Abstract
Objective: Stressful events increase in traumatic conditions. Coronavirus is a new and serious challenge and significant public health problem, which can cause different stressors. This study has identified stressful events experienced by Iranian adults during the COVID-19 epidemic.
Method: Data on stressful events during the COVID-19 epidemic were collected online from 418 adults (mean age 37.16 years; 57.4% female and 42.6% male) using quota sampling method. Epidemic Stressful Events Checklist was applied for data collection. Data were analyzed by applying descriptive graphs and tables, the independent sample t-test, the Fisher’s F test, and post hoc Bonferroni test.
Results: The most frequent stressful event was rise in essential goods prices (84.7%); however, its perceived stress was not at the highest level. The highest severity of perceived stress was related to the death of a family member (4.83) due to COVID-19 infection, which was an event with the least occurrence, and the lowest severity of perceived stress was related to medical team performance (2.50). The results showed the severity of perceived stress is higher in women than men (t = 3.42; P value < 0.01) and also in the laboring occupations compared to other occupations (F = 3.18; P value < 0.05).
Conclusion: Traumatic events can lead to more serious concerns, eg., worrying about those we love, concerns about the future of our life, and about what politicians and macro planners will do to protect our lives. Moreover, traumatic events can cause concerns about food, basic needs, and lack of resources to survive.
Key Words: COVID-19 Epidemic, Coronavirus Epidemic, Infection, Stress
Coronavirus infection is a significant public health problem, and its first outbreak started in Wuhan, Hubei, China, but it soon spread around the world (1). As soon as the virus spread, the main news of all the media for days and even months was dedicated to monitoring this serious public health concern. The behavioral and lifestyle changes were obvious, such as shopping habits, consumption patterns, personal and health habits, changes in communication, etc. (2). These changes are the source of psychological pressure. People differ in tolerance and the amount of stress they suffer (3, 4). Stressful life events are with subsequent psychosocial problems (5), psychological somatic disorders, chronic illnesses (6), physical and mental disorders (7), fatalism, and depression (8), recurrence of episodes of major depression (9), and suicide ideation (10). These events also affect self-esteem, identity, and physical well-being (11).
Trauma, abuse, and other stressful events have been studied extensively (12). We have ample knowledge of correlation of stressors and disease risk (13).
However, our current understanding of the incubation period for COVID-19 is limited (14). Epidemics are usually followed by fear. The Scarlet Plague had already allowed modern readers to reflect on the worldwide fear of pandemics, a fear that remains very much alive (15). The anxiety of social/physical distancing that results in lack of contact with family or friends, phobia of going out, the compulsive need to hoard food and essentials or medical supplies, and stigma toward people with symptoms of coronavirus infection are the possible experiences of people during a pandemic (16). Identifying the emotional and stress problems of individuals is an important part of the basis for psychological intervention (17). Thus, opportune interventions should not be delayed (12, 18).
Documenting these stressful experiences leads to a reference that can be used to plan more effective interventions, in particular, to provide policymakers and emergency responders with information about public perception and behavior in the aftermath of biological disasters, such as a deadly epidemic.
Considering the lack of current knowledge about the sources of stressful events during the COVID-19 pandemic and the severity of perceived stress, this study was designed to identify the sources of stressful events and the severity of perceived stress among adults during the outbreak of COVID-19 in Iran.
Materials and Methods
Study Design and Participants
This cross sectional study was conducted in the peak of the COVID-19 epidemic in the first 2 months of the virus outbreak in Iran from March 4 to May 21, 2020. A total of 600 people were selected as a research sample using a quota sampling method. With a 67% response rate, valid data of 418 participants were obtained for final analysis. In selecting the quotas, an attempt was made to select individuals from all age groups. The final sample consisted of 240 (57.4%) women (mean age 35.65, SD 9.33) and 178(42.6%) men (mean age 39.21 SD 9.91). Inclusion criteria were as follow: age older than 20 years and accessing online devices directly. The exclusion criteria were having a severe physical illness and non-Iranian ethnicity. The reason for the set exclusion criteria was that these factors could be the source of much stress, which could lead to distorted results.
