al. [17] |
| Recruitment, survival and activation | CXCL12 and IL-6 | Liver | Cheng et al. [33] | |
| Recruitment | CXCL1, CXCL2 and CXCL5 | Breast | Yu et al. [34] | |
| Mast cells | Recruitment | CXCL12 | Prostate | Ellem et al. [35] |
1 CAF: cancer-associated-fibroblast. CCL: chemokine-ligand. CXCL: C-X-C motif chemokine. DC: dendritic cells. IL: interleukin. M-CSF: macrophage colony-stimulating factor. MDSC: myeloid-derived suppressor cells. NA: not available. TAM: tumor-associated macrophages. TAN: tumor-associated neutrophils. TSLP: thymic stromal lymphopoietin. VEGF: vascular endothelial growth factor.
Table 2.
Summary of studies evaluating modulation of lymphoid cells by cancer-associated fibroblasts 1.
| Lymphoid Cells | Effect | CAF-Induced Mechanism | Cancer Type | Study |
|---|---|---|---|---|
| CTL | Exclusion | Chi3L1 secretion | Breast | Cohen et al. [16] |
| Inhibition of cytotoxicity | MDSC recruitment | Colorectal | Chen et al. [24] | |
| Inhibition of cytotoxicity and activation | MDSC recruitment | Skin (squamous) | Ruhland et al. [25] | |
| Exclusion | NA | Breast | Liao et al. [23] | |
| Inhibition of cytotoxicity | IDO-producing regulatory DC | Liver | Cheng et al. [30] | |
| Inhibition of proliferation | MDSC differentiation | Pancreas | Mace et al. [29,36] | |
| Exclusion | CXCL12 secretion | Pancreas | Feig et al. [37] | |
| Exclusion | TGFβ secretion | Urothelial | Mariathasan et al. [38] | |
| Exclusion | TGFβ secretion | Colon | Tauriello et al. [39] | |
| Exclusion | βig-h3 stromal protein | Pancreas | Goehrig et al. [40] | |
| Killing Exclusion | PD-L2 and FASL expression | Lung and melanoma | Lakins et al. [41] | |
| Inhibition of proliferation | NO secretion | Breast | Cremasco et al. [42] | |
| Inhibition of proliferation, activation and cytotoxicity | Production of adenosine | Cervical | De Lourdes Mora-García et al. [43] | |
| Helper T lymphocytes | Promotion of Th2 phenotype | Chi3L1 secretion | Breast | Cohen et al. [16] |
| Promotion of Th2 phenotype | NA | Breast | Liao et al. [23] | |
| Promotion of Th2 phenotype | DC secretion of Th2 chemokines | Pancreas | De Monte et al. [32] | |
| Treg | Recruitment | MDSC recruitment | Skin (squamous) | Ruhland et al. [25] |
| Recruitment | NA | Breast | Liao et al. [23] | |
| Expansion | IDO-producing regulatory DC | Liver | Cheng et al. [30] | |
| Recruitment Retention Differentiation |
CXCL12 (recruitment) OX-40L, PD-L2, JAM2 (retention) B7H3, CD73, DPP4 (differentiation) |
Breast | Costa et al. [44] | |
| Recruitment, survival and differentiation | CXCL12 secretion | Ovary | Givel et al. [45] | |
| NK cells | Inhibition of cytotoxicity and cytokine production | PGE2 secretion | Melanoma | Balsamo et al. [46] |
| Inhibition of cytotoxicity and cytokine production | PGE2 and IDO secretion | Liver | Li et al. [47] |
1 Abbreviations. CAF: cancer-associated-fibroblast. CCL: chemokine-ligand. CXCL: C-X-C motif chemokine. CTL: cytotoxic T lymphocytes. DC: dendritic cells. JAM2: Junctional Adhesion Molecule 2. IDO: indoleamine 2,3-dioxygenase. MDSC: myeloid-derived suppressor cells. TGF: transforming growth factor β. PD-L2: Programmed death-ligand 2. PGE2: prostaglandin E2. VEGF: vascular endothelial growth.
2.1. Myeloid Cells
2.1.1. Tumor-Associated Macrophages (TAMs)
TAMs comprise different subpopulations with distinct functionalities and derive from circulating monocytes or resident tissue macrophages. CAFs enrich the TME with TAMs by promoting monocytes precursors recruitment. In 2012, Ren, et al. showed that mesenchymal stromal cells from lymphoma, one of the precursors for CAFs, led to the intratumoral accumulation of CD11b+Ly6C+circulating monocytes by secreting chemokine-ligand 2 (CCL2) [17]. This chemokine binds to C-C chemokine receptor type 2 (CCR2) on monocytes and macrophages and attracts them to the tumor. Other preclinical studies suggested involvement of the CCR2-chemokine axis to TAM recruitment in breast cancer [19,20]. Once TAMs infiltrate tumor tissue, CAFs are able to differentiate them toward an M2-like phenotype. This phenotype is characterized by the promotion of Th2-type immune responses, angiogenesis and the inhibition of cytotoxic T lymphocytes (CTL) that lead to immune suppression and support cancer progression [48]. M2 differentiation is induced by CAF-secreted molecules such as Chitinase 3 Like 1 (Chi3L1), C-X-C motif chemokine 12 (CXCL12) and interleukin 6 (IL-6) in breast [16], prostate [21] and pancreatic cancers [22], respectively. Conversely, M1 differentiation is characterized by promotion of Th1-type immune responses and CTL activation. An increased M1/M2 ratio in cancer tissue is associated with a prolonged overall survival (OS) in cervical, ovarian and gastric cancers, and in lymphoma and myeloma [49].
2.1.2. Myeloid-Derived Suppressor Cells (MDSCs)
MDSCs are immature myeloid cells that are only present in pathological conditions associated with chronic inflammation. In the case of cancer, they exert an immunosuppressive function by inhibiting T cell functions and promoting carcinogenesis [50]. Like TAMs, they are recruited by CAFs within the TME through the CCR2-chemokine axis as illustrated by Yang et al. [26] in the example of intrahepatic cholangiocarcinoma. Fibroblast activation protein (FAP) expression by CAFs activates fibroblastic STAT3 signaling leading to CCL2 secretion. Similar results were observed in colorectal and pancreatic cancers [24,29]. Other studies described additional mechanisms of the recruitment of MDSCs by CAFs involving the CXCL1 chemokine, followed by differentiation by CXCL12, IL-6, vascular endothelial growth factor (VEGF) and macrophage colony-stimulating factor (M-CSF) [28,29]. A single-cell RNA sequencing study conducted in prostate cancer demonstrated that different clusters of CAFs secreted various levels of proinflammatory cytokines such as CXCL12 and CCL2, highlighting that several CAF subpopulations may interact with MDSCs [51].
2.1.3. Dendritic Cells (DCs)
The CTL antitumoral response requires the recognition of tumor epitopes presented by antigen presenting cells (APCs). APCs ingest tumor antigens and process them for presentation to T cells. Further, the activation of naive CD8+ T cells, leading to their proliferation and differentiation, also requires a costimulation signal in addition to antigen recognition. Once activated, tumor antigen-specific T cells are able to recognize and destroy pathologic cells presenting the same epitope. Tumor cells express major histocompatibility complex (MHC) class I molecules but often do not express costimulatory molecules. DCs can recognize antigens from a cell (e.g., tumoral) and activate another cell (e.g., CTL); this is called cross-priming [52]. DC modulation is a therapeutic avenue actively explored in immune-oncology [53]. CAFs can hijack DCs by recruiting them and deflect their function [23]. Indeed, De Monte, et al. [32] showed that pancreatic CAFs secreted thymic stromal lymphopoietin (TSLP) that conditioned myeloid DCs toward promotion of the protumorigenic Th2 response. CAFs modulate DCs to create an immunosuppressive TME through other mechanisms such as induction of regulatory hepatic DCs or inhibition of lung DC differentiation by IL-6 [30] and kynurenine secretion [31], respectively.
2.1.4. Tumor-Associated Neutrophils (TANs)
TANs are associated with poor prognosis in several cancer types, including melanoma, renal, pancreatic, colorectal and gastric cancers [54]. Like TAMs, TANs can be roughly separated into two polarized populations: antitumorigenic N1 TANs, which are cytotoxic against tumoral cells, and protumorigenic N2 TANs, inhibiting CTL functions [55]. The interactions between CAFs and N2 TANs have not been explored yet, but studies in liver [33] and breast cancers [34] showed that CAFs recruit TANs using the same molecules as those involved in M2-reprogramming (i.e., CCL2, CXCL12 and IL-6).
2.1.5. Mast Cells
Mast cells are tissue-resident quiescent cells acting as sentinels, releasing cytokines and chemokines when activated. They play an immunosuppressive role in the TME by secreting free adenosine and IL-13 that, respectively, inhibit CTL and activate M2 polarization, as well as promoting MDSCs and regulatory T cells (Tregs). Ellem, et al. [35] described that estrogen-activated prostatic CAFs secrete CXCL12 to recruit mast cells in a CXCR4-dependent manner.
2.2. Lymphoid Cells
2.2.1. Cytotoxic T Lymphocytes (CTLs)
The main immune mechanism of tumor eradication is driven by CTLs specific for tumor antigens. Indeed, a strong intra-tumoral infiltration by CD3+/CD8+ CTLs, and CD45RO+ memory T lymphocytes is correlated with longer OS in most cancers [56]. Several studies have shown that CAFs are able to inhibit CTLs, either directly or indirectly. For example, Lakins et al. [41] showed that CAFs could kill and exclude CTLs from the TME by expressing programmed death ligand 2 (PD-L2) and Fas ligand in immunogenic tumors such as lung and melanoma. CTL exclusion is also promoted by the secretion of CXCL12 [37], TGFβ [38,39] and βig-h3 stromal protein [40] by CAFs. Moreover, CAFs can inhibit CTL cytotoxic activity and proliferation by producing immunosuppressive molecules such as nitric oxide [42] and adenosine [43] or by recruiting immunosuppressing cells such as MDSCs [24,25,29] or regulatory DCs [30].
2.2.2. Helper T Lymphocytes
As mentioned above, an enrichment in cytotoxic and memory T-lymphocytes is associated with a favorable prognosis. This infiltration is associated with a Th1-type immune orientation of CD4+ T lymphocytes involving T-bet, STAT-1 and IRF1 transcription factors leading to the local production of IL-12 and interferon γ. In order to counteract this antitumor immune phenotype, CAFs promote a Th2 orientation, mutually exclusive of Th1, leading to the secretion of the immunosuppressive IL-10 cytokine. This Th2 phenotype can be induced either by CAF-secreting Chi3L1, or by orientating DCs to secrete Th2 chemokines, such as IL-13, in breast [16] and pancreatic cancers [32], respectively. Another CAF subset was recently discovered with the ability to present antigens to CD4+ T cells by expression of the MHC class II [57]. However, the absence of costimulatory molecules deactivates CD4+ T cells and decreases the CD8+ T cells/Tregs ratio [57] thus inhibiting the antitumor response.
2.2.3. Regulatory T Cells (Tregs)
Tregs are CD4+ T cells whose function is to inhibit or attenuate immune responses. Most of Tregs strongly express CD25 (alpha chain of the IL-25 receptor) and the transcription factor FoxP3. The prognostic value associated with a high Treg density within the tumor is controversial [58]. A negative prognostic value has been described in pancreatic [59], ovarian [60], liver [61] and breast cancers [62], whereas a positive prognostic value has been observed in lymphomas [63], head and neck [64] and colorectal cancers [65]. There are many reasons for these conflicting observations, such as an insufficiently in-depth analysis of this population requiring consideration of their functionality and subpopulations; hence, FoxP3 expression is not limited to Tregs [66] and Tregs may lose FoxP3 expression [67]. Besides, the favorable prognosis associated with Treg infiltrates may be due to the concomitant presence of effector T cells. As CTLs, Tregs can be recruited and expanded by CAFs either directly by CXCL12, OX40L, PD-L2, and JAM2 expression [44,45], or indirectly through MDSCs and regulatory DCs recruitment [25,30]. A recent study by Kieffer et al. [68] used a single-cell RNA sequencing approach to analyze intratumoral heterogeneity and showed that FAP+ CAFs with an ECM signature drive immunosuppression in several cancer types by recruiting Tregs.
