Abstract
The current study investigated the protective potential of Azolla pinnate ethanolic extract (APE) against lead-induced hepatotoxicity in rats. Sixty male Wistar albino rats were randomly allocated into six groups (n = 10). The control group was orally administrated with saline. The second group received lead acetate (100 mg/kg body weight (BW) orally for 60 days). The third group was fed with APE (10 mg/kg BW orally for 60 days). The fourth group was administrated with lead acetate like the second group and APE like the third group, concomitantly, for 60 days. The fifth group was administrated with APE like the third group for 30 days, then orally administrated with the lead acetate like the second group for another 30 days. The sixth group was administrated with lead acetate like the second group for 30 days, then with APE like the third group for a further 30 days. Phytochemical analysis of APE indicated the presence of peonidin 3-O-glucoside cation, vitexin, rutin, thiamine, choline, tamarixetin, hyperoside, astragalin, and quercetin. The latter has been elucidated using one- and two-dimensional nuclear magnetic resonance (1D and 2D NMR) and liquid chromatography–mass spectrometry (LC–MS-MS). Lead acetate increased the serum levels of alanine and aspartate aminotransferases and that of urea, creatinine, tumor necrosis factor alpha, and interleukin 1β, hepatic tissue malondialdehyde contents, and caspase 3 protein expression, as well as altering the hepatic tissue architecture. However, it decreased the serum levels of interleukin 10 and glutathione (GSH) contents, and the activities of catalase and superoxide dismutase in hepatic tissue. In contrast, the administration of APE ameliorated the lead-induced alterations in liver function and structure, exemplifying the benefits of Azolla’s phytochemical contents. Collectively, A. pinnate extract is a protective and curative agent against lead-induced hepatotoxicity via its antioxidant, anti-inflammatory, and anti-apoptotic impacts.
Keywords: lead acetate, hepatotoxicity, Azolla pinnata, caspase 3, NMR, LC–MS-MS, TNF-α, IL-1β, IL-10
1. Introduction
The main cause of hepatotoxicity in all living organisms is exposure to heavy metals, toxins, drugs, or harmful compounds, including carbon tetrachloride, sodium oxalate, and ethylene glycol [1]. Lead acetate is a white crystalline chemical compound found under the earth’s crust and has a sweet taste [2]. The contamination of air, water, soil, food by paints, disposable materials of factories like batteries and leaded gasoline is the main reason for lead poisoning [3,4]. Water is an important source for lead poisoning, particularly due to the leaking of lead from water pipes [5]. Lead acetate induces experimental hepatic injury in rats via the induction of oxidative stress following an imbalance between free radical generation and the antioxidant defense system [6]. This oxidative stress leads to the generation of reactive oxygen species (ROS), including the hydroperoxides, singlet oxygen, and hydrogen peroxide, resulting in serious damage to different biomolecules, i.e., DNA, enzymes, proteins, and membrane lipids. It also impairs homeostasis simultaneously [6,7]. Lead generates free radicals that damage the vital organs, including the liver [8], via reducing the activities of antioxidant enzymes and increasing lipid peroxidation [9]. Furthermore, lead toxicity has an inferior impact on various organs, including the nervous system, bones, teeth, kidneys, cardiovascular, immune, and reproductive systems [10], usually leading to hearing loss and tooth decay [11,12,13]. Lead toxicity also results in neuropsychiatric disorders ranging from headache, difficulty concentrating, and delayed motor nerve conduction, as well as to delayed reaction times and irritability [14]. Furthermore, exposure to higher levels of lead causes encephalopathy, characterized by swelling of the brain tissue associated with delirium, coma, and seizures [15]. Chronic lead toxicity results in short-term memory loss, nausea, depression, loss of coordination, numbness and tingling in the extremities, and abdominal pain [16], in addition to anemia [14]. Lead toxicity harms both adults and children [17].
Medicinal plants possess an important role in the human healthcare system. Herbal medicine has received tremendous attention in the primary health sector, mainly due to its effectiveness and popularity [18]. In traditional medicine, herbal prescriptions were claimed to be effective in treating liver disorders; hence, the development and validation of a new herbal drug is of prime concern [19].
A. pinnata is the only genus in the family Salviniaceae that has a worldwide distribution; it can tolerate both temperate and tropical climates. A. pinnata is a species of fern that has several common names, including mosquito fern, feathered mosquito fern, and water velvet. It is native to Africa and Asia [20]. It is an aquatic fern consisting of a short, branched, floating stem, with bearing roots hanging down in the water. The leaves are alternately arranged; each consists of a thick aerial dorsal lobe containing green chlorophyll and a thin, floating ventral colorless lobe of a slightly larger size [21]. A. pinnata contains many bioactive compounds such as essential amino acids, vitamins, Beta-carotene, minerals, saponin, and flavonoids [22]. It is also considered a good source of high-quality protein [23]. To investigate further the protective effect of A. pinnata ethanolic extract against lead acetate-induced hepatotoxicity in rats, we elucidated the underlying molecular mechanism as part of our ongoing project of phytochemical analysis of Egyptian plants, with particular emphasis on the antioxidant, anti-inflammatory and anti-apoptotic activities [24].
2. Materials and Methods
2.1. Animals
A total of 60 male Wistar albino rats, weighing 90–110 g each, were purchased from Vac Sera lab., Helwan City, Cairo, Egypt. The rats were kept in polypropylene cages under standard laboratory conditions of temperature 20–25 °C and a 12 h light/12 h dark cycle. Rats were provided with clean water and had access to food ad libitum. A balanced diet of commercial pellets was fed to the rats (Atmida Company for international commerce and development, Egypt). The rats were kept for 10 days before the beginning of the experiments for acclimatization. Animal rearing and handling, and the experimental design and procedures, were approved by the Research Ethics Committee of the Faculty of Veterinary Medicine, University of Sadat City, Egypt (VUSC-006-2-20).
2.2. Chemicals
All chemicals used in this study were of analytic grades.
2.3. Preparation of Plant Extract
For the preparation of A. pinnata ethanolic extract (APE), fresh green leaves of A. pinnata were obtained from the botanical gardens of the National Research Centre, Giza, Egypt. The extract was prepared according to the methods of Kunjiappan et al. (2014) [25]. Briefly, fresh leaves of A. pinnata were collected and dried under shade at room temperature (22 °C and 65% relative humidity) for 7 days. The dried leaves were grounded into powder and soaked in ethanol 70% (500 g/L) for 48 h with gentle shaking in an incubator shaker at 37 °C. The content was filtered through a Whatman No. 1 paper filter, and the filtrate was evaporated until dryness. The yield was 10%, and the content was kept in an airtight bottle in a refrigerator at 4 °C until usage.
2.4. NMR Analysis
1H-NMR spectra and heteronuclear single quantum coherence spectroscopy (HSQC) spectra were recorded at 298 K on a Bruker 600 MHz spectrometer (TCI CRPHe TR-1H and 19F/13C/15N 5 mm-EZ CryoProbe). Chemical shifts were referenced to the solvent peaks for (CD3)2SO at δH 2.50 and δC 39.52.
2.5. UPLC–MS-QToF Analysis and Molecular Networking for a Screening of Secondary Metabolites
High-resolution mass spectrometric measurements were acquired using a ultra-performance liquid chromatography coupled with quadrupole time-of-flight mass spectrometry (UPLC-QToF) nanospray MS (Waters nanoAcquity, QToF Micro). The UPLC column used was a Waters ACQUITY UPLC M-Class Peptide BEH C18 column (1.7 μm, 130 Å, 75 μm × 150 mm), using solvents A (0.1%), FA (Formic acid) in water and B (0.1% FA in AcN). A total run of 75 mins with a flow rate of 0.3 µL/min is used as follows. A gradient from 1–90% of AcN in 50 min, washing the column with 90% AcN for 4 min, and finally, equilibration of a column to 1% AcN again in 20 min. MS and MSMS data were acquired in positive electro spray ionization mode (+ESI), nanoelectrospray (NSI) is at 90°. The mass range was from 50–2000 Da/ms and 50–1300/msms, the scan time was 1 s, and the inter-scan delays were 0.1 s. The collision gas, argon, spray energy 4300 V collision energy is 30 volts, the sample cone is 30 V, the extraction cone is 2.5 V, the source temperature is 80 °C and the desolvation temperature is 100 °C. Furthermore, molecular networking provides a valuable tool in metabolite identification by grouping metabolites with the same fragmentation in clusters and linking them to each other; so, if some metabolites are identified, the whole cluster can be identified from mass loss. Moreover, it can give information on the similarities and variances among the species that have been subjected to MS fragmentation.
2.6. Experimental Design
A total of 60 male Wistar albino rats were equally divided into 6 groups, (n = 10).
2.6.1. Control Group
Rats were orally given normal physiological saline (0.9% sodium chloride).
2.6.2. Lead Acetate Group
Lead acetate was orally administered to rats at a dose of 100 mg/kg body weight (BW) for 60 days [26].
2.6.3. A. pinnata Ethanolic Extract (APE) Group
Rats were orally administered with 10 mg/kg BW of APE, extracted daily for 60 days [27].
2.6.4. Lead Acetate and A. pinnata Ethanolic Extract Group
Rats were orally administrated with lead acetate as the second group, and APE as the third group, simultaneously for 60 days.
2.6.5. A. pinnata Ethanolic Extract then Lead Acetate Group
Rats were orally administrated with APE as the third group for 30 days, then administrated with the lead acetate as the second group for another 30 days.
2.6.6. Lead Acetate then A. pinnata Ethanolic Extract Group
Rats were orally administrated with lead acetate as the second group for 30 days, then administered with APE as the third group for further 30 days.
2.7. Recording the Initial and Final Rats’ Weights
Rats’ initial and final weights were recorded at the beginning and the end of the experiment, respectively.