Tools and Measures
Demographic information included gender, age, education, job, and marital status, which were measured by a demographic form.
Epidemic Stressful Events Checklist: New events should be measured by an appropriate checklist, unlike traditional checklists to assess life events (13). The list of stressful events in the COVID-19 pandemic was obtained by the emphasis on 4 features of stressful events: adaptation, threat or harm, demands exceed resources, and Interruption of goals (12). The initial checklist was created by literature review, including events related to the prevalence of previous infectious diseases and psychological stress theory. Then, an in-depth interview with some adults was performed to obtain detailed narrative information about life events that were experienced since the COVID-19 outbreak. The initial checklist with 40 stressful events was reviewed by experts in the online focus group session and reduced to 28 items. After the initial response analysis on the 40 online samples, the number of items was reduced to 26. The content validity ratio for each item ranged from 0.83 to 0.99. The administration of the draft checklist on 200 online samples showed 5 macro stressors: (1) lifestyle changes, (2) finance and necessities of life events, (3) macro-level events, (4) family events, (5) illness or death events. The reliability coefficient of the whole checklist is 0.73. Each item on this checklist receives 2 responses. In the first response, participants determine if they have experienced the stressor; if so, they should determine how much stress has been perceived under that event. Perceived stress varies from 1 to 5 for each event, with score 1 indicating the least stress and 5 the most severely perceived stress.
Procedure: The data of this research were gathered in the survey project that studied stressful events and also psychiatric symptomatology in adults during COVID-19 epidemic by DSM-5 Self-Rated Level 1 Cross-Cutting Symptom Measure. The data were obtained from participants using an online administration, and research data were collected between March to May 2020.
Data Analysis: The IBM SPSS software was used for data analysis. The independent sample t test was performed to compare the sexual and marital groups. The Fisher’s F test by analysis of variance was performed to compare educational and job categories. Bonferroni post hoc test was used to compare the paired group.
Results
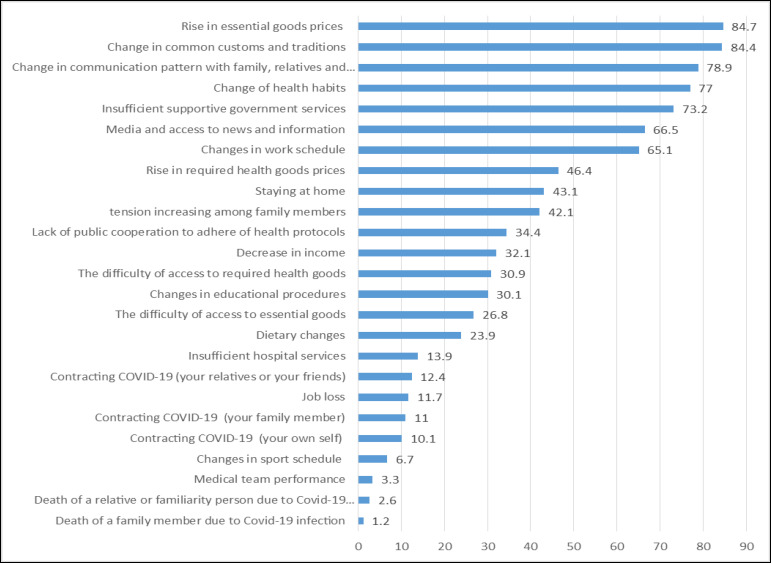
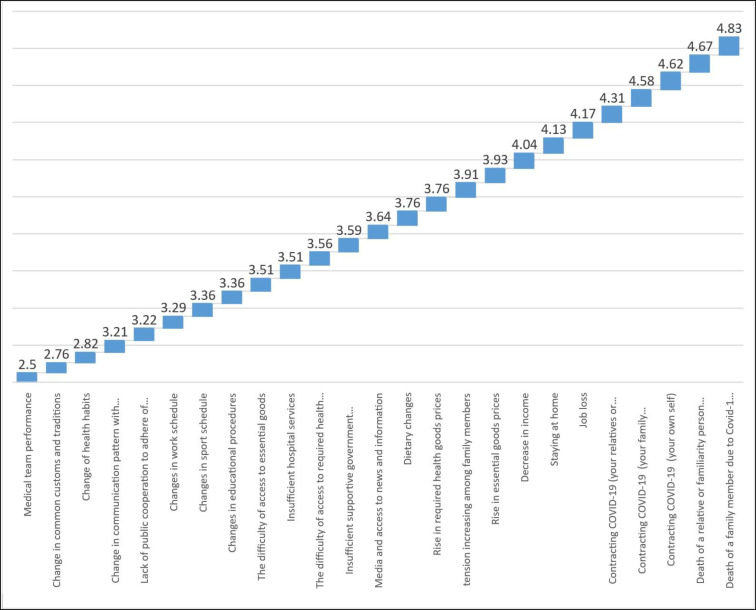
Table 1 represents the demographic information of the sample group. Table 2 shows which of the stressors were experienced by participants during the COVID-19 epidemic and also how much psychological stress was perceived under each stressor. Table 2 and Figure 1 demonstrate the most frequent stressful event in the COVID-19 epidemic is “the rise in prices of essential goods” (84.7% of participants have experienced this source of stress) and the least frequent stress was “death of a family member due to COVID-19 infection” (1.2% of participants have experienced this stressor). Also, the results showed (Table 2 and Figure 2) the stressor “death of a family member” is the most severe stressful event (Mean: 4.83 SD: 0.41) for those people who experienced it. Moreover, the