Abstract
Background and Purpose: The European Association of Urology guidelines recommend restaging transurethral resection of bladder tumours (reTURB) 2–6 weeks after primary TURB. However, in clinical practice some patients undergo a second TURB procedure after Bacillus Calmette-Guérin immunotherapy (BCG)induction. To date, there are no studies comparing post-BCG reTURB with the classic pre-BCG approach. The aim of this study was to assess whether the performance of reTURB after BCG induction in T1HG bladder cancer is related to potential oncological benefits. Materials and Methods: Data from 645 patients with primary T1HG bladder cancer treated between 2001 and 2019 in 12 tertiary care centres were retrospectively reviewed. The study included patients who underwent reTURB before BCG induction (Pre-BCG group: 397 patients; 61.6%) and those who had reTURB performed after BCG induction (Post-BCG group: 248 patients, 38.4%). The decision to perform reTURB before or after BCG induction was according to the surgeon’s discretion, as well as a consideration of local proceedings and protocols. Due to variation in patients’ characteristics, both propensity-score-matched analysis (PSM) and inverse-probability weighting (IPW) were implemented. Results: The five-year recurrence-free survival (RFS) was 64.7% and 69.1% for the Pre- and Post-BCG groups, respectively, and progression-free survival (PFS) was 82.7% and 83.3% for the Pre- and Post-BCG groups, respectively (both: p > 0.05). Similarly, neither RFS nor PFS differed significantly for a five-year period or in the whole time of observation after the PSM and IPW matching methods were used. Conclusions: Our results suggest that there might be no difference in recurrence-free survival and progression-free survival rates, regardless of whether patients have reTURB performed before or after BCG induction.
Keywords: bladder cancer, BCG, reTURB
1. Introduction
According to the current European Association of Urology (EAU) guidelines, the treatment of patients with high-risk, non-muscle-invasive bladder cancer (NMIBC) should be based on performing transurethral resection of bladder tumour (TURB), followed by 1–3 years of Bacillus Calmette-Guérin (BCG) immunotherapy (induction + maintenance regimen) [1]. One of the significant risks of such a procedure, however, is the presence of one or more residual tumour(s) following initial TURB. This can be especially problematic if the stage of the tumour(s) is underestimated, as is often the case [1]. Because of these disadvantages, a second transurethral resection (reTURB) has been suggested as a potential solution to properly stage the disease, reduce recurrence/progression rates, and improve oncological outcomes following BCG treatment [2,3]. Currently, the EAU guidelines recommend reTURB 2–6 weeks after the primary TURB [1]. However, reTURB timing has not yet been agreed upon, due to the lack of strong evidence behind current recommendations. In the majority of centres in Europe, initial TURB is followed by reTURB before the BCG therapy implementation. However, in some cases, reTURB may be performed after the BCG induction course. This is mainly due to logistical reasons and long waiting lists. In the available literature, no data assessing this sequence of events were found. The aim of this study was to compare the oncological outcomes of patients with T1 high-grade (HG) NMIBC who underwent reTURB according to the EAU guidelines (before BCG therapy) and of those who had reTURB performed after the BCG induction course.
2. Materials and Methods
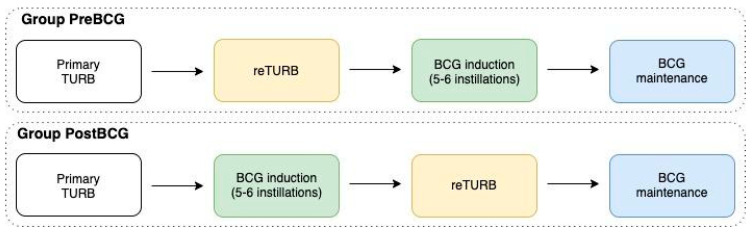
Data sharing from all participating sites used in this observational, retrospective cohort study was approved by an institutional review board. Data from 645 patients from 12 tertiary care centres with primary T1HG NMIBCs, with or without concomitant carcinoma in situ (CIS), who were treated with reTURB and BCG maintenance immunotherapy between 2001 and 2019 were included in the retrospective assessment. The study included patients who underwent the reTURB procedure before BCG induction (Pre-BCG group: 397 patients; 61.6%), as well as those who had reTURB performed after a BCG induction course (5–6 weekly instillations)—Post-BCG group: 248 patients, 38.4% (Figure 1). The decision to perform the reTURB procedure before or after a BCG induction course was determined by the surgeon with the consideration of local protocols. Enhanced visualization modalities (e.g., photodynamic diagnostics/narrow-band imaging) were also used during the procedure, at the urologists’ discretion and based on equipment availability.
Figure 1.
Therapeutic sequence after primary TURB (transurethral resection of bladder tumour).
All patients were treated with BCG induction and maintenance courses. The BCG instillations were given according to the international guidelines and local protocols at the time, with at least one year of planned maintenance. Every patient included in the study received a minimum of five instillations of induction and at least two maintenance instillations [4]. The BCG strains administered varied between the centres, but mainly TICE, RIVM, Moreau, and Connaught BCG were used.