2.2.4. Natural Killer Cells (NK Cells)
NK cells, or type I innate lymphoid cells, are lymphocytes belonging to innate immunity and do not express antigen receptors clonally synthesized by B and T lymphocytes. NK cells exert an antitumor activity by secreting pro-Th1 cytokines or by directly killing tumoral cells through the release of cytotoxic granules containing perforins and granzymes [69]. Previous studies showed that a high cytotoxic activity of NK cells correlated with a prolonged OS in head and neck cancers [70] while a decrease in the cytotoxic activity was associated with shorter OS and the occurrence of metastases in gastric [71], liver [72] and colorectal cancers [73]. The study of tumoral NK cells revealed functional and phenotypic alterations, such as reduced cytotoxicity, decreased production of antitumoral IFNγ and tumor necrosis factor α (TNFα) cytokines, and low expression of activating receptors [74]. CAFs are responsible for these functional defects by secreting prostaglandin E2 (PGE2) and indoleamine 2,3-dioxygenase (IDO) in melanoma [46] and hepatocellular carcinoma [47].
3. CAFs Constitute a Physical Immune Barrier
CAFs secrete excess deposits of collagenous and noncollagenous ECM along with degradation enzymes that promote metastasis and cancer progression [75]. Besides the direct effect on cancer cells [76], ECM-remodeling also contributes to modulation of immune cells by creating a physical immune barrier. Indeed, mouse models of pancreatic adenocarcinoma have shown that T cells lose their ability to infiltrate the tumor area when the ECM density is high [77]. Enriched type I collagen ECM activates the expression of leucocyte inhibitory receptors such as LAIR-1 and decreases T cell infiltration [78]. In the ECM of melanoma, the loss of HAPLN1 secretion (hyaluronic protein) by aged fibroblasts induces protumorigenic effects by inhibiting T cell motility while increasing that of polymorphonuclear immune cells, which, in turn, recruit Tregs [79]. Furthermore, ECM stiffness may also impact the innate immunity. Preclinical studies suggest that macrophage polarization and migration is affected by the ECM physical properties [80]. ECM alterations in cancer, such as increased stiffness, type I collagen and hyaluronan, promote infiltration of motile M2 macrophages [81,82,83]. In addition to ECM stiffness and composition, Salmon et al. showed that the fibers’ orientation controls the migration of T cells so that aligned fibers around vascular and tumoral regions exclude T cells from lung tumor islets [84]. Besides, the recruitment of immunosuppressive innate immune cells by the ECM can also result from indirect interactions. For example, the high-density of the ECM in breast and pancreatic cancers activates tumor cells and CAFs that secrete the monocyte cytokines CCL2 and colony-stimulating factor 1 (CSF-1) [85,86].
Finally, CAF-induced fibrosis generates a high interstitial pressure leading to a poorly vascularized, hypoxic TME, which constrains access to cell nutrients and, thus, cellular phenotype and metabolism. Moreover, a positive-feedback loop exists since fibrosis is enhanced in hypoxic regions [87]. Indeed, hypoxia activates CAFs to secrete type I collagen (i.e., immune physical barrier) and immunosuppressive cytokines such as IL-12 and CXCL12 (i.e., immune chemical barrier) [88]. Besides, activation of hypoxia-inducible factor-1α (HIF-1α) by hypoxia plays a central role in creating an immunosuppressive TME. First, HIF-1α upregulates the expression of PD-L1 by MDSCs, macrophages, DCs, and tumor cells, thereby promoting T cell inactivation through the PD-1/PD-L1 axis [89]. Secondly, HIF-1α impacts T cell activity by increasing NF-κB activation, which decreases the transduction of the cell receptor (TCR) signal [90]. Thirdly, hypoxia triggers the CD39 and CD73 ectonucleotidases, generating extracellular formation of immunosuppressive adenosine [91]. Furthermore, there is a positive-feedback loop between recruited immunosuppressive macrophages and CAFs, with macrophages activating CAFs by granulin secretion [86,92]. Overall, the CAFs-induced ECM constitutes a physical immune barrier by impeding both adaptive and innate immunity directly through mechanical forces or indirectly by promoting an immunosuppressive hypoxic microenvironment.
4. Good Cop CAFs: Looking for A Needle in A Haystack
The literature predominantly supports the tumor-promoting role of CAFs, but there is also evidence that some CAF subsets restrain tumor activity. This is particularly important because therapeutic ablation of antitumoral CAFs can be deleterious. Indeed, nonspecific depletion of α-SMA+ myofibroblasts and SHH-dependent CAFs in pancreatic cancer generated more aggressive tumors (poorly differentiated, more vascularized and infiltrated by Tregs) worsening patient survival [93,94,95]. Current CAFs markers such as α-SMA, vimentin, FAP, platelet-derived growth factor receptor α (PDGFRα) and FSP1 are nonexclusive for fibroblasts and expressed across multiple CAFs subtypes [96]. Several studies in many cancer types deciphered CAFs subsets according to their phenotype and function in order to target appropriate subpopulations and ultimately sensitize tumors to systemic therapies (i.e., immunotherapies and chemotherapies) [44,97].
Identifying tumor-restraining CAFs is not an easy task. First, studies can be conflicting regarding the same marker. As an example, podoplanin-expressing CAFs were shown to be associated with good prognoses in breast [98] and colon cancers [99] but the opposite finding was reported in breast [100,101,102] and lung cancers [103,104]. Secondly, the impact of CAFs on tumor cells varies according to the cancer type. Haro et al. highlighted that a stromal signature representing CAFs and ECM components was predictive of good survival in B lymphomas and decreased survival in carcinomas [105]. The authors supported the hypothesis that the immune suppressive functions of CAFs, notably on B cells through the TGF-β pathway, disrupted tumorigenesis in B lymphomas while promoting cancer progression in carcinomas. Similarly, hedgehog-signaling CAFs are associated with reduced colon cancer progression [106] but act as enhancers of pancreatic cancer progression [107,108].
To date, the exact phenotypes of good tumor-restraining CAFs remains unknown. Some studies suggested that normal quiescent fibroblasts resistant to activation may suppress tumorigenesis and metastasis [109,110,111]. Other studies showed the presence of active antitumor CAFs that can directly act on tumor cells by inhibiting their growth and phenotype transformation [109,112,113]. Several single cell RNA sequencing studies have uncovered CAF heterogeneity in pancreatic [97,114,115,116], head and neck [117], breast [118,119], lung [120], colorectal [121] cancers and melanoma [122]. However, CAF functionality hypothesized from the transcriptomic profiles requires further experimental validations. Indeed, there is a need to functionally assess and validate CAF functions in vitro and in vivo, but this is challenging since isolating and growing pure subpopulations of CAFs without disturbing their functionality is challenging [123].
5. Therapeutic Implications
It is now acknowledged that increasing tumor immunogenicity is relevant to induce cancer regression and prolonged survival in cancer patients [124]. Considering that CAFs are TME orchestrators and modulate immune cells, targeting their functions may be a promising strategy. As depleting all CAFs is harmful, identifying and selectively targeting the deleterious pathways and subpopulations remains the main avenue of research. However, this is a hard task since cells within the TME interact with each other in a complex network. Here, we will develop current strategies aimed at modulating CAF functions to improve tumor immunogenicity. Since fibrosis is an immune physical barrier, desmoplasia depletion may sensitize tumor cells to immune attack and several strategies are underway to achieve this goal (Figure 1).
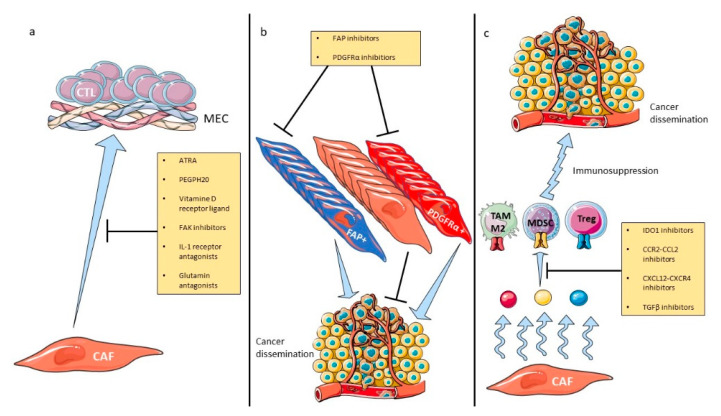
Figure 1.
Therapeutic strategies modulating CAF activities. CAF-related drugs, with or without ICI combination, inhibit fibrosis (a), CAF-protumoral subsets (b) or CAF-secreted immunosuppressive molecules (c). Abbreviations: CAF: cancer-associated fibroblasts, CCL2: chemokine-ligand 2, CCR2: C-C chemokine receptor type 2, CXCL12: C-X-C motif chemokine 12, CXCR4: C-X-C motif chemokine receptor 4, ECM: extracellular matrix, FAK: focal adhesion kinase, FAP: fibroblast activation protein, ICI: immune checkpoint inhibitors, IDO1: indoleamine 2,3-dioxygenase 1, MDSC: myeloid-derived suppressor cells, PDGFRα: platelet-derived growth factor receptor α, TAM: tumor-associated macrophage, TGFβ: transforming growth factor β, Treg: regulatory lymphocyte.
The first strategy is to reduce ECM production. The clinical use of all-trans retinoic acid (ATRA) is well established in acute promyelocytic leukemia for its differentiating effect. ATRA has also been associated with ECM suppression and pancreatic stellate cells (pancreatic resident fibroblasts) inhibition (i.e., quiescence induction) [125]. ATRA is currently explored in early phase trials in melanoma, pancreatic, breast and prostate cancers in combination with other drugs including immune therapies (NCT04241276, NCT04113863, NCT03572387, NCT02403778). Similarly, vitamin D receptors are major transcriptional factors to get pancreatic stellate cells back to a quiescent state and reduce ECM remodeling [126]. Paricalcitol, a vitamin D receptor ligand, was evaluated in metastatic pancreatic cancer in early phase trials in association with chemotherapy (NCT03520790, NCT03415854) and yielded a 83% objective response rate in combination with chemotherapy and nivolumab in a phase II pilot trial [127], leading an expansion cohort (NCT02754726). Furthermore, normalization of the deleterious high interstitial pressure and resulting hypoxia could be achieved with the systemic administration of PEG-fused hyaluronidase (PEHPH20) [128]. The clinical development of PEHPH20 has mainly been carried out in pancreatic cancer. An efficacy signal was detected in combination with gemcitabine plus nab-paclitaxel in hyaluronan-high tumors in a randomized phase II study including 279 patients with untreated metastatic PDAC [129]. However, PEGPH20 failed to improve OS in the HALO 301 phase III trial [130]. Moreover, a phase Ib/II trial showed a negative effect on OS and additional digestive toxicities when PEGPH20 was added to FOLFIRINOX (5-fluorouracil, leucovorin, irinotecan and oxaliplatin) in pancreatic cancer [131]. Some trials are ongoing in resectable and advanced pancreatic cancer in combination with immune checkpoints inhibitors (ICI) (NCT03634332, NCT03979066), following evidence that PEGPH20 can promote T cell infiltration into the TME [132]. Additional ECM targets, such as matrix metalloproteinases (MMPs) inhibitors, showed disappointing clinical results with severe musculoskeletal toxicities [133,134,135], despite encouraging preclinical data [136,137]. Besides, glutamine is involved in hyaluronan synthesis through the hexosamine biosynthesis pathway [138] and its antagonism increases TILs and sensitizes anti-PD1 therapy in preclinical models [139]. Glutamine antagonism was limited by gastrointestinal toxicities in previous clinical trials owing to overdosing and is now redeveloped in a low dose regimen to avoid significant toxicity [140]. Furthermore, the focal adhesion kinase (FAK) signaling pathway regulates fibrosis [141] but also has immunomodulatory functions through Treg recruitment [142]. Its inhibition by a tyrosine kinase inhibitor, defactinib, was evaluated in advanced solid tumors in combination with anti-PD1 therapy (NCT0254653, NCT03727880, NCT02758587) based on preclinical evidence. Moreover, IL-1 mediated signaling promotes CAF proliferation and fibrosis [143]. The IL-1 receptor blockade has shown interesting efficacy results (disease control rate 84%) in metastatic colorectal cancer in combination with 5-fluorouracil and bevacizumab [144] in a single-arm phase II study, and is now being explored in pancreatic cancer (NCT02021422). Additionally, other antifibrosis molecules approved for lung fibrosis are currently being evaluated in oncology following the demonstration of their immunomodulatory properties in animal models. Pirfenidone has been shown to reduce lung cancer growth in murine models by down-regulating the TGFβ pathway leading to an increase in NK and T cells infiltration [145] and giving a rationale for combination with atezolizumab in patients with lung cancer (NCT04467723). Nintedanib is a tyrosine kinase inhibitor that targets drivers of fibrosis and angiogenesis such as vascular endothelial growth factor receptors, fibroblast growth factors receptors, and platelet-derived growth factors receptors [146]. This drug inhibited activation of protumoral lung CAFs in preclinical models [147] and is currently being evaluated in patients with lung cancer in combination with nivolumab and ipilimumab (NCT03377023). Losartan is an approved angiotensin II receptor inhibitor to treat high blood pressure and also inhibits collagen I synthesis [148]. A single-arm phase II trial evaluating its association with chemotherapy showed interesting downstaging rates (R0 resection rate 61%) in 49 patients with pancreatic cancer [149]. A randomized phase II is ongoing in combination with chemotherapy, immunotherapy and radiotherapy in patients with localized pancreatic cancer (NCT03563248).
