Abstract
Background
The impact of COVID-19 on pre-hospital and hospital services and hence on the prevalence and outcomes of out-of-hospital cardiac arrests (OHCA) remain unclear. The review aimed to evaluate the influence of the COVID-19 pandemic on the incidence, process, and outcomes of OHCA.
Methods
A systematic review of PubMed, EMBASE, and pre-print websites was performed. Studies reporting comparative data on OHCA within the same jurisdiction, before and during the COVID-19 pandemic were included. Study quality was assessed based on the Newcastle-Ottawa Scale.
Results
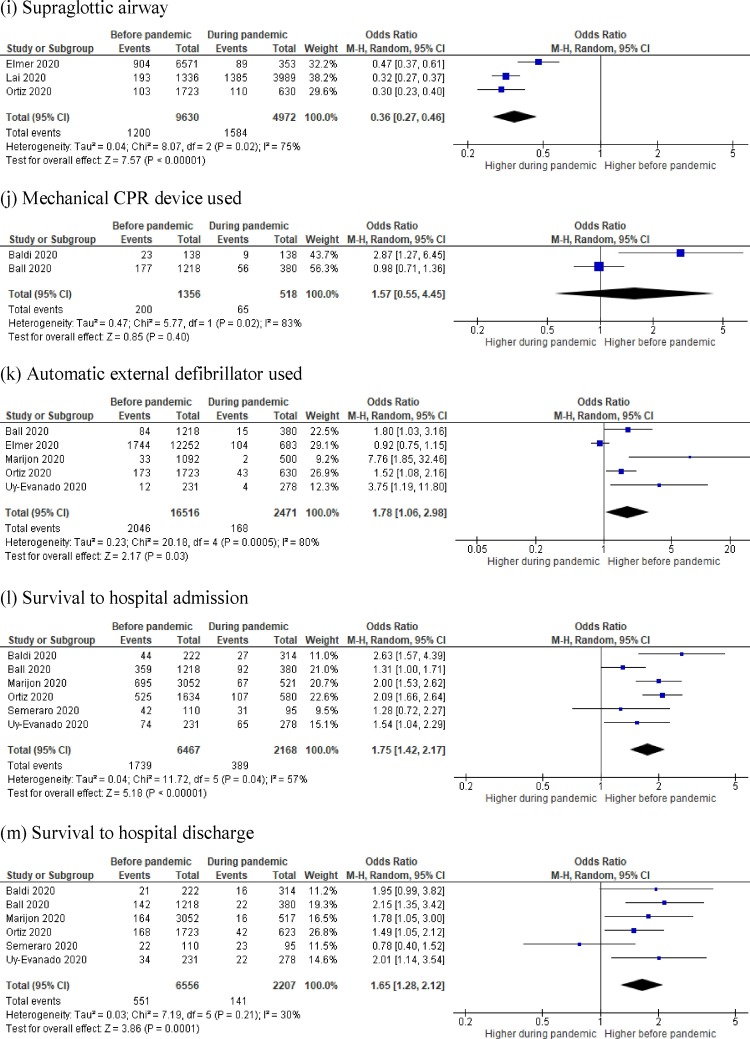
Ten studies reporting data from 35,379 OHCA events were included. There was a 120% increase in OHCA events since the pandemic. Time from OHCA to ambulance arrival was longer during the pandemic (p = 0.036). While mortality (OR = 0.67, 95%-CI 0.49−0.91) and supraglottic airway use (OR = 0.36, 95%-CI 0.27−0.46) was higher during the pandemic, automated external defibrillator use (OR = 1.78 95%-CI 1.06–2.98), return of spontaneous circulation (OR = 1.63, 95%CI 1.18-2.26) and intubation (OR = 1.87, 95%-CI 1.12-–3.13) was more common before the pandemic. More patients survived to hospital admission (OR = 1.75, 95%-CI 1.42–2.17) and discharge (OR = 1.65, 95%-CI 1.28–2.12) before the pandemic. Bystander CPR (OR = 1.18, 95%-CI 0.95-1.46), unwitnessed OHCA (OR = 0.84, 95%-CI 0.66–1.07), paramedic-resuscitation attempts (OR = 1.19 95%-CI 1.00–1.42) and mechanical CPR device use (OR = 1.57 95%-CI 0.55–4.55) did not defer significantly.
Conclusions
The incidence and mortality following OHCA was higher during the COVID-19 pandemic. There were significant variations in resuscitation practices during the pandemic. Research to define optimal processes of pre-hospital care during a pandemic is urgently required.
Review registration
PROSPERO (CRD42020203371).
Keywords: COVID-19, SARS-CoV-2, Out of hospital, Cardiac arrest, OHCA
Introduction
The novel coronavirus disease 2019 (COVID-19) pandemic, caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) has been associated with more than 39 million cases and 1 million deaths worldwide as of October 16th 2020.1 Health systems are under significant sustained stress with many parts of world experiencing second and subsequent waves of infection. The understanding of how the pandemic affects overall population health and access to health care; the nature and extent of disruptions it causes to pre-hospital and in hospital health care delivery is still evolving.
For example, an increase in out-of-hospital cardiac arrest (OHCA) incidence has been reported since the very early phase of the COVID-19 epidemic.2 A recent population-based cross-sectional study reported that out-of-hospital cardiac arrests had increased 3-fold during the 2020 COVID-19 period when compared with during the comparison period in 2019.3 Patients with OHCA during 2020 were older, more likely to have comorbidities and substantially less likely to have return and sustained return of spontaneous circulation.3
The chain of survival refers to a series of actions such as early access, early cardiopulmonary resuscitation (CPR), early defibrillation, early advanced life support and early post resuscitative care. These actions should be optimally executed to reduce the mortality associated with OHCA. Like any chain, the chain of survival is only as strong as its weakest link.4 A pandemic can disrupt this chain of survival in multiple ways and influence patient outcomes.
The study hypothesis was that the incidence of OHCA and the associated mortality was higher during the COVID-19 pandemic period when compared to an earlier period. In this systematic review and meta-analysis, the authors aimed to determine the influence of the COVID-19 pandemic on the incidence, processes of care and mortality among OHCA patients.