The sociodemographic data of patients collected comprises age at surgery, gender, and smoking history. The pathological data available included the tumour stage, grade, size, focality, presence of concomitant CIS, and presence of muscularis propria (MP) in the specimen, for both primary and restaging TURB. Data on the immediate, single chemotherapy instillation, lymphovascular invasion (LVI), variant histology (VH), and prostatic involvement of the tumours were not uniformly reported and/or were unreliable, and were therefore not included in this analysis.
Tumours included in this analysis were graded according to the WHO 2004 system. Lesions were staged according to the American Joint Committee on Cancer TNM classification. Specimens were evaluated by dedicated uropathologists at each participating centre; no central assessment was applied. Patients were followed up according to the EAU guidelines at the time.
Concomitant CIS was defined as the coexistence of carcinoma in situ and an exophytic tumour. A recurrence was defined as the reappearance of a tumour of any stage, and the grade was confirmed by TURB and histologic assessment. Residual tumours at reTURB and tumour recurrence in the upper urinary tract were not considered as a recurrence. Progression was defined as tumour relapse at tumour stage T2 or higher in the bladder or stromal invasion of the prostatic urethra, or as distant (e.g., lymph nodes) progression. Patients with T2 lesions at both pre- and post-BCG reTURB were not included in the analysis as they did not qualify for BCG therapy and/or underwent radical therapy.
The primary database included 1431 high-risk NMIBC patients from 12 centres. The exclusion criteria for this study included incomplete major variables data, tumours other than T1HG, recurrent tumours, incomplete primary TURB with evident residual disease, time interval between TURB and reTURB of >90 days in the Pre-BCG group and >180 days in the Post-BCG group, number of BCG instillations <7, follow-up <6 months, and other than a full dose concentration of BCG for a given strain. After the exclusion process, 645 cases were included.
The main aim of the study was to determine whether administration of the induction BCG course before reTURB results in significantly better oncological outcomes, as defined by recurrence-free survival (RFS) and progression-free survival (PFS).
Statistical Analysis
The results between study groups were compared using the chi2 and Mann–Whitney test. The RFS and PFS were estimated with the log-rank method, and Kaplan–Meier curves were plotted. Additionally, Cox regression analyses were performed for both RFS and PFS. Patients without an adverse event or death before the end of the study were removed from the study after the last follow-up. Times to adverse events were calculated by taking the date of primary resection as time zero. Due to differences in baseline patient characteristics in the groups, we used a 1:1 propensity-score-matched analysis (PSM) adjusted for gender, smoking status, age, presence of MP in primary specimen, tumour focality, size, and concomitant CIS incidence [5]. Moreover, to reduce the bias of unweighted estimators and adjust for covariates’ imbalance between treatment groups without losing patients, inverse probability of treatment weighting (IPW) was used, using the same variables as in PSM [6].
Statistical significance was considered as p < 0.05. Statistical analyses were performed using STATA 14 (Stata Corp., College Station, TX, USA) and R platform (R project, Vienna, Austria).
3. Results
The study included 397 patients with the reTURB procedure performed before BCG induction (Pre-BCG group: mean age 65.9 ± 11.8 y; 321 males) and 248 patients with reTURB performed after BCG induction course (Post-BCG group: mean age 67.2 ± 9.9 y; p = 0.074, 217 males, p = 0.027). Baseline patient characteristics are presented in Table 1.
Table 1.
