Abstract
Liver transplantation during the COVID-19 pandemic is challenging. Both donor and recipient issues can be influenced by the risks attributed to the pandemic. Allocation policy may need to be modified and criteria may be influenced by local infection rates and availability of medical facilities. Modifying immunosuppression (IS) protocols is controversial and is not evidence-based. In this study, we review the published literature on liver transplant recipients who were infected with COVID-19.
A literature review was performed using PubMed, ScienceDirect, and WHO databases to identify relevant English-language articles published up to May 20, 2020.
Fifteen articles reported 120 liver transplant recipients who were infected with COVID-19. Only 10 papers with 22 patients reported full encounter characteristics. Four papers reported 23, 17, 13, and 6 patients, respectively, but with minimal data. One paper reported the authors’ own 39 patients’ characteristics and demographics. The mean age was 58.2 years with 66% males. The most commonly reported presentations in descending order were fever (91%), cough (36.7%), shortness of breath (SOB) (31.8%), and diarrhea (31.8%). Liver transplant patients infected with COVID-19 were maintained on Tac (79%), mycophenolate (MMF) (48.4%), and Prednisone (29.6%) and were managed by reducing MMF in 14.3% of patients and reducing Tac in 14.3% of patients; 28.6% of patients needed ICU admission, 13.6% of patients had died, and the reported general population COVID-19 mortality rate was 3.4%.
The clinical presentation of COVID-19 in liver transplant recipients may be different from the general population, with higher rates of severe disease, complications, and mortality.
MeSH Keywords: COVID-19, Liver Transplantation, Organ Transplantation, SARS Virus
Background
Coronavirus disease 2019 (COVID-19) is caused by the severe acute respiratory syndrome coronavirus type 2 (SARS-CoV2) [1]. The disease was initially confirmed in China and then rapidly spread worldwide with more than 4.8 million infected individuals and over 300 000 deaths worldwide [2]. This disease is especially deadly in elderly patients (over 70 years old) with comorbidities [3]. Most published data regarding COVID-19 and organ transplant recipients are nonspecific and lack quality evidence. Data on demographics, characteristics, and clinical presentations of COVID-19 in organ transplant recipients are scarce. In the present study, we review the published literature regarding liver transplant patients who were infected with COVID-19.
Material and Methods
Literature Search
A systematic literature review was performed using PubMed and ScienceDirect databases to identify relevant English-language articles published through May 20, 2020. Search terms were COVID-19, coronavirus, severe acute respiratory syndrome coronavirus 2, 2019-nCoV, SARS-CoV-2, SARS-CoV, MERS-CoV, liver transplantation, and liver transplant. All article types were included: case reports, case series, commentaries, and review articles. A search in the database of the COVID-19 Global Research on Coronavirus Disease section of the WHO website through May 20, 2020 was performed using the following criteria: liver transplantation or liver transplant with English language as limit or filter [4]. Additional articles were retrieved by screening the reference lists of the included studies. The search strategy was approved and reviewed by all authors.
Eligibility criteria and study selection
The authors independently reviewed the titles and abstracts for inclusion. Figure 1 displays the flow diagram for this systematic review, based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 [5]. Databases were screened, filtered, and assessed for eligibility. Cases of COVID-19 in liver transplant patients were included in this study. Articles with unrelated topics and/or with missed information were excluded.
Figure 1.
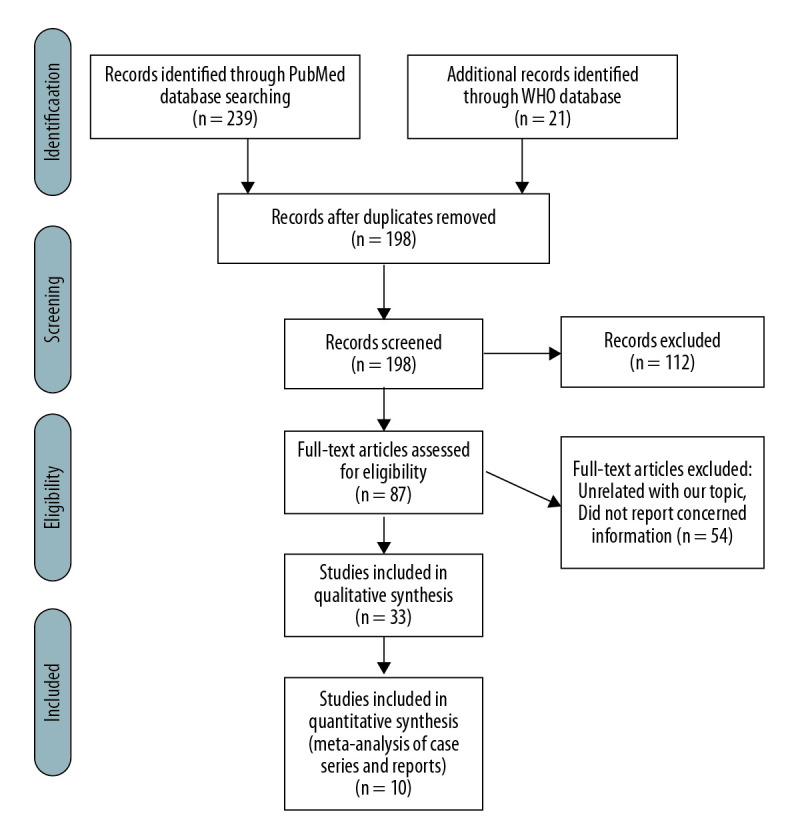
PRISMA flow chart for the present study.
