Abstract
Many nursing home design models can have a negative impact on older people and these flaws have been compounded by Coronavirus Disease 2019 and related infection control failures. This article proposes that there is now an urgent need to examine these architectural design models and provide alternative and holistic models that balance infection control and quality of life at multiple spatial scales in existing and proposed settings. Moreover, this article argues that there is a convergence on many fronts between these issues and that certain design models and approaches that improve quality of life, will also benefit infection control, support greater resilience, and in turn improve overall pandemic preparedness.
Keywords: Nursing home design, Covid-19, infection control, quality of life, resilience, pandemic preparedness, health care architecture
Residential care settings for older people are known variously as “nursing homes,” “long-term care facilities,” or “care homes.”1 In general, it is argued that the design of many of these facilities do not adequately support quality of life for older people,2 , 3 and now this is compounded by the COVID-19 pandemic which illustrates how they are ill-designed for infection control and the protection of older people who are most at risk in our society.4 Furthermore, this pandemic has illustrated the importance of space and spatial practices such as social distancing, isolation, or quarantine,5 all of which have immediate and long-term implications for the built environment in terms of planning, urban design, and architecture.6 , 7 This article identifies the urgent need to examine these design models and provide alternative and holistic models that balance infection control and quality of life at multiple spatial scales in existing and proposed settings. The convergence on many fronts between these issues alongside certain design models and approaches that improve quality of life can also benefit infection control, support greater resilience, and in turn improve overall pandemic preparedness.
The Built Environment of Nursing Homes and COVID-19
Built environment issues are of considerable importance in long-term care settings where older residents live in close quarters and often have high levels of impairment and chronic illness, all of which can lead to a greater infection rates and mortality.8, 9, 10 In addition to physical health issues, the built environment of long-term care exacerbates psychosocial and mental health challenges of COVID-19 as a result of quarantine, constrained social interaction, restricted visits from family and friends, the cancellation of shared activities, or the wearing of personal protective equipment by staff.11 , 12 These interventions are particularly difficult for people with a cognitive impairment or a person that walks with purpose, formerly termed “wandering.”4
Finding a Balance and Convergence Among Infection Control, Quality of Life, and Overall Resilience
Although the COVID-19 pandemic has made it apparent that the design or retrofit of long-term care settings will have to tackle many difficult infection control challenges, additional recognition that the convergence between design for infection control and design for improved quality of life can yield an overall resilience is needed. In the following sections we explore these concepts further.
Design for Quality of Life
In a series of studies, nursing home residents describe a range of issues important to their well-being, consistently identifying space and the built environment as factors.
Barney13 argues that community involvement and interaction is critical to quality of life in nursing homes. At the community scale, Rijnaard et al.14 highlight the importance of proximity to a person's home community, contact with a familiar neighborhood, and access to local services or shops for small purchases.
Other major themes identified as important to nursing home residents include generativity, spiritual well-being, homelike environment, and privacy.15 Aspects contributing to thriving in nursing homes challenge the traditional passive perspective of residents and instead emphasize more active aspects.16 These include positive relationships with other residents including visiting each other's rooms, participation in meaningful activities, and opportunities to go outside the residence, including visiting family, organized tours, attending church, or experiencing nature. Qualities of the physical environment includes bright, spacious and private rooms with private bathrooms.
Qualities of the environment are also connected to the well-being of older adults in institutions, linked to 2 main categories including “well-being in public and private spaces” and “lack of well-being in public and private spaces.” Experiences of being together and forming friendships is important for public spaces such as a lounge, whereas peacefulness is fundamental to relaxation and sleep in a resident's private room. Conversely, being excluded from the group in lounge settings can be a source of negative feelings, whereas feelings of incompetence in private spaces such as not being able to use the bathroom can undermine well-being.17
The sense of home experienced by residents is influenced by a number of jointly identified factors, including the building and interior design. Residents and relatives stress the importance of having a connection with nature and the outdoors.18 Important themes contributing to a sense of home include the physical view; mobility and accessibility; and space, place, and the social environment.