Finally, the hedgehog signaling pathway involving the Sonic Hedgehog (SHH) proteins promoted desmoplasia [107] and stimulated stellate cell differentiation and myofibroblast activation in pancreatic cancer. SHH inhibition showed promising results in mouse models but did not improve OS in clinical trials [150,151]. As hedgehog-signaling CAFs are heterogenous and encompass several subsets [6], one hypothesis for this failure is the absence of targeting of protumoral CAF subsets. This second strategy has been explored by targeting protumoral CAF markers. As an example, FAP is linked to angiogenesis and immunosuppression [152] and its inhibition by monoclonal antibodies or small molecules was clinically inefficient in pancreatic [153], lung [154] and colorectal cancer [155]. Based on data showing immune control of tumor growth and effectiveness of immune checkpoint inhibitors after FAP inhibition in a KPC mouse model [37], FAP inhibition is currently being explored in association with pembrolizumab (anti-PD1) (NCT04171219, NCT03910660, NCT04007744). RO 6874281 is a recombinant fusion protein composed of a human monoclonal antibody directed against FAP linked to a variant form of IL-2. This drug stimulates a local immune response by the accumulation of CTLs and NK cells in FAP-expressing areas and is currently under evaluation in combination with anti-PD1 (NCT04171219, NCT03910660, NCT04007744), and with trastuzumab (anti-HER2) or cetuximab (anti-EGFR) in head and neck, and breast cancers (NCT02627274). Similarly, PDGFRα is one of the CAF markers associated with protumorigenic properties [109], which can be targeted by olaratumab. Olaratumab is approved for the treatment of soft tissue sarcoma [156] and is being investigated in pancreatic cancer (NCT03086369). Moreover, inhibition of NAD(P)H Oxidase-4 (NOX4) was able to revert protumoral CAF subsets such as myofibroblastic [157] and immune-suppressive CAFs [158] in preclinical models making its clinical development promising. A recent study found a new CAF lineage associated with poor response to anti-PD-L1 therapy across six cancer types by using single-cell transcriptomics [116]. This subpopulation expresses the leucine-rich repeat containing 15 (LRRC15) protein, is driven by TGFβ and could represent a new target in combination with immunotherapy.
The third therapeutic approach is to target the CAF-secreted molecules that promote the immunosuppressive TME, such as CCL2, CXCL12 and IDO. As mentioned above, the CCR2-CCL2 axis is involved in the recruitment of M2 TAM, and its blockade consequently reduces TAM infiltration [159]. However, no objective responses were observed with CCR2-CCL2 inhibitors when administrated as monotherapy in metastatic castration-resistant prostate cancer [160] or in combination chemotherapy in pancreatic cancer [161,162]. Despite these disappointing results, murine models showed that the CCR2-CCL2 axis blockade may potentiate ICI efficacy [163] leading to exploration of the combination with nivolumab (anti-PD1) in early phase trials in several cancer types (NCT03496662, NCT03767582, NCT03184870, NCT04123379). Furthermore, CXCL12-CXCR4 signaling is involved in stromal-immune crosstalk [164] giving a rationale for the clinical investigation of CXCR4 inhibitors in combination with anti-PD1 in metastatic pancreatic (NCT04177810, NCT02826486) and head and neck cancers (NCT04058145). In addition, since IDO is secreted by CAFs, and is involved in local immunosuppression by inducing NK defects, T-cell apoptosis and Treg activity, its inhibition is being actively explored in oncology. The first efficacy results showed no clinical benefit in melanoma [165] when an IDO inhibitor was added to anti-PD1, but objective response rates were up to 40–60% in head and neck, kidney and breast cancers [166]. Finally, the TGFβ secreted by tumor cells can turn CAFs into an inflammatory phenotype producing the protumoral and immunosuppressive IL-6 cytokine. Targeting the TGFβ pathway is being evaluated in ongoing clinical trials in several cancer types (NCT02423343, NCT02452008, NCT02581787, NCT03834662, NCT02937272, NCT02423343). As TGFβ is associated with poor response to ICI, its inhibition by galunisertib in combination with durvalumab (anti-PD-L1) was tested in metastatic pancreatic cancer and showed an acceptable safety profile [167]. Bintrafusp alfa is a bifunctional fusion protein composed of the TGF-β receptor combined to an antibody blocking PD-L1 with a manageable safety profile and encouraging activity in phase I trials in pretreated advanced solid tumors [168,169]. However, prediction of efficacy is difficult regarding both the antitumoral and protumoral effects of TGFβ signaling.
Overall, combining selective stromal modulation with ICI is being actively explored in early phase trials (Table 3) since the stroma-only modulation appeared disappointing. Many of the abovementioned drugs aimed at targeting the TME do not necessarily block CAF signals selectively but inhibit a specific target from multiple sources including cancer cells and recruited inflammatory cells. Although CAFs certainly affect the immune response, it is still unknown whether targeting both tumor-derived and CAF-derived signals would be more beneficial than an antitumor strategy targeted toward one specific cell type, and more work needs to be done to differentiate these two sources. Furthermore, it is still unknown if CAF immunomodulatory functions are organ-specific or pan-tumor since studies are usually conducted in one cancer type. However, single-cell studies showed that CAFs may share common characteristics independently of the primary cancer [68,116].
Table 3.
Ongoing clinical trials evaluating modulation of cancer-associated fibroblasts in combination with ICI in solid tumors 1.
| Strategy | Target | Molecule | ICI | Phase | Solid Tumors | Population | ClinicalTrial.gov Reference |
|---|---|---|---|---|---|---|---|
| Inhibition of protumoral CAF subsets | FAP | CAR-T cell | Pembrolizumab | II | All | Advanced | NCT02546531 |
| Pembrolizumab | I/II | Prostate | Metastatic castration-resistant | NCT03910660 | |||
| Sonidegib | Pembrolizumab | I | All | Advanced | NCT02758587 | ||
| Inhibition of CAF-secreted immunosuppressive molecules | CXCL12/CXCR4 axis | AMD3100 | Cemiplimab | II | Pancreas | Metastatic | NCT04177810 |
| Pembrolizumab | II | Head and neck | Recurrent, metastatic | NCT04058145 | |||
| BL-8040 | Pembrolizumab | II | Pancreas | Metastatic | NCT02826486 | ||
| Ulocuplumab | Nivolumab | I/II | All | Advanced | NCT02472977 | ||
| CCR2/CCL2 axis | BMS-813160 | Nivolumab | I/II | Pancreas | Borderline, locally advanced | NCT03496662 | |
| Nivolumab | I/II | Pancreas | Locally advanced | NCT03767582 | |||
| Nivolumab | I/II | All | Advanced | NCT03184870 | |||
| Nivolumab | II | Lung, liver | Resectable | NCT04123379 | |||
| IDO1 | Epacadostat | Pembrolizumab | II | Bladder | Muscle-invasive | NCT03832673 | |
| Pembrolizumab | I/II | All | Advanced | NCT02959437 | |||
| Pembrolizumab | II | Lung | Metastatic | NCT03322540 | |||
| Pembrolizumab | II | Lung | Metastatic | NCT03322566 | |||
| Pembrolizumab | I/II | All | Metastatic | NCT03085914 | |||
| Nivolumab | I/II | All | Advanced | NCT03347123 | |||
| Durvalumab | I/II | All | Advanced | NCT02318277 | |||
| Atezolizumab | I | Lung, bladder | Advanced | NCT02298153 | |||
| Pembrolizumab | II | Pancreas | Metastatic | NCT03006302 | |||
| BMS-986205 | Nivolumab | II | Bladder | Non-muscle invasive | NCT03519256 | ||
| Nivolumab | I/II | Bladder | Muscle-invasive | NCT03661320 | |||
| Nivolumab, ipilimumab | I/II | All | Advanced | NCT02658890 | |||
| Nivolumab | II | Head and neck | Localized, Metastatic | NCT03854032 | |||
| Nivolumab | I/II | Liver | Advanced | NCT03695250 | |||
| TGFβ | Galunisertib | Nivolumab | I/II | All | Advanced | NCT02423343 | |
| Inhibition of fibrosis | FAK | Defatinib | Pembrolizumab | I | All | Advanced | NCT02546531 |
| Pembrolizumab | II | Pancreas | Resectable | NCT03727880 | |||
| Pembrolizumab | II | All | Advanced | NCT02758587 | |||
| CAF precursor | ATRA | Ipilimumab | II | Melanoma | Advanced | NCT02403778 | |
| Paricalcitol | Nivolumab | II | Pancreas | Advanced | NCT02754726 | ||
| Hypoxia | PEGPH20 | Pembrolizumab | II | Pancreas | Metastatic | NCT03634332 | |
| Atezolizumab | II | Pancreas | Resectable | NCT03979066 | |||
| IL-1 | Isunakinra | Unknown | I/II | All | Advanced | NCT04121442 | |
| Canakinumab | Pembrolizumab | II | Lung | Resectable | NCT03968419 | ||
| Pembrolizumab | III | Lung | Advanced | NCT03631199 | |||
| Spartalizumab | I | Renal | Localized | NCT04028245 | |||
| TGFβ | Pirfenidone | Atezolizumab | I/II | Lung | Advanced | NCT04467723 | |
| VEGFR, FGFR, PDGFR | Nintedanib | Nivolumab and Ipilumab | I/II | Lung | Advanced | NCT03377023 | |
| Collagen | Losartan | Nivolumab | II | Pancreas | Localized | NCT03563248 |
1 Abbreviations. ATRA: all-trans retinoic acid. CCL2: chemokine-ligand 2. CCR2: C-C chemokine receptor type 2. CXCL12: C-X-C motif chemokine 12. CXCR4: C-X-C motif chemokine receptor 4. ECM: extracellular matrix. FAK: focal adhesion kinase. FAP: fibroblast activation protein. FGFR: fibroblast growth factor receptor. ICI: immune checkpoint inhibitors. IDO1: indoleamine 2,3-dioxygenase 1. IL-1: interleukin-1. PDGFR: platelet-derived growth factor receptor. TGFβ: transforming growth factor β. VEGF: vascular endothelial growth factor receptor.
6. Conclusions
CAFs are highly involved in tumor immune evasion by physically and chemically impeding the immune system and interacting with both myeloid and lymphoid cells. However, CAFs do not represent a single cell entity but are divided into several subtypes with different functions that may be antagonistic. Targeting CAFs functions is a promising strategy currently being explored in early phase trials. However, published clinical trials solely aimed at targeting the stroma showed disappointing results, despite being based on solid preclinical evidence. This shows that a deeper understanding of CAF subpopulations and heterogeneity in the context of immune evasion is the cornerstone to propose relevant therapies that will ultimately improve survival of patients with cancers [123]. To achieve this goal, collaboration between clinicians and researchers is mandatory.