Risk of bias
The National Institutes of Health Quality Assessment Tool for Case Series Studies was used to qualify the reviewed articles [6]. Table 1 shows the results of the 2 reviewers who independently rated the quality of the included studies.
Table 1.
Quality ratings of included studies according to NIH Quality Assessment Tool for case series studies.
| Study | Q 1 | Q 2 | Q 3 | Q 4 | Q 5 | Q 6 | Q 7 | Q 8 | Q 9 | Reviewer 1 | Reviewer 2 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Zhong | Yes | No | CD | Yes | CD | Yes | No | Yes | Yes | Fair | Fair |
| Liu | Yes | Yes | NA | NA | Yes | Yes | No | NA | Yes | Fair | Fair |
| Huang | Yes | Yes | CD | No | Yes | Yes | Yes | NA | Yes | Fair | Fair |
| Qin | Yes | Yes | CD | Yes | Yes | Yes | Yes | NA | Yes | Fair | Fair |
| Morand | Yes | Yes | NA | NA | No | Yes | No | NA | Yes | Fair | Fair |
| Lagana | Yes | Yes | CD | Yes | Yes | Yes | Yes | NA | No | Fair | Fair |
| Kates | Yes | Yes | NA | NA | Yes | Yes | Yes | NA | Yes | Fair | Fair |
| Hammami | Yes | Yes | NA | NA | Yes | Yes | No | NA | Yes | Fair | Fair |
| Fernández-Ruiz | Yes | No | NA | NA | No | Yes | No | NA | Yes | Fair | Fair |
| Donato | Yes | NO | CD | Yes | No | Yes | Yes | Yes | Yes | Fair | Fair |
NIH – National Institutes of Health: NR – not reported: CD – cannot determine; NA – not applicable. The NIH Quality Assessment Tool for Case Series Studies poses nine questions: 1=Was the study question or objective clearly stated?, 2=Was the study population clearly and fully described, including a case definition?, 3=Were the cases consecutive?, 4=Were the subjects comparable?, 5=Was the intervention clearly described?, 6=Were the outcome measures clearly defined, valid, reliable, and implemented consistently across all study participants?, 7=Was the length of follow-up adequate?, 8=Were the statistical methods well-described?, 9=Were the results well-described?
Data extraction and synthesis
Data were independently extracted from reports by 2 reviewers. All reported patients’ demographic and clinical characteristics (country, age, sex, time from transplant, comorbidities, clinical presentation and maximum body temperature, initial laboratory values, baseline immunosuppressant medications (ISM), need for intensive care unit (ICU), duration of illness, and outcomes) were extracted, collected, and analyzed. Due to the lack of sufficient data, we did not perform a meta-analysis to assess the association of various patients’ findings with demographic data, disease and patient characteristics, or outcomes. The principal summary measures used were the median, mean, standard deviation, and incidence.
Results
Overview of the included studies
A total of 260 articles were retrieved using the search strategy. After removing duplicate articles, 198 articles were screened, of which 112 articles were excluded due to unrelated content. The remaining 87 articles were assessed for eligibility through full-text screening, then 54 articles were excluded due to unrelated content or lack of relevant information. There were 33 articles included but only 15 articles reported liver transplant recipients infected with COVID-19 (Figure 1). Of these 15 articles, there were 2 case series and 8 case reports that reported a total of 22 liver transplant patients. Four articles reported 23, 17, 13, and 6 patients, respectively, but with minimal data [7–10]. One paper reported the authors’ own 39 patients’ characteristics and demographics [11] and was used in Table 2 for comparison and to extract pooled measurements. The remaining 18 articles were commentaries and review articles. Patients’ characteristics and demographics were included in Tables 3–7.
Table 2.