A holistic understanding of which features of the built environment are appreciated by the residents can lead to the design and retrofitting of nursing homes that are more in line with personal wishes and can impact positively on the quality of life and the sense of home of nursing home residents.19
Design for Resilience
The term “resilience” is gaining momentum within design professions given increasing environmental uncertainty and the current pandemic events. Hildon et al.20 define resilience as “flourishing despite adversity” and examine the connection between resilience and quality of life for older people. For people with dementia, Christie et al.21 argue that resilience or “adaptation in the face of adversity” is influenced by a person's “protective factors,” including “a sense of connectedness with others,” a “sense of mastery and control,” and “meaning making opportunities.” In this context, the quality of life issues discussed in the previous section have implications for resilience, yet very little attention has been paid to these issues in relation to nursing home design.22
Although current design strategies have been primarily reactive to the context of COVID-19, a prospective approach to improving quality of life through architectural design, which includes maintaining connection to others and an overall focus on health, is a critical part of pandemic preparedness as it strengthens resilience.
From Site Location to Building Details: Design Issues Across Key Spatial Scales
Quality of life and care issues pertain to all aspects of the nursing home built environment (ie, from nursing home location and interaction with the community, down to building details, components, and technology), therefore we adopt a spatial framework spanning macro (overall urban setting), meso (neighborhoods and districts), and micro-scale level issues (site/building design). This multi-scalar approach (Figure 1 ) draws on both urban design23 and geographical gerontology24 and is used to briefly investigate examples of convergence/divergence among quality of life, infection control or pandemic preparedness, and overall resilience of nursing homes. Furthermore, this spatial framework helps understand the issues around the lived experience of older people, community integration, and quality of life in nursing homes; issues that are also critical for resilience.
Fig. 1.

Nursing home design and the macro, meso, and micro spatial scales.
Macro-scale Issues
Proximity to a person's home community
Place attachment and a sense of home are complex issues tied not only to a particular dwelling, but also to the broader community, familiarity, and sense of belonging.25 For instance, a nursing home within a person's community has been shown to have pragmatic benefits (proximity to family), but also a factor in maintaining a sense of self through continuity with a place or community.26 These factors are rarely taken into account, reflected in comments from advocacy groups27 that state that the practice of locating nursing homes outside towns and villages “cuts residents off from community life and social interaction, and isolates those residing in them, thereby lessening their quality of life.” Given the importance that Christie et al.21 ascribe to a “sense of connectedness” for resilience, proximity to a person's home community may be a critical factor in supporting and helping them adapt to adversity.
Although access by family and friends during a pandemic may be an infection risk and has resulted in restricted visiting has been enforced during COVID-19,11 , 12 this cannot be sustained due to the loneliness, anxiety, and sense of loss and besiegement that this creates.28
Integration with health and social care, and emergency services
Mapping local resources and creating service and care pathways among acute care, long-term care, health services, and the local community are critical to the implementation of integrated care for older persons.29 This integration is vital during certain emergency situations, first for evacuating residents of nursing homes to hospitals if required, and second for bringing emergency and medical aid to residents where evacuation is not safe or appropriate.22
Meso-scale Issues
Neighborhood and public realm
Many of the overall neighborhood issues that support quality of life and resilience (eg, public transportation, access to amenities, access and size of open and green spaces23), will also benefit the residents and staff of nursing homes, and family members. For older people in particular, a well-designed public realm with safe, accessible, and attractive pedestrian space is linked to walkability and improved social outcomes.30
Furthermore, if nursing homes are to be more integrated with communities as promoted by certain nursing home models such as the Green House model,31 then the neighborhoods in which they are embedded must be of a certain quality. Indeed, walkable and activity friendly neighborhoods have been shown to have benefits for noncommunicable and infectious diseases by supporting walking and cycling, and by providing local amenity spaces for safe exercise and socialization.32 Urban design that unites quality of life and pandemic resilience is vital. For instance, accessibility for wheelchairs and mobility devices is crucial for many older people and this requires wide footpaths,33 a feature that also supports COVID-19–related social distancing.34
Air quality issues at local community level
Research shows that older people are more vulnerable to both short-term and long-term air pollution.35 Emerging research is also linking poor air quality to higher rates of COVID-19,36 making air quality at a neighborhood scale both a quality of life and resilience issue.