Author Contributions
Writing—original draft preparation, M.H.; writing—review and editing, R.N., C.B., C.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
C.N.: OSE Immunotherapeutics, Servier, Celgene, Roche, Amgen; M.H., R.N., C.B.: none.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dunn G.P., Old L.J., Schreiber R.D. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004;21:137–148. doi: 10.1016/j.immuni.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 2.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 3.Hanahan D., Coussens L.M. Accessories to the crime: Functions of cells recruited to the tumor microenvironment. Cancer Cell. 2012;21:309–322. doi: 10.1016/j.ccr.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 4.Hinshaw D.C., Shevde L.A. The Tumor Microenvironment Innately Modulates Cancer Progression. Cancer Res. 2019;79:4557–4566. doi: 10.1158/0008-5472.CAN-18-3962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kalluri R. The biology and function of fibroblasts in cancer. Nat. Rev. Cancer. 2016;16:582–598. doi: 10.1038/nrc.2016.73. [DOI] [PubMed] [Google Scholar]
- 6.Helms E., Onate M.K., Sherman M.H. Fibroblast Heterogeneity in the Pancreatic Tumor Microenvironment. Cancer Discov. 2020;10:648–656. doi: 10.1158/2159-8290.CD-19-1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hosaka K., Yang Y., Seki T., Fischer C., Dubey O., Fredlund E., Hartman J., Religa P., Morikawa H., Ishii Y., et al. Pericyte-fibroblast transition promotes tumor growth and metastasis. Proc. Natl. Acad. Sci. USA. 2016;113:E5618–E5627. doi: 10.1073/pnas.1608384113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jotzu C., Alt E., Welte G., Li J., Hennessy B.T., Devarajan E., Krishnappa S., Pinilla S., Droll L., Song Y.H. Adipose tissue-derived stem cells differentiate into carcinoma-associated fibroblast-like cells under the influence of tumor-derived factors. Anal. Cell. Pathol. 2010;33:61–79. doi: 10.1155/2010/695162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Radisky D.C., Kenny P.A., Bissell M.J. Fibrosis and cancer: Do myofibroblasts come also from epithelial cells via EMT? J. Cell. Biochem. 2007;101:830–839. doi: 10.1002/jcb.21186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zeisberg E.M., Potenta S., Xie L., Zeisberg M., Kalluri R. Discovery of endothelial to mesenchymal transition as a source for carcinoma-associated fibroblasts. Cancer Res. 2007;67:10123–10128. doi: 10.1158/0008-5472.CAN-07-3127. [DOI] [PubMed] [Google Scholar]
- 11.Raz Y., Cohen N., Shani O., Bell R.E., Novitskiy S.V., Abramovitz L., Levy C., Milyavsky M., Leider-Trejo L., Moses H.L., et al. Bone marrow-derived fibroblasts are a functionally distinct stromal cell population in breast cancer. J. Exp. Med. 2018;215:3075–3093. doi: 10.1084/jem.20180818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koliaraki V., Pallangyo C.K., Greten F.R., Kollias G. Mesenchymal Cells in Colon Cancer. Gastroenterology. 2017;152:964–979. doi: 10.1053/j.gastro.2016.11.049. [DOI] [PubMed] [Google Scholar]
- 13.Smith R.S., Smith T.J., Blieden T.M., Phipps R.P. Fibroblasts as sentinel cells. Synthesis of chemokines and regulation of inflammation. Am. J. Pathol. 1997;151:317–322. [PMC free article] [PubMed] [Google Scholar]
- 14.Chakravarthy A., Khan L., Bensler N.P., Bose P., De Carvalho D.D. TGF-β-associated extracellular matrix genes link cancer-associated fibroblasts to immune evasion and immunotherapy failure. Nat. Commun. 2018;9:4692. doi: 10.1038/s41467-018-06654-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Derynck R., Turley S.J., Akhurst R.J. TGFβ biology in cancer progression and immunotherapy. Nat. Rev. Clin. Oncol. 2020 doi: 10.1038/s41571-020-0403-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen N., Shani O., Raz Y., Sharon Y., Hoffman D., Abramovitz L., Erez N. Fibroblasts drive an immunosuppressive and growth-promoting microenvironment in breast cancer via secretion of Chitinase 3-like 1. Oncogene. 2017;36:4457–4468. doi: 10.1038/onc.2017.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ren G., Zhao X., Wang Y., Zhang X., Chen X., Xu C., Yuan Z.R., Roberts A.I., Zhang L., Zheng B., et al. CCR2-dependent recruitment of macrophages by tumor-educated mesenchymal stromal cells promotes tumor development and is mimicked by TNFalpha. Cell Stem Cell. 2012;11:812–824. doi: 10.1016/j.stem.2012.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gunderson A.J., Yamazaki T., McCarty K., Phillips M., Alice A., Bambina S., Zebertavage L., Friedman D., Cottam B., Newell P., et al. Blockade of fibroblast activation protein in combination with radiation treatment in murine models of pancreatic adenocarcinoma. PLoS ONE. 2019;14:e0211117. doi: 10.1371/journal.pone.0211117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jia X.H., Du Y., Mao D., Wang Z.L., He Z.Q., Qiu J.D., Ma X.B., Shang W.T., Ding D., Tian J. Zoledronic acid prevents the tumor-promoting effects of mesenchymal stem cells via MCP-1 dependent recruitment of macrophages. Oncotarget. 2015;6:26018–26028. doi: 10.18632/oncotarget.4658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ksiazkiewicz M., Gottfried E., Kreutz M., Mack M., Hofstaedter F., Kunz-Schughart L.A. Importance of CCL2-CCR2A/2B signaling for monocyte migration into spheroids of breast cancer-derived fibroblasts. Immunobiology. 2010;215:737–747. doi: 10.1016/j.imbio.2010.05.019. [DOI] [PubMed] [Google Scholar]
- 21.Comito G., Giannoni E., Segura C.P., Barcellos-de-Souza P., Raspollini M.R., Baroni G., Lanciotti M., Serni S., Chiarugi P. Cancer-associated fibroblasts and M2-polarized macrophages synergize during prostate carcinoma progression. Oncogene. 2014;33:2423–2431. doi: 10.1038/onc.2013.191. [DOI] [PubMed] [Google Scholar]
- 22.Mathew E., Brannon A.L., Del Vecchio A., Garcia P.E., Penny M.K., Kane K.T., Vinta A., Buckanovich R.J., di Magliano M.P. Mesenchymal Stem Cells Promote Pancreatic Tumor Growth by Inducing Alternative Polarization of Macrophages. Neoplasia. 2016;18:142–151. doi: 10.1016/j.neo.2016.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liao D., Luo Y., Markowitz D., Xiang R., Reisfeld R.A. Cancer associated fibroblasts promote tumor growth and metastasis by modulating the tumor immune microenvironment in a 4T1 murine breast cancer model. PLoS ONE. 2009;4:e7965. doi: 10.1371/journal.pone.0007965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen L., Qiu X., Wang X., He J. FAP positive fibroblasts induce immune checkpoint blockade resistance in colorectal cancer via promoting immunosuppression. Biochem. Biophys. Res. Commun. 2017;487:8–14. doi: 10.1016/j.bbrc.2017.03.039. [DOI] [PubMed] [Google Scholar]
- 25.Ruhland M.K., Loza A.J., Capietto A.H., Luo X., Knolhoff B.L., Flanagan K.C., Belt B.A., Alspach E., Leahy K., Luo J., et al. Stromal senescence establishes an immunosuppressive microenvironment that drives tumorigenesis. Nat. Commun. 2016;7:11762. doi: 10.1038/ncomms11762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang X., Lin Y., Shi Y., Li B., Liu W., Yin W., Dang Y., Chu Y., Fan J., He R. FAP Promotes Immunosuppression by Cancer-Associated Fibroblasts in the Tumor Microenvironment via STAT3-CCL2 Signaling. Cancer Res. 2016;76:4124–4135. doi: 10.1158/0008-5472.CAN-15-2973. [DOI] [PubMed] [Google Scholar]
- 27.Kumar V., Donthireddy L., Marvel D., Condamine T., Wang F., Lavilla-Alonso S., Hashimoto A., Vonteddu P., Behera R., Goins M.A., et al. Cancer-Associated Fibroblasts Neutralize the Anti-tumor Effect of CSF1 Receptor Blockade by Inducing PMN-MDSC Infiltration of Tumors. Cancer Cell. 2017;32:654–668.e655. doi: 10.1016/j.ccell.2017.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Deng Y., Cheng J., Fu B., Liu W., Chen G., Zhang Q., Yang Y. Hepatic carcinoma-associated fibroblasts enhance immune suppression by facilitating the generation of myeloid-derived suppressor cells. Oncogene. 2017;36:1090–1101. doi: 10.1038/onc.2016.273. [DOI] [PubMed] [Google Scholar]
- 29.Mace T.A., Ameen Z., Collins A., Wojcik S., Mair M., Young G.S., Fuchs J.R., Eubank T.D., Frankel W.L., Bekaii-Saab T., et al. Pancreatic cancer-associated stellate cells promote differentiation of myeloid-derived suppressor cells in a STAT3-dependent manner. Cancer Res. 2013;73:3007–3018. doi: 10.1158/0008-5472.CAN-12-4601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cheng J.T., Deng Y.N., Yi H.M., Wang G.Y., Fu B.S., Chen W.J., Liu W., Tai Y., Peng Y.W., Zhang Q. Hepatic carcinoma-associated fibroblasts induce IDO-producing regulatory dendritic cells through IL-6-mediated STAT3 activation. Oncogenesis. 2016;5:e198. doi: 10.1038/oncsis.2016.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hsu Y.L., Hung J.Y., Chiang S.Y., Jian S.F., Wu C.Y., Lin Y.S., Tsai Y.M., Chou S.H., Tsai M.J., Kuo P.L. Lung cancer-derived galectin-1 contributes to cancer associated fibroblast-mediated cancer progression and immune suppression through TDO2/kynurenine axis. Oncotarget. 2016;7:27584–27598. doi: 10.18632/oncotarget.8488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.De Monte L., Reni M., Tassi E., Clavenna D., Papa I., Recalde H., Braga M., Di Carlo V., Doglioni C., Protti M.P. Intratumor T helper type 2 cell infiltrate correlates with cancer-associated fibroblast thymic stromal lymphopoietin production and reduced survival in pancreatic cancer. J. Exp. Med. 2011;208:469–478. doi: 10.1084/jem.20101876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cheng Y., Li H., Deng Y., Tai Y., Zeng K., Zhang Y., Liu W., Zhang Q., Yang Y. Cancer-associated fibroblasts induce PDL1+ neutrophils through the IL6-STAT3 pathway that foster immune suppression in hepatocellular carcinoma. Cell Death Dis. 2018;9:422. doi: 10.1038/s41419-018-0458-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yu P.F., Huang Y., Han Y.Y., Lin L.Y., Sun W.H., Rabson A.B., Wang Y., Shi Y.F. TNFalpha-activated mesenchymal stromal cells promote breast cancer metastasis by recruiting CXCR2(+) neutrophils. Oncogene. 2017;36:482–490. doi: 10.1038/onc.2016.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ellem S.J., Taylor R.A., Furic L., Larsson O., Frydenberg M., Pook D., Pedersen J., Cawsey B., Trotta A., Need E., et al. A pro-tumourigenic loop at the human prostate tumour interface orchestrated by oestrogen, CXCL12 and mast cell recruitment. J. Pathol. 2014;234:86–98. doi: 10.1002/path.4386. [DOI] [PubMed] [Google Scholar]