least severe stressful event was related to “medical team performance” (Mean: 2.50; SD: 0.52). More information for the source of stressful events and also their perceived psychological stress is provided in Table 2 and Figures 1 and 2. Table 3 examines the role of demographic variables on perceived stress, and the results showed perceived stress was higher in women than in men (T416 = 3.419; P value = 0.001). Job occupations are difference in the perceived stress (F3, 414= 3.177; P value = 0.024). The post hoc test results show this difference is related to laboring jobs; they have higher levels of perceived stress than other job occupations. The results were not significant based on marital status and education.
Table 1.
Distribution of Demographic Characteristics in the Participants of the study
| Demographic Variables | F (%) | Mean(SD) | |
|---|---|---|---|
| Age | 37.16(9.73) | ||
| Sex | Female | 240(57.4) | |
| Male | 178(42.6) | ||
| Married status | Single | 172(41.1) | |
| Married | 246(58.9) | ||
| Educations | Diploma or below | 22(5.3) | |
| Associated degree | 40(9.6) | ||
| Bachelor | 168(40.2) | ||
| Masters or Higher | 188(45.0) | ||
| Jobs | Housewife/unemployed | 68(16.3) | |
| Laborer | 62(14.8) | ||
| employee | 172(41.1) | ||
| tradesman | 116(27.8) | ||
| Total | 418(100) | ||
Table 2.
Descriptive Statistic for Stressful Events in COVID-19 Epidemic among Participants of the Study
| Epidemic Stressful Events | Experienced stress |
perceived
stress |
|
|---|---|---|---|
| F (%) | Mean (SD) | ||
|
Finance and
necessities of life events |
The difficulty of access to essential goods | 112(26.8) | 3.51(0.78) |
| The difficulty of access to required health goods | 129(30.9) | 3.56(0.64) | |
| Rise in essential goods prices | 354(84.7) | 3.93(0.72) | |
| Rise in required health goods prices | 194(46.4) | 3.76(0.63) | |
| Decrease in income | 134(32.1) | 4.04(0.64) | |
| Job loss | 49(11.7) | 4.17(0.38) | |
|
Macro level
events |
Insufficient supportive government services | 306(73.2) | 3.59(0.78) |
| Insufficient hospital services | 58(13.9) | 3.51(0.78) | |
| Medical team performance | 14(3.3) | 2.50(0.52) | |
| Lack of public cooperation to adhere to health protocols |
144(34.4) | 3.22(0.65) | |
| Family events | Change in communication pattern with family, relatives, and friends |
330(78.9) | 3.21(0.74) |
| Tension increase among family members | 176(42.1) | 3.91(1.14) | |
| Life style changes | Change in health habits | 322(77.0) | 2.82(0.72) |
| Changes in work schedule | 272(65.1) | 3.29(0.67) | |
| Changes in educational procedures | 126(30.1) | 3.36(0.79) | |
| Dietary changes | 100(23.9) | 3.76 (1.06) | |
| Changes in sport schedule | 28(6.7) | 3.36(0.68) | |
| Media and access to news and information | 278(66.5) | 3.64(0.63) | |
| Staying at home | 180(43.1) | 4.13(0.56) | |
| Change in common customs and traditions | 353(84.4) | 2.76(0.78) | |
| Illness or death | Contracting COVID-19 (your own self) | 42(10.1) | 4.62(0.49) |
| Contracting COVID-19 (your family member) | 46(11.0) | 4.58(0.58) | |
| Contracting COVID-19 (your relatives or your friends) | 52(12.4) | 4.31(0.75) | |
| Death of a family member due to COVID-19 | 5(1.2) | 4.83(0.41) | |
| Death of a relative or familiarity person due to COVID-19 |
11(2.6) | 4.67(0.49) |
Figure 1.