2.8. Blood and Tissue Sampling
At the end of the experiment, rats were anaesthetized, then blood samples were collected from the medial canthus of the eye with a heparinized capillary tube. Sera samples were separated and stored at −20 °C to be used for measuring the biochemical parameters. The liver was removed and divided into two parts. The first part was kept at −80 °C for further investigation of lipid peroxidation and antioxidant activity biomarkers. The second part was kept in 10% neutral formalin to be used for histopathological and immunohistochemical investigations.
2.9. Biochemical Assays
Liver and kidney function biomarkers were determined by using specific commercial diagnostic kits. The serum concentration of urea was measured according to the methods of Fawcett et al. (1960) [28] and serum creatinine concentrations were measured according to the methods of Bartels et al. (1972) and Larsen et al. (1972) [29,30], according to the manufacturer’s instructions. Serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) activities were analyzed according to the methods of Reitman et al. (1957) [31].
Malondialdehyde (MDA) was determined in liver homogenate according to the procedure described by Satoh, 1978 [32], using Biodiagnostic Kits for MDA. Reduced glutathione (GSH) concentration was determined in liver homogenate, according to the procedure described by Beutler et al. (1963) [33], using Biodiagnostic Kits. Superoxide dismutase (SOD) activity was determined in liver homogenate, according to the procedure described by Nishikimi et al. (1972) [34], using Biodiagnostic Kits for SOD. Catalase activity was determined in liver homogenate according to the procedure described by Fossati et al. (1980) and Aebi (1984) [35,36], using Biodiagnostic Kits.
Serum levels of interleukin 1 beta (IL-1 β), tumor necrosis factor alpha (TNF-α), and interleukin 10 (IL-10) were determined by using ELISA kits according to methods described by Vidal et al. (2000), Brynskov et al. (2002), and Odewumi et al. (2015), respectively [37,38,39].
2.10. Histopathological Examination
Following necropsy, liver tissue samples were collected and fixed in 10% neutral buffered formalin for 3 days. Fixed samples were routinely processed, embedded in paraffin wax, cut into 4-µm sections, and stained with hematoxylin and eosin (H&E) [40]. Five fields per section were examined for the evaluation of hepatic damage. The severity of pathological findings was assessed by using a modified semiquantitative scoring system (- means no changes were present, + means mild changes, ++ means moderate, and +++ means severe changes) [41,42].
2.11. Immunohistochemical Analysis
The immunohistochemical staining was done according to the methods of Orabi et al. (2020) [43]. Rabbit polyclonal caspase 3 primary antibodies (abcam, abc2302; 1:100 dilution) and anti-rabbit IgG secondary antibodies (EnVision + System HRP; Dako) were used. Diaminobenzidine commercial kits (Liquid DAB+Substrate Chromogen System; Dako) were used to visualize the stained caspase 3; finally, slides were counterstained with Mayer’s hematoxylin. The negative control procedure was carried out using the aforementioned procedures, while the primary antibody was replaced by normal rat serum. The labeling index of caspase 3 was expressed as the percentage of positive cells per 1000 counted cells in about 10 high-power fields.
2.12. Statistical Analysis
An analysis of the results was performed by using SPSS program software, version 16 (IBM®, USA). Data were subjected to an analysis of variance (ANOVA) and Duncan’s post-hoc tests to determine significant differences among the data. The differences between means were analyzed at the 5% probability level (p ≤ 0.05), which was statistically significant.
3. Results
3.1. Nuclear Magnetic Resonanse (NMR) Analysis
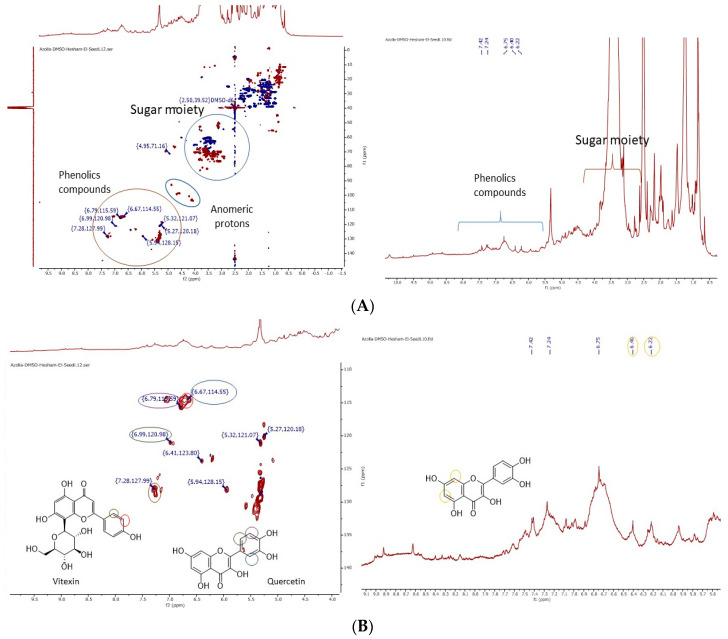
The 1H-NMR spectra of A. pinnata ethanolic extract showed a dominance of signals in the aliphatic region (e.g., methyl proton peak at δ 0.9, methylene protons [CH2]n peaks in the region of δ 1.2–3.5 ppm). Particular glycosides (e.g., anomeric hydrogen at δ 4.8 ppm) and some of the aromatic moieties at δ (6.00–8.2 ppm) are presented in Figure 1A. Heteronuclear single quantum coherence spectroscopy (HSQC) with a decoupled sensitive spectrum prescribed the presence of glycosides, CH groups as red spots at a range of δ 60–80 ppm, and SP2 methylene groups as blue spots with a range of δ 54–66 ppm. Additionally, anomeric proton CH groups can be seen as red spots around chemical shifts at δ 100 ppm. Kaempferol and vitexin are flavanones characterized by the presence of the 1,4 di-substitution benzene ring H-2′-3′ at δ 7.24 and 6.67 and 13C δ 127 and 114 ppm, respectively. Quercetin is characterized by the ABX, A-B is in ortho position and A-X is in meta position, benzene ring H-2′-3′ and 6′ at δ 6.99, 6.79, and 6.67, with 13C δ 120, 117, and 114 ppm, respectively, as seen in Figure 1B.
Figure 1.
(A) 1H-NMR and heteronuclear single quantum coherence spectroscopy (HSQC) spectrum of A. pinnata ethanolic extract. (B) 1H-NMR and HSQC spectrum of A. pinnata ethanolic extract that prescribes the phenolic areas of quercetin and vitexin.
3.2. UPLC–MS-QToF and Molecular Networking Analysis
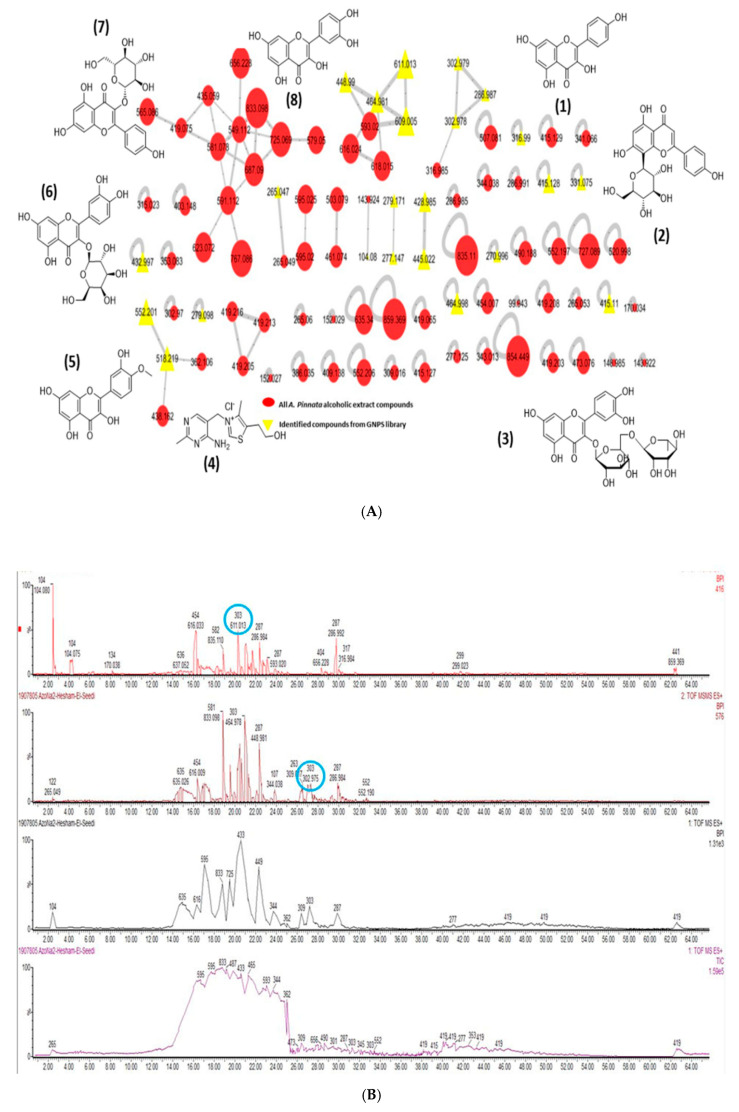
The mass profiling molecular networking for the metabolites of the species A. pinnata presented 89 nodes for 89 parent masses, as seen in Figure 2.
Figure 2.
(A) Base peak MS chromatogram showing the major components of A. pinnata. (B) A. pinnata metabolite parent masses molecular network. The red circular nodes refer to all metabolite parent masses revealed from raw mass spectra. The yellow triangle nodes are for the identified metabolites from the Global Natural Product Social Molecular Networking (GNPS) library.
All the nodes are reflections of metabolites with unique peaks in the raw mass spectra. The bigger the node size, the higher the intensity of the metabolites. The intensity indicates the number of the compounds’ ions in the extract. Five clusters for chemically related metabolites with common classes are detected in the molecular network. Out of 89 metabolites, only 22 were identified based on the molecular networking database. Eight metabolites were found to be reliable and are considered, as shown in Table 1 [44].