- 36.Mace T.A., Shakya R., Pitarresi J.R., Swanson B., McQuinn C.W., Loftus S., Nordquist E., Cruz-Monserrate Z., Yu L., Young G., et al. IL-6 and PD-L1 antibody blockade combination therapy reduces tumour progression in murine models of pancreatic cancer. Gut. 2018;67:320–332. doi: 10.1136/gutjnl-2016-311585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Feig C., Jones J.O., Kraman M., Wells R.J., Deonarine A., Chan D.S., Connell C.M., Roberts E.W., Zhao Q., Caballero O.L., et al. Targeting CXCL12 from FAP-expressing carcinoma-associated fibroblasts synergizes with anti-PD-L1 immunotherapy in pancreatic cancer. Proc. Natl. Acad. Sci. USA. 2013;110:20212–20217. doi: 10.1073/pnas.1320318110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mariathasan S., Turley S.J., Nickles D., Castiglioni A., Yuen K., Wang Y., Kadel E.E., III, Koeppen H., Astarita J.L., Cubas R., et al. TGFbeta attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature. 2018;554:544–548. doi: 10.1038/nature25501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tauriello D.V.F., Palomo-Ponce S., Stork D., Berenguer-Llergo A., Badia-Ramentol J., Iglesias M., Sevillano M., Ibiza S., Canellas A., Hernando-Momblona X., et al. TGFbeta drives immune evasion in genetically reconstituted colon cancer metastasis. Nature. 2018;554:538–543. doi: 10.1038/nature25492. [DOI] [PubMed] [Google Scholar]
- 40.Goehrig D., Nigri J., Samain R., Wu Z., Cappello P., Gabiane G., Zhang X., Zhao Y., Kim I.S., Chanal M., et al. Stromal protein βig-h3 reprogrammes tumour microenvironment in pancreatic cancer. Gut. 2019;68:693–707. doi: 10.1136/gutjnl-2018-317570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lakins M.A., Ghorani E., Munir H., Martins C.P., Shields J.D. Cancer-associated fibroblasts induce antigen-specific deletion of CD8 (+) T Cells to protect tumour cells. Nat. Commun. 2018;9:948. doi: 10.1038/s41467-018-03347-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cremasco V., Astarita J.L., Grauel A.L., Keerthivasan S., MacIsaac K., Woodruff M.C., Wu M., Spel L., Santoro S., Amoozgar Z., et al. FAP Delineates Heterogeneous and Functionally Divergent Stromal Cells in Immune-Excluded Breast Tumors. Cancer Immunol. Res. 2018;6:1472–1485. doi: 10.1158/2326-6066.CIR-18-0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de Lourdes Mora-Garcia M., Garcia-Rocha R., Morales-Ramirez O., Montesinos J.J., Weiss-Steider B., Hernandez-Montes J., Avila-Ibarra L.R., Don-Lopez C.A., Velasco-Velazquez M.A., Gutierrez-Serrano V., et al. Mesenchymal stromal cells derived from cervical cancer produce high amounts of adenosine to suppress cytotoxic T lymphocyte functions. J. Transl. Med. 2016;14:302. doi: 10.1186/s12967-016-1057-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Costa A., Kieffer Y., Scholer-Dahirel A., Pelon F., Bourachot B., Cardon M., Sirven P., Magagna I., Fuhrmann L., Bernard C., et al. Fibroblast Heterogeneity and Immunosuppressive Environment in Human Breast Cancer. Cancer Cell. 2018;33:463–479.e410. doi: 10.1016/j.ccell.2018.01.011. [DOI] [PubMed] [Google Scholar]
- 45.Givel A.M., Kieffer Y., Scholer-Dahirel A., Sirven P., Cardon M., Pelon F., Magagna I., Gentric G., Costa A., Bonneau C., et al. miR200-regulated CXCL12beta promotes fibroblast heterogeneity and immunosuppression in ovarian cancers. Nat. Commun. 2018;9:1056. doi: 10.1038/s41467-018-03348-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Balsamo M., Scordamaglia F., Pietra G., Manzini C., Cantoni C., Boitano M., Queirolo P., Vermi W., Facchetti F., Moretta A., et al. Melanoma-associated fibroblasts modulate NK cell phenotype and antitumor cytotoxicity. Proc. Natl. Acad. Sci. USA. 2009;106:20847–20852. doi: 10.1073/pnas.0906481106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li T., Yang Y., Hua X., Wang G., Liu W., Jia C., Tai Y., Zhang Q., Chen G. Hepatocellular carcinoma-associated fibroblasts trigger NK cell dysfunction via PGE2 and IDO. Cancer Lett. 2012;318:154–161. doi: 10.1016/j.canlet.2011.12.020. [DOI] [PubMed] [Google Scholar]
- 48.Qian B.Z., Pollard J.W. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141:39–51. doi: 10.1016/j.cell.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jayasingam S.D., Citartan M., Thang T.H., Mat Zin A.A., Ang K.C., Ch’ng E.S. Evaluating the Polarization of Tumor-Associated Macrophages Into M1 and M2 Phenotypes in Human Cancer Tissue: Technicalities and Challenges in Routine Clinical Practice. Front. Oncol. 2019;9:1512. doi: 10.3389/fonc.2019.01512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Monu N.R., Frey A.B. Myeloid-derived suppressor cells and anti-tumor T cells: A complex relationship. Immunol. Investig. 2012;41:595–613. doi: 10.3109/08820139.2012.673191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vickman R.E., Broman M.M., Lanman N.A., Franco O.E., Sudyanti P.A.G., Ni Y., Ji Y., Helfand B.T., Petkewicz J., Paterakos M.C., et al. Heterogeneity of human prostate carcinoma-associated fibroblasts implicates a role for subpopulations in myeloid cell recruitment. Prostate. 2020;80:173–185. doi: 10.1002/pros.23929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sanchez-Paulete A.R., Teijeira A., Cueto F.J., Garasa S., Perez-Gracia J.L., Sanchez-Arraez A., Sancho D., Melero I. Antigen cross-presentation and T-cell cross-priming in cancer immunology and immunotherapy. Ann. Oncol. 2017;28:xii44–xii55. doi: 10.1093/annonc/mdx237. [DOI] [PubMed] [Google Scholar]
- 53.Kim J., Mooney D.J. In Vivo Modulation of Dendritic Cells by Engineered Materials: Towards New Cancer Vaccines. Nano Today. 2011;6:466–477. doi: 10.1016/j.nantod.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ocana A., Nieto-Jimenez C., Pandiella A., Templeton A.J. Neutrophils in cancer: Prognostic role and therapeutic strategies. Mol. Cancer. 2017;16:137. doi: 10.1186/s12943-017-0707-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shaul M.E., Fridlender Z.G. Neutrophils as active regulators of the immune system in the tumor microenvironment. J. Leukoc. Biol. 2017;102:343–349. doi: 10.1189/jlb.5MR1216-508R. [DOI] [PubMed] [Google Scholar]
- 56.Fridman W.H., Pages F., Sautes-Fridman C., Galon J. The immune contexture in human tumours: Impact on clinical outcome. Nat. Rev. Cancer. 2012;12:298–306. doi: 10.1038/nrc3245. [DOI] [PubMed] [Google Scholar]
- 57.Elyada E., Bolisetty M., Laise P., Flynn W.F., Courtois E.T., Burkhart R.A., Teinor J.A., Belleau P., Biffi G., Lucito M.S., et al. Cross-Species Single-Cell Analysis of Pancreatic Ductal Adenocarcinoma Reveals Antigen-Presenting Cancer-Associated Fibroblasts. Cancer Discov. 2019;9:1102–1123. doi: 10.1158/2159-8290.CD-19-0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Whiteside T.L. What are regulatory T cells (Treg) regulating in cancer and why? Semin. Cancer Biol. 2012;22:327–334. doi: 10.1016/j.semcancer.2012.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hiraoka N., Onozato K., Kosuge T., Hirohashi S. Prevalence of FOXP3+ regulatory T cells increases during the progression of pancreatic ductal adenocarcinoma and its premalignant lesions. Clin. Cancer Res. 2006;12:5423–5434. doi: 10.1158/1078-0432.CCR-06-0369. [DOI] [PubMed] [Google Scholar]
- 60.Curiel T.J., Coukos G., Zou L., Alvarez X., Cheng P., Mottram P., Evdemon-Hogan M., Conejo-Garcia J.R., Zhang L., Burow M., et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat. Med. 2004;10:942–949. doi: 10.1038/nm1093. [DOI] [PubMed] [Google Scholar]
- 61.Fu J., Xu D., Liu Z., Shi M., Zhao P., Fu B., Zhang Z., Yang H., Zhang H., Zhou C., et al. Increased regulatory T cells correlate with CD8 T-cell impairment and poor survival in hepatocellular carcinoma patients. Gastroenterology. 2007;132:2328–2339. doi: 10.1053/j.gastro.2007.03.102. [DOI] [PubMed] [Google Scholar]
- 62.Merlo A., Casalini P., Carcangiu M.L., Malventano C., Triulzi T., Menard S., Tagliabue E., Balsari A. FOXP3 expression and overall survival in breast cancer. J. Clin. Oncol. 2009;27:1746–1752. doi: 10.1200/JCO.2008.17.9036. [DOI] [PubMed] [Google Scholar]
- 63.Tzankov A., Meier C., Hirschmann P., Went P., Pileri S.A., Dirnhofer S. Correlation of high numbers of intratumoral FOXP3+ regulatory T cells with improved survival in germinal center-like diffuse large B-cell lymphoma, follicular lymphoma and classical Hodgkin’s lymphoma. Haematologica. 2008;93:193–200. doi: 10.3324/haematol.11702. [DOI] [PubMed] [Google Scholar]
- 64.Badoual C., Hans S., Rodriguez J., Peyrard S., Klein C., Agueznay Nel H., Mosseri V., Laccourreye O., Bruneval P., Fridman W.H., et al. Prognostic value of tumor-infiltrating CD4+ T-cell subpopulations in head and neck cancers. Clin. Cancer Res. 2006;12:465–472. doi: 10.1158/1078-0432.CCR-05-1886. [DOI] [PubMed] [Google Scholar]
- 65.Salama P., Phillips M., Grieu F., Morris M., Zeps N., Joseph D., Platell C., Iacopetta B. Tumor-infiltrating FOXP3+ T regulatory cells show strong prognostic significance in colorectal cancer. J. Clin. Oncol. 2009;27:186–192. doi: 10.1200/JCO.2008.18.7229. [DOI] [PubMed] [Google Scholar]
- 66.Hoffmann P., Boeld T.J., Eder R., Huehn J., Floess S., Wieczorek G., Olek S., Dietmaier W., Andreesen R., Edinger M. Loss of FOXP3 expression in natural human CD4+CD25+ regulatory T cells upon repetitive in vitro stimulation. Eur. J. Immunol. 2009;39:1088–1097. doi: 10.1002/eji.200838904. [DOI] [PubMed] [Google Scholar]
- 67.Komatsu N., Mariotti-Ferrandiz M.E., Wang Y., Malissen B., Waldmann H., Hori S. Heterogeneity of natural Foxp3+ T cells: A committed regulatory T-cell lineage and an uncommitted minor population retaining plasticity. Proc. Natl. Acad. Sci. USA. 2009;106:1903–1908. doi: 10.1073/pnas.0811556106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kieffer Y., Hocine H.R., Gentric G., Pelon F., Bernard C., Bourachot B., Lameiras S., Albergante L., Bonneau C., Guyard A., et al. Single-cell analysis reveals fibroblast clusters linked to immunotherapy resistance in cancer. Cancer Discov. 2020 doi: 10.1158/2159-8290.CD-19-1384. [DOI] [PubMed] [Google Scholar]
- 69.Waldhauer I., Steinle A. NK cells and cancer immunosurveillance. Oncogene. 2008;27:5932–5943. doi: 10.1038/onc.2008.267. [DOI] [PubMed] [Google Scholar]
- 70.Schantz S.P., Shillitoe E.J., Brown B., Campbell B. Natural killer cell activity and head and neck cancer: A clinical assessment. J. Natl. Cancer Inst. 1986;77:869–875. [PubMed] [Google Scholar]
- 71.Takeuchi H., Maehara Y., Tokunaga E., Koga T., Kakeji Y., Sugimachi K. Prognostic significance of natural killer cell activity in patients with gastric carcinoma: A multivariate analysis. Am. J. Gastroenterol. 2001;96:574–578. doi: 10.1111/j.1572-0241.2001.03535.x. [DOI] [PubMed] [Google Scholar]