Micro-scale Issues
Care model and overall building configuration
Some of the environmental issues that make nursing homes prone to infection may include the number and density of residents, the numbers of staff and visitors accessing a single building, staff movement between multiple residents rooms, and singular high-traffic communal areas such as dining rooms or living spaces.8 , 9
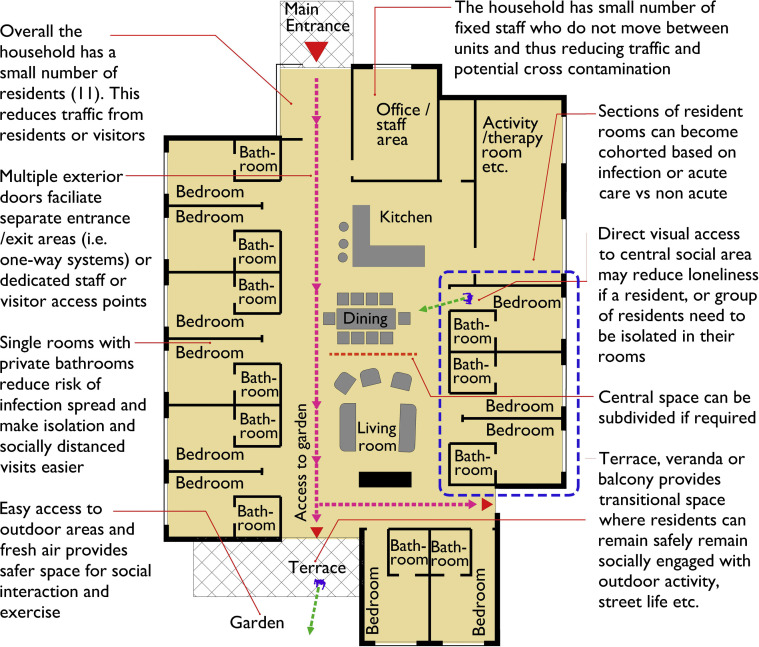
Early research has suggested small settings with fixed staff that minimized entry/re-entry lower COVID-19 infection rates.37 , 38 These studies found that staff were a key source of outbreaks, suggesting that smaller, more autonomous residences with dedicated staff may improve infection control. In this regard, small-scale, homelike settings, known variously as “household” or “green care” models,39 , 40 may prove beneficial. The “Green House”31 model is an example of these households and typically have 10 to 12 residents with private bedrooms and bathrooms and small number of fixed staff (Figure 2 ). The bedrooms surround a central living area and open kitchen and have access to a protected outdoor space.
Fig. 2.
Generic and hypothetical ground floor plan of a household model showing a unit with 11 single rooms with private bathrooms organized around a central communal area and access to a protected outdoor space.
Household models are linked to improved outcomes for residents, staff, and visitors,41 at the same time some aging advocates have promoted household models as a they allow COVID-19 outbreaks to be managed in one household without affecting adjacent or colocated settings.42
Access and internal circulation
The small number of people in a typical “household” setting reduces the amount of human traffic that may consequently reduce infection spread.43
Signage at entrances and on key internal routes instructing people not to enter if they have certain symptoms, advising them about social distancing and hygiene, along with the provision of hand sanitizing facilities is advised.44 Hand sanitizers should also be place in all resident rooms (ideally inside and outside door) and at other key spaces such as common rooms.44
Although not specifically aimed at nursing homes, the American Institute of Architect's (AIA) Re-occupancy Assessment Tool45 contains useful advice, such as the use of one-way traffic flow systems in circulation areas; removing clutter from corridors to increase space for social distancing; the use of separate entrances and exits; or separate staff, resident, and visitor entrances. They also suggest contactless, motion sensor, or automatic operating doors.
Key resident spaces
Private rooms with bathrooms are linked to quality of life in nursing homes,16 improved infection control, and can be used to isolate confirmed or suspected cases of COVID-1946 and to facilitate visitors. The quality of these rooms is important and therefore size, good natural light, and ideally access to a private outdoor space or balcony would improve the experience for the resident, visitor, and staff.