The Sources of Stressful Events during COVID-19 Epidemic
Figure 2.
Severity of Perceived Stress for any Stressful Event during COVID-19 Epidemic
Table 3.
Mean Score for Severity of Stressful Epidemic Events Based on Demographic Variables among Participants
| Demographic Variables | Mean(SD) | t test | F test | |
|---|---|---|---|---|
| Sex | Female | 92.08(9.83) | 3.42** | |
| Male | 88.67(10.40) | |||
| Married status | Single | 90.61(10.34) | 0.026 | |
| Married | 90.64(10.13) | |||
| Educations | Diploma or below | 90.45(10.89) | 0.590 | |
| Associated degree | 91.15(9.32) | |||
| Bachelor | 91.32(10.80) | |||
| Masters or Higher | 89.92(9.81) | |||
| Jobs | Housewife/unemployed | 92.88(8.91) | 3.18* | |
| Laborer | 92.93(10.32) | |||
| employee | 89.58(10.49) | |||
| tradesman | 89.64(10.14) | |||
| Total | 90.63(10.21) | |||
P value < 0.01
P value < 0.05
Discussion
Natural disasters are usually severe and affect millions of people and their mental health. They can disrupt social protection systems, create economic instability, and exacerbate mental disorders (19, 20). According to results of this study, the sources of stressful events can be placed in 3 categories: (1) events that most people experience, (2) events that half or less than half of people experience, and (3) events that only a few people experience. Each of these events, regardless of their frequency of occurrence, leads to different levels of psychological pressure. For example, although the death of a family member was the least common source of stress (Graph 1), it was the most stressful event (Graph 2). Even under normal situations, death of loved ones is the most stressful event and there is more guilt and fear in the event of an outbreak (21). The COVID-19 epidemic is even more critical because it does not give people the chance for a usual mourning process. Over the years, humans have learned mechanisms to deal with grief, like mass mourning (22); however, during the COVID-19 outbreak there is no opportunity for a mass mourning. Modern communication tools still cannot provide an opportunity for virtual mourning (23). On the other hand, the psychological pressure increases when the patient has been in intensive care (24, 25). The results of a study by Alfheim et al showed more than half of the caregivers who had patients in the ICU, reported high rates of PTS symptoms (26).
Although the deaths of a loved one have the greatest psychological pressure, rise in essential goods prices were the most frequent source of stress. Economic insecurity is one of the determinants of mental health and is highly relevant to the labor market (27). These problems increase when some jobs are lost or incomes are greatly reduced (28). Also, those with laboring jobs experience higher levels of stress than others. People with low economic level are more affected by neutral events (29). Job loss means loss of income, and loss of income means lack of access to essential goods for life, and problems with rent payment, installments, etc. The effects of natural disasters can never be determined by nature alone, and they are also related to economic, cultural, and social issues. Natural disasters usually lead to social problems and difficulty in accessing essential goods (30). Rapid economic changes, decrease in incomes, job loss, and rise in prices of goods, raise peoples’ expectations of government support. If that support is not enough or does not exist at all, it becomes a source of stress (31, 32). People expect to be supported while in quarantine. Quarantine is an effective method to prevent the spread of the virus, but there is always debate, and many people are skeptical about it. People worry that social or political goals are preferred to their individual rights. During the plague and cholera outbreak, the fear of quarantine led to powerless social groups and some minorities flee the affected areas and this led to a spread of those deadly diseases (33). This can be due to a lack of trust as a result of social capital reduction (34).