Clinical characteristics of the 22 reported liver transplant patients infected with COVID-19 compared with previous published studies.
| Variable | This study | Webb et al. [11] | Pooled (mean) |
|---|---|---|---|
| Number of patients | 22 | 39 | 61 |
| Age (Mean) | 55.96 | 60.50 | 58.25 |
| Sex | |||
| Male | 68.2% | 64.1% | 66.15% |
| Liver transplant years age (mean) | 8.75 | 5.5 | 7.125 |
| Comorbidities | |||
| HTN | 18.2% | 46.2% | 32.2% |
| DM | 22.7% | 38.5% | 30.6% |
| Heart disease | 22.7% | 15.4% | 19% |
| Obesity | 4.6% | 25.7% | 15.15% |
| Baseline Immunosuppression | |||
| Tacrolimus | 68.2% | 89.7% | 79% |
| Mycophenolate mofetil | 45.5% | 51.3% | 48.4% |
| Prednisone | 18.2% | 41% | 29.6% |
Table 3.
Characteristics of all available reported liver transplant recipients infected with COVID-19.
| Study; Country | Age | Sex | Time from transplant (years) | Comorbidities | Clinical presentation | Highest temp (°C) | Baseline ISM |
|---|---|---|---|---|---|---|---|
| Zhong; China [30] | 37 | M | 9 days | Fever 38.6°C, Weakness, Abdominal discomfort, sleep disorders | 38.6 | Tac, IVMP | |
| Liu; China [31] | 50 | M | 2.5 | Fever 37.7°C, SOB, | 39.6 | Tac, | |
| Huang; China [32] | 59 | M | 2.7 | Fever 40, Cough, Chills, Fatigue, Diarrhea, Jaundice, Splenomegaly, Ascites, | 40 | Tac, MMF | |
| Qin; China [33] | 37 | M | 12 days | Fever 39, | 39 | Tac, Pred | |
| Morand; France [34] | 4.6 | F | 5 months | Fever, Cough, SOB, Rhinitis, | Tac | ||
| Lagana; USA [35] | 6 months | F | 2 days | Fever, SOB, Diarrhea | MMF | ||
| Kates; USA [36] | 67 | M | 19 | Fever, Cough, Fatigue, confusion, Diarrhea, Wheezing | cyclosporine | ||
| Hammami; USA [37] | 63 | M | 9.5 | HTN, DM, ESRD, PVD, CHF, | Fever 38.3, Cough, Headache, Fatigue, Myalgia, Chest pain, Chills, Abdominal pain, | 39.1 | Tac, |
| Fernández-Ruiz; Spain [38] | 63 | M | 7.9 | HTN, DM | Fever, SOB, Cough, Myalgia, Fatigue, Diarrhea | everolimus | |
| 72 | M | 5.5 | HTN, DM, Obesity, | Fever, SOB, Cough, | MMF, everolimus | ||
| 79 | F | 15.3 | DM, ESRD, | SOB, Cough, Fatigue, Diarrhea | Everolimus, Pred, azathioprine | ||
| 73 | M | 16.4 | DM, Asthma, bronchiectasis | Fever, SOB, Cough, Fatigue, | MMF | ||
| 76 | F | 26.5 | HTN | Fever, Chest pain | Tac | ||
| 46 | F | 6.4 | Diarrhea | Tac | |||
| Donato; Italy [39] | 60 | M | 3 | Fever, Respiratory symptoms | Tac, MMF | ||
| 78 | M | 19.1 | Heart Disease | Fever, Respiratory symptoms | Tac, MMF | ||
| 65 | M | 5.4 | Lung disease | Fever, Respiratory symptoms | Pred | ||
| 57 | M | 15.6 | Heart and lung diseases | Fever, Respiratory symptoms | Tac, MMF | ||
| 57 | M | 8 | Fever, Respiratory symptoms | Tac, MMF | |||
| 62 | F | 11.4 | Lung disease | Fever, Respiratory symptoms | Tac, MMF | ||
| 75 | M | 17.6 | Heart disease | Fever, Diarrhea | Tac, MMF | ||
| 50 | F | 3 months | Heart and lung diseases | Fever, Respiratory symptoms | Tac, Pred |
Table 4.
Laboratory characteristics of all available reported liver transplant recipients infected with COVID-19.
| Study | Initial bilirubin (μmol/L) | Highest bilirubin | Initial WBC | Initial LC | Initial PLT | Initial CRP | Initial AST | Highest AST | Initial ALT | Highest ALT |
|---|---|---|---|---|---|---|---|---|---|---|
| Zhong | 38.9 | 103.7 | 2.46 | 0.48 | 74 | 122 | 240 | 424 | ||
| Liu | 5.9 | 0.42 | 32.1 | N | N | |||||
| Huang | 83.9 | 528.8 | 3.2 | 0.7 | 35.1 | 60 | ||||
| Qin | 0.64 | 132 | 80 | |||||||
| Morand | 3.2 | 120 | 224 | |||||||
| Lagana | 163 | 908 | 215 | 1253 | ||||||
| Kates | 1.93 | 0.9 | 39 | 12 | ||||||
| Hammami | 4.1 | 0.77 | 71 | 11 | 21 | 17 |
Table 5.