Methods
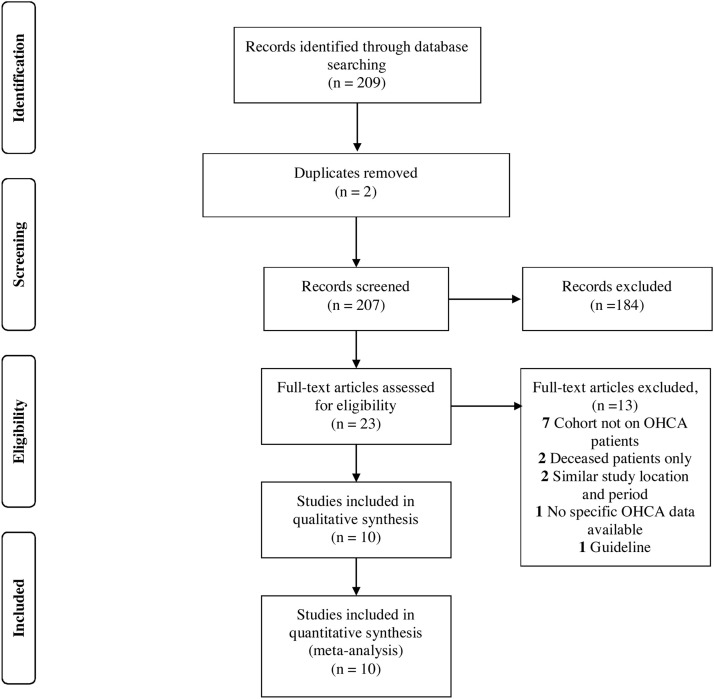
This systematic review and meta-analysis were reported using the PRISMA framework5 and has been registered on PROSPERO (CRD42020203371). Fig. 1 illustrates the study flow diagram.
Fig. 1.
PRISMA 2009 flow diagram.
Eligibility criteria
Studies reporting comparative OHCA data before and during the COVID-19 pandemic within the same location were included. Studies were excluded if (a) results of original research were not presented; (b) the study only reported on deceased patients.
Search strategy, information sources and study selection
Two authors independently searched the publicly available COVID-19 living systematic review.6 This living systematic review provides a dynamic update of research papers related to COVID-19 that are indexed by PubMed, EMBASE, MedRxiv and BioRxiv, and has been validated in previously published COVID-19-related research.7 Data was extracted between 01/01/2020 to 16/10/2020 using the search terms “arrest”, “OHCA”, “OOHCA” within the title and the abstract columns of the systematic review list. These terms were combined with the Boolean operator “OR”. Pre-print and non-English language articles were considered. Conflicts in data extraction were resolved by discussion between the reviewers or adjudication by a third author.
Quality assessment and risk of bias in individual studies
The Newcastle-Ottawa Scale (NOS) is a quality assessment tool used to evaluate non-randomized studies based on an eight-item score divided into three domains.8 These domains assess selection, comparability, and ascertainment of the outcome of interest. NOS was used by the two reviewers to independently evaluate the quality of included studies and assess for risk of bias. The same set of decision rules was used by each reviewer to score the studies. Any discrepancies from the NOS were reviewed and resolved by a third author.
Data analysis and data collection process
To evaluate the effect of the COVID-19 pandemic, the studies with direct comparison to an earlier time frame (termed “before pandemic”) were selected. This enabled a direct comparison between the two-time frames to help understand any differences in incidences.
Statistical analyses were performed using the Review Manager 5.4 (Cochrane Collaboration) and Stata/MP 15.1 (Statacorp). Numerical data was summarized using mean and standard deviation and categorical data using proportion and percentage. To enable an analysis of results between studies, median values were converted to means, derived using an estimation formula.9 Between-group differences were compared using Fischer’s exact test. An analysis of non-parametric values was conducted using the Kruskal Wallace test. A p-value <0.05 was considered statistically significant. The Mentel-Haenszel random-effects model demonstrate better properties in the presence of heterogeneity accounting for both within-study and between-study variances which was considered for the pooled odds ratio (OR). Results were presented in Forest plots. Heterogeneity was tested by using the χ² test on Cochran’s Q statistic, which was calculated by means of H and I² indices. The I² index estimates the percentage of total variation across studies based on true between-study variances rather than on chance. Conventionally, I2 values of 0–25% indicate low heterogeneity, 26–75% indicate moderate heterogeneity, and 76–100% indicate substantial heterogeneity.
Corresponding authors were contacted for additional information, where data were incomplete. Study period and location were analyzed as part of the data collection process, and studies were excluded if a significant overlap in patient cohorts were identified.
Study outcomes
The primary outcome was to evaluate the incidence and mortality rate of OHCA during the COVID-19 pandemic.
Additional secondary outcomes include analyzing the characteristics and outcomes of OHCA during the COVID-19 pandemic. Time from OHCA notification to ambulance arrival was also analyzed. The frequency of COVID-19 patients among OHCA was also assessed.
Results
A total of 209 studies were obtained from the living systematic review, with 23 full-text articles assessed for eligibility. Ten studies across five countries (Australia, France, Italy, Spain and USA) were included in the qualitative and statistical analysis.3, 10, 11, 12, 13, 14, 15, 16, 17, 18 Six studies were fair10, 12, 13, 15, 16, 17 and four studies were of good quality based on NOS 3, 11, 14, 18 (Supplementary Table 1). Six studies compared the COVID-19 pandemic with the same period in 2019.3, 10, 13, 15 , 17, 18 One study compared OHCA during the COVID-19 pandemic against OHCA earlier in the year.16 While one study compared data collected during COVID-19 pandemic with data from 2011−2019,13 the remaining studies compared COVID-19 data against the time periods of 2016–2019,12 2017-201814 and 2017−2019.11 The mean age reported among nine studies was 70.8 years during the COVID-19 pandemic, and 65.6 years before the pandemic. Time from call to ambulance arrival was significantly higher during the pandemic (p = 0.036). The incidence and outcomes of OHCA of each study is outlined in Table 1 .
Table 1.
Summary of studies.