Table 1.
Identified compounds from A. pinnata ethanolic extract (APE) using GNPS molecular networking database.
| Compound | M.F | M.W(Da) |
|---|---|---|
| Kaempferol (1) | [C15H10O6] + | 286.987 |
| Vitexin (2) | [C21H20O10] + | 432.997 |
| Rutin (3) | [C27H30O16] + | 611.013 |
| Thiamine (4) | [C12H17N4OS] + | 265.047 |
| Tamarixetin (5) | [C16H12O7] + | 316.99 |
| Hyperoside (6) | [C21H20O12] + | 464.981 |
| Astragalin (7) | [C21H20O11] + | 448.99 |
| Quercetin (8) | [C15H10O7] + | 302.979 |
M.F; molecular formula, + Correlated to [M+H], M.W. (Da); molecular weight (Dalton).
A. pinnata ethanolic extract was found to be rich in flavonoids. These flavonoids were identified using molecular networking (GNPS) and prescribed as follows: kaempferol with m/z 286.987 [C15H10O6]+ [M + H]+ and its glucoside derivative, i.e., m/z 448.99 [C21H20O11]+ by loss of glucoside (−162 amu), annotated as kaempferol-O-glucoside (astragalin); a flavonoid with m/z 302.979 [C15H10O7]+ [M + H]+, reported as quercetin, and its glucoside moieties with m/z 464.91 [C22H23O11]+ by loss of glucoside (−162 amu), annotated as quercetin-O-glucoside (hyperoside), and loss of two glucoside units (−324 amu) m/z 611.013 [C27H30O16]+ [M + H]+, annotated as rutin; vitexin m/z 432.997 [C21H20O10]+ [M + H]+, which is the flavone C-glycoside. Additionally, vitexin was revealed to exert notable antioxidant activity against 5-(6-)chloromethyl-2′,7′-dichlorodihydrofluorescein diacetate (CM-H2DCFDA), and robust free radical scavenging activity in UVB-irradiated human dermal fibroblasts. We also identified the following: amarixetin m/z 316.99 [C16H12O7]+ [M + H]+; peonidin-O-glucoside m/z 464.998 [C22H23O11]+ [M + H]+; a flavonoid with m/z 609 [C27H31O16]+ [M + H]+ with two glucoside moieties (−324 amu), annotated as delphinidin-3-rutinoside.
3.3. A. pinnata Extract Normalized Lead Acetate Reduced Final Body Weight of Rtas
Table 2 shows the initial and final weights of the rats of different experimental groups. The intoxication of rats with lead acetate significantly (p < 0.05) decreased the final weights compared with those of the control group. However, the administration of lead acetate-intoxicated rats with APE (fourth, fifth, and sixth groups) normalized body weights. On the other hand, APE itself had no significant effect on rats’ final body weights (Table 2).
Table 2.
Initial and final body weights of rats of all experimental groups.
| Parameters | Control | Lead | APE | Lead and APE | APE Then Lead | Lead Then APE |
|---|---|---|---|---|---|---|
| Initial BW (g) | 121.20 ± 1.28 | 120.20 ± 1.14 | 120.30 ± 1.03 | 120.00 ± 0.85 | 120.30 ± 1.03 | 120.40 ± 0.79 |
| Final BW (g) | 166.90 ± 2.91 a | 101.29 ± 3.39 b | 161.30 ± 2.54 a | 150.33 ± 0.88 a | 154.56 ± 4.19 a | 151.50 ± 3.33 a |
The values are expressed as the means ± SE. Values carrying different letters in the same row are significantly different. Azolla pinnata ethanolic extract, APE; body weight, BW.
3.4. A. pinnata Extract Modulated the Toxic Effects of Lead Acetate on Liver and Kidney Functions Biomarkers
The intoxication of the rats with lead acetate significantly elevated (p < 0.05) the activities of serum ALT and AST, and serum levels of urea and creatinine compared with the control group. However, the supplementation of rats with APE—before, during, or after their intoxication with lead acetate (fourth, fifth or sixth groups)—significantly reduced the lead acetate-elevated activities of serum ALT and AST, and serum levels of urea and creatinine compared with rats intoxicated with lead acetate only (second group) (p < 0.05). Treating rats with APE (third group) had no significant effect on liver and kidney function biomarkers compared with the control rats (first group) (p < 0.05) (Table 3).
Table 3.
The effect of lead acetate and/or Azolla pinnata ethanolic extract (APE) on liver and kidney function biomarkers in rats.
| Parameters | Control | Lead | APE | Lead and APE | APE Then Lead | Lead Then APE |
|---|---|---|---|---|---|---|
| ALT (U/L) | 18.00 ± 3.42 b | 52.00 ± 0.85 a | 19.00 ± 2.09 b | 22.75 ± 3.21 b | 45. 80 ± 0.88 a | 23.75 ± 5.61 b |
| AST (U/L) | 110.40 ± 6.35 c | 157.20 ± 8.5 a | 110.00 ± 7.78 c | 135.00 ± 4.44 b | 132.40 ± 3.02 b | 137.00 ± 4.69 b |
| Creatinine (mg/dL) | 0.72 ± 0.02 b | 1.03 ± 0.05 a | 0.62 ± 0.02 b | 0.85 ± 0.03 b | 0.73 ± 0.04 b | 0.74 ± 0.02 b |
| Urea (mg /dL) | 19.41 ± 1.08 d | 38.03 ± 0.65 a | 21.60 ± 0.66 cd | 23.85 ± 1.29 c | 27.73 ± 0.42 b | 29.72 ± 1.78 b |
The values are expressed as the means ± SE. Values carrying different letters in the same row are significantly different. Azolla pinnata ethanolic extract, APE; alanine aminotransferase, ALT; aspartate aminotransferase, AST.
3.5. A. pinnata Extract Reversed the Effects of Lead Acetate on Serum Levels of Inflammatory and Anti-Inflammatory Cytokines
The effects of lead acetate and/or APE on serum levels of IL-1β, IL-10, and TNF-α are presented in Table 3. The administration of rats of the second group with lead acetate significantly elevated (p < 0.05) serum levels of IL-1β and TNF-α, while it reduced serum levels of IL-10 compared with the control rats. However, treating lead acetated-intoxicated rats (fourth, fifth and sixth groups) with APE significantly reduced (p < 0.05) the elevated serum levels of IL-1β and TNF- α, while it increased serums level of IL-10 compared with the lead acetate-intoxicated group (second group). Supplementation of rats with APE (third group) significantly elevated (p < 0.05) serum levels of IL-10, while it had no significant effects on serum levels of IL-1β and TNF-α compared with the control rats (Table 4).
Table 4.
The effects of lead and/or Azolla pinnata ethanolic extract (APE) on serum levels of tumor necrosis factor alpha (TNF-α), interleukin 1 beta (IL-1 β) and IL-10 in rats.
| Parameters | Control | Lead | APE | Lead and APE | APE Then Lead | Lead Then APE |
|---|---|---|---|---|---|---|
| TNF-α (pg/mL) | 85.80 ± 2.10 c | 117.75 ± 2.78 a | 86.60 ± 2.56 c | 97.50 ± 2.96 b | 95.0 ± 2.59 b | 104.20 ± 2.54 b |
| IL-1β (pg/mL) | 177.20 ± 3.34 b | 284.60 ± 3.30 a | 169.20 ± 1.93 b | 194.75 ± 3.07 b | 193.60 ± 5.27 b | 199.40 ± 4.23 b |
| IL-10 (pg/mL) | 5.82 ± 0.32 b | 1.73 ± 0.23 d | 8.92 ± 0.46 a | 5.70 ± 0.38 b | 3.73 ± 0.71 c | 3.725 ± 0.55 c |
The values are expressed as the means ± SE. Values carrying different letters in the same row are significantly different. Azolla pinnata ethanolic extract, APE; tumor necrosis factor alpha, TNF-α; interleukin 1 beta, IL-1β; interleukin 10, IL-10.
3.6. A. pinnata Extract Ameliorated the Deleterious Effects of Lead Acetate on Oxidative/Antioxidant Status in Hepatic Tissues of Rats
The effects of lead acetate and/or APE on the hepatic tissue lipid peroxidation and antioxidant defense system biomarkers of rats are shown in Table 4. Orally administrated lead acetate significantly increased the hepatic tissue level of MDA (p < 0.05) compared with the normal control rats. However, treatment of lead acetate-intoxicated rats (fourth, fifth, and sixth groups) with APE significantly reduced MDA contents in the hepatic tissue (p < 0.05) compared with lead acetate-intoxicated group (second group). In contrast, lead acetate significantly reduced GSH contents, SOD, and CAT activities in hepatic tissues of the second groups compared with the control group. However, supplementation of lead acetate-intoxicated rats with APE significantly elevated GSH contents, SOD, and CAT activities in hepatic tissues of fourth, fifth and sixth groups compared with the rats intoxicated with lead acetate alone (second group). APE itself had no significant effect on MDA and GSH contents, SOD, and CAT activities in hepatic tissues of rats of the second group compared with normal control rats (Table 5).
Table 5.