Management and outcomes of all available reported liver transplant recipients infected with COVID-19.
| Study | ISM management | COVID-19 targeted management | ICU | Complications | Outcome |
|---|---|---|---|---|---|
| Zhong | Tac held; IVMP | Oseltamivir, Abx, | Yes | None | Recovered, 40d |
| Liu | Tac held; IVMP | Umifenovir, lopinavir/ritonavir, IVIG, Abx, INF-a | No | None | Recovered, 35d |
| Huang | Reduced Tac, MMF; IVMP | Umifenovir, lopinavir/ritonavir, Abx, INF-a | Respiratory failure, AKI, MOF, | Died, 45d | |
| Qin | No change | Oseltamivir, IVIG, rh-GCSF, Abx | Recovered, 53d | ||
| Morand | Reduced Tac | Paracetamol | Recovered, 11d | ||
| Lagana | Reduced MMF | Hydroxychloroquine | Yes | None | Hospitalized, 16d |
| Kates | No change | Yes | AKI | Recovered, 6d | |
| Hammami | No change | Hydroxychloroquine, Azithromycin, Abx, tocilizumab | Recovered, 16d | ||
| Fernández-Ruiz | Held EVE and start Tac, MMF | Hydroxychloroquine, lopinavir/ritonavir | Recovered, 19d | ||
| Held EVE, MMF and start Tac | Hydroxychloroquine, lopinavir/ritonavir, IFN-b | AKI, ARDS, | Died, 7d | ||
| No change | Hydroxychloroquine, IFN-b | Recovered, 14d | |||
| Held MMF | Yes | ARDS, Refractory shock | Died, 24d | ||
| No change | Hydroxychloroquine | Recovered, 15d | |||
| No change | Recovered, 18d | ||||
| Donato | 6 Recovered, 2 Hospitalized |
Table 6.
Clinical characteristics for the 22 reported liver transplant patients infected with COVID-19.
| Variable (n=22) | Value |
|---|---|
| Age (mean, range) | 55.96 (0.5–79) |
| Sex, Male | 15/22 (68.2%) |
| Liver transplant years age (mean, range) | 8.75 (0.005–26) |
| Within 1 year | 5/22 (22.7%) |
| Beyond 1 year | 17/22 (77.2%) |
| Comorbidities | |
| HTN | 4/22 (18.2%) |
| DM | 5/22 (22.7%) |
| Lung disease | 5/22 (22.7%) |
| Heart disease | 5/22 (22.7%) |
| Obesity | 1/22 (4.6%) |
| None or N/A | 9/22 (40.9%) |
| Clinical presentation | |
| Fever | 20/22 (90.9%) |
| Max. temp (average, SD) | 39.26 (±0.54) |
| Cough | 8/22 (36.7%) |
| SOB | 7/22 (31.8%) |
| Unspecified respiratory symptoms | 7/22 (31.8%) |
| Fatigue | 6/22 (27.3%) |
| Diarrhea | 7/22 (31.8%) |
| Laboratory | |
| White cell count | |
| Median (SD) per l | 3.2×109 (±1.56×109) |
| Leukopenia (<4×109/l) | 3/5 (60%) |
| Lymphocyte count | |
| Median (SD) per l | 0.67×109 (±0.18×109) |
| Lymphopenia (<1×109/l) | 6/6 (100%) |
| Initial C-reactive protein (CRP) | |
| Median (SD) | 21.5 (±15.6) |
| High CRP (>5 mg/dl) | 3/4 (75%) |
| Initial ALT | |
| Median (SD) | 80 (±101) |
| High ALT (>50 U/l) | 5/7 (71.4%) |
| Initial AST | |
| Median (SD) | 120 (±61.7) |
| High AST (>54 U/l) | 3/5 (60%) |
Table 7.