- 72.Taketomi A., Shimada M., Shirabe K., Kajiyama K., Gion T., Sugimachi K. Natural killer cell activity in patients with hepatocellular carcinoma: A new prognostic indicator after hepatectomy. Cancer. 1998;83:58–63. doi: 10.1002/(SICI)1097-0142(19980701)83:1<58::AID-CNCR8>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 73.Kondo E., Koda K., Takiguchi N., Oda K., Seike K., Ishizuka M., Miyazaki M. Preoperative natural killer cell activity as a prognostic factor for distant metastasis following surgery for colon cancer. Dig. Surg. 2003;20:445–451. doi: 10.1159/000072714. [DOI] [PubMed] [Google Scholar]
- 74.Sabry M., Lowdell M.W. Tumor-primed NK cells: Waiting for the green light. Front. Immunol. 2013;4:408. doi: 10.3389/fimmu.2013.00408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Eble J.A., Niland S. The extracellular matrix in tumor progression and metastasis. Clin. Exp. Metastasis. 2019;36:171–198. doi: 10.1007/s10585-019-09966-1. [DOI] [PubMed] [Google Scholar]
- 76.Ecker B.L., Kaur A., Douglass S.M., Webster M.R., Almeida F.V., Marino G.E., Sinnamon A.J., Neuwirth M.G., Alicea G.M., Ndoye A., et al. Age-Related Changes in HAPLN1 Increase Lymphatic Permeability and Affect Routes of Melanoma Metastasis. Cancer Discov. 2019;9:82–95. doi: 10.1158/2159-8290.CD-18-0168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hartmann N., Giese N.A., Giese T., Poschke I., Offringa R., Werner J., Ryschich E. Prevailing role of contact guidance in intrastromal T-cell trapping in human pancreatic cancer. Clin. Cancer Res. 2014;20:3422–3433. doi: 10.1158/1078-0432.CCR-13-2972. [DOI] [PubMed] [Google Scholar]
- 78.Meyaard L. The inhibitory collagen receptor LAIR-1 (CD305) J. Leukoc. Biol. 2008;83:799–803. doi: 10.1189/jlb.0907609. [DOI] [PubMed] [Google Scholar]
- 79.Kaur A., Ecker B.L., Douglass S.M., Kugel C.H., 3rd, Webster M.R., Almeida F.V., Somasundaram R., Hayden J., Ban E., Ahmadzadeh H., et al. Remodeling of the Collagen Matrix in Aging Skin Promotes Melanoma Metastasis and Affects Immune Cell Motility. Cancer Discov. 2019;9:64–81. doi: 10.1158/2159-8290.CD-18-0193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Van Goethem E., Poincloux R., Gauffre F., Maridonneau-Parini I., Le Cabec V. Matrix architecture dictates three-dimensional migration modes of human macrophages: Differential involvement of proteases and podosome-like structures. J. Immunol. 2010;184:1049–1061. doi: 10.4049/jimmunol.0902223. [DOI] [PubMed] [Google Scholar]
- 81.McWhorter F.Y., Davis C.T., Liu W.F. Physical and mechanical regulation of macrophage phenotype and function. Cell. Mol. Life Sci. 2015;72:1303–1316. doi: 10.1007/s00018-014-1796-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Stahl M., Schupp J., Jager B., Schmid M., Zissel G., Muller-Quernheim J., Prasse A. Lung collagens perpetuate pulmonary fibrosis via CD204 and M2 macrophage activation. PLoS ONE. 2013;8:e81382. doi: 10.1371/journal.pone.0081382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kobayashi N., Miyoshi S., Mikami T., Koyama H., Kitazawa M., Takeoka M., Sano K., Amano J., Isogai Z., Niida S., et al. Hyaluronan deficiency in tumor stroma impairs macrophage trafficking and tumor neovascularization. Cancer Res. 2010;70:7073–7083. doi: 10.1158/0008-5472.CAN-09-4687. [DOI] [PubMed] [Google Scholar]
- 84.Salmon H., Franciszkiewicz K., Damotte D., Dieu-Nosjean M.C., Validire P., Trautmann A., Mami-Chouaib F., Donnadieu E. Matrix architecture defines the preferential localization and migration of T cells into the stroma of human lung tumors. J. Clin. Investig. 2012;122:899–910. doi: 10.1172/JCI45817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Acerbi I., Cassereau L., Dean I., Shi Q., Au A., Park C., Chen Y.Y., Liphardt J., Hwang E.S., Weaver V.M. Human breast cancer invasion and aggression correlates with ECM stiffening and immune cell infiltration. Integr. Biol. 2015;7:1120–1134. doi: 10.1039/c5ib00040h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Nielsen S.R., Quaranta V., Linford A., Emeagi P., Rainer C., Santos A., Ireland L., Sakai T., Sakai K., Kim Y.S., et al. Macrophage-secreted granulin supports pancreatic cancer metastasis by inducing liver fibrosis. Nat. Cell Biol. 2016;18:549–560. doi: 10.1038/ncb3340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bentovim L., Amarilio R., Zelzer E. HIF1alpha is a central regulator of collagen hydroxylation and secretion under hypoxia during bone development. Development. 2012;139:4473–4483. doi: 10.1242/dev.083881. [DOI] [PubMed] [Google Scholar]
- 88.Chouaib S., Noman M.Z., Kosmatopoulos K., Curran M.A. Hypoxic stress: Obstacles and opportunities for innovative immunotherapy of cancer. Oncogene. 2017;36:439–445. doi: 10.1038/onc.2016.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Noman M.Z., Desantis G., Janji B., Hasmim M., Karray S., Dessen P., Bronte V., Chouaib S. PD-L1 is a novel direct target of HIF-1alpha, and its blockade under hypoxia enhanced MDSC-mediated T cell activation. J. Exp. Med. 2014;211:781–790. doi: 10.1084/jem.20131916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jiang C., Kim J.H., Li F., Qu A., Gavrilova O., Shah Y.M., Gonzalez F.J. Hypoxia-inducible factor 1alpha regulates a SOCS3-STAT3-adiponectin signal transduction pathway in adipocytes. J. Biol. Chem. 2013;288:3844–3857. doi: 10.1074/jbc.M112.426338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sitkovsky M.V., Kjaergaard J., Lukashev D., Ohta A. Hypoxia-adenosinergic immunosuppression: Tumor protection by T regulatory cells and cancerous tissue hypoxia. Clin. Cancer Res. 2008;14:5947–5952. doi: 10.1158/1078-0432.CCR-08-0229. [DOI] [PubMed] [Google Scholar]
- 92.Elkabets M., Gifford A.M., Scheel C., Nilsson B., Reinhardt F., Bray M.A., Carpenter A.E., Jirström K., Magnusson K., Ebert B.L., et al. Human tumors instigate granulin-expressing hematopoietic cells that promote malignancy by activating stromal fibroblasts in mice. J. Clin. Investig. 2011;121:784–799. doi: 10.1172/JCI43757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ozdemir B.C., Pentcheva-Hoang T., Carstens J.L., Zheng X., Wu C.C., Simpson T.R., Laklai H., Sugimoto H., Kahlert C., Novitskiy S.V., et al. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell. 2014;25:719–734. doi: 10.1016/j.ccr.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rhim A.D., Oberstein P.E., Thomas D.H., Mirek E.T., Palermo C.F., Sastra S.A., Dekleva E.N., Saunders T., Becerra C.P., Tattersall I.W., et al. Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell. 2014;25:735–747. doi: 10.1016/j.ccr.2014.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lee J.J., Perera R.M., Wang H., Wu D.C., Liu X.S., Han S., Fitamant J., Jones P.D., Ghanta K.S., Kawano S., et al. Stromal response to Hedgehog signaling restrains pancreatic cancer progression. Proc. Natl. Acad. Sci. USA. 2014;111:E3091–E3100. doi: 10.1073/pnas.1411679111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sugimoto H., Mundel T.M., Kieran M.W., Kalluri R. Identification of fibroblast heterogeneity in the tumor microenvironment. Cancer Biol. Ther. 2006;5:1640–1646. doi: 10.4161/cbt.5.12.3354. [DOI] [PubMed] [Google Scholar]
- 97.Neuzillet C., Tijeras-Raballand A., Ragulan C., Cros J., Patil Y., Martinet M., Erkan M., Kleeff J., Wilson J., Apte M., et al. Inter- and intra-tumoural heterogeneity in cancer-associated fibroblasts of human pancreatic ductal adenocarcinoma. J. Pathol. 2019;248:51–65. doi: 10.1002/path.5224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cai D., Wu X., Hong T., Mao Y., Ge X., Hua D. CD61+ and CAF+ were found to be good prognosis factors for invasive breast cancer patients. Pathol. Res. Pract. 2017;213:1296–1301. doi: 10.1016/j.prp.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 99.Yamanashi T., Nakanishi Y., Fujii G., Akishima-Fukasawa Y., Moriya Y., Kanai Y., Watanabe M., Hirohashi S. Podoplanin expression identified in stromal fibroblasts as a favorable prognostic marker in patients with colorectal carcinoma. Oncology. 2009;77:53–62. doi: 10.1159/000226112. [DOI] [PubMed] [Google Scholar]
- 100.Kumcu E., Unverdi H., Kaymaz E., Oral O., Turkbey D., Hucmenoglu S. Stromal podoplanin expression and its clinicopathological role in breast carcinoma. Malays. J. Pathol. 2018;40:137–142. [PubMed] [Google Scholar]
- 101.Pula B., Jethon A., Piotrowska A., Gomulkiewicz A., Owczarek T., Calik J., Wojnar A., Witkiewicz W., Rys J., Ugorski M., et al. Podoplanin expression by cancer-associated fibroblasts predicts poor outcome in invasive ductal breast carcinoma. Histopathology. 2011;59:1249–1260. doi: 10.1111/j.1365-2559.2011.04060.x. [DOI] [PubMed] [Google Scholar]
- 102.Schoppmann S.F., Berghoff A., Dinhof C., Jakesz R., Gnant M., Dubsky P., Jesch B., Heinzl H., Birner P. Podoplanin-expressing cancer-associated fibroblasts are associated with poor prognosis in invasive breast cancer. Breast Cancer Res. Treat. 2012;134:237–244. doi: 10.1007/s10549-012-1984-x. [DOI] [PubMed] [Google Scholar]
- 103.Neri S., Ishii G., Taira T., Hishida T., Yoshida J., Nishimura M., Nagai K., Ochiai A. Recruitment of podoplanin positive cancer-associated fibroblasts in metastatic lymph nodes predicts poor prognosis in pathological N2 stage III lung adenocarcinoma. Ann. Surg. Oncol. 2012;19:3953–3962. doi: 10.1245/s10434-012-2421-4. [DOI] [PubMed] [Google Scholar]
- 104.Kubouchi Y., Yurugi Y., Wakahara M., Sakabe T., Haruki T., Nosaka K., Miwa K., Araki K., Taniguchi Y., Shiomi T., et al. Podoplanin expression in cancer-associated fibroblasts predicts unfavourable prognosis in patients with pathological stage IA lung adenocarcinoma. Histopathology. 2018;72:490–499. doi: 10.1111/his.13390. [DOI] [PubMed] [Google Scholar]