| Lai 2020 | Baldi 2020 | Ball 2020 | Elmer 2020 | Marijon 2020 | Ortiz 2020 | Paoli 2020 | Sayre 2020 | Semeraro 2020 | Uy-Evanado 2020 | Total | p-value | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Location of study |
New York, USA | Lombardy, Italy | Victoria, Australia | Pennsylvania, USA | Paris, France | Spain | Pauda, Italy | Washington, USA | Bologna, Italy | Oregon and California, USA | ||||
| NOS Score | Good | Fair | Good | Fair | Fair | Good | Fair | Fair | Fair | Good | ||||
| Time period | Before pandemic | March 1 to April 25, 2019 | February 21 to April 21, 2019 | March 16 to May 12, 2017−2019 | January 2016 to February 2020 | March 18 to April 28, 2019 | April 1−30 2017, and February 1 to March 31 2018 | March 1 to April 30, 2019 | January 1 to February 25, 2019 | January 1 to June 30, 2019 | March 1 to May 31, 2019 | |||
| During pandemic | March 1 to April 25, 2019 | February 21 to April 20, 2020 | March 16 to May 12, 2020 | March 1 to May 25, 2020 | March 16 to April 26, 2020 | March 11 to April 30, 2020 | March 1 to April 30, 2020 | February 26 to April 15, 2020 | January 1 to June 30, 2020 | March 1 to May 31, 2020 | ||||
| Sample Size | Before pandemic | 2302 | 321 | 2599 | 12252 | 3052^ | 1723# | 206 | 540 | 563 | 231 | 23789 | NA | |
| During pandemic | 6709 | 490 | 935 | 683 | 521 | 683# | 200 | 527 | 624 | 278 | 11590 | NA | ||
| Difference in OHCA incidence | 2019 | 2302 | 321 | NR* | NR* | 395 | NR* | 206 | NR* | 563 | 231 | 4018 | NA | |
| 2020 | 6709 | 490 | NR* | NR* | 521 | NR* | 200 | NR* | 624 | 278 | 8822 | |||
| Percentage change | 191.4% | 52.6% | NR* | NR* | 31.9% | NR* | −3% | NR* | 10.8% | 20.3% | 119.6% | |||
| Age (Years), Mean (SD) | Before pandemic | 68 (19) | 77 (14) | 66 (19) | 63 (19) | 69 (18) | 66 (17) | 77 (14) | NR | 83 (13) | 69 (17) | 65.6 | NA | |
| During pandemic | 72 (18) | 76 (13) | 68 (19) | 64 (19) | 70 (17) | 64 (16) | 79 (17) | NR | 83 (13) | 65 (18) | 70.8 | NA | ||
| Male patients, N (%) | Before pandemic | 752/1336 (56.3%) | 188/321 (58.6%) | 845/1218# (69.4%) | 7700/12252 (62.8%) | 1826/3047 (59.9%) | 1210/1723# (70.2%) | 98/179 (54.7%) | NR | 284/563 (50.4%) | 137/231 (59.3%) | 13040/20870 (62.5%) | <0.001 | |
| During pandemic | 2183/3989 (54.7%) | 321/490 (65.5%) | 250/380# (65.8%) | 430/683 (63.0%) | 334/519 (64.4%) | 433/623# (69.5%) | 89/175 (50.9%) | NR | 318/624 (51.0%) | 174/278 (62.6%) | 4532/7761 (58.4%) | |||
| Mortality, N (%) | Before pandemic | 1922/2302 (83.5%) | 156/321 (48.6%) | 827/1218# (67.9%) | 6302/12252 (51.4%) | 2357/3052 (77.2%) | 1109/1634# (67.9%) | 200/206 (97.1%) | 292/540 (54.1%) | 509/563 (90.4%) | 157/231 (68.0%) | 13831/22319 (62.0%) | <0.001 | |
| During pandemic | 6244/6709 (93.1%) | 253/490 (51.6%) | 285/380# (75.0%) | 329/683 (48.2%) | 454/521 (87.1%) | 473/580# (81.6%) | 194/200 (97.0%) | 297/527 (56.4%) | 586/624 (93.9%) | 213/278 (76.6%) | 9328/10992 (84.9%) | |||
| Bystander CPR, N (%) | Before pandemic | 441/1336 (33.0%) | 87/192 (45.3%) | 889/1218# (73.0%) | 4125/12,252 (33.7%) | 1165/1822 (63.9%) | 788/1723# (45.7%) | 15/60 (25.0%) | 227/540 (42.0%) | 29/110# (26.4%) | 142/231 (61.5%) | 7908/19484 (40.6%) | 0.003 | |
| During pandemic | 1359/3989 (34.1%) | 89/257 (34.6%) | 299/380# (78.7%) | 246/683 (36.0%) | 239/500 (47.8%) | 230/623# (36.9%) | 10/55 (18.2%) | 207/527 (39.3%) | 30/95# (31.6%) | 141/278 (50.7%) | 2850/7387 (38.6%) | |||
| Unwitnessed OHCA, N (%) | Before pandemic | 982/1336 (73.5%) | 147/321 (45.8%) | 329/1218# (27.0%) | 8772/12252 (71.6%) | 1021/2908 (35.1%) | 392/1723# (22.8%) | 42/59 (71.1%) | NR | NR | 109/231 (47.2%) | 11794/20048 (58.8%) | <0.001 | |
| During pandemic | 2909/3989 (72.9%) | 261/490 (53.3%) | 179/380# (47.1%) | 466/683 (68.2%) | 206/500 (41.2%) | 130/623# (20.9%) | 39/52 (75.0%) | NR | NR | 138/278 (49.6%) | 4328/6995 (61.9%) | |||
| EMS Resuscitation attempted, N (%) | Before pandemic | 1336/2302 (58.0%) | 222/321 (69.2%) | 1218/2599 (46.9%) | NR | NR | NR | 48/90 (53.3%) | 248/540 (45.9%) | 110/563 (19.5%) | NR | 3182/6415 (49.6%) | <0.001 | |
| During pandemic | 3989/6709 (59.5%) | 324/490 (64.1%) | 380/935 (40.6%) | NR | NR | NR | 45/114 (39.5%) | 230/527 (43.6%) | 95/624 (15.2%) | NR | 5053/9399 (53.8%) | |||
| ROSC, N (%) | Before pandemic | 463/1336 (34.7%) | 44/222 (19.8%) | 416/1218 (34.2%) | 1529/12252 (12.5%) | NR | 525/1723# (30.5%) | 4/206 (1.9%) | NR | 54/563 (9.6%) | 95/231 (41.1%) | 3130/17751 (17.6%) | 0.22 | |
| During pandemic | 727/3989 (18.2%) | 27/314 (8.6%) | 112/380 (29.5%) | 95/683 (13.9%) | NR | 107/623# (17.2%) | 2/200 (1.0%) | NR | 38/624 (6.1%) | 95/278 (34.2%) | 1203/7091 (17.0%) | |||
| Shockable cardiac rhythm/shocked events, N (%) | Before pandemic | 38/345 (11.0%) | 37/222 (16.7%) | 318/1218# (26.1%) | NR | 472/2471 (19.1%) | 386/1723# (22.4%) | NR | NR | 34/563 (6.0%) | 64/231 (27.7%) | 1349/6773 (19.9%) | <0.001 | |
| During pandemic | 45/1254 (3.6%) | 36/314 (11.5%) | 90/380# (23.7%) | NR | 46/500 (9.2%) | 118/623# (18.9%) | NR | NR | 33/624 (5.3%) | 64/278 (23.0%) | 432/3973 (10.9%) | |||