Effect of lead and/or Azolla Pinnata ethanolic extract (APE) on lipid peroxidation and antioxidant biomarkers in hepatic tissues in rats.
| Parameters | Control | Lead | APE | Lead and APE | APE Then Lead | Lead Then APE |
|---|---|---|---|---|---|---|
| MDA (nmol/g tissue) | 8.85 ± 0.38 c | 17.64 ± 0.27 a | 10.32 ± 0.44 bc | 12.42 ± 0.73 b | 12.34 ± 0.16 b | 10.95 ± 0.63 b |
| GSH (mmol/g tissue) | 2.84 ± 0.14 a | 0.49 ± 0.0 c | 2.69 ± 0.11 a | 1.22 ± 0.09 b | 2.63 ± 0.21 a | 1.31 ± 0.30 b |
| CAT (U/ g tissue) | 0.66 ± 0.01 a | 0.22 ± 0.0 c | 0.63 ± 0.01 a | 0.35 ± 0.02 b | 0.35 ± 0.02 b | 0.33 ± 0.05 b |
| SOD (U/g tissue) | 3.43 ± 0.08 a | 1.67 ± 0.06 c | 3.57 ± 0.06 a | 2.84 ± 0.09 b | 3.16 ± 0.18 a | 2. 82 ± 0.16 b |
The values are expressed as the means ± SE. Values carrying different letters in the same row are significantly different. Azolla pinnata ethanolic extract, APE; malondialdehyde, MDA; reduced glutathione, GSH; catalase, CAT; superoxide dismutase, SOD.
3.7. A. pinnata Extract Ameliorated the Degenerative Effect of Lead Acetate on Hepatic Tissues of Rats
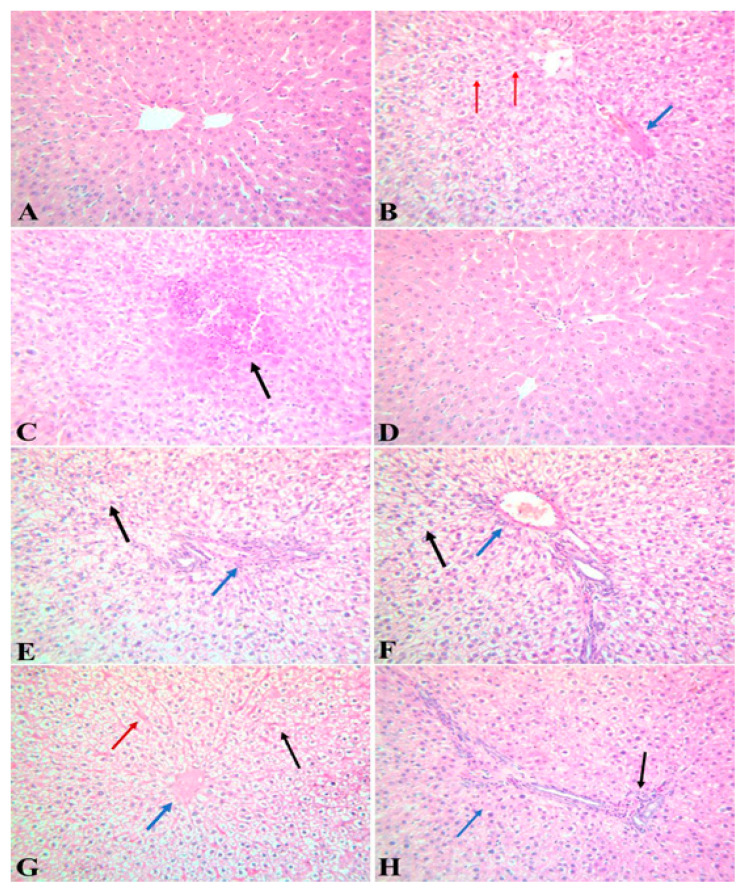
Figure 3 and Table 5 show a histopathological examination of the liver tissues of the different experimental groups. The liver tissues of the control group showed a normal hepatic tissue structure (Figure 3A). The hepatic tissue of the lead acetate-intoxicated group showed a variety of pathological changes represented as severely congested blood vessels and hepatic sinusoids, degenerative changes in the hepatic parenchyma, and multiple areas of coagulative necrosis. Mononuclear cell infiltrations and the proliferation of Kupffer cells were present (Figure 3B,C). A microscopic examination of the hepatic tissue of the APE group showed normal hepatic tissue (Figure 3D). A microscopic examination of the hepatic tissue of rats administrated with lead acetate and the APE group showed moderately congested blood vessels with perivascular infiltration; the hepatocytes showed diffuse swelling and vacuolar degeneration (Figure 3E,F). An examination of hepatic tissue of rats treated with APE, then intoxicated with lead acetate, showed congested blood vessels and hepatic sinusoids with diffuse vacuolation of hepatocytes (Figure 3G). The liver tissue of rats intoxicated with lead acetate, then treated with APE extract, showed congested blood vessels with perivascular infiltration, while the hepatocytes showed single-cell necrosis (Figure 3H).
Figure 3.
Photomicrographs of liver tissues sections of different groups stained with hematoxylin and eosin (H&E). (A) Liver tissue from rats of the control group showed a normal hepatic tissue structure; (B,C) hepatic tissues of rats from the lead acetate-intoxicated group showed congested blood vessels (blue arrow) and hepatic sinusoids, multiple areas of coagulative necrosis (black arrow) and mononuclear cell infiltrations, as well as the activation and proliferation of Kupffer cells (red arrow); (D) liver tissue of rats from the APE group showed normal hepatic tissue; (E,F) liver tissue of rats intoxicated with lead acetate and treated with APE showed congested blood vessels with perivascular infiltration (blue arrow), while the hepatocytes showed swelling and vacuolar degeneration (black arrow); (G) hepatic tissue of rats administrated with APE then intoxicated with lead acetate showed congested blood vessels (blue arrow) and hepatic sinusoids (red arrow) with vacuolation of hepatocytes (black arrow); (H) liver tissue of rats intoxicated with lead acetate then treated with APE showed congested blood vessels with perivascular infiltration (black arrow), while the hepatocytes showed single-cell necrosis (blue arrow) (H and E × 40). The severity of the pathological findings was assessed by using a modified semiquantitative scoring system (- means no changes were present, + means mild changes, ++ means moderate and +++ means severe).
3.8. A. pinnata Extract Reduced Lead Acetate-Induced Caspase 3 Protein Expression in Hepatic Tissues of Rats
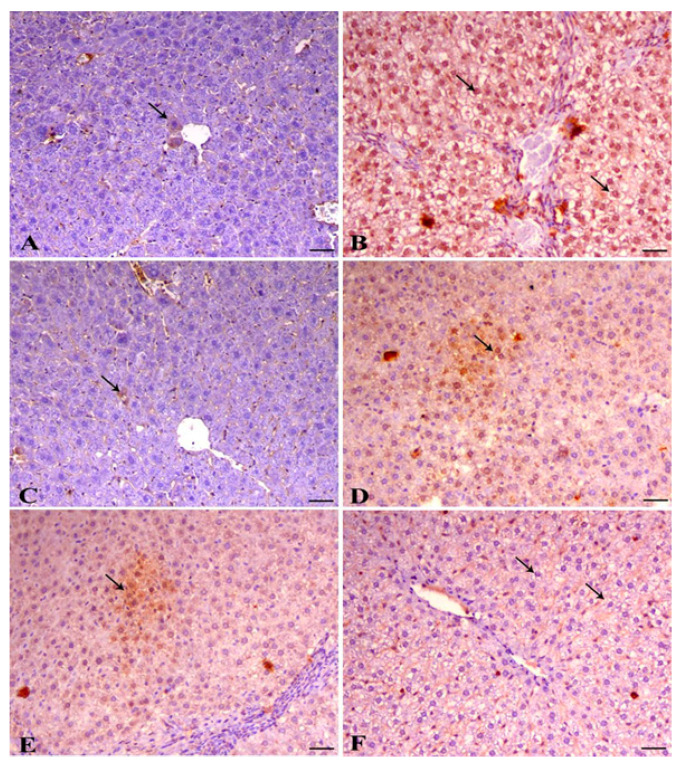
The effects of lead acetate and/or APE on caspase 3 protein expression in the hepatic tissue of rats are shown in Figure 3 and Table 6. The livers of control rats showed a mild expression of caspase 3 within the hepatocytes (arrow indicates nuclear expression) Figure 4A. The oral administration of lead acetate in the second group significantly elevated (p < 0.05) the protein expression of caspase 3 in the nucleus and cytoplasm of hepatic tissue compared with the control group (Figure 4B and Table 6). The livers of rats treated with Azolla showed a mild expression of caspase 3 within the hepatocytes (arrow indicates cytoplasmic expression) Figure 4C. However, treating the lead acetate-intoxicated rats with APE extract (fourth, fifth and sixth groups) significantly reduced hepatic caspase 3 protein expression compared with rats intoxicated with lead acetate alone (second group) Figure 4D–F and Table 7.
Table 6.
Histopathologic changes induced by lead and ameliorative effect of Azolla pinnata ethanolic extract (APE) in hepatic tissues.
| Lesions | Control | Lead | APE | Lead and APE | APE Then Lead | Lead Then APE |
|---|---|---|---|---|---|---|
| Vascular and inflammatory changes | - | +++ | - | + | + | ++ |
| Degenerative and necrotic changes | - | +++ | - | + | + | ++ |
| Proliferative changes | - | ++ | - | - | - |
- means no changes, + means mild changes, ++ means moderate changes, +++ means severe changes. Azolla pinnata ethanolic extract, APE.
Figure 4.
Immunohistochemical analysis of activated caspase 3 in liver tissue of rats. (A) Liver of control animal showing mild expression of caspase 3 within the hepatocytes (arrow indicates nuclear expression), cleaved form of caspase 3 IHC, bar = 50 µm, ×200. (B) Liver of lead-intoxicated animal showing marked expression of caspase 3 of both cytoplasmic and nuclear expression within the hepatocytes (arrows), cleaved form of caspase 3 IHC, bar = 50 µm, ×200. (C) Liver of normal animal treated with Azolla showing mild expression of caspase 3 within the hepatocytes (arrow indicates cytoplasmic expression), cleaved form of caspase 3 IHC, bar = 50 µm, ×200. (D) Liver of animal treated with both lead and Azolla showing decrease the expression of caspase 3 (arrow), cleaved form of caspase 3 IHC, bar = 50 µm, ×200. (E) Liver of diseased animal pretreated with Azolla showing mild cytoplasmic expression of caspase 3 (arrows), cleaved form of caspase 3 IHC, bar = 50 µm, ×200. (F) Liver of diseased animal treated with Azolla showing marked decrease in caspase 3 expression within the hepatocytes (arrow), cleaved form of caspase 3 IHC, bar = 50 µm, ×200. The labelling indices of caspase 3 were expressed as the percentage of positive cells per total 1000 counted cells in about 10 high-power fields.