Management and outcomes of the 22 reported liver transplant patients infected with COVID-19.
| Variable | Value |
|---|---|
| Baseline Immunosuppression | |
| Tacrolimus | 15/22 (68.2%) |
| Mycophenolate mofetil | 10/22 (45.5%) |
| Prednisone | 4/22 (18.2%) |
| Azathioprine | 1/22 (4.5%) |
| Everolimus | 3/22 (13.6%) |
| Ciclosporin | 1/22 (4.5%) |
| Management | |
| Immunosuppression | |
| Held tacrolimus | 2/14 (14.3%) |
| Reduced tacrolimus | 2/14 (14.3%) |
| No change tacrolimus | 4/14 (28.6%) |
| Held mycophenolate mofetil | 1/14 (7.1%) |
| Reduced mycophenolate mofetil | 2/14 (14.3%) |
| Prednisone | No change 2 |
| Azathioprine | No change 1 |
| Everolimus | Held 2 |
| Ciclosporin | No change 1 |
| Other Tx | |
| Lopinavir/Ritonavir | 4/14 (28.6%) |
| Hydroxychloroquine | 6/14 (42.9%) |
| Azithromycin | 1/14 (7.1%) |
| Oseltamivir | 2/14 (14.3%) |
| Antibiotics | 5/14 (35.7%) |
| Intravenous methylprednisolone | 3/14 (21.4%) |
| Intravenous immunoglobulin | 2/14 (14.3%) |
| Interferon a,b | 4/14 (28.6%) |
| Tocilizumab | 1/14 (7.1%) |
| ICU admission | 4/14 (28.6%) |
| Outcomes | |
| Clinically recovered/discharged | 16/22 (72.7%) |
| Illness days duration (median, range) | 17 (6–53) |
| Alive but suffers/In hospital | 3/22 (13.6%) |
| Illness days duration (median) | 16 |
| Death | 3/22 (13.6%) |
| Illness days duration (median, range) | 24 (7–45) |
Patients demographics and characteristics
Ten articles reported 22 liver transplant patients infected with COVID-19. There were 8 from Italy, 6 from Spain, 4 from China, 3 from the USA, and 1 from France. There were 15 (68.2%) males. The mean age was 55.96 (0.5–79) years. The mean post-transplant period was 8.75 (0.005–26) years, and 22.7% of patients were within the first year after transplantation. The most common reported comorbidities were diabetes mellitus in 22.7%, heart disease in 22.7%, lung disease in 22.7%, HTN in 18.2%, and obesity in 4.6%, and 40.9% of patients had no reported comorbidities.
Clinical presentation
The most frequently reported clinical presentation was fever; it was reported in 90.9%, with a mean maximum temperature of 39.26°C (±0.54). Other reported clinical symptoms were cough (36.7%), shortness of breath (31.8%), unspecified respiratory symptoms (31.8%), diarrhea (31.8%), and fatigue (27.3%). Less frequently reported symptoms included headache, dizziness, weakness, abdominal discomfort, sleep disorders, chills, rhinitis, confusion, myalgia, and chest pain.
Laboratory results
The initial white blood cell count median was 3.2×103 (±1.56×103). The initial median lymphocyte cell count was 0.67×103 (±0.18×103). Initial leukopenia and lymphopenia were reported in 60% and 100%, respectively. The median initial CRP was 21.5 (±15.6) mg/L, and high CRP (>5 mg/dl) levels were noted in 75%. High ALT (>50 U/l) and AST (>54 U/l) were reported in 71.4% and 60%, respectively.
Immunosuppression management
Patients were treated with different IS regimens. Tacrolimus (Tac) was prescribed in 68.2% of patients and discontinued in 14.3%, reduced in 14.3%, and not changed in 28.6%. MMF was prescribed in 45.5% of patients and discontinued in 7.1% and reduced in 14.3%. The exact MMF management was not reported in the remaining 79% of patients. Pred was prescribed in 18.2% of patients and not changed in 50% of patients; the exact Pred management was not reported in the remaining 50% of patients. Other baseline ISMs were Azathioprine, Everolimus, and Cyclosporin. These medications were held in some patients and not changed in others; 27.2% of patients had no change in ISM and recovered.
Deceased patients were prescribed MMF in 100%, Tac in 33.3%, and EVE in 33.3% and had their ISM held (MMF 66.6%; EVE 100%) or reduced (MMF 33.3%; Tac 33.3%).
COVID-19 directed management
Treatment targeted COVID-19 included hydroxychloroquine (42.9%), antibiotics (35.7%), lopinavir/ritonavir (28.6%), INF-a,b (28.6%), intravenous methylprednisolone (21.4%), intravenous immunoglobulin (14.3%), oseltamivir (14.3%), azithromycin (7.1%), and tocilizumab (7.1%). COVID-19 targeting treatment used in patients who died included antibiotics (33.3%), hydroxychloroquine (33.3%), lopinavir/ritonavir (66.6%), INF-a,b (66.6%), and umifenovir (33.3%).