The patients’ baseline characteristics. Chi2 and Mann–Whitney test p-values of the differences between the two study groups.
| All Patients (n = 645) | Pre-BCG Group (n = 397; 61.6%) |
Post-BCG Group (n = 248; 38.4%) |
p-Value | |
|---|---|---|---|---|
| Age (mean; SD) | 66.5; 10.9 | 65.9; 11.8 | 67.2; 9.9 | 0.074 |
| Gender (M/F) | 538/107 (83.4/16.6%) | 321/76 (80.9/19.1%) | 217/31 (87.5/12.5%) | 0.027 |
| Smoking history; n (%) | 0.293 | |||
| Never | 191 (29.6%) | 121 (30.5%) | 70 (28.2%) | |
| Former | 266 (41.2%) | 165 (41.6%) | 101 (40.7%) | |
| Current | 167 (25.9%) | 95 (23.9%) | 72 (29%) | |
| Unknown | 21 (3.3%) | 16 (4%) | 5 (2%) | |
| Concomitant CIS; n (%) | 0.054 | |||
| Yes | 126 (19.5%) | 67 (16.9%) | 59 (23.8%) | |
| No | 514 (79.7%) | 328 (82.6%) | 186 (75%) | |
| unknown | 5 (0.8%) | 2 (0.5%) | 3 (1.2%) | |
| Tumour size; n (%) | 0.102 | |||
| <3 cm | 315 (48.8%) | 187 (47.1%) | 137 (55.2%) | |
| ≥3 cm | 279 (43.3%) | 180 (45.3%) | 94 (37.9%) | |
| Unknown | 51 (7.9%) | 30 (7.6%) | 17 (6.9%) | |
| Tumour focality; n (%) | 0.254 | |||
| Solitary | 299 (46.4%) | 180 (45.3%) | 119 (48%) | |
| Multiple | 317 (49.2%) | 195 (49.1%) | 122 (49.2%) | |
| Unknown | 29 (4.5%) | 22 (5.5%) | 7 (2.8%) | |
| Muscularis propria in the primary specimen | 0.034 | |||
| Yes | 467 (72.4%) | 279 (70.3%) | 188 (75.8%) | |
| No | 141 (21.9%) | 99 (24.9%) | 42 (16.9%) | |
| Unknown | 37 (5.7%) | 19 (4.8%) | 18 (7.3%) | |
| Residual NMIBC at reTURB (yes/no) | 226/419 (35/65%) | 152/245 (38.3/61.7%) | 74/174 (29.8/70.2%) | 0.029 |
| Stage of residual disease at reTURB | ||||
| T1 | 105 (46.5%) | 70 (46.1%) | 35 (47.3%) | 0.860 |
| Ta | 66 (29.2%) | 44 (28.9%) | 22 (29.7%) | 0.903 |
| CIS | 55 (24.3%) | 38 (25%) | 17 (23%) | 0.739 |
| Muscularis propria in the reTURB specimen (yes/no) | 439/181/25 (68.1/28.1/3.9%) | 268/115/14 (67.5/29/3.5%) | 171/66/11 (69/26.6/4.4%) | 0.714 |
| BCG strain; n (%) | 0.017 | |||
| Moreau | 138 (21.4%) | 99 (24.9%) | 39 (15.7%) | |
| TICE | 272 (42.4%) | 153 (38.5%) | 119 (48%) | |
| RIVM | 180 (27.9%) | 114 (28.7%) | 66 (26.6%) | |
| Other | 55 (8.5%) | 31 (7.8%) | 24 (9.7%) | |
| Total number of BCG instillations (mean; SD) | 14.7; 6.5 | 14.4; 6.2 | 14.9; 6.0 6.5 | 0.101 |
| Observation time in months (median; IQR) | 43.5 (24.5–58.5) | 40 (27.6–58.6) | 45.4 (23.3–58.0) | >0.001 |
| Recurrence | 218 (33.8%) | 128 (32.2%) | 90 (36.6%) | 0.290 |
| Progression | 94 (14.6%) | 54 (13.6%) | 40 (16.1) | 0.376 |
| Cancer-specific death | 38 (5.9%) | 26 (6.5%) | 12 (4.8%) | 0.369 |
The value of adjusted p < 0.05 was considered statistically significant (in bold). Abbreviations: SD, standard deviation; IQR, interquartile range; M, male; F, female; CIS, carcinoma in situ; NMIBC, non-muscle-invasive bladder cancer
The median follow-up period for the Pre-BCG group was 40 months (IQR: 27.6–58.6), and it was 45.4 months (IQR: 23.3–58.0) for the Post-BCG group (p > 0.001). Groups did not differ statistically in terms of smoking history, tumour size and focality, the presence of MP in the reTURB specimen, and the BCG instillation number. However, patients in the Pre-BCG group had a higher rate of MP presence in the primary TURB specimen, and more residual cancers were found during reTURB. Also, a borderline difference was observed for concomitant CIS, with more observed in the Post-BCG group.
Recurrence was observed in 128 patients (32.2%) in the Pre-BCG group and in 90 patients (36.6%; p = 0.290) in the Post-BCG group. Progression was observed in 94 patients (14.6%) in the Pre-BCG group and in 40 (16.1%; p = 0.376) in the Post-BCG group. There were 26 (6.5%) and 12 (4.8%) cancer-specific deaths in the Pre-BCG and Post-BCG groups, respectively (p = 0.369).
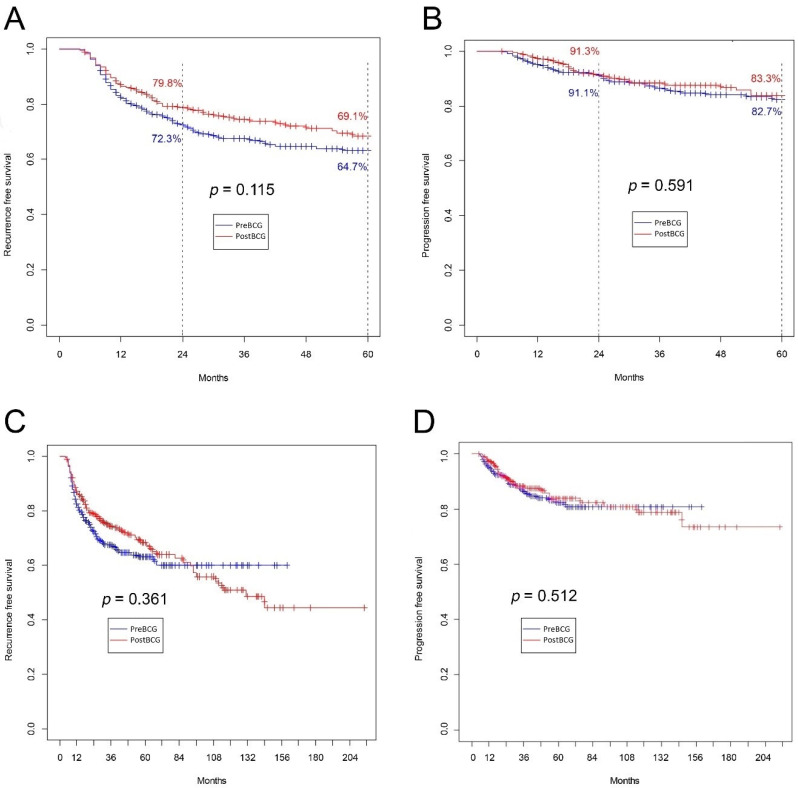
The five-year RFS and PFS were 64.7% vs. 69.1% and 82.7% vs. 83.3% for the Pre-BCG and Post-BCG groups, respectively (both p > 0.05) (Figure 2A,B). Also, no differences were found for the whole observation period, either for RFS (Figure 2C) or for PFS (Figure 2D).