Restricted access to common areas or shared living areas can be isolating for residents and a balance must be struck among social engagement, communal activities, and infection control. This issue pre-dates COVID-19, with Stone et al.47 arguing that “Maximizing quality of life for the resident while minimizing transmission of infections is a known challenge facing NH staff.” Although more research is required in this area, it is useful to consider the advice set out by the AIA45 to change layouts in shared spaces to facilitate social distancing or provide outdoor seating and exterior social areas for occupants and visitors.
Although some nursing homes may need to zone or cohort patients, it is still important to ensure there is safe walking space, especially for residents with a cognitive impairment who may “walk with purpose.”48
Transitional spaces
In addition to the resident room and communal shared spaces, the integration of “intermediate spaces” (ie, porches, alcoves in corridors, and seating placed strategically to allow viewing of the streetscape) supports the activities of viewing, watching, and observing, which have been noted as critical components of nursing home life.49 In an analysis of these transitional spaces, Granger49 notes that they provide visual stimulus through purposeful design, critical for physical and mental health “Even in old age… there is joy, companionship, and spontaneity which, I would add, is facilitated by the material context—the places and porches—that allow the elderly to touch the world beyond.” Although COVID-19 has challenged architects and nursing homes to consider design strategies for minimizing outbreaks in these congregate living facilities, “it is imperative that the social needs of institutionalized seniors are accounted for, both in physical form and in programmatic strategy.”
Outdoor areas and spaces to exercise
Space to exercise, access to nature, exposure to sun, and fresh air are some of the proven benefits of outdoor spaces in nursing homes.50 The outdoors can boost beneficial vitamin D51 for residents and provide an environment that is inhospitable to pathogens through reduced moisture, UV light, and the diluting effects of fresh air and air movement. Early research from Chinese hospitals treating COVID-19 found outdoor hospital spaces had undetectable or very low concentrations of the virus.52 Although more research is required in this area, reviews of previous pandemics argue for the benefits of spending time outdoors.53
Key staff spaces
Although there has been a focus on dedicated staff entrances in the context of this current pandemic, staff must also be provided with adequate changing and hygiene facilities, with the flexibility to segregate these areas further in the setting of pandemic preparedness. Space that can be converted to accommodate staff testing, in addition to a central command center, which might be needed to oversee facilities operations in this context, can also be considered. In addition, we advocate for respite areas for staff members that include access to natural light and nature, given the challenges posed by COVID-19 in the context of mental health.54 , 55
Ventilation and air quality at the building level
Ventilation and air quality are critical to the well-being of older people in nursing homes56 , 57 and are an important infection control issues.58 Increasing air flow through natural and mechanical ventilation within buildings may help dilute and remove the virus, whereas higher relative humidity can be detrimental to viruses.59 Although many heating, ventilation, and air conditioning systems (HVAC) will not have built-in air humidification equipment, these systems may be appropriate in high-risk settings or low humidity regions.
Although most nursing homes may not have airborne infection isolation rooms, Lynch and Goring60 outline a number of steps to adapt a resident rooms with existing HVAC to create a slightly negative-pressure room to reduce the spread of infected airborne droplets to the main facility. This involves installing supplemental exhaust ventilation, upgrading filters, and keeping doors closed to maintain the negative pressure.
The macro, meso, and micro issues identify examples of the overlaps between design for quality of life, infection control/pandemic preparedness, and overall resilience. Examining any new approaches to nursing home design through the lens of quality of life and resilience will help reduce fragility of long-term care and protect against ongoing infectious threats such as influenza or COVID-19, or future pandemics. Table 1 provides an overview of each spatial scale with proposed design solutions for consideration.
Table 1.