Patients outcomes
Intensive care unit (ICU) admission occurred in 28.6% of patients, 72.7% of patients had recovered and were discharged with a median illness duration of 17 days (range, 6–53 days), 13.6% of patients were alive and hospitalized at the time of publication with a median illness duration of 16 days, and 13.6% of patients had died with a median illness duration of 24 days (range, 7–45 days).
Characteristics of patients who died
The mean age of patients who dies was 68 years, 66.6% of patients were older than 65 years, 100% of patients were male, and the mean time from transplant was 8.2 years. Diabetes mellitus, hypertension (HTN), obesity, asthma, and bronchiectasis were reported in these patients; 66.6% had lymphopenia and 66.6% had high CRP serum levels. ARDS and acute renal failure were reported in 100% and 66.6% of patients, respectively.
Pooled results
One study reported 39 patients without demographics and characteristics for each patient and these were thus not included in our tabulated results. However, the study was used to draw pooled measures for all reported liver transplant patients infected with COVID-19 in the literature. A total of 61 liver transplant patients with COVID-19 used in the comparison. The age mean was 58.25 years and 66.15% were males. The mean age at transplant was 7.13 years. HTN, DM, heart disease, and obesity were reported in 32.2%, 30.6%, 19%, and 15.1% of patients, respectively. Liver transplant patients infected with COVID-19 were maintained on Tac (79%), MMF (48.4%), and Pred (29.6%).
Discussion
Most published reports on COVID-19 in organ transplant recipients are nonspecific and lack quality evidence. Data on demographics, characteristics, and clinical presentations of COVID-19 in organ transplant recipients is scarce. However, it is well known that among patients with advanced age and medical comorbidities, COVID-19 is frequently severe. Studies have reported that COVID-19 can present differently in immunosuppressed patients, including organ transplant recipients.
Fever in COVID-19 in the general population is reported in 99% of patients [12,13]. Our study has shown that 9% of the liver transplant patients did not have fever on presentation or during their hospitalization. On the other hand, cough, SOB, myalgia, headache, sore throat, and gastrointestinal symptoms were different in incidence from the typical COVID-19 presentation [12–15]. Additionally, this review shows that there are several unreported symptoms that can appear in the COVID-19-positive liver transplant patients, including chest tightness and pain and jaundice [14]. Notably, the unreported chest tightness and pain in other cohorts have an incidence of 9% in this cohort.
COVID-19 causes pneumonia that can be severe enough to be lethal, especially in patients with advanced age or underlying medical comorbidities [16]. Those comorbidities include cardiovascular disease, diabetes mellitus, HTN, chronic lung disease, cancer, chronic kidney disease, and obesity (body mass index ≥30) [3,16]. Liver transplant patients infected with COVID-19 are a fragile and high-risk group due to immunosuppression and common comorbidities. In this review, 60% of patients had comorbidities. These comorbidities predispose these patients to a more severe COVID-19 infection. The attendant IS is an additional risk factor for severe disease. Liver transplant recipients and candidates are in a high-risk group due to the high incidence and prevalence of hypertension, renal failure, diabetes, obesity, and advanced age in this group.
It was previously reported that a progressive decline in lymphocyte count was observed in non-survivors compared to more stable levels in survivors [12]. In the present study, 100% of patients who died had lymphopenia. Given the fact that ISM can induce lymphopenia, many liver transplant patients have a baseline lymphopenia that might further deteriorate and worsen the prognosis [17,18].
Several studies and a report from the Chinese Center for Disease Control and Prevention have classified COVID-19 severity in the general population [19,20] as mild, severe, and critical disease in 81%, 14%, and 5% of patients, respectively. In this report, severe disease defined by SOB and/or hypoxemia was reported in 31.3% of patients.
The WHO reported that recovery time appears to be around 2 weeks for mild infections and 3 to 6 weeks for severe disease [21]. In the present study, we found that 72% of patients recovered clinically from the COVID-19, with a median duration of illness of 17 (6–53) days. Rates of ICU admission were reported to range between 5% and 12% in the general population [22]. In our cohort, 28.6% of patients were admitted to the ICU.
The most recently reported mortality rate of COVID-19 was 3.77% [23]. The mortality rate of liver transplant patients infected with COVID-19 in this cohort was 13.6% (3 out of 22 patients). Despite the small number of patients included in the present study, this high mortality indicates that COVID-19 in liver transplant patients may portend an ominous outcome. Surprisingly, 17.6% of patients with time from transplant longer than 1 year had died, while there were no deaths within the first year of transplantation. This is despite the fact that the first year is fraught with postoperative complications and higher immunosuppression.