Lack of customs, celebrations, and traditions due to quarantine leads to a change in the pattern of communication with family and relatives. While individuals are exposed to different sources of stress, staying home and spending too much time with each other is another stressful source. When people change their daily routine, they have more time to spend together, while they cannot go out to have fun, travel, or see relatives, and this amount of proximity may also lead to domestic violence (35, 36). Staying home, having enough free time, curiosity for virus epidemic monitoring, and being vigilant about health advices encourage people to use the media more while the media and negative news are the sources of increased stress (37, 38). This even includes media used to facilitate online learning and virtual classes for students or parents of school children because of challenges such as access to appropriate environment (39) and difficulty to access high quality of internet network (40).
In addition to these results, another interesting finding was related to the performance of the medical team. Only 3.3% of participants had assessed their performance as stressful. Nonstop efforts, adherence to commitments, and empathy with the patients and caregivers are the factors that lead to trust and also stress reduction among the public population. There are 2 experiences with the spread of previous infectious diseases: During the plague, the medical team provided fewer services because of the fear of spreading the virus; there was no certain treatment at the time, and the mortality rate was high. However, during the SARS epidemic, the result was similar to the current study; the health care team became popular heroes, even though SARS was a deadly and unknown biological enemy (15).
The results also showed the perceived stress rate was higher in women than in men. The ability to cope with stressful events depends on individual characteristics and environmental factors. Negative life events increase psychological problems and are an indicator of increase in daily fears and stress (41). Women, because of their evolutionary roles and their biological and physiological differences with men, seem more responsible and supportive of their family, children, and the elderly; thus, long-term stressful events that threaten their family have a greater impact on them (11, 30). Women are more likely to be victims in disasters events than men (20).
Limitation
The use of online tools to collect data led to this finding that most of the participants were highly educated who had easier access to online communication. The problems caused by online implementation have been minimized by getting help from children to reach out to parents who do not have such facilities. Another limitation of this study was that some groups such as the medical team and severely ill patients were not studied as a comparable group. This limitation reduces the generalizability of the survey results. Another limitation of this research was the use of a non-probabilistic sampling method instead of probabilistic sampling. The authors tried to minimize the effect of this limitation by selecting participants by age group quotas.
Conclusion
Natural disasters, especially when they are an epidemic event, lead to appearance of other sources of stress. The greatest human suffering is always the loss of loved one; on the other hand, the greatest pressure that society puts on people is related to basic needs. The 2 most vulnerable groups are still women and people with low-income. These results remind us we need more long-term preventive and protective plans. There may be a need to think beyond the health interventions, such as thrive for a secure economy, public support, and protectionist policies, to reduce some of the sufferings in such stressful times.
Acknowledgment
We thank all the people who participated in this study. This study was implemented without funding, so we thank all the project partners who patiently collaborated in collecting data and editing information.
Conflict of Interest
The authors declare they have no competing interests.