Figure 2.
(A) Recurrence-free survival for five-year follow-up (p = 0.115); (B) progression-free survival for five-year follow-up (p = 0.591); (C) recurrence-free survival for whole observation period (p = 0.36); (D) progression-free survival for whole observation period (p = 0.512).
Considering multivariate analyses, reTURB timing was not associated with statistically significant differences for RFS or PFS (Table 2). Positive reTURB increased the risk of recurrence and progression by 2.6- and 3-fold, respectively.
Table 2.
Multivariable analysis assessing factors associated with disease recurrence and progression.
| Recurrence-Free Survival | Progression-Free Survival | |||||
|---|---|---|---|---|---|---|
| Variable | HR | 95% CI | p-Value | HR | 95% CI | p-Value |
| Age | 1.00 | 0.99–1.02 | 0.537 | 1.00 | 0.98–1.02 | 0.829 |
| Gender (female vs. male) | 1.07 | 0.67–1.46 | 0.971 | 0.97 | 0.47–1.58 | 0.627 |
| Smoking (never/any) | 1.02 | 0.74–1.39 | 0.917 | 1.01 | 0.60–1.57 | 0.902 |
| MP (yes/no) | 0.92 | 0.64–1.32 | 0.657 | 0.76 | 0.47–1.31 | 0.360 |
| Concomitant CIS (yes vs. no) | 1.35 | 0.95–1.92 | 0.094 | 1.33 | 0.79–2.22 | 0.278 |
| Size (≤3 cm vs. >3 cm) | 1.05 | 0.72–1.30 | 0.802 | 1.26 | 0.79–2.01 | 0.332 |
| Focality (solitary vs. multiple) | 0.99 | 0.73–1.33 | 0.932 | 1.35 | 0.86–2.13 | 0.194 |
| reTURB before/after | 0.93 | 0.67–1.27 | 0.667 | 0.96 | 0.60–1.53 | 0.864 |
| Residual tumour at reTURB yes/no | 2.62 | 1.94–3.54 | 0.000 | 3.01 | 1.90–4.77 | 0.000 |
The value of adjusted p < 0.05 was considered statistically significant (in bold); HR > 1 worse outcome for the option in bold, HR < 1 better outcome for the option in bold. Abbreviations: HR, hazard ratio; 95% CI, 95% confidence interval; CIS, carcinoma in situ; MP, muscularis propria.
Because of the retrospective and multicentre nature of the study, some disparities in baseline patient characteristics were observed. Therefore, the PSM was performed. The groups were adjusted for gender, smoking status, age, MP presence in primary specimen, tumour focality, size, and CIS concomitant incidence. After matching, 342 patients were included in the analysis (Table 3).
Table 3.
The patients’ baseline characteristics after propensity-score-matched analysis (PSM). Chi2 and Mann–Whitney test p-values of the differences between the two study groups.
| All Patients (n = 645) | Pre-BCG Group after Matching (n = 171) | Post-BCG Group after Matching (n = 171) | p-Value | |
|---|---|---|---|---|
| Age (mean; SD) | 66.5; 10.9 | 66.2; 10.9 | 67.6; 9.9 | 0.248 |
| Gender M/F; (%) | 538/107 (83.4/16.6%) | 146/25 (85.4/14.6%) | 150/21 (87.7/12.3%) | 0.526 |
| Smoking history; n (%) | 0.931 | |||
| Never | 191 (29.6%) | 48 (28.1%) | 51 (29.8%) | |
| Former | 266 (41.2%) | 73 (42.7%) | 69 (40.4%) | |
| Current | 167 (25.9%) | 47 (27.5%) | 49 (28.6%) | |
| Unknown | 21 (3.3%) | 3 (1.7%) | 2 (1.2%) | |
| Concomitant CIS; n (%) | 0.634 | |||
| Yes | 126 (19.5%) | 30 (17.5%) | 37 (21.6%) | |
| No | 514 (79.7%) | 140 (81.9%) | 133 (77.8%) | |
| unknown | 5 (0.8%) | 1 (0.6%) | 1 (0.6%) | |
| Tumour size; n (%) | 0.393 | |||
| <3 cm | 315 (48.8%) | 80 (46.8%) | 68 (39.8%) | |
| ≥3 cm | 279 (43.3%) | 82 (47.9%) | 91 (53.2%) | |
| Unknown | 51 (7.9%) | 9 (5.3%) | 12 (7%) | |
| Tumour focality; n (%) | 0.267 | |||
| Solitary | 299 (46.4%) | 88 (51.5%) | 83(48.5%) | |
| Multiple | 317 (49.2%) | 77 (45%) | 86 (50.3%) | |
| Unknown | 29 (4.5%) | 6 (3.5%) | 2 (1.2%) | |
| Muscularis propria in the primary specimen | 0.949 | |||
| Yes | 467 (72.4%) | 140 (81.9%) | 142 (83%) | |
| No | 141 (21.9%) | 23 (13.4%) | 22 (12.9%) | |
| Unknown | 37 (5.7%) | 8 (4.7%) | 7 (4.1%) |
The value of adjusted p < 0.05 was considered statistically significant. Abbreviations: SD, standard deviation; M, male; F, female; CIS, carcinoma in situ.