Table 7.
Effects of lead and/or Azolla Pinnata ethanolic extract (APE) on the expression of caspase 3 in hepatic tissues of rats.
| Control | Lead | APE | Lead and APE | APE then Lea | Lead then APE | |
|---|---|---|---|---|---|---|
| Caspase 3 expression | 10.25 ± 0.67 e | 70.5 ± 3.73 a | 9.20 ± 0.61 e | 27.03 ± 1.97 c | 18.37 ± 1.01 d | 38.83 ± 1.22 b |
Values are expressed as the means ± SE. Values carrying different letters in the same row are significantly different. Azolla pinnata ethanolic extract, APE.
4. Discussion
The intoxication of rats with lead acetate decreased the rats’ final body weight. These findings were in line with that of Amjad et al., who indicated that lead induces weight loss in rats [45]. This decrement in the lead acetate-intoxicated rats’ final body weights was caused by the metal toxicity, which induced nausea, vomiting, and anorexia [46] as well as the oxidative stress [47,48,49] that leads dramatically to catabolic states where wasted muscles and cachexia are seen, followed by low body weight [50]. Moreover, lead toxicity has been shown to disrupt hepatic tissue architecture and function [51,52,53]. The results of the current study showed that the intoxication of rats with lead acetate-induced hepatotoxicity, as represented by the elevated activities of serum ALT and AST (Table 3). This finding was in line with those reported by [54], who indicated that lead acetate increases the activities of serum ALT and AST. This finding was explained by the fact that lead acetate induced oxidative stress in hepatic tissues, as it increased the hepatic tissue contents of MDA, while it decreased the hepatic tissue contents of GSH and similarly decreased the activities of SOD and CAT (Table 5). The findings were also in agreement with those discussed by [7], who indicated that lead induces oxidative stress in hepatic tissues as a result of the increase in lipid peroxidation and the antioxidant defense system disturbance in hepatocytes, leading to hepatic injury. Thus, lead acetate and its metabolites induce the redox cycle, with the generation of superoxide radicals and hydrogen peroxide, which subsequently increases lipid peroxidation and decreases antioxidant enzyme activities, resulting in hepatocyte destruction, the activation of innate immunity by producing pro-inflammatory cytokines such as TNF-α and IL-1β in hepatic tissues (Table 4) [55,56]. Lead damages many tissues through the induction of oxidative stress [26,57], leading to lipid peroxidation, which induces inflammatory processes [58]. Moreover, occupational exposure of humans to lead increases serum levels of some pro-inflammatory cytokines [59] such as IL-1, IL-6, and TNF- α [60]. TNF-α is produced at the site of inflammation by activated macrophages and lymphocytes and participates with IL-1β and IL-6 to induce systemic inflammatory reactions [61]. Furthermore, the intoxication of rats with lead acetate in the current study decreased the serum level of the anti-inflammatory cytokine IL-10 (Table 4). This finding was consistent with that of [62,63], who indicated that exposure to lead acetate decreases IL-10 in the rats’ cerebral cortex, confirming the role of leadership in the development of an inflammatory response in rat brain tissue [62]. Such a decrease in IL-10 due to lead acetate exposure may be implicated in the increased serum levels of IL-1β and the promotion of inflammatory signals, as it was shown that IL-10 can block IL-1β gene expression [64]. These inflammatory cytokines may injure the hepatic tissues through activation of the caspase cascade signaling pathway and, as our results revealed, lead acetate intoxication increased caspase 3 protein expression in hepatic tissue. TNF-α has been indicated to induce the apoptosis of hepatocytes through the activation of caspase, while caspase inhibitors block TNF-α production and its signaling pathways [65]. Caspase 3 can be activated in the apoptotic cells either by extrinsic stimuli, including lead acetate, or intrinsic factors inducing mitochondrial stress [66], and it plays important roles in cell apoptosis [67]. In addition, it causes the activation of the innate immunity system by producing pro-inflammatory markers such as TNF-α and IL-1. Furthermore, our study was in accordance with that of [7] who reported that the lead acetate intoxication of rats induces hepatic tissue necrosis and increases serum transaminase activity and hepatic lipid peroxidation. Collectively, lead acetate induced oxidative stress and increased pro-inflammatory mediators, leading to histopathological changes in hepatic tissues (Figure 3), which matched with the results of Arun et al. (2014) [27]. Finally, hepatic tissue injury damages hepatocytes and cause the discharge of liver enzymes, which consequently raises their activities [25].
Regarding the ameliorative effects of the Azolla pinnata ethanolic extract against lead acetate-induced hepatotoxicity, our results showed that oral administration of A. pinnata decreased the activities of serum ALT and AST and normalized serum levels of urea and creatinine (Table 2). These findings were in line with those of Debashis et al. (2016) [21], who reported that A. pinnata reduces serum activities of ALT and AST. The ameliorative effects of A. pinnata against lead acetate-induced hepatotoxicity may be attributed to the antioxidant and anti-inflammatory activities of its constituents as 10 metabolites were found to be reliable (Figure 3 and Figure 4, Table 1) [44]. A. pinnata ethanolic extract was found to be rich in flavonoids, which are well-known for their antioxidant and anti-inflammatory activities [68]. These flavonoids include kaempferol and its glucoside derivative, namely kaempferol-O-glucoside (astragalin). Kaempferol sugar derivatives were studied for their antioxidant and anti-inflammatory scavenging activity for DPPH radicals and protection against oxidative stress-induced cell death [69]. Quercetin and its glucoside moieties are produced by the loss of glucoside annotated as quercetin-O-glucoside (hyperoside) or by the loss of two glucoside units that were annotated as rutin [70]. Quercetin and its glucoside moieties were reported to inhibit glioma cell proliferation and migration and modulate inflammatory and growth factors [71]. Vitexin, which is a flavone C-glycoside known for possessing anti-inflammatory activity and inhibiting IL-1β, IL-33 [72], IL-6 and TNF-α [73], was revealed to exert notable antioxidant activity against 5-(6-)chloromethyl-2′,7′-dichlorodihydrofluorescein diacetate (CM-H2DCFDA), and robust free radical scavenging activity in UVB-irradiated human dermal fibroblasts [74]. Tamarixetin exhibited superior anti-inflammatory activity by reducing the secretion of several inflammatory cytokines [73]. These compounds may reduce lipid peroxidation and inflammatory cytokines while increasing antioxidant and anti-inflammatory activities (Table 3 and Table 4), thus consequently modulating lead acetate-induced apoptosis and injury of hepatic tissues (Figure 3 and Figure 4, Table 5 and Table 6). These beneficial effects of APE against lead acetate-induced hepatotoxicity confirmed the findings of Mandal et al. (1993) [66], who indicated that A. pinnata suppresses lipid peroxidation and scavenges free radicals, preventing pathological changes in the hepatic tissue architecture [25]. Quercetin normalizes thioacetamide and thus increases the liver biomarkers ALT and AST through the inhibition of p-extracellular signal-regulated kinase (ERK)1/2 and an increase in Bax/Bcl-2 ratio, causing the prevention of cell apoptosis [67]. Moreover, quercetin suppresses prenatal stress–increased serum IL-1β levels via increasing serum IL-10 levels in rats [75]. Thus, the hepatoprotective effect of A. pinnata might be attributed to its free radical scavenging activity [76], which suppresses, with the help of Tamarixetin (quercetin 4-methylether), the activity of caspase 3 [77]. The reduction in lead acetate toxicity-induced oxidative stress in our study was not achieved only by quercetin, but also by thiamine [78] as it reduces ethanol-induced oxidative stress in rats by scavenging free radicals or by the regeneration of vitamin E, reducing glutathione levels. Rutin suppresses the activity of pro-inflammatory cytokines through diminishing TNF-α and IL-1β levels [79] and inhibits the hypoxia and excessive glutamate stress-induced caspase 3 expression in retinal ganglion cell [80]. Hence, rutin has hepatoprotective effects against paracetamol, and carbon tetrachloride-induced hepatic toxicity [81]. Hyperoside present in A. pinnata has an antioxidant activity by increasing the expression of heme oxygenase-1 (HO-1) and inducing extracellular signal-regulated kinase (ERK) phosphorylation and nuclear factor erythroid 2-related factor 2 (Nrf2) antioxidant response and binding activity, preventing hydrogen peroxide-induced cytotoxicity [72]. Vitexin (Apigenin-8-C-β-D-glucopyranoside) is a chemical compound found in many plants [82] and has a variety of pharmacological activities, including antioxidant [83] and anti-inflammatory effects [84,85]. The antioxidant activity of vitexin is related to its capability to donate electrons, which enables it to act as a good free radical scavenger as it reacts with ROS as 4-OH, 7-OH, and 5-OH [86]. Moreover, the astragalin content of A. pinnata in our study may have an anti-inflammatory effect through decreasing serum levels of TNF-α and IL-1β, as it has been indicated that astragalin reduced lipopolysaccharide-induced inflammatory cell infiltration, myeloperoxidase activity and TNF-α, IL-1β and IL-6 expression through inhibiting nuclear factor-kappa B (NF-κB) activation and nuclear factor of kappa light polypeptide gene enhancer in B-cells alpha (IκBα) in the mammary glands of a murine model [87]. Taken together, the possible causes of the hepatoprotective effects of A. pinnata against lead acetate-induced hepatotoxicity in our study are the antioxidant, anti-inflammatory and anti-apoptotic activities of A. pinnata phytochemical contents as they decreased serum levels of TNF-α and IL-1β as well as oxidative stress and caspase 3 protein expression in hepatic tissue, while they increased serum levels of IL-10 and antioxidant activity in hepatic tissues. These activities ameliorated lead acetate-induced histopathological changes in hepatic tissues.