Proposed Design Solutions for Nursing Home Design at Various Spatial Scales
| Spatial Scale | Design-Related Problems | Potential Design Solutions |
|---|---|---|
| MACRO (overall urban setting) | ||
| Proximity to home community | Isolation and undermining sense of self, connectedness, and resilience. | Strategic location and integration of nursing homes within existing communities. |
| Integration with health or social care | Disconnection from community health organizations and emergency services. | Strategic planning to integrate nursing homes with existing community services. |
| MESO (neighborhoods and districts) | ||
| Overall neighborhood factors, public realm | Disconnection from, or location within poor-quality neighborhood or public realm. | Age-attuned urbanism that creates walkable, safe, accessible, and attractive neighbors as the nursing home context. |
| Air quality | Poor community or neighborhood air quality. | Local policies to reduced traffic emissions, or improve air quality, the presence/planting of urban trees. |
| MICRO (site/building design) | ||
| Care model and overall building configuration | Large institutional settings that undermine quality of life and increase potential ingress of virus. | Small-scale homelike models that enhance well-being and reduce potential ingress of virus. |
| Access and internal circulation | Large settings with high-traffic levels, singular entrances/exits with high usage and contamination risk, lack of signage or information, lack of social distancing space in corridors. | Smaller settings with dedicated resident/visitor and staff access, contact free doors, generous circulation space and controlled traffic flow. |
| Key resident spaces | Shared rooms and bathrooms, poor-quality rooms, and lack of direct access to outside, infection-related restricted access to shared spaces and isolation. | High-quality single rooms with outdoor spaces, carefully managed shared spaces, provision for transitional spaces, safe walking areas, and access and views to outside. |
| Staff space | Consolidated spaces currently provided (ie, central locker room, centralized care stations). | Decentralized care stations, ability to subdivide staff spaces and provision for respite areas to support mental health. |
| Outdoor areas and spaces to exercise | Lack of access to outdoors and nature, and lack of outdoor exercise areas. | Provision of safe, secure, and easily observed/monitored outdoor space within easy access for all residents. |
| Air quality/ventilation | Poor ventilation and air quality. | Provision of high-quality natural and mechanical ventilation as required, carefully designed/maintained HVAC. |
Implications for Practice, Policy, and Research
Although current gaps exist in the research for residential buildings for older adults and health outcomes, we propose a convergence between design for infection control and design for improved quality of life in order to yield resilience and subsequently, pandemic preparedness.
Although we recognize that issues around cost in the context of retrofitting existing facilities in addition to new construction are an important part of the necessary changes in nursing home living, monetary analysis is outside the scope of this paper. Although cost-effectiveness of using evidence-based design strategies in the acute care setting is well documented,61 further exploration is needed in the area of nursing home design and health outcomes.
The future of residential design for older adults should promote quality of life, social interaction, and engagement, but more importantly foster choice and collaboration with older adults. This culture of resilience and care must occur at various spatial scales and include individual buildings in addition to a broader integration within communities.
Resilient nursing home building design needs to respond to potential vulnerabilities and allow the built environment certain flexibility in the face of changing conditions. Given the impending consequences of infectious outbreaks, it is imperative that health care leaders collaborate with architects and designers to invest in long-term care facility designs for maximum resiliency. Collaboration between the health and design professions can yield design solutions that promote quality of life alongside pandemic preparedness and resiliency.
Footnotes
The authors declare no conflicts of interest.