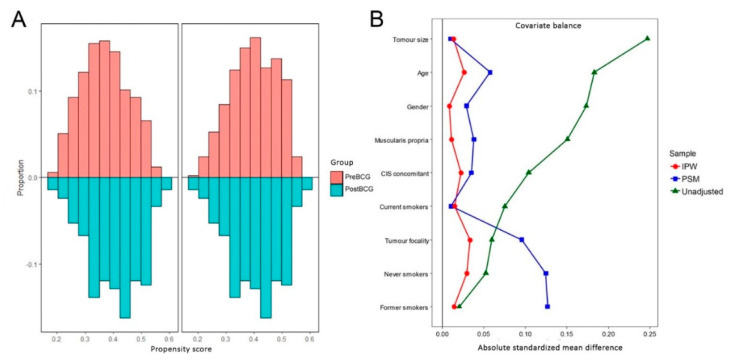
Due to the fact that almost a half of patients were excluded after the PSM, the IPW was later performed for the whole population using the same variables for weighting as for the PSM adjusting (Figure 3).
Figure 3.
(A) Histogram distribution of propensity scores before and after PSM between the study groups. (B) Covariate balance before adjustment and after PSM and IPW (inverse probability of treatment weighting). IPW, inverse-probability weighting; PSM, propensity-score-matching.
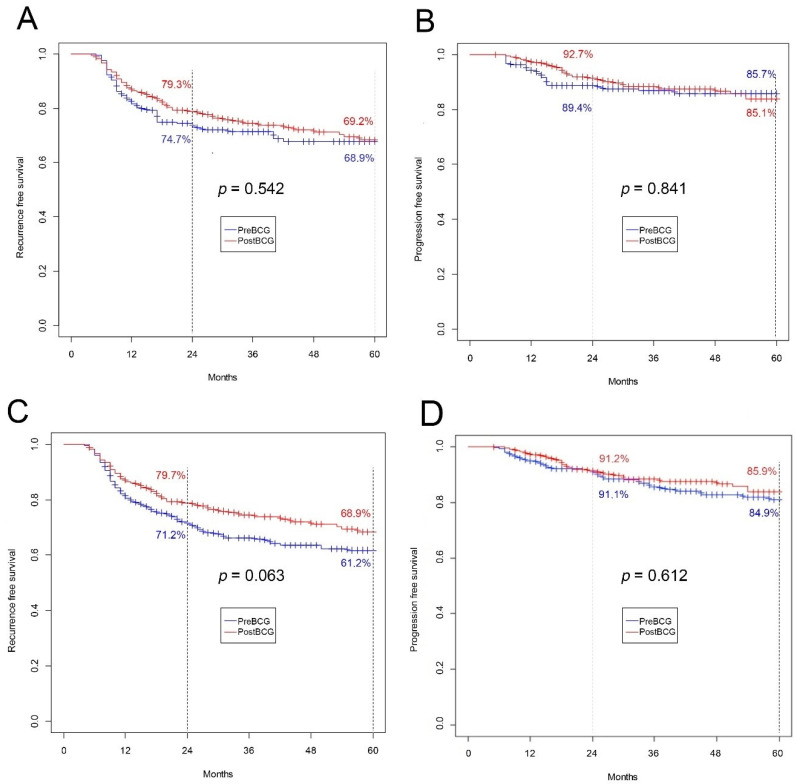
Similarly, after PSM, neither RFS nor PFS differed for the five-year (Figure 4A,B) and total observation periods (data not shown). When IPW was implemented, borderline significance was observed for five-year RFS, with better results for the Post-BCG group (68.9% vs. 61.2%; p = 0.063) (Figure 4C). For other IPW survival analyses, differences in RFS and PFS did not reach statistical significance (Figure 4D).
Figure 4.
(A) Recurrence-free survival for five-year follow-up after PSM (p = 0.542); (B) progression-free survival for five-year follow-up after PSM (p = 0.841); (C) recurrence-free survival for five-year follow-up after IPW (p = 0.063); (D) progression-free survival for five-year follow-up after IPW (p = 0.612). IPW, inverse-probability weighting; PSM, propensity-score-matching.