5. Conclusions
Lead acetate-induced hepatotoxicity in rats is manifested by oxidative stress, increased pro-inflammatory cytokines, and pro-apoptotic protein in hepatic tissue. However, A. pinnata ethanolic extract ameliorated lead acetate-induced hepatotoxicity by reducing oxidative stress and pro-apoptotic protein expression in hepatic tissue, as well as pro-inflammatory cytokine production. Moreover, A. pinnata ethanolic extract increased anti-inflammatory cytokine production and antioxidant activities in hepatic tissue; thus, it appears to be a promising hepatoprotective agent against toxicants that induce hepatotoxicity.
Acknowledgments
The authors would like to extend their sincere appreciation to the Researchers Supporting Project (RSP-2020/96), King Saud University, Riyadh, Saudi Arabia, and to the Swedish Research links grant 2016-05885 (VR for the years 2017–2019) and the Department of Molecular Biosciences, Wenner-Grens Institute, Stockholm University, Sweden, for the financial support.
Author Contributions
Study design, A.S.A.E. and M.A.A.E.; acquisition, A.A.M. and S.H.O.; experimental work, A.S.A.E., A.A.M., S.H.O., M.A.E.-G.M. and S.M.G.-A.; analysis, A.S.A.E., H.R.E.-S., S.A.M.K. and M.A.A.E.; interpretation of data, M.M.A.-D., A.S.A.E., R.A. and M.A.A.E.; writing, A.S.A.E., A.A.M., S.H.O., M.A.E.-G.M., S.M.G.-A., R.A. and M.A.A.E.; writing and reviewing, S.A.M.K., H.R.E.-S., M.M.A.-D. and M.A.A.E.; funding, H.R.E.-S., M.M.A.-D., and M.A.A.E.; substantially revising the manuscript, H.R.E.-S. and M.A.A.E. All authors have read and agreed to the published version of the manuscript.
Funding
We are very grateful to the Swedish Research links grant VR 2016-05885 and the Department of Molecular Biosciences, Wenner-Grens Institute, Stockholm University, Sweden, as well as project number RSP-2020/96 of King Saud University, Riyadh, Saudi Arabia, for the financial support.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pal A., Banerjee B., Banerjee T., Masih M., Pal K. Hepatoprotective activity of Chenopodium album Linn. plant against paracetamol induced hepatic injury in rats. Int. J. Pharm. Pharm. Sci. 2011;3:55–57. [Google Scholar]
- 2.Gurer H., Ercal N. Can antioxidants be beneficial in the treatment of lead poisoning? Free Radic. Biol. Med. 2000;29:927–945. doi: 10.1016/S0891-5849(00)00413-5. [DOI] [PubMed] [Google Scholar]
- 3.Lightfoot T.L., Yeager J.M. Pet bird toxicity and related environmental concerns. Vet. Clin. N. Am. Exot. Anim. Pract. 2008;11:229–259. doi: 10.1016/j.cvex.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 4.Ferreyra H., Romano M., Uhart M. Recent and chronic exposure of wild ducks to lead in human-modified wetlands in Santa Fe Province, Argentina. J. Wildl. Dis. 2009;45:823–827. doi: 10.7589/0090-3558-45.3.823. [DOI] [PubMed] [Google Scholar]
- 5.Campbell J.R., Moss M.E., Raubertas R.F. The association between caries and childhood lead exposure. Environ. Health Perspect. 2000;108:1099–1102. doi: 10.1289/ehp.001081099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flora S.J.S., Saxena G., Mehta A. Reversal of lead-induced neuronal apoptosis by chelation treatment in rats: Role of reactive oxygen species and intracellular Ca2+ J. Pharmacol. Exp. Ther. 2007;322:108–116. doi: 10.1124/jpet.107.121996. [DOI] [PubMed] [Google Scholar]
- 7.Alhusaini A.M., Faddah L.M., Hasan I.H., Jarallah S.J., Alghamdi S.H., Alhadab N.M., Badr A., Elorabi N., Zakaria E., Al-Anazi A. Vitamin C and Turmeric Attenuate Bax and Bcl-2 Proteins’ Expressions and DNA Damage in Lead Acetate-Induced Liver Injury. Dose-Response. 2019;17:1559325819885782. doi: 10.1177/1559325819885782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bray T.M., Bettger W.J. The physiological role of zinc as an antioxidant. Free Radic. Biol. Med. 1990;8:281–291. doi: 10.1016/0891-5849(90)90076-U. [DOI] [PubMed] [Google Scholar]
- 9.Atawodi S.E. Evaluation of the Hypoglycemic, Hypolipidemic and Antioxidant Effects of Methanolic Extract of” Ata-Ofa” Polyherbal Tea (APolyherbal) in Alloxan-Induced Diabetic Rats. Drug Invent. Today. 2011;3:11. [Google Scholar]
- 10.White L.D., Cory-Slechta D.A., Gilbert M.E., Tiffany-Castiglioni E., Zawia N.H., Virgolini M., Rossi-George A., Lasley S.M., Qian Y.C., Basha M.R. New and evolving concepts in the neurotoxicology of lead. Toxicol. Appl. Pharmacol. 2007;225:1–27. doi: 10.1016/j.taap.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 11.Billings R.J., Berkowitz R.J., Watson G. Teeth. Pediatrics. 2004;113:1120–1127. [PubMed] [Google Scholar]
- 12.Lanphear B.P., Hornung R., Khoury J., Yolton K., Baghurst P., Bellinger D.C., Canfield R.L., Dietrich K.N., Bornschein R., Greene T. Low-level environmental lead exposure and children’s intellectual function: An international pooled analysis. Environ. Health Perspect. 2005;113:894–899. doi: 10.1289/ehp.7688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pokras M.A., Kneeland M.R. Lead poisoning: Using transdisciplinary approaches to solve an ancient problem. EcoHealth. 2008;5:379–385. doi: 10.1007/s10393-008-0177-x. [DOI] [PubMed] [Google Scholar]
- 14.Merill J.C., Morton J.J.P., Soileau S.D. Metals. In: Hayes A.W., editor. Principles and Methods of Toxicology. 5th ed. CRC Press; Boca Raton, FL, USA: 2007. [Google Scholar]
- 15.Henretig F.M. Lead. In: Golgfrank L.R., editor. Goldfrank’s Toxicoliogic Emergencies. 8th ed. McGraw Hill Professional; New York, NY, USA: 2006. [Google Scholar]
- 16.Patrick L. Lead toxicity, a review of the literature. Part 1: Exposure, evaluation, and treatment. Altern. Med. Rev. 2006;11:2–22. [PubMed] [Google Scholar]
- 17.El Safoury O.S., Abd El Fatah D.S., Ibrahim M. Treatment of periocular hyperpigmentation due to lead of kohl (surma) by penicillamine: A single group non-randomized clinical trial. Indian J. Dermatol. 2009;54:361. doi: 10.4103/0019-5154.57614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shamsi-Baghbanan H., Sharifian A., Esmaeili S., Minaei B. Hepatoprotective herbs, avicenna viewpoint. Iran. Red Crescent Med. J. 2014;16:e12313. doi: 10.5812/ircmj.12313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boonstra A., van der Laan L.J.W., Vanwolleghem T., Janssen H.L.A. Experimental models for hepatitis C viral infection. Hepatology. 2009;50:1646–1655. doi: 10.1002/hep.23138. [DOI] [PubMed] [Google Scholar]
- 20.Lal S.S., Nayak P.L. Green synthesis of gold nanoparticles using various extract of plants and spices. Int. J. Sci. Innov. Discov. 2012;2:325–350. [Google Scholar]
- 21.Roy D., Kumar V., Kumar M., Sirohi R., Singh Y., Singh J.K. Effect of feeding Azolla pinnata on growth performance, feed intake, nutrient digestibility and blood biochemical’s of Hariana heifers fed on roughage based diet. Indian J. Dairy Sci. 2016;69:190–196. [Google Scholar]
- 22.Mithraja M.J., Marimuthu J., Mahesh M., Paul Z.M., Jeeva S. Phytochemical studies on Azolla pinnata R. Br., Marsilea minuta L. and Salvinia molesta Mitch. Asian Pac. J. Trop. Biomed. 2011;1:S26–S29. doi: 10.1016/S2221-1691(11)60116-0. [DOI] [Google Scholar]
- 23.Kumar G., Chander H. Study on the Potential of Azolla pinnata as livestock Feed Supplement for climate Change adaptation and Mitigation. Asian J. Adv. Basic Sci. 2017;5:65–68. [Google Scholar]
- 24.Mousa A.A., El-Gansh H.A.I., Abd Eldaim M.A., Mohamed M.A.E.-G., Morsi A.H., El Sabagh H.S. Protective effect of Moringa oleifera leaves ethanolic extract against thioacetamide-induced hepatotoxicity in rats via modulation of cellular antioxidant, apoptotic and inflammatory markers. Environ. Sci. Pollut. Res. 2019;26:32488–32504. doi: 10.1007/s11356-019-06368-4. [DOI] [PubMed] [Google Scholar]
- 25.Kunjiappan S., Chowdhury R., Bhattacharjee C. A green chemistry approach for the synthesis and characterization of bioactive gold nanoparticles using Azolla microphylla methanol extract. Front. Mater. Sci. 2014;8:123–135. doi: 10.1007/s11706-014-0246-8. [DOI] [Google Scholar]