| OHCA at home, N (%) | Before pandemic | NR | 267/321 (83.2%) | 965/1218# (79.2%) | NR | 2336/3042 (76.8%) | 1042/1723# (60.5%) | NR | NR | 82/110# (74.5%) | 145/231 (62.8%) | 4837/6645 (72.8%) | <0.001 | |
| During pandemic | NR | 442/490 (90.2%) | 342/380# (90.0%) | NR | 460/510 (90.2%) | 478/623# (76.7%) | NR | NR | 65/95# (68.4%) | 210/278 (75.5%) | 1997/2376 (84.0%) | |||
| Intubation | Before pandemic | NR | NR | 594/1218# (48.8%) | 2760/6571 (42.0%) | NR | 1224/1723# (71.0%) | NR | NR | NR | NR | 5589/10848 (51.5%) | <0.001 | |
| During pandemic | NR | NR | 171/380# (45.0%) | 127/353 (36.0%) | NR | 320/630# (50.8%) | NR | NR | NR | NR | 2533/5352 (47.3%) | |||
| Supraglottic airway | Before pandemic | NR | NR | NR | 904/6571 (13.8%) | NR | 103/1723# (6.0%) | NR | NR | NR | NR | 1200/9630 (12.5%) | <0.001 | |
| During pandemic | NR | NR | NR | 89/353 (25.2%) | NR | 110/630# (17.5%) | NR | NR | NR | NR | 1584/4972 (31.9%) | |||
| Mechanical CPR | Before pandemic | NR | 23/138 (16.7%) | 177/1218# (14.5%) | NR | NR | NR | NR | NR | NR | NR | 200/1356 (14.7%) | 0.24 | |
| During pandemic | NR | 9/138 (6.5%) | 56/380# (14.7%) | NR | NR | NR | NR | NR | NR | NR | 65/518 (12.5%) | |||
| AED use | Before pandemic | NR | NR | 84/1218# (6.9%) | 1744/12252 (14.2%) | 33/1092 (3.0%) | 173/1723# (10.0%) | NR | NR | NR | 12/231 (5.2%) | 2046/16516 (12.4%) | <0.001 | |
| During pandemic | NR | NR | 15/380# (3.9%) | 104/683 (15.2%) | 2/500 (0.4%) | 43/630# (6.8%) | NR | NR | NR | 4/278 (1.4%) | 168/2471 (6.8%) | |||
| Survival to hospital admission | Before pandemic | NR | 44/222 (19.8%) | 359/1218# (29.5%) | NR | 695/3052 (22.8%) | 525/1634# (32.1%) | NR | NR | 42/110# (38.2%) | 74/231 (32.0%) | 1739/6467 (26.9%) | <0.001 | |
| During pandemic | NR | 27/314 (8.6%) | 92/380# (24.2%) | NR | 67/521 (12.9%) | 107/580# (18.4%) | NR | NR | 31/95# (32.6%) | 65/278 (23.4%) | 389/2168 (17.9%) | |||
| Survival to hospital discharge | Before pandemic | NR | 21/222 (9.5%) | 142/1218# (11.7%) | NR | 164/3052 (5.4%) | 168/1723# (9.8%) | NR | NR | 22/110# (20.0%) | 34/231 (14.7%) | 551/6556 (8.4%) | 0.002 | |
| During pandemic | NR | 16/314 (5.1%) | 22/380# (5.8%) | NR | 16/517 (3.1%) | 42/623# (6.7%) | NR | NR | 23/95# (24.2%) | 22/278 (7.9%) | 141/2207 (6.4%) | |||
| Call to arrival in minutes, Median (IQR) | Before pandemic | 5.1 (2.3−7.2) | 12 (9−15) | 8.5 (6.6−11.4) | NR | 9.4 (7.9−12.6) | 12 (8−19) | 15 (11−19) | NR | 9 (7−13) | 6.4 (1.6−13.7) | NA | 0.036 | |
| During pandemic | 5.9 (2.3−9.6) | 15 (11−20) | 9.8 (8.0−12.8) | NR | 10.4 (8.4−13.8) | 15 (9−23) | 16 (12−22) | NR | 9 (7−12) | 7 (0.7−22.8) | NA | |||
| Etiology of OHCA, N (%) | Medical | Before pandemic | NR | 175/204 (58.8%) | 979/1218# (80.4%) | 11,153/12252 (91.0%) | NR | NR | 287/321 (89.4%) | NR | 99/110# (90.0%) | NR | 12693/14105 (90.0%) | 0.56 |
| During pandemic | NR | 179/197 (90.9%) | 293/380# (77.1%) | 643/683 (94.1%) | NR | NR | 465/490 (94.9%) | NR | 89/95# (93.7%) | NR | 1669/1845 (90.5%) | |||
| Trauma | Before pandemic | 43/2302 (1.9%) | 17/204 (8.3%) | 60/1218# (4.9%) | 1099/12252 (9.0%) | NR | NR | 28/321 (8.7%) | NR | 6/110# (5.5%) | NR | 1253/14105 (8.9%) | 0.031 | |
| During pandemic | 42/6709 (0.6%) | 15/197 (7.6%) | 22/380# (5.8%) | 40/683 (5.9%) | NR | NR | 13/490 (2.7%) | NR | 4/95# (4.2%) | NR | 136/1845 (7.4%) | |||
| Drowning | Before pandemic | NR | 0/204 (0.0%) | NR | NR | NR | NR | 0/321 (0.0%) | NR | 1/110# (0.9%) | NR | 1/635 (0.2%) | 1.00 | |
| During pandemic | NR | 1/197 (0.5%) | NR | NR | NR | NR | 0/490 (0.0%) | NR | 0/95# (0.0%) | NR | 1/782 (0.1%) | |||
| Overdose | Before pandemic | NR | 1/204 (0.5%) | 58/1218# (4.8%) | NR | NR | NR | 1/321 (0.3%) | NR | 4/110# (3.6%) | NR | 64/1853 (3.5%) | 0.58 | |
| During pandemic | NR | 0/197 (0.0%) | 18/380# (4.7%) | NR | NR | NR | 1/490 (0.2%) | NR | 2/95# (2.1%) | NR | 21/1162 (1.8%) | |||
| Asphyxia | Before pandemic | NR | 7/204 (3.4%) | 44/1218# (3.6%) | NR | NR | NR | 5/321 (1.6%) | NR | NR | NR | 56/1743 (3.2%) | 1.00 | |
| During pandemic | NR | 6/197 (3.0%) | 15/380# (3.9%) | NR | NR | NR | 11/490 (2.2%) | NR | NR | NR | 32/1067 (3.0%) | |||
NOS: Newcastle Ottawa Scale; USA: United States of America; SD: Standard deviation; N: Number; CPR: NR: Not reported; Cardiopulmonary resuscitation; OHCA: Out of hospital cardiac arrest; EMS: Emergency medical services; ROSC: Return of spontaneous circulation; AED: Automatic external defibrillator.
* The study did not compare the incidence of OHCA between 2019 and 2020 and was thus excluded from this analysis.
# Out of resuscitations attempted by emergency medical services.
^ Marijon et al looked at two different timeframes and compared the incidence and outcomes of OHCA against data from the pandemic period in 2020.
Table 2 summarizes the comparison of suspected and confirmed COVID-19 patients among the OHCA in 2020. Five studies (n = 2044) reported on the prevalence of COVID-19 infections among OHCA.10, 13, 16 A total of 194 patients were suspected (n = 126, 6.2%) or confirmed COVD-19 patients (n = 68, 3.3%).
Table 2.