- 105.Haro M., Orsulic S. A Paradoxical Correlation of Cancer-Associated Fibroblasts With Survival Outcomes in B-Cell Lymphomas and Carcinomas. Front. Cell Dev. Biol. 2018;6:98. doi: 10.3389/fcell.2018.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Gerling M., Buller N.V., Kirn L.M., Joost S., Frings O., Englert B., Bergstrom A., Kuiper R.V., Blaas L., Wielenga M.C., et al. Stromal Hedgehog signalling is downregulated in colon cancer and its restoration restrains tumour growth. Nat. Commun. 2016;7:12321. doi: 10.1038/ncomms12321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bailey J.M., Swanson B.J., Hamada T., Eggers J.P., Singh P.K., Caffery T., Ouellette M.M., Hollingsworth M.A. Sonic hedgehog promotes desmoplasia in pancreatic cancer. Clin. Cancer Res. 2008;14:5995–6004. doi: 10.1158/1078-0432.CCR-08-0291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Olive K.P., Jacobetz M.A., Davidson C.J., Gopinathan A., McIntyre D., Honess D., Madhu B., Goldgraben M.A., Caldwell M.E., Allard D., et al. Inhibition of Hedgehog signaling enhances delivery of chemotherapy in a mouse model of pancreatic cancer. Science. 2009;324:1457–1461. doi: 10.1126/science.1171362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Djurec M., Grana O., Lee A., Troule K., Espinet E., Cabras L., Navas C., Blasco M.T., Martin-Diaz L., Burdiel M., et al. Saa3 is a key mediator of the protumorigenic properties of cancer-associated fibroblasts in pancreatic tumors. Proc. Natl. Acad. Sci. USA. 2018;115:E1147–E1156. doi: 10.1073/pnas.1717802115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lim P.K., Bliss S.A., Patel S.A., Taborga M., Dave M.A., Gregory L.A., Greco S.J., Bryan M., Patel P.S., Rameshwar P. Gap junction-mediated import of microRNA from bone marrow stromal cells can elicit cell cycle quiescence in breast cancer cells. Cancer Res. 2011;71:1550–1560. doi: 10.1158/0008-5472.CAN-10-2372. [DOI] [PubMed] [Google Scholar]
- 111.Madar S., Brosh R., Buganim Y., Ezra O., Goldstein I., Solomon H., Kogan I., Goldfinger N., Klocker H., Rotter V. Modulated expression of WFDC1 during carcinogenesis and cellular senescence. Carcinogenesis. 2009;30:20–27. doi: 10.1093/carcin/bgn232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chen S., Giannakou A., Wyman S., Gruzas J., Golas J., Zhong W., Loreth C., Sridharan L., Yamin T.T., Damelin M., et al. Cancer-associated fibroblasts suppress SOX2-induced dysplasia in a lung squamous cancer coculture. Proc. Natl. Acad. Sci. USA. 2018;115:E11671–E11680. doi: 10.1073/pnas.1803718115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Costanza B., Umelo I.A., Bellier J., Castronovo V., Turtoi A. Stromal Modulators of TGF-beta in Cancer. J. Clin. Med. 2017;6:7. doi: 10.3390/jcm6010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Hosein A.N., Huang H., Wang Z., Parmar K., Du W., Huang J., Maitra A., Olson E., Verma U., Brekken R.A. Cellular heterogeneity during mouse pancreatic ductal adenocarcinoma progression at single-cell resolution. JCI Insight. 2019;5 doi: 10.1172/jci.insight.129212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Bernard V., Semaan A., Huang J., San Lucas F.A., Mulu F.C., Stephens B.M., Guerrero P.A., Huang Y., Zhao J., Kamyabi N., et al. Single-Cell Transcriptomics of Pancreatic Cancer Precursors Demonstrates Epithelial and Microenvironmental Heterogeneity as an Early Event in Neoplastic Progression. Clin. Cancer Res. 2019;25:2194–2205. doi: 10.1158/1078-0432.CCR-18-1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Dominguez C.X., Müller S., Keerthivasan S., Koeppen H., Hung J., Gierke S., Breart B., Foreman O., Bainbridge T.W., Castiglioni A., et al. Single-Cell RNA Sequencing Reveals Stromal Evolution into LRRC15(+) Myofibroblasts as a Determinant of Patient Response to Cancer Immunotherapy. Cancer Discov. 2020;10:232–253. doi: 10.1158/2159-8290.CD-19-0644. [DOI] [PubMed] [Google Scholar]
- 117.Puram S.V., Tirosh I., Parikh A.S., Patel A.P., Yizhak K., Gillespie S., Rodman C., Luo C.L., Mroz E.A., Emerick K.S., et al. Single-Cell Transcriptomic Analysis of Primary and Metastatic Tumor Ecosystems in Head and Neck Cancer. Cell. 2017;171:1611–1624.e1624. doi: 10.1016/j.cell.2017.10.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Sebastian A., Hum N.R., Martin K.A., Gilmore S.F., Peran I., Byers S.W., Wheeler E.K., Coleman M.A., Loots G.G. Single-Cell Transcriptomic Analysis of Tumor-Derived Fibroblasts and Normal Tissue-Resident Fibroblasts Reveals Fibroblast Heterogeneity in Breast Cancer. Cancers. 2020;12:1307. doi: 10.3390/cancers12051307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Bartoschek M., Oskolkov N., Bocci M., Lövrot J., Larsson C., Sommarin M., Madsen C.D., Lindgren D., Pekar G., Karlsson G., et al. Spatially and functionally distinct subclasses of breast cancer-associated fibroblasts revealed by single cell RNA sequencing. Nat. Commun. 2018;9:5150. doi: 10.1038/s41467-018-07582-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Lambrechts D., Wauters E., Boeckx B., Aibar S., Nittner D., Burton O., Bassez A., Decaluwé H., Pircher A., Van den Eynde K., et al. Phenotype molding of stromal cells in the lung tumor microenvironment. Nat. Med. 2018;24:1277–1289. doi: 10.1038/s41591-018-0096-5. [DOI] [PubMed] [Google Scholar]
- 121.Li H., Courtois E.T., Sengupta D., Tan Y., Chen K.H., Goh J.J.L., Kong S.L., Chua C., Hon L.K., Tan W.S., et al. Reference component analysis of single-cell transcriptomes elucidates cellular heterogeneity in human colorectal tumors. Nat. Genet. 2017;49:708–718. doi: 10.1038/ng.3818. [DOI] [PubMed] [Google Scholar]
- 122.Tirosh I., Izar B., Prakadan S.M., Wadsworth M.H., 2nd, Treacy D., Trombetta J.J., Rotem A., Rodman C., Lian C., Murphy G., et al. Dissecting the multicellular ecosystem of metastatic melanoma by single-cell RNA-seq. Science. 2016;352:189–196. doi: 10.1126/science.aad0501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Sahai E., Astsaturov I., Cukierman E., DeNardo D.G., Egeblad M., Evans R.M., Fearon D., Greten F.R., Hingorani S.R., Hunter T., et al. A framework for advancing our understanding of cancer-associated fibroblasts. Nat. Rev. Cancer. 2020;20:174–186. doi: 10.1038/s41568-019-0238-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Blankenstein T., Coulie P.G., Gilboa E., Jaffee E.M. The determinants of tumour immunogenicity. Nat. Rev. Cancer. 2012;12:307–313. doi: 10.1038/nrc3246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Chronopoulos A., Robinson B., Sarper M., Cortes E., Auernheimer V., Lachowski D., Attwood S., García R., Ghassemi S., Fabry B., et al. ATRA mechanically reprograms pancreatic stellate cells to suppress matrix remodelling and inhibit cancer cell invasion. Nat. Commun. 2016;7:12630. doi: 10.1038/ncomms12630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kong F., Li L., Wang G., Deng X., Li Z., Kong X. VDR signaling inhibits cancer-associated-fibroblasts’ release of exosomal miR-10a-5p and limits their supportive effects on pancreatic cancer cells. Gut. 2019;68:950–951. doi: 10.1136/gutjnl-2018-316627. [DOI] [PubMed] [Google Scholar]
- 127.Borazanci E.H., Jameson G., Korn R.L., Caldwell L., Ansaldo K., Hendrickson K., Marceau K., Gosselin K., Hoff D.D.V. Abstract CT152: A Phase II pilot trial of nivolumab (N) + albumin bound paclitaxel (AP) + paricalcitol (P) + cisplatin (C) + gemcitabine (G) (NAPPCG) in patients with previously untreated metastatic pancreatic ductal adenocarcinoma (PDAC) Cancer Res. 2019;79:CT152. doi: 10.1158/1538-7445.Am2019-ct152. [DOI] [Google Scholar]
- 128.Provenzano P.P., Cuevas C., Chang A.E., Goel V.K., Von Hoff D.D., Hingorani S.R. Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell. 2012;21:418–429. doi: 10.1016/j.ccr.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Hingorani S.R., Zheng L., Bullock A.J., Seery T.E., Harris W.P., Sigal D.S., Braiteh F., Ritch P.S., Zalupski M.M., Bahary N., et al. HALO 202: Randomized Phase II Study of PEGPH20 Plus Nab-Paclitaxel/Gemcitabine Versus Nab-Paclitaxel/Gemcitabine in Patients With Untreated, Metastatic Pancreatic Ductal Adenocarcinoma. J. Clin. Oncol. 2018;36:359–366. doi: 10.1200/JCO.2017.74.9564. [DOI] [PubMed] [Google Scholar]
- 130.Hakim N., Patel R., Devoe C., Saif M.W. Why HALO 301 Failed and Implications for Treatment of Pancreatic Cancer. Pancreas. 2019;3:e1–e4. doi: 10.17140/POJ-3-e010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ramanathan R.K., McDonough S.L., Philip P.A., Hingorani S.R., Lacy J., Kortmansky J.S., Thumar J., Chiorean E.G., Shields A.F., Behl D., et al. Phase IB/II Randomized Study of FOLFIRINOX Plus Pegylated Recombinant Human Hyaluronidase Versus FOLFIRINOX Alone in Patients With Metastatic Pancreatic Adenocarcinoma: SWOG S1313. J. Clin. Oncol. 2019;37:1062–1069. doi: 10.1200/JCO.18.01295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Blair A.B., Kim V.M., Muth S.T., Saung M.T., Lokker N., Blouw B., Armstrong T.D., Jaffee E.M., Tsujikawa T., Coussens L.M., et al. Dissecting the Stromal Signaling and Regulation of Myeloid Cells and Memory Effector T Cells in Pancreatic Cancer. Clin. Cancer Res. 2019;25:5351–5363. doi: 10.1158/1078-0432.CCR-18-4192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Radisky E.S., Raeeszadeh-Sarmazdeh M., Radisky D.C. Therapeutic Potential of Matrix Metalloproteinase Inhibition in Breast Cancer. J. Cell. Biochem. 2017;118:3531–3548. doi: 10.1002/jcb.26185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bramhall S.R., Schulz J., Nemunaitis J., Brown P.D., Baillet M., Buckels J.A. A double-blind placebo-controlled, randomised study comparing gemcitabine and marimastat with gemcitabine and placebo as first line therapy in patients with advanced pancreatic cancer. Br. J. Cancer. 2002;87:161–167. doi: 10.1038/sj.bjc.6600446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Bramhall S.R., Rosemurgy A., Brown P.D., Bowry C., Buckels J.A. Marimastat as first-line therapy for patients with unresectable pancreatic cancer: A randomized trial. J. Clin. Oncol. 2001;19:3447–3455. doi: 10.1200/JCO.2001.19.15.3447. [DOI] [PubMed] [Google Scholar]
- 136.Watson S.A., Morris T.M., Robinson G., Crimmin M.J., Brown P.D., Hardcastle J.D. Inhibition of organ invasion by the matrix metalloproteinase inhibitor batimastat (BB-94) in two human colon carcinoma metastasis models. Cancer Res. 1995;55:3629–3633. [PubMed] [Google Scholar]