- 26.Gurer-Orhan H., Sabır H.U., Özgüneş H. Correlation between clinical indicators of lead poisoning and oxidative stress parameters in controls and lead-exposed workers. Toxicology. 2004;195:147–154. doi: 10.1016/j.tox.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 27.Kumar A., Kumari J., Kumar H., Nath A., Singh J.K., Ali M., Kumar R. Hepatoprotective and antioxidant effect of Azolla filiculoides on profenofos induced hepatotoxicity in swiss albino mice. Carib. J. Sci. Tech. 2014;2:372–377. [Google Scholar]
- 28.Fawcett J.K., Scott J.E. A rapid and precise method for the determination of urea. J. Clin. Pathol. 1960;13:156–159. doi: 10.1136/jcp.13.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bartels H., Böhmer M., Heierli C. Serum creatinine determination without protein precipitation. Clin. Chim. Acta Int. J. Clin. Chem. 1972;37:193. doi: 10.1016/0009-8981(72)90432-9. [DOI] [PubMed] [Google Scholar]
- 30.Larsen K. Creatinine assay by a reaction-kinetic principle. Clin. Chim. Acta. 1972;41:209–217. doi: 10.1016/0009-8981(72)90513-X. [DOI] [PubMed] [Google Scholar]
- 31.Reitman S., Frankel S. A colorimetric method for the determination of serum glutamic oxalacetic and glutamic pyruvic transaminases. Am. J. Clin. Pathol. 1957;28:56–63. doi: 10.1093/ajcp/28.1.56. [DOI] [PubMed] [Google Scholar]
- 32.Kei S. Serum lipid peroxide in cerebrovascular disorders determined by a new colorimetric method. Clin. Chim. Acta. 1978;90:37–43. doi: 10.1016/0009-8981(78)90081-5. [DOI] [PubMed] [Google Scholar]
- 33.Beutler E. Improved method for the determination of blood glutathione. J. Lab. Clin. Med. 1963;61:882–888. [PubMed] [Google Scholar]
- 34.Nishikimi M., Rao N.A., Yagi K. The occurrence of superoxide anion in the reaction of reduced phenazine methosulfate and molecular oxygen. Biochem. Biophys. Res. Commun. 1972;46:849–854. doi: 10.1016/S0006-291X(72)80218-3. [DOI] [PubMed] [Google Scholar]
- 35.Fossati P., Prencipe L., Berti G. Use of 3, 5-dichloro-2-hydroxybenzenesulfonic acid/4-aminophenazone chromogenic system in direct enzymic assay of uric acid in serum and urine. Clin. Chem. 1980;26:227–231. doi: 10.1093/clinchem/26.2.227. [DOI] [PubMed] [Google Scholar]
- 36.Aebi H. Methods in Enzymology. Volume 105. Elsevier; Amsterdam, The Netherlands: 1984. Catalase in vitro; pp. 121–126. [DOI] [PubMed] [Google Scholar]
- 37.Vidal-Vanaclocha F., Fantuzzi G., Mendoza L., Fuentes A.M., Anasagasti M.J., Martín J., Carrascal T., Walsh P., Reznikov L.L., Kim S.-H. IL-18 regulates IL-1β-dependent hepatic melanoma metastasis via vascular cell adhesion molecule-1. Proc. Natl. Acad. Sci. USA. 2000;97:734–739. doi: 10.1073/pnas.97.2.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brynskov J., Foegh P., Pedersen G., Ellervik C., Kirkegaard T., Bingham A., Saermark T. Tumour necrosis factor α converting enzyme (TACE) activity in the colonic mucosa of patients with inflammatory bowel disease. Gut. 2002;51:37–43. doi: 10.1136/gut.51.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Odewumi C., Latinwo L.M., Sinclair A., Badisa V.L.D., Abdullah A., Badisa R.B. Effect of cadmium on the expression levels of interleukin-1α and interleukin-10 cytokines in human lung cells. Mol. Med. Rep. 2015;12:6422–6426. doi: 10.3892/mmr.2015.4316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hopwood D., Bamcroft J.D., Stevens A. Fixation and Fixatives. 4th ed. Churchill Livingstone; Hong Kong: 1996. Theory and practice of histopathological techniques; pp. 23–46. [Google Scholar]
- 41.Hsu B.-G., Lee R.-P., Yang F.-L., Harn H.-J., Chen H.I. Post-treatment with N-acetylcysteine ameliorates endotoxin shock-induced organ damage in conscious rats. Life Sci. 2006;79:2010–2016. doi: 10.1016/j.lfs.2006.06.040. [DOI] [PubMed] [Google Scholar]
- 42.Chen T.M., Subeq Y.M., Lee R.P., Chiou T.W., Hsu B.G. Single dose intravenous thioacetamide administration as a model of acute liver damage in rats. Int. J. Exp. Pathol. 2008;89:223–231. doi: 10.1111/j.1365-2613.2008.00576.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Orabi S.H., Al-Sabbagh E.S.H., Khalifa H.K., Mohamed M.A.E.-G., Elhamouly M., Gad-Allah S.M., Abdel-Daim M.M., Eldaim M.A.A. Commiphora myrrha Resin Alcoholic Extract Ameliorates High Fat Diet Induced Obesity via Regulation of UCP1 and Adiponectin Proteins Expression in Rats. Nutrients. 2020;12:803. doi: 10.3390/nu12030803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aron A.T., Gentry E.C., McPhail K.L., Nothias L.-F., Nothias-Esposito M., Bouslimani A., Petras D., Gauglitz J.M., Sikora N., Vargas F. Reproducible molecular networking of untargeted mass spectrometry data using GNPS. Nat. Protoc. 2020;15:1954–1991. doi: 10.1038/s41596-020-0317-5. [DOI] [PubMed] [Google Scholar]
- 45.Amjad Z., Yasmin T., Ashraf I., Perveen K., Mirza T., Shoro A.A. Lead-induced morphometric changes in the kidneys of albino rats ameliorated by ginkgo biloba extract (EGb 761) J. Pak. Med. Assoc. 2017;67:58–65. [PubMed] [Google Scholar]
- 46.Rafique M., Perveen K., Khan N., Nigar S. Lead intoxication causing loss of body weight and loss of absolute weight of testes in albino rats. Hamdard Med. 2008;51:123–128. [Google Scholar]
- 47.Ercal N., Gurer-Orhan H., Aykin-Burns N. Toxic metals and oxidative stress part I: Mechanisms involved in metal-induced oxidative damage. Curr. Top. Med. Chem. 2001;1:529–539. doi: 10.2174/1568026013394831. [DOI] [PubMed] [Google Scholar]
- 48.Yeh Y.C., Liu T.J., Wang L.C., Lee H.W., Ting C.T., Lee W.-L., Hung C.-J., Wang K.Y., Lai H.C. A standardized extract of Ginkgo biloba suppresses doxorubicin-induced oxidative stress and p53-mediated mitochondrial apoptosis in rat testes. Br. J. Pharmacol. 2009;156:48–61. doi: 10.1111/j.1476-5381.2008.00042.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Patra R.C., Rautray A.K., Swarup D. Oxidative stress in lead and cadmium toxicity and its amelioration. Vet. Med. Int. 2011;2011:457327. doi: 10.4061/2011/457327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li Y.P., Schwartz R.J., Waddell I.D., Holloway B.R., Reid M.B. Skeletal muscle myocytes undergo protein loss and reactive oxygen-mediated NF-kappaB activation in response to tumor necrosis factor alpha. FASEB J. 1998;12:871–880. doi: 10.1096/fasebj.12.10.971. [DOI] [PubMed] [Google Scholar]
- 51.Singh R., Kumar S., Rana A.C., Sharma N. Different models of hepatotoxicity and related liver diseases: A review. Int. Res. J. Pharm. 2012;3:86–95. [Google Scholar]
- 52.Suganthi V., Gowri S., Gurusamy K. Hepatoprotective activity of Cayratia carnosa on liver damage caused by lead acetate in rats. Sch. Res. Lib. 2013;3:76–79. [Google Scholar]
- 53.Haouem S., Chargui I., Najjar M.F., Sriha B., El Hani A. Liver Function and Structure in Rats Treated Simultaneously with Cadmium and Mercury. Open J. Pathol. 2013;3:26–31. doi: 10.4236/ojpathology.2013.31005. [DOI] [Google Scholar]
- 54.Drill V.A. Pharmacology of hepatotoxic agents. NYASA. 1963;104:858–874. doi: 10.1111/j.1749-6632.1963.tb57088.x. [DOI] [Google Scholar]
- 55.Gao B., Seki E., Brenner D.A., Friedman S., Cohen J.I., Nagy L., Szabo G., Zakhari S. Innate immunity in alcoholic liver disease. Am. J. Physiol. Gastrointest. Liver Physiol. 2011;300:G516–G525. doi: 10.1152/ajpgi.00537.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Núñez M. Hepatotoxicity of antiretrovirals: Incidence, mechanisms and management. J. Hepatol. 2006;44:S132–S139. doi: 10.1016/j.jhep.2005.11.027. [DOI] [PubMed] [Google Scholar]
- 57.Malekirad A.A., Oryan S., Fani A., Babapor V., Hashemi M., Baeeri M., Bayrami Z., Abdollahi M. Study on clinical and biochemical toxicity biomarkers in a zinc-lead mine workers. Toxicol. Ind. Health. 2010;26:331–337. doi: 10.1177/0748233710365697. [DOI] [PubMed] [Google Scholar]
- 58.Sirivarasai J., Wananukul W., Kaojarern S., Chanprasertyothin S., Thongmung N., Ratanachaiwong W., Sura T., Sritara P. Association between inflammatory marker, environmental lead exposure, and glutathione S-transferase gene. Biomed. Res. Int. 2013;2013 doi: 10.1155/2013/474963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Valentino M., Rapisarda V., Santarelli L., Bracci M., Scorcelletti M., Di Lorenzo L., Cassano F., Soleo L. Effect of lead on the levels of some immunoregulatory cytokines in occupationally exposed workers. Hum. Exp. Toxicol. 2007;26:551–556. doi: 10.1177/0960327107073817. [DOI] [PubMed] [Google Scholar]