Comparison of suspected and confirmed COVID-19 patients among OHCA in 2020.
| 2020 | Suspected COVID-19 cases, N (%) | Confirmed COVID-19 cases, N (%) | |
|---|---|---|---|
| Baldi 2020 | 490 | 106 (21.6%) | 19 (3.9%) |
| Ball 2020 | 380 | NR | 0 (0.0%) |
| Marijon 2020 | 521 | 17 (3.3%) | 25 (4.8%) |
| Sayre 2020 | 527 | 3 (0.6%) | 23 (4.4%) |
| Uy-Evanado 2020 | 126* | NR | 1 (0.8%) |
| Total | 2044 | 126 (6.2%) | 68 (3.3%) |
| 194 (9.5%) | |||
N: Number, NR: Not reported.
* Out of 126 cases in Oregon.
Primary outcome: incidence and mortality rate of OHCA during the COVID-19 pandemic
Six studies made a direct comparison of OHCA incidence between the same time period in 2020 and 2019 and recorded 8822 OHCA events in 2020 during the COVID-19 pandemic in contrast to 4018 OHCA in 2019, representing a 119.6% increase (Table 1).3, 10, 13, 15 , 17, 18
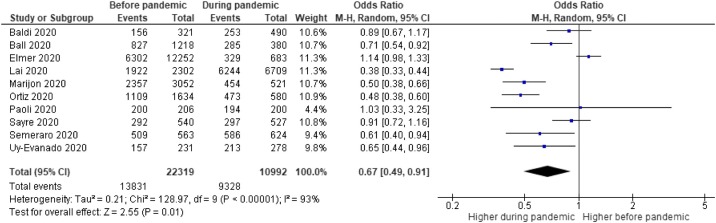
During the pandemic, all ten studies recorded 11,590 OHCA events. Outcomes were known for 10992 patients (94.8%), of which 9328 (84.9%) patients died. In comparison, the before pandemic group recorded 22319 OHCA across various comparison time periods with 13,831 (62.0%) deaths (p < 0.001). The forest plot for mortality of OHCA is illustrated in Fig. 2 (OR = 0.67, 95% CI 0.49−0.91; p = 0.01). Heterogeneity was high (I2 = 93%).
Fig. 2.
Forest plot comparison before COVID-19 pandemic vs. during COVID-19 pandemic for mortality.
M-H: Mantel-Haenszel; CI: Confidence Interval.
Secondary outcome
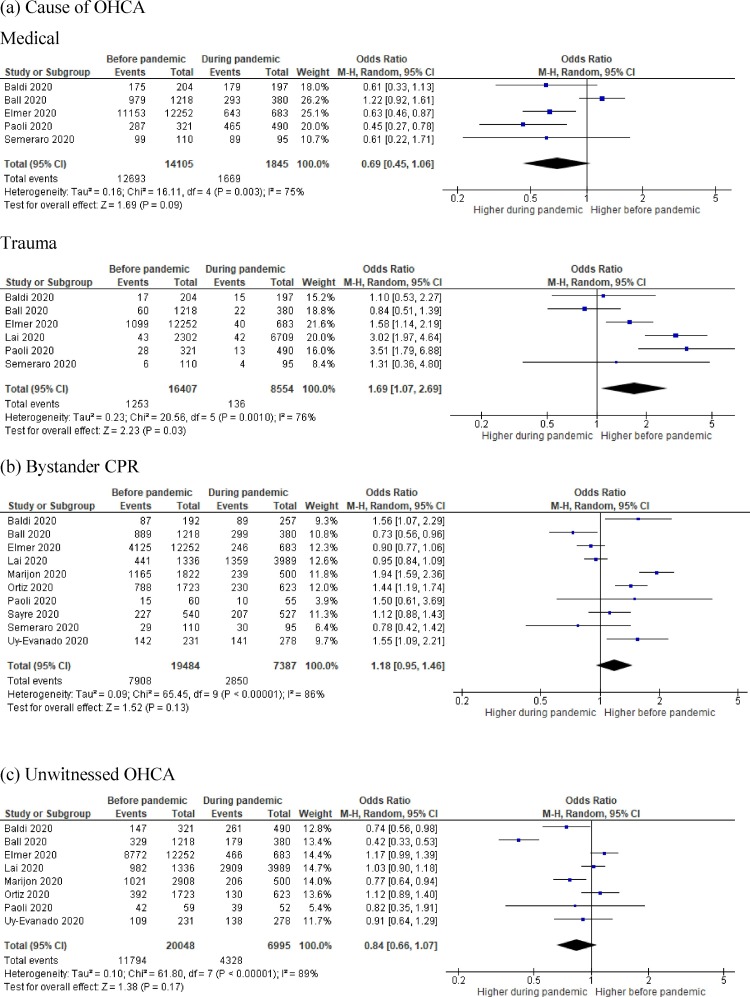
The incidence proportion of OHCA due to a medical cause was similar before and during the pandemic (90.0% (12693/14105) versus 90.5% (1669/1845), p = 0.56; OR = 0.69, 95% CI 0.45-1.06;0.45–1.06; p = 0.09; I2 = 75%).3, 10, 11, 12, 15, 17 However, trauma-related OHCA was more common before the pandemic (8.9% (1253/14105) versus 7.4% (136/1845), p = 0.031; OR = 1.69, 95% CI 1.07–2.69; p = 0.03; I2 = 76%).3, 10, 11, 12, 15, 17 This is illustrated in Fig. 3 a.
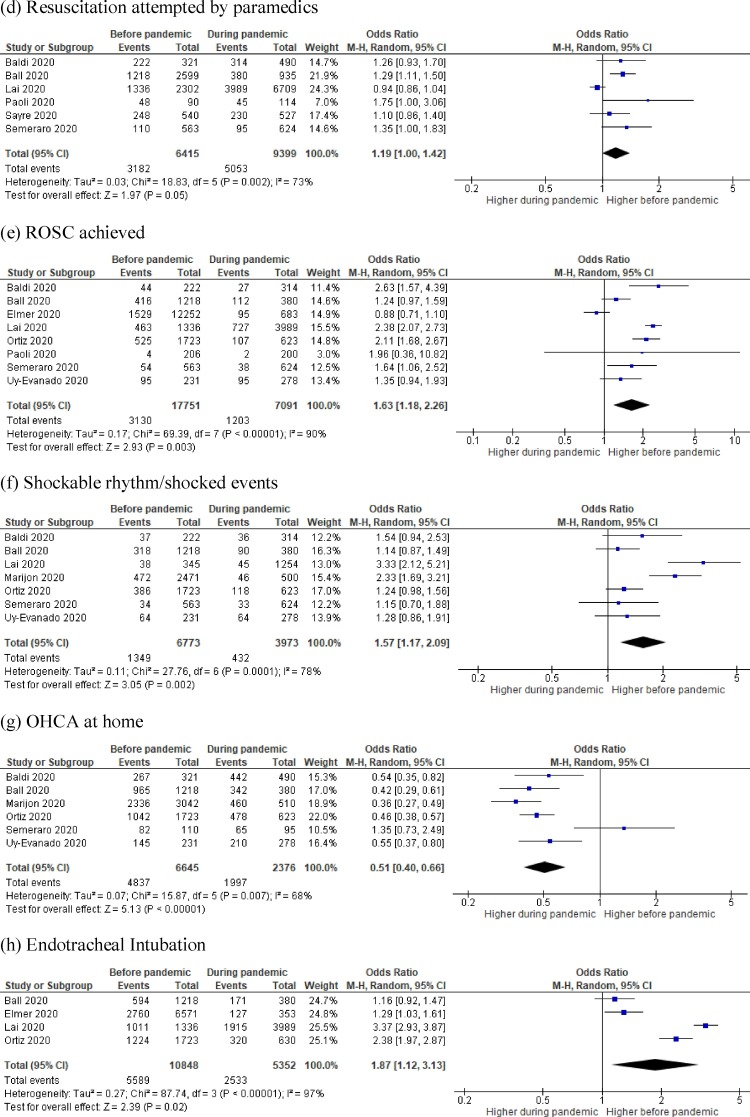
Fig. 3.