References
- 1.Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395(10225):689–97. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chauhan V, Shah MH. An Empirical Analysis into Sentiments, Media Consumption Habits, and Consumer Behaviour during the Coronavirus (COVID-19) Outbreak. Purakala with ISSN 0971-2143 is an UGC CARE Journal. 2020;31(20):353–78. [Google Scholar]
- 3.Zarghami M. Psychiatric aspects of Coronavirus (2019-nCoV) infection. Iran J Psychiatry Behav Sci. 2020;14(1):e102957. [Google Scholar]
- 4.Karami A. Investigating the psychological effects of Bam earthquake survivors . International Journal of Behavioral Sciences, 2007 Nov 1;1(1):27–32. [Google Scholar]
- 5.Suedfeld P. Extreme and unusual environments: challenges and Responses. The Oxford handbook of environmental and conservation psychology. Oct 18;:2012–71. [Google Scholar]
- 6.Hassanzadeh A, Heidari Z, Feizi A, Hassanzadeh Keshteli A, Roohafza H, Afshar H, et al. Association of Stressful Life Events with Psychological Problems: A Large-Scale Community-Based Study Using Grouped Outcomes Latent Factor Regression with Latent Predictors. Comput Math Methods Med. 2017;2017:3457103. doi: 10.1155/2017/3457103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McFarlane AC. The effects of stressful life events and disasters: research and theoretical issues. Aust N Z J Psychiatry. 1985;19(4):409–21. doi: 10.1080/00048678509158849. [DOI] [PubMed] [Google Scholar]
- 8.Zuo B, Zhang X, Wen FF, Zhao Y. The influence of stressful life events on depression among Chinese university students: Multiple mediating roles of fatalism and core self-evaluations. J Affect Disord. 2020;260:84–90. doi: 10.1016/j.jad.2019.08.083. [DOI] [PubMed] [Google Scholar]
- 9.Kessler RC. The effects of stressful life events on depression. Annu Rev Psychol. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- 10.Brailovskaia J, Teismann T, Margraf J. Positive Mental Health, Stressful Life Events, and Suicide Ideation. Crisis. 2020:1–6. doi: 10.1027/0227-5910/a000652. [DOI] [PubMed] [Google Scholar]
- 11.Cohen S, Murphy MLM, Prather AA. Ten Surprising Facts About Stressful Life Events and Disease Risk. Annu Rev Psychol. 2019;70:577–97. doi: 10.1146/annurev-psych-010418-102857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tosevski DL, Milovancevic MP. Stressful life events and physical health. Curr Opin Psychiatry. 2006;19(2):184–9. doi: 10.1097/01.yco.0000214346.44625.57. [DOI] [PubMed] [Google Scholar]
- 13.Dohrenwend BP. Inventorying stressful life events as risk factors for psychopathology: Toward resolution of the problem of intracategory variability. Psychol Bull. 2006;132(3):477–95. doi: 10.1037/0033-2909.132.3.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, et al. The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application. Ann Intern Med. 2020;172(9):577–82. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Riva MA, Benedetti M, Cesana G. Pandemic fear and literature: observations from Jack London's The Scarlet Plague. Emerg Infect Dis. 2014;20(10):1753–7. doi: 10.3201/eid2010.130278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Banerjee D. ‘Age and ageism in COVID-19’: Elderly mental health-care vulnerabilities and needs. Asian J Psychiatr. 2020;51:102154. doi: 10.1016/j.ajp.2020.102154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang J, Wu W, Zhao X, Zhang W. Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: a model of West China Hospital. Precision Clinical Medicine. 2020 Mar 25;3(1):3–8. doi: 10.1093/pcmedi/pbaa006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akbar B, Yadollah E, Sam-E Aram E, Forouzan S, Mostafa E. An investigation about the living conditions of Bam earthquake survivals. Social Welfare Quarterly. 2004;4(13):113–32. [Google Scholar]
- 19.Bolhari J, Chime N. Mental health intervention in Bam earthquake crisis: a qualitative study. Tehran University Medical Journal TUMS Publications. 2008;65(13):7–13. [Google Scholar]
- 20.Shafique Sajid M. Unearthing the most vulnerable: Psychological impact of natural disasters. Eur J Psychiatry. 2007;21(3):230–1. [Google Scholar]
- 21.Banerjee D. How COVID-19 is overwhelming our mental health. Nature India. 2020;2020 [Google Scholar]