References
- 1.Sanford A.M., Orrell M., Tolson D. An international definition for “nursing home”. J Am Med Dir Assoc. 2015;16:181–184. doi: 10.1016/j.jamda.2014.12.013. [DOI] [PubMed] [Google Scholar]
- 2.Bradshaw S.A., Playford E.D., Riazi A. Living well in care homes: A systematic review of qualitative studies. Age Ageing. 2012;41:429–440. doi: 10.1093/ageing/afs069. [DOI] [PubMed] [Google Scholar]
- 3.Schwarz B. Nursing home design: A misguided architectural model. J Archit Plann Res. 1997;14:343–359. [Google Scholar]
- 4.Fallon A., Dukelow T., Kennelly S.P., O'Neill D. COVID-19 in nursing homes. QJM. 2020;113:391–392. doi: 10.1093/qjmed/hcaa136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention Social distancing, quarantine, and isolation. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html Available at:
- 6.Wianwright O. Smart lifts, lonely workers, no towers or tourists: Architecture after coronavirus. The Guardian. https://www.theguardian.com/artanddesign/2020/apr/13/smart-lifts-lonely-workers-no-towers-architecture-after-covid-19-coronavirus Available at:
- 7.Giacobbe A. How the COVID-19 pandemic will change the built environment. Architectural Digest. https://www.architecturaldigest.com/story/covid-19-design Available at:
- 8.Barnett M.L., Grabowski D.C. Nursing homes are ground zero for COVID-19 pandemic. American Medical Association. 2020;1:e200369. doi: 10.1001/jamahealthforum.2020.0369. [DOI] [PubMed] [Google Scholar]
- 9.Dosa D., Jump R.L.P., LaPlante K., Gravenstein S. Long-term care facilities and the coronavirus epidemic: Practical guidelines for a population at highest risk. J Am Med Dir Assoc. 2020;21:569–571. doi: 10.1016/j.jamda.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.D'Adamo H., Yoshikawa T., Ouslander J.G. Coronavirus disease 2019 in geriatrics and long-term care: The ABCDs of COVID-19. J Am Geriatr Soc. 2020;68:912–917. doi: 10.1111/jgs.16445. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization Mental health and psychosocial considerations during the COVID-19 outbreak 2020. 2020. file:///C:/Users/greyt/Downloads/WHO-2019-nCoV-MentalHealth-2020.1-eng.pdf Available at:
- 12.World Health Organization Infection prevention and control guidance for long-term care facilities in the context of COVID-19: Interim guidance, 21 March 2020. https://apps.who.int/iris/handle/10665/331490 Available at:
- 13.Barney J.L. Community presence as a key to quality of life in nursing homes. Am J Public Health. 1974;64:265–268. doi: 10.2105/ajph.64.3.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rijnaard M.D., van Hoof J., Janssen B.M. The factors influencing the sense of home in nursing homes: A systematic review from the perspective of residents. J Aging Res. 2016;2016:6143645. doi: 10.1155/2016/6143645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McKinley K., Adler G. Quality of life in nursing homes. J Soc Policy. 2006;4:37–51. [Google Scholar]
- 16.Bergland A., Kirkevold M. Thriving in nursing homes in Norway: Contributing aspects described by residents. Int J Nurs Stud. 2006;43:681–691. doi: 10.1016/j.ijnurstu.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 17.Motteran A., Trifiletti E., Pedrazza M. Well-being and lack of well-being among nursing home residents. Ageing International. 2016;41:150–166. [Google Scholar]
- 18.van Hoof J., Verbeek H., Janssen B.M. A three perspective study of the sense of home of nursing home residents: The views of residents, care professionals and relatives. BMC Geriatr. 2016;16:169. doi: 10.1186/s12877-016-0344-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Hoof J., Verhagen M., Wouters E. Picture your nursing home: Exploring the sense of home of older residents through photography. J Aging Res. 2015;2015:312931. doi: 10.1155/2015/312931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hildon Z., Montgomery S.M., Blane D. Examining resilience of quality of life in the face of health-related and psychosocial adversity at older ages: What is “right” about the way we age? Gerontologist. 2009;50:36–47. doi: 10.1093/geront/gnp067. [DOI] [PubMed] [Google Scholar]
- 21.Christie J., Mitchell W., Marshall M. Jessica Kingsley Publishers; London, England: 2020. Promoting resilience in dementia care: A Person-Centred Framework for Assessment and Support Planning. [Google Scholar]
- 22.Peterson L., Hyer K., Brown L.M. Building resilience in nursing homes in disasters. In: Cefalu C.A., editor. Disaster Preparedness for Seniors: A Comprehensive Guide for Healthcare Professionals. Springer; New York, NY: 2014. pp. 103–117. [Google Scholar]