Forest plot comparison before COVID-19 pandemic vs. during COVID-19 pandemic for (a) Cause of OHCA, (b) Bystander CPR, (c) Unwitnessed OHCA, (d) Resuscitation attempted by paramedics, (e) ROSC achieved, (f) Shockable rhythm/shocked events, (g) Frequency of OHCA at home, (h) Endotracheal Intubation, (i) Supraglottic airway, (j) Mechanical CPR device used, (k) Automatic external defibrillator used, (l) Survival to hospital admission, and (m) Survival to hospital discharge.
Bystander CPR (Fig. 3b) was reported in all ten studies in a total of 7908/19549 patients (40.5%) before pandemic and 2850/7322 patients (38.9%) during the pandemic (p < 0.001).3, 10, 11, 12, 13, 15, 16, 17, 18 Bystander CPR occurred more frequently before the pandemic but was not statistically significant (OR = 1.08 95% CI 0.86–1.35; p = 0.51; I2 = 88%).
Unwitnessed OHCA (Fig. 3c) was reported in eight studies across 11794/20048 patients (58.8%) before the pandemic and 4328/6995 patients (61.9%) during the pandemic (p < 0.001).3, 10, 11, 12, 13, 14, 15, 18 Unwitnessed OHCA occurred less often before the pandemic, however, was not statistically significant (OR = 0.84 95% CI 0.66–1.07; p = 0.17; I2 = 89%).
Resuscitation was attempted by paramedics in six studies in a total of 3182/6415 patients (49.6%) before the pandemic and 5053/9399 patients (53.8%) during the pandemic (p < 0.001).3, 10, 11, 15, 16, 17 While there was no difference in the number of arrests who had resuscitation attempted in the two timeframes (OR = 1.19 95% CI 1.00–1.42; p = 0.05; I2 = 73%), only one study reported an increase in frequency of resuscitation attempts during the pandemic (Fig. 3d).3
ROSC (Fig. 3e) was achieved in eight studies in a total of 3130/17751 patients (17.6%) before the pandemic and 1203/7091 patients (17.0%) during the pandemic (p = 0.22).3, 10, 11, 12, 14, 15, 17 , 18 ROSC occurred more frequently before the pandemic (OR = 1.63 95% CI 1.18–2.26; p = 0.003; I2 = 90%).
OHCA (Fig. 3f) due to shockable rhythm or shocked events was reported in seven studies in a total of 1349/6773 patients (19.9%) before the pandemic and 432/3973 patients (10.9%) during the pandemic (p < 0.001).3, 10, 11, 13 , 17, 18 Shockable rhythm or shocked events occurred more frequently before the pandemic (OR = 1.57 95% CI 1.17–2.09; p = 0.002; I2 = 78%).
There were more OHCA occurring at home during the pandemic (Fig. 3g). Across six studies, 4837/6645 OHCA occurred at home before the pandemic (72.8%) compared to 1997/2376 arrests (84.0%) during the pandemic (p < 0.001).10, 11, 13, 14 , 17, 18 OHCA more frequently occurred at home during the pandemic (OR = 0.51 95% CI 0.40−0.66; p < 0.0001; I2 = 68%).
Airway management differed before and during the pandemic as reported in four studies.3, 11, 12, 14 More patients were intubated before the pandemic (51.5% (5589/10848) versus 47.3% (2533/5352), p < 0.001; OR = 1.87, 95% CI 1.12–3.13; p = 0.02; I2 = 97%) (Fig. 3h). While supraglottic airway was less frequently used before the pandemic (12.5% (1200/9630) versus 31.9% (1584/4972), p < 0.001); OR = 0.36 95% CI 0.27−0.46; p < 0.0001; I2 = 75%) (Fig. 3i).
There was no difference in the use of mechanical CPR devices for OHCA before and during the pandemic, as reported in two studies (14.7% (200/1356) versus 12.5% (65/518); p = 0.24); and did not reach statistical significance (OR = 1.57 95% CI 0.55–4.55; p = 0.40; I2 = 83%) (Fig. 3j).10, 11 Automated external defibrillators (AEDs,) reported in five studies, were used more frequently before the pandemic (12.4% (2046/16516) versus 6.8% (168/2471), p < 0.001; OR = 1.78 95% CI 1.06–2.98; p = 0.03; I2 = 80%) (Fig. 3k).11, 12, 13, 14, 18
Survival to hospital admission, reported in six studies, occurred in 1739/6467 (26.9%) patients before the pandemic and 389/2168 (17.9%) during the pandemic (p < 0.001).10, 11, 13, 14 , 17, 18 Patients were more likely to survive to hospital admission before the pandemic (OR = 1.75 95% CI 1.42–2.17; p=<0.0001; I2 = 57%) (Fig. 3l). Similarly, survival to hospital discharge occurred in 551/6556 (8.4%) of patients before the pandemic and 141/2207 patients (6.4%) during the pandemic (p = 0.002), demonstrating that survival to hospital discharge occurred more frequently before the pandemic (OR = 1.65 95% CI 1.28–2.12; p < 0.001; I2 = 30%) (Fig. 3m).10, 11, 13, 14 , 17, 18
Discussion
Across the selected studies, we observed a more than two-fold increase in OHCA incidence during the COVID-19 pandemic, with an overall significant increase in mortality. Our analysis found several disruptions to the chain of survival in OHCA victims during the pandemic and this may have at least in part contributed to the outcomes seen. There was reduced bystander CPR and AED use, along with increased supraglottic airway management by paramedic personnel. Also, time from call to ambulance arrival was longer during the pandemic.