- 22.Cozza SJ, Hefner KR. The Politics of Mourning: Death and Honor in Arlington National Cemetery. Psychiatry, 2019 May;82(2):1790182. [Google Scholar]
- 23.Klastrup L. Death and Communal Mass-Mourning: Vin Diesel and the Remembrance of Paul Walker. Social Media+ Society. 2018;4(1):2056305117751383. [Google Scholar]
- 24.Probst DR, Gustin JL, Goodman LF, Lorenz A, Wells-Di Gregorio SM. ICU versus Non-ICU Hospital Death: Family Member Complicated Grief, Posttraumatic Stress, and Depressive Symptoms. J Palliat Med. 2016;19(4):387–93. doi: 10.1089/jpm.2015.0120. [DOI] [PubMed] [Google Scholar]
- 25.Petrinec AB, Daly BJ. Post-Traumatic Stress Symptoms in Post-ICU Family Members: Review and Methodological Challenges. West J Nurs Res. 2016;38(1):57–78. doi: 10.1177/0193945914544176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alfheim HB, Hofsø K, Småstuen MC, Tøien K, Rosseland LA, Rustøen T. Post-traumatic stress symptoms in family caregivers of intensive care unit patients: A longitudinal study. Intensive Crit Care Nurs. 2019;50:5–10. doi: 10.1016/j.iccn.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 27.Kopasker D, Montagna C, Bender KA. Economic insecurity: A socioeconomic determinant of mental health. SSM Popul Health. 2018;6:184–94. doi: 10.1016/j.ssmph.2018.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Watson B, Osberg L. Job insecurity and mental health in Canada. Applied Economics. 2018;50(38):4137–52. [Google Scholar]
- 29.Chan EYY, Man AYT, Lam HCY. Scientific evidence on natural disasters and health emergency and disaster risk management in Asian rural-based area. Br Med Bull. 2019;129(1):91–105. doi: 10.1093/bmb/ldz002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Neumayer E, Plümper T. The gendered nature of natural disasters: The impact of catastrophic events on the gender gap in life expectancy, 1981–2002. Ann Assoc Am Geogr. 2007;97(3):551–66. [Google Scholar]
- 31.Cohen RE. Mental health services for victims of disasters. World Psychiatry. 2002;1(3):149–52. [PMC free article] [PubMed] [Google Scholar]
- 32.Schofield DJ, Shrestha RN, Percival R, Passey ME, Callander EJ, Kelly SJ. The personal and national costs of mental health conditions: impacts on income, taxes, government support payments due to lost labour force participation. BMC Psychiatry. 2011;11:72. doi: 10.1186/1471-244X-11-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tognotti E. Lessons from the history of quarantine, from plague to influenza A. Emerging infectious diseases. 2013 Feb;19(2):254. doi: 10.3201/eid1902.120312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mohammadi MR, Hooshyari Z, Ezanloo B, Shakiba A, Mostafavi SA, Salmanian M, Ahmadi A, Alavi SS, Khaleghi A, Zarafshan H. Application of Different Techniques of Factor Analysis to Develop Neighborhood Social Capital Rating Scale. Social Indicator Research. 2020 [Google Scholar]
- 35.Hatchimonji JS, Swendiman RA, Seamon MJ, Nance ML. Trauma does not Quarantine: Violence during the COVID-19 Pandemic. Ann Surg. 2020;272(2):e53–e54. doi: 10.1097/SLA.0000000000003996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mazza M, Marano G, Lai C, Janiri L, Sani G. Danger in danger: Interpersonal violence during COVID-19 quarantine. Psychiatry research. 2020 Apr 30;:113046. doi: 10.1016/j.psychres.2020.113046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hampton KN, Lu W, Shin I. Digital media and stress: the cost of caring 2.0. Information. Communication & Society. 2016 Sep 1;19(9):1267–86. [Google Scholar]
- 38.Marin MF, Morin-Major JK, Schramek TE, Beaupré A, Perna A, Juster RP, Lupien SJ. There is no news like bad news: women are more remembering and stress reactive after reading real negative news than men. PloS one. 2012 Oct 10;7(10):e47189. doi: 10.1371/journal.pone.0047189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gillett-Swan J. The challenges of online learning: Supporting and engaging the isolated learner. Journal of Learning Design. 2017;10(1):20–30. [Google Scholar]
- 40.Gilbert B. Online learning revealing the benefits and challenges. 2015. [Google Scholar]
- 41.Marum G, Clench-Aas J, Nes RB, Raanaas RK. The relationship between negative life events, psychological distress and life satisfaction: a population-based study. Qual Life Res. 2014;23(2):601–11. doi: 10.1007/s11136-013-0512-8. [DOI] [PubMed] [Google Scholar]