- 60.Machoń-Grecka A., Dobrakowski M., Boroń M., Lisowska G., Kasperczyk A., Kasperczyk S. The influence of occupational chronic lead exposure on the levels of selected pro-inflammatory cytokines and angiogenic factors. Hum. Exp. Toxicol. 2017;36:467–473. doi: 10.1177/0960327117703688. [DOI] [PubMed] [Google Scholar]
- 61.Turner M.D., Nedjai B., Hurst T., Pennington D.J. Cytokines and chemokines: At the crossroads of cell signalling and inflammatory disease. Biochim. Biophys. Acta (BBA) Mol. Cell Res. 2014;1843:2563–2582. doi: 10.1016/j.bbamcr.2014.05.014. [DOI] [PubMed] [Google Scholar]
- 62.Kasten-Jolly J., Pabello N., Bolivar V.J., Lawrence D.A. Developmental lead effects on behavior and brain gene expression in male and female BALB/cAnNTac mice. Neurotoxicology. 2012;33:1005–1020. doi: 10.1016/j.neuro.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chibowska K., Baranowska-Bosiacka I., Falkowska A., Gutowska I., Goschorska M., Chlubek D. Effect of lead (Pb) on inflammatory processes in the brain. Int. J. Mol. Sci. 2016;17:2140. doi: 10.3390/ijms17122140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wong M.-L., Bongiorno P.B., Rettori V., McCann S.M., Licinio J. Int.erleukin (IL) 1β, IL-1 receptor antagonist, IL-10, and IL-13 gene expression in the central nervous system and anterior pituitary during systemic inflammation: Pathophysiological implications. Proc. Natl. Acad. Sci. USA. 1997;94:227–232. doi: 10.1073/pnas.94.1.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schuchmann M., Varfolomeev E.E., Hermann F., Rueckert F., Strand D., Koehler H., Strand S., Lohse A.W., Wallach D., Galle P.R. Dominant negative MORT1/FADD rescues mice from CD95 and TNF-induced liver failure. Hepatology. 2003;37:129–135. doi: 10.1053/jhep.2003.50011. [DOI] [PubMed] [Google Scholar]
- 66.Salvesen G.S. Program in apoptosis and cell death research, The Burnham Institute. Chem. Rev. 2002;102:4489–4500. doi: 10.1021/cr010183n. [DOI] [PubMed] [Google Scholar]
- 67.Alnemri E.S., Livingston D.J., Nicholson D.W., Salvesen G., Thornberry N.A., Wong W.W., Yuan J. Human ICE/CED-3 protease nomenclature. Cell. 1996;87:171. doi: 10.1016/S0092-8674(00)81334-3. [DOI] [PubMed] [Google Scholar]
- 68.Chen G.-L., Fan M.-X., Wu J.-L., Li N., Guo M.-Q. Antioxidant and anti-inflammatory properties of flavonoids from lotus plumule. Food Chem. 2019;277:706–712. doi: 10.1016/j.foodchem.2018.11.040. [DOI] [PubMed] [Google Scholar]
- 69.Lin C., Wu F., Zheng T., Wang X., Chen Y., Wu X. Kaempferol attenuates retinal ganglion cell death by suppressing NLRP1/NLRP3 inflammasomes and caspase-8 via JNK and NF-κB pathways in acute glaucoma. Eye. 2019;33:777–784. doi: 10.1038/s41433-018-0318-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dohaei M., Karimi K., Rahimmalek M., Satari B. Integrated biorefinery of aquatic fern Azolla filiculoides for enhanced extraction of phenolics, protein, and lipid and methane production from the residues. J. Clean. Prod. 2020;276:123175. doi: 10.1016/j.jclepro.2020.123175. [DOI] [Google Scholar]
- 71.Da Silva A.B., Coelho P.L.C., das Neves Oliveira M., Oliveira J.L., Amparo J.A.O., da Silva K.C., Soares J.R.P., Pitanga B.P.S., dos Santos Souza C., de Faria Lopes G.P. The flavonoid rutin and its aglycone quercetin modulate the microglia inflammatory profile improving antiglioma activity. Brain Behav. Immun. 2020;85:170–185. doi: 10.1016/j.bbi.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 72.Borghi S.M., Carvalho T.T., Staurengo-Ferrari L., Hohmann M.S.N., Pinge-Filho P., Casagrande R., Verri W.A., Jr. Vitexin inhibits inflammatory pain in mice by targeting TRPV1, oxidative stress, and cytokines. J. Nat. Prod. 2013;76:1141–1149. doi: 10.1021/np400222v. [DOI] [PubMed] [Google Scholar]
- 73.Park J.Y., Han X., Piao M.J., Oh M.C., Fernando P.M.D.J., Kang K.A., Ryu Y.S., Jung U., Kim I.G., Hyun J.W. Hyperoside induces endogenous antioxidant system to alleviate oxidative stress. J. Cancer Prev. 2016;21:41. doi: 10.15430/JCP.2016.21.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kim J.H., Lee K.-H., Yoo D.H., Kang D., Cho S.-H., Hong Y.-C. GSTM1 and TNF-α gene polymorphisms and relations between blood lead and inflammatory markers in a non-occupational population. Mutat. Res. Genet. Toxicol. Environ. Mutagenesis. 2007;629:32–39. doi: 10.1016/j.mrgentox.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 75.Mkhize N.V.P., Qulu L., Mabandla M.V. The effect of quercetin on pro-and anti-inflammatory cytokines in a prenatally stressed rat model of febrile seizures. J. Exp. Neurosci. 2017;11:1179069517704668. doi: 10.1177/1179069517704668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Russo G.L., Russo M., Spagnuolo C., Tedesco I., Bilotto S., Iannitti R., Palumbo R. Advances in Nutrition and Cancer. Springer; Berlin/Heidelberg, Germany: 2014. Quercetin: A pleiotropic kinase inhibitor against cancer; pp. 185–205. [DOI] [PubMed] [Google Scholar]
- 77.Murakami A., Ashida H., Terao J. Multitargeted cancer prevention by quercetin. Cancer Lett. 2008;269:315–325. doi: 10.1016/j.canlet.2008.03.046. [DOI] [PubMed] [Google Scholar]
- 78.Portari G.V., Marchini J.S., Vannucchi H., Jordao A.A. Antioxidant effect of thiamine on acutely alcoholized rats and lack of efficacy using thiamine or glucose to reduce blood alcohol content. Basic Clin. Pharmacol. Toxicol. 2008;103:482–486. doi: 10.1111/j.1742-7843.2008.00311.x. [DOI] [PubMed] [Google Scholar]
- 79.Wang G.-Q., Xu T., Bu X.-M., Liu B.-Y. Anti-inflammation effects of corn silk in a rat model of carrageenin-induced pleurisy. Inflammation. 2012;35:822–827. doi: 10.1007/s10753-011-9382-9. [DOI] [PubMed] [Google Scholar]
- 80.Nakayama M., Aihara M., Chen Y.-N., Araie M., Tomita-Yokotani K., Iwashina T. Neuroprotective effects of flavonoids on hypoxia-, glutamate-, and oxidative stress–induced retinal ganglion cell death. Mol. Vis. 2011;17:1784. [PMC free article] [PubMed] [Google Scholar]
- 81.Janbaz K.H., Saeed S.A., Gilani A.H. Protective effect of rutin on paracetamol-and CCl4-induced hepatotoxicity in rodents. Fitoterapia. 2002;73:557–563. doi: 10.1016/S0367-326X(02)00217-4. [DOI] [PubMed] [Google Scholar]
- 82.Abbasi E., Nassiri-Asl M., Sheikhi M., Shafiee M. Effects of vitexin on scopolamine-induced memory impairment in rats. Chin. J. Physiol. 2013;56:184–1889. doi: 10.4077/CJP.2013.BAB123. [DOI] [PubMed] [Google Scholar]
- 83.Bai Y., Chang J., Xu Y., Cheng D., Liu H., Zhao Y., Yu Z. Antioxidant and myocardial preservation activities of natural phytochemicals from mung bean (Vigna radiata L.) seeds. J. Agric. Food Chem. 2016;64:4648–4655. doi: 10.1021/acs.jafc.6b01538. [DOI] [PubMed] [Google Scholar]
- 84.Choi J.S., Islam M.N., Ali M.Y., Kim E.J., Kim Y.M., Jung H.A. Effects of C-glycosylation on anti-diabetic, anti-Alzheimer’s disease and anti-inflammatory potential of apigenin. Food Chem. Toxicol. 2014;64:27–33. doi: 10.1016/j.fct.2013.11.020. [DOI] [PubMed] [Google Scholar]
- 85.Nikfarjam B.A., Hajiali F., Adineh M., Nassiri-Asl M. Anti-inflammatory effects of quercetin and vitexin on activated human peripheral blood neutrophils-The effects of quercetin and vitexin on human neutrophils. J. Pharmacopunct. 2017;20:127–131. doi: 10.3831/KPI.2017.20.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Praveena R., Sadasivam K., Kumaresan R., Deepha V., Sivakumar R. Experimental and DFT studies on the antioxidant activity of a C-glycoside from Rhynchosia capitata. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2013;103:442–452. doi: 10.1016/j.saa.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 87.Li F., Liang D., Yang Z., Wang T., Wang W., Song X., Guo M., Zhou E., Li D., Cao Y. Astragalin suppresses inflammatory responses via down-regulation of NF-κB signaling pathway in lipopolysaccharide-induced mastitis in a murine model. Int. Immunopharmacol. 2013;17:478–482. doi: 10.1016/j.intimp.2013.07.010. [DOI] [PubMed] [Google Scholar]