- 137.Watson S.A., Morris T.M., Collins H.M., Bawden L.J., Hawkins K., Bone E.A. Inhibition of tumour growth by marimastat in a human xenograft model of gastric cancer: Relationship with levels of circulating CEA. Br. J. Cancer. 1999;81:19–23. doi: 10.1038/sj.bjc.6690645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Chanmee T., Ontong P., Izumikawa T., Higashide M., Mochizuki N., Chokchaitaweesuk C., Khansai M., Nakajima K., Kakizaki I., Kongtawelert P., et al. Hyaluronan Production Regulates Metabolic and Cancer Stem-like Properties of Breast Cancer Cells via Hexosamine Biosynthetic Pathway-coupled HIF-1 Signaling. J. Biol. Chem. 2016;291:24105–24120. doi: 10.1074/jbc.M116.751263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Sharma N.S., Gupta V.K., Garrido V.T., Hadad R., Durden B.C., Kesh K., Giri B., Ferrantella A., Dudeja V., Saluja A., et al. Targeting tumor-intrinsic hexosamine biosynthesis sensitizes pancreatic cancer to anti-PD1 therapy. J. Clin. Investig. 2020;130:451–465. doi: 10.1172/JCI127515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Lemberg K.M., Vornov J.J., Rais R., Slusher B.S. We’re Not “DON” Yet: Optimal Dosing and Prodrug Delivery of 6-Diazo-5-oxo-L-norleucine. Mol. Cancer Ther. 2018;17:1824–1832. doi: 10.1158/1535-7163.MCT-17-1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Wong V.W., Rustad K.C., Akaishi S., Sorkin M., Glotzbach J.P., Januszyk M., Nelson E.R., Levi K., Paterno J., Vial I.N., et al. Focal adhesion kinase links mechanical force to skin fibrosis via inflammatory signaling. Nat. Med. 2011;18:148–152. doi: 10.1038/nm.2574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Serrels A., Lund T., Serrels B., Byron A., McPherson R.C., von Kriegsheim A., Gómez-Cuadrado L., Canel M., Muir M., Ring J.E., et al. Nuclear FAK controls chemokine transcription, Tregs, and evasion of anti-tumor immunity. Cell. 2015;163:160–173. doi: 10.1016/j.cell.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Biffi G., Oni T.E., Spielman B., Hao Y., Elyada E., Park Y., Preall J., Tuveson D.A. IL1-Induced JAK/STAT Signaling Is Antagonized by TGFβ to Shape CAF Heterogeneity in Pancreatic Ductal Adenocarcinoma. Cancer Discov. 2019;9:282–301. doi: 10.1158/2159-8290.CD-18-0710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Isambert N., Hervieu A., Rébé C., Hennequin A., Borg C., Zanetta S., Chevriaux A., Richard C., Derangère V., Limagne E., et al. Fluorouracil and bevacizumab plus anakinra for patients with metastatic colorectal cancer refractory to standard therapies (IRAFU): A single-arm phase 2 study. Oncoimmunology. 2018;7:e1474319. doi: 10.1080/2162402X.2018.1474319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Marwitz S., Turkowski K., Nitschkowski D., Weigert A., Brandenburg J., Reiling N., Thomas M., Reck M., Drömann D., Seeger W., et al. The Multi-Modal Effect of the Anti-fibrotic Drug Pirfenidone on NSCLC. Front. Oncol. 2019;9:1550. doi: 10.3389/fonc.2019.01550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Wollin L., Maillet I., Quesniaux V., Holweg A., Ryffel B. Antifibrotic and anti-inflammatory activity of the tyrosine kinase inhibitor nintedanib in experimental models of lung fibrosis. J. Pharmacol. Exp. Ther. 2014;349:209–220. doi: 10.1124/jpet.113.208223. [DOI] [PubMed] [Google Scholar]
- 147.Gabasa M., Ikemori R., Hilberg F., Reguart N., Alcaraz J. Nintedanib selectively inhibits the activation and tumour-promoting effects of fibroblasts from lung adenocarcinoma patients. Br. J. Cancer. 2017;117:1128–1138. doi: 10.1038/bjc.2017.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Diop-Frimpong B., Chauhan V.P., Krane S., Boucher Y., Jain R.K. Losartan inhibits collagen I synthesis and improves the distribution and efficacy of nanotherapeutics in tumors. Proc. Natl. Acad. Sci. USA. 2011;108:2909–2914. doi: 10.1073/pnas.1018892108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Murphy J.E., Wo J.Y., Ryan D.P., Clark J.W., Jiang W., Yeap B.Y., Drapek L.C., Ly L., Baglini C.V., Blaszkowsky L.S., et al. Total Neoadjuvant Therapy With FOLFIRINOX in Combination With Losartan Followed by Chemoradiotherapy for Locally Advanced Pancreatic Cancer: A Phase 2 Clinical Trial. JAMA Oncol. 2019;5:1020–1027. doi: 10.1001/jamaoncol.2019.0892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.De Jesus-Acosta A., Sugar E.A., O’Dwyer P.J., Ramanathan R.K., Von Hoff D.D., Rasheed Z., Zheng L., Begum A., Anders R., Maitra A., et al. Phase 2 study of vismodegib, a hedgehog inhibitor, combined with gemcitabine and nab-paclitaxel in patients with untreated metastatic pancreatic adenocarcinoma. Br. J. Cancer. 2020;122:498–505. doi: 10.1038/s41416-019-0683-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Catenacci D.V., Junttila M.R., Karrison T., Bahary N., Horiba M.N., Nattam S.R., Marsh R., Wallace J., Kozloff M., Rajdev L., et al. Randomized Phase Ib/II Study of Gemcitabine Plus Placebo or Vismodegib, a Hedgehog Pathway Inhibitor, in Patients With Metastatic Pancreatic Cancer. J. Clin. Oncol. 2015;33:4284–4292. doi: 10.1200/JCO.2015.62.8719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Chen X., Song E. Turning foes to friends: Targeting cancer-associated fibroblasts. Nat. Rev. Drug Discov. 2019;18:99–115. doi: 10.1038/s41573-018-0004-1. [DOI] [PubMed] [Google Scholar]
- 153.Nugent F.W., Cunningham C., Barve M.A., Fisher W., Patel H., Meiri E., Oza Y.V., Yang Z., Jurkowski E.C., Uprichard M.J. Phase 2 study of talabostat/gemcitabine in Stage IV pancreatic cancer. J. Clin. Oncol. 2007;25:4616. doi: 10.1200/jco.2007.25.18_suppl.4616. [DOI] [Google Scholar]
- 154.Eager R.M., Cunningham C.C., Senzer N., Richards D.A., Raju R.N., Jones B., Uprichard M., Nemunaitis J. Phase II trial of talabostat and docetaxel in advanced non-small cell lung cancer. Clin. Oncol. (R. Coll. Radiol.) 2009;21:464–472. doi: 10.1016/j.clon.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 155.Hofheinz R.D., al-Batran S.E., Hartmann F., Hartung G., Jäger D., Renner C., Tanswell P., Kunz U., Amelsberg A., Kuthan H., et al. Stromal antigen targeting by a humanised monoclonal antibody: An early phase II trial of sibrotuzumab in patients with metastatic colorectal cancer. Onkologie. 2003;26:44–48. doi: 10.1159/000069863. [DOI] [PubMed] [Google Scholar]
- 156.Penniman L., Parmar S., Patel K. Olaratumab (Lartruvo): An Innovative Treatment for Soft Tissue Sarcoma. Pharm. Ther. 2018;43:267–270. [PMC free article] [PubMed] [Google Scholar]
- 157.Hanley C.J., Mellone M., Ford K., Thirdborough S.M., Mellows T., Frampton S.J., Smith D.M., Harden E., Szyndralewiez C., Bullock M., et al. Targeting the Myofibroblastic Cancer-Associated Fibroblast Phenotype Through Inhibition of NOX4. J. Natl. Cancer Inst. 2018;110:109–120. doi: 10.1093/jnci/djx121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Ford K., Hanley C.J., Mellone M., Szyndralewiez C., Heitz F., Wiesel P., Wood O., Machado M., Lopez M.A., Ganesan A.P., et al. NOX4 Inhibition Potentiates Immunotherapy by Overcoming Cancer-Associated Fibroblast-Mediated CD8 T-cell Exclusion from Tumors. Cancer Res. 2020;80:1846–1860. doi: 10.1158/0008-5472.CAN-19-3158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Mitchem J.B., Brennan D.J., Knolhoff B.L., Belt B.A., Zhu Y., Sanford D.E., Belaygorod L., Carpenter D., Collins L., Piwnica-Worms D., et al. Targeting tumor-infiltrating macrophages decreases tumor-initiating cells, relieves immunosuppression, and improves chemotherapeutic responses. Cancer Res. 2013;73:1128–1141. doi: 10.1158/0008-5472.CAN-12-2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Pienta K.J., Machiels J.P., Schrijvers D., Alekseev B., Shkolnik M., Crabb S.J., Li S., Seetharam S., Puchalski T.A., Takimoto C., et al. Phase 2 study of carlumab (CNTO 888), a human monoclonal antibody against CC-chemokine ligand 2 (CCL2), in metastatic castration-resistant prostate cancer. Investig. New Drugs. 2013;31:760–768. doi: 10.1007/s10637-012-9869-8. [DOI] [PubMed] [Google Scholar]
- 161.Nywening T.M., Wang-Gillam A., Sanford D.E., Belt B.A., Panni R.Z., Cusworth B.M., Toriola A.T., Nieman R.K., Worley L.A., Yano M., et al. Targeting tumour-associated macrophages with CCR2 inhibition in combination with FOLFIRINOX in patients with borderline resectable and locally advanced pancreatic cancer: A single-centre, open-label, dose-finding, non-randomised, phase 1b trial. Lancet Oncol. 2016;17:651–662. doi: 10.1016/S1470-2045(16)00078-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Noel M., O’Reilly E.M., Wolpin B.M., Ryan D.P., Bullock A.J., Britten C.D., Linehan D.C., Belt B.A., Gamelin E.C., Ganguly B., et al. Phase 1b study of a small molecule antagonist of human chemokine (C-C motif) receptor 2 (PF-04136309) in combination with nab-paclitaxel/gemcitabine in first-line treatment of metastatic pancreatic ductal adenocarcinoma. Investig. New Drugs. 2020;38:800–811. doi: 10.1007/s10637-019-00830-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Janson C., Jung H., Ertl L., Liu S., Dang T., Zeng Y., Krasinski A., McMahon J., Zhang P., Charo I., et al. Abstract 5655: Inhibition of CCR2 potentiates checkpoint inhibitor immunotherapy in murine model of pancreatic cancer. Cancer Res. 2017;77:5655. doi: 10.1158/1538-7445.Am2017-5655. [DOI] [Google Scholar]
- 164.Zhou W., Guo S., Liu M., Burow M.E., Wang G. Targeting CXCL12/CXCR4 Axis in Tumor Immunotherapy. Curr. Med. Chem. 2019;26:3026–3041. doi: 10.2174/0929867324666170830111531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Long G.V., Dummer R., Hamid O., Gajewski T.F., Caglevic C., Dalle S., Arance A., Carlino M.S., Grob J.J., Kim T.M., et al. Epacadostat plus pembrolizumab versus placebo plus pembrolizumab in patients with unresectable or metastatic melanoma (ECHO-301/KEYNOTE-252): A phase 3, randomised, double-blind study. Lancet Oncol. 2019;20:1083–1097. doi: 10.1016/S1470-2045(19)30274-8. [DOI] [PubMed] [Google Scholar]
- 166.Siu L.L., Gelmon K., Chu Q., Pachynski R., Alese O., Basciano P., Walker J., Mitra P., Zhu L., Phillips P., et al. Abstract CT116: BMS-986205, an optimized indoleamine 2,3-dioxygenase 1 (IDO1) inhibitor, is well tolerated with potent pharmacodynamic (PD) activity, alone and in combination with nivolumab (nivo) in advanced cancers in a phase 1/2a trial. Cancer Res. 2017;77:CT116. doi: 10.1158/1538-7445.Am2017-ct116. [DOI] [Google Scholar]
- 167.Melisi D., Hollebecque A., Oh D.-Y., Calvo E., Varghese A.M., Borazanci E.H., Mercade T.M., Simionato F., Park J.O., Bendell J.C., et al. A phase Ib dose-escalation and cohort-expansion study of safety and activity of the transforming growth factor (TGF) β receptor I kinase inhibitor galunisertib plus the anti-PD-L1 antibody durvalumab in metastatic pancreatic cancer. J. Clin. Oncol. 2019;37:4124. doi: 10.1200/JCO.2019.37.15_suppl.4124. [DOI] [Google Scholar]
- 168.Strauss J., Heery C.R., Schlom J., Madan R.A., Cao L., Kang Z., Lamping E., Marté J.L., Donahue R.N., Grenga I., et al. Phase I Trial of M7824 (MSB0011359C), a Bifunctional Fusion Protein Targeting PD-L1 and TGFβ, in Advanced Solid Tumors. Clin. Cancer Res. 2018;24:1287–1295. doi: 10.1158/1078-0432.CCR-17-2653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Yoo C., Oh D.Y., Choi H.J., Kudo M., Ueno M., Kondo S., Chen L.T., Osada M., Helwig C., Dussault I., et al. Phase I study of bintrafusp alfa, a bifunctional fusion protein targeting TGF-β and PD-L1, in patients with pretreated biliary tract cancer. J. Immunother Cancer. 2020;8 doi: 10.1136/jitc-2020-000564. [DOI] [PMC free article] [PubMed] [Google Scholar]