It was reported that 81% of COVID-19 patients present with mild disease and can be managed at home, and those with severe and critical COVID-19 disease should be managed with prompt hospitalization while ensuring appropriate infection control and supportive care [19,24,25]. The hospitalized patients should be managed with empiric treatment for bacterial pneumonia in selected patients, prevention of venous thromboembolism, and avoiding nebulized medications. The WHO and CDC recommend against use of systemic glucocorticoids in COVID-19 patients unless there are other indications [24,25]. To date, all suggested medications are under investigation, with no proven efficacy against COVID-19. These medications include Remdesivir, hydroxychloroquine/chloroquine, azithromycin, hydroxychloroquine, convalescent plasma, tocilizumab, favipiravir, interferon beta, and lopinavir/ritonavir. Most of our cohort were hospitalized and could not be managed at home due to the severity of the disease. They were managed with hydroxychloroquine (42.9%), antibiotics (35.7%), lopinavir/ritonavir (28.6%), INF-a,b (28.6%), intravenous methylprednisolone (21.4%), intravenous immunoglobulin (14.3%), oseltamivir (14.3%), azithromycin (7.1%), and tocilizumab (7.1%).
The effect of IS on the progression of COVID-19 is unclear. There are 2 aspects that should not be ignored when dealing with IS and COVID-19. First, it was proved that COVID-19 patients have a high prevalence of lymphopenia [26] but its unclear whether lymphopenia is a risk factor for COVID-19 or is a result of it. Second, it is thought that the severity of COVID-19 may be the result of a hyperinflammatory response (cytokine storm). Thus, the role of immunomodulation may have a positive and not just a negative effect in the treatment of severe cases [27,28].
Interestingly, a recent Italian report by Lorezo D’Antiga concluded that immunocompromised patients do not have an increased risk of developing severe pulmonary disease compared to the general population [29]. Nevertheless, it is evident from this study that liver transplant patients are at an increased risk for serious, critical, and fatal disease when infected with COVID-19.
Conclusions
Liver transplant patients may have an atypical clinical presentation of COVID-19 infection. Fever may be absent while other atypical symptoms may prevail. Therefore, a high index of suspicion for COVID-19 and perhaps even surveillance in this population may help in early diagnosis and prevention of further transmission. The role of IS therapy should be assessed in every case individually.
Footnotes
Conflicts of interest
None.
Source of support: Departmental sources
References
- 1.World Health Organization (WHO) Novel coronavirus (2019 nCoV) 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 2.World Health Organization (WHO) Coronavirus disease 2019 (COVID-19) Situation Report – 88. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200417-sitrep-88-covid-191b6cccd94f8b4f219377bff55719a6ed.pdf?sfvrsn=ebe78315_6.
- 3.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395(10229):1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO) COVID-19 global literature on coronavirus disease. 2020. https://search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/
- 5.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Heart Blood Institute. Study quality assessment tools. 2020. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
- 7.Boyarsky BJ, Chiang TPY, Werbel WA, et al. Early impact of COVID-19 on transplant center practices and policies in the United States. Am J Transplant. 2020;20(7):1809–18. doi: 10.1111/ajt.15915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maggi U, De Carlis L, Yiu D, et al. The impact of the COVID-19 outbreak on Liver Transplantation programmes in Northern Italy. Am J Transplant. 2020;20(7):1840–48. doi: 10.1111/ajt.15948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pereira MR, Mohan S, Cohen DJ, et al. COVID-19 in Solid Organ Transplant Recipients: Initial Report from the US Epicenter. Am J Transplant. 2020;20(7):1800–8. doi: 10.1111/ajt.15941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhoori S, Rossi RE, Citterio D, et al. COVID-19 in long-term liver transplant patients: Preliminary experience from an Italian transplant centre in Lombardy. Lancet Gastroenterol Hepatol. 2020;5(6):532–33. doi: 10.1016/S2468-1253(20)30116-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Webb GJ, Moon AM, Barnes E, et al. Determining risk factors for mortality in liver transplant patients with COVID-19. Lancet Gastroenterol Hepatol. 2020;5(7):643–44. doi: 10.1016/S2468-1253(20)30125-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus – infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–69. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization (WHO) Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19) 2020. https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-fnal-report.pdf.
- 15.Cheung KS, Hung IFN, Chan PPY, et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from the Hong Kong cohort and systematic review and meta-analysis. Gastroenterology. 2020;159(1):81–95. doi: 10.1053/j.gastro.2020.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [Online ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Banerjee D, Popoola J, Shah S, et al. COVID-19 infection in kidney transplant recipients. Kidney Int. 2020;97(6):1076–82. doi: 10.1016/j.kint.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen S, Yin Q, Shi H, et al. A familial cluster, including a kidney transplant recipient, of Coronavirus Disease 2019 (COVID-19) in Wuhan, China. Am J Transplant. 2020;20(7):1869–74. doi: 10.1111/ajt.15903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–81. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kujawski SA, Wong KK, Collins JP, et al. First 12 patients with coronavirus disease 2019 (COVID-19) in the United States. MedRxiv. 2020 doi: 10.1038/s41591-020-0877-5. 20032896. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization. Director-General’s opening remarks at the media briefing on COVID-19. Feb 24, 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-themedia-briefng-on-covid-19---24-february-2020.