The majority of OHCA was attributed to medical causes and was more frequently the reason for arrest. Public health measures may have role in reduction seen in the incidence of non-medical causes for OHCA. This is potentially due to a complex interplay of heightened financial difficulties, social isolation, uncertainty about the future, redistribution of the health workforce and the disruption to clinical services due to the pandemic-related lockdown, resulting in a delay in receiving care.19, 20 There was not only a substantial reduction in the use of pre-hospital services to transport STEMI patients to hospitals,10 but also a significant reduction in cardiology admissions21 and STEMI activations22 in 2020. Conversely, trauma causes of OHCA were less frequently observed, which is consistent with national lockdowns restricting mass gathering recreational and sporting events.23 This may have also resulted in reduced road traffic accidents.24
Despite most OHCA events occurring at home, a higher frequency of unwitnessed OHCA was observed. This may be explained by strict self-quarantine measures adopted, resulting in vulnerable populations such as the elderly being isolated from family members who would otherwise visit frequently. With “stay home” measures, it is unsurprising that significantly more cardiac arrests occurred at home, where quarantine isolation may have enforced living in different areas at home or different houses from family members.10 It could be postulated that although OHCA events occurred at home where family may be present, they may be less likely to commence CPR due to psychological and emotional effects of the sudden event.25
Bystander CPR was more frequent before the pandemic. While there is an ongoing fear of contracting COVID-19 during CPR administration,26 limited evidence exists surrounding the transmission of infection from patient to rescuer.27 Although likely underreporting and/or identification of SARS-CoV-2 virus, the overall low prevalence of confirmed COVID-19 cases among OHCA during the pandemic suggests that any concerns regarding bystander CPR may be unwarranted especially in jurisdictions wherein risks of community transmission may be minimal. It should be noted, however, that CPR has the potential to generate aerosols28 and safety of bystanders and pre-hospital healthcare workers is equally important. Community education, advanced healthcare planning and people wearing bands to indicate their wish not to receive CPR may go a long way in promoting dignity and comfort of the person who has suffered an OHCA and who has a poor chance of survival even outside a pandemic. During a pandemic it may of even greater relevance when health services are stretched, and an element of risk exists to responders providing CPR and ACLS.
There have been significant practice variations during the pandemic. For instance, there was an increase in use of supraglottic airway which may at least in part driven by risks of endotracheal intubation. The international liaison committee on resuscitation (ILCOR) recommends the use of supraglottic airways as first line for adults with OHCA (weak recommendation, very low certainty of evidence). However, the aerosol risks of supraglottic airway use when resuscitating patients with COVID-19 remian unclear anda supraglottic airway may potentially cause a false sense of security among healthcare providers.28, 29, 30 Similarly, although ILCOR recommends the use of mechanical chest compression devices (weak recommendation, very low certainty of evidence), it is interesting to note that there was no difference in the use of mechanical CPR devices during the pandemic.28
Interestingly, the frequency of a shockable rhythm/shocked events and ROSC was higher before the pandemic. This may reflect disruptions in the chain of survival, where the probability of ROSC diminishes significantly with time and it is unclear whether increased non-shockable rhythm is a consequence of delayed response or underlying pathophysiology.31 Additionally, this may be related to the delay from call to ambulance arrival that is observed in this study. The quantitative increase in OHCA calls and the need to properly apply personal protective equipment and disinfect ambulances between calls likely contributed to the delay in response and regrettably contributed to the observed increase in OHCA mortality.10 This may also be compounded by the increased frequency of unwitnessed OHCA and reduction in bystander CPR. As a result, patients may be found long after cardiac arrest where they may no longer be in a shockable rhythm.
The absolute increase in OHCA incidence and corresponding rise in mortality was reported in our analysis. Direct COVID-19 deaths would account for a proportion of these deaths,3, 13 while indirect factors such as lockdown and behavioral changes for fear of infection or reluctance to burden health systems may have resulted in delays in presenting to hospital.10, 13 Worldwide, a decrease in acute hospital presentations have been observed, with reports of reduced ST-elevation myocardial infarction presentations in Spain, Italy and USA.32 Emergency department presentations have also decreased following the implementation of lockdown measures in the UK, Germany and USA.33, 34 Emergency medicine services may also be overwhelmed with the surge in OHCA calls, resulting in a strain in pre-hospital services.15
There are several limitations that need to be acknowledged. Firstly, most of the included studies were from the early phase of the pandemic from countries that were significantly affected and had little time to prepare. Moreover, some degree of lockdown in many of the countries, due to the fear of contracting the virus, which implied that many people continued to avoid health care facilities. Hence the result may still be representative during the pandemic. Secondly, postmortem testing to confirm COVID-19 was not reported, hence the direct causation of COVID-19 infection and OHCA or its indirect association due to unattended comorbid diseases during this pandemic was not readily available. Thirdly, there was limited information about the previous medical history or comorbidities of these OHCA patients. Finally, it would been helpful to map the OHCA event curve against that of the epidemiological pandemic curve (based upon hospital confirmed cases) in each of the reporting areas to observe any correlations between the incidence of COVID-19 and OHCA event rates, however this data was not provided in the studies. This information would be critical in helping systems better prepare for future resurgences in COVID-19 cases.
Conclusion
The incidence and mortality of OHCA during the COVID-19 pandemic was significantly higher as compared to time periods before the pandemic. Multiple factors may have contributed to the increased mortality, including increased time from call to ambulance arrival and the reduced frequency of unwitnessed events, bystander CPR and AED use. There were significant practice changes during the pandemic. Urgent research to improve pre-hospital care during a pandemic is required.
Author contributions
Zheng Jie Lim: This author has conceived the project idea, conducted the systematic review, statistical analysis, assisted with data analysis, wrote the initial drafts of the manuscript, created tables and figures and finalized the manuscript.
Mallikarjuna Reddy: This author has conducted the systematic review, assisted with data analysis, wrote the initial drafts of the manuscript and finalized the manuscript.
Afsana Afroz: This author has conducted the statistical analysis, created the figures and wrote the statistical section in methods.
Baki Billah: This author has conducted the statistical analysis, created the figures and wrote the statistical section in methods.
Kiran Shekar: This author has analyzed the data, edited and critically evaluated the manuscript and finalized the manuscript.
Ashwin Subramaniam: This author has conducted the systematic review, statistical analysis, assisted with data analysis, wrote the initial drafts of the manuscript, created tables and figures and finalized the manuscript.
All authors critically reviewed the manuscript and approved the final version prior to submission.
Funding
No funding sources to declare.