- 23.Sharifi A., Yamagata Y. Resilient urban form: A conceptual framework. In: Yamagata Y., Sharifi A., editors. Resilience-Oriented Urban Planning: Theoretical and Empirical Insights. Springer International Publishing; New York, NY: 2018. pp. 167–179. [Google Scholar]
- 24.Skinner M.W., Andrews G.J., Cutchin M.P. Routledge; New York, NY: 2017. Geographical Gerontology: Perspectives, Concepts, Approaches. [Google Scholar]
- 25.Wiles J.L., Leibing A., Guberman N. The meaning of “aging in place” to older people. Gerontologist. 2011;52:357–366. doi: 10.1093/geront/gnr098. [DOI] [PubMed] [Google Scholar]
- 26.Reed J., Roskell Payton V., Bond S. The importance of place for older people moving into care homes. Soc Sci Med. 1998;46:859–867. doi: 10.1016/s0277-9536(97)00210-4. [DOI] [PubMed] [Google Scholar]
- 27.Alone. Housing Choices for Older People in Ireland - Time for Action. 2018 http://alone.ie/wp-content/uploads/2018/07/Housing-Choices-for-Older-People-in-Ireland-Time-for-Action-1.pdf Available at: [Google Scholar]
- 28.Trabucchi M., De Leo D. Nursing homes or besieged castles: COVID-19 in northern Italy. Lancet Psychiatry. 2020;7:387–388. doi: 10.1016/S2215-0366(20)30149-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harnett P.J., Kennelly S., Williams P. A 10 step framework to implement integrated care for older persons. Ageing Int. 2020;45:288–304. [Google Scholar]
- 30.Alidoust S., Bosman C., Holden G. Talking while walking: An investigation of perceived neighbourhood walkability and its implications for the social life of older people. J Hous Built Environ. 2018;33:133–150. [Google Scholar]
- 31.Cohen L.W., Zimmerman S., Reed D. The green house model of nursing home care in design and implementation. Health Serv Res. 2016;51(Suppl 1):352–377. doi: 10.1111/1475-6773.12418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Adlakha D., Sallis J.F. Activity-friendly neighbourhoods can benefit non-communicable and infectious diseases. Cities & Health. 2020:1–5. doi: 10.1080/23748834.2020.1783479. Available at: [DOI] [Google Scholar]
- 33.Rosen B. Planning and designing for pedestrians using mobility equipment. Planning News. 2012;38:24. [Google Scholar]
- 34.Polis. COVID-19: Keeping things moving. https://www.polisnetwork.eu/document/covid-19-keeping-things-moving/ Available at:
- 35.Simoni M., Baldacci S., Maio S. Adverse effects of outdoor pollution in the elderly. J Thorac Dis. 2015;7:34–45. doi: 10.3978/j.issn.2072-1439.2014.12.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhu Y., Xie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China. Sci Total Environ. 2020;727:138704. doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abrams H.R., Loomer L., Gandhi A., Grabowski D.C. Characteristics of U.S. nursing homes with COVID-19 cases. J Am Geriatr Soc. 2020;68:1653–1656. doi: 10.1111/jgs.16661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Koshkouei M., Abel L., Pilbeam C. How can pandemic spreads be contained in care homes? https://www.cebm.net/covid-19/how-can-pandemic-spreads-be-contained-in-care-homes/ Available at:
- 39.Cutler L.J., Kane R.A. Post-occupancy evaluation of a transformed nursing home: The first four Green House® settings. J Hous Elderly. 2009;23:304–334. [Google Scholar]
- 40.Schwarz B., Chaudhury H., Tofle R.B. Effect of design interventions on a dementia care setting. Am J Alzheimers Dis Other Demen. 2004;19:172–176. doi: 10.1177/153331750401900304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Verbeek H. Small-scale homelike care in nursing homes. In: Pachana N.A., editor. Encyclopedia of Geropsychology. Springer; Singapore: 2015. pp. 1–6. [Google Scholar]
- 42.Sage Advocacy Sage Advocacy Submission to COVID-19 Nursing Home Expert Panel sage advocacy. https://www.sageadvocacy.ie/news/2020/june/sage-advocacy-submission-to-covid-19-nursing-home-expert-panel Available at:
- 43.Koshkouei A., Abel L., Pilbeam C. 2020. How can pandemic spreads be contained in care homes.https://www.cebm.net/covid-19/how-can-pandemic-spreads-be-contained-in-care-homes/ Available at: Accessed August 19, 2020. [Google Scholar]
- 44.Rios P., Radhakrishnan A., Thomas S.M. Guidelines for preventing respiratory illness in older adults aged 60 years and above living in long-term care: A rapid review of clinical practice guidelines. medRxiv. 2020 [Google Scholar]
- 45.AIA AIA - Re-occupancy Assessment Tool V3.0. 2020. https://www.aia.org/resources/6292441-re-occupancy-assessment-tool Available at: Accessed August 19, 2020.