4. Discussion
The issue of reTURB is recently gaining increased attention, with reasons both for and against this procedure. The EAU guidelines recommend the performance of reTURB a few weeks after the primary TURB procedure. However, in select urological centres, some patients undergo reTURB after the BCG induction. Reasons why reTURB is performed after BCG induction may include the diminished physical performance of patients after primary TURB and-even more important-a desire to speed up the commencement of BCG (a long waiting period for second, pre-BCG TURB). This might be particularly true during events like the COVID-19 pandemic.
Although this treatment is common, the issue of the performance of reTURB after the BCG induction has not been thoroughly analysed yet. In this study, a uniform group of patients with primary T1HG cancers was analysed. Out of a total of 645 patients identified from referral centres, 248 (38%) underwent reTURB after the BCG induction was completed. It was shown that the performance of reTURB after the induction course of BCG did not influence the oncological outcomes of treated patients. In a simple survival analysis, the results of RFS and PFS did not differ significantly between examined groups.
Furthermore, after PSM application, RFS and PFS did not differ significantly statistically for any observation period. However, when IPW was applied, the results showed statistical significance (p = 0.063) for the five-year observation of RFS.
Therapeutic decisions in the NMIBC setting are mainly based on the results of the initial TURB. However, primary TURB may unintentionally fail to control all present lesions or reliably detect cancer muscular infiltration.
Literature data show that up to half of patients are found to have residual disease after a completely resected T1 NMIBC. Additionally, some of them are finally proven to be muscle invasive disease [3,7,8]. It is also worth noting that patients with residual tumours in reTURB were shown to have higher risk of further recurrence and progression [9,10]. Because of the abovementioned TURB disadvantages, the reTURB concept was created in the mid-1990s [11]. The main aim of reTURB is to correctly assess the possible muscular invasion and resect all residual cancer. During the procedure, all gross lesions, as well as resection scars and/or oedematous/suspicious areas, are resected deep enough to include a sufficient amount of muscle in the histopathological specimens.
In 35% of reTURBs, some residual lesions were found. Interestingly, the rate of residual disease was lower in the Post-BCG group (38% vs. 30%; p = 0.029), possibly because of the BCG effect. Even though there is a statistically different occurrence of MP in primary specimens, the higher incidence rate of residual disease detected in reTURB was preserved after PSM, which was adjusted for MP (data not presented). Out of all cases of residual tumours, 105 (46%) were T1 tumours: 70 in the Pre-BCG group and 35 in Post-BCG. The difference was not statistically significant (p = 0.860). As stated in the available literature and as shown in this study, a viable tumour in reTUBR is associated with an increased risk of cancer recurrence and progression (2.6- and 3-fold higher, respectively). Unfortunately, the number of T2 lesions detected in reTURB was not reliably recorded in all centres, so these patients were not included in the analysis. Similarly, the influence of a time delay (resulted from T2 diagnosis at post-BCG reTURB) on some patients’ survival was not assessed.
Despite the advantages of the procedure, the influence of reTURB on oncological survival is not clear since the available studies present heterogenous populations treated with various adjuvant modalities. In a paper by Calo et al. that included 118 patients from a prospectively maintained nonrandomized high-risk NMIBC database, the authors showed that reTURB was not associated with any oncological benefit in RFS, PFS, and cancer-specific survival (CSS) [12]. In the largest study to date, performed by Gontero et al., reTURB had a positive impact on survival only if MP involvement was not present in the primary specimen [13]. Finally, in a recent meta-analysis of six studies including more than 3000 patients, it was shown that reTURB does not improve survival outcomes in patients with T1 bladder tumours [14].
The optimal timing of reTURB is still to be confirmed. In the literature, we found various time periods between primary and reTURB, ranging from a few days to 12 weeks [7]. Baltaci et al. showed that reTURB should not be performed more than 42 days after the primary TURB [15]. Krajewski et al. demonstrated that there is no benefit to reTURB if the procedure is performed eight weeks after the primary TURB and assumed that optimal timing of reTURB is from 2 to 6 weeks after initial TURB. Also, it was shown that each day of reTURB postponement results in a 4% increase in the risk of all analysed clinical events [16]. Because of this, it might be hypothesized that the time intervals in post-BCG reTURB play a similar role as in conventional reTURB. However, this aspect was not analysed in our study.