Competing interests
All authors declare no support from any organization for the submitted work, no competing interests with regards to the submitted work
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgements
Prof Shekar acknowledges research support from Metro North Hospital and Health Service. We would like to acknowledge the work of pre-hospital health professionals in providing excellent health care during the COVID-19 pandemic.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.resuscitation.2020.10.025.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.World Health Organisation . 2020. Coronavirus disease (COVID-19) Situation reports. [Google Scholar]
- 2.Baldi E., Sechi G.M., Mare C., et al. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. New England Journal of Medicine. 2020;383:496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lai P.H., Lancet E.A., Weiden M.D., et al. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA cardiology. 2020 doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bossaert L.L. Fibrillation and defibrillation of the heart. Br J Anaesth. 1997;79:203–213. doi: 10.1093/bja/79.2.203. [DOI] [PubMed] [Google Scholar]
- 5.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- 6.2020. Project C-OA. Living Evidence on COVID-19. [Google Scholar]
- 7.Wynants L., Van Calster B., Collins G.S., et al. Prediction models for diagnosis and prognosis of covid-19: systematic review and critical appraisal. BMJ. 2020;369:m1328. doi: 10.1136/bmj.m1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.GA Wells BS, D O’Connell, J Peterson, V Welch, M Losos, P Tugwell. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses.
- 9.Wan X., Wang W., Liu J., Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baldi E., Sechi G.M., Mare C., et al. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. European Heart Journal. 2020 doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ball J., Nehme Z., Bernard S., Stub D., Stephenson M., Smith K. Collateral damage: Hidden impact of the COVID-19 pandemic on the out-of-hospital cardiac arrest system-of-care. Resuscitation. 2020;156:157–163. doi: 10.1016/j.resuscitation.2020.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elmer J., Okubo M., Guyette F.X., Martin-Gill C. Indirect effects of COVID-19 on OHCA in a low prevalence region. Resuscitation. 2020 doi: 10.1016/j.resuscitation.2020.08.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marijon E., Karam N., Jost D., et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. The Lancet Public health. 2020;5:e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosell Ortiz F., Fernández del Valle P., Knox E.C., Jiménez Fábrega X., Navalpotro Pascual J.M., Mateo Rodríguez I., et al. Influence of the Covid-19 pandemic on out-of-hospital cardiac arrest. A Spanish nationwide prospective cohort study. Resuscitation. [DOI] [PMC free article] [PubMed]
- 15.Paoli A., Brischigliaro L., Scquizzato T., Favaretto A., Spagna A. Out-of-hospital cardiac arrest during the COVID-19 pandemic in the Province of Padua, Northeast Italy. Resuscitation. 2020;154:47–49. doi: 10.1016/j.resuscitation.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sayre M.R., Barnard L.M., Counts C.R., et al. Prevalence of COVID-19 in Out-of-Hospital Cardiac Arrest: Implications for Bystander CPR. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.048951. [DOI] [PubMed] [Google Scholar]
- 17.Semeraro F., Gamberini L., Tartaglione M., et al. Out-of-hospital cardiac arrest during the COVID-19 era in Bologna: System response to preserve performances. Resuscitation. 2020;157:1–2. doi: 10.1016/j.resuscitation.2020.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uy-Evanado A., Chugh H.S., Sargsyan A., et al. Out-of-hospital cardiac arrest response and outcomes during the COVID-19 pandemic. JACC: Clinical Electrophysiology. 2020 doi: 10.1016/j.jacep.2020.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim J.U., Majid A., Judge R., et al. Effect of COVID-19 lockdown on alcohol consumption in patients with pre-existing alcohol use disorder. The Lancet Gastroenterology & Hepatology. 2020 doi: 10.1016/S2468-1253(20)30251-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adam S., Zahra S.A., Chor C.Y.T., Khare Y., Harky A. COVID-19 pandemic and its impact on service provision: a cardiology prospect. Acta Cardiologica. 2020:1–8. doi: 10.1080/00015385.2020.1787636. [DOI] [PubMed] [Google Scholar]
- 21.Negreira Caamaño M., Piqueras Flores J., Mateo Gómez C. Impact of COVID-19 pandemic in cardiology admissions. Medicina clinica (English ed). 2020;155:179–180. doi: 10.1016/j.medcle.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garcia S., Albaghdadi M.S., Meraj P.M., et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. Journal of the American College of Cardiology. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mitchell R.D., O’Reilly G., Mitra B., Smit D.V., Miller J.-P., Cameron P.A. Impact of COVID-19 State of Emergency restrictions on presentations to two Victorian emergency departments. Emergency Medicine Australasia.n/a. [DOI] [PMC free article] [PubMed]
- 24.Katrakazas C., Michelaraki E., Sekadakis M., Yannis G. A descriptive analysis of the effect of the COVID-19 pandemic on driving behavior and road safety. Transportation Research Interdisciplinary Perspectives. 2020;7:100186. doi: 10.1016/j.trip.2020.100186. Epub 2020 Aug 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sato N., Matsuyama T., Kitamura T., Hirose Y. Disparities in bystander cardiopulmonary resuscitation performed by a family member and a non-family member. Journal of epidemiology. 2020 doi: 10.2188/jea.JE20200068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scquizzato T., Olasveengen T.M., Ristagno G., Semeraro F. The other side of novel coronavirus outbreak: Fear of performing cardiopulmonary resuscitation. Resuscitation. 2020;150:92–93. doi: 10.1016/j.resuscitation.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Couper K., Taylor-Phillips S., Grove A., et al. COVID-19 in cardiac arrest and infection risk to rescuers: a systematic review. Resuscitation. 2020;151:59–66. doi: 10.1016/j.resuscitation.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perkins G.D., Morley P.T., Nolan J.P., et al. International Liaison Committee on Resuscitation: COVID-19 consensus on science, treatment recommendations and task force insights. Resuscitation. 2020;151:145–147. doi: 10.1016/j.resuscitation.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lim W.Y., Wong P. Supraglottic airways in the management of COVID-19 patients. Anaesthesia Critical Care & Pain Medicine. 2020;39:589–590. doi: 10.1016/j.accpm.2020.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sorbello M., Di Giacinto I., Falcetta S., Greif R. Ventilation and airway management during Cardiopulmonary Resuscitation in COVID-19 era. Resuscitation. 2020;153:35–36. doi: 10.1016/j.resuscitation.2020.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Corina de Graaf D.N.V.D., Beesems Stefanie G., Koster Rudolph W. Time to return of spontaneous circulation (ROSC) and survival in out-of-hospital cardiac arrest (OHCA) patients in the Netherlands. Resuscitation. 2018:130. [Google Scholar]
- 32.Kulkarni P., Mahadevappa M. COVID-19 pandemic and the reduction in ST-elevation myocardial infarction admissions. Postgraduate Medical Journal. 2020;96:436–437. doi: 10.1136/postgradmedj-2020-137895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wong L.E., Hawkins J.E., Langness S., Murrell K.L., Iris P., Sammann A. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. New England Journal of Medicine. 2020 [Google Scholar]
- 34.Deerberg-Wittram J., Knothe C. 2020. Do Not Stay at Home: We Are Ready for You: NEJM Catal Innov Care Deliv. May 5. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.