- 46.European Centre for Disease Prevention and Control Infection prevention and control for COVID-19 in healthcare settings – Fourth update. 2020. https://www.ecdc.europa.eu/en/publications-data/infection-prevention-and-control-and-preparedness-covid-19-healthcare-settings#copy-to-clipboard Available at: Accessed August 19, 2020.
- 47.Stone P.W., Herzig C.T.A., Pogorzelska-Maziarz M. Understanding infection prevention and control in nursing homes: A qualitative study. Geriatr Nurs. 2015;36:267–272. doi: 10.1016/j.gerinurse.2015.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.BGS COVID-19: Managing the COVID-19 pandemic in care homes for older people. https://www.bgs.org.uk/resources/covid-19-managing-the-covid-19-pandemic-in-care-homes Available at:
- 49.Granger W. Viewing, watching, observing: Aging and the architecture of intermediate space. PLATFORM. https://www.platformspace.net/home/viewing-watching-observing-aging-and-the-architecture-of-intermediate-space Available at:
- 50.Bengtsson A., Carlsson G. Outdoor environments at three nursing homes. J Hous Elderly. 2006;19:49–69. [Google Scholar]
- 51.McCartney D., Byrne D. Optimisation of vitamin D status for enhanced immuno-protection against Covid-19. Irish Med J. 2020;113:58. [PubMed] [Google Scholar]
- 52.Liu Y., Ning Z., Chen Y. Aerodynamic characteristics and RNA concentration of SARS-CoV-2 aerosol in Wuhan hospitals during COVID-19 outbreak. bioRxiv. 2020 [Google Scholar]
- 53.Hobday R.A., Cason J.W. The open-air treatment of pandemic influenza. Am J Public Health. 2009;99:S236–S242. doi: 10.2105/AJPH.2008.134627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen Q., Liang M., Li Y. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McGilton K.S., Escrig-Pinol A., Gordon A. Uncovering the devaluation of nursing home staff during COVID-19: Are we fueling the next health care crisis? J Am Med Dir Assoc. 2020;21:962–965. doi: 10.1016/j.jamda.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mendes A., Bonassi S., Aguiar L. Indoor air quality and thermal comfort in elderly care centers. Urban Climate. 2015;14:486–501. [Google Scholar]
- 57.Bentayeb M., Norback D., Bednarek M. Indoor air quality, ventilation and respiratory health in elderly residents living in nursing homes in Europe. Eur Respir J. 2015;45:1228–1238. doi: 10.1183/09031936.00082414. [DOI] [PubMed] [Google Scholar]
- 58.Ulrich R.S., Zimring C., Zhu X. A review of the research literature on evidence-based healthcare design. HERD. 2008;1:61–125. doi: 10.1177/193758670800100306. [DOI] [PubMed] [Google Scholar]
- 59.Dietz L., Horve P.F., Coil D.A. 2019 novel coronavirus (COVID-19) pandemic: Built environment considerations to reduce transmission. mSystems. 2020;5:e00245–e00320. doi: 10.1128/mSystems.00245-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lynch R.M., Goring R. Practical steps to improve air flow in long-term care resident rooms to reduce COVID-19 infection risk. J Am Med Dir Assoc. 2020;21:893–894. doi: 10.1016/j.jamda.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sadler B.L., Berry L.L., Guenther R. Fable Hospital 2.0: The business case for building better health care facilities. Hastings Cent Rep. 2011;41:13–23. doi: 10.1002/j.1552-146x.2011.tb00093.x. [DOI] [PubMed] [Google Scholar]