Study Limitations
Although our study presented several strengths, it also had some limitations. First, the majority of the clinical and pathological data was collected retrospectively. However, when compared with recently published high-quality data, this study population is representative in terms of basic characteristics [17]. Recurrence and progression rates may seem low when compared with classic EORTC or CUETO nomograms, but our observations did not differ significantly from those in similar studies [18]. Additionally, allocation to groups was not intentionally randomized. Conclusively, to overcome the limitations of a retrospective design, we performed a PSM and IPW analysis matching patients for baseline characteristics. We did not include BCG strain in the matching analysis, as it led to a substantial limitation on case numbers and consequently a limitation on the number of adverse events. Secondly, one of the major post-BCG reTURB limitations is the fact that patients who are understaged during primary TURB will be diagnosed with a delay that could be fatal. Third, the data included in this study were mainly gathered from outpatient departments performing BCG procedures. This meant that thorough details about patients who were not qualified or not eligible for BCG (according to the total amount of T2 at reTURB in each centre, further treatment modalities of tumours that progressed, survival, etc.) were excluded from the analysis. Fourth, to preserve the homogeneity of the population, only patients who received at least five induction and two maintenance instillations, representing adequate BCG exposure, were included. Unfortunately, this might have resulted in the exclusion of some suitable patients (e.g., patients with a poor outcome at reTURB after BCG induction). Fifth, there was no central specimen review and no substaging of T1 tumours. Sixth, all data used in this paper originated from large oncological centres. Therefore, the results of this study may not be applicable to centres with less experience of bladder cancer treatment. Seventh, data regarding the experience of surgeons and technical details (e.g., en bloc, reTURB range) were not available and therefore were not included in the analysis. Also, data on the WHO 1973 grade, immediate single-dose chemotherapy, LVI, VH, and prostatic involvement of the tumours were not uniformly reported and/or unreliable and therefore were not included in the analysis. Finally, we did not perform CSS analysis, because the number of events (cancer-specific deaths) was low and therefore not statistically representative.
5. Conclusions
Despite a lack of evidence for its efficacy, the reTURB procedure is performed at many urological centres following the BCG induction course. Our results suggest that there might be no difference in recurrence-free survival or progression-free survival between patients with high-grade T1 disease who had reTURB before BCG induction and patients with reTURB after BCG induction. This study also confirms that patients with residual tumours in reTURB are characterised by lower survival rates compared with patients with negative reTURB.
Author Contributions
Conceptualization: W.K. and M.M.; Methodology: W.K. and M.M.; Software: A.T. (Andrzej Tukiendorf); Validation: W.K., M.M. and R.Z.; Formal analysis: W.K., M.M., S.P., S.J., A.A., K.H., G.S., E.X., A.P. and A.K.; Investigation: W.K. and M.M.; Acquisition of data: Ł.N., L.A., J.T., T.M., A.T. (Alessandro Tafuri), A.G., A.M., E.D.T., M.A.-M., A.R.S., S.Z., C.S., M.C.M., R.M., G.P., P.R., J.K., E.L., A.Z.-W., K.T. and R.P.; Data curation: W.K.; Writing—original draft preparation: W.K., M.M., and Ł.N.; Writing—review and editing: S.P., S.J., A.A., K.H., G.S., E.X., A.P. and R.Z.; Supervision: S.P., S.J., A.A., K.H., G.S., E.X., R.Z. and M.M.; Project administration: A.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Babjuk M., Burger M., Compérat E.M., Gontero P., Mostafid H., Palou J., Van Rhijn B.W., Rouprêt M., Shariat S.F., Sylvester R., et al. European Association of Urology Guidelines on Non-muscle-invasive Bladder Cancer (TaT1 and Carcinoma In Situ)-2019 Update. Eur. Urol. 2019;76:639–657. doi: 10.1016/j.eururo.2019.08.016. [DOI] [PubMed] [Google Scholar]
- 2.Bishr M., Lattouf J.-B., Latour M., Saad F. Tumour stage on re-staging transurethral resection predicts recurrence and progression-free survival of patients with high-risk non-muscle invasive bladder cancer. Can. Urol. Assoc. J. 2014;8:306–310. doi: 10.5489/cuaj.1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brausi M., Collette L., Kurth K., Van Der Meijden A.P., Oosterlinck W., Witjes J., Newling D., Bouffioux C., Sylvester R.J. Variability in the Recurrence Rate at First Follow-up Cystoscopy after TUR in Stage Ta T1 Transitional Cell Carcinoma of the Bladder: A Combined Analysis of Seven EORTC Studies. Eur. Urol. 2002;41:523–531. doi: 10.1016/S0302-2838(02)00068-4. [DOI] [PubMed] [Google Scholar]