- 22.Grasselli G, Pesenti A, Cecconi M, et al. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: Early experience and forecast during an emergency response. JAMA. 2020 doi: 10.1001/jama.2020.4031. [Online ahead of print] [DOI] [PubMed] [Google Scholar]
- 23.Zhang J, Wang X, Jia X, et al. Risk factors for disease severity, unimprovement, and mortality of COVID-19 patients in Wuhan, China. Clin Microbiol Infect. 2020;26(6):767–72. doi: 10.1016/j.cmi.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Interim clinical guidance for management of patients with confirmed 2019 novel coronavirus (2019-nCoV) infection. 2020 [Google Scholar]
- 25.World Health Organization. Home care for patients with suspected novel coronavirus (nCoV) infection presenting with mild symptoms and management of contacts. 2020. [Google Scholar]
- 26.Guan W, Ni Z, Hu Y, et al. Clinical characteristics of 2019 novel coronavirus infection in China. MedRxiv. 2020 20020974. [Google Scholar]
- 27.Ritchie AI, Singanayagam A. Immunosuppression for hyperinflammation in COVID-19: a double-edged sword? Lancet (London, England) 2020;95:1111. doi: 10.1016/S0140-6736(20)30691-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Booth CM, et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA. 2003;289(12):2801–9. doi: 10.1001/jama.289.21.JOC30885. [DOI] [PubMed] [Google Scholar]
- 29.D’Antiga L. Coronaviruses and immunosuppressed patients: The facts during the third epidemic. Liver Transpl. 2020;26(6):832–34. doi: 10.1002/lt.25756. [DOI] [PubMed] [Google Scholar]
- 30.Zhong Z, Zhang Q, Xia H, et al. Clinical characteristics and immunosuppressant management of coronavirus disease 2019 in solid organ transplant recipients. Am J Transplant. 2020;20(7):1916–21. doi: 10.1111/ajt.15928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bin L, Wang Y, Zhao Y, et al. Successful treatment of severe COVID-19 pneumonia in a liver transplant recipient. Am J Transplant. 2020;20(7):1891–95. doi: 10.1111/ajt.15901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang J-F, Zheng KI, George J, et al. Fatal outcome in a liver transplant recipient with COVID-19. Am J Transplant. 2020;20(7):1907–10. doi: 10.1111/ajt.15909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qin J, Wang H, Qin X, et al. Perioperative presentation of COVID-19 disease in a liver transplant recipient. Hepatology. 2020 doi: 10.1002/hep.31257. [Online ahead of print] [DOI] [PubMed] [Google Scholar]
- 34.Morand A, Roquelaure B, Colson P, et al. Child with liver transplant recovers from COVID-19 infection. A case report. Arch Pediatr. 2020;27(5):275–76. doi: 10.1016/j.arcped.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lagana SM, De Michele S, Lee MJ, et al. COVID-19 associated hepatitis complicating recent living donor liver transplantation. Arch Pathol Lab Med. 2020 doi: 10.5858/arpa.2020-0186-SA. [Online ahead of print] [DOI] [PubMed] [Google Scholar]
- 36.Kates OS, Fisher CE, Stankiewicz-Karita HC, et al. Earliest cases of coronavirus disease 2019 (COVID-19) identified in solid organ transplant recipients in the United States. Am J Transplant. 2020;20(7):1885–90. doi: 10.1111/ajt.15944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hammami MB, Garibaldi B, Shah P, et al. Clinical course of COVID-19 in a liver transplant recipient on hemodialysis and response to tocilizumab therapy: A case report. Am J Transplant. 2020;20(8):2254–59. doi: 10.1111/ajt.15985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fernández-Ruiz M, Andrés A, Loinaz CA, et al. COVID-19 in solid organ transplant recipients: a single-center case series from Spain. Am J Transplant. 2020;20(7):1849–58. doi: 10.1111/ajt.15929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Donato MF, Invernizzi F, Lampertico P, Rossi G. Health status of liver transplanted patients during the coronavirus outbreak in Italy: a large single center experience from Milan. Clin Gastroenterol Hepatol. 2020 Apr 01;18 doi: 10.1016/j.cgh.2020.04.041. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]