- 4.Kamat A.M., Flaig T.W., Grossman H.B., Konety B., Lamm D., O’Donnell M.A., Uchio E., Efstathiou J.A., Taylor J.A. Consensus statement on best practice management regarding the use of intravesical immunotherapy with BCG for bladder cancer. Nat. Rev. Urol. 2015;12:225–235. doi: 10.1038/nrurol.2015.58. [DOI] [PubMed] [Google Scholar]
- 5.Sjölander A. Propensity scores and M-structures. Stat. Med. 2009;28:1416–1420. doi: 10.1002/sim.3532. [DOI] [PubMed] [Google Scholar]
- 6.Olmos A., Govindasamy P. A Practical Guide for Using Propensity Score Weighting in R. Pract. Assess. Res. Eval. 2015;20:1–8. [Google Scholar]
- 7.Cumberbatch M.G., Foerster B., Catto J.W., Kamat A.M., Kassouf W., Jubber I., Shariat S.F., Sylvester R.J., Gontero P. Repeat Transurethral Resection in Non–muscle-invasive Bladder Cancer: A Systematic Review. Eur. Urol. 2018;73:925–933. doi: 10.1016/j.eururo.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 8.Naselli A., Hurle R., Paparella S., Buffi N.M., Lughezzani G., Lista G., Casale P., Saita A., Lazzeri M., Guazzoni G. Role of Restaging Transurethral Resection for T1 Non–muscle invasive Bladder Cancer: A Systematic Review and Meta-analysis. Eur. Urol. Focus. 2018;4:558–567. doi: 10.1016/j.euf.2016.12.011. [DOI] [PubMed] [Google Scholar]
- 9.Sternberg I.A., Paz G.E.K., Chen L.Y., Herr H.W., Dalbagni G. Role of immediate radical cystectomy in the treatment of patients with residual T1 bladder cancer on restaging transurethral resection. BJU Int. 2012;112:54–59. doi: 10.1111/j.1464-410X.2012.11391.x. [DOI] [PubMed] [Google Scholar]
- 10.Chen J.C., Li T., Ning X.H., Peng S.H., Wang J.Y., Qi N.N., Cai L., Gong K. Clinical significance of residual tumors at repeat transurethral resection in patients with T1 bladder cancer. Zhonghua Yi Xue Za Zhi. 2016;96:1124–1127. doi: 10.3760/cma.j.issn.0376-2491.2016.14.013. [DOI] [PubMed] [Google Scholar]
- 11.Herr H.W. The Value of a Second Transurethral Resection in Evaluating Patients with Bladder Tumors. J. Urol. 1999;162:74–76. doi: 10.1097/00005392-199907000-00018. [DOI] [PubMed] [Google Scholar]
- 12.Calò B., Chirico M., Fortunato F., Sanguedolce F., Carvalho-Dias E., Autorino R., Carrieri G., Cormio L. Is Repeat Transurethral Resection Always Needed in High-Grade T1 Bladder Cancer? Front. Oncol. 2019;9:456. doi: 10.3389/fonc.2019.00465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gontero P., Sylvester R., Pisano F., Joniau S., Oderda M., Serretta V., Larre’ S., Di Stasi S., Van Rhijn B., Witjes A.J., et al. The impact of re-transurethral resection on clinical outcomes in a large multicentre cohort of patients with T1 high-grade/Grade 3 bladder cancer treated with bacille Calmette-Guérin. BJU Int. 2015;118:44–52. doi: 10.1111/bju.13354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krajewski W., Nowak Ł., Poletajew S., Tukiendorf A., Moschini M., Mari A., Di Trapani E., Xylinas E., Kiełb P., Wełna M., et al. The Impact of Restaging Transurethral Resection of Bladder Tumor on Survival Parameters in T1 Nonmuscle-Invasive Bladder Cancer: Systematic Review and Meta-Analysis. J. Endourol. 2020;34:795–804. doi: 10.1089/end.2020.0301. [DOI] [PubMed] [Google Scholar]
- 15.Baltacı S., Bozlu M., Yıldırım A., Gökce M.I., Tinay I., Aslan G., Can C., Turkeri L., Kuyumcuoğlu U., Mungan A., et al. Significance of the interval between first and second transurethral resection on recurrence and progression rates in patients with high-risk non-muscle-invasive bladder cancer treated with maintenance intravesical Bacillus Calmette-Guérin. BJU Int. 2015;116:721–726. doi: 10.1111/bju.13102. [DOI] [PubMed] [Google Scholar]
- 16.Krajewski W., Zdrojowy R., Dembowski J., Poletajew S., Wróbel M., Łuczak M., Tukiendorf A., Kolodziej A. The Optimal Timing of Restaging Resection before Introduction of Bacillus Calmette-Guerin Immunotherapy in Patients with High-Risk Non-Muscle-Invasive Bladder Cancer. Urol. Int. 2018;102:60–68. doi: 10.1159/000491642. [DOI] [PubMed] [Google Scholar]
- 17.Grimm M.-O., Van Der Heijden A.G., Colombel M., Muilwijk T., Martínez-Piñeiro L., Babjuk M.M., Türkeri L.N., Palou J., Patel A., Bjartell A.S., et al. Treatment of High-grade Non–muscle-invasive Bladder Carcinoma by Standard Number and Dose of BCG Instillations Versus Reduced Number and Standard Dose of BCG Instillations: Results of the European Association of Urology Research Foundation Randomised Phase III Clinical Trial “NIMBUS”. Eur. Urol. 2020 doi: 10.1016/j.eururo.2020.04.066. in press. [DOI] [PubMed] [Google Scholar]
- 18.Cambier S., Sylvester R.J., Collette L., Gontero P., Brausi M.A., Van Andel G., Kirkels W.J., Da Silva F.C., Oosterlinck W., Prescott S., et al. EORTC Nomograms and Risk Groups for Predicting Recurrence, Progression, and Disease-specific and Overall Survival in Non–Muscle-invasive Stage Ta–T1 Urothelial Bladder Cancer Patients Treated with 1–3 Years of Maintenance Bacillus Calmette-Guérin. Eur. Urol. 2016;69:60–69. doi: 10.1016/j.eururo.2015.06.045. [DOI] [PubMed] [Google